First Aid USMLE STEP 1: Respiratory
1/417
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
418 Terms
How many periods does it take to develop the lung?
What are they?
5
1) Embryonic (weeks 4-7)
2) Pseudoglandular (weeks 5-16)
3) Canalicular (weeks 16-26)
4) Saccular (weeks 26-birth)
5) Alveolar (weeks 32-8 years)
Describe the embryonic stage
Lung bud-> trachea-> mainstem bronchi-> secondary (lobar) bronchi-> tertiary (segmental) bronchi
**Errors at this stage can lead to TE fistula
Describe the Pseudoglandular stage
Endodermal tubules-> terminal bronchioles. Surrounded by modest capillary network
**Respiration impossible, incompatible with life
Describe the Canalicular stage
Terminal bronchioles-> respiratory bronchioles-> alveolar ducts.
Surrounded by prominent capillary network
Describe the Saccular stage
Alveolar ducts-> terminal sacs.
Terminal sacs separated by primary septae. Pneumocytes develop.
Describe the Alveolar stage
Terminal sacs-> adult alveoli (d/t secondary septation).
In utero, "breathing" occurs via aspiration and expulsion of amniotic fluid-> increase in vascular resistance through gestation. At birth, fluid gets replaced w/ air-> decrease in pulmonary vascular resistance
**At birth: 20-70 million alveoli
**By 8 years: 300-400 million alveoli
What are the 2 congenital lung malformations & describe them
1) Pulmonary hypoplasia= poorly developed bronchial tree w/ abnormal histology usually involving the right lung. Associated w/ congenital diaphragmatic hernia, bilateral renal agenesis (Potter Syndrome)
2) Bronchogenic cysts= Caused by abnormal budding of foregut & dilation of terminal or large bronchi. Discrete, round, sharply defined & air-filled densities on CXR. Drain poorly & cause chronic infections.
What are Type I pneumocytes?
thin squamous cells present in the alveoli, functioning in optimal gas diffusion
Where are Type I pneumocytes found?
97% of alveolar surfaces. (line the alveoli)
Role & epithelium of Type I pneumocytes
squamous. Thin for optimal gas diffusion
How is collapsing pressure calculated?
P = (2 x surface tension) / radius
What is the function of Type II pneumocytes?
secrete pulmonary surfactant --> decrease alveolar surface tension; prevent alveolar collapse, decrease lung recoil & increase compliance
What type of cells, histologically, are Type II pneumocytes?
cuboidal
Do Type II cells originate from Type I cells, or are Type II cells progenitors for Type I cells?
Type II cells are progenitors for Type I cells. Type II cells can also give rise to other Type II cells.
When do Type II cells proliferate?
in LUNG DAMAGE
What is the Law of Laplace?
As the radius decreases upon expiration, alveoli have an increased tendency to collapse.
What does "atelectasis" mean, and how is it caused?
DEFINITION collapse of alveoli
CAUSES obstruction, compression, or contraction
--> damage to Type II pneumocytes --> loss of surfactant
NOTE Even reinflation may not return full function due to the loss of surfactant.
What is surfactant, chemically?
a complex mix of lecithins, most importantly DIPALMITOYLPHOSPHATIDYLCHOLINE
What are Clara (Club) cells?
nonciliated, columnar cells with secretory granules
What do Clara cells secrete?
a "watery" component of surfactant
What are the functions of Clara cells?
to secrete a component of surfactant, to degrade toxins, and to act as reserve cells
When does surfactant synthesis begin?
around week 26 of gestation
When are mature levels of surfactant reached?
around week 35 of gestation
If a child is born premature, is it likely that they will produce sufficient levels of surfactant? If not, what is the child at risk of developing?
no
atelectasis
What measurement indicates if a fetus has mature lung function?
lecithin : sphingomyelin above 2
This can be measured in the amniotic fluid.
What is the cause of neonatal respiratory distress syndrome?
inadequate surfactant --> increased surface tension --> alveolar sac collapse after expiration --> formation of hyaline membranes
What lecithin:sphingomyelin ratio in amniotic fluid is predictive of neonatal RDS?
ratio <1.5
With what is neonatal RDS associated?
prematurity: adequate surfactant levels are not reached until week 35
C-section: d/t lack of release of stress-induced steroids (fetal glucocorticoids) --> no increased synthesis of surfactant
maternal diabetes: increased fetal glucose-> increased fetal insulin-> decreased surfactant levels
What are the clinical features of neonatal RDS?
increasing respiratory effort after birth
tachypnea with use of accessory muscles
grunting
hypoxemia with cyanosis
CXR showing "ground-glass" appearance of lung
What are the complications of neonatal RDS?
(1) persistently low O2 tension --> hypoxemia --> increased risk of PDA, necrotizing enterocolitis
(2) Therapeutic supplemental oxygen--> increased risk of free radical injury (O2 can be toxic!) --> "RIB"
R= Retinopathy of prematurity
I= Intraventricular hemorrhage
B= Bronchopulmonary dysplasia
What is the treatment for neonatal RDS?
maternal steroids before birth;
artificial surfactant for infant
What is the order of structures in the Respiratory tree?
Trachea-> bronchi-> bronchioles-> terminal bronchioles-> respiratory bronchioles-> alveolar sacs
What does smoking do the epithelial lining of the trachea?
pseudo stratified ciliated columnar-> squamous (via metaplasia & now sputum cannot be cleared)
Where is the highest & lowest resistance in the Respiratory Tree?
Highest= medium-size bronchi (turbulent airflow)
Lowest= terminal bronchioles (high CSA)
What is the conducting zone?
the larger airways that warm, humidify, and filter air without participating in gas exchange (i.e. anatomic dead space)
What are the large airways of the conducting zone?
nose, pharynx, trachea, bronchi
What are the small airways of the conducting zone?
bronchioles and terminal bronchioles (large #'s in parallel-> least airway resistance)
To what level of the conducting zone will cartilage and goblet cells extend?
bronchi
To what level of the conducting zone will psuedostratified ciliated columnar cells extend?
terminal bronchioles
**clear mucus & debris from lungs (mucociliary escalator)
To what level of the conducting zone will smooth muscle cells extend?
terminal bronchioles
What is the respiratory zone?
the airways participating in gas exchange
What are the airways of the respiratory zone?
lung parenchyma; respiratory bronchioles, alveolar ducts, alveoli
What is the histology of the respiratory bronchioles?
cuboidal cells
What is the histology of the alveoli?
simple squamous cells
You see simple squamous cells on a histology slide. From what level of the respiratory system is the slide?
alveoli or alveolar ducts
You see psuedostratified ciliated columnar cells on a histology slide. From what level of the respiratory system is the slide?
terminal bronchioles or above
You see cartilage on a histology slide. From what level of the respiratory system is the slide?
bronchi or above
You see goblet cells on a histology slide. From what level of the respiratory system is the slide?
bronchi or above
You see cuboidal cells on a histology slide. From what level of the respiratory system is the slide?
respiratory bronchioles
Are cilia present in the respiratory zone?
no
Where in the respiratory system may macrophages be found?
alveoli-> clear debris & participate in the immune response
Which lung has three lobes?
right lung
Which lung has two lobes?
left lung; in place of the middle lobe, the lung accommodates the space necessary for the heart.
"Left Lung has Less Lobes
Which lung has a lingula?
left lung
**lingula is a tongue shaped portion of the left lung
Which lung is the more common site for inhaled foreign bodies and why?
right lung; right main stem bronchus is wider and more vertical
"Swallow a bite, goes down the right"
The relation of the pulmonary artery to the bronchus at each lung hilum is described by?
RALS: Right Anterior; Left Superior
If a patient aspirates a peanut while upright, where in the lungs will it be found?
inferior (AKA basilar) portion of the right inferior lobe
If a patient aspirates a peanut while supine, where in the lungs will it be found?
superior portion of the right inferior lobe OR posterior portion of the right upper lobe
What structures perforate the diaphragm at T8, T10, and T12, respectively?
T8= IVC
T10= esophagus, vagus nerve (CN 10)
T12= aortic (red), thoracic duct (white), azygous vein (blue)
"I 8 10 Eggs At 12"
What is the innervation of the diaphragm?
C3, C4, C5 (phrenic nerve)
--C3, 4, and 5 keep the diaphragm alive--
Where might pain from the diaphragm be referred?
shoulder (C5)
trapezius ridge (C3, C4)
Name the bifurcations for the common carotid, trachea & abdominal aorta
C4= common carotid
T4= trachea
L4= abdominal aorta
"biFOURcates"
In quiet breathing, what muscle is responsible for inspiration?
diaphragm
In quiet breathing, what muscle is responsible for expiration?
none (passive process)
In exercise, what muscles are responsible for inspiration?
external intercostals, scalenes, sternocleidomastoid
--inSpiration: external, Scalene, Scm--
In exercise, what muscles are responsible for expiration?
rectus abdominus
internal obliques
external obliques
transversus abdominis
internal intercostals
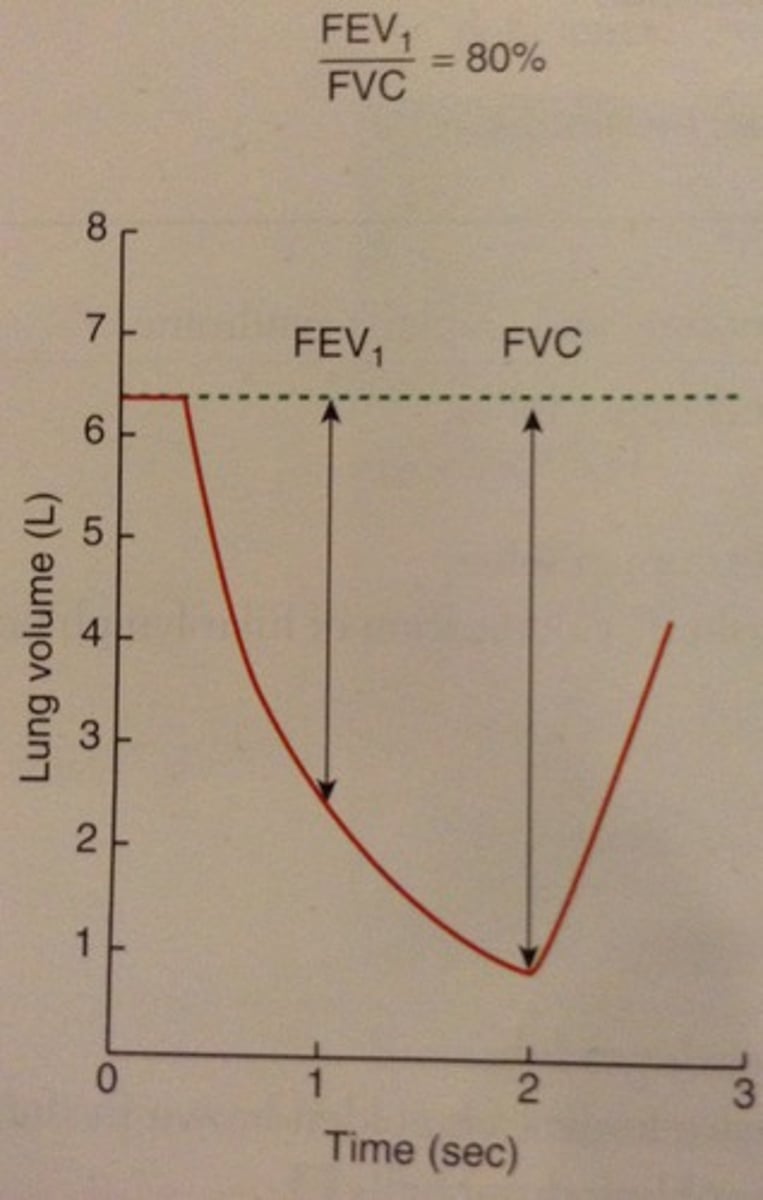
Graph: Normal Lung
What is the IRV?
Inspiratory Reserve Volume:
the air that can still be breathed in after normal inspiration
What is the TV?
Tidal Volume:
air that moves into lung with each quiet inspiration
What is the normal TV?
500
What is ERV?
Expiratory Reserve Volume:
air that can still be breathed out after normal expiration
What is RV?
Residual Volume:
the air in lung after maximal expiration
Which lung volume measurement cannot be read by spirometry?
RV (residual volume)
How is IC calculated?
Inspiratory Capacity = IRV + TV
How is FRC calculated?
Functional Residual Capacity = RV + ERV
Volume of gas in lungs after normal expiration; cannot be measured on spirometry
How is VC calculated?
Vital Capacity = IRV + TV + ERV
Maximum volume of gas that can be expired after a maximal inspiration
How is TLC calculated?
Total Lung Capacity = IRV + TV + ERV + RV
Volume of gas present in the lungs after a maximal inspiration; cannot be measured on spirometry
What is physiologic dead space?
anatomic dead space of conducting airways plus alveolar dead space (capable of gas exchange but no exchange occurs) in alveoli; volume of inspired air that does NOT take place in gas exchange
How is physiologic dead space calculated?
Vd = Vt x [(PaCO2 - PeCO2) / PaCO2]
"Taco, PAco, PEco, PAco"
Vd= physiologic dead space
Vt= Tidal Volume
PaCO2 = arterial PCO2
PeCO2 = expired air PCO2
What is the largest contributor of alveolar dead space?
apex of the lung d/t not enough blood flow
When is the physiologic dead space = anatomic dead space?
normal lungs
When is the physiological dead space grater than the anatomic dead space?
lung diseases w/ V/Q defects
What is pathologic dead space?
when part of the respiratory zone becomes unable to perform in gas exchange. Ventilation but no perfusion
Equation for Minute Ventilation
Total volume of gas entering lungs per minute
*Ve= VtRR
Equation for Alveolar Ventilation
Volume of gas per unit of time that reaches alveoli
*Va= (Vt-Vd)RR
What are the normal values for RR, Vd & Vt
RR= 12-20 breaths/min
Vd= 150 mL/breath
Vt= 500 mL/breath
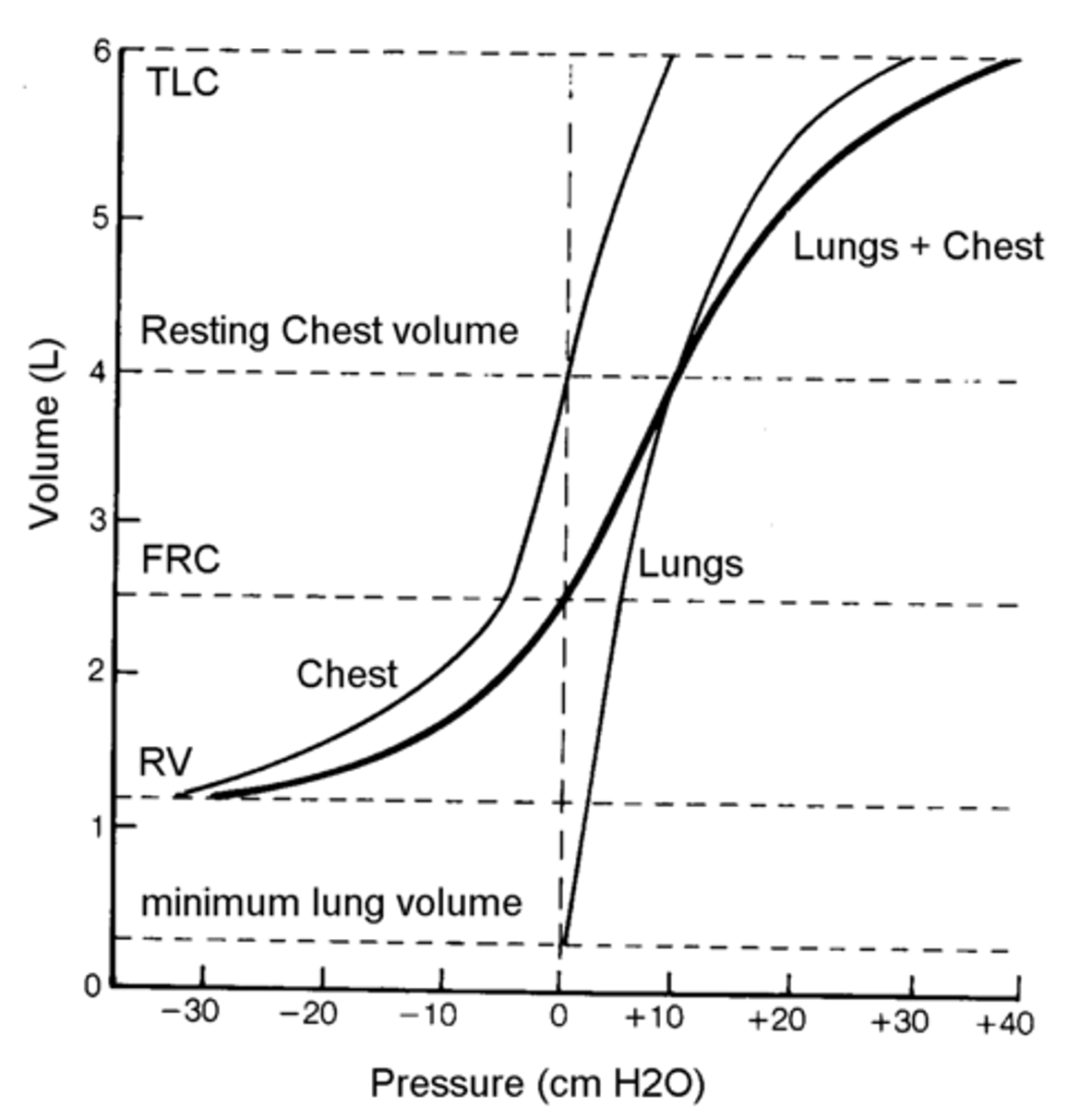
There is a tendency for the lungs to _____ _____ and chest wall to ____ ______.
collapse inward
spring outward
At FRC, what is the system pressure?
atmospheric; the inward pull of the lung is balanced by the outward pull of the chest wall.
What determines the combined volume of the chest wall and lungs?
their elastic properties
At FRC, what is the airway pressure?
0
At FRC, what is the alveolar pressure?
0
At FRC, what is the intrapleural pressure?
negative (This prevents pneumothorax). PVR is at a minimum
What is compliance?
the change in lung volume for a given change in pressure
[C= V/P]
**higher compliance= lung easier to fill
**lower compliance= lung hard rot fill
In what processes does compliance decrease?
pulmonary fibrosis
pneumonia
pulmonary edema
**FRC decreases b/c the lungs are now exerting more inward collapsing pressure
What are the causes of pulmonary edema?
HEMODYNAMIC: increased vascular pressure, decreased oncotic pressure
MICROVASCULAR DAMAGE: infection
ARDS
DIC
UNCLEAR: neurogenic, high altitude
In what processes does compliance increase?
emphysema
normal aging
**FRC increases because the lungs don't do a good job of resisting the outward pull of the chest wall
Pressure-Volume Curves of Lung and Chest Wall
Does surfactant increase or decrease compliance?
increase
What happens to intra-thoracic volume when the lung collapses?
increases d/t unopposed chest expansion
Discuss PVR for extra alveolar vessels & alveolar vessels at RV & TLC
RV= extra alveolar vessels have highest PVR
TLC= alveolar vessels have highest PVR