Going viral test #3
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
Most human viral diseases are caused by…
RNA viruses
Can entire virion (capsid and genome) enter the animal cell?
Yes
Eukaryotic cells contain….
a nucleus, the site of replication for many animal viruses. Leads to additional complexity in where the viral genome goes.
Retroviruses
RNA viruses that convert their RNA genome into DNA
What do retroviruses contain?
a reverse transcriptase (copies information from RNA to DNA)
Example of a retrovirus
Human Immunodeficiency Virus, (HIV) a virus that attacks the immune system and can lead to AIDS.
gag
A protein-coding gene essential for the construction of the viral core in retroviruses.
pol
A gene that encodes for enzymes crucial for viral replication, including reverse transcriptase and integrase.
env
A gene that encodes for the envelope protein, facilitating the virus's entry into host cells.
Covid is not a retrovirus, but…
if you provide reverse transcriptase it will integrate into DNA
reverse transcriptase
an enzyme that converts RNA into DNA, allowing certain viruses to integrate their genetic material into the host genome.
enveloped proteins
proteins that surround the viral RNA or DNA, helping the virus enter host cells.
Viral infection of animal cells: typically used for cell-cell contact or immune function
binding specific host cell receptors
Viral infection of animal cells: different tissues and organs…
express different cell surface proteins, often only infecting specific tissues.
What is needed for Covid-19 entry?
SARS-CoV-2 uses the spike protein to bind to ACE2 receptors on host cells.
There are often many subtypes of cells within…
each system or grouping of tissue. Viruses also need access to these tissues
Examples of combinations of different proteins across multiple tissues
Nasal: goblet/basal/ciliated, lungs: secretory/basal/multi-ciliated
animal (“hosts”) body plans have…
Symmetry. Presence/absence of balanced proportions or correspondence of size and shape on opposite sides of a median plane.
bilateral
divided along the sagittal plane into mirrored halves
How is segmenation controlled?
Hox genes: determine the proper development of different body regions (anterior-posterior axis)
Hox genes are ___ among bilateral animals
homologous
What are hox genes essentially?
a position indicator “GPS” for where along the length of the organism a set of tissues are (front end, middle etc.)
Different hox gene expression produces different ___ patterns in organisms
mix and match. Scientists can use genetic studies to produce their own patterns to better understand how the process works.
Why are there so many different combinations of receptors?
•Many different cell types are required, thus different receptor are needed to make each cell type unique
•Patterning/directing
•Differentiation (stem cells)
•Establishment/proper functioning
Virulent infection
•: lysis of host cell, most common (just like in bacteria)
Latent infection
Viral DNA exists in host genome and virions are not produced; host cell is unharmed unless/until virulence is triggered. Herpes, Epstein-barr, cytomegalovirus, chickenpox
Persistent infections
•Release of virions from host cell by budding does not result in cell lysis. Infected cell remains alive and continues to produce virus. HIV, some herpesvirus members, papovavirus encephalitis
Transforamtion/oncovirus
conversion of normal cell into tumor cell. HPV, RSV
Formation of proviral state and transformation into tumor cell
Transformation: tumor cell division
Lysis: death of the cell and release of the virus
Persistent infection: slow release of the virus without causing cell death
Latent infection: viruses present but not replicating
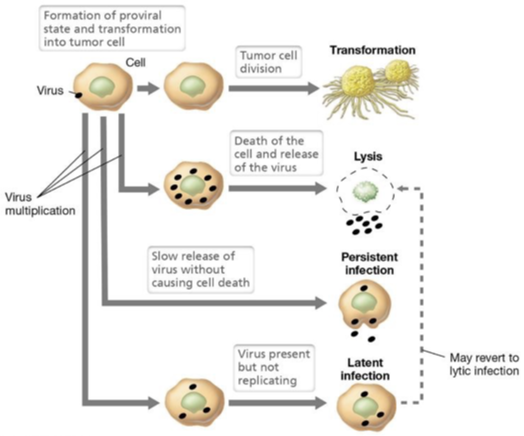
Lysis
the disintegration of a cell by rupture of the cell wall or membrane.
transformation
the process where a cell takes up and incorporates foreign genetic material (DNA) from its environment, leading to a stable genetic change
Lines of defense against viruses: body defences
Innate (nonspecific) and adaptive (specific) Immunity specific resistance to disease
Immune system is a ___ system rather than an organ system in an anatomical sense
functional
Innate (non specific) defence system
•Responds immediately to protect body from all foreign materials
•Includes intact skin, mucous membranes, inflammatory response, various proteins
Adaptive (specific) defence system
•Fights invaders that get past the innate system
•Specific defense is required for each type of invader
•The highly specific resistance to disease is immunity
First line of defence (innate)
skin, mucous membranes, secretions of skin and mucous membranes.
Second line of defence (innate)
Phagocytic cells, natural killer cells, antimicrobial proteins, the inflammatory response, fever
Third line of defence (adaptive)
Lymphocytes, antibodies, macrophages, and other anti-gen presenting cells
Surface membrane barriers
such as the skin (dead) and mucous membranes, provide the 1st line of defence against the invasion of microorganisms
Protective secretions produced by these membranes
1.Acidic skin secretions inhibit bacterial growth
2.Mucus traps microorganisms
3.Gastric juices are acidic and kill pathogens
4.Saliva and tears contain lysozyme (enzyme that destroys bacteria)
Cells and chemicals (2nd kine of defense)
1.Natural killer cells and phagocytes
2.Inflammatory response
3.Fever
4.Chemicals that kill pathogens
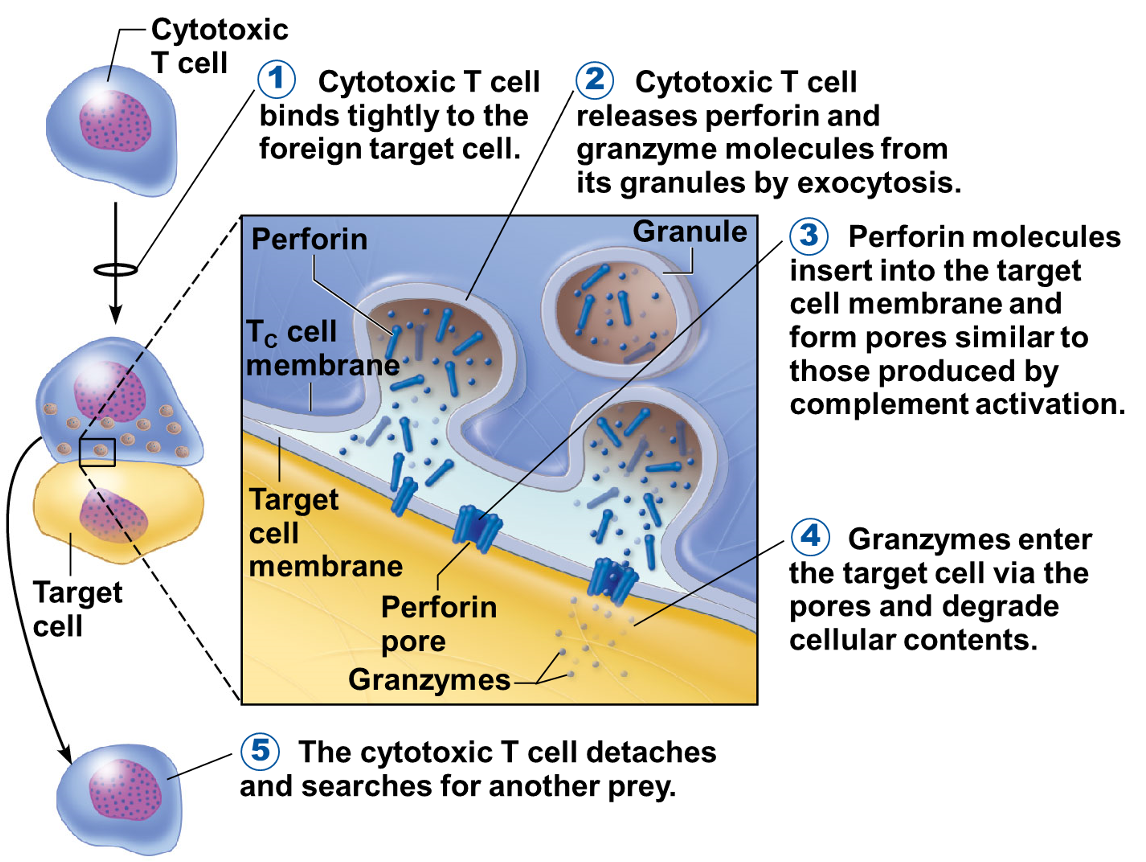
natural killer (NK) cells
•Roam the body in blood and lymph
•Lyse (burst) and kill cancer cells, virus-infected cells, and some other non-specific targets
•Release chemicals called perforin and granzymes to degrade target cell contents
•Release powerful inflammatory chemicals
Inflammatory response
•Triggered when body tissues are injured
•Four most common indicators (cardinal signs) of acute inflammation:
A.Redness
B.Heat
C.Pain
D.Swelling (edema)
Process of the infamitory response step 1
WBC migrate to the area of inflammation by rolling along the vessel wall (following the scent of chemicals from inflammation)
Process of the inflammatory response step 2
WBC squeeze through the capillary walls by diapedesis to sites of inflammation
Process of the inflammatory response step 3
WBC gather in the precise site of tissue injury (positive chemotaxis) and consume any foreign material present
Phagocytes
•Cells such as neutrophils and macrophages engulf foreign material by phagocytosis
•The phagocytic vesicle is fused with a lysosome, and enzymes digest the cell’s contents
What does local heat do to the metabolism?
Speeds and repairs it
Clotting proteins
walls off damaged areas with fibrin
Fever (2nd line of defence)
•Abnormally high body temperature is a systemic response to invasion by microorganisms.
•High temperatures inhibit the release of iron and zinc (needed by bacteria) from the liver and spleen
•Fever also increases the speed of repair processes
How does the hypothalamus help with fevers?
•Hypothalamus regulates body temperature at 37°Celsius (98.6°Fahrenheit)
•The hypothalamus thermostat can be reset higher by pyrogens (secreted by white blood cells)
Antimicrobial proteins (kill pathogens)
•Enhance innate defences by:
•Attacking microorganisms directly
•Hindering reproduction of microorganisms
Most important types of antimicrobial proteins
•Complement proteins (bacterial)
•Interferon (virus)
Complement proteins for bacteria step 1
Activated complement proteins attach to the pathogen’s membrane attack complex (a MAC attack)
Complement proteins for bacteria step 2
MAC pores in the membrane allow water to rush into the cell
Complement proteins for bacteria step 3
influx of water causes cell lysis
Interferons
Serve as a warning system to prevent viral replication by activating antiviral proteins. Small proteins secreted by virus-infected cells.
Can viruses reprogram cells?
•Some viruses can reprogram cells to not release interferons and thus spread more easily in infected tissue
Why do interferons bind to membrane receptors on healthy cell surfaces?
•to activate infection sensing genes (ISG) and growth arrest genes (GAS)
ISG and GAS
interfere with the ability of viruses to multiply
Interferons process
signals neighbouring uninfected cells to destroy RNA and reduce protein synthesis.
Signals neighbouring infected cells to undergo apoptosis
Activates immune cells
Immune response
the immune system’s response to a threat. Most metabolically costly (takes very large resources)
What are antibodies destroyed by?
antigens
Antigen
Any substance that triggers an immune response.
•An antigen is a marker that tells your immune system whether something in your body is harmful or not
•Antigens are found on viruses, bacteria, tumors and normal cells of your body
3 aspects of adaptive defense
antigen specific, systemic, and memory
Antigen specific
the adaptive defence system recognizes and acts against foreign substances - previous lines of defence were nonspecific (ie general)
Systemic
immunity is not restricted to the initial infection site - previous lines of defence were mostly local
Memory
the adaptive defence system recognizes and mounts a stronger attack on previously encountered pathogens - previous lines of defence were not learned from earlier infections
2 arms of the adaptive defence system
humoral immunity = antibody-mediated immunity and cellular immunity = cell-mediated immunity
Humoral immunity = antibody-mediated immunity
•Provided by antibodies present in body fluids (mostly blood)
•B lymphocytes (B cells) produce antibodies and oversee humoral immunity
Cellular immunity = cell-mediated immunity
•Targets virus-infected cells, cancer cells, and cells of foreign grafts
•T lymphocytes (T cells) constitute the cell-mediated arm of the adaptive defences; do not make antibodies
B cell response to infection
•In the initial encounter with an antigen or primary response a free antigen binds to a receptor on a specific B cell
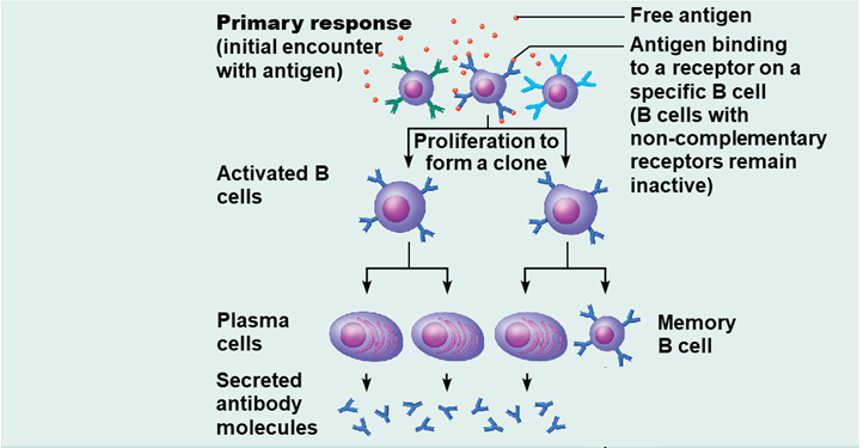
B cells with non-complementary receptors
remain inactive
Activated B cell proliferates to…
form two clones, then one cell becomes two plasma cells that secrete antibody molecules, and one clone cell becomes a plasma cell and a memory B cell
Neutralizing antibodies
are part of the humoral response of the adaptive immune system against viruses, intracellular bacteria and microbial toxin
How do antibodies work?
By binding specifically to surface structures (antigen) on an infectious particle, neutralizing antibodies prevent the particle from interacting with its host cells it might infect and destroy
B cell response to infection
•In the secondary response that can be years later, or additional challenge by same antigen may result in more rapid response, memory B cells that are clones of cells identical to ancestral cells, make multiple plasma cells that secrete antibody molecules and two memory B cells
Primary immune response
•Occurs on first exposure to antigen
•Characteristics
•Lag time of 3–6 days for antibody production
•Peaks at 10–12 days
Secondary immune response
•Occurs on second and subsequent exposure to antigen
•Characteristics
•Lag time is hours
•Peaks in days
•Much more antibody produced
Antigen antibody complex
antigens and antibodies form this. Either inactivities the pathogens or fixes it. It fixes and activates a complement which enhances phagocytosis and inflammation which causes chemotaxis and histamine release and leads to cell lysis
Active immunity
•Occurs when B cells encounter antigens and produce antibodies
•Active immunity can be:
•Naturally acquired during bacterial and viral infections
•Artificially acquired from vaccines
Passive immunity
•Occurs when antibodies are obtained from someone else
•Naturally acquired from a mother to her fetus or in the breast milk
•Artificially acquired from immune serum or gamma globulin (donated antibodies)
•Memory does not occur
Steps for creating antibodies to cure diseases
immunize mouse with antigen
entract B cells from the mouse’s spleen
fuse antibody-producing B cells with cancer cells to produce fast-growing cells
select cells that produce the desired antibody
clone antibody-producing hybridoma cells
grow large numbers of the cells in culture
Main difference between 2 arms of the adaptive response
B cells secrete antibodies, T cells fight antigens directly and bind to free antigens , both use antibodies to recognize infection targets
antigen-presenting cells (APC’s)
•Engulf antigens and then present fragments of them on their own surfaces, where they can be recognized by T cells
•When they present antigens, dendritic cells and macrophages activate T cells, which release chemicals
Different classes of T cells
Helper and cytotoxic
•T cells must recognize nonself and self through…
the process of antigen presentation.
•Non-self the antigen fragment presented by A P C
•Self-coupling with a specific glycoprotein on the A P C’s surface at the same time
When dendritic cells encounter an antigen…
they process it and present an antigen that is identified by the T Cell antigen receptor on a helper cell
Releases cytokines that stimulate helper T cells, cytotoxic killer T cells which cause…
cell mediated immunity by attacks on infected cells, and B cells which enhance humoral immunity by secretion of antibodies on plasma cells.
Cytotoxic (killer). T cells
•Specialize in killing infected cells
•Insert a toxic chemical (perforin or granzyme)
•The perforin enters the foreign cell’s membrane
•Pores now appear in the target cell’s membrane
•Granzymes (protein-digesting enzymes) enter and kill the foreign cell
•Cytotoxic T cell detaches and seeks other targets
How many deaths come from measles in north america
-0.2%, but underdeveloped can be as high as 6% death is a result of respiratory and/or neurological issues (encephalitis)
CDC definition of vaccine
A preparation that is used to stimulate the body’s immune response against diseases.
Not 100% guaranteed to prevent all cases
Reduces severe disease symptoms even if vaccine “fails” to prevent infection
The nature of vaccines
•Most agents used for immunization are either attenuated or inactivated pathogens or inactivated forms of microbial products, such as toxins.
•Newer area of research is in RNA based vaccines
•Allows scientists to custom tune a vaccine for a specific virus rapidly
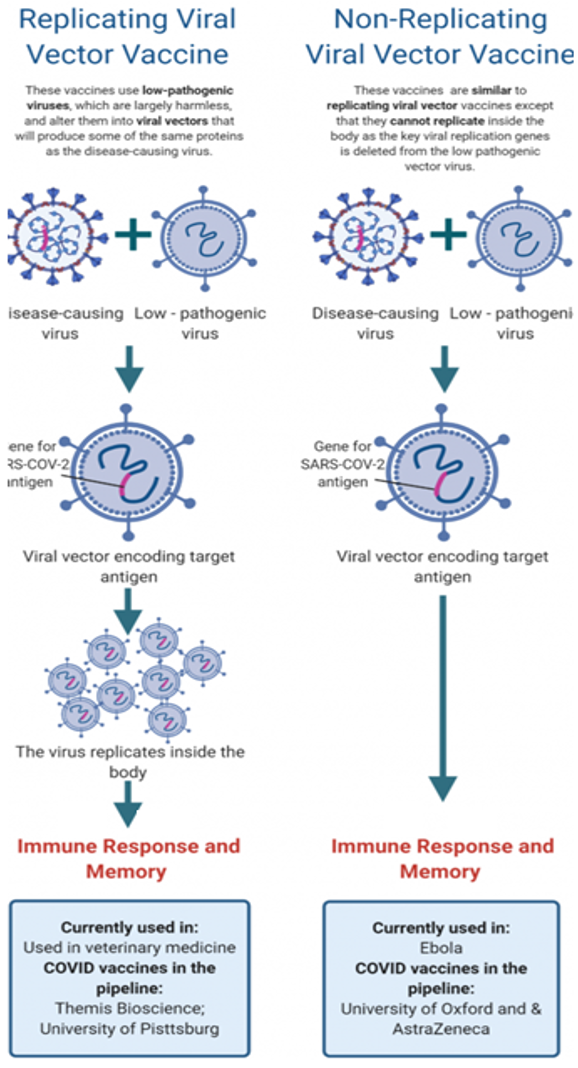
Types of vaccines
1. Live vaccines use a weakened (or attenuated) form of the germ that causes a disease
2.Inactivated vaccines use the killed version of the germ that causes a disease
3. Viral vector vaccines use a modified version of a different virus as a vector to deliver protection
4.Instead of injecting a weakened form of a virus or bacteria into the body as with a traditional vaccine, DNA and RNA vaccines use part of the virus' own genetic code to stimulate an immune response
5.Subunit vaccines are made from a piece of a pathogen, not the whole organism, so they do not contain any live pathogens
DNA and RNA vaccine
Uses DNA or RNA molecules to teach the immune system to target key viral proteins
Advantages: easy and quick to design
Disadvantages: never been done before
Existing examples: none
Group testing this approach for Covid-19: moderna RNA and Inovio (DNA)
Live attenuated
How it works: this is a weakened version of the actual virus
Advantages: stimulates a robust immune response without causing serious disease
Disadvantages: may not be safe for those with compromised immune systems
Existing examples: measles, mumps, rubella
Group testing this approach for Covid-19: codagenix, indian immunologicals Ltd
Inactivated
How it works: an inactivated vaccine uses the whole virus after it has been killed with heat or chemicals
Advantages: safe because the virus is already dead and is easy to make
Disadvantages: not as effective as a live virus. Some previous inactivated vaccines have made the disease worse; safety for the novel coronavirus needs to be shown in clinical trials
Existing examples: polio
Group testing this approach for Covid-19: Sinovac and sinopharm
Subunit
How it works: this vaccine uses a piece of a virus’ surface to focus your immune system on a single target
Advantages: focuses the immune response on the most important part of the virus for protection and cannot cause infection
Disadvantages: may not stimulate a strong response, other chemicals may need to be added to boost long-term immunity
Existing examples: pertussis, hepatitis B, human papiliomavirus (HPV)
Group testing this approach for Covid-19: novavax and adaptVac
Viral vector
How it works: this approach takes a harmless virus and uses it to deliver viral genes to build immunity
Advantages: live viruses tend to elicit stronger immune responses than dead viruses or subunit vaccines
Disadvantages: important to pick a viral vector that is truly safe. An immune response to the viral vector could make the vaccine less effective
Effective examples: ebola and veterinary medicine
Group testing this approach for Covid-19: university of Oxford & AstraZeneca, CanSino Biologics, and Johnson & Johnson
How are vaccines made?
•Food, water and the human body
•Egg based vaccines have been in use since the 1930’s
•Cell based vaccines have been in use since the early 2000’s
•RNA based vaccines have been in use since ~2012