Diversity in Cognitive Aging Quiz 2
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
normal aging
age-relative cognition declines, but is never impaired
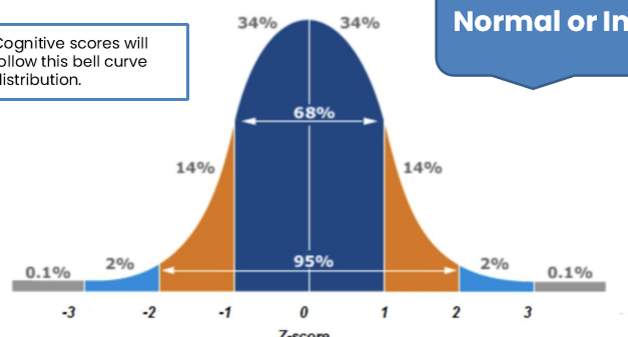
impaired cognition score on normal distribution
bottom 16%
pathological aging
when people perform in the impaired range on 1 or more cognitive tests within a cognitive domain
dementia
syndrome associated with changes in thinking, emotions, and behavior that impair an individual’s capacity for independent living
syndrome
a constellation of signs and symptoms that often occur together
sign
objective measurable phenomenon observed by another person
symptom
subjective experience of individual affected
major neurocognitive disorder
-evidence of significant cognitive decline in 1 or more cognitive domains based on:
concern of the individual, a knowledgeable informant, or the clinician
a substantial impairment in cognitive performance, preferably documented by standardized neuropsychological testing
-the cognitive deficits interfere with capacity for independence in everyday activities
-synonymous with the term dementia
mild cognitive impairment (MCI)
-term used to describe the condition of individuals whose cognition lies between the cognitive changes of normal aging and early dementia
-patient has objective evidence of cognitive impairment that represents a decline from the past, but their independent activities of daily living are intact
mild neurocognitive disorder
-evidence of a modest cognitive decline in 1 or more cognitive domains based on:
concern of the individual, a knowledgeable informant, or the clinician
a modest impairment in cognitive performance, preferably documented by standardized neuropsychological testing
-the cognitive deficits do not interfere with capacity for independence in everyday activities
-synonymous with the term mild cognitive impairment
cortical dementia syndromes
deficits arising from brain damage that primarily affects the cerebral cortex
subcortical dementia syndromes
deficits arising from brain damage that primarily affects subcortical structures (e.g. basal ganglia, thalamus)
primary cortical pathology
Alzheimer’s disease, frontotemporal dementia
primary subcortical pathology
Parkinson’s disease, Huntington’s disease
primary cortical and subcortical pathology (mixed)
dementia with Lewy bodies, vascular dementia
AD signs
formation of amyloid plaques and tau tangles, cortical atrophy, neuron loss, synapse loss
amyloid cascade hypothesis
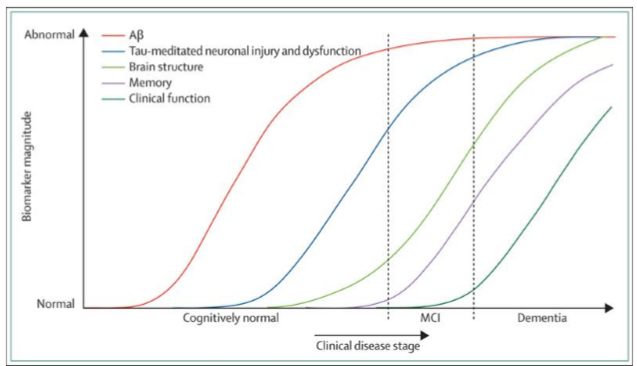
accumulation of amyloid plaques cause tau tangles, which affects brain structure, which affects memory, which affects clinical function
not the right disease model for all races/ethnicities
early-onset AD (EOAD)
-before 65
-5-10% of all AD cases
-sporadic or familial
-PSEN1, PSEN2, APP are deterministic genes that virtually guarantee that an individual will develop AD
late-onset AD (LOAD)
-after 65
-about 90% of all AD cases
-apolipoprotein E (APOE) is a risk gene for LOAD
APOE gene
-provides instructions for a protein called apolipoprotein E, which affects the pathogenesis of AD through multiple pathways, including the differential regulation of Aβ (key component of amyloid plaques) aggregation and clearance
-3 allelic variants: e2, e3, e4
-e4 variant has highest risk for Aβ aggregation and clearance; increases risk for Alzheimer’s disease and earlier onset
-e2 may provide some protection against the disease
-e3 plays a neutral role
signs of AD
language production and comprehension
prominent amnesia with rapid forgetting
marked executive dysfunction
visuospatial impairments
processing speed
a significant deficit in episodic memory is usually the earliest and most prominent manifestation of AD
early stage of AD (2-4 years)
signs and symptoms often not recognized by friends and family
repeatedly asking questions or making statements
misplaces items
gets lost easily
word-finding problems
personality changes (irritability, anger)
middle/moderate stage of AD (2-10 years)
signs and symptoms usually obvious to family and others
wandering, pacing, disruptive behaviors
delusions (often paranoid) and hallucinations
require supervision
sleep cycles disturbed
sun-downing and radical mood swings common
require help with basic care activities
late/advanced stage of AD (last 1-3 years)
little or no self care activities
cannot speak or understand language
bedbound, chair bound, unable to walk
cannot recognize even closest relatives
difficulty swallowing, pneumonia is common
brain no longer can control body
AD treatment
symptomatic drugs
address the cognitive and behavioral symptoms of AD
do not stop or prevent disease
disease modifying drugs
affect the underlying pathology
designed to prevent onset or progression of AD
PD
progressive neurodegenerative disorder that affects balance and motor control regions of the brain
early onset before 50; late onset after 50 (more common)
first symptom is often resting tremors
starts on one side then becomes bilateral
PD pathology
progressive neurodegenerative condition characterized by loss of dopaminergic neurons in basal ganglia and substantia nigra
main pathology is alpha synucleinopathy (Lewy body)
PD motor symptoms
tremors, rigidity, postural instability, bradykinesia
PD non-motor symptoms
constipation, low BP, sexual dysfunction, urine incontinence, apathy, depression, visual hallucinations, drooling, dysphagia, fatigue/sleep problems, speech problems, masked facies
cognitive symptoms in PD
visuospatial impairments
memory profile: retrieval deficits
marked executive dysfunction
micrographia
neuropsychiatric features: apathy, anxiety, depression
dysphonia and dysphagia
AD memory deficit
encoding
PD memory deficit
retrieval
treatment of PD
symptomatic in nature
pharmacotherapy
dopaminergic drugs
behavioral
speech therapy
occupational therapy
physical therapy
exercise programs
surgical
deep brain stimulation
vascular cognitive impairment prevalence
hard to determine
overlap with AD (34% of all dementia have vascular pathology)
inconsistent criteria and cognitive findings
vascular dementia
due to single or multiple infarcts
white matter hyperintensities: chronic hypoperfusion and degeneration of white matter; small vessel disease
related to hypertension and has other vascular risk factors
associated with greater risk of stroke, cognitive impairment, progressive cognitive decline
heterogeneous causes (many different causes)
lack of pathologic diagnostic framework
linked in time or anatomy to vascular disease
cognitive deficits in vascular dementia
attention/processing speed impaired
more severe executive dysfunction
memory profile: retrieval deficits
executive dysfunction is generally more severe than memory declines
limbic-predominant age-related TDP-43 encephalopathy (LATE)
new
can cause scarring of the hippocampus
people diagnosed with AD may actually have LATE
caused by a different type of tau
need better in-vivo biomarkers
health inequality
differences in the health of individuals or groups; absent from the definition of health inequality is any moral judgement on whether observed differences are fair or just
health inequity/health disparity
-specific type of inequality that denotes an unjust difference in health
-health differences that are avoidable, unnecessary, and unjust
health inequalities are not all ____________
-health disparities
-ex: a higher rate of arm injuries among professional tennis players than in the general population
healthcare disparity
differences between social groups in health insurance coverage, access to and use of care, and quality of care
why are there disparities?
produced and sustained by deeply entrenched systems of power and structural drivers that are not based on what is morally right or fair
structural racism
-societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice
-denial of structural racism a consequence of these systems
health equity
absence of unfair and avoidable or remediable differences in health among social groups
Heckler report on Black and minority health
examined the health status of Americans by race/ethnicity and identified the gaps in disease rates, mortality, and other outcomes among Blacks compared to Whites
helped lead to the creation of the NIH officed of minority health and health disparities
found that Black people experienced about 60,000 excess deaths each year for people under 70
race
socially constructed way of grouping people, based on skin color and other apparent physical differences
ethnicity
socially constructed way of grouping that emphasizes cultural commonalities
Hispanic/Latinos is the largest minority group in the US
US census racial categories
white, black/African American, American Indian/Alaska native, Asian, native Hawaiian/other Pacific islander, some other race
which racial/ethnic group has the highest rate of dementia?
Hispanic
dementia prevalence vs race
blacks and whites prevalence has decreased
gap between blacks and whites has decreased
Hispanic prevalence has been stable over time
gap between Hispanics and whites increasing
Asian American AD
less likely to have AD
only 18% of Asian Americans are aware of MCI
harder for individuals or families to recognize symptoms and seek professional care
African American and Hispanic disparities in AD
more likely to get AD, but less likely than whites to have a diagnosis
typically diagnosed in later stages of the disease and therefore in need of more medical care (more expensive)
less likely to be included in clinical trials and have not been included in most AD research initiatives
why are African American and Hispanic older adults less likely to be diagnosed with AD and why aren’t they included in AD clinical trials?
less likely to present for care
less likely to have access to early/critical care initiatives
clinicians may have a harder time diagnosing earlier stages of MCI/dementia
neuropsychological measures are culturally based
clinicians are not adequately trained or prepared to consider relevant cultural factors of influence
perceptions of care and historical injustices
discrimination
underlying pathology
different for racial/ethnic minority groups, likely because these groups are at increased risk for other detrimental health conditions (esp cardiovascular health conditions)
racial differences in mixed pathology
whites more AD while blacks more AD/LB
Hispanics smallest proportion of pure AD pathology
blacks and Hispanics greater proportions of cardiovascular disease and AD + CVD
racial/ethnic disparities in AD summary
racial/ethnic minority groups are at increased risk for AD
likely the consequence of social disadvantage and other disparities
seem to be general differences but needs to be further explored
manifestation of AD (prevalence of amyloid/tau) differs across groups (relevant to treatments)
racial/ethnic disparities in neural imaging
black and Hispanic AD caused more by sociodemographic factors and mixed pathology
white AD caused more by amyloid and APOE e4
WEIRD problem in science
western, educated, industrialized, rich, democratic
inclusion in clinical trials
minority groups make up about 39% of the US population but are under enrolled in clinical trials
largest minority in US
Latinos
sex assigned at birth
sex assignment by doctors that is usually based on genitals
gender identity
internal experience and understanding of our own gender
gender expression
the way in which we present ourselves, which can include physical appearance, clothing, or behaviors
sexual orientation
different forms of attraction; can be attracted to one gender, multiple genders, or different genders throughout your life
sexual minority
encompasses lesbian, gay, two-spirited, bisexual, and queer identifying populations
gender minority
umbrella term for transgender and non-binary people whose gender identity/expression does not conform to social expectations based on their sex assigned at birth
issue 1 for SAGM
LGBT older adults are more likely to age without a spouse or partner, more likely to live alone, and less likely to have children to support them
issue 2 for SAGM
LGBT older adults have a greater number of chronic diseases (HIV/AIDS, diabetes, cardiovascular disease) when compared to their non-LGBT peers, and LGBT elders of color face greater health disparities than their white LGBT counterparts (many of these health conditions have been linked to an increased risk of AD and VD)
issue 3 for SAGM
these disparities mean that this population needs supportive services, but many LGBT elders experience barriers to accessing help, including discrimination, heterosexist attitudes, and a lack of cultural competence on the part of providers
rainbows of aging preliminary findings
at increased risk for dementia due to health disparities
higher levels of subjective cognitive complaints
underserved within our healthcare system
face unique financial and social caregiving barriers
less likely to seek out medical care
SAGM study 1
examined ICD-9 diagnostic codes in electronic health records
trans people more likely to be on disability
trans people experience multiple chronic conditions at higher rates than CMBs
SAGM studies 2 and 3
8% LGB vs 9% heterosexual were diagnosed with dementia
8% opposite-sex vs 12% same-sex were diagnosed with dementia (not statistically significant)
bias
systematic error in an epidemiologic study that results in an incorrect estimate of the association between exposure and the health outcome
sources of bias
data source, data collection, sexual/gender identity categorizations within the study, disclosure of relevant information, ICD-10 codes, and how dementia was diagnosed
selection bias
occurs when the subjects studied are not representative of the target population about which conclusions are to be drawn (study 2 (Kaiser Permanente study) was predominantly white, educated, middle-class older adults)
measurement bias
is a distortion in the measurement of an association that is caused by inaccurate measurements of key study variables (how we measure who is and isn’t LGBT (ICD-10 codes), as well as who does and does not have dementia impacts our observation of an association)
SAGM study 4
significantly higher rates of subjective cognitive decline in 16% LGBTQ+ group vs 11% non-LGBTQ+
highest in bisexuals, then trans people, then lesbians, then gays
HIV associated neurocognitive disorder (HAND)
clinical diagnostic criteria differs from other neurological disorders/dementias
neurocognitive profile indicates impairments across multiple cognitive domains
executive dysfunction is more common than memory problems
can be diagnosed at any point in time
HAND/HAD are analogous to __________
HAND analogous to MCI (mild neurocognitive disorder)
HAD (HIV associated dementia) analogous to major neurocognitive disorder
HAND/HAD
not amyloid or tau causing problems but poor immune functioning has negative effects on the brain
Nadir CD4 count is best predictor of whether someone will have HAND (lower than healthy adults)
when you have a low CD4 count, you have an increased risk for opportunistic infections
rates of HAND/HAD have decreased since antiretroviral therapy and are on the decline with PrEP
ADRD in SAGM summary
research on understanding cognitive aging, brain health, and dementia risk in LGBTQ+ members started very recently
large retrospective epidemiological studies of dementia prevalence have been mixed and may be subject to bias
LGBTQ+ have more subjective cognitive complaints and demonstrate health disparities (chronic disease burden, HIV) that place them at risk for dementia
stigma, caregiving, and income factors are also necessary points of consideration for management of dementia
IOM report conclusions
sex is an important human variable that should be considered in health-related research, as there are sex differences in health and illness
the study of sex differences needs to move beyond descriptions into a mature science that explores biological mechanisms
there have been profound barriers to the advancement of knowledge about sex differences that must be eliminated
sex differences
differences in immune function
differences in symptoms, type, and onset of cardiovascular disease
differences in response to toxins
differences in brain organization
differences in pain
sex differences in AD risk
increased in women but most likely due to the fact that women live longer than men on average