2B - Wound Healing Models
1/108
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
109 Terms
wound that heals in timely fashion
acute wound
slow to heal
“Wound that have failed to proceed through an orderly and timely process to produce an anatomic and function integrity” – Wound Healing Society
chronic wound
Healing rate affected by:
depth, location, cause of wound, patient age, physical condition etc..
medicare says longer than ___ days to be acute
30
_____ phase = 24 – 48 hrs
acute inflammatory → innate
_____ phase = 2-10 days
subacute inflammatory → acquired + innate
_____ phase = 2-20 days
proliferative
_____ phase = 9 days - up to 2 years
remodeling
what is another name for neutrophils?
polymorphonuclear cells
what are the chemical mediators of inflammation?
histamine
leukotrienes
prostaglandins
bradykinin
what are the 3 steps to the inflammatory phase?
Vascular response to injury
Cellular response to injury
Chemical mediators of inflammation
what are the hemostatic mechanisms in the inflammatory stage?
curtail blood flow
reduce oxygen delivery to wound
produces hypoxia
what is the key signal to control wound healing?
HYPOXIA
why is hypoxia a key signal in wound healing?
recruits endothelial cells and facilitates angiogenesis in repair phase
local hypoxia causes what processes?
shift to anaerobic glycolysis
increases lactate production
activates angiogenesis and collagen synthesis
wound space becomes ___ and ___ after hypoxic processes take place
hyperlactive and acidotic
what are the platelets role in vasoconstriction in the inflammatory phase?
first to arrive → activate, adhere, aggregate
release serotonin
release PDGF
what is PDGF? function?
platelet derived growth factor
chemotaxis (calls in) neutrophils and macrophages
purpose of serotonin in wound healing? what releases it?
vasoconstrictor
platelets
what is the purpose of vasoconstriction in the inflammatory response?
seals injured area, delays bacterial invasion
brief arteriolar vasoconstriction to restrict blood flow, followed by ____
vasodilation
what triggers the immune response? (concerning wounds)
damaged tissue
what is mast cell degranulation?
when mast cells release inflammatory substances into circulation
what is the purpose of vasodilation in the inflammatory stage?
release of chemical triggers → histamine, prostaglandins, leukotrienes
opens microvascular beds
opening of microvascular beds allow what to happen?
Increased heat, redness, cellular mediators
Increased intravascular pressure - early transudate into interstitium
what are the components of the vascular response to injury?
vasoconstriction, followed by vasodilation
what are the polymorphonuclear leucocytes from the blood included in the cellular response?
neutrophils
eosinophils
basophils
mast cells
neutrophils proliferate in what type of environment?
hypoxic acidotic environment
neutrophils produce ____ to fight bacteria
superoxide
neutrophils mostly are phagocytic of what type of cell?
granulocytes
neutrophils secrete ____ and ____ to hydrolyze necrotic tissue
proteases; collagenases
accumulation of dead neutrophils that have phagocytized debris in wound
pus
T/F Neutrophils have a short lifespan
true
at what stage does pus come from the wound?
inflammatory → cellular response
function of eosinophils in the cellular response of the inflammatory phase
modulate allergic inflammatory response, kill parasites
function of basophils in the cellular response of the inflammatory phase
Release histamine & heparin
function of mast cells in the cellular response of the inflammatory phase
chemotactic factor for leucocytes and macrophages
release histamine
release heparin which stimulates migration of endothelial cells
heparin also accelerates the activity of leukocyte phagocytosis
function of neutrophils in the cellular response of the inflammatory phase
proliferate in hypoxic acidotic environment
most phagocytic of granulocytes
Produce superoxide to fight bacteria
Secrete proteases and collagenases to hydrolyze necrotic tissue
Wound pours forth pus
Short lifespan
the release of heparin stimulates the migration of ____ cells
endothelial cells
difference between endothelial and epithelial cells
epi- barrier on body surfaces and line internal organs
endo- specialized epithelial cell, line the inner surfaces of blood lymphatic vessels
heparin also accelerates the activity of what?
leukocyte phagocytosis
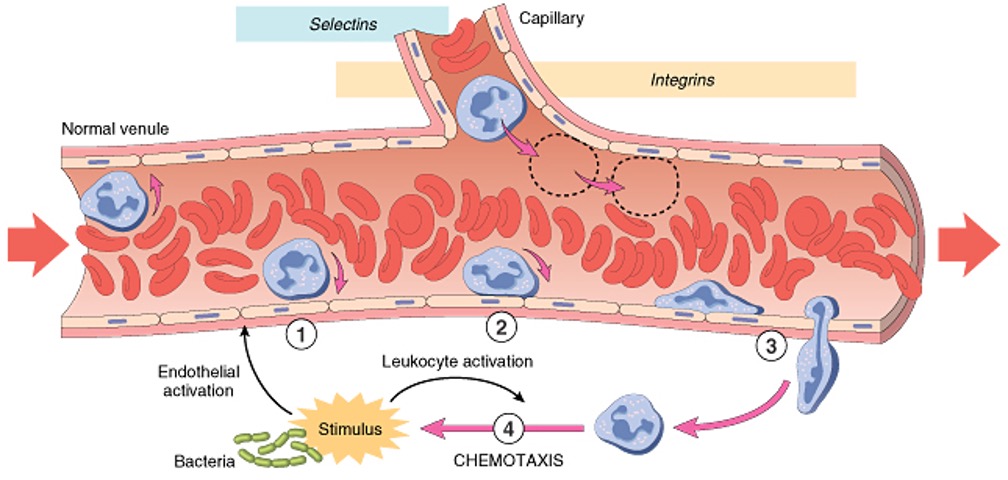
what is the process of leukocyte emigration?
margination and rolling
adhesion
transmigration (diapedesis)
chemotaxis and activation
what is the most important regulatory cell type in the cellular response of the inflammatory stage?
macrophages
function of macrophages in the cellular response of the inflammatory stage?
Differentiate from monocytes when they leave bloodstream
Large phagocytic cell that can ingest large microorganisms & debris
Excretes ascorbic acid, hydrogen peroxide leading to more macrophage recruitment (prolonging inflammatory response)
Tolerate severe hypoxia and acidotic environment
Attracts fibroblasts, endothelial cells and vascular smooth muscle cells
Essential for the transition between inflammatory and repair phases
macrophages differentiate from _____ when they leave the _____
monocytes; bloodstream
Large phagocytic cell that can ingest large microorganisms & debris
Essential for the transition between inflammatory and repair phases
Transcend all phases of wound healing
macrophages
macrophages excretes ____ ___ and _____ ____ leading to more macrophage recruitment → prolonging inflammatory response
ascorbic acid and hydrogen peroxide
macrophages attract what type of cells to the injury site?
fibroblasts, endothelial cells, and vascular smooth muscle cells
what is AGF?
angiogenesis growth factor
what does AGF do?
stimulates budding of endothelial cells from damaged blood vessels
macrophages are chemotactic for ____ during late stages of inflammatory phase
fibroblasts
M2 microphages can activate what type of cells?
FAP = fibro-adipogenic progenitor cell
what lymphocytes are released in the cellular response of the inflammatory stage?
B & T Lymphocytes
Helper B cells
Suppressor B cells
lymphocytes are part of the ___ immune response
acquired
why are lymphocytes up-regulated so late?
because the lymph system is super slow
increased blood flow
rubor
fluid accumulation (plasma protein and blood cells)
tumor
increased blood flow to superficial tissues, histamine release
calor
chemical mediators, nerve compression? (pain is normal response)
Dolor
Functio laesa
loss of function, becomes very severe
Should you try to prevent acute or chronic inflammation?
want acute to start the process → enflamed tissue activates healing
do not want chronic to delay process → won’t let you move into the proliferative phase
what are the 3 steps of the proliferative phase?
Re-enforcement of injured tissue (fibroplasia)
Blood Supply (neovascularization)
Permeability Barrier (re-epithelialization
how do you know you’re in the proliferative phase?
Presence of Fibroplasia → yellow slough
Presence of pink granulation dots → neovascularization
Contraction
Endothelial cells → “white / pink crushed glass”
Most important cell in production of dermal matrix is the fibroblast → stimulated by low O2
fibroblasts
what is in the ECM during the proliferative phase?
Collagen, Fibronectin, Laminin → structural and metabolic support
Elastin → elastic properties
Hyaluronic acid → fibroblast proliferation
Cross-linkage welding together of the collagen matrix produces →
durability and tensile strength
the better the organization & cross-linkage, the better the →
tensile strength of the scar
why is scar tissue mobilization important?
allows for the tissue to return to normal function and not break apart as easily
what vitamin is important for cross-linkage?
vitamin C
Myofibroblasts contain ?
actin & myosin
myofibroblast function in the proliferative phase
Differentiate from fibroblasts
Contract & extend
Draw the edges of the wound together
Influence rate & amount of wound contraction
Proliferative Phase → neovascularization (proud flesh) steps
Angiogenesis (neovascularization)
Endothelial cells respond to AGF
Development of new blood vessels gives bright red appearance (granulation tissue)
pink, soft, granular appearance underneath wounds (fibroblasts and angiogenic tissues in ECM)
Provides matrix upon which epithelial cell migration occurs
What triggers endothelial cells to respond in angiogenesis?
AGFs secreted by macrophages and a hypoxic environment.
what is angiogenesis?
preexisting vessels send out capillary-like sprouts
What is the visual appearance of newly developed blood vessels in granulation tissue?
Bright red due to increased blood supply
How does granulation tissue appear under wounds?
Pink, soft, and granular due to the presence of fibroblasts and angiogenic tissues in the extracellular matrix (ECM).
What is the role of granulation tissue in wound healing?
provides a matrix for epithelial cell migration, aiding in tissue repair and regeneration.
Why does hypoxia stimulate angiogenesis?
low oxygen environment signals the need for new blood vessels to restore oxygen supply.
Proliferative Phase → re-epithelialization steps
Keratinocytes respond to epidermal defect by migrating from wound edges
Superficial wounds heal by reepitheliatlization
Epithelial Islands
Epithelial cells migrate towards center of wounds
Contact inhibition stops migration
Migration is O2 dependent (want high O2 levels)
How do keratinocytes respond to an epidermal defect?
migrate from the wound edges to cover the defect
How do superficial wounds heal?
By re-epithelialization, where new epithelial cells cover the wound
What are epithelial islands?
Clusters of epithelial cells lining skin appendages such as hair follicles and sweat glands, which contribute to wound healing.
in which direction do epithelial cells migrate during wound healing?
Toward the center of the wound.
What stops epithelial cell migration once the wound is covered?
Contact inhibition, where cells stop moving once they touch each other.
What environmental factor is essential for epithelial cell migration?
High oxygen (O₂) levels, as migration is oxygen-dependent.
What are the two migration patterns of keratinocytes during wound healing?
Leapfrog or train fashion, depending on wound depth.
In what type of wound environment do keratinocytes migrate best?
A moist wound environment
What happens when contact inhibition occurs during wound healing?
Migration stops, leading to curled or rolled wound edges
what is the 4 step process of re-epithelialization?
mobilization
migration
proliferation
differentiation
new skin is initially ___% strength of orifinal
15%
when new skin forms, it is ___& of original strength
70-80% → never gets back to 100%
Remodeling phase steps
Fibroblasts disappear
Collagenase
As wound mature collagen lysis increases
Too much O2 causes hypergranulation (synthesis is O2 dependent – lysis is not)
What happens to fibroblasts during the remodeling phase of wound healing?
Fibroblasts disappear as the wound matures.
What enzyme regulates fibroplasia by balancing collagen synthesis and lysis?
Collagenase
What happens to collagen lysis as a wound matures?
Collagen lysis increases to remodel the wound
How does oxygen affect collagen synthesis and lysis?
Collagen synthesis is O₂-dependent, but collagen lysis is not
What is a potential consequence of excessive oxygen levels in wound healing?
Hypergranulation, or excessive granulation tissue formation
Genetic inhibition of lysis, unbalanced synthesis and lysis of collagen
larger than original region of injury
keloid formation
what are the 3 Rs of a hypertrophic scar?
red, rigid, raised → prevents normal movement
what are the long list of causes of chronic inflammation?
Wound sealed by necrotic tissue
Presence of pathogens (critical colonization)
Foreign material that cannot be phagocytized
Inefficient cellular activity
Misuse of cytotoxic agents
Frequent irritation
Repeated trauma
Granuloma (fibroblasts produce large amount of collagen to surround foreign material)