Liver - 3 lecture series overview
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
Functions of the liver
1. Metabolism of Carbohydrates / Proteins / Fats / Hormones / Drugs/toxins)
Carbohydrates: Glycogen storage, gluconeogenesis, glycogenolysis.
Proteins: Deamination of amino acids, urea synthesis (detoxifies ammonia).
Fats: Beta-oxidation, lipoprotein synthesis (VLDL, HDL), cholesterol metabolism.
Hormones: Breaks down insulin, aldosterone, steroid hormones.
Bilirubin: Conjugates indirect (unconjugated) bilirubin → direct (conjugated) for excretion.
Drugs/toxins: Detoxifies via cytochrome P450 enzymes (Phase I/II reactions).
2. Synthesis of Proteins / Cholesterol for Bile / Vitamin D
Proteins: Albumin (maintains oncotic pressure), clotting factors (I [fibrinogen], II, V, VII, IX, X).
Cholesterol: Precursor for bile acids/steroid hormones.
25-OH Vitamin D: Converts vitamin D to its storage form.
3. Immunological
Kupffer cells (liver macrophages): Phagocytose bacteria, old RBCs, toxins from portal blood.
4. Storage
Vitamins: A, D, E, K (fat-soluble), B12, folic acid.
Minerals: Iron (as ferritin), copper.
Glycogen: Glucose reserve.
5. Homeostasis
Blood glucose: Balances glycogen storage/release.
Blood volume: Albumin maintains osmotic pressure.
6. Bile Production & Enterohepatic Circulation
Bile salts: Emulsify fats (essential for digestion).
Recycles bile acids (95% reabsorbed in ileum).
7. Clearance
Bilirubin: Removes heme breakdown products.
Drugs/toxins: Metabolizes and excretes toxins (e.g., alcohol, medications).
![<p><strong>1. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Metabolism of Carbohydrates / Proteins / Fats / Hormones / Drugs/toxins)</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Carbohydrates</strong>: Glycogen storage, gluconeogenesis, glycogenolysis.</p></li><li><p class="ds-markdown-paragraph"><strong>Proteins</strong>: Deamination of amino acids, urea synthesis (detoxifies ammonia).</p></li><li><p class="ds-markdown-paragraph"><strong>Fats</strong>: Beta-oxidation, lipoprotein synthesis (VLDL, HDL), cholesterol metabolism.</p></li><li><p class="ds-markdown-paragraph"><strong>Hormones</strong>: Breaks down <strong>insulin, aldosterone, steroid hormones</strong>.</p></li><li><p class="ds-markdown-paragraph"><strong>Bilirubin</strong>: Conjugates indirect (unconjugated) bilirubin → direct (conjugated) for excretion.</p></li><li><p class="ds-markdown-paragraph"><strong>Drugs/toxins</strong>: Detoxifies via <strong>cytochrome P450 enzymes</strong> (Phase I/II reactions).</p></li></ul><p><strong>2. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Synthesis of Proteins / Cholesterol for Bile / Vitamin D</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Proteins</strong>: Albumin (maintains oncotic pressure), clotting factors (I [fibrinogen], II, V, VII, IX, X).</p></li><li><p class="ds-markdown-paragraph"><strong>Cholesterol</strong>: Precursor for bile acids/steroid hormones.</p></li><li><p class="ds-markdown-paragraph"><strong>25-OH Vitamin D</strong>: Converts vitamin D to its storage form.</p></li></ul><p><strong>3. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Immunological</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Kupffer cells</strong> (liver macrophages): Phagocytose bacteria, old RBCs, toxins from portal blood.</p></li></ul><p><strong>4. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Storage</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Vitamins</strong>: A, D, E, K (fat-soluble), B12, folic acid.</p></li><li><p class="ds-markdown-paragraph"><strong>Minerals</strong>: Iron (as ferritin), copper.</p></li><li><p class="ds-markdown-paragraph"><strong>Glycogen</strong>: Glucose reserve.</p></li></ul><p><strong>5. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Homeostasis</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Blood glucose</strong>: Balances glycogen storage/release.</p></li><li><p class="ds-markdown-paragraph"><strong>Blood volume</strong>: Albumin maintains osmotic pressure.</p></li></ul><p><strong>6. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Bile Production & Enterohepatic Circulation</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Bile salts</strong>: Emulsify fats (essential for digestion).</p></li><li><p class="ds-markdown-paragraph"><strong>Recycles bile acids</strong> (95% reabsorbed in ileum).</p></li></ul><p><strong>7. <mark data-color="purple" style="background-color: purple; color: inherit"><u>Clearance</u></mark></strong></p><ul><li><p class="ds-markdown-paragraph"><strong>Bilirubin</strong>: Removes heme breakdown products.</p></li><li><p class="ds-markdown-paragraph"><strong>Drugs/toxins</strong>: Metabolizes and excretes toxins (e.g., alcohol, medications).</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/ff8170b5-2de4-4bbd-b7a0-8e923a31aa31.png)
Can the liver regenerate ? True or false
True
Why can some patients have liver disease and be unaware?
- Many patients can be asymptomatic until developing hepatic complications
- Often a long time interval between disease occurrence and detection
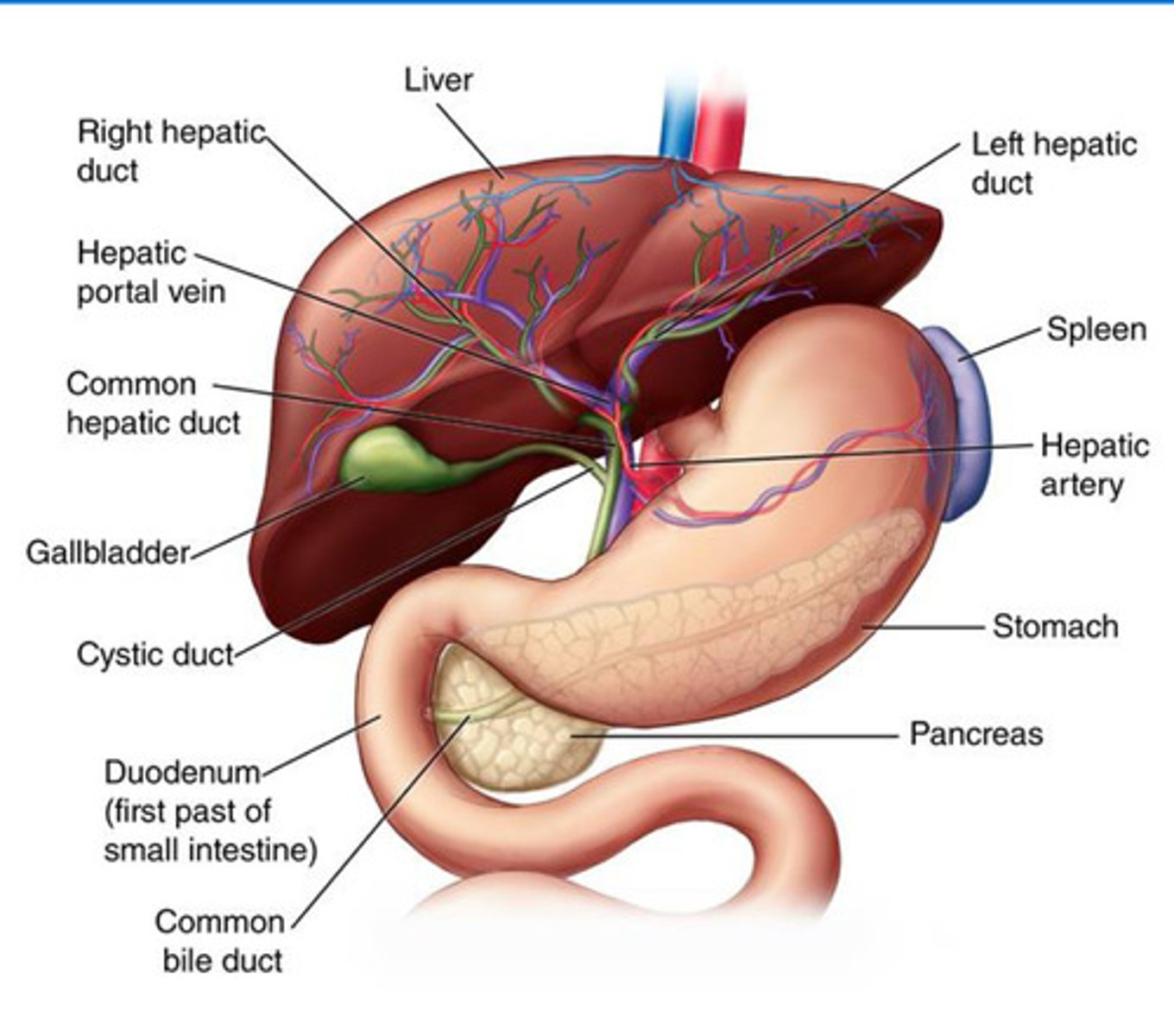
Liver structure
Liver: Large, reddish-brown organ responsible for detoxification, metabolism, and bile production.
Right and Left Hepatic Duct: Tube that drains bile from the liver's lobe for digestion.
Common Hepatic Duct: Channel formed by the right and left hepatic ducts, carrying bile from the liver.
Hepatic Portal Vein: Vessel that transports nutrient-rich blood from the digestive tract to the liver.
Hepatic Artery: Artery supplying oxygenated blood to the liver.
Gallbladder: Small sac that stores and concentrates bile for digestion.
Cystic Duct: Tube connecting the gallbladder to the common bile duct, regulating bile flow.
Common Bile Duct: Passageway that delivers bile from the liver and gallbladder to the duodenum.
Duodenum: First part of the small intestine where bile and enzymes aid in digestion.
Pancreas: Gland that produces digestive enzymes and hormones, aiding digestion.
Stomach: Organ that breaks down food with acid and enzymes before passing it to the duodenum.
Spleen: Organ that filters blood and supports immune function.
How is liver disease classified? - understand*
Liver disease is categorised based on:
Pattern of Damage (Hepatocellular vs. Cholestatic)
Time Course (Acute vs. Chronic)
End-Stage Consequences (Fibrosis → Cirrhosis)
- These are not distinct entities, OVERLAP occurs
- Both of these can lead to fibrosis and cirrhosis
—
Mnemonic: "HepC vs. CholeD"
HepC: Hepatocellular (ALT/AST ↑).
CholeD: Cholestatic (ALP/GGT ↑).
What is Cholestasis?
Cholestasis is a disruption of bile flow, leading to:
Bile stagnation in ducts (intrahepatic or extrahepatic).
Backflow of bile components (bilirubin, bile salts) into blood where bile fails to flow from hepatocytes to duodenum and is diverted to blood. → Jaundice (yellow skin/sclera), dark urine (conjugated bilirubin), pale stools (no bilirubin in gut).
Failure of bile to reach the duodenum → impaired fat digestion.
Intrahepatic: due to dysfunction of biliary ductules e.g. primary biliary cholestasis (PBC), primary sclerosing cholangitis (PSC), drugs, inflammation
Extrahepatic: mechanical obstruction e.g. inflammation of bile ducts, strictures, gall stones
Drug Metabolism Implications
Bile salts compete with drugs for protein binding → ↑ free drug toxicity.
Reduced bile flow → Accumulation of biliary-excreted drugs (e.g., rifampicin, statins).
Fat malabsorption → Poor uptake of lipid-soluble drugs (e.g., cyclosporine, vitamin K-dependent anticoagulants).
—
Bile Salt Accumulation → Hepatocyte damage (inflammatory/apoptotic pathways).
Bilirubin Backup → Jaundice (yellow skin/sclera), dark urine (conjugated bilirubin), pale stools (no bilirubin in gut).
Fat Malabsorption → Steatorrhea (fatty stools), deficiency of fat-soluble vitamins (A, D, E, K).
Pruritus (Itching) → Due to bile salts depositing in skin.
—
Types of Bile stagnation:
1. Intrahepatic Cholestasis
Dysfunction at the hepatocyte/bile ductule level.
Primary biliary cholangitis (PBC) (autoimmune destruction of small bile ducts).
Drug-induced (e.g., anabolic steroids, chlorpromazine).
Inflammation (viral hepatitis, sepsis).
Genetic disorders (e.g., PFIC [progressive familial intrahepatic cholestasis]).
2. Extrahepatic Cholestasis
Physical obstruction of large bile ducts.
Gallstones (choledocholithiasis).
Tumors (pancreatic cancer, cholangiocarcinoma).
Strictures (post-surgical, primary sclerosing cholangitis [PSC]).
Pancreatitis (compressing the common bile duct).
What is Hepatocellular disease?
Hepatocellular disease refers to direct injury to hepatocytes (liver cells) [toxins, viruses, drug induced], leading to:
Inflammation (hepatitis).
Fat accumulation (steatosis). → within the hepatocyte which can be micro or macrovesicular
Cell death (necrosis/apoptosis).
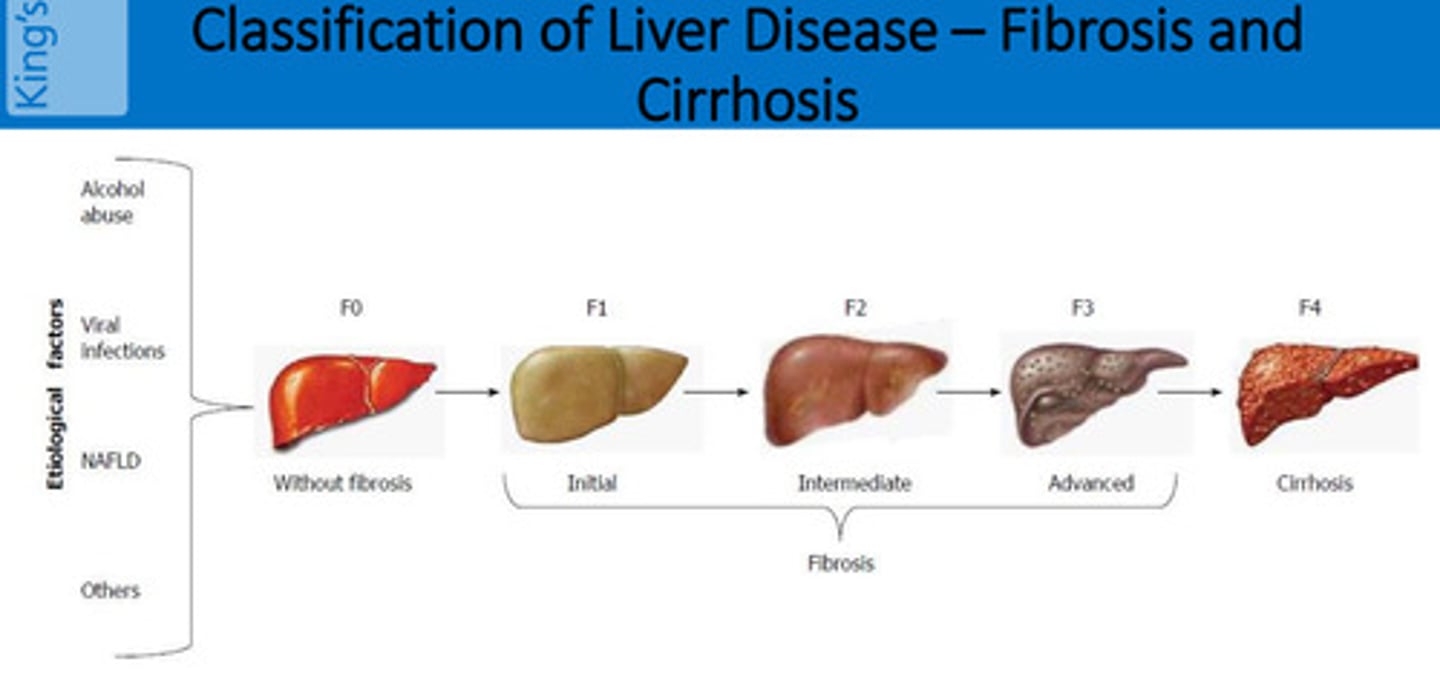
What is Fibrosis and Cirrhosis?
Fibrosis: Scarring of the liver due to chronic injury (e.g., hepatitis, alcohol, fatty liver).
Persistent damage → Activation of stellate cells → Excess collagen deposition → Scar tissue replaces healthy liver tissue.
Blood flow becomes disrupted as sinusoids get blocked.
Reversibility:
Early fibrosis (F1-F3) may be reversible if the cause is treated (e.g., stopping alcohol, curing hepatitis C).
Advanced fibrosis (F4) = Cirrhosis (usually irreversible).
Cirrhosis: End-stage liver disease where fibrosis is so severe that the liver becomes shrunken, nodular, and dysfunctional.
Extensive scarring → Nodular regeneration (liver tries to heal but forms disorganized lumps).
Blood flow severely disrupted → Portal hypertension (high pressure in liver veins).
Irreversibility:
Compensated cirrhosis: Liver still functions but is damaged.
Decompensated cirrhosis: Liver fails (jaundice, ascites, bleeding, coma).
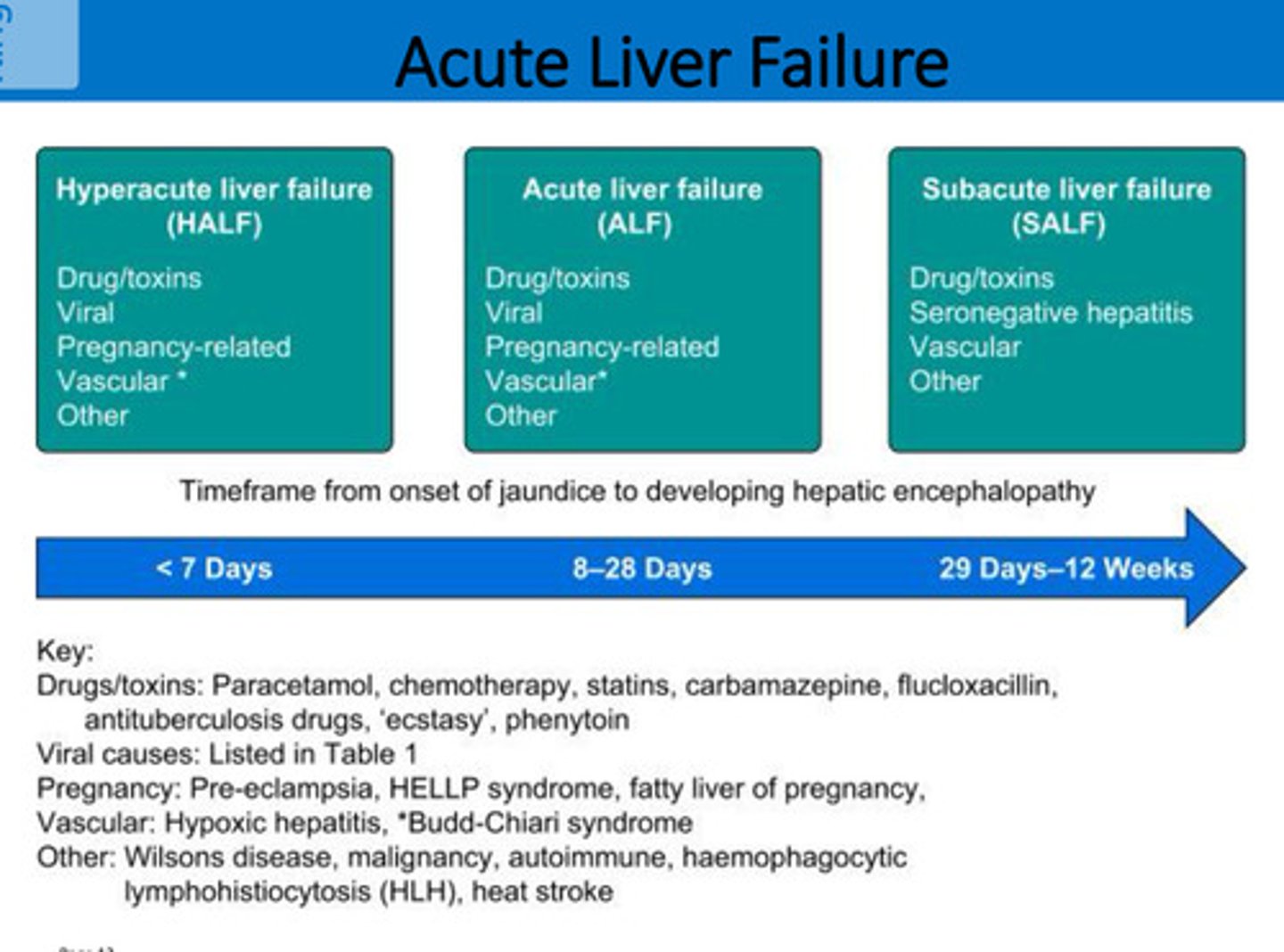
What is the difference between acute and chronic liver disease?
Acute:
History of onset of symptoms does not exceed 6 months
Acute liver failure (e.g. paracetamol overdose) - hyperacute, acute or subacute depending on time from jaundice to Encephalopathy (brain dysfunction)
Chronic (e.g. chronic hep B):
Persists for more than 6 months, permanent
Structural changes following long-standing cell damage
Compensated (liver is working ) vs decompensated (liver iss unable to carry out its functions listed in the previous card) disease
actute liver failure timeline
< 7 days = Hyperacute
8-28 = Acute
29 days to 12 wks = Subacute
How do we interpret LFTs
Liver Function Tests:
- Fairly non-specific
- Generally is 2 x U Limit Normal considered abnormal
- Liver dysfunction present = usually at least 2 will be deranged
- Trends not isolation—check references ranges and units
- LFTs are not always abnormal even in patients with cirrhosis
- Abnormal LFTs not necessarily due to liver dysfunction
What are the liver function tests (LFTs)?
Bilrubin fact profile - LFTs
• Usual range 5-20micromol/L
• Product of RBC breakdown
• Transported to the liver in the serum attached to albumin
• Transformed into a water-soluble conjugate which is excreted via the bile into the intestine
• In Liver damage, transformed into a water-soluble conjugates accumulate in blood and tissues
—
• Bilirubin Levels ↑ in: Haemolysis, Hepatocellular damage and Cholestasis
• Clinical jaundice = ≥ 50μmol/L of Bilirubin in blood
Transaminase Enzymes fact profile -LFTs
AST (0-40 iu/L):
• Found in liver, heart, skeletal muscle, pancreas, kidney and RBC
—
ALT (5-30 iu/L):
• Often termed 'Liver specific enzyme'
• Levels increase in viral hepatitis, alcohol related liver injury, drugs, sepsis
Not All patients with liver disease will have raised transaminase enzymes
ALP and γ-GT fact profile - LFTs
Alkaline Phosphatase → ALP range 30-120 iu/L
• Found in liver, bone, intestine and placenta
• Level increase in cholestasis, infiltrative liver disease, damage to biliary tree
• If raised ALP in isolation may be due to other reasons e.g. Paget's disease
γ-Glutamyltransferase (Gamma) → GGT-(5-55 iu/L)
• Found in liver and biliary epithelial cells, pancreas, kidneys, prostate, intestine
• Level increased by enzyme inducers including alcohol, cholestasis, carcinoma of pancreas & GIT
Albumin and PT fact profile - LFTs
Albumin (35-50 g/dL)
• One of the proteins produced by the liver
• Long half-life (20-26 days)
• Increased level - oedema
• Decreased in chronic liver disease
PT Prothrombin Time (10-14 secs) or INR
• Clotting factors produced by the liver
• Short half-life (2-3 days)
• PT/INR increased in acute and chronic liver disease
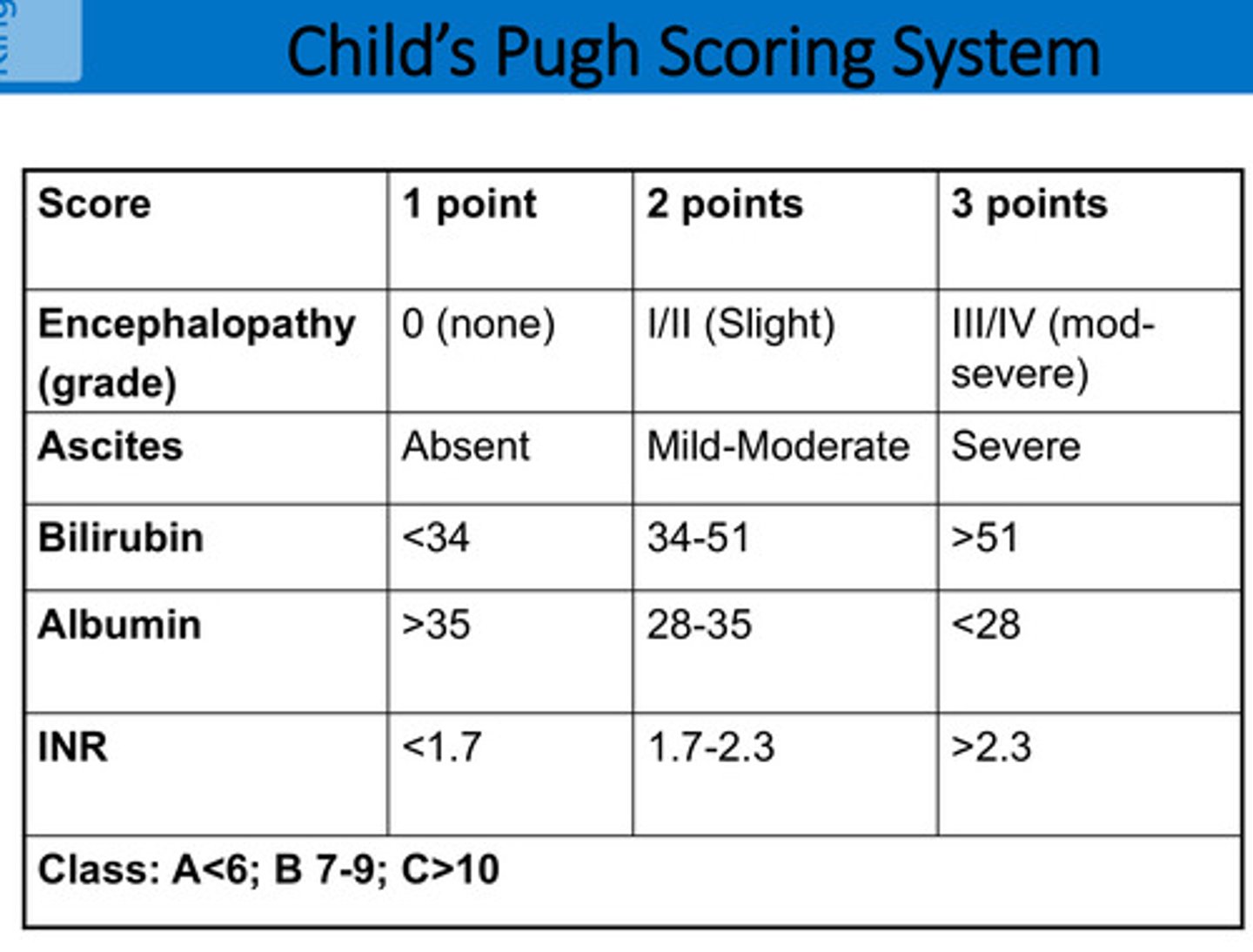
What is the Child’s Pugh Scoring System?
Shows severity of liver disease:
Class A < 6
Class B 7-9
Class C > 10
What other investigations/scoring systems are used for liver disease?
Liver ultrasound, CT, MRI
ERCP and MRCP → Endoscopic Retrograde Cholangiopancreatography / Magnetic Resonance Cholangiopancreatography
Fibroscan, Liver biopsy
Calculate MELD [Model for End-Stage Liver Disease] or UKELD or Lille score -> this is usually used, Child Pugh not really used
What are the signs and symptoms of liver disease? understand why all of these happen
1. Jaundice: ↑ Bilirubin (liver can’t conjugate/excrete it).
Hepatocellular disease (e.g., hepatitis) → impaired conjugation.
Cholestasis (e.g., gallstones) → bile can’t reach gut.
Yellow skin/sclera, dark urine (conjugated bilirubin excreted in urine), pale stools (no bilirubin in stool).
—
2. Ascites: Portal hypertension + low albumin (↓ oncotic pressure).
Why?
Cirrhosis → ↑ resistance in portal vein → fluid leaks into peritoneum.
Hypoalbuminemia → reduced blood osmotic pressure.
—-
3. Bruising/Bleeding: ↓ Clotting factors (II, VII, IX, X) + ↓ Vitamin K (cholestasis → malabsorption).
Why? Liver synthesizes clotting factors; damage → prolonged PT/INR.
—
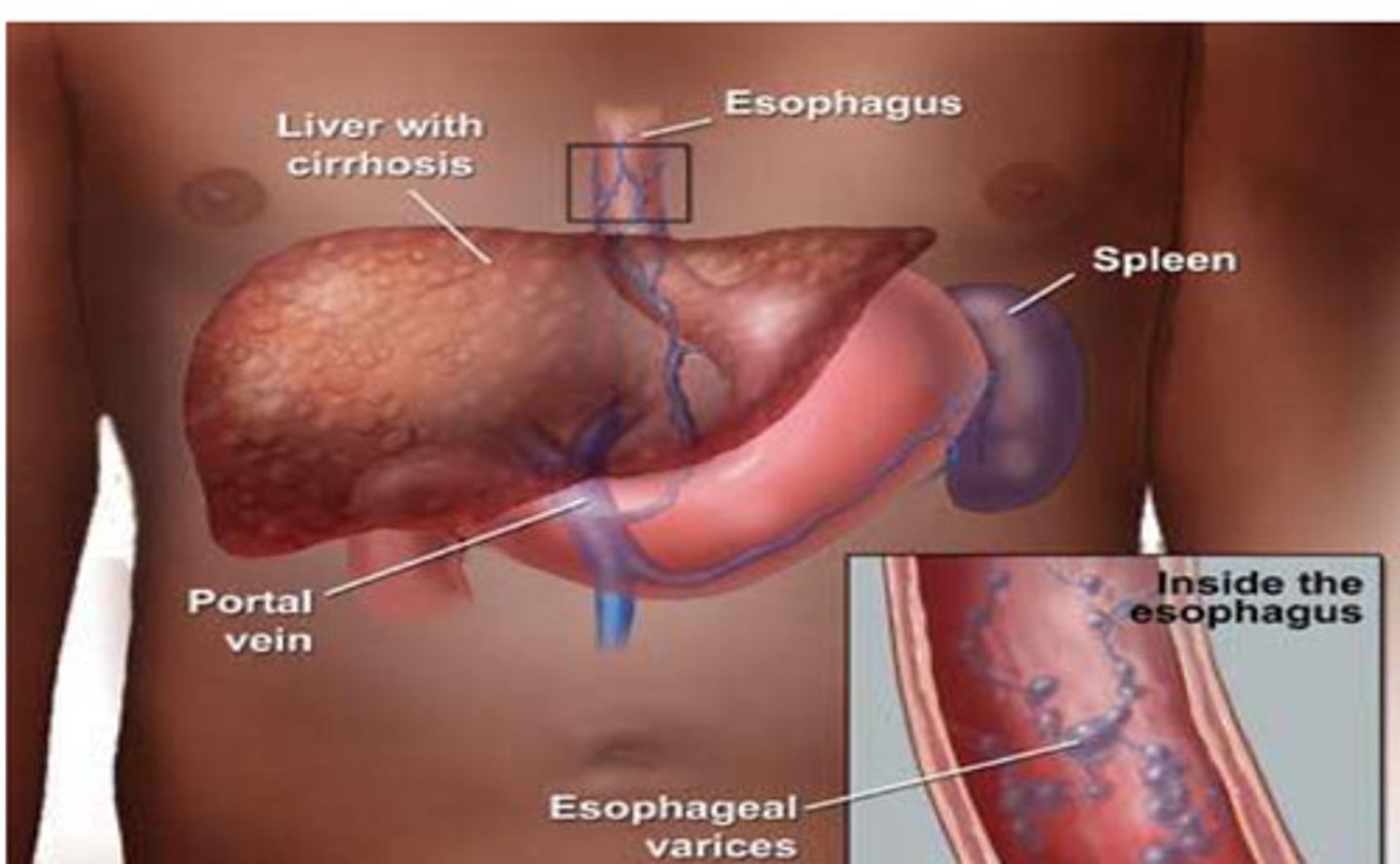
4. Varices (Oesophageal/Gastric): Portal hypertension (cirrhosis → blood shunts to collateral veins).
Risk: Life-threatening bleeding (hematemesis/melena).
—
5. Hepatic Encephalopathy: ↑ Ammonia (liver can’t convert it to urea).
Why? Toxins cross blood-brain barrier → confusion, asterixis, coma.
—
6. Abdominal Pain: Liver capsule stretch (hepatomegaly), gallbladder inflammation, or ascites pressure.
—
7. Pale Stools & Dark Urine
Pale stools: No bilirubin reaching gut (cholestasis).
Dark urine: Conjugated bilirubin excreted by kidneys.
—
8. Gynaecomastia: ↑ Oestrogen (liver can’t metabolize hormones).
Why? Impaired breakdown of androgens → skewed oestrogen:testosterone ratio.
—
9. Fatty Stools (Steatorrhea): ↓ Bile salts (cholestasis → fat malabsorption).
Why? No bile to emulsify fats → bulky, greasy stools.
—
10. Spider Naevi: ↑ Oestrogen → vasodilation.
Location: Upper body (face, chest).
—
11. Finger Clubbing: Chronic hypoxia (portopulmonary shunting) or biliary disease.
—
12. Pruritus (Itching): ↑ Bile salts depositing in skin (cholestasis).
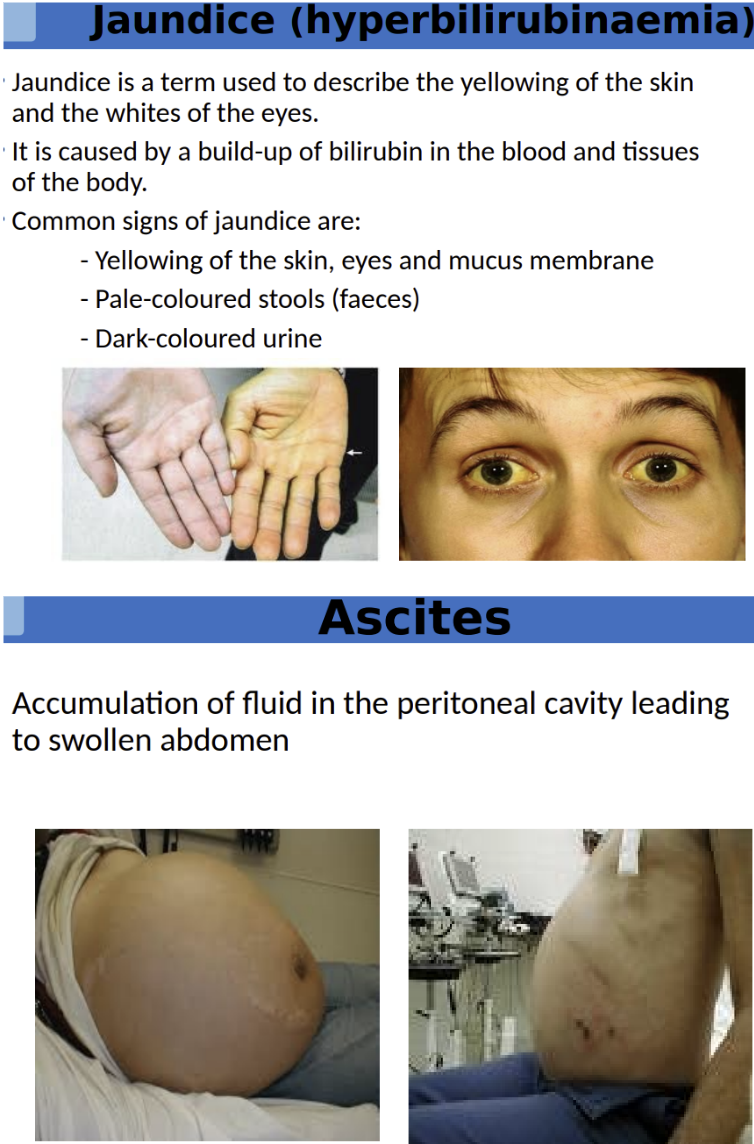
What is jaundice? What are the different types of jaundice ?
Yellow discoloration of the skin, sclera (whites of the eyes), and mucous membranes due to ↑ bilirubin in blood (>2.5 mg/dL).
Other Key Features: Pale stools (lack of bilirubin in gut). / Dark urine (excess conjugated bilirubin excreted by kidneys).
—
Pre-Hepatic: Too much bilirubin made (hemolysis).
Bilirubin type: Unconjugated (indirect, water-insoluble).
Urine: Dark (bilirubin present) but no bilirubin in urine dipstick (only conjugated bilirubin is excreted in urine).
Hepatic: Liver dysfunction (hepatocytes can’t conjugate/excrete bilirubin).
Bilirubin type: Both unconjugated & conjugated (mixed pattern).
Post-Hepatic: Bile flow blocked (gallstones, pancreatic cancer).
Bilirubin type: Conjugated (direct, water-soluble).
Stools: Pale (no bile reaching intestines).
1. Pre-Hepatic Jaundice: Excessive RBC breakdown → overwhelms liver’s ability to conjugate bilirubin.
Mechanism:
↑ Unconjugated (indirect) bilirubin (water-insoluble, bound to albumin).
Liver function normal, but bilirubin load too high.
Conditions:
Hemolytic anemia (e.g., sickle cell, malaria, G6PD deficiency).
Neonatal jaundice (immature liver enzymes).
2. Intra-Hepatic (Hepatocellular) Jaundice: Liver damage → impaired bilirubin uptake/conjugation/excretion.
Mechanism:
↑ Both unconjugated AND conjugated bilirubin.
Liver enzymes (ALT/AST) typically elevated.
Conditions:
Viral hepatitis (HBV, HCV).
Cirrhosis.
Gilbert’s syndrome (mild UDP-glucuronosyltransferase deficiency).
Drug/toxin-induced liver injury (e.g., paracetamol, alcohol).
3. Post-Hepatic (Obstructive) Jaundice: Bile flow obstruction → conjugated bilirubin backs up into blood.
Mechanism:
↑ Conjugated (direct) bilirubin (water-soluble).
↑ ALP & GGT (markers of cholestasis).
Conditions:
Gallstones (choledocholithiasis).
Pancreatic cancer (compressing bile duct).
Primary sclerosing cholangitis (PSC).
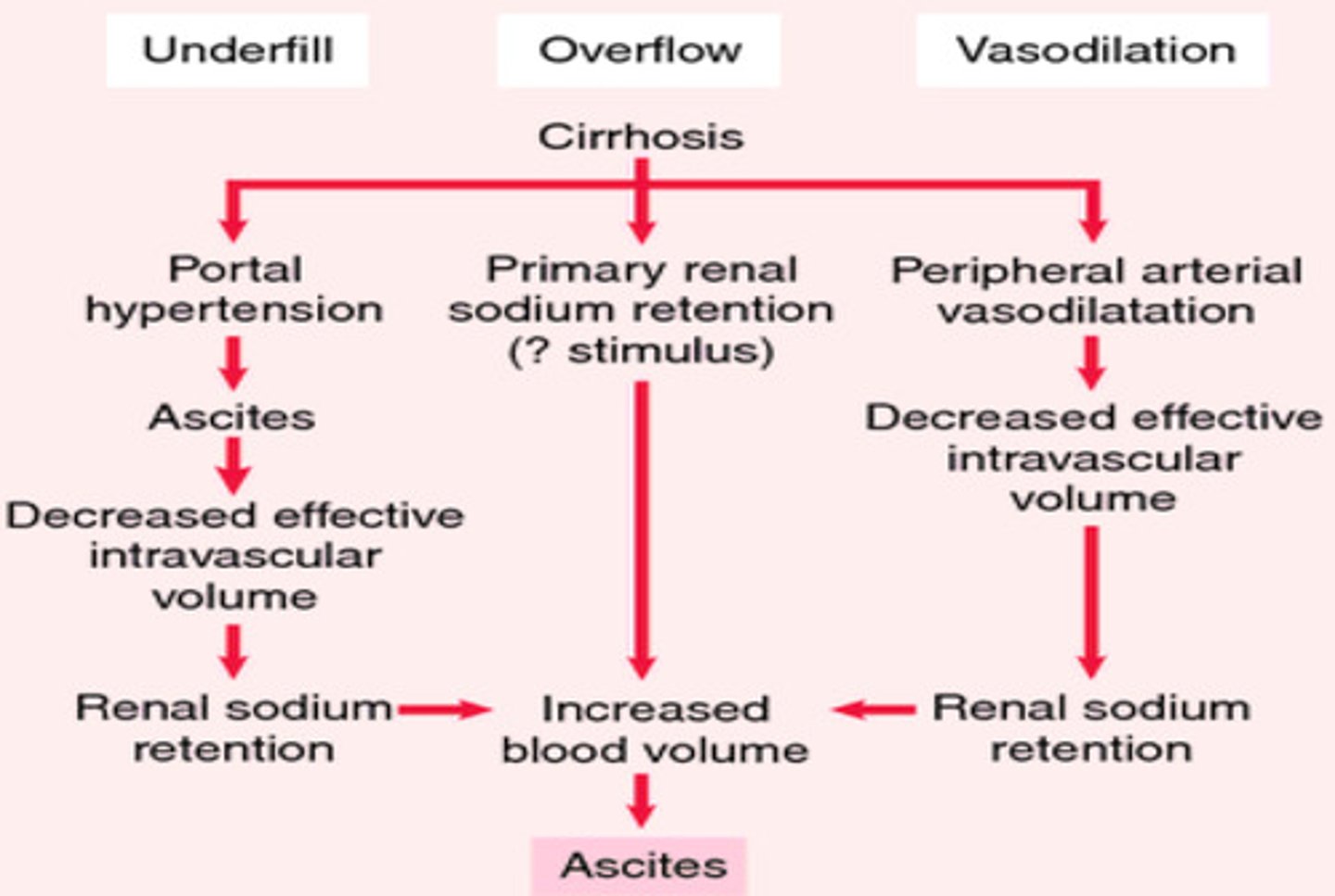
What is ascites?
Accumulation of fluid in the peritoneal cavity leading to swollen abdomen

How ascites occurs diagram?
Portal hypertension occurs when there is increased resistance to blood flow in the liver (often due to cirrhosis or fibrosis).
This causes increased pressure in the portal vein, leading to:
Splanchnic vasodilation (dilation of abdominal blood vessels).
Increased hydrostatic pressure in capillaries, pushing fluid into the peritoneal cavity.
Reduced effective arterial blood volume, even though total blood volume is high.
RAAS Activation & Fluid Retention:
Kidneys sense low perfusion AND release Renin → Angiotensin II → Vasoconstriction + Aldosterone & ADH release.
Aldosterone → Sodium & water retention.
ADH → Water reabsorption.
Result: More fluid retention, worsening ascites as excess fluid shifts into the peritoneal cavity
How is ascites treated?
Diuretic resistant—25-50% mortality within a year
Consider fluid and/or sodium restriction
1) Diuretic therapy includes:
Aldosterone antagonists e.g., Spironolactone (Potassium sparing diuretic)
Loop diuretics e.g., furosemide
Amiloride
2) Paracentesis for large volume if diuretics don't work for large volume. Need to maintain adequate circulating volume – colloids, albumin, terlipressin
3) Transjugular intrahepatic portosystemic shunting (TIPSS) for more refractory ascites along with paracentesis
Diagram of Paracentesis
Paracentesis is a medical procedure to remove ascitic fluid (excess fluid in the peritoneal cavity) from the abdomen, commonly used in patients with cirrhosis, heart failure, or cancer.
Sterilization of the puncture site (usually midline or left lower quadrant).
—
Local Anesthesia
Lidocaine numbs the skin and deeper tissues.
Needle Insertion
A trocar or catheter is inserted into the peritoneal cavity.
Z-track technique (displacing skin before insertion) reduces leakage.
Fluid Drainage
Diagnostic tap (50–100 mL) for lab tests.
Therapeutic tap (≥5 L) for symptom relief (may use a vacuum bottle or manual suction).
Post-Procedure
Bandage applied; monitor for complications.
For large-volume paracentesis (>5 L), IV albumin (6–8 g/L removed) prevents circulatory dysfunction.
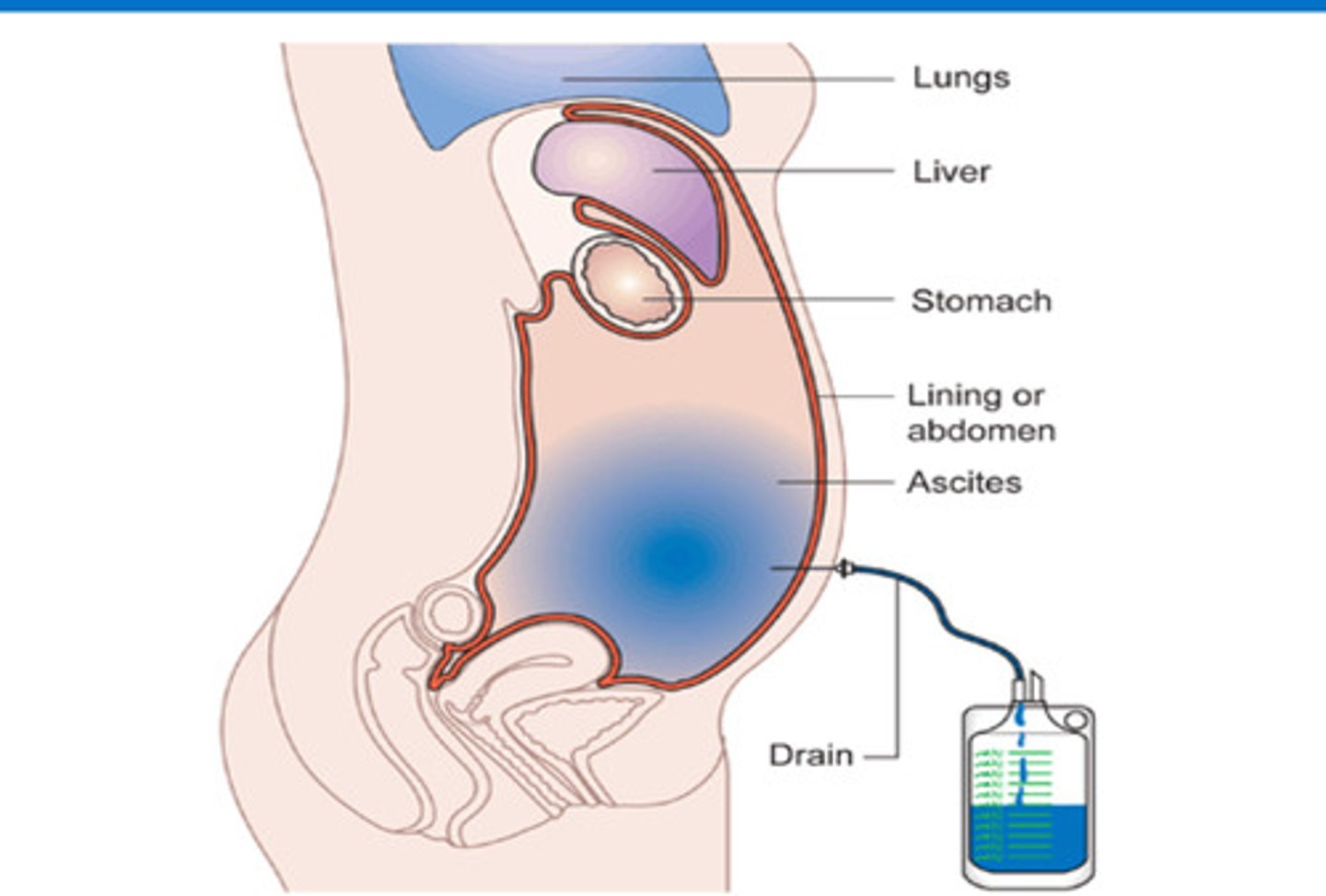
Diagram of TIPPS
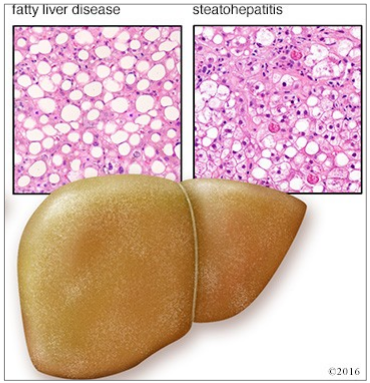
Portal hypertension [PHT] causes blood flow to be forced backward, causing veins to enlarge and varices to develop across the oesophagus and stomach from the pressure in the portal vein
Pressure backup also causes the spleen to enlarge
—
Shunt allows the blood to flow normally through the liver to the hepatic vein.
This reduces portal hypertension, and allows the veins to shrink to a normal size helping to stop variceal bleeding
![<p>Portal hypertension [PHT] causes blood flow to be forced backward, <strong><mark data-color="red" style="background-color: red; color: inherit">causing veins to enlarge</mark></strong><mark data-color="red" style="background-color: red; color: inherit"> and varices to develop across the oesophagus and stomach from the pressure in the portal vein </mark></p><p><mark data-color="red" style="background-color: red; color: inherit">Pressure backup also causes the spleen to enlarge </mark></p><p>—</p><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">Shunt allows the blood to flow normally through the liver to the hepatic vein. </mark></strong></p><p><strong><mark data-color="purple" style="background-color: purple; color: inherit">This reduces portal hypertension, and allows the veins to shrink to a normal size helping to stop variceal bleeding</mark></strong></p>](https://knowt-user-attachments.s3.amazonaws.com/008cef53-ac15-4828-8c0f-2a0123987be7.png)
Can patients with an AKI use diuretics
No as diuretics are renally cleared.
Want to avoid toxic drug accumulation!
What side effects of diuretics?
-Hyponatraemia = sodium level in the blood is lower than normal
-Potassium levels altered
What are the cautions associated with ascites? - WHAT SHOULD WE MONITOR
Monitor:
Daily Urea and Electrolytes → especially sodium, potassium and creatinine
Daily weight—aim for 0.5-1 kg/day loss
Fluid chart—note fluid restriction, urine output
Avoid high sodium preparations
—
Complications:
dilutional hyponatraemia, hepatic encephalopathy, hepato-renal
syndrome, gynaecomastia, hyperkalaemia, muscle cramps, spontaneous bacterial
peritonitis
What is Spontaneous Bacterial Peritonitis?
- Infection of the ascitic fluid without intra-abdominal source of sepsis (infection of the ascites)
- Build-up of fluid in peritoneal space becomes a breeding ground for bacteria
- 75% from gut 25% from skin
- Neutrophil count >250 cells per mm3
- Mortality ~40%
- 1 st line: 3rd generation cephalosporins, co-amoxiclav, Tazocin
- Prophylaxis: (broad spectrum antimicrobials) Norfloxacin, Ciprofloxacin
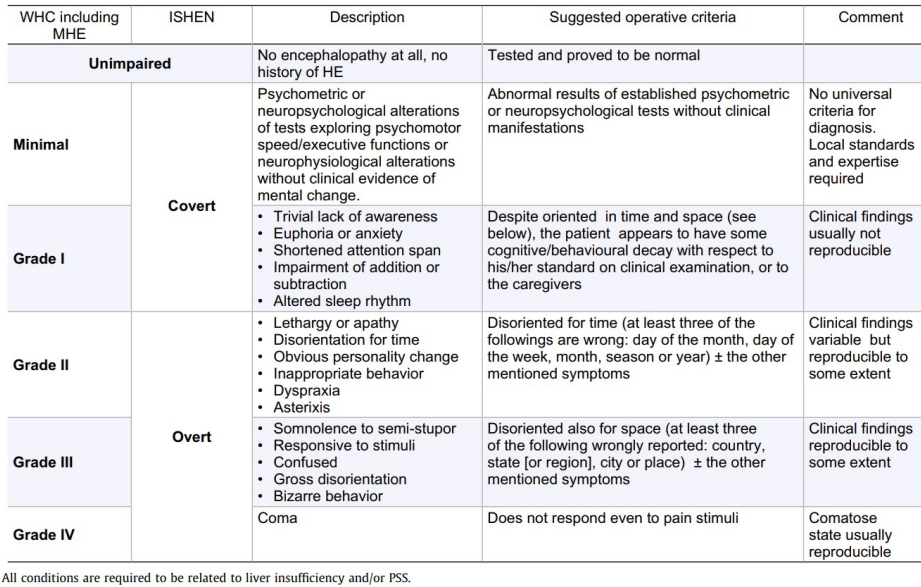
What is Hepatic Encephalopathy?
List potential differential diganosis'
A brain dysfunction caused by liver insufficiency and/or PSS [portosystemic shunting] leading to toxin accumulation in the brain.
Portosystemic shunting refers to abnormal blood flow diversion from the portal venous system (which normally carries blood from the gut to the liver for detoxification) directly into systemic circulation, bypassing the liver.
—
- Manifests as a wide-spectrum of neurological or psychiatric abnormalities from ranging from subclinical alterations to coma
- Can occur in either acute or chronic liver disease
- Classifies from grade 1 to 4
—
Potentially correctable if precipitating factors are addressed
Differential diagnoses:
Hypoglycaemia Alcohol intoxication
Alcohol intoxication
Withdrawal May occur due to:
Accumulation of toxins
Increased BBB permeability
Increased levels of neurotransmitters
Grades 1-4 of HE diagram
Summary of Grades 1-4:
Minimal HE: No overt encephalopathy or psychometric/neuropsychological deficits, but abnormal results on psychometric/neuropsychological tests. No universal diagnostic criteria; local standards and expertise required.
Grade I (Covert): Symptoms include trivial lack of awareness, euphoria/anxiety, shortened attention span, impaired arithmetic, and altered sleep rhythm. Patients appear oriented and behave normally to caregivers, but clinical findings are not consistently reproducible.
Grade II: Symptoms escalate to lethargy/apathy, disorientation for time, obvious personality changes, inappropriate behavior, dyspraxia, and asterixis. Patients are disoriented for time (e.g., misjudging the day of the month/week/season) alongside other symptoms. Findings are variable but reproducible to some extent.
Grade III (Overt): Marked by somnolence to semi-stupor, responsiveness to stimuli, confusion, gross disorientation, and bizarre behavior. Patients are disoriented for space (e.g., unaware of country, state, or city) alongside other symptoms. Findings are reproducible to some extent.
Grade IV: Coma, where the patient does not respond even to painful stimuli. This state is usually reproducible.
What are the precipitating factors of HE?
Increased protein load
Reduced ammonia excretion: By-product of bacterial replication / Builds up and crosses BBB
Electrolyte imbalance/disturbance
Infections
Dehydration
Drugs
why is HE a problem in liver dysfunction?
Ammonia isn't cleared as well and can travel to the brain = brain dysfunction
How do we get rid of excess ammonia for HE patients
Laxatives → lactulose given as first line
Helps remove ammonia through increased number of stools
Ammonia → ammonium ions that can be excreted
Aim for 2-3 stools a day
Promotes growth of beneficial microorganisms which process ammonia
Reduces gut protein load
Lowers colonic pH which discourages ammonia producing bacteria
Enemas can be used if patient is constipated
What are the treatment options for HE?
1. Lactulose (non-absorbable disaccharide) → Laxatives
Aim for 2-3 soft stools per day
Promotes growth of beneficial micro-organisms
Reduces gut protein load
Lower colonic pH which discourages ammonia producing bacteria (Enemas can be used when patient is constipated)
2. Rifaximin • 550mg twice daily
Reduces Ammonia Production
Gut bacteria (e.g., E. coli, Klebsiella) break down protein → produce ammonia (NH₃).
Rifaximin suppresses these bacteria → ↓ NH₃ absorption from intestinal lumen → ↓ neurotoxicity.
• Semi-synthetic rifamycin derivative, poorly absorbed (reduced systemic side effects)
• Broad-spectrum with activity against aerobic and anaerobic, gram positive and negative organisms
• Binds to the β-subunit of bacterial DNA-dependent RNA polymerase resulting in inhibition of bacterial RNA synthesis.
• NOT to be used in acute infection, to be held when patient on broad-spectrum antibiotics
—
Other options include:
• Metronidazole, Neomycin, Sodium benzoate
• Dietary protein restriction not recommended
link asterixis to HE
What is Portal Hypertension and Variceal Bleeding?
Portal hypertension is caused by increased resistance to flow due to:
Disruption of hepatic architecture:
Compression of hepatic venules by regenerating nodules
Collateral vessels form and enable blood to bypass the liver
Variceal bleeding is a serious complication of pHTN (> 12 mmHg) with reduced clotting factors and vitamin K absorption
Bleeding varices → mortality 50% index bleed and 30% for subsequent bleeds
Oesophageal varices can burst and cause massive bleeding into oesophagus
Drug options for Variceal Bleeding and Portal Hypertension - mechanisms of treatment
*Not that important for exam
Terlipressin:
• Synthetic analogue of vasopressin which acts on 3 vasopressin receptors.
• Greater selectivity for V1 and longer half-life.
Administer in bolus doses 1-2mg every 4-6hours (continue until haemostasis achieved)
• Monitor - Blood pressure, sodium, potassium, fluid balance • Side-effects include headaches, abdominal cramps, ischaemia (monitor extremities)
Somatostatin and Analogues:
• Inhibits splanchnic vasodilatation - decrease of splanchnic hypervolaemia.
• Results in decreased arterial blood supply leading to reduction in pressure in the portal circulation.
What are some endoscopic procedures used to prevent variceal bleeding? *Not that important for exam → extra info
-Band litigation - superior to sclerotherapy in terms of re-bleeding and mortality
-Sclerotherapy - Injection of sclerosants ("glue") e.g. cyanoacrylate
-Balloon Tamponade - temporary, Mechanical "pressure" over bleeding points, hig rates of re-bleeding when deflated
Why should all liver disease patients with pHTN or variceal bleed receive broad-spectrum antibiotics prophylaxis?
Infection common after upper GI bleed in cirrhotic patients (20% pts within 48hrs)
Major cause of mortality and morbidity
7 days antibiotics decreases mortality RISK when given IV broad-spectrum antibiotic (e.g. Tazocin) or meropenem/ciprofloxacin for penicillin allergic pts
What can we use for secondary prophylaxis of portal hypertension?
- Non-selective β-blocker e.g. Propranolol or carvedilol
- Splanchnic Vasoconstriction (beta2 blockade) → reduced portal pressures → prevent re-bleeding → increase survival
Cardiac output results in reduced portal pressures (beta1 blockade)
—
• Role of Nitrates
• Problems with tolerability
• Dose titration and monitoring
What is Spider naevi
- Central red arteriole surrounded by radial pattern of thin capillaries
- Raised oestrogen—pregnant women, HRT, OCP
- Hepatic disease—failure to metabolise oestrogen

What are treatments for pruritis?
Pruritus (itching) is a symptom in cholestatic liver diseases due to Bile Acid Accumulation, activate itch receptors.
—
- Colestyramine
- UDCA
- Chlorphenamine, hydroxyzine (sedating histamine)
- Loratadine, cetirizine (non-sedating histamine)
- Calamine lotion, menthol 2%
- Rifampicin
- Ondansetron
- Naltrexone, nalaxone
- Sertraline
Lecture 2
What are the causes of liver disease?
-Alcohol
• Viral infections - Hepatitis (A, B, C, D, E)
• Inherited and metabolic disorders
• Immune disease of the liver
• Vascular abnormalities
• Non-alcoholic fatty liver disease (NAFLD)
• Drugs and toxins
• Cancer
• Biliary tract disorders
• Infections
• Other
How many mls is a unit of alcohol
1 Unit of Alcohol = 10 mL (8g) of Pure Alcohol
14 units is recommended PER WEEK
Binge drinking means drinking enough on a single occasion to get drunk (drinking 6+ units (women) or 8+ units (men) in a single session) and may be worse than regular drinking in terms of cancer risk
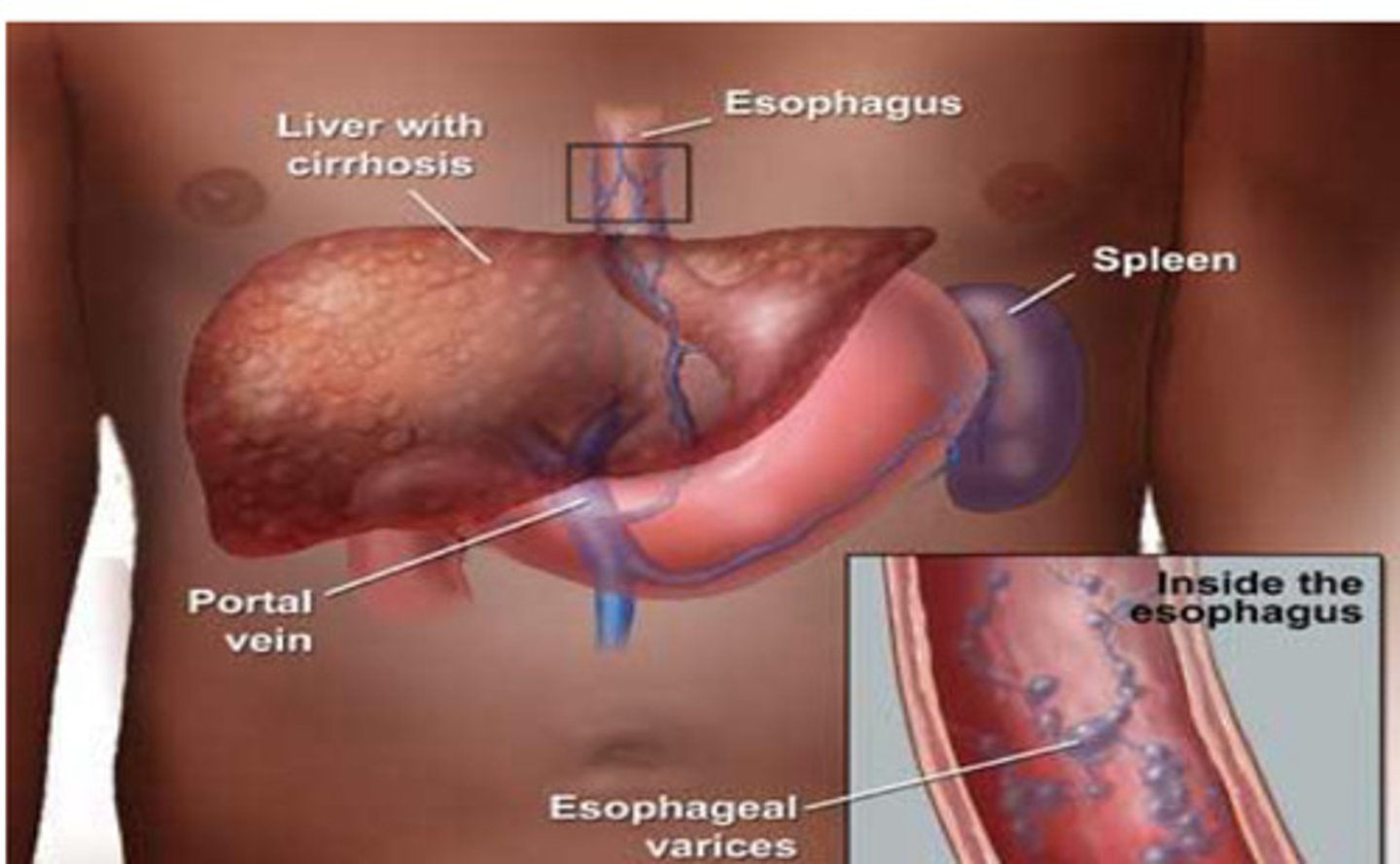
Effects on alcohol on the body
Short term:
• Anxiety
• Decreased respiratory rate
• GI disturbances
• Impaired judgement
• Loss of consciousness
• Impotence
• Acute poisoning
• Complexion/ effect on appearance
• Unintentional injuries
—
Long term effects:
• Liver disease
• Cancer (several types)
• Pancreatitis
• GI ulceration
• Osteoporosis
• Infertility
• Heart disease
• Stroke
• Increased BP
• Obesity
• Dementia
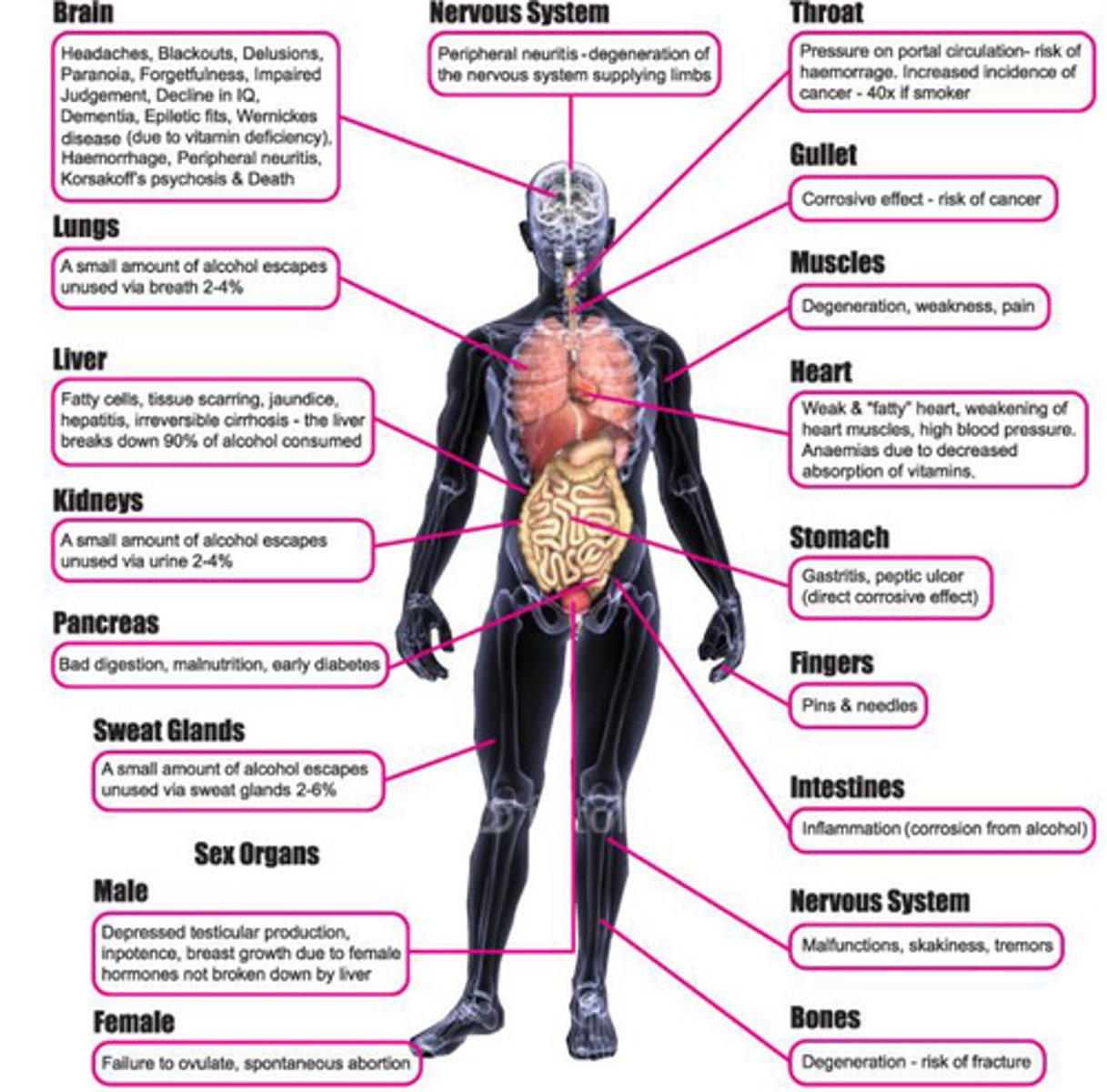
How is alcohol metabolised?
Alcohol is oxidised to acetaldehyde via alcohol dehydrogenase
Acetaldehyde is most important to liver damage
—
Dehydrogenase metabolises acetaldehyde which is metabolised to water, fatty acids and CO2
—
Higher alcohol intake increases CYP450 2E1 oxidising system which metabolises alcohol to unstable free radicals
What is Steatosis?
Fatty acid accumulation in the liver
Reversible with abstinence
Accumulation of large droplets of lipid within hepatocyte caused by disruption of metabolic pathways (NADH redox imbalance)
Usually has minimal effect on liver function
Liver is scanned to see fatty acid accumulation
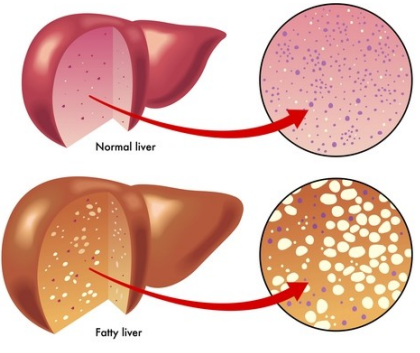
What is Steatohepatitis? Acute Alcoholic Hepatitis (AAH)
- Accumulation of fat AND hepatocyte injury with fibrosis
- Caused by many things e.g.: Oxidative stress, acetaldehyde accumulation and altered protein function
-Usually improves with abstinence although proportion patients will develop cirrhosis despite abstinence
What is fibrosis/cirrhosis?
• Inflammation - fibrogenesis + collagen deposition
• Mechanism activation unclear but thought to include direct injury by free radicals plus expression inflammatory cytokines
• Patient may exhibit signs of decompensation including encephalopathy, ascites, coagulopathy
• Proportion patients will go onto develop HCC
• Abstinence key to management
Why doesn't everyone with high alcohol intake get liver damage?
- Differences in intake and threshold
- Consumption patterns
- Dependency
- Genetics
- Gender (men tend to break down alcohol better than women)
- BMI (higher BMI → already have a degree of fatty liver disease ∴ alcohol only makes it worse)
- Race (Asians → Asian Flush)
- Environmental influences e.g. chronic viral disease, or on hepatically-cleared medication (increased risk of liver damage)
What drugs are used to treat Alcoholic Liver Disease?
- Sedatives and vitamin supplementation since drinking alcohol means patients are not eating as much = lacking vitamins
- Chlordiazepoxide and Pabrinex (Lorazepam- (double check this drug choice))
- Withdrawal Protocol
- Lorazepam = shorter half-life easier to manage symptoms
—
Combination of sedatives (e.g. BZDs) and vit supplementation
- Chlordiazepoxide + Pabrinex
Protocol:
○ Lorazepam PO PRN based on age and AWS score (better tolerated)
○ Pabrinex ONE or TWO pairs IV TDS After 24hrs discontinue PRN script and prescribe reducing regimen based on total lorazepam requirement in first 24hrs
Why is Chlordiazepoxide used?
Long half-life (decreased chance of abuse)
Sedative and anti-convulsant properties
Slower onset of action
low dependence forming potential
Better than chlormethiazole which was given traditionally
Caused resp. depression, addiction/dependence
Can be given as:
Front loading (loading dose followed by repeat dosing every 90 mins)
Light sedation
Symptom triggered dosing
Tapering dose regimen
Shorter acting e.g. Oxazepam/lorazepam is more suitable in patients with hepatic impairment ○ Higher risk of dependence though
- Lorazepam better in hepatic impairment
- Highly lipophilic and extensive liver metabolism = in cirrhosis = higher active drug in
system
Why is Pabrinex used? Thiamine, ascorbic acid, nicotinamide, pyridoxine
- Malnourished - vitamin supplementation
- High in carbs, low in proteins
- IM not given due to clotting factor risk (coagulopathic) = high risk of bleeding
- Malabsorption in intestinal mucosa
Thiamine deficiency can cause polyneuritis with motor and sensory defects
Can cause Werknicke's encephalopathy
Ophthalmoplegia, nystagmus and ataxia
Learning and memory are impaired
- Dose: 1-3 pairs BD-TDS
- 1 pair = 250mg thiamine, 500mg ascorbic acid, 160mg nicotinamide, 50mg pyridoxine, 4mg riboflavin
- IM available (NOT if coagulopathic) IV in 50-100mL NaCl 0.9% or Dex 5% over 30 mins
○ Allergic reactions if bolus
Why is Prednisolone (steroid) used?
- For inflammation 5-7 days then 1 month if works but stopped after 7 days if no fall in bilirubin
- Increased risk infection and GI bleed
Usually prednisolone 40mg OD for 5-7 days (with PPI)
○ May prescribe Ca and vit D if long-term
○ Stop after 7 days if no fall in bilirubin
SE:
-Immunosuppressed
-Appetite increase
-Weight gain
-Drastic mood fluctuations
-Agitation
-Tapered dose necessary
How can abstinence be acheieved and What are the abstinence drugs ?
Abstinence can be achieved by:
• Psychological treatments
• Pharmacological treatments
• Combination of both
—
Drugs: Abstinence aids
- Acamprosate = taurine derivate stimulates GABA neurotransmission, crosses BBB, no hepatic excretion, no sedative effect
- Disulfiram = reduces alcohol consumption, irreversibly inhibits dehydrogenase
- Naltrexone = opiate antagonist = reduce alcohol craving
Symptoms of Acute Alcoholic Hepatitis?
- Jaundice and liver failure
- Reversible
- Fever, large liver, leucocytosis, ascites
- High creatinine too (renal pressure to excrete)
-Transplant is an option if patient is abstinent
LFT results for liver disease
• Raised AST, WCC, neutrophil count, Bilirubin and INR
-There are different s
Why do we no longer use Clormethiazole ?
- respiratory depression, addiction/dependence
Liver disease and clotting factors?
not being made as well
Other pharmacological management includes:
• Diuretics for ascites
• Propranolol for portal hypertension
• Vitamin K for coagulopathy
• Antibiotics for spontaneous bacterial peritonitis (SBP)
• Lactulose for hepatic encephalopathy (+ avoidance precipitants)
-TransplantatioN
Describe how alcohol dependece occurs and the effects of abrupt withdrawal - condense these notes
1️⃣ Neurotransmitter Effects & Dependence
Alcohol affects GABA, glutamate, dopamine, and opioid systems.
β-endorphins released during alcohol consumption stimulate dopamine, reinforcing pleasurable effects and dependence.
Alcohol enhances GABAergic inhibition, but chronic use leads to GABA receptor downregulation as the body adapts.
Glutamate (excitatory) is inhibited at low doses, but chronic use upregulates NMDA receptors to compensate.
2️⃣ Withdrawal & CNS Hyperactivity
Chronic alcohol use causes GABA-glutamate imbalance.
Sudden alcohol withdrawal removes inhibition, leading to excess glutamate activity and CNS hyperexcitability.
This can result in withdrawal seizures, tremors, and agitation.
Lecture 3
What to consider about drugs in liver disease?
• Pharmacokinetic properties (F, Vd, Cl) • Pharmacodynamic properties • Side-effect profile • Therapeutic Index • Route of administration
Resources to guide treatment
BNF/SPC recommendations
What does bilurubin tell us
- Drug absorption for highly lipophilic drugs = reduced absorption
- Biliary clearance - reduced
- Enterohepatic recirculation = reduced exposure and therapeutic effect
- Competition for protein binding = displace drug
What do Transaminase Enzymes, ALP and γ-GT tell us? - i don't understand this ngl gang
1️⃣ Transaminase Enzymes (AST & ALT) – Liver Cell (Hepatocellular) Damage
AST (Aspartate Aminotransferase) & ALT (Alanine Aminotransferase) are markers of liver cell injury.
No direct link between AST/ALT levels and drug concentration (AUC).
Drug-induced liver injury (DILI) can cause elevated AST/ALT.
2️⃣ Alkaline Phosphatase (ALP) & γ-Glutamyltransferase (γ-GT) – Cholestasis & Bile Flow Issues
ALP & γ-GT are markers of cholestasis (bile flow obstruction).
Some drugs cause cholestasis, which can reduce drug absorption.
Enzyme-inducing drugs (e.g., anticonvulsants, alcohol) can elevate γ-GT without liver damage.
What do Albumin and INR tell us?
1️⃣ Albumin & Liver Synthetic Function
Albumin is made by the liver → Low albumin = Reduced liver function.
The International Normalized Ratio (INR) measures blood clotting ability → High INR = Impaired liver function.
Both indicate reduced liver synthetic capacity, common in liver disease.
2️⃣ Effects on Drug Binding & Clinical Impact
Albumin binds many drugs; low albumin = less protein binding.
Highly protein-bound drugs (e.g., Phenytoin) have more "free" drug in circulation → Increased drug effect/toxicity.
3️⃣ Therapeutic Drug Monitoring (TDM) & Dose Adjustments
Low albumin can cause misinterpretation of TDM results (total drug levels may seem normal, but active free drug is higher).
If prothrombin time > 130% of normal, a dose adjustment may be needed for drugs affected by liver metabolism
What is the pharmacokinetics in liver disease?
- Reduced absorption
- Reduced protein binding
- Ascites
- Portal systemic shunting
- Reduced metabolism
- Cholestasis = reduced elimination
- Increase half-life and toxicity with repeat dosing
What are high extraction ratio drugs and low extraction drugs, how do they effect bioavailability?
drugs that are highly first-pass metabolised
- High 1 st pass = hepatic blood flow in liver disease reduced so bioavailability increases
- Low extraction drugs = bioavailability not affected
When is hepatic blood flow reduced
- Cirrhosis
- Portal vein thrombosis
- Cardiac failure
- Shock (low BP)
- Portal systemic shunting
What does hepatic cell mass show us
= functional capacity of the liver
Drug cautions
- Sedation
- GI ulceration - risk of bleedin in coagulopathy
- Constipation
- Clotting effect (interfere or have adverse effect on)
- Fluid retention
- Narrow Therapeutic index
Administration prefrences
- Oral preferred
- Avoid modified release and long acting preparations, if patient doesnt get on well with the drug, they have to deal with SE's for long
- Avoid IM in coagulopathy
- Topical may irritate but can be considered
What to consider for drugs for liver disease
• Is drug highly metabolised in liver? • What is the route of elimination? • What is it side-effect profile? • Consider hepatic blood flow and synthetic function • Be aware of potential renal impairment • Where possible - TDM • Think about route of administration • Titrate to patient response
Risk factors which may pre-dispose to drug induced liver diseas (DILD)
• Gender (tends to be more common in females) • Age • Genetics • Concurrent diseases e.g. obesity, diabetes, co-infection with HIV • Polypharmacy
Intrinsic vs. Idiosyncratic reactions
Intrinsic
• Predictable
• Reproducible
• Dose dependent
• Tend to occur rapidly e.g. within hours
• Tend to cause necrosis, acute liver failure
• E.g. paracetamol overdose
Idiosyncratic
• Not predictable
• Not reproducible
• Not dose dependent
• Tend to take longer to occur – weeks to months • Can result from metabolic idiosyncrasy or immunoallergic reaction
• Can cause any type of liver injury e.g. increased LFTs, jaundice, fever, rash, eosinophilia • E.g. NSAIDS (metabolic), carbamazepine (immunoallegic)
Types of DILD and associated drugs:
- Cholestasis = warfarin, azathioprine
- ALF = allopurinol, NSAIDs
- Steatosis = amiodarone, steroids, TPN
- Fibrosis cirrhosis = methotrexate
- Vascular = azathioprine