MOORES CH.10 CRANIAL NERVES
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
116 Terms
Cranial Nerves
Identify all cranial nerves: olfactory nerve(s), optic nerve and chiasm, oculomotor, trochlear, trigeminal, abducens, facial, vestibulocochlear, glossopharyngeal, vagus, accessory, and hypoglossal nerves including their origin, course (exit from skull), types of fibers, structures which their innervate.
Describe the etiology of the most common clinical cases pertaining to the cranial nerves.
Moore's Clinically Oriented Anatomy
Chapter 10, Summary of Cranial Nerves
OVERVIEW
Like spinal nerves, cranial nerves are bundles of sensory or motor fibers that innervate muscles or glands, carry impulses from sensory receptors, or have a combination of motor and sensory fibers.
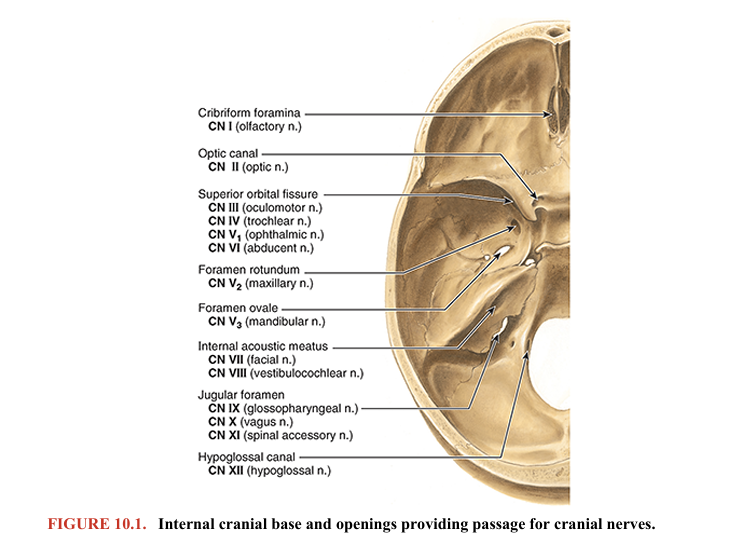
They are called cranial nerves because they emerge from the cranial cavity via foramina or fissures in the cranium (Fig. 10.1) and are covered by tubular sheaths derived from the cranial meninges.
There are 12 pairs of cranial nerves, which are numbered I–XII, from rostral to caudal (Figs. 10.1, 10.2, 10.3, and 10.4). Their names reflect their general distribution or function.
rostral: toward the beak/nose
caudal: toward the tail
how many cranial nerves are there?
12
how is naming done?
naming is done in a rostral (nose) to caudal fashion (tail) fashion.
what do the names reflect?
the general distribution of function
picture of the 12 cranial nerves from rostral to caudal
cribriform foramina (olfactory), most rostral
hypoglossal canal (CN XII)
motor and sensory cranial nerves
2 types of motor cranial nerves (efferent)
sensory cranial nerves (afferent)
Cranial nerves carry one or more of the following five main functional components:
Motor (efferent) fibers (to innervate voluntary (striated muscle) AND to innervate INvoluntary (smooth muscle).
striated muscle means skeletal muscle.
1. Motor fibers to voluntary (striated) muscle. These are somatic motor (general somatic efferent) axons.
On the basis of the embryologic/phylogenetic derivation of certain muscles of the head and neck, some motor fibers conveyed by cranial nerves to striated muscle have traditionally been classified as “special visceral.” When appropriate, these fibers are designated somatic (branchial) motor, referring to the muscle tissue derived from the pharyngeal arches in the embryo (e.g., muscles of mastication).
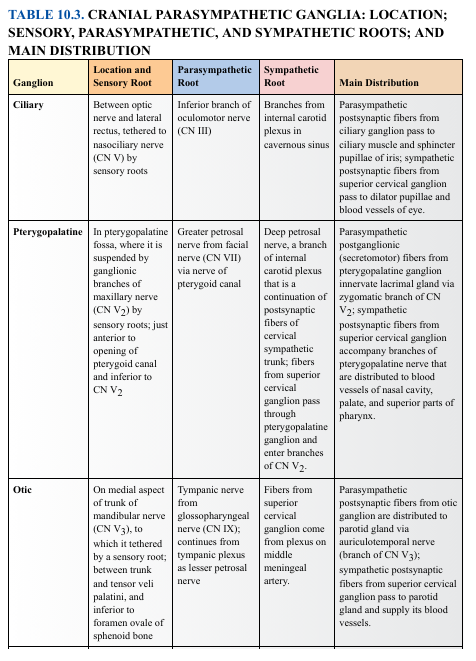
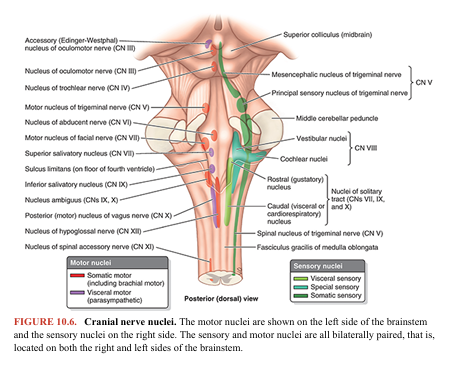
2. Motor fibers involved in innervating involuntary (smooth) muscles or glands. These are visceral motor (general visceral efferent) axons that constitute the cranial outflow of the parasympathetic division of the autonomic nervous system (ANS). The presynaptic (preganglionic) fibers emerge from the brain and synapse outside the central nervous system (CNS) in parasympathetic ganglia (Fig. 10.5; Table 10.3). The postsynaptic (postganglionic) fibers continue to innervate smooth muscles and glands (e.g., the sphincter pupillae and lacrimal gland).
Sensory (afferent) fibers
3. Fibers transmitting general sensation (e.g., touch, pressure, heat, cold) from the skin and mucous membranes. These are somatic sensory (general somatic afferent) fibers, mainly carried not only by CN V but also by CN VII, CN IX, and CN X. 5,7,9,10
4. Fibers conveying sensation from the viscera. These fibers are visceral sensory (general visceral afferent) fibers conveying information from the carotid body and carotid sinus (see Fig. 9.18 in Chapter 9, Neck), pharynx, larynx, trachea, bronchi, lungs, heart, and gastrointestinal tract.
5. Fibers transmitting unique sensations. These include special sensory fibers conveying taste and smell (special visceral afferent fibers) and those serving the special senses of vision, hearing, and balance (special somatic afferent fibers).

TABLE 10.1. CRANIAL NERVES: ATTACHMENT TO CENTRAL NERVOUS SYSTEM, GENERAL FUNCTIONS, AND DISTRIBUTION

olfactory (cranial nerve I)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
olfactory is called cranial nerve I because it’s the most rostral (in the nose)
ole: “to emit a scent.”
factory: '“to make”
“pertaining to the production or perception of smell.”
Prosencephalon | pros = forward + enkephalos = brain | “Forward brain” | It is the forebrain |
Telencephalon | telos = end + enkephalos = brain | “End brain” | Most rostral, final part |
Diencephalon | dia = between + enkephalos = brain | “Between brain” | Sits between telencephalon and midbrain |
-enters the forebrain (fore: front, frontbrain), cerebral hemispheres (telencephon) and diencephalon (between brain)
-general function type: sensory (because the olfactory is smell)
-distribution: olfactory mucosa of nose
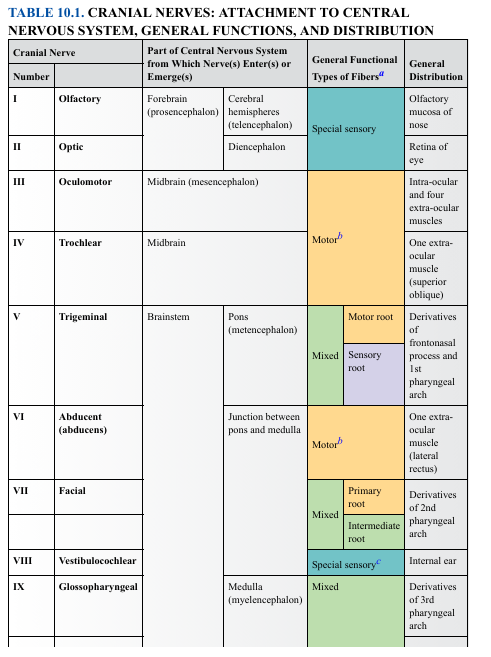
optic nerve (CN II)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
optic nerve is cnII because it’s directly behind the olfactory nerve.
optic nerve and olfactory nerve share the same “part of the nervous system from which nerves enter or emerge.
Term | Greek Roots | Literal Meaning | Why Appropriate |
|---|---|---|---|
Prosencephalon | pros = forward + enkephalos = brain | “Forward brain” | It is the forebrain |
Telencephalon | telos = end + enkephalos = brain | “End brain” | Most rostral, final part |
Diencephalon | dia = between + enkephalos = brain | “Between brain” | Sits between telencephalon and midbrain |
-enters the forebrain (fore: front, frontbrain), cerebral hemispheres (telencephon) and diencephalon (between brain)
-general function type: sensory (because the olfactory is smell)
-distribution: retina of the eye
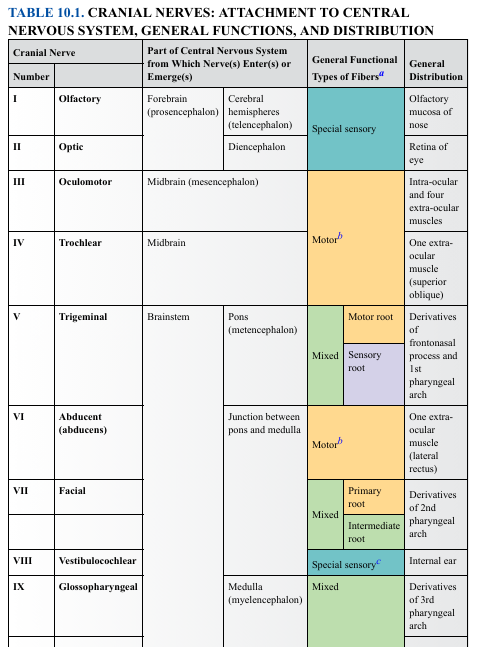
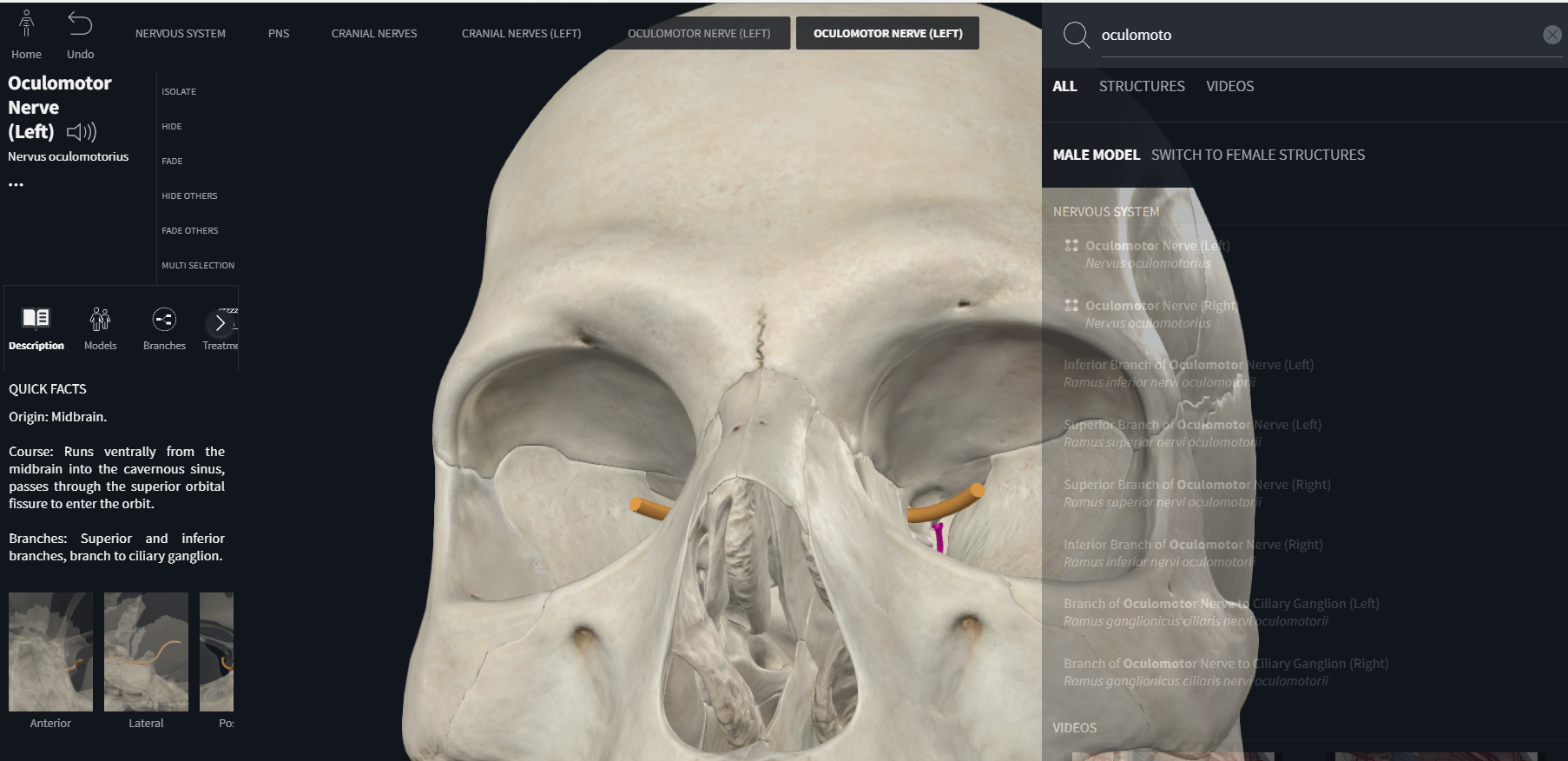
oculomotor (CN III)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
oculo: “eye”
“Motor” = mover / one that causes movement.
Oculomotor = “eye mover.”
The oculomotor nerve supplies motor innervation to:
Four extraocular muscles
superior rectus
inferior rectus
medial rectus
inferior oblique
Part of Central Nervous System from Which Nerve(s) Enter(s) or Emerge(s): midbrain
The oculomotor nerve (CN III) emerges from the midbrain because the neurons that control eye movements and parasympathetic eye functions DEVELOP and RESIDE in the midbrain.
-general function type: motor
general distribution: intra-ocular and four extra-ocular muscles
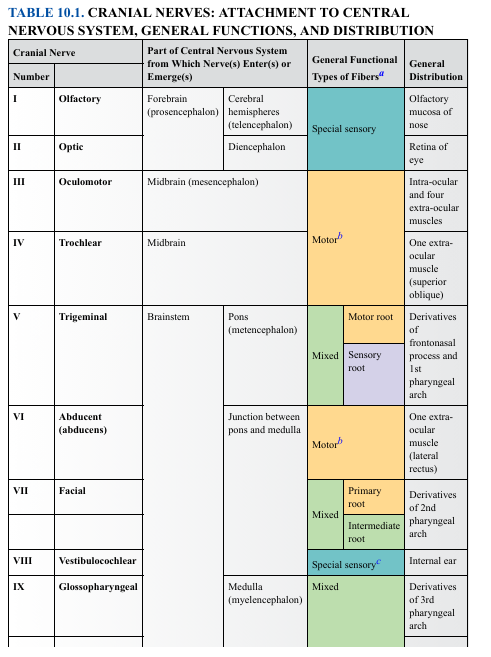
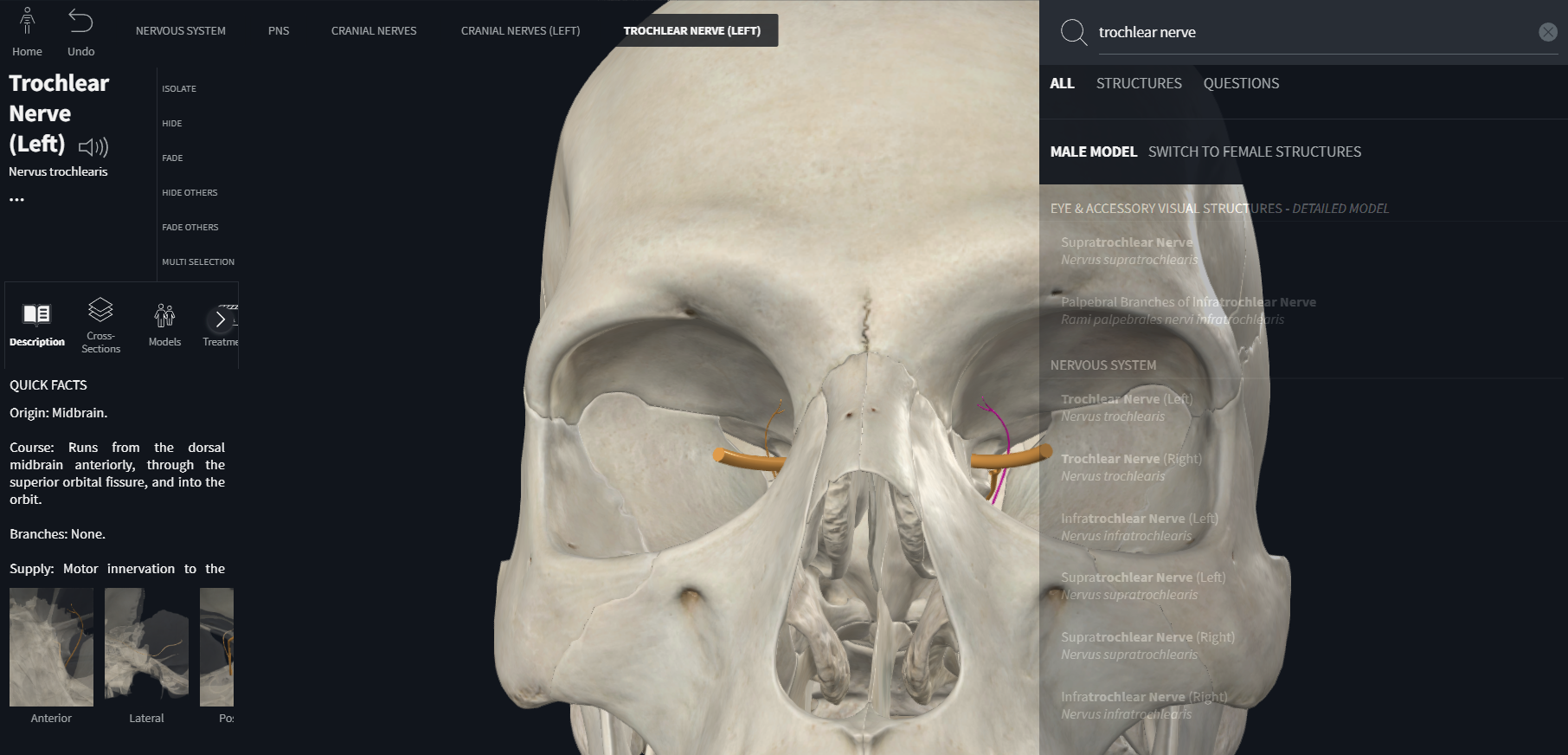
Trochlear (CN IV)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
Part of Central Nervous System from Which Nerve(s) Enter(s) or Emerge(s): Midbrain
General Functional type: motor
“trochlea”: “a pulley, a wheel, or something that rotates.”
The trochlear nerve (CN IV) innervates the superior oblique muscle, which passes through a fibrocartilaginous pulley called the trochlea located on the medial orbital wall.
general distribution: superior oblique

Trigeminal (CN V)
what are the three major divisions of the trigeminal nerve?
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
tri-
= “three”
geminus
= “twin,” “double,” “paired.”
(from Latin gemini = twins)
Trigeminal = “triple twin” or “threefold pair.”
The trigeminal nerve has three major divisions, each occurring on both left and right sides (pairs):
Ophthalmic (V1): sensory
Maxillary (V2): sensory
Mandibular (V3): motor + sensory
opthalmic is greek for “eye”
maxillary is latin for “upper jaw”
mandibular is latin for “lower jaw”
So there are three pairs (“three twins”) of branches.
CRANIAL NERVE V — TRIGEMINAL
Origin: Pons/brainstem
The trigeminal nerve (CN V) originates from the pons because the neurons that carry out ALL of its sensory and motor functions develop in—and are located in—the pontine region of the brainstem.
Function type: Mixed
Distribution:
Motor root: Muscles from the 1st pharyngeal arch (mastication)
Sensory root: Face, orbit, nasal, oral cavities
Why?
V3 innervates chewing muscles (1st arch), while V1–V3 provide sensation to the face.
Abducent (abducens) (VI)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
CRANIAL NERVE VI — ABDUCENT (ABDUCENS)
part of the central nervous system from which nerve enters of emerges: Junction of pons + medulla
Function type: Motor
Distribution: Lateral rectus muscle (abducts the eye)
Why?
Controls outward eye movement.
Facial (VII)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
CRANIAL NERVE VII — FACIAL
Origin: Pons + junction between pons and medulla
Function type: Mixed
Distribution:
Motor (primary root): 2nd pharyngeal arch muscles → facial expression
Sensory (intermediate root): taste (anterior 2/3 tongue), parasympathetics to glands
Why?
VII innervates muscles of facial expression and also provides taste and secretomotor functions.
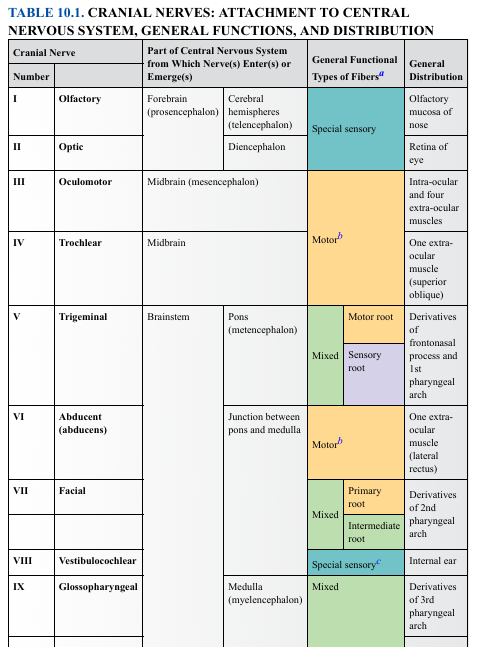
Vestibulocochlear (VIII)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
CRANIAL NERVE VIII — VESTIBULOCOCHLEAR
Vestibulo- = relating to balance / equilibrium structures of the inner ear.
Cochlear = relating to the hearing organ of the inner ear.
Origin: Brainstem + Pons/medulla junction
Function: Special sensory
Distribution: Inner ear (hearing + balance)
Why?
VIII carries auditory and vestibular (balance) information.
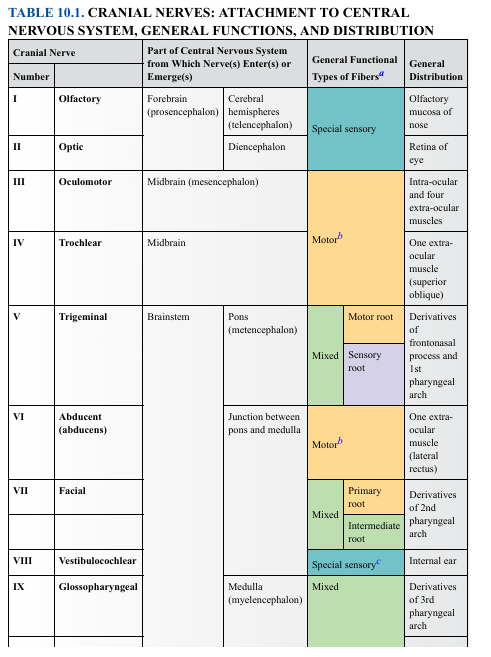
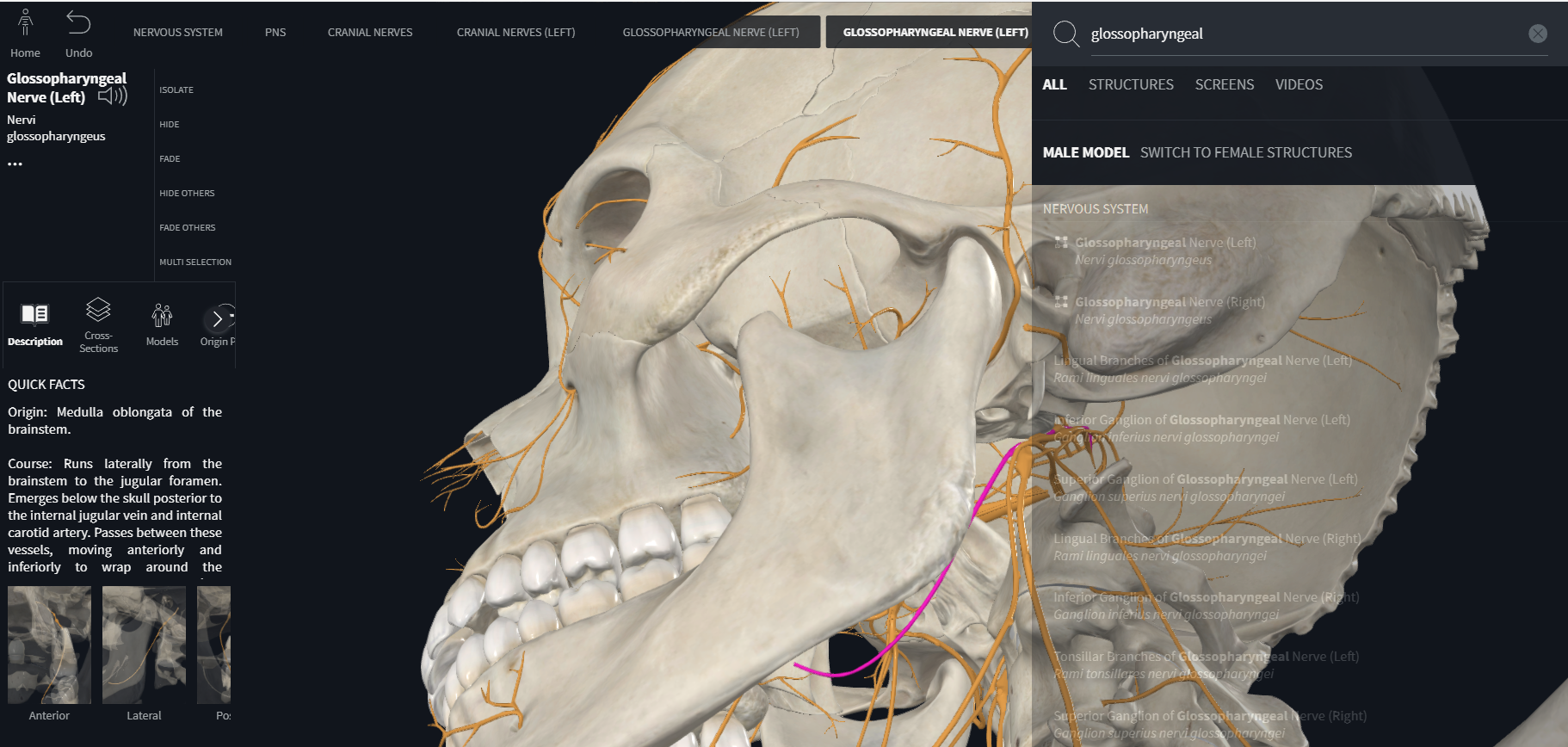
Glossopharyngeal (IX)
CRANIAL NERVE IX — GLOSSOPHARYNGEAL
glosso: “tongue.”
“-pharyngeal”: “throat.”
Origin: Medulla
Function: Mixed
Embryologic origin: 3rd pharyngeal arch
Distribution:
Sensation + taste posterior 1/3 tongue
Carotid sinus/body
Parotid gland
Stylopharyngeus muscle
Why?
IX carries taste, visceral sensation, and innervates a 3rd arch muscle
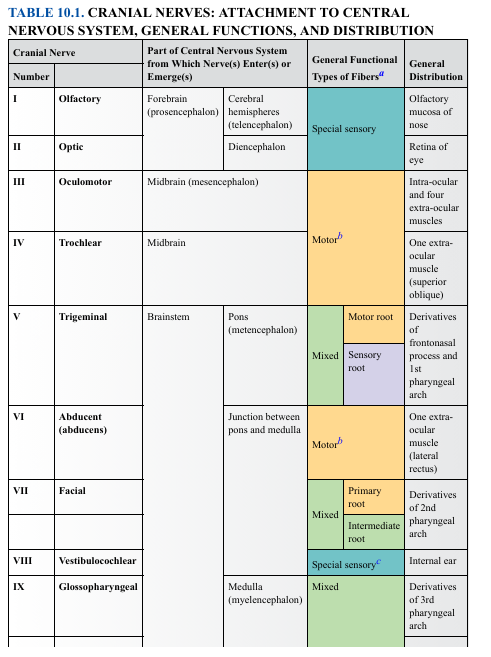
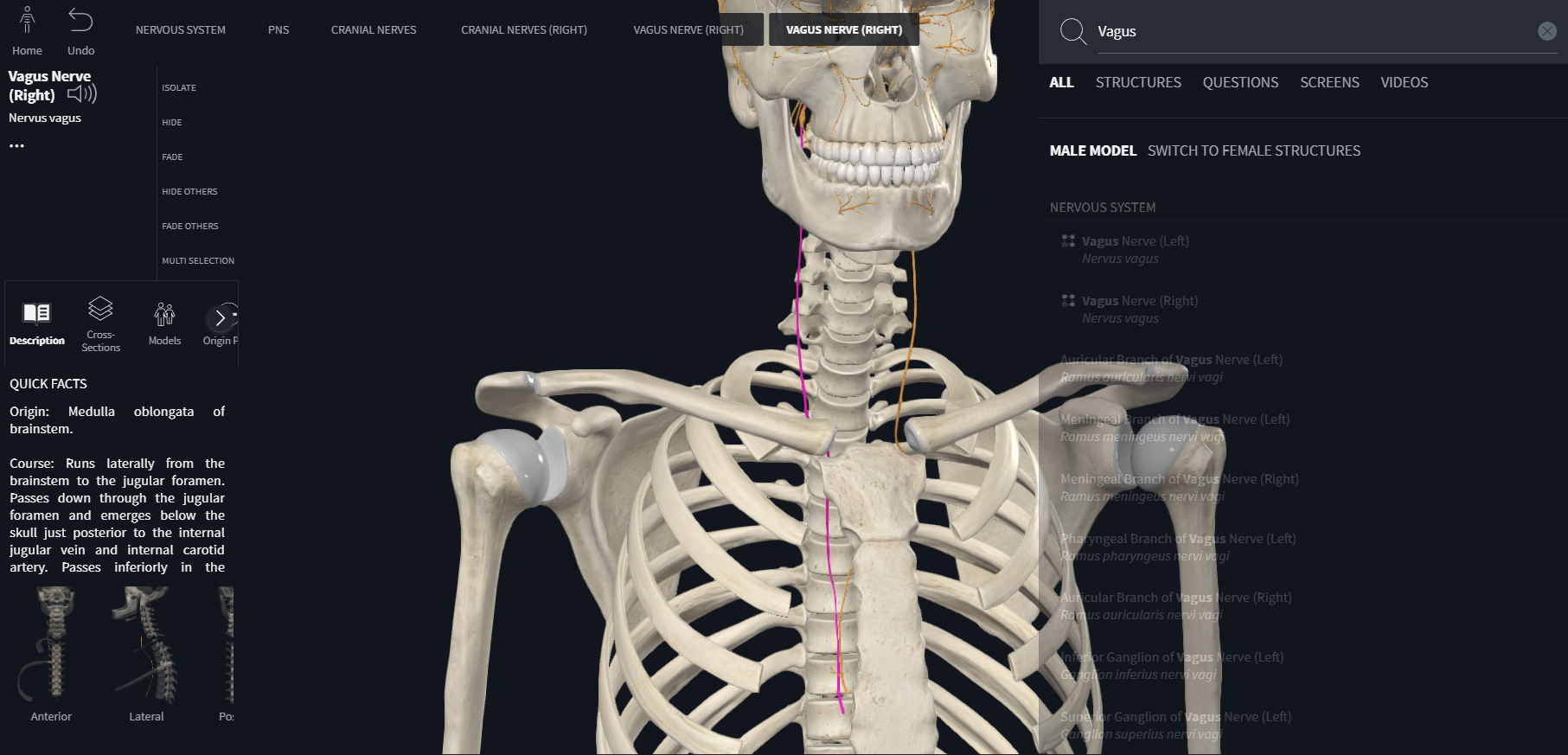
Vagus (X)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
CRANIAL NERVE X — VAGUS
Origin: Medulla
Function: Mixed
Embryologic origin: 4th pharyngeal arch
Distribution:
Pharynx, larynx
Thoracic and abdominal organs
Taste (epiglottis)
Why?
X is the major parasympathetic nerve of the body
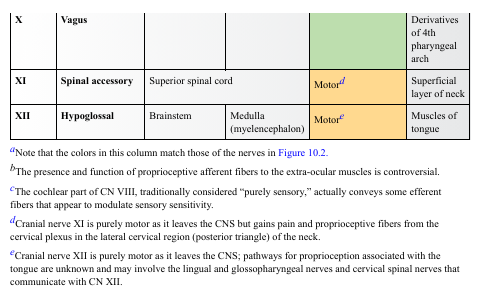
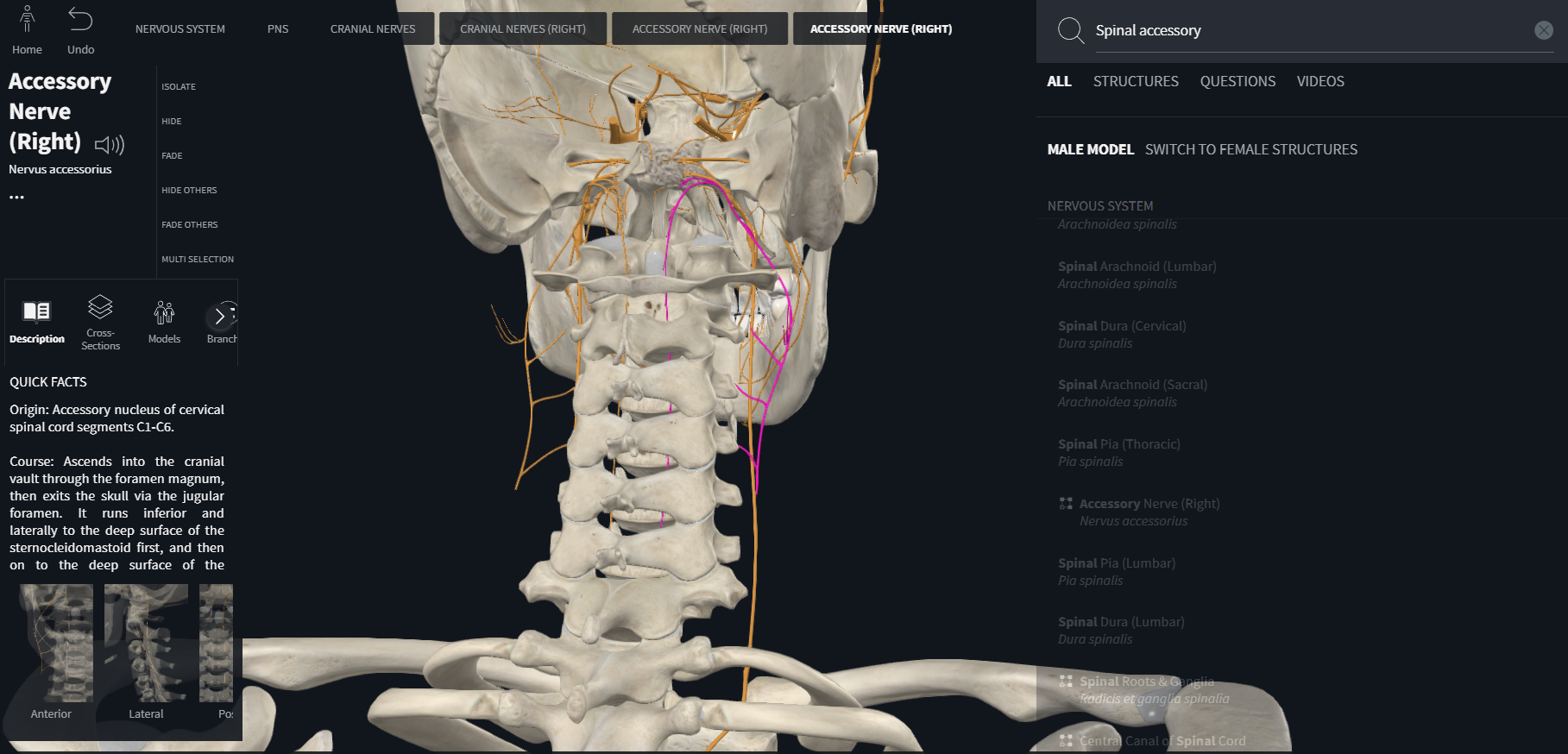
Spinal accessory (XI)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
“spine,” “thorn,” or “backbone.”
accessorius =
“added,” “supplementary,” “serving as a helper.”
CRANIAL NERVE XI — SPINAL ACCESSORY
Origin: Upper spinal cord
Function: Motor
Distribution: Sternocleidomastoid + trapezius
Why?
XI innervates superficial neck muscles responsible for head/shoulder movement.
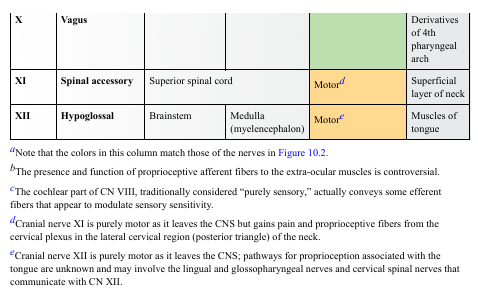
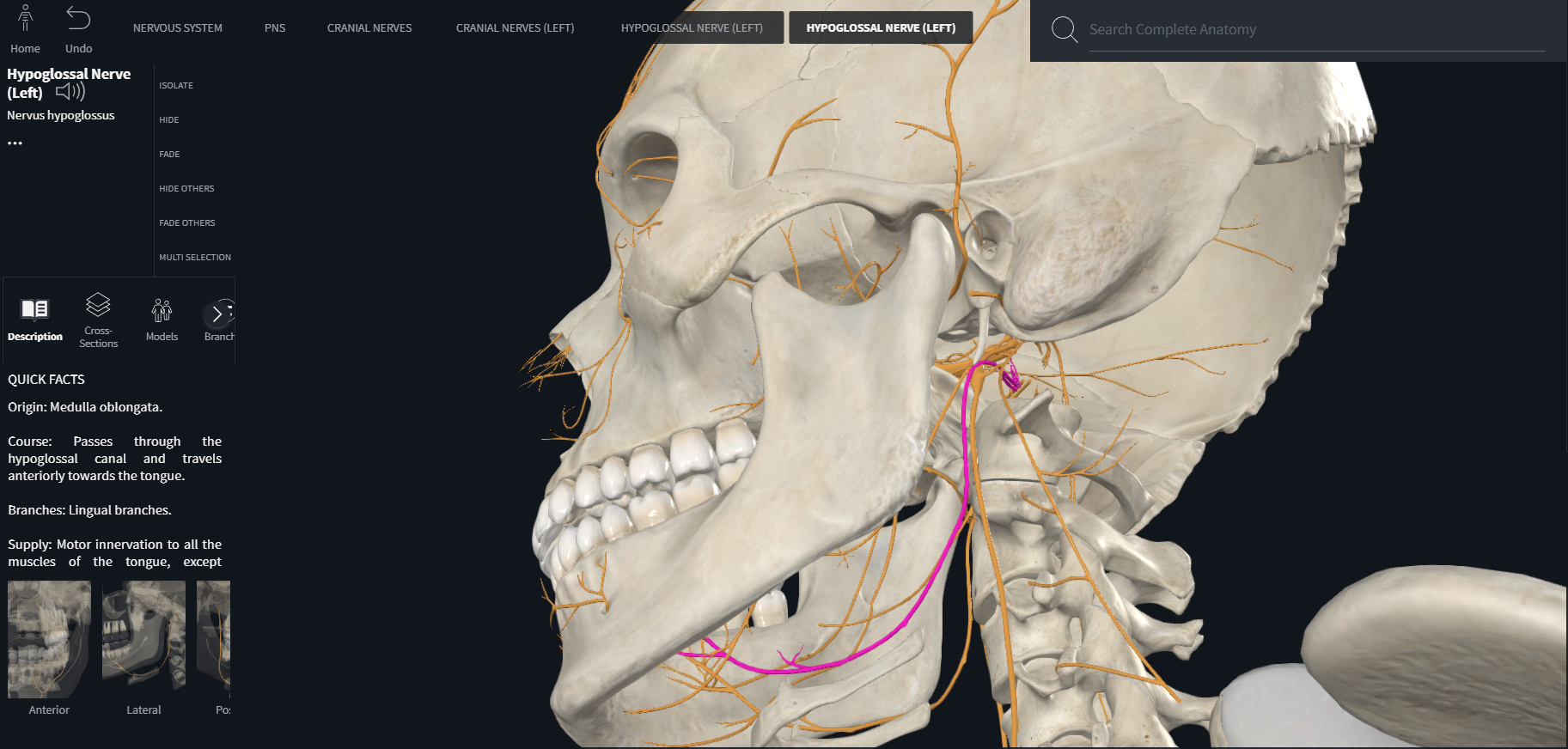
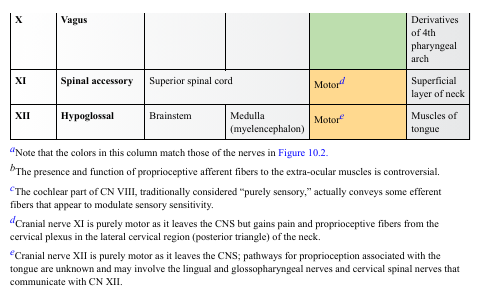
Hypoglossal (XII)
part of central nervous system from which nerve enters or emerges
general function types of fibers
general distribution
CRANIAL NERVE XII — HYPOGLOSSAL
Origin: Medulla
Function: Motor
Distribution: Muscles of the tongue
Why?
XII controls tongue movement needed for speech and swallowing.
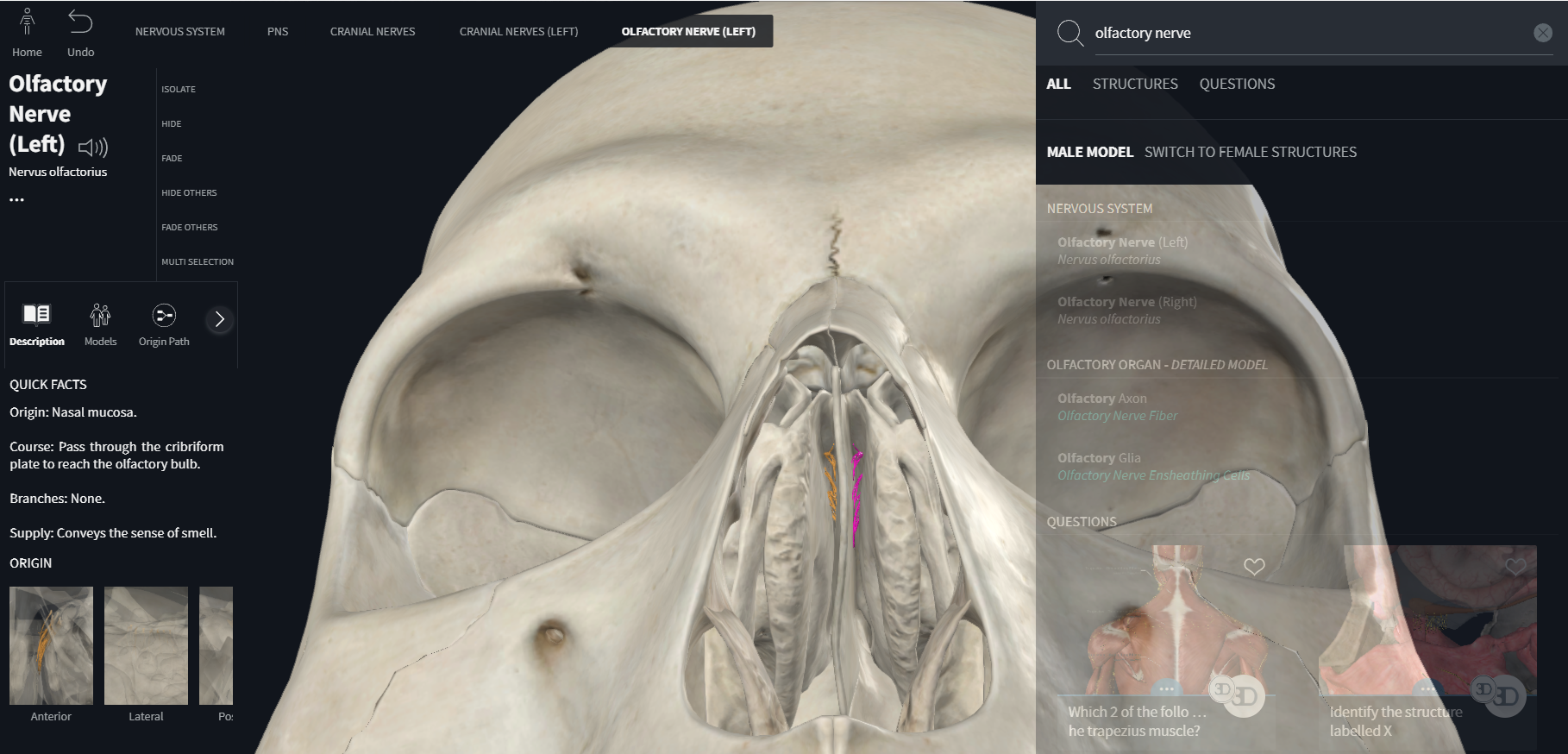
olfactory (CN I)
components, location of nerve cell bodies, cranial exit, function
CN I – Olfactory
Why it looks like this:
Special sensory → because smell is a special sense
Cell bodies in olfactory epithelium → neurons outside CNS
Enters brain through cribriform plate → path from nose into brain
Function = smell → exactly what olfactory neurons detect
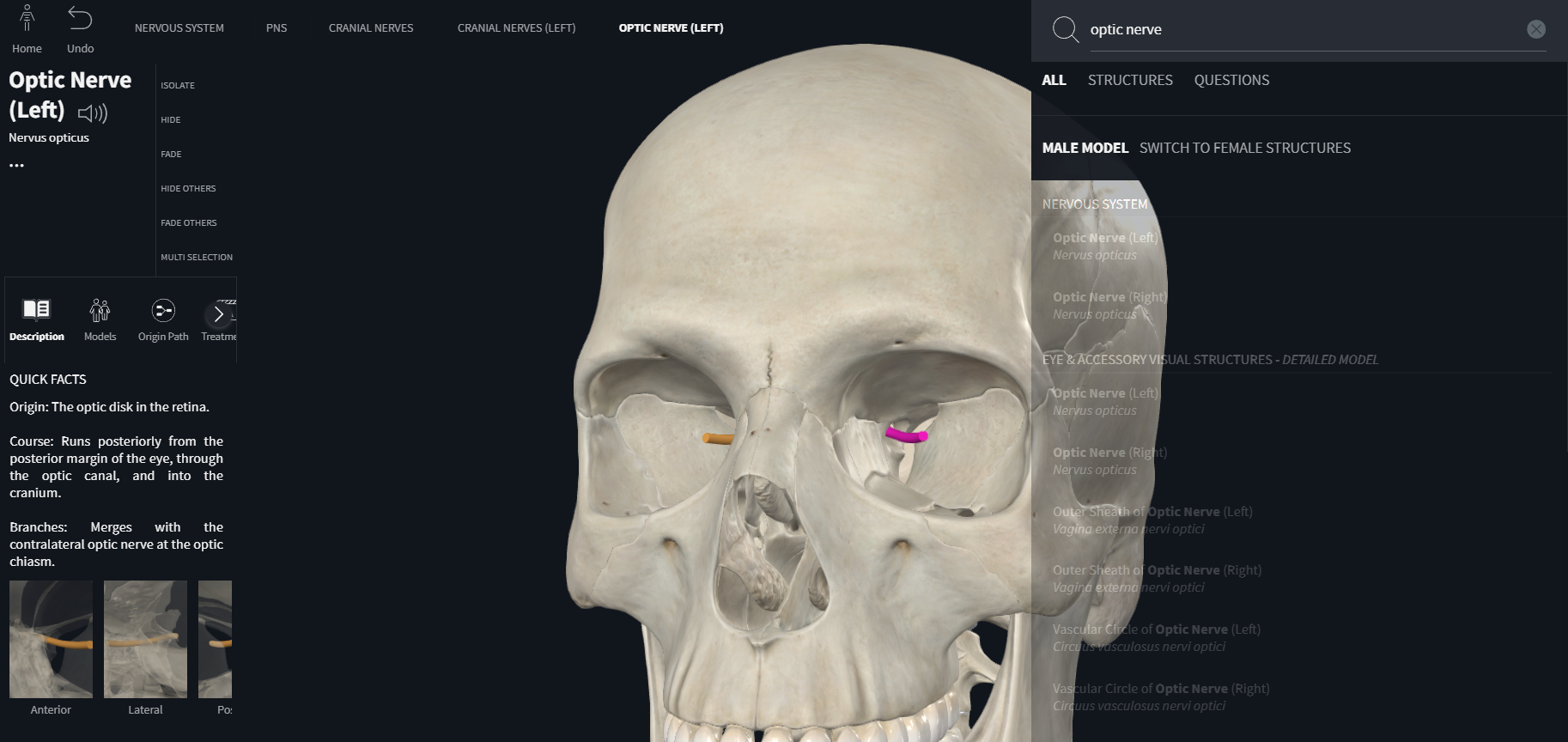
optic nerve (CN II)
components, location of nerve cell bodies, cranial exit, function
CN II – Optic
Why:
Special sensory → vision
Cell bodies in retina → retina develops from diencephalon
Optic canal → route from eyeball to brain
Function: vision → carried by retinal ganglion cells
Oculomotor (CN III)
components, location of nerve cell bodies, cranial exit, function
CN III – Oculomotor
Why:
Cell bodies in midbrain → CN III nucleus sits at level of superior colliculus
Exits via superior orbital fissure → path into orbit
Somatic motor → moves most extraocular muscles
Visceral motor (parasympathetic) → Edinger–Westphal nucleus controls pupil & lens
Everything it innervates sits inside the eye/orbit → which is why it exits through the SOF
trochlear (CN IV)
components, location of nerve cell bodies, cranial exit, function
CN IV – Trochlear
Why:
Nucleus in midbrain → inferior colliculus level
Innervates superior oblique, which uses a trochlea (“pulley”)
Only cranial nerve to exit dorsally
This nerve only serves 1 muscle → so its entry in the table is small.
trigeminal (CN V) Ophthalmic division (CN V1)
components, location of nerve cell bodies, cranial exit, function
CN V – Trigeminal (V1, V2, V3) ✔ CN V is sensory nerve of the face ✔ And motor nerve of 1st pharyngeal arch
Why:
Sensory ganglion = trigeminal (semilunar) ganglion
Motor nucleus in pons → because 1st arch motor neurons migrate there
V1 exits via superior orbital fissure
V2 exits via foramen rotundum
V3 exits via foramen ovale
Each branch takes the skull opening closest to the region it innervates.
V1 → orbit & forehead V2 → midface & maxilla V3 → mandible & chewing muscles
V3 is mixed because chewing muscles come from the 1st arch, which V3 supplies.
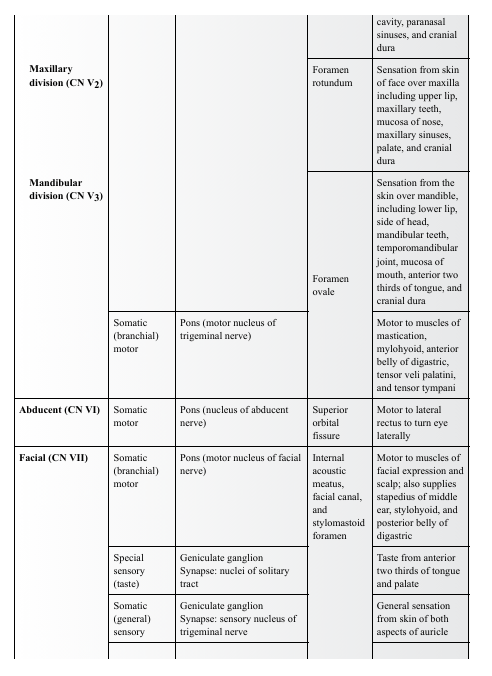
Trigeminal (CN V) Maxillary division (CN V2)
components, location of nerve cell bodies, cranial exit, function
CN V – Trigeminal (V1, V2, V3) ✔ CN V is sensory nerve of the face ✔ And motor nerve of 1st pharyngeal arch
Why:
Sensory ganglion = trigeminal (semilunar) ganglion
Motor nucleus in pons → because 1st arch motor neurons migrate there
V1 exits via superior orbital fissure
V2 exits via foramen rotundum
V3 exits via foramen ovale
Each branch takes the skull opening closest to the region it innervates.
V1 → orbit & forehead V2 → midface & maxilla V3 → mandible & chewing muscles
V3 is mixed because chewing muscles come from the 1st arch, which V3 supplies
Trigeminal (CN V) Mandibular division (CN V3)
components, location of nerve cell bodies, cranial exit, function
CN V – Trigeminal (V1, V2, V3) ✔ CN V is sensory nerve of the face ✔ And motor nerve of 1st pharyngeal arch
Why:
Sensory ganglion = trigeminal (semilunar) ganglion
Motor nucleus in pons → because 1st arch motor neurons migrate there
V1 exits via superior orbital fissure
V2 exits via foramen rotundum
V3 exits via foramen ovale
Each branch takes the skull opening closest to the region it innervates.
V1 → orbit & forehead V2 → midface & maxilla V3 → mandible & chewing muscles
V3 is mixed because chewing muscles come from the 1st arch, which V3 supplies
Abducent (CN VI)
components, location of nerve cell bodies, cranial exit, function
CN VI – Abducens
Why:
Nucleus in pons → right next to eye movement centers
Exits via SOF → same as CN III & IV, because they all go to orbit
Controls lateral rectus → abducts the eye, hence the name
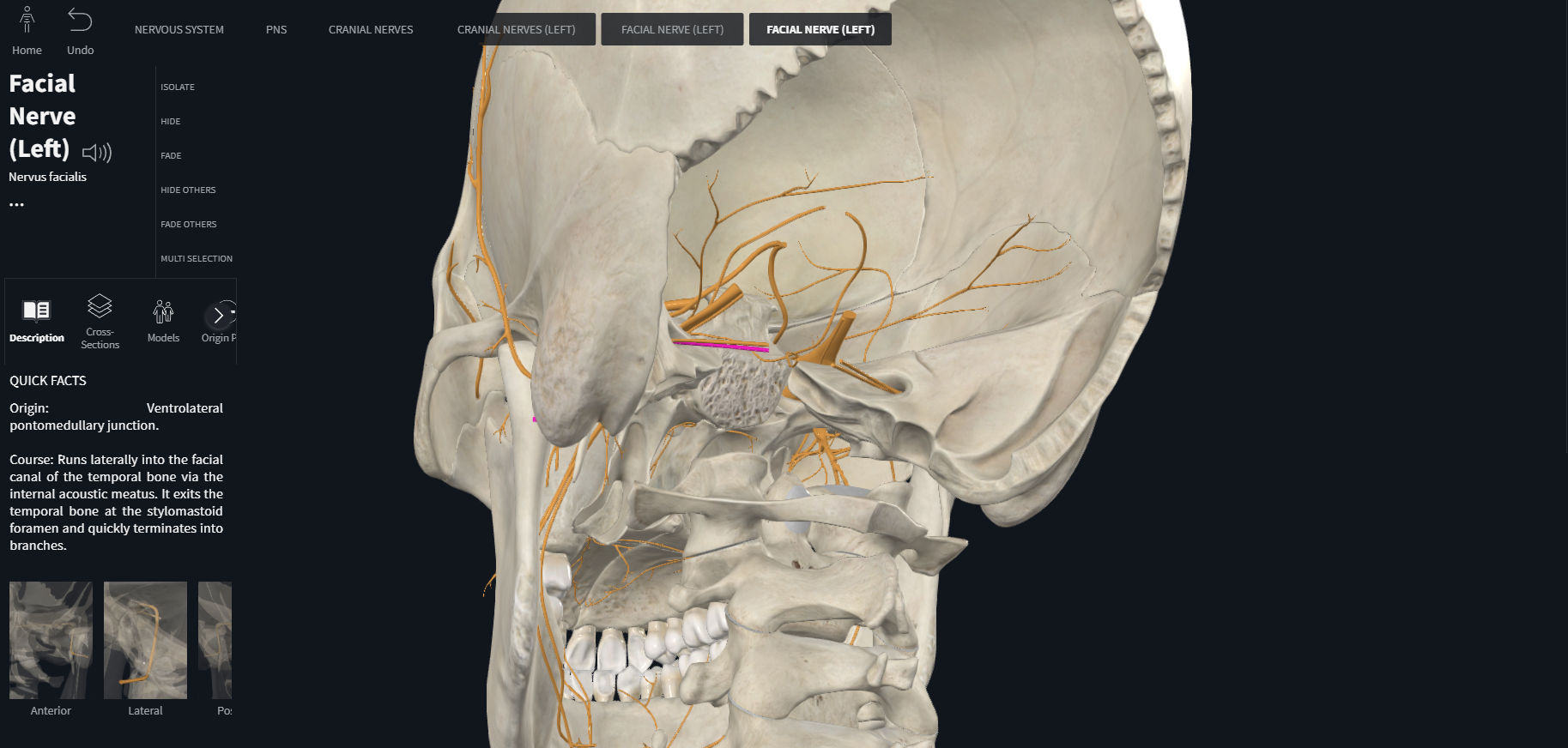
Facial (CN VII)
components, location of nerve cell bodies, cranial exit, function
CN VII – Facial Nerve
The most complex cranial nerve.
Why:
Motor nucleus in pons → 2nd arch derivatives
Sensory (taste) in geniculate ganglion
Parasympathetic from superior salivatory nucleus
Exits through internal acoustic meatus → facial canal → stylomastoid foramen
Functions line up with embryology:
2nd arch muscles → facial expression
Taste (SVA) → anterior 2/3 tongue
Parasympathetic → salivary & lacrimal glands
Sensory → small patch of ear
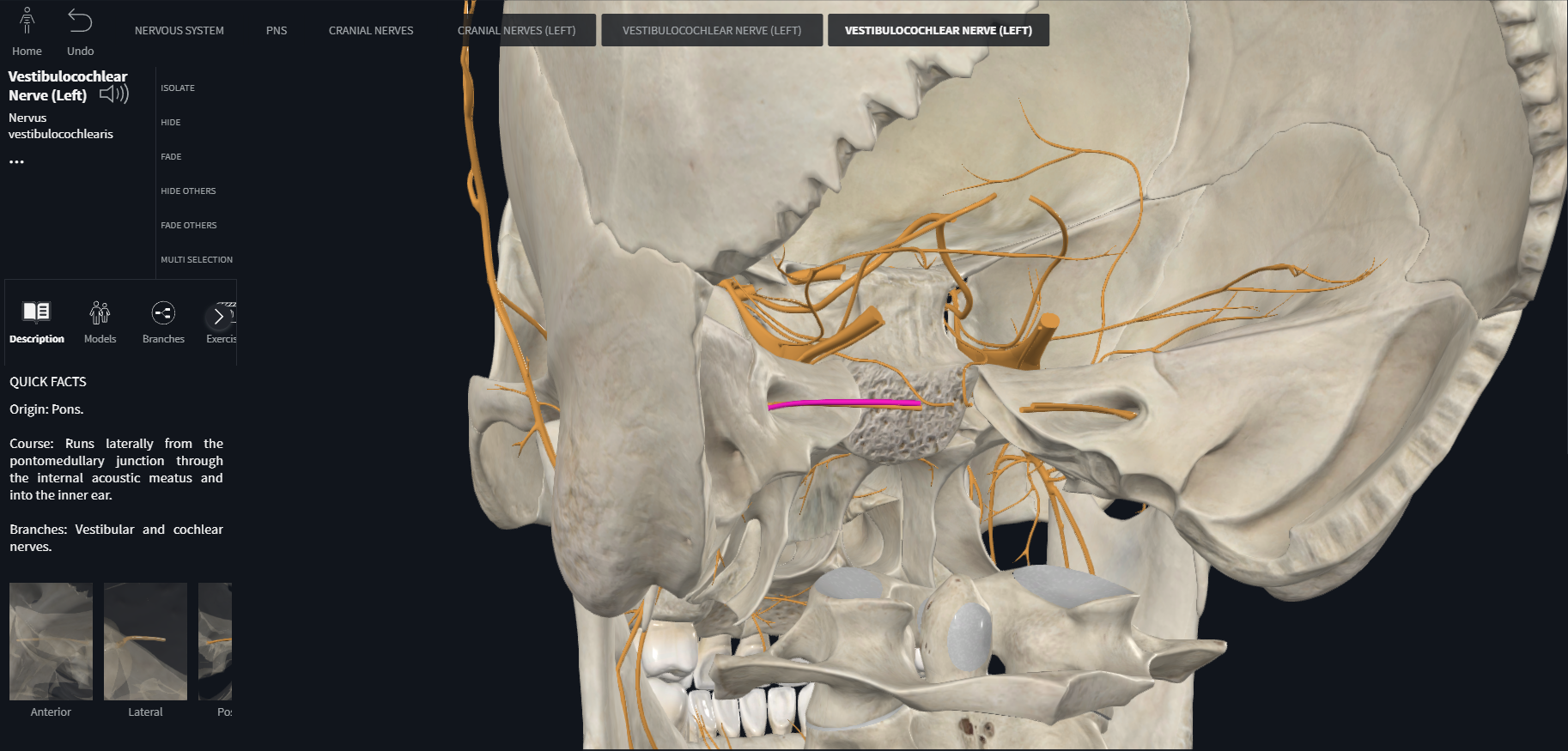
Vestibulocochlear (CN VIII) Vestibular
components, location of nerve cell bodies, cranial exit, function
CN VIII – Vestibulocochlear
Why:
Special sensory → hearing and balance
Ganglia: vestibular (balance), spiral (hearing)
Goes through internal acoustic meatus → into inner ear
Vestibulocochlear (CN VIII) Cochlear
components, location of nerve cell bodies, cranial exit, function
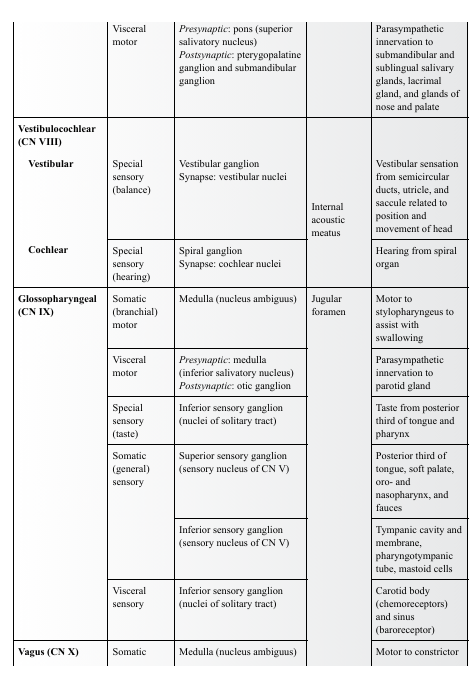
Glossopharyngeal (CN IX)
components, location of nerve cell bodies, cranial exit, function
Vagus (CN X)
components, location of nerve cell bodies, cranial exit, function
Spinal accessory nerve (CN XI)
components, location of nerve cell bodies, cranial exit, function
Hypoglossal (CN XII)
components, location of nerve cell bodies, cranial exit, function
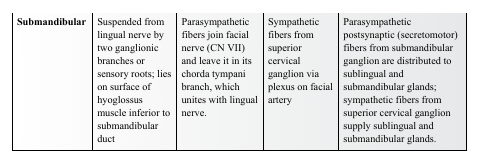
Some cranial nerves are purely sensory, others are considered purely motor, and several are mixed. CN III, CN IV, CN VI, CN XI, CN XII, and the motor root of CN V are considered to be “pure” motor nerves that appear to have evolved from primordial anterior roots. However, a small number of sensory fibers for proprioception (nonvisual perception of movement and position) are also present in these nerves, the cell bodies of which are probably located in the mesencephalic nucleus of CN V. The sensory root of CN V is purely a somatic (general) sensory nerve. Four cranial nerves (CN III, CN VII, CN IX, and CN X) contain presynaptic parasympathetic (visceral motor) axons as they emerge from the brainstem (Fig. 10.5; Table 10.3). CN V, CN VII, CN IX, and CN X are mixed nerves with both somatic (branchial) motor and somatic (general) sensory components. Each of these nerves supplies derivatives of a different pharyngeal arch (Fig. 10.4; Table 10.2).
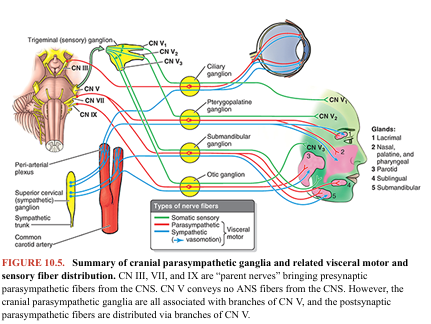
The fibers of cranial nerves connect centrally to cranial nerve nuclei—groups of neurons in which sensory or afferent fibers terminate and from which motor or efferent fibers originate (Fig. 10.6). Except for CN I and CN II, which involve extensions of the forebrain, and CN XI with nuclei in the C1–C3 segment of the spinal cord, the nuclei of the cranial nerves are located in or adjacent to the brainstem. Nuclei of similar functional components (e.g., somatic or visceral motor, or somatic or visceral sensory) are generally aligned into functional columns in the brainstem.
OLFACTORY NERVE (CN I)
Functions: special sensory (special visceral afferent) for the special sense of smell. “Olfaction is the sensation of odors that results from the detection of odorous substances aerosolized in the environment” (Simpson, 2018). The cell bodies of olfactory receptor neurons are located in the olfactory organ (the olfactory part of the nasal mucosa or olfactory area), which is located in the roof of the nasal cavity, and along the nasal septum and medial wall of the superior nasal concha (Fig. 10.7). Olfactory receptor neurons are both receptors and conductors. The apical surfaces of the neurons possess fine olfactory cilia, bathed by a film of watery mucus secreted by the olfactory glands of the epithelium. The olfactory cilia are stimulated by molecules of an odiferous gas dissolved in the fluid
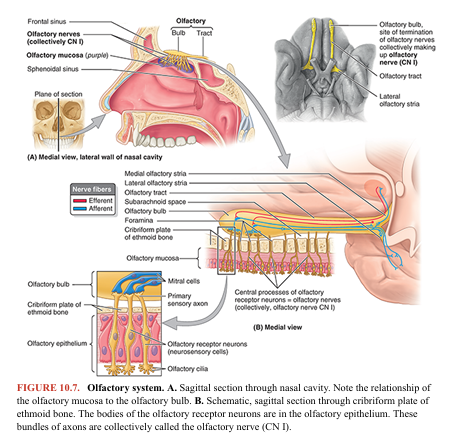
The basal surfaces of the bipolar olfactory receptor neurons of the nasal cavity of one side give rise to central processes that are collected into approximately 20 olfactory nerves (L. fila olfactoria), constituting the right or left olfactory nerve (CN I). They pass through tiny foramina in the cribriform plate of the ethmoid bone, surrounded by sleeves of dura mater and arachnoid mater, and enter the olfactory bulb in the anterior cranial fossa (Figs. 10.1, 10.2, and 10.3). The olfactory bulb lies in contact with the inferior or orbital surface of the frontal lobe of the cerebral hemisphere. The olfactory nerve fibers synapse with mitral cells in the olfactory bulb. The axons of these secondary neurons form the olfactory tract. The olfactory bulbs and tracts are anterior extensions of the forebrain. Each olfactory tract divides into lateral and medial olfactory striae (distinct fiber bands). The lateral olfactory stria terminates in the piriform cortex of the anterior part of the temporal lobe, and the medial olfactory stria projects through the anterior commissure to contralateral olfactory structures. The olfactory nerves are the only cranial nerves to enter the cerebrum directly
The Bottom Line: Olfactory Nerve
■ The olfactory nerves (CN I) have sensory fibers concerned with the special sense of smell. ■ The olfactory receptor neurons are in the olfactory epithelium (olfactory mucosa) in the roof of the nasal cavity. ■ The central processes of the olfactory receptor neurons ascend through foramina in the cribriform plate of the ethmoid bone to reach the olfactory bulbs in the anterior cranial fossa. These nerves synapse on neurons in the bulbs, and the processes of these neurons follow the olfactory tracts to the primary and associated areas of the cerebral cortex.
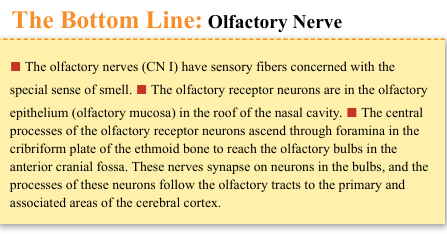
OPTIC NERVE (CN II)
Functions: special sensory (special somatic afferent) for the special sense of vision. Although officially nerves by convention, the optic nerves (CN II) develop in a completely different manner from the other cranial nerves. The structures involved in receiving and transmitting optical stimuli (the optical fibers and neural retina, together with the pigmented epithelium of the eyeball) develop as evaginations of the diencephalon. The optic nerves are paired, anterior extensions of the forebrain (diencephalon), and are therefore actually CNS fiber tracts formed by axons of retinal ganglion cells (Moore et al., 2020). In other words, they are third-order neurons, with their cell bodies located in the retina (Fig. 10.8B).
The optic nerves are surrounded by extensions of the cranial meninges and subarachnoid space, which is filled with cerebrospinal fluid (CSF). The meninges extend all the way to the eyeball. The central artery and vein of the retina traverse the meningeal layers and course in the anterior part of the optic nerve. CN II begins where the unmyelinated axons of retinal ganglion cells pierce the sclera (the opaque part of the external fibrous coat of the eyeball) and become myelinated, deep to the optic disc. The nerve passes posteromedially in the orbit, exiting through the optic canal to enter the middle cranial fossa, where it forms the optic chiasm (Figs. 10.2 and 10.8A). Here, fibers from the nasal (medial) half of each retina decussate in the chiasm and join uncrossed fibers from the temporal (lateral) half of the retina to form the optic tract. The partial crossing of optic nerve fibers in the chiasm is a requirement for binocular vision, allowing depth-of-field perception (three-dimensional vision). Therefore, fibers from the right halves of both retinas form the right optic tract. The decussation of nerve fibers in the chiasm results in the right optic tract conveying impulses from the left visual field and vice versa. The combined visual field is what is seen by a person who has both eyes wide open and who is looking straight ahead. Most fibers in the optic tracts terminate in the lateral geniculate bodies of the thalamus. From these nuclei, axons are relayed to the visual cortices of the occipital lobes of the brain
The Bottom Line: Optic Nerve
■ The optic nerves (CN II) have sensory fibers concerned with the special sense of vision. ■ The optic nerve fibers arise from ganglion cells in the retina. ■ The nerve fibers exit the orbit via the optic canals; fibers from the nasal half of the retina cross to the contralateral side at the optic chiasm. ■ The nerve fibers then pass via the optic tracts to the geniculate bodies of the thalamus, where they synapse on neurons whose processes form the optic radiations to the primary visual cortex of the occipital lobe.
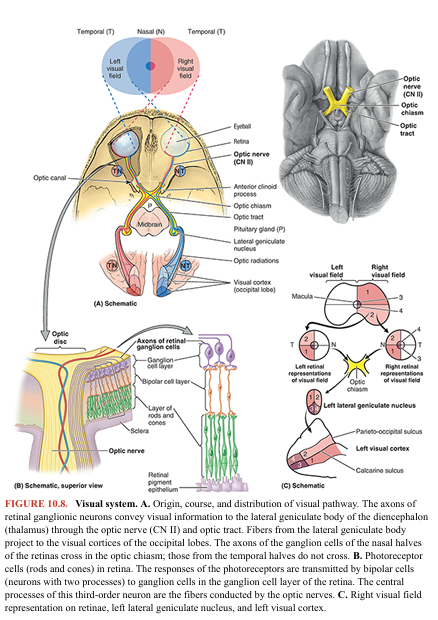
OCULOMOTOR NERVE (CN III)
Functions: somatic motor (general somatic efferent) and visceral motor (general visceral efferent–parasympathetic). Nuclei: There are two oculomotor nuclei, each serving one of the functional components of this nerve. The somatic motor nucleus of the oculomotor nerve is in the midbrain (Fig. 10.6). The visceral motor (parasympathetic) accessory (Edinger-Westphal) nucleus of the oculomotor nerve lies dorsal to the rostral two thirds of the somatic motor nucleus (Haines & Mihailoff, 2018). The oculomotor nerve (CN III) provides the following (Fig. 10.9): • Motor innervation to the striated muscle of four of the six extra-ocular muscles (superior, medial, and inferior recti and inferior oblique) and superior eyelid (L. levator palpebrae superioris), hence the nerve’s name • Parasympathetic innervation through the ciliary ganglion to the smooth muscle of the sphincter pupillae that causes constriction of the pupil and ciliary muscle, producing accommodation (allowing the lens to become more rounded) for near vision
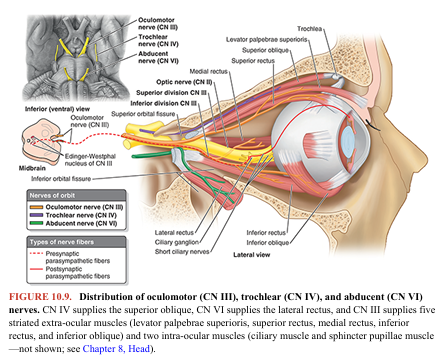
CN III is the chief motor nerve to the ocular and extra-ocular muscles. It emerges from the midbrain, pierces the dura mater lateral to the diaphragma sellae roofing over the hypophysis, and then runs through the roof and lateral wall of the cavernous sinus. CN III leaves the cranial cavity and enters the orbit through the superior orbital fissure. Within this fissure, CN III divides into a superior division (which supplies the superior rectus and levator palpebrae superioris) and an inferior division (which supplies the inferior and medial rectus and inferior oblique). The inferior division also carries presynaptic parasympathetic (visceral efferent) fibers to the ciliary ganglion, where they synapse (see Fig. 10.5; Table 10.3). Postsynaptic fibers from this ganglion pass to the eyeball in the short ciliary nerves to innervate the ciliary body and sphincter pupillae (see Fig. 8.51 in Chapter 8, Head).
The Bottom Line: Oculomotor Nerve
■ The oculomotor nerves (CN III) send somatic motor fibers to all extra ocular muscles, except the superior oblique and lateral rectus. ■ These nerves also send presynaptic parasympathetic fibers to the ciliary ganglion for innervation of the ciliary body and sphincter pupillae. ■ These nerves originate from the upper brainstem (midbrain) and run in the lateral wall of the cavernous sinus. ■ These nerves enter the orbit through the superior orbital fissures and divide into superior and inferior branches.
TROCHLEAR NERVE (CN IV)
Functions: somatic motor (general somatic efferent) to one extra-ocular muscle (superior oblique). Nucleus: The nucleus of the trochlear nerve is located in the midbrain, immediately caudal to the oculomotor nucleus (Fig. 10.6). The trochlear nerve (CN IV) is the smallest cranial nerve. It emerges from the posterior (dorsal) surface of the midbrain (the only cranial nerve to do so), passing anteriorly around the brainstem. It has the longest intracranial (subarachnoid) course of the cranial nerves. The trochlear nerve pierces the dura mater at the margin of the tentorium cerebelli and passes anteriorly in the lateral wall of the cavernous sinus (Fig. 10.3A–C). CN IV then continues through the superior orbital fissure into the orbit, where it supplies the superior oblique—the only extra-ocular muscle that uses a pulley, or trochlea, to redirect its line of action (hence the nerve’s name) (Fig. 10.9).
The Bottom Line: Trochlear Nerve
■ The trochlear nerves (CN IV) supply somatic motor fibers to the superior oblique muscles, which abduct, depress, and medially rotate the pupil. ■ The trochlear nerves emerge from the posterior aspect of the brainstem. ■ The nerves run a long intracranial course, passing around the brainstem to enter the dura mater in the free edge of the tentorium cerebelli close to the posterior clinoid process. ■ The nerves then run in the lateral wall of the cavernous sinus, entering the orbit via the superior orbital fissures.
TRIGEMINAL NERVE (CN V)
Functions: somatic (general) sensory and somatic (branchial) motor to derivatives of the 1st pharyngeal arch. Nuclei: There are four trigeminal nuclei (Fig. 10.6)—one motor (motor nucleus of trigeminal nerve) and three sensory (mesencephalic, principal sensory, and spinal nuclei of trigeminal nerve). The trigeminal nerve (CN V) is the largest cranial nerve (if the atypical optic nerve is excluded). It emerges from the lateral aspect of the pons of the brainstem by a large sensory root and a small motor root (Figs. 10.2, 10.3, and 10.4). The roots of CN V are comparable to the posterior and anterior roots of spinal nerves. CN V is the principal somatic (general) sensory nerve for the head (face, teeth, mouth, nasal cavity, and dura mater of the cranial cavity). The large sensory root of CN V is composed mainly of the central processes of the pseudounipolar neurons that make up the sensory trigeminal ganglion (Fig. 10.10). The ganglion is flattened and crescent shaped (hence its unofficial name, semilunar ganglion) and is housed within a dural recess (trigeminal cave) lateral to the cavernous sinus.
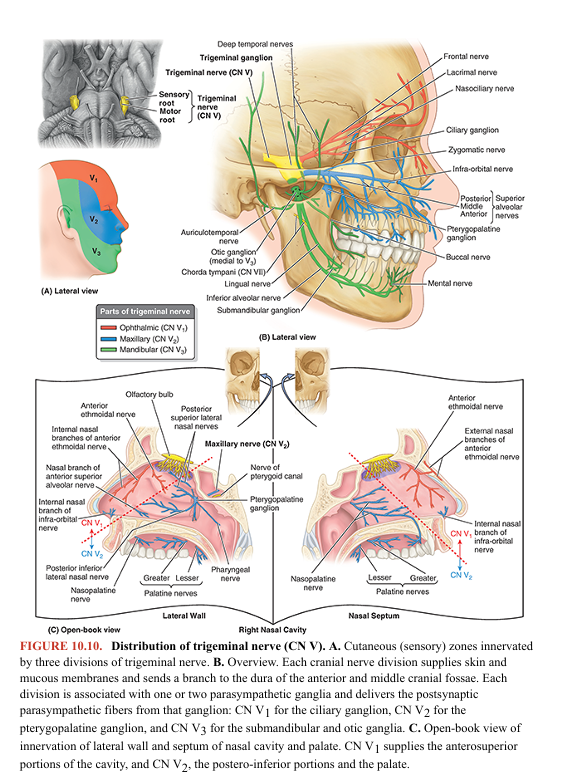
The peripheral processes of the ganglionic neurons form three nerves or divisions: ophthalmic nerve (CN V1), maxillary nerve (CN V2), and sensory component of the mandibular nerve (CN V3). Maps of the zones of cutaneous innervation by the three divisions resemble the dermatome maps for cutaneous innervation by spinal nerves (Fig. 10.10A). Unlike spinal nerve dermatomes, however, there is little overlap in innervation by the divisions; lesions of a single nerve result in clearly demarcated areas of numbness. The motor root of CN V passes adjacent to the trigeminal ganglion, bypassing the ganglion and merging with the mandibular division of CN V immediately distal to the ganglion. The motor fibers are distributed exclusively via the mandibular nerve (CN V3), blending with its sensory fibers as the nerve traverses the foramen ovale to exit the cranium (Figs. 10.1, 10.3A–C, and 10.4). This is similar to the way that anterior roots of spinal nerves bypass the spinal sensory (dorsal root) ganglia, also merging with the sensory fibers of the nerves immediately distal to the ganglion, as the nerves traverse the intervertebral foramina, exiting the spine (see Fig. 1.41 in Chapter 1, Overview and Basic Concepts). Motor fibers of the mandibular nerve are distributed to the muscles of mastication, mylohyoid, anterior belly of the digastric, tensor veli palatini, and tensor tympani (see Fig. 8.76 in Chapter 8, Head), which are derived from the 1st pharyngeal arch. Although CN V conveys no presynaptic parasympathetic fibers from the CNS, all four parasympathetic ganglia are associated with the divisions of CN V. Postsynaptic parasympathetic fibers from the ganglia join branches of CN V and are carried to their destinations along with the CN V sensory and motor fibers (Fig. 10.5; Table 10.3).
Ophthalmic Nerve (CN V1)
In contrast to the other two CN V divisions, CN V1 is not a branchial nerve (i.e., it does not supply pharyngeal arch derivatives). It serves structures derived from the paraxial mesoderm of the embryonic frontonasal process. The ophthalmic nerve’s association with the other CN V divisions is a secondary occurrence. The somatic (general) sensory fibers of CN V1 are distributed to skin and mucous membranes and conjunctiva of the front of the head and nose (Fig. 10.10).
Testing CN V1: The integrity of this division is tested by checking the corneal reflex—touching the cornea, which is also supplied by CN V1, with a wisp of cotton will evoke a reflexive blink if the nerve is functional (Table 10.4; see Fig. B8.14B).
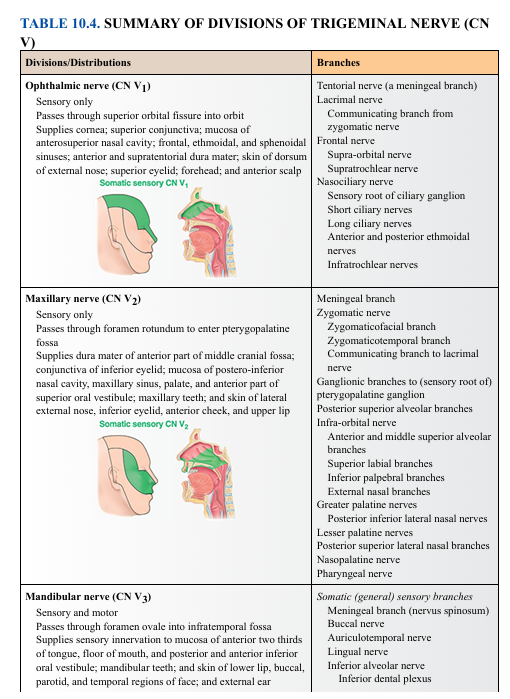
Maxillary Nerve (CN V2) CN V2 innervates derivatives of the maxillary prominence of the 1st pharyngeal arch. Exiting the cranial cavity via the foramen rotundum, its somatic (general) sensory fibers are mainly distributed to skin and mucous membranes associated with the upper jaw (Fig. 10.10; Table 10.4). The pterygopalatine (parasympathetic) ganglion is associated with this division of CN V, involved in innervating the lacrimal gland and glands of the nose and palate (Fig. 10.5; Table 10.3).
Mandibular Nerve (CN V3) CN V3 innervates derivatives of the mandibular prominence of the 1st pharyngeal arch. CN V3 is the only division of CN V to convey somatic (branchial) motor fibers, distributed to the striated muscle derived from mandibular prominence mesoderm, primarily the muscles of mastication. Two parasympathetic ganglia, the otic and submandibular, are associated with this division of CN V; both are concerned with the innervation of salivary glands. Tables 10.1, 10.2, and 10.3 provide a general summary of CN V. Table 10.4 summarizes the branches of the three divisions.
The Bottom Line: Trigeminal Nerve
■ CN V is the chief nerve for general sensory innervation of the head. ■ Via its three divisions, it provides sensory innervation to dura of the anterior and middle cranial fossae, skin of the face, teeth, gingiva, mucous membrane of the nasal cavity, paranasal sinuses, and mouth. ■ The trigeminal nerve (CN V) supplies somatic motor fibers to the muscles of mastication, mylohyoid, anterior belly of the digastric, tensor tympani, and tensor veli palatini muscles. ■ It also distributes postsynaptic parasympathetic fibers of the head to their destinations. ■ CN V originates from the lateral surface of the pons by two roots: motor and sensory. ■ These roots cross the medial part of the crest of the petrous part of the temporal bone and enter the trigeminal cave of the dura mater lateral to the body of the sphenoid and cavernous sinus. ■ The sensory root leads to the trigeminal ganglion; the motor root runs parallel to the sensory root, bypasses the ganglion, and becomes part of the mandibular nerve (CN V3).
ABDUCENT NERVE (CN VI)
Functions: somatic motor (general somatic efferent) to one extra-ocular muscle, the lateral rectus. Nucleus: The abducent nucleus is in the pons near the median plane (Fig. 10.6). The abducent nerve (CN VI) emerges from the brainstem between the pons and the medulla and traverses the pontine cistern of the subarachnoid space, the right and left nerves straddling the basilar artery (Fig. 10.3A and inset; see Fig. 8.42 in Chapter 8, Head). Each abducent nerve then pierces the dura mater to run the longest intradural course within the cranial cavity of all the cranial nerves— that is, its point of entry into the dura mater covering the clivus is the most distant from its exit from the cranium via the superior orbital fissure. During its intradural course, it bends sharply over the crest of the petrous part of the temporal bone and then courses through the cavernous sinus, surrounded by the venous blood in the same manner as the internal carotid artery, which it parallels in the sinus (Fig. 10.3A–C). CN VI traverses the common tendinous ring (L. anulus tendineus communis) as it enters the orbit (see Fig. 8.55 in Chapter 8, Head), running on and penetrating the medial surface of the lateral rectus, which abducts the pupil (Fig. 10.9).
The Bottom Line: Abducent Nerve
■ The abducent nerves (CN VI) supply somatic motor fibers to the lateral rectus muscles of the eyeballs. ■ The nerves originate from the pons, pierce the dura mater on the clivus, traverse the cavernous sinuses and superior orbital fissures, and enter the orbits.
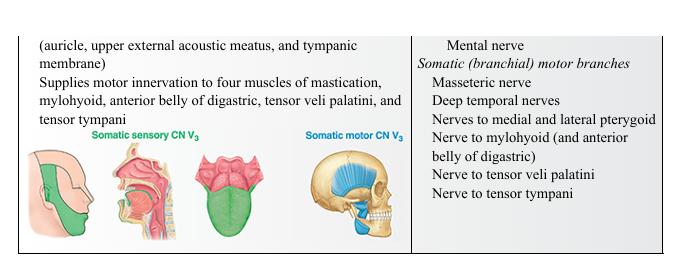
FACIAL NERVE (CN VII)
Functions: sensory—special sensory (taste) and somatic (general) sensory; motor —somatic (branchial) motor and visceral (parasympathetic) motor. It also carries proprioceptive fibers from the muscles it innervates, although the muscles of facial expression include relatively few muscle spindles (mechanoreceptors for muscle stretch), so proprioceptive sensory fibers are fewer than in other motor nerves (Haines & Mihailoff, 2018). Nuclei: The motor nucleus of the facial nerve is a branchiomotor nucleus in the ventrolateral part of the pons of the brainstem (Fig. 10.6). The cell bodies of the primary sensory neurons are in the geniculate ganglion (Fig. 10.11). The central processes of those concerned with taste end in the nuclei of the solitary tract in the medulla. The processes of those concerned with general sensations (pain, touch, and thermal) from around the external ear end in the spinal nucleus of the trigeminal nerve (Fig. 10.5).
VERY IMPORTANT PICTURE
The facial nerve (CN VII) emerges from the junction of the pons and medulla as two divisions: the primary root and the intermediate nerve (Fig. 10.2; Table 10.1). The larger primary root (facial nerve proper) innervates the muscles of facial expression, and the smaller intermediate nerve (L. nervus intermedius) carries taste, presynaptic parasympathetic, and somatic sensory fibers. During its course, CN VII traverses the posterior cranial fossa, internal acoustic meatus, facial canal, stylomastoid foramen of the temporal bone, and parotid gland (Fig. 10.11A, B). After traversing the internal acoustic meatus, the nerve proceeds a short distance anteriorly within the temporal bone and then turns abruptly posteriorly to course along the medial wall of the tympanic cavity. The sharp bend, the geniculum of the facial nerve (L. genu, knee), is the site of the geniculate ganglion, the sensory ganglion of CN VII. While traversing the temporal bone within the facial canal (Fig. 10.11A; see Fig. 8.116B in Chapter 8, Head), CN VII gives rise to the: • Greater petrosal nerve • Nerve to the stapedius • Chorda tympani nerve Then, after running the longest intra-osseous course of any cranial nerve, CN VII emerges from the cranium via the stylomastoid foramen (see Fig. 8.16B in Chapter 8, Head), gives off the posterior auricular branch, enters the parotid gland, and forms the parotid plexus, which gives rise to the following five terminal motor branches: temporal, zygomatic, buccal, marginal mandibular, and cervical (see Fig. 8.16 in Chapter 8, Head)
Somatic (Branchial) Motor As the nerve of the embryonic 2nd pharyngeal arch, the facial nerve supplies striated muscles derived from its mesoderm, mainly the muscles of facial expression and auricular muscles. It also supplies the posterior belly of the digastric, stylohyoid, and stapedius muscles.
Visceral (Parasympathetic) Motor The visceral (parasympathetic) motor distribution of the facial nerve is presented in Figure 10.11B–D. CN VII provides presynaptic parasympathetic fibers to the pterygopalatine ganglion for innervation of the lacrimal, nasal, palatine, and pharyngeal glands and to the submandibular ganglion for innervation of the sublingual and submandibular salivary glands. The pterygopalatine ganglion is associated with the maxillary nerve (CN V2), which distributes its postsynaptic fibers, whereas the submandibular ganglion is associated with the mandibular nerve (CN V3). The distribution of visceral motor and sensory fibers to or through the parasympathetic ganglia supplied by the facial nerve and certain other cranial nerves is summarized in Figure 10.5 and Table 10.3. Parasympathetic fibers synapse in these ganglia, whereas sympathetic and sensory fibers pass through them.
Somatic (General) Sensory Some fibers from the geniculate ganglion accompany the auricular branch of the vagus nerve to supply small areas of skin on both aspects of the auricle, in the region of the concha and at the opening of the external acoustic meatus.
Special Sensory (Taste) Peripheral fibers of sensory neurons of the geniculate ganglion are carried by the chorda tympani. They join the lingual nerve of CN V3 in the infratemporal fossa to supply taste buds of the anterior two thirds of the tongue and soft palate (Fig. 10.11B). Central fibers of the neurons pass to the brainstem via the intermediate nerve
The Bottom Line: Facial Nerve
■ The facial nerves (CN VII) supply motor fibers to the stapedius, posterior belly of the digastric, stylohyoid, facial, and scalp muscles. ■ They also supply presynaptic parasympathetic fibers via the intermediate nerve (smaller root of CN VII) destined for the pterygopalatine and submandibular ganglia via the greater petrosal nerve and chorda tympani, respectively. ■ CN VII is sensory to some skin of the external acoustic meatus and, via the intermediate nerve, is sensory to taste from the anterior two thirds of the tongue and the soft palate. ■ CN VII originates from the caudal border of the pons and runs through the internal acoustic meatus and facial canal in the petrous part of the temporal bone. ■ CN VII exits via the stylomastoid foramen; its main trunk forms the intraparotid nerve plexus.
VESTIBULOCOCHLEAR NERVE (CN VIII)
Functions: special sensory (special somatic afferent), that is, special sensations of hearing, equilibrium, and motion (acceleration/deceleration). Nuclei: Vestibular nuclei are located at the junction of the pons and medulla of the brainstem in the lateral part of the floor of the 4th ventricle; the cochlear nuclei, anterior and posterior, are in the medulla (Fig. 10.6). The vestibulocochlear nerve (CN VIII) emerges from the junction of the pons and medulla and enters the internal acoustic meatus (Figs. 10.2, 10.3A, 10.4, and 10.12). Here, it separates into the vestibular and cochlear nerves.
The vestibular nerve is composed of the central processes of bipolar neurons in the vestibular ganglion. The peripheral processes of the neurons extend to the maculae of the utricle and saccule (sensitive to linear acceleration and the pull of gravity relative to the position of the head) and to the cristae of the ampullae of the semicircular ducts (sensitive to rotational acceleration). • The cochlear nerve is composed of the central processes of bipolar neurons in the spiral ganglion; the peripheral processes of the neurons extend to the spiral organ for the sense of hearing.
Within the internal acoustic meatus, the two divisions of CN VIII are accompanied by the primary root and intermediate nerve of CN VII and the labyrinthine artery (Fig. 10.3A; see Figs. 8.42 and 8.43 in Chapter 8, Head).
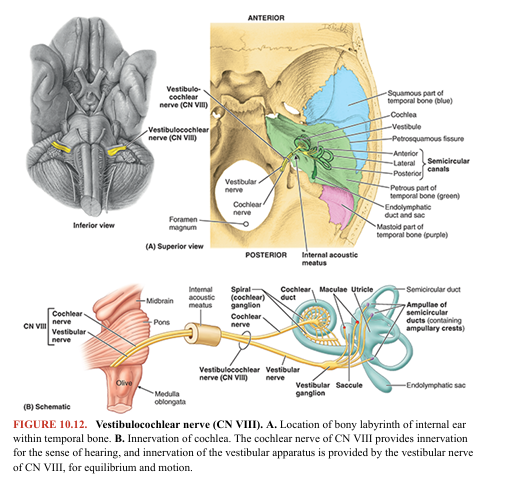
The Bottom Line: Vestibulocochlear Nerve
■ The vestibulocochlear nerves (CN VIII) carry fibers concerned with the special senses of hearing, equilibrium, and motion. ■ The nerves originate from the grooves between the pons and medulla. ■ They run through the internal acoustic meatus and divide into the cochlear and vestibular nerves. ■ The cochlear nerve is sensory to the spiral organ (for the sense of hearing). ■ The vestibular nerve is sensory to the cristae of the ampullae of the semicircular ducts and the maculae of the saccule and utricle (for the sense of equilibration and motion)
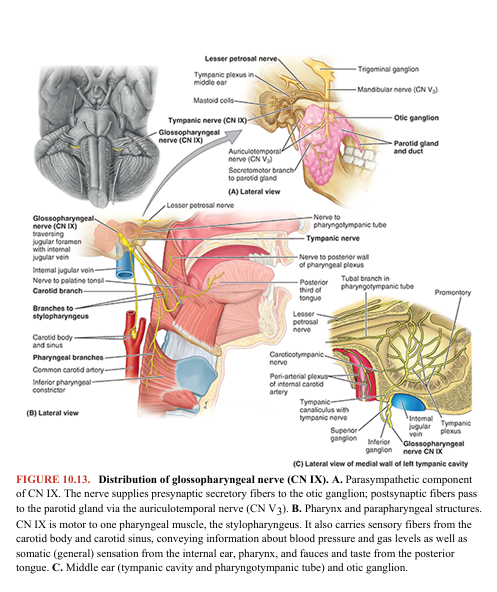
GLOSSOPHARYNGEAL NERVE (CN IX)
Functions: sensory—somatic (general) sensory, special sensory (taste), and visceral sensory; motor—somatic (branchial) motor and visceral (parasympathetic) motor for derivatives of the 3rd pharyngeal arch. Nuclei: Four nuclei in the medulla send or receive fibers via CN IX: two motor (nucleus ambiguus and inferior salivary nucleus) and two sensory (sensory nuclei of the trigeminal nerve [CN V] and nuclei of the solitary tract). Three of these nuclei (in italics) are shared with CN X (Fig. 10.6). The glossopharyngeal nerve (CN IX) emerges from the lateral aspect of the medulla and passes anterolaterally to leave the cranium through the anterior aspect of the jugular foramen (Figs. 10.13 and 10.14). At this foramen are the sensory superior and inferior ganglia of CN IX, which contain the pseudounipolar cell bodies for the afferent components of the nerve. CN IX follows the stylopharyngeus, the only muscle the nerve supplies, and passes between the superior and middle pharyngeal constrictor muscles to reach the oropharynx and tongue. It contributes sensory fibers to the pharyngeal plexus of nerves. CN IX is afferent from the tongue and pharynx (hence its name) and efferent to the stylopharyngeus and parotid gland.
![<p>Functions: sensory—somatic (general) sensory, special sensory (taste), and visceral sensory; motor—somatic (branchial) motor and visceral (parasympathetic) motor for derivatives of the 3rd pharyngeal arch. Nuclei: Four nuclei in the medulla send or receive fibers via CN IX: two motor (nucleus ambiguus and inferior salivary nucleus) and two sensory (sensory nuclei of the trigeminal nerve [CN V] and nuclei of the solitary tract). Three of these nuclei (in italics) are shared with CN X (Fig. 10.6). The glossopharyngeal nerve (CN IX) emerges from the lateral aspect of the medulla and passes anterolaterally to leave the cranium through the anterior aspect of the jugular foramen (Figs. 10.13 and 10.14). At this foramen are the sensory superior and inferior ganglia of CN IX, which contain the pseudounipolar cell bodies for the afferent components of the nerve. CN IX follows the stylopharyngeus, the only muscle the nerve supplies, and passes between the superior and middle pharyngeal constrictor muscles to reach the oropharynx and tongue. It contributes sensory fibers to the pharyngeal plexus of nerves. CN IX is afferent from the tongue and pharynx (hence its name) and efferent to the stylopharyngeus and parotid gland.</p>](https://knowt-user-attachments.s3.amazonaws.com/ae102905-776c-48ab-ba2c-fe20c3839d26.png)
Somatic (Branchial) Motor Motor fibers pass to one muscle, the stylopharyngeus, derived from the 3rd pharyngeal arch.
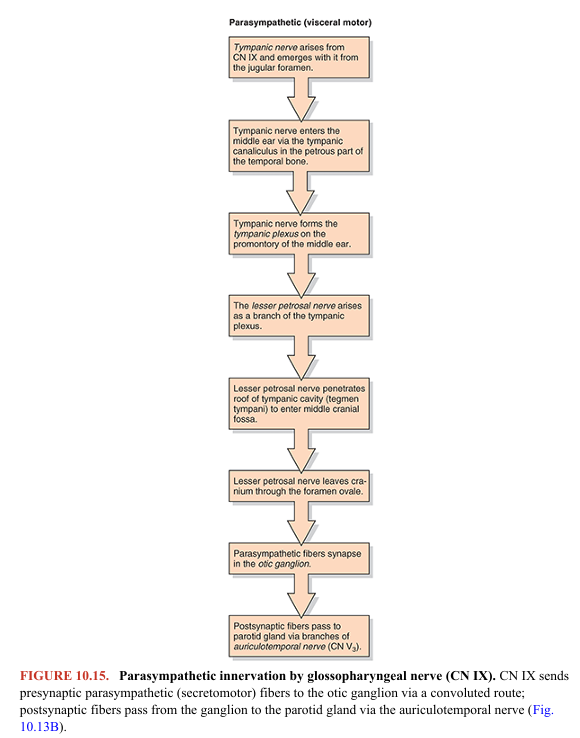
Visceral (Parasympathetic) Motor
Following a circuitous route initially involving the tympanic nerve, presynaptic parasympathetic fibers are provided to the otic ganglion for innervation of the parotid gland (Fig. 10.15). The otic ganglion is associated with the mandibular nerve (CN V3), branches of which convey the postsynaptic parasympathetic fibers to the parotid gland.
Somatic (General) Sensory The general sensory branches of CN IX are as follows (Fig. 10.13): • The tympanic nerve passes via the tympanic canaliculus between the carotid canal and jugular foramen to form the tympanic plexus within the tympanic cavity. The plexus provides sensory innervation for the mucosa of the tympanic cavity, antrum of mastoid air cells, and the posterolateral portion of the pharyngotympanic tube. • The pharyngeal, tonsillar, and lingual nerves to the mucosa of the oropharynx and isthmus of the fauces (L., throat), including palatine tonsil, soft palate, and posterior third of the tongue. In addition to general sensation (touch, pain, temperature), tactile (actual or threatened) stimuli determined to be unusual or unpleasant here may evoke the gag reflex or even vomiting. The gag reflex is absent in about 37% of normal individuals (Davies et al., 1995). CN IX provides the afferent (sensory) limb of the reflex, while the efferent (motor) limb is via the vagus nerve (CN X).
Special Sensory (Taste) Taste fibers are conveyed from the posterior third of the tongue to the sensory inferior ganglia of CN IX (Fig. 10.14). Details of the distribution of CN IX are outlined in Figure 10.13.
Visceral Sensory The carotid branch of CN IX supplies the carotid sinus, a baroreceptor (pressoreceptor) sensitive to changes in blood pressure, and the carotid body, a chemoreceptor sensitive to blood gas (oxygen and carbon dioxide levels).
The Bottom Line: Glossopharyngeal Nerve
■ The glossopharyngeal nerves (CN IX) send somatic motor fibers to the stylopharyngeus and visceral motor (presynaptic parasympathetic) fibers to the otic ganglion for innervation of the parotid gland. ■ They also send sensory fibers to the posterior third of the tongue (including taste), pharynx, tympanic cavity, pharyngotympanic tube, carotid body, and carotid sinus. ■ The nerves originate from the rostral end of the medulla and exit from the cranium via the jugular foramina. ■ They pass between the superior and the middle pharyngeal constrictors to the tonsillar sinus and enter the posterior third of the tongue.
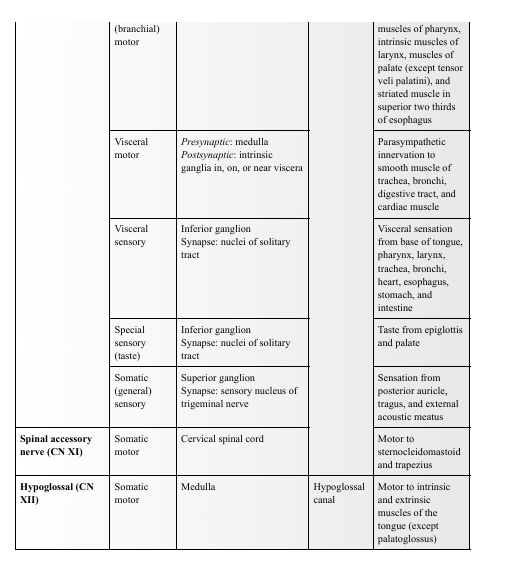
VAGUS NERVE (CN X)
Functions: sensory—somatic (general) sensory, special sensory (taste), visceral sensory; motor—somatic (branchial) motor and visceral (parasympathetic) motor. • Somatic (general) sensory from the inferior pharynx and larynx. The vagus provides the afferent (sensory) limb of the cough reflex stimulated by foreign irritants, preventing aspiration and infection. • Visceral sensory from the thoracic and abdominal organs • Taste and somatic (general) sensation from the root of the tongue and taste buds on the epiglottis. Branches of the internal laryngeal nerve (a branch of CN X) supply a small area, mostly somatic (general) sensory but also some special sensation (taste). • Somatic (branchial) motor to the soft palate, pharynx, intrinsic laryngeal muscles (phonation), and a nominal extrinsic tongue muscle, the palatoglossus, which is actually a palatine muscle based on its derivation and innervation • Proprioceptive to the muscles listed above • Visceral (parasympathetic) motor to thoracic and abdominal viscera Nuclei: sensory—sensory nucleus of the trigeminal nerve (somatic sensory) and nuclei of the solitary tract (taste and visceral sensory); motor—nucleus ambiguus (somatic [branchial] motor) and dorsal vagal nucleus (visceral [parasympathetic] motor) (Fig. 10.6). The vagus nerve (CN X) has the longest course and most extensive distribution of all the cranial nerves, most of which is outside of (inferior to) the head. The term vagus is derived from the Latin word vagary, meaning “wandering.” CN X was called that because of its wide distribution extending far from the head (Table 10.5). It arises by a series of rootlets from the lateral aspect of the medulla that merge and leave the cranium through the jugular foramen positioned between CN IX and CN XI (Figs. 10.14 and 10.16).
![<p>Functions: sensory—somatic (general) sensory, special sensory (taste), visceral sensory; motor—somatic (branchial) motor and visceral (parasympathetic) motor. • Somatic (general) sensory from the inferior pharynx and larynx. The vagus provides the afferent (sensory) limb of the cough reflex stimulated by foreign irritants, preventing aspiration and infection. • Visceral sensory from the thoracic and abdominal organs • Taste and somatic (general) sensation from the root of the tongue and taste buds on the epiglottis. Branches of the internal laryngeal nerve (a branch of CN X) supply a small area, mostly somatic (general) sensory but also some special sensation (taste). • Somatic (branchial) motor to the soft palate, pharynx, intrinsic laryngeal muscles (phonation), and a nominal extrinsic tongue muscle, the palatoglossus, which is actually a palatine muscle based on its derivation and innervation • Proprioceptive to the muscles listed above • Visceral (parasympathetic) motor to thoracic and abdominal viscera Nuclei: sensory—sensory nucleus of the trigeminal nerve (somatic sensory) and nuclei of the solitary tract (taste and visceral sensory); motor—nucleus ambiguus (somatic [branchial] motor) and dorsal vagal nucleus (visceral [parasympathetic] motor) (Fig. 10.6). The vagus nerve (CN X) has the longest course and most extensive distribution of all the cranial nerves, most of which is outside of (inferior to) the head. The term vagus is derived from the Latin word vagary, meaning “wandering.” CN X was called that because of its wide distribution extending far from the head (Table 10.5). It arises by a series of rootlets from the lateral aspect of the medulla that merge and leave the cranium through the jugular foramen positioned between CN IX and CN XI (Figs. 10.14 and 10.16).</p>](https://knowt-user-attachments.s3.amazonaws.com/fe9e1c6e-3969-49e4-add3-a7888d4ead6a.png)
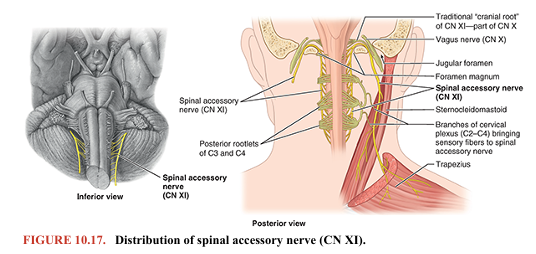
TABLE 10.5. SUMMARY OF VAGUS NERVE (CN X)
What was formerly called the “cranial root of the accessory nerve” is actually a part of CN X (Fig. 10.17). CN X has a superior ganglion in the jugular foramen that is mainly concerned with the general sensory component of the nerve. Inferior to the foramen is an inferior ganglion (nodose ganglion) concerned with the visceral and special sensory components of the nerve (Fig. 10.14). In the region of the superior ganglion are connections to CN IX and the superior cervical (sympathetic) ganglion. CN X continues inferiorly in the carotid sheath to the root of the neck (see Chapter 9, Neck), supplying branches to the palate, pharynx, and larynx and cardiac branches to the cardiac and pulmonary plexuses (Fig. 10.16; Table 10.5)

The courses of the vagi (pl. of vagus) are asymmetrical in the thorax, a consequence of transitions of the great vessels and rotation of the midgut during development (see Chapter 4, Thorax, and Chapter 5, Abdomen). CN X supplies branches to mixed motor and sensory plexuses that serve the heart, bronchi, lungs, and esophagus. Anterior and posterior vagal trunks form as continuations of the esophageal plexus surrounding the esophagus, which is also joined by branches of the sympathetic trunks. The trunks pass with the esophagus through the diaphragm into the abdomen, where the vagal trunks break up into branches that innervate the stomach and intestinal tract as far as the left colic flexure.
The Bottom Line: Vagus Nerve
■ The vagus nerves (CN X) supply motor fibers to the voluntary muscles of the larynx and superior esophagus. ■ They also send visceral motor (presynaptic parasympathetic) fibers to the involuntary muscles and glands of (1) the tracheobronchial tree and esophagus via the pulmonary and esophageal plexuses, (2) to the heart via the cardiac plexus, and (3) to the alimentary tract as far as the left colic flexure via the vagal trunks. ■ The vagus nerves also send sensory fibers to the pharynx, larynx, and reflex afferents from these same areas (1–3 above). ■ They originate via 8–10 rootlets from the lateral sides of the medulla of the brainstem. They enter the superior mediastinum posterior to the sternoclavicular joints and brachiocephalic veins. ■ The nerves give rise to right and left recurrent nerves and then form the esophageal plexus, reform as anterior and posterior vagal trunks, and continue into the abdomen.
SPINAL ACCESSORY NERVE (CN XI)
Functions: somatic motor to the striated sternocleidomastoid and trapezius muscles. Nuclei: The spinal accessory nerve arises from the nucleus of the spinal accessory nerve, a column of anterior horn motor neurons in the superior five or six cervical segments of the spinal cord (Fig. 10.6). The traditional “cranial root” of CN XI is actually a part of CN X (Lachman et al., 2002). It may be united for a short distance with the spinal accessory nerve (CN XI) (Fig. 10.17). CN XI emerges as a series of rootlets from the first five or six cervical segments of the spinal cord. The spinal accessory nerve joins the CN X temporarily as they pass through the jugular foramen, separating again as they exit (Fig. 10.14). CN XI descends along the internal carotid artery, penetrates and innervates the sternocleidomastoid, and emerges from the muscle near the middle of its posterior border. Next, CN XI crosses the posterior cervical region and passes deep to the superior border of the trapezius to descend on its deep surface, providing multiple branches to the muscle. Branches of the cervical plexus conveying sensory fibers from spinal nerves C2–C4 join the spinal accessory nerve in the posterior cervical region, providing these muscles with pain and proprioceptive fibers.
The Bottom Line: Spinal Accessory Nerve
■ The spinal accessory nerves (CN XI) supply somatic motor fibers to the sternocleidomastoid and trapezius muscles. ■ The nerves arise as rootlets from the sides of the spinal cord in the superior five or six cervical segments. ■ They ascend into the cranial cavity via the foramen magnum and exit through the jugular foramina, crossing the lateral cervical region, where pain and proprioceptive fibers from the cervical plexus join the nerves.
HYPOGLOSSAL NERVE (CN XII)
Functions: somatic motor to the intrinsic and extrinsic muscles of the tongue (G. glossa)—styloglossus, hyoglossus, and genioglossus. The hypoglossal nerve (CN XII) arises as a purely motor nerve by several rootlets from the medulla and leaves the cranium through the hypoglossal canal (Figs. 10.2 and 10.3). After exiting the cranial cavity, CN XII is joined by a branch or branches of the cervical plexus conveying general somatic motor fibers from C1 and C2 spinal nerves and somatic (general) sensory fibers from the spinal ganglion of C2 (Fig. 10.18). These spinal nerve fibers “hitch a ride” with CN XII to reach the hyoid muscles, with some of the sensory fibers passing retrograde along it to reach the dura mater of the posterior cranial fossa (see Fig. 8.34B in Chapter 8, Head). CN XII passes inferiorly medial to the angle of the mandible and then curves anteriorly to enter the tongue (Fig. 10.18).
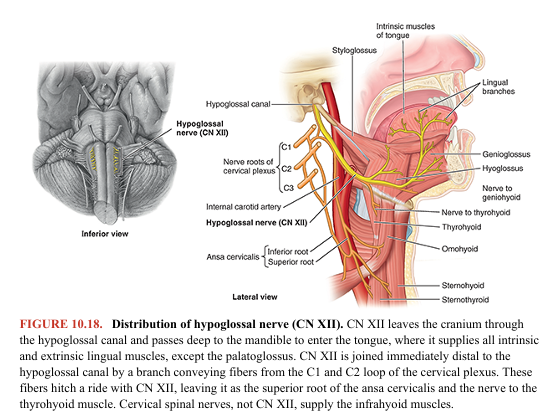
CN XII ends in many branches that supply all the extrinsic muscles of the tongue, except the palatoglossus (a palatine muscle). CN XII has the following branches:
• A meningeal branch returns to the cranium through the hypoglossal canal and innervates the dura mater on the floor and posterior wall of the posterior cranial fossa. The nerve fibers conveyed are from the sensory spinal ganglion of spinal nerve C2 and are not hypoglossal fibers. • The superior root of the ansa cervicalis branches from CN XII to supply the infrahyoid muscles (sternohyoid, sternothyroid, and omohyoid). This branch conveys only fibers from the cervical plexus (the loop between the anterior rami of C1 and C2) that joined the nerve outside the cranial cavity, not hypoglossal fibers (Fig. 10.18). Some fibers continue past the origin of the superior root to reach the thyrohyoid muscle. • Terminal lingual branches supply the styloglossus, hyoglossus, genioglossus, and intrinsic muscles of the tongue.
The Bottom Line: Hypoglossal Nerve
■ The hypoglossal nerves (CN XII) supply somatic motor fibers to the intrinsic and extrinsic muscles of the tongue, except the palatoglossus (a palatine muscle). ■ They arise by several rootlets between the pyramids and the olives of the medulla. ■ They pass through the hypoglossal canals and run inferiorly and anteriorly, passing medial to the angles of the mandible and between the mylohyoid and the hyoglossus to reach the muscles of the tongue.
Because of their location within the confined cranial cavity, relatively fixed positions, and sometimes close relationships to bony or vascular formations, the intracranial portions of certain cranial nerves are also susceptible to compression owing to a tumor or aneurysm. In such cases, the onset of symptoms usually occurs gradually, and the effects depend on the extent of the pressure exerted. Because of their close relationship to the cavernous sinus, CN III, CN IV, CN V1, and especially CN VI are susceptible to compression or injury related to pathologies (infections, thrombophlebitis) affecting the sinus.
OLFACTORY NERVE (CN I)/ Anosmia: Loss of Smell
The loss of smell (anosmia) is frequently associated with upper respiratory infections, sinus disease, and head trauma. Loss of olfactory fibers occurs with aging. Consequently, elderly people often have reduced acuity of the sensation of smell, resulting from progressive reduction in the number of olfactory receptor neurons in the olfactory epithelium. The chief complaint of most people with anosmia is the loss or alteration of taste; however, clinical studies reveal that in all but a few people, the dysfunction is in the olfactory system (Simpson, 2018). The reason is that most people confuse taste with flavor. Transitory olfactory impairment occurs as a result of viral or allergic rhinitis—inflammation of the nasal mucous membrane. To test the sense of smell, the person is blindfolded and asked to identify common odors, such as freshly ground coffee placed near the external nares (nostrils). One naris is occluded, and the eyes are closed. Because anosmia is usually unilateral, each naris is tested separately. If the loss of smell is unilateral, the person may not be aware of it without clinical testing. Injury to the nasal mucosa, olfactory nerve fibers, olfactory bulbs, or olfactory tracts may also impair smell. In severe head injuries, the olfactory bulbs may be torn away from the olfactory nerves, or some olfactory nerve fibers may be torn as they pass through a fractured cribriform plate. If all the nerve bundles on one side are torn, a complete loss of smell will occur on that side; consequently, anosmia may be a clue to a fracture of the cranial base and cerebrospinal fluid rhinorrhea (leakage of the fluid through the nose). A tumor and/or abscess in the frontal lobe of the brain or a tumor of the meninges (meningioma) in the anterior cranial fossa may also cause anosmia by compressing the olfactory bulb and/or tract (D’Amico & Sisti, 2022).
Olfactory Hallucinations
Occasionally, olfactory hallucinations (false perceptions of smell) may accompany lesions in the temporal lobe of the cerebral hemisphere. A lesion that irritates the lateral olfactory area (deep to the uncus) may cause temporal lobe epilepsy or “uncinate fits,” which are characterized by imaginary disagreeable odors and involuntary movements of the lips and tongue.
OPTIC NERVE (CN II)/ Demyelinating Diseases and Optic Nerves
Because the optic nerves are actually CNS tracts, the myelin sheath that surrounds the sensory fibers from the point at which the fibers penetrate the sclera is formed by oligodendrocytes (glial cells) rather than by neurolemma (Schwann) cells, as in other cranial or spinal nerves of the peripheral nervous system (PNS). Consequently, the optic nerves are susceptible to the effects of demyelinating diseases of the CNS, such as multiple sclerosis (MS), which usually do not affect other nerves of the PNS.
Optic Neuritis
Optic neuritis refers to lesions of the optic nerve that cause diminution of visual acuity, with or without changes in peripheral fields of vision (Moss, 2022). Optic neuritis may be caused by inflammatory, degenerative, demyelinating, or toxic disorders. The optic disc appears pale and smaller than usual on ophthalmoscopic examination. Many toxic substances (e.g., methyl and ethyl alcohol, tobacco, lead, and mercury) may also injure the optic nerve.
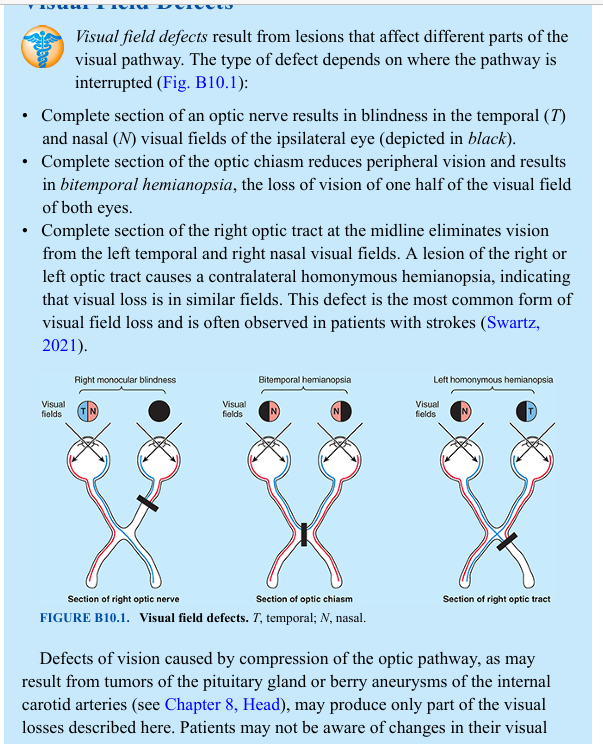
Visual Field Defects
Visual field defects result from lesions that affect different parts of the visual pathway. The type of defect depends on where the pathway is interrupted (Fig. B10.1): • Complete section of an optic nerve results in blindness in the temporal (T) and nasal (N) visual fields of the ipsilateral eye (depicted in black). • Complete section of the optic chiasm reduces peripheral vision and results in bitemporal hemianopsia, the loss of vision of one half of the visual field of both eyes. • Complete section of the right optic tract at the midline eliminates vision from the left temporal and right nasal visual fields. A lesion of the right or left optic tract causes a contralateral homonymous hemianopsia, indicating that visual loss is in similar fields. This defect is the most common form of visual field loss and is often observed in patients with strokes (Swartz, 2021).
Defects of vision caused by compression of the optic pathway, as may result from tumors of the pituitary gland or berry aneurysms of the internal carotid arteries (see Chapter 8, Head), may produce only part of the visual losses described here. Patients may not be aware of changes in their visual fields until late in the course of disease because lesions affecting the visual pathway often develop insidiously.
OCULOMOTOR NERVE (CN III)/ Injury to Oculomotor Nerve
A lesion of CN III results in ipsilateral oculomotor palsy, in which the eye is abducted and depressed, with the pupil dilated. This palsy is summarized in Table 10.6 and discussed and illustrated in the Clinical Box “Paralysis of Extra-Ocular Muscles/Palsies of Orbital Nerves” in Chapter 8, Head
