Biochemistry - Biomolecules + Enzymes
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
Drug definition + types of bonding in biomolecules
Drug = chemical which changes biochemistry
~ To change biochemistry, act on it at a chemical level, need some kind of interaction - bonding.
Covalent:
Rarely used with drugs, as requires high reactivity and often heat.
Exception: cisplatin.
Electrostatic interactions:
Proteins contain both CO2- and NH3+ residues, may be present at binding site to interact with oppositely charged groups on drug.
Ion-ion interactions:
Stronger in a hydrophobic environment, than a polar environment, due to competition by water.
Non directional.
Hydrogen bonds:
Electrostatic interaction between a polarised, delta plus H, with a nearby delta minus atom, bearing a lone pair.
Donor provides H, HBD, while acceptor provides an electron pair, HBA.
~ Size of force (strength of interaction) varies inversely proportional to the square of distance between two ions.
~ Strength of interaction increases as square of charges of each ion.
~ Strength of interaction does not increase linearly with charge of each ion.
R and S enantiomers + Isoelectric point
R = clockwise enantiomers, stereochemistry that are mirror images of each other.
S = anticlockwise enantiomers, stereochemistry that are mirror images of each other.
Isoelectric point = pH at which amino acid exists largely as neutral.
~ For neutral amino acids, the pI is average of the two pKa values.
‘Towards which electrode would a protein with pI 9 move in electrophoresis with a buffer of pH 7?’
As this pH is below the pI, protein will have a net positive charge (and v.v.)
So, positively charged proteins will move towards the negative electrode - cathode.
PANIC for electrodes.
Amino acids basic structure
Always write N-terminus → C-terminus
Anything smaller than 50 amino acids = small molecule, oligopeptide.
Anything greater than 50 amino acids = larger molecule, polypeptide.
Peptide sequence: nitrogen, carbon, carbonyl, repeat…
Amide bond structure + amines vs amides
Amide bond structure:
Nitrogen lone pair is conjugated to the C=O bond, creating a partial double bond between N and C. An amide bond is formed between a carboxylic acid and an amine.
Due to orbital constraints, no free rotation about C-N bond, group is planar.
Amide bonds not easily hydrolysed.
Amines vs amides:
Amines are basic, amine nitrogens are nucleophilic.
Amides are not basic, amide nitrogens are not nucleophilic.
Amines act as nucleophiles, acid derivatives as electrophiles.
DCC is a common activating agent for amide synthesis.
After DCC, EDAC used next most commonly, due to water solubility.
When we react two amino acids by addition together, we end up with a random polymer - polypeptide:
No control of length and sequence.
Use protecting groups (PG) to prevent reaction at undesired state.
Protein structure + Types of secondary and tertiary structure
Primary structure = residue sequence
Secondary structure = local (peptide scale) regular structural motifs.
Tertiary structure = folding of entire protein
Quaternary structure = multiple proteins
Types of secondary structure:
Alpha helix
Beta pleated sheet
Antiparallel, pleated, side chains point up and down.
Beta branched amino acids, bulky aromatic residues.
‘What secondary structure might be promoted by certain amino acids sequence?’
Look up amino acids in table - it states if they are hydrophobic etc.
Beta sheet structure favoured by: hydrophobic amino acids, aromatic ring structures, stacking.
Types of tertiary structure:
Pi-Pi stacking, hydrogen bonds, hydrophobic effect, disulfide bridges, salt bridges.
Disulfide bonds:
Can be broken down by exchange with other thioles.
Require oxidative conditions to form.
Not formed by any amino acid other than cysteine.
Only covalent interaction which determined tertiary structure.
Structure Determination: X Ray Diffraction (XRD), Gel Electrophoresis, NMR Spectrometry
X Ray Diffraction:
Protein in water with non solvent (precipitant) placed on drop on lid.
Non solvent in well/flask.
Water evaporates from drop (equilibrating with non solvent in flask).
Ideally protein crystals form.
Gel electrophoresis:
Use mass/charge ratio to analyse proteins by polyacrylamide gel electrophoresis (GEL).
Under ‘naïve conditions, movement depends on: protein charge, pKa’s and pI.
Proteins can be denatured, given uniform negative charge using sodium dodecyl sulfate - SDS - PAGE more common.
DTT can be used to reduce disulfides.
NMR:
More naïve conditions
Less precise positions
No need for crystallisation
Less automated
Types of proteins + antigen vs antibody
Fibrous proteins create long structures, provides structural integrity to biology.
Globular proteins are individual units, perform more ‘chemical tasks’.
Antigen = a foreign substance that enters the body, creating a response.
Antibody = protein produced by immune system, to attack and fight off antigens.
Nucleotides, Hybridisation + constructing complementary sequences + nucleosomes
Nucleosides = sugar attached
Nucleotides = phosphate attached
Hybridisation = process in which two complementary single stranded DNA and/or RNA molecules bond together, forming a double stranded molecule.
Constructing complementary sequences:
Split strand into three base units, write down complementary bases, then reverse the order, for the 5’ to 3’ format.
E.g., For the sequence 5'-ATCG-3', the complementary bases would be 3'-TAGC-5', which is then written as 5'-CGAT-3'.
‘Melting temp.’ of DNA is when half of strands are in a random coil single strand state.
Double helix:
Negatively charged phosphate groups repel each other.
Base pairs H-bond.
B-DNA + A-DNA = right handed.
Z-DNA = left handed.
Nucleosomes = DNA is coiled around proteins - histones, producing nucleosomes, further packed to produce chromosomes.
Eight protein units are required for each nucleosome.
Polymerase Chain Reaction (PCR) and Transcription
Polymerase Chain Reaction (PCR):
Double stranded template DNA.
Denaturation, at 94 degrees Celsius.
Hybridise primer, at 68 degrees Celsius.
Elongation, at 72 degrees Celsius.
2 x double stranded DNA.
Transcription:
Production of proteins by DNA.
Protein cluster termed ‘transcription factors’ signals to RNA polymerase where to begin transcription.
Resulting strand produced is ‘messenger RNA’ or mRNA, used to make code specific peptide sequences.
RNA also produced 5’ to 3’ direction.
Carbohydrates structure + nomenclature of carbohydrates
Hemiacetals are formed by reaction of a carbonyl and an alcohol.
These structures often are all in eqm. with others, i.e., carbs exist in two forms: linear + cyclic.
C6 (hexose) sugars are in eqm. through hemiacetal formation.
Open chain, pyranose (6 membered ring) and furanose (5 membered ring) forms exist.
Pyranose forms (6) tend to dominate.
Aldehyde carbon in open chain form = anomeric position.
Product of pyranose hemiacetal formation can have resultant OH axial or equatorial at anomeric position.
Axial OH = alpha, equatorial OH = beta
Axial = less stable, equatorial = more stable.
Nomenclature:
Alpha/beta = anomeric configuration
D/L = absolute stereochemistry
Pyran/furan = 6/5 ring form
Glycosides + small molecule part on its own name
= small non sugar molecule found attached through anomeric position to a sugar.
Small molecule part on its own = aglycon
Is form in which many natural products exist, as can store compounds in inactive form.
Lipids + fatty acids (phospholipids, sphingolipids, steroids, cholesterol)
Lipids = group of naturally occurring, hydrophobic molecules
Fatty acids, two parts:
Long hydrocarbon chain, hydrophobic, water insoluble, not reactive chemically.
Carboxylic acid group, ionised in solution, hydrophilic, water soluble.
Readily reacts with a hydroxyl or an amino group on a second molecule to form esters and amides.
Phospholipids:
Comprised of two fatty acids, glycerol, phosphodiester head group.
~ Fatty acids + phospholipids are amphiphilic, as hydrophilic heads and hydrophobic tails.
Sphingolipids:
Linked via sphingosine
Steroids:
Fixed shape, due to cyclisation
Stereochemistry greatly influences shape
Important as hormones, maintenance of homeostasis…
Can be a chemical messenger.
Cholesterol:
Controls membrane fluidity
Membrane bilayers + Factors affecting fluidity + cellular membranes
Membrane bilayers are 2D fluids:
Lateral diffusion occurs rapidly within plane of membrane.
Individual phospholipids may rotate axially or fatty acids tails flex, due to v.d.w. interactions.
Flip-flopping from one side to other is rare, as it is energetically unfavourable, would require head group to pass through non polar layer.
Factors affecting fluidity:
Length - shorter, reduced interactions of hydrocarbon tails, so more fluid.
Saturation - each double bond in an unsaturated tail creates a small kink.
~ Shorter alkyl chains lead to less v.d.w. interactions.
~ Alkene groups make packing more difficult.
Fluidity decreases with:
An increase in membrane’s cholesterol content.
With more saturation of acyl tails as packing of phospholipids is closer.
Cellular membranes are asymmetric:
Two layers of bilayer have different compositions, different phospholipid/glycolipid inside vs outside.
Membrane proteins embedded into membrane with specific orientation.
All lipids are synthesised on cytosolic surface of endoplasmic reticulum, lipids in outer leaflets are transported there by flippases.
Cell membrane
Provides a boundary between living cell and external world.
Hydrophobic layer prevents polar and larger molecules passing through, non polar molecules pass through.
Highly hydrophobic molecules will enter + not leave.
~ Local anaesthetics block conduction of nerve impulses by affecting influx of ions through transmembrane channels.
~ Lipid layer as drug target: inhalable anaesthetics are thought to change neuron membrane permeability, hence signalling.
~ Breaking ‘barrier’, can be done by adding molecules, tunnel + disrupt membrane. Or by adding specific carriers which will bring another molecule across membrane.
Nucleus, nucleosome, chromatin, nucleolus
Nucleus:
Composition = DNA, proteins (histones, transcription factors), lipid membrane.
Nucleosome = basic repeating subunit of chromatin packaged inside cell’s nucleus.
Chromatin = mixture of DNA + proteins that form chromosomes found in cells of humans and higher organisms.
Nuclear membrane consist of glycerophospholipids, sphingolipids, some of which are phosphorylated.
Pores allow proteins in, mRNA and ribosomes out.
Nucleolus:
Densest area of nucleus, site of ribosome production.
Requires RNA transcription + associated with proteins.
Composition: proteins, DNA, RNA
~ Camptothecin = drug which disrupts topoisomerase in nucleolus to stop ribosome production, in cancer.
Cytoplasm + mitochondria
Cytoplasm:
Viscous liquid that fills inside of cells.
Composition = water, ions, small molecules, proteins
More viscous than water
Molecules move slowly due to collisions
Medium for signal transduction
Mitochondria:
Composition: lipids, proteins, DNA, RNA, small molecules
Production of ATP, by ATP synthase, sits on inner membrane
Heat production
Have their own DNA, transcription etc.
Dysfunction contributes to neurodegeneration, metabolic disease, heart failure, infections.
Endoplasmic reticulum (ER) + Golgi apparatus
Endoplasmic reticulum (ER):
Composition: lipids (phospholipids), proteins, RNA
Calcium storage, protein synthesis, lipid metabolism
Continuous with nuclear membrane
Intracellular transport system
Rough ER studded with ribosomes, smooth ER lack these, involved in lipid biosynthesis
Golgi Apparatus:
Helps process and package proteins and lipid molecules, especially proteins, to be exported from cell
Receives proteins from ER in vesicles.
Applies post-translational modifications to proteins
Phosphorylation
Glycosylation
Sulfation
Transports them to internal or external vesicles.
Ribosomes, endosomes + lysosomes
Ribosomes:
Produce proteins by translating mRNA into polypeptides via tRNAs.
Found in cytoplasm, mitochondria, rough ER.
Endosomes + lysosomes:
Endosomes are lipid bilayer bounded compartments within cell
Bud off from ER and G.A. to transport or excrete proteins etc.
Bud off from cell membrane, to allow cell to uptake material from without (endocytosis).
Endosomes can evolve into lysosomes, which are acidic, break down their contents.
Lysosomal escape is critical for nucleic acid therapeutics, since large molecules cannot diffuse through membranes.
Cytoskeleton
Composition: proteins
Helps cells to keep shape, move, divide.
Microtubules:
Polymers of tubulin proteins
Hollow
Transport of organelles
Division of chromosomes
Microfilaments:
Polymers of actin proteins
Double helix
Cell motility contraction
Muscle movement
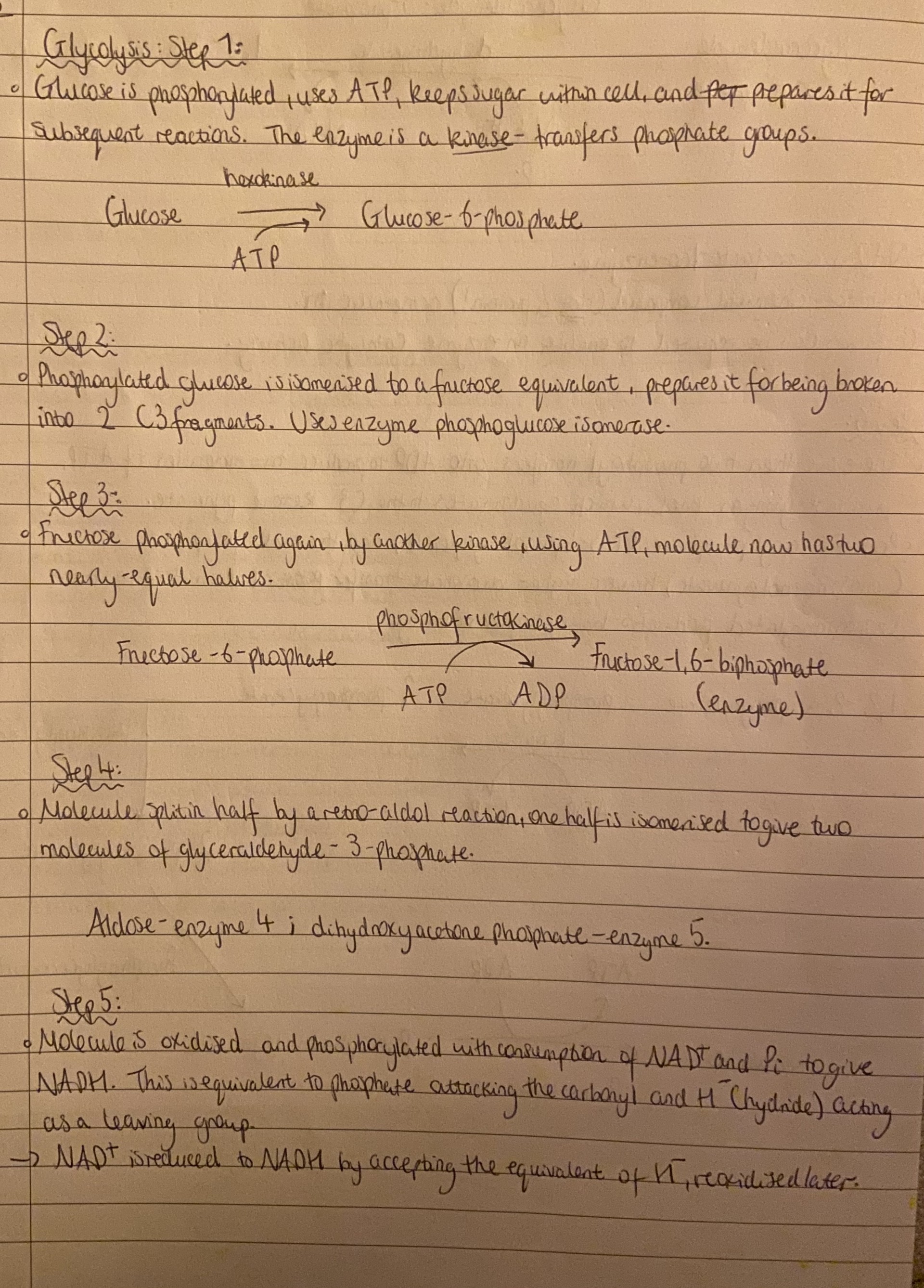
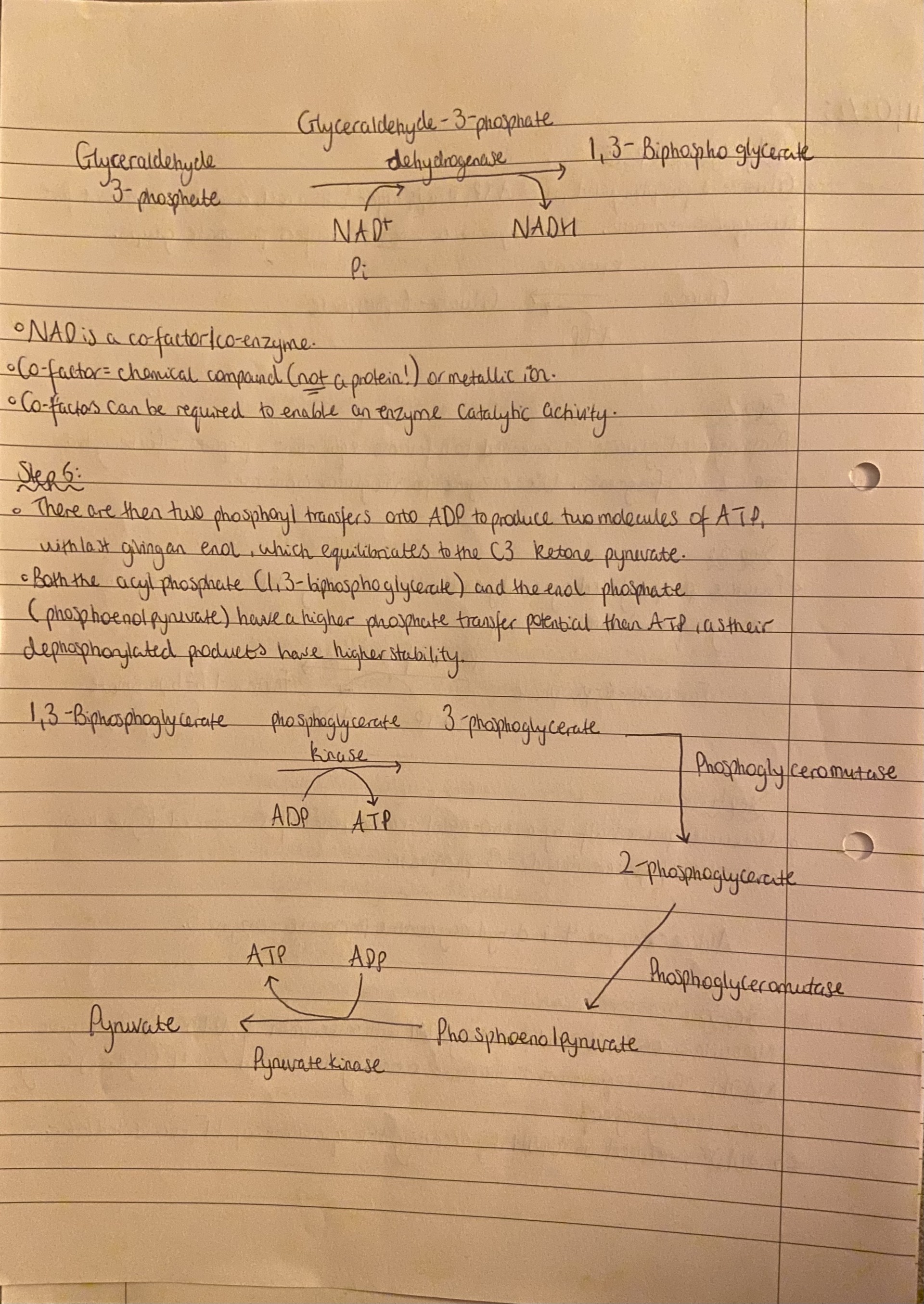
Glycolysis
Glycolysis, overall:
4 x ATP
2 x NADH
2 x pyruvate
And consumed 2 x ATP
Overall + 2 ATP, 2 NADH, 2 pyruvate.
Citric acid/Krebs cycle + net reaction
Citric acid/Krebs cycle:
Glucose, with help of oxygen, from lungs or bloodstream, is broken down into carbon dioxide, and water.
Pyruvate diffuses from cytosol into matrix of mitochondria.
All fuel molecules (sugars, lipids, amino acids), enter cycle as Acetyl CoA.
Net reaction:
Two carbons entered as an acetyl group, and two left as carbon dioxide.
Equivalent of 4 x hydrogens has been released in reduction of NAD+ and FAD.
CoA is regenerated of Ac-CoA.
Carbon atoms of incoming Ac-CoA get integrated into oxaloacetate in one cycle. Next, one is lost as carbon dioxide, other moves down chain two cycles later.
So for one molecule of glucose: 2ATP + 8NADH + 2FADH2 + 2GTP + 6CO2.
Oxidative phosphorylation
Electrons from NADH are passed through membrane proteins on cristae on mitochondria, pumping H+ out as they go, eventually with O2.
Resultant imbalance of H+ across membrane is used to drive ATP synthase as protons flow back in through protein.
Electrons flow from NADH to O2, each step is a small decline in potential, transports protons across membrane.
Protons are removed at oxidative process, takes place on outer side of membrane, leading to a build up of protons in intermembrane space.
Protons can return to matrix by passing through ATP synthase.
Flow of protons in one direction results in transmembrane part of ATP synthase, to rotate.
Results in a sequential change of conformation at the matrix-exposed unit.
Changes in conformation ‘squash’ together ADP and Pi to give ATP.
= ADP + Pi + 4H+ (intermembrane) → ATP + H2O + 4H+ (matrix)
Enzymes - co-factors + prosthetic groups
Enzymes increase rate of reaction by 1011 or higher!
Catalytic activity of enzymes depends on presence of co-factors.
Co-factors either be metal ions or organic molecules.
Loosely bound cofactors = coenzymes
Tightly bound cofactors = prosthetic groups.
Coenzymes:
Small non protein molecules that catalyse reactions.
Transfer electrons, form or break a covalent bond, transfer a group.
Prosthetic groups:
Small inorganic ions, mostly metal ions.
Act as activators and/or inhibitors of activity.
Michaelis-Menten Kinetics, KM
To measure KM and Vmax, measure rate at varying concentrations.
Usually, [S] < KM
KM is a measure of affinity for enzyme for substrate, high KM = low affinity.
Types of enzyme inhibition
Competitive = inhibitor competes reversibly with substrate for active site. Does not change maximum rate of enzyme reaction (Vmax)
Uncompetitive = inhibitor binds only to ES complex, leading to intermediates - rare.
Non competitive = inhibitor binds non covalently to sites other than active site, allosteric inhibition. Changes the tertiary structure and conformation of the active site, whole protein shape. Maximum rate of substrate catalysis reduced (Vmax)
Irreversible = inhibitors form covalent or tight bonds with functional groups in active site.
Substance binds enzyme in such a way that normal ligand cannot displace it, preventing substrate binding.
Enzyme/inhibitor is degraded.
For enzyme system to function, new enzyme has to be synthesised.
General Receptor Principles + Ion channel receptors
General Receptor principles:
Chemical messenger (neurotransmitter/hormone) binds to a receptor.
Induces a change in protein conformation affecting region inside cell.
Changed conformation activates intracellular domain.
After sending message many times, chemical messenger leaves.
Ion channel receptors:
Neurons propagate pulses by letting ions flow in/out.
As ions are polar, they would pass through channel proteins, not through cell membrane.
Most channel protein have narrow, highly selective pores that open/close.
Transport is passive, along concentration gradient.
G protein coupled receptors (GPCRs) + G-protein signal transduction
G protein coupled receptors (GPCRs):
Includes muscurinic, a drenergic, and opioid receptors → nervous system.
Activated by neurotransmitters, ligand binding results in activation or deactivation of certain membrane bound organelles, called G proteins.
1.) G proteins are membrane bound and comprise of 3 subunits (alpha, beta, gamma).
2.) Alpha unit binds guanyl nucleotides, hosts GDP in its resting state.
3.) Activation by GPCR eventually results in cleavage of alpha unit from beta-gamma unit.
G-protein signal transduction:
Ligand binds G protein hosting GDP in the alpha unit.
Binding changes conformation of G protein, releasing GDP, creating a ‘pocket’, binds GTP.
Binding of GTP causes another conformational change, results in alpha unit departing separately.
Alpha subunit with GTP diffuses along membrane to adenylate cyclase, then is activated to catalyse ATP → cAMP.
Alpha subunit has intrinsic GTPase activity, resulting in GTP → GDP after some time.
Reverses binding + deactivates adenylate cyclase.
Phosphorylation + kinase receptors
Phosphorylation:
cAMP activates protein kinase A.
Protein kinase A phosphorylates other proteins.
Phosphorylation changes their conformational + activates them in turn.
Each step can have multiple turnovers = huge signal amplification.
Kinase receptors:
Are simpler than GPCRs.
Binding of ligand extracellular side results in direct activation of proteins as a kinase on intracellular side.
Often binding results in some level of dimerization, turns on activity.
Agonist, partial agonist, antagonist + inverse agonist
Drugs can interact with receptors in four ways:
Agonist = a ligand that binds to, and provokes a signal from a receptor, via conformational changes to produce active state. Typically binds in a similar way to natural ligand.
Partial agonist = binds and provokes a signal, but diminished compared to full agonist. Binding is suboptimal and conformational switch may not fully engage.
Antagonist = a ligand that binds to a receptor and induces no signal, blocks agonist binding, hinders conformational switch to active site.
Inverse agonist = removes any base level activity the receptor had in absence of ligand.
Competitive + non-competitive antagonists
Competitive reversible antagonist:
Binds to same receptor site as an agonist
Inhibition is reversible as can be overcome by increasing agonist conc.
~ Maximum response for agonist occurs at a higher conc. than in absence of antagonist.
Competitive irreversible antagonist:
Binds to same receptor sites as agonist
Inhibition is irreversible and cannot be overcome by increasing agonist conc.
Non competitive antagonist: (always irreversible)
Does not bind to same receptor sites as agonist
Decreases affinity of receptor for agonist: allosteric inhibition
Inhibition cannot be overcome by increasing agonist conc. (as irreversible)
Agonist maximal response will be depressed, agonist potency may or may not be affected.
Drug definitions, natural products benefits + drawbacks + phenotypic drug discovery
Drug:
1.) A chemical or substance used to prevent or cure a disease.
2.) A substance which has a physiological effect when introduced to body.
Natural products
Benefits:
All natural products have some kind of biological activity already.
Could be produced by agricultural or or biotechnological methods.
Provides access to unusual/diverse structures.
Drawbacks:
Difficult in obtaining high yields
Total synthesis challenging
Compounds not optimised
Could be allergens
Phenotypic drug discovery:
Phenotypic screening = approaches looking only at final effect of a drug, rather than relying on knowledge of how drug works.
Can also work for larger libraries of synthetic compounds, not natural products.
Fitting drug to target - docking, binding site mapping + denovo drug design
Modifications can make drug stimulate receptors’ signalling (agonist) or disrupt it (antagonist), depending on how it binds.
Docking = calculate where and how well a molecule binds to target, often using a large virtual library of compounds which could be synthesised.
Binding site mapping = creating a model illustrating what arrangement of intermolecular interactions can be addressed.
Denovo drug design = de novo asks computer to generate a molecule which could bind in chosen site.
~ De novo drug design will usually map desired interaction site, dock fragments, and link up fragments in a synthetically realistic way.
Designed synthetic compounds + screening and selection benefits and drawbacks
Designed synthetic compounds:
Benefits:
Synthesis straightforward
Readily modified at any point to tune properties
Mechanism of action usually well understood
Drawbacks:
Limited to molecules which are easily made
Chirality and larger structures rarer.
Does not work so well on proteins without small molecule binding pockets.
Screening and selection:
Measure each molecule’s interaction with target
Use some affinity measurement to separate binders from non binders.
Benefits:
Test millions of molecules at a time
Could uncover unexpected activities
Exploit molecular biology techniques
Target any protein with larger molecules.
Drawbacks:
Limited to libraries which can easily be made
Larger molecules may have trouble getting through membranes
Biological assays + hit-to-lead and lead optimisation
Biological assays:
In vitro = on isolated cells, tissues, proteins
~ Usually preferred for initial tests, as is cheaper, quicker, less controversial. Will test whether drug engages target, whether it changes target’s activity, whether it kills cells, often fluorescent output.
In vivo = on entire organisms, no difference it looking at bacteria
~ Performed on a smaller section of compounds, e.g., mice. Uncovers information about system toxicity + absorption, distribution, metabolism, excretion (ADME).
Hit-to-lead and lead optimisation:
Hit-to-lead compounds from library are short listed according to:
Synthetic accessibility, specificity, toxicity, physical properties
Lead optimisation, compounds will be optimised for:
Physiochemical properties, ADME, toxicity
Clinical Trials - Phases
Phase I:
Testing safety in a small group of healthy volunteers (10-100). Safe dosages established, and how body processes drug (pharmacokinetics) monitored. Unblinded = both doctors and patients know if given the drug, and what it contains.
Phase II:
Small scale test for efficacy, 50-500 patients, with disease. Safety + pharmacokinetics monitored, placebos act as comparison. Either single blind (patient unaware if they are in test or placebo group) or double blind (both unaware).
Phase III:
Large scale test for efficacy, 500-3000 patients, with disease. Stringent comparison to existing treatment, randomised controlled double blind trials.
If successful, company applies for approval.
Phase IV:
Follow up studies are conducted post approval to monitor, response in wider population.
Pharmacology - pharmacokinetics vs pharmacodynamics
Pharmacokinetics:
How the body deals with the drugs.
Fate of drugs once ingested
Variability of response between patients
How drugs move through body (ADME)
Pharmacodynamics:
Effects drug has on body
How drug binds to binding site
How drug reaches binding site
Drug administration, route, local routes, deeper tissues, arterial supply + systematic route
Administration:
Drugs may be: acidic, basic, neutral.
Small organic molecules, large polymers (proteins, carbohydrates)
Route of administration - (depends on):
Physical + chemical property of drug (pH, solubility)
Site of desired action - localised, generalised
Effect of digestive juices and first pass metabolism of drug
Condition of patient, unconscious, vomiting
Local routes:
Typical - external application of drug to surface, e.g., lotion, cream powders, spray, drops.
Deeper tissues - certain deep areas can be approached by syringe + needle:
Intracellular (joint)
Intramedullary (bone marrow or spinal cord)
Intrathecal pump (spinal fluid)
Arterial supply - closed intra arterial injection, e.g., angiography + anticancer drugs.
Systematic routes - Systematic circulation is part of cardiovascular system which carries oxygenated blood away from heart to body, returns deoxygenated blood back to heart.
Routes to systematic system + advantages and disadvantages of each
1.) Oral
Self medication, larger area for absorption, easy to take, both solid and liquid forms available.
Potentially causes negative side effects, patient cannot take if unconscious.
2.) Sublingual: kept under tongue or crushed + spread over mouth
Rapid absorption
Liver is passed, directly in systemic circulation
Drug can be consumed for unconscious patients
Only lipid and saliva soluble drugs
Uncooperative patients
Irritate mucosa
3.) Intradermal, Subcutaneous, intramuscular:
Intradermal - e.g., sensitivity tests
Subcutaneous - self injection, e.g., insulin
Intramuscular - for nausea + vomiting, RNA vaccines
4.) Intravenous: direct entry to systemic circulation, rapid onset of action, can deliver large volumes.
Quick action, emergencies
Desired conc. easily obtained
Drugs can be taken on unconscious patients
Costly, potential irritation, self medication not possible
Lipinski’s Rule of 5
~ States that in general, an orally active compound has no more than one violation of:
< 5 H bond donors (count no. of NH and OH)
< 10 H bond acceptors (count no. of N and O atoms)
Molecular weight < 500
Log P < 5
ADME definitions
Absorption = process which a drug moves from its site of administration to systemic circulation.
Distribution = reversible transfer of a drug to and from systemic circulation.
Metabolism = any chemical alteration, of a drug, by lining system to enhance water solubility, hence excretion.
Excretion (elimination) = irreversible transfer of a drug from systemic circulation, e.g., renal excretion, sweat.
Properties of oral drugs + bioavailability of drugs
Oral drug must be able to:
Dissolve
Survive a range of pHs
Cross membrane
Survive liver metabolism
Avoid excretion to kidneys
Avoid partition into undesired places, e.g., brain
Partition into target organ
Bioavailability of drug = refers to fraction of drug that is available in blood supply, after administration:
Dose → Destroyed in gut → Not absorbed → Destroyed by gut wall → Destroyed by liver → Systemic circulation
Plasma concentration/time profiles
Oral does taken, absorbed, enters bloodstream, conc. increases.
Compound distributes into tissues + absorption rates slow
Drug is metabolised and excreted from systemic circulation
Activity at desired target sufficient to achieve the Minimum Effective Concentration (MEC).
Ensures that the conc. does not reach levels which might cause side effects, etc. exceeding the Maximum Tolerated Concentration (MTC).
~ Hence drugs taken 2 x day, to increase the conc. after it decreasing slightly after first dose.
~ Conc. reaches a steady state, amount dosed - Css.
Factors affecting absorption
Acid stability:
Tablet passes through stomach (pH ~ 2), before reaching systemic circulation.
pH of small intestine is (~ 7), large S.A. for absorption.
Basic compounds will not be so well absorbed in stomach, compared to acidic compounds, since is generally the unionised drug form which diffuses into bloodstream.
Solubility + permeability:
Poor aspects of this = poor absorption
Lipophilicity:
Sufficiently lipophilic to cross cell membranes, yet polar enough to be water soluble.
Metabolism - gut wall/first pass metabolism:
Some of compound may be metabolised (first pass metabolism), before reaching systemic circulation.
Absorption mechanisms
Transcellular absorption:
Main route for most oral drugs
Drug must be unionised
Lipophilicity important
Along conc. gradient
Paracellular absorption:
Drug passes through gaps between cells
Inefficient, pores have less S.A. than cellular surface
Restricted to low molecular weight (< 200) molecules
Distribution + plasma protein binding (PPB)
Factors affecting distribution:
pKa, lipophilicity, plasma protein binding
Tissue pH is lower than plasma blood pH
So, basic compounds tend to distribute out of plasma, into tissue, more than acidic compounds.
Plasma protein binding (PPB):
Compounds with high PPB are retained in plasma, no distribution into tissues
Blood contains enzymes, degrades drugs
~ Serium albumin is most abundant protein in blood, binding various hydrophobic molecules in a non specific fashion, preference for fatty acids + steroids.
~ Basic drugs → bind to alpha-1-glycoprotein
Drug metabolism concepts + factors affecting metabolism
Drug metabolism concepts:
Metabolism divided into two categories:
Catabolism = breaking down of organic substances
Anabolism = building up/synthesis of substances
Factors affecting metabolism:
Complex sites = more potential sites for metabolism
Altering sites of metabolism improves availability of drug
~ Hydrophobic compounds are metabolised during two metabolic phases:
Phase I:
Oxidative transformations, catalysed by enzyme cytochrome (CYP)
Production of new polar groups by oxidation, reduction, hydrolysis.
Phase II:
Conjugation - original drug made polar by conjugation reactions
Prodrugs
An inactive compound being converted to an active compound
Usually through metabolic processes, improves ADME.
Improves membrane permeability by reducing polarity.
Esters broken down by endogenous esterates
Slow release of drug, prolonging drug activity
Mask toxicity, side effects
Alter physiochemical processes
Tap into metabolic pathways
Urine formation + renal excretion
Urine formation:
Tubular formation:
Removal of water and solutes from filtrate
Water and solutes return to blood via peritubular capillaries
Tubular secretion:
Transport of excess solutes and wastes to peritubular fluid into tubular fluid
Renal excretion of drugs:
All unbound drug in plasma is filtered in glomerulus
Some compounds are actively secreted into urine along proximal tubule
Unionised drug can undergo passive reabsorption from urine into blood along length of nephron
Drug that is bound to plasma proteins not filtered.
Formulation of drugs
Active pharmaceutic ingredient (API), drug itself, is combined with excipient (other ingredients which improves its delivery, quality)
Filters = bulking agents which make a small quantity easier to handle (e.g., starch, calcium)
Lubricants/antiadherents = reduce friction during manufacturing
Binders = polymers used to turn powders into granules + pills (e.g., gelatin)
Preservatives = usually anti-oxidants, (e.g., vitamin C), or antifungal, bacterials
Flavourings = sweeteners (usually artificial), masking unpleasant taste
Coatings = protects from taste, capsules coated in gelatin, all dissolves in stomach
Vehicles = in liquids, and gels, rest of liquid: water, mineral oil
Bacteria - gram positive vs gram negative + mechanisms of antibacterial action
Positive:
Thick, outer wall
Inner membrane
Dye can access and retained in wall
Negative:
Thin wall between two membranes
Dye easily washed out
More resistant to antibiotics, due to double layer
Mechanisms of antibacterial action:
Inhibition of metabolism:
Antimetabolites interfere with bacterial, but not human metabolism
Usually target a specific bacterial enzyme
Inhibition of cell wall synthesis:
Humans have no cell wall, so bacteria specific, e.g., penicillins
Interaction with plasma membranes:
Bacterial membranes have a different composition, can be targeted
Disruption of protein synthesis:
Interfere with bacterial translation machinery
Inhibition of nucleic acids transcription + replication:
Prevents cell division + protein production
Bacterial cell wall structure
Cell wall made of peptidoglycan - cross linked to make cell wall strong, achieved by an enzyme transpeptidase, replaces terminal D-Ala with end of Gly4 branch of a nearby chain (enzyme which penicillin inhibits).
Layers of parallel alternating NAM and NAG
NAM has a carboxylic acid which is starting point for attachment of an unconventional peptide
Contains D amino acids, as well as ‘normal’ D amino acids
Glutamate is connected via its side chain carboxylic acid
Resistance to penicillin + vancomycin
Penicillin:
Gram negative bacteria can be resistant to it, due to outer membrane being low permeability.
Some bacteria have developed beta-lactamases mutated transpeptidases, decomposes penicillins.
Vancomycin:
Core of structure is heptapeptide, aromatic rings not free to rotate
Vancomycin binds to D-Ala-D-Ala, involved in cross linking
Steric bulk prevents enzymatic access
Bacteria replace final D-Ala with D-lactic acid, introducing repulsive interactions, D-lactic acid not in way of cross linking.
Disrupting cell membranes - valinomycin + polymxin B, + aminoglycosides
Valinomycin (isolated from certain bacteria):
Provides a hydrophobic shield for K, ions. K+ is usually at a higher conc., inside cell - valinomycin will equilibrate it with surroundings
Polymxin B (from soil bacterium):
A lasso shaped peptide featuring hydrophobic anchor and non standard amino acids
Causes leakage of small molecules
Aminoglycosides:
Protonated around neutral pH
Aids their transport through outer membrane of gram -ve bacteria, comprised of mainly anionic lipids
Highly polar molecules are poorly bioavailable, if taken orally, often given intravenously, but oral formulations are available.
Aminoglycosides form many H bonds with sugar phosphate backbone on RNA in which they bind prevents movement of ribosome along mRNA by flipping out bases which get in way
Bacteria develop resistance by evolving enzymes modifying structure - acetylation of amino groups, phosphorylation of hydroxyl groups.
Tetracyclines + chloramphenicol + macrolides
Tetracyclines:
Against both gram +ve and -ve bacteria
Inhibits protein synthesis, preventing tRNA from binding to ribosome
H bonds find an area in bacterial ribosome, complemented by pi-pi stacking with a nucleobase
Chloramphenicol:
Conjugation to an acid by excretion, occurs in Phase II metabolism
Binds large ribosomal subunit, prevents transfer of incoming amino acid
Drug binds through pi-pi stacking, H bonds, O-K+ coordination
Develop resistance by acetylating primary O-H to prevent K+ coordination
Macrolides:
Also binds large ribosomal subunit, prevents transfer of incoming amino acid
Cancer - metastasis definition + causes of mutations + treatments
Metastasis = cancer cells invading other parts of body, starting new tumours
Causes of mutations:
Chemical damage (smoking, diet, pollution)
Viruses (potentially leading to cancer)
Genetics
Random mistakes in biochemistry
Treatments:
1.) Surgery - cancer cut out, for those which are localised.
2.) Radiotherapy - kills cells by radiation, often after surgery
3.) Chemotherapy - using medicines (chemicals) to kill cells
Anticancer cells generally cytotoxic
Drug design aims to make compounds more toxic to cancer cells, but difficult, as cells come from same source as normal cells.
Kinase Inhibitors + targets
Kinases are enzymes which perform phosphorylation reactions.
Changes structure + function of phosphorylated protein
Phosphorylation often used to activate another kinase
Signal transduction from receptors to nucleus
Targets:
1 = Drug binds active conformation
2 = Drug binds inactive conformation
3 = Drug binds nearby hydrophobic pocket
4 = Drug binds elsewhere (allosteric site)