Unseen case revision
1/120
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
121 Terms
What is Erosion??
Chemical means of TSL
Extrinsic - acidic diet
Intrinsic - Diet, bulimia
What is attrition?
Tooth-Tooth contact
Bruxism
Edge to edge contact - Class III
This is shown via flattening
What is Abrasion?
contact other than tooth to tooth
Brushing
tongue piercing
food
What is abfraction?
Flexural forces along the long axis of the tooth
What are the special investigations for toothwear?
Plaque bleeding
OH assessment
Diet analysis - find aetiology
BEWE
Tooth wear index
Clinical photos
Study models
What is the critical pH?
5.5 for enamel
6.2 for cementum
What are the affects of TSL?
Poor aesthetics
Reduced clincial crown height
Yellow teeth
Overclosing - angular cheilitis
Occlusal instability
Loss of function
Pulp inflammation and devitalisation
Difficulty bonding, less enamel
What is important to note in terms of tooth surface loss?
It is multifactorial, ensure that do not tunnel vision on one cause.
What is the tooth wear index?
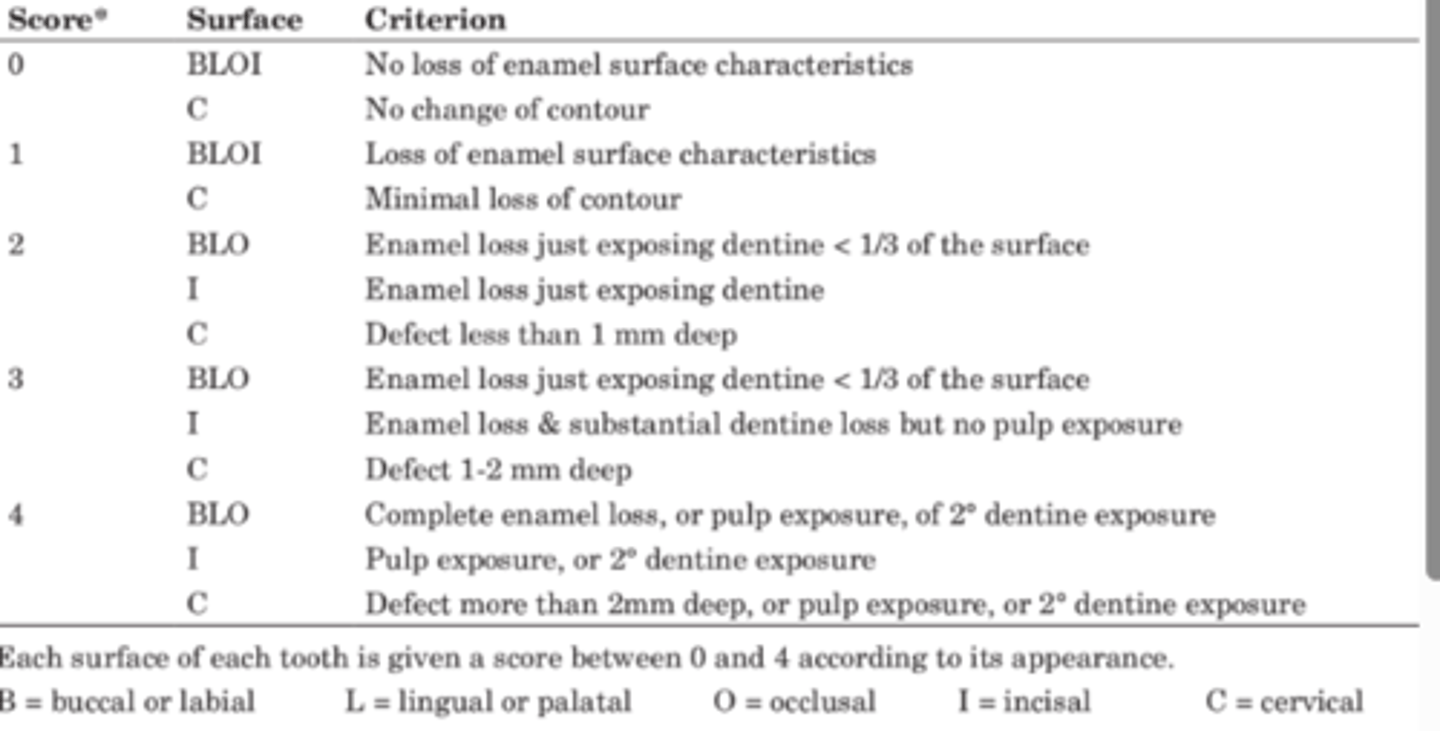
What does the BEWE measure?
Erosion only but DBO says it is used for toothwear as a whole
What is a facebow?
Device that records the relationship of max arch to horizontal axis of rotation of the mandible. (transfers info to articulator)
How to treatment plan? fixed pros / TSL
- Patient expectations?
- Management of the aetiology
- Periodontal stability - Poor prognosis teeth?
- Pulp and periodontal support
- Tooth tissue? - Suitable for certain treatments? Ferrule?
- Occlusion
What is Canine guidance?
When you slide your jaw to the side with upper and lower canines touching, they should "guide" the rear teeth apart - i.e. slide to the side and your molars should separate immediately.
What is group function?
Multiple contact relations between the max and mand teeth in lateral movements on the working side whereby simultaneous contact of several teeth acts as a group to distribute occlusal forces.
What is ICP?
Centric occlusion
Maximum intercuspation, stable reproducible bite
What is retruded contact point?
First point of tooth contact where the mandible is in the most anterior superior position in the glenoid fossa.
What is RVD?
Resting vertical dimension
Relationship of maxilla and mandible at rest
What is Occlusal vertical dimension?
Relationship of maxilla and mandible during occlsion
What is the average free way space?
2-4mm
RVD - OVD
What can an increased FWS indicate and difficult to manage?
Tooth surface loss
Can have TMJ issues where changing the relationship of the jaws
Indications for fixed pros
Heavily broken down teeth
Cracks and fractures
Post RCT
Tooth surface loss
How to determine whether a tooth is restorable?
- Patient expectations?
-Periodontal stability - Poor prognosis teeth?
- Pulp and periodontal support
- Tooth tissue? - Suitable for certain treatments? Ferrule?
- Interocclusal space
+
tooth restorability index
Tooth tissue for restorabiity:
Clinical crown height - Posterior: 3mm
Anterior: 4mm - Crown lengthing, increased height with comoposite
Supra/ subgingival margins
Biological width - Prep no further than 0.5mm subgingival to avoid this area.
Crack
How to determine prognosis of a crack?
Supraginginval - good prognosis to be saved
Subgingival - Poor prognosis as difficult to get coronal seal,. Isolated deep pocket with sub gingival cracks
If crack extends to pulp floor - unrestorable
What are the principles of crown prep?
Retention and resistance form
Structural durability
Preservation of peridontium
Preservation of tooth structure
Marginal integrity
Why not alginate for crown impressions?
Not dimensionally stable
Can distort and become inaccurate
Types of crowns for GIC cements?
PFM, FGC
Types of crowns for RMGIC?
PFM,. Full metal
Types of crowns for resin cement?
All ceramic, PFM, Full metal
Types of crowns for Zinc poly carboxylate cements?
PFM and full metal
Advantages and disadvantages of PFM crown:
Good aesthetics, Stronger than fullc eramic
Disadvantages:
Wear on opposing teeth
Heavy tooth prep
Advantages and disadvantages of Zirconia crown:
Aesthetic
Heavy tooth prep
Wear to opposing teeth
Advantages and disadvatages of lithium disilicate
Best Aesthetic
Heavy tooth prep
Wear to opposing teeth
Advantages and disadvantages of Non-previous metal crown:
Minimal tooth prep
Best mechanical properties
Least wear on opposing teeth
Poor aesthetics
Describe post-core crown:
Root canal must take place
Finish line must finish on natural tooth
Types
Pre-fabricated
Direct cast
Indirect cast
What is a Nayyar Core?
Posts are not viable and extensive coronal tissue
Remove 3-4mm of GP
Pack amalgam or composite. Then crown prep
Ferrule must be present, margins on tooth structure
Advantages of resin retained bridge?
And disadvantages
Fixed
Minimal prep, Minimally invasive
Replace 1 unit
Dependent on occlusion
Poor aesthetics in spaced
Can debond easily
80% survival 10 years
Advatntages and disadvantages of conventional bridge?
Fixed
Can reinforced heavily restored teeth
Significant tooth prep
Irreversible
Potential Devitalisation of pulp
Replace minimal number of teeth
Poor aesthetics in spaced dentition
72% survival 10 years
Advantages and disadvantages of dentures:
Replaces multiple teeth
Aesthetcis
Can alter facial profile
Protect existing teeth
Plaque trap
Removable
Altered temperature and taste detection
Fungal infections
Trauma
Pre denture assessment?
Expectations, concernsm,
Denture history?
Medical history - Xerostomia? Risk of fungal?
Oral hygiene
Ridge shape, Arch shape
Gag reflex?
Lip line - aesthetics
Periodontal support
Occlusion, excursions, and guidance
Interocclusal space
How does kennedy classi 1 & 2 affect denture?
More likely to be unstable due to unbound saddles
How does Cawood and Howell class affect our dentures?
First 4 months post extraction will be the most resorption which will affect the extensions and retention
What are the stress bearing regions in maxillary complete denture?
Palatal rugae
Residual ridge
Maxillaryu tuberosity
What areas need to be relieved in maxillary complete denture?
Frenal attachments
Insive papilla
Mid palatine raphe
What are the support areas of a mandibular complete denture?
Residual ridge
Buccal shelf
Retromolar pad
What are the relief areas of a mandibular complete denture?
Frenal attachments
Mental foramen
Genial tubercle
Mandibular tori
Mylohyoid ridge
Acrylic denture versus Cobalt chrome
Can easily add poor prognosis / lost teeth
Plaque trap can worsen perio
Tissue supported only
Disturbed temperature perception
Cheaper
Less hygiene, weaker and less tolerable
Co/Cr:
Tissue and tooth supported
More difficult to do additions, need to be planned for before construction of denture
Minimal gingival coverage
More hygienic
More expensive
Better tolerance
How do we get retention in dentures?
Clasps and precision attachmemnts
Indirect retention
Guide plans and friction
Well extended flanges within neutral zone
Peripheral seal
Gravity
How do we get support from dentures?
Tooth borne: Rest seats, milled
Mucosa borne
Implant
Where do we get stability in dentures?
Combination of retention and support
Denture instructions at fit:
Show them how to insert and remove
Advise that it can take up to 6 months to adapt to speech, eating and comfort
Remove the denture at night, brush with a soft bristle brush and soap over a basin of water and keep in sterilising solution
Call back with any concerns.
How should I note down the HPC?
See if socrates is answered for the complaint
And write the differentials
Other considerations for History of case: EO/ IO
Limited mouth opening, nocturnal
Bad taste? Systemic unwell, swelling
What questions to ask about epilepsy?
Last fit?
Any triggers?
What sort of symptoms do they have?
Aura?
How do they want to helped during seizure?
Self limiting?
What should I think if they are taking omeprazole or similar?
GORD, reflux
Aetiology of erosion
Questions regarding asthma?
Stable or unstable
When was the last asthma attack?
Any hospitalisations?
Think varnish, colophony
What should we note regarding social history?
Smoking: How long, how many a day. What type? (chewing). Have they tried to quit before
Drinking: How many units a week? 14 is recommended, Lots of alcohols can be erosive
Combined together - oral cancer risk
Stress? Bruxism, occupation
Recreational drug use.
Past dental history?
Regular?
Only attend when in pain?
Anxiety?
Will they be reliable.
Oral hygiene regime
What to note intraorally from the photographs
Swelling
gingival condition
Inflammation
Recession
Potential areas of caries - even if suspiscious, do not sit on fence
Fractures
Discolouration
Pigmentation
Toothwear
Deficient restoration
Colour - with probing can state
What differential periodontal diagnoses are there?
Gingivitis - localised / generalised
Periodontitis - Localised / Generalised / Molar - incisal
If not full mouth IOPA state this for stage and grading
When to take xrays and why?
Bitewings - investigation of caries, overhangs and plaque retentive factors
IOPA - Apical pathology, horizontal bone levels for perio.
OPG: ID canal, developing dentition, gag reflex. Poor for anterior
How to infer prognosis of teeth?
Bone loss - Perio
Is there enough tooth tissue
Root morphology, infection
How does tooth tissue affect prognosis?
Structure for coronal seal? can it support restroation?
Cracks?
Equ/Sub gingival
Into pulp?
Ferrule
Bone levels
Template of treatment planning?
Emergency Phase
Prevention and stabilisation phase
Restorative
Maintenance and recall
Prevention and stabilisation phase?
DOFF
Periodontal disease
On going carious lesions
Parafunctional habits
Restorative phase:
Indirect and direct restorations
Denture work
Endodontic work
Review periods
Periodontal - 6 to 8 weeks for review of charting, plus 2 years radiographs
Endodontic - 1 year post endo for xray and clinical findings
Caries - high risk 3 months, 6 months radiographs
How to get informed consent?
Give the patient every realistic option
Always offer no active treatment
Risks, benefits and costs
Dentine hypersensitivity:
Exposed dentine tubules causes pulpal hyperalgesia
Cause: TSL, Internal bleaching, Gingival recession
Sharp pain, lasts no longer than a few seconds
Manage aetiology, varnish, ohi and diet advice, desensitising agents
Describe Symptomatic apical periodontitis:
Pain on biting - TTP +ve
Easy to localise
Radiograph:
Widening of PDL, Apical radiolucency +/-
Asymptomatic apical periodontis:
Asymptomatic but has an apical radiolucency
Describe acute apical abscess
Rapid onset of severe pain
Extreme tenderness, suppuration, swelling, fever, systemic
Widening of PDL, apical radiolucencyt +/-
RCT. XLA
Describe chronic apical abscess
Typically asymptomatic, sinus tract formation
Foul or metallic taste
Apical radiolucency
Key indicator diagnosing cracked tooth?
Pain on release of biting
How to investigate cracked tooth syndrome?
Transilumination, dye
Tooth sleuth
Sensibility testing
Occlusal assessment
Radiology - can show bone loss
Mobility
Pocketing
What is emergency treatment for cracked teeth?
Occlusal reduction
Composite splint
Orthoband
Keys to an access cavity:
Straight line access
Able to support restoration
convergent walls
No unsupported enamel
How do we assess endo in review?
Abscence from pain, swelling, sinus with no loss of function, evidence.
Is the GP condense suitably
Is the GP 0-2mm away from the apex
No overhangs, good contour
Indications for surgical endodontics
Evidence of apical pathology that cannot be accessed conventionally
Extruded apical material
Persisting pathology following RCT where Re-RCT inapproapriate
Perforation that cannot be accessed via chamber
Types of surgical endo?
Incision and drainage
Apicectomy and curretage
Root hemisection
What are the risk factors for periodontitis?
Poor OH
Smoking
Increased age
Dentures
Pregnancy
Diabetes
Stress
Genetics
Plaque retentive factors
Medication induced gingival englargement
What are the 5 As of smoking:
Ask: Regularly inquire about your patient's smoking status.
Advise: Strongly and clearly advise all smokers to quit for their health.
Assess: Determine their readiness to quit and their stage of change (e.g., precontemplation, contemplation, action).
Assist: Help them quit by providing support, counseling, and potentially medication or other cessation aids.
Arrange: Schedule follow-up appointments to monitor progress and provide ongoing support.
What is the cage questionnaire regarding alcoho?
Every thought about cutting down alcohol consumption
Ever become angry when questionned on alcohol consumption
Ever felt guilt about drinking habits
Eye opener - do you drink first thing in the morning
What is tunnelling surgery?
Reconoturing furcation to allow cleaning with an interdental brush
Degree 3 furcation
What is resective surgery?
gingival and bone contouring to shift the margins apical and produce a healthy sulcus depth
Reduced PPD and improved hygiene
Recession has to be accepted
Single wall defects or class 1 furcation
What is regenerative surgery?
Regeneration of soft and hard tissues
Guided tissue regernation, bone graft and enamel matrix derivative
Two or three sided wall defects or degree 2 furcations
How is asthma relevant to dental appt
Medical emergency
Allergy to colophony with severe asthma contraindicated
Well controlled
Hospitalised?
Steroid inhaler?
What is preventative stages for caries:
Diet, oral hygiene advice
Smoking cessation
Fluoride - 5000ppm, varnish 2-4x a year
What are 3 factors to create an ideal occlusion?
ICP coincident with RCP
Posterior teeth make initial contact
Anterior teeth provide guidance on excursion and protrusion
When is group function preferred over canine guidance?
When you cannot get canine guidance - class 3, AOB, class 2 div 1
Unfavourable canines
short crown:root
Conseuqences of occlusal interfences ?
symptomatical apical periodontitis
TMJ pain.
Cusp fracture
increase mobility
root fracture
What are 5 principles of post and core prep:
Length if post should be longer than height of crown
4-5mm apical GP
At least 2mm of circumferential ferrule
Post no more than 1/3 diameter of root
Post shouldn't exceed diameter of shaped canal
If there is not enough supragingival tooth for crown, what can be done?
Ortho extrusion, crown lengthen, gingevectomy
What splint should be suggested for a bruxism?
Soft splint first line and mild
Hard acrylic full coverage splint the gold standard
When are antibiotics/steroids used in RCTs?
Vital teeth when haemorrhage control is difficult
Acutely inflamed pulp where analgesia cannot occur
Insufficient time for RCT following pulp exposure
What are the requirements for the ferrule effect?
Axial wall = 1.5-2mm above marginal gingivae and 1mm thick
Parallel axial walls
Margins of prep should sit on sound tooth structure
4-5mm of supra bony tooth structure should be available
What are main reasons for RCT failing?
Accessory canals unfilled
Loss of coronal or apical seal
Root fracture
Perforation
Periodontal pathology
Composition of amalgam and what was added to help with corrosion?
Mercury, Silver, Tin, Copper
Copper was added to help
Factors of composite?
Poor compressive strength
Relatively high tensile strength
Good aesthetics
Adhesive bond
Moderate wear resistance
Staining
Polymerisation shrinkage, - increased filler helps
What aspect of the panavia methods bonds to tooth?
MDP bonds to hydroxapatite