NURS330 Exam 1 Study Guide
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
148 Terms
First Pass Effect
- Absorbability of a drug
- First pass effect REDUCES the bioavailability of the drug
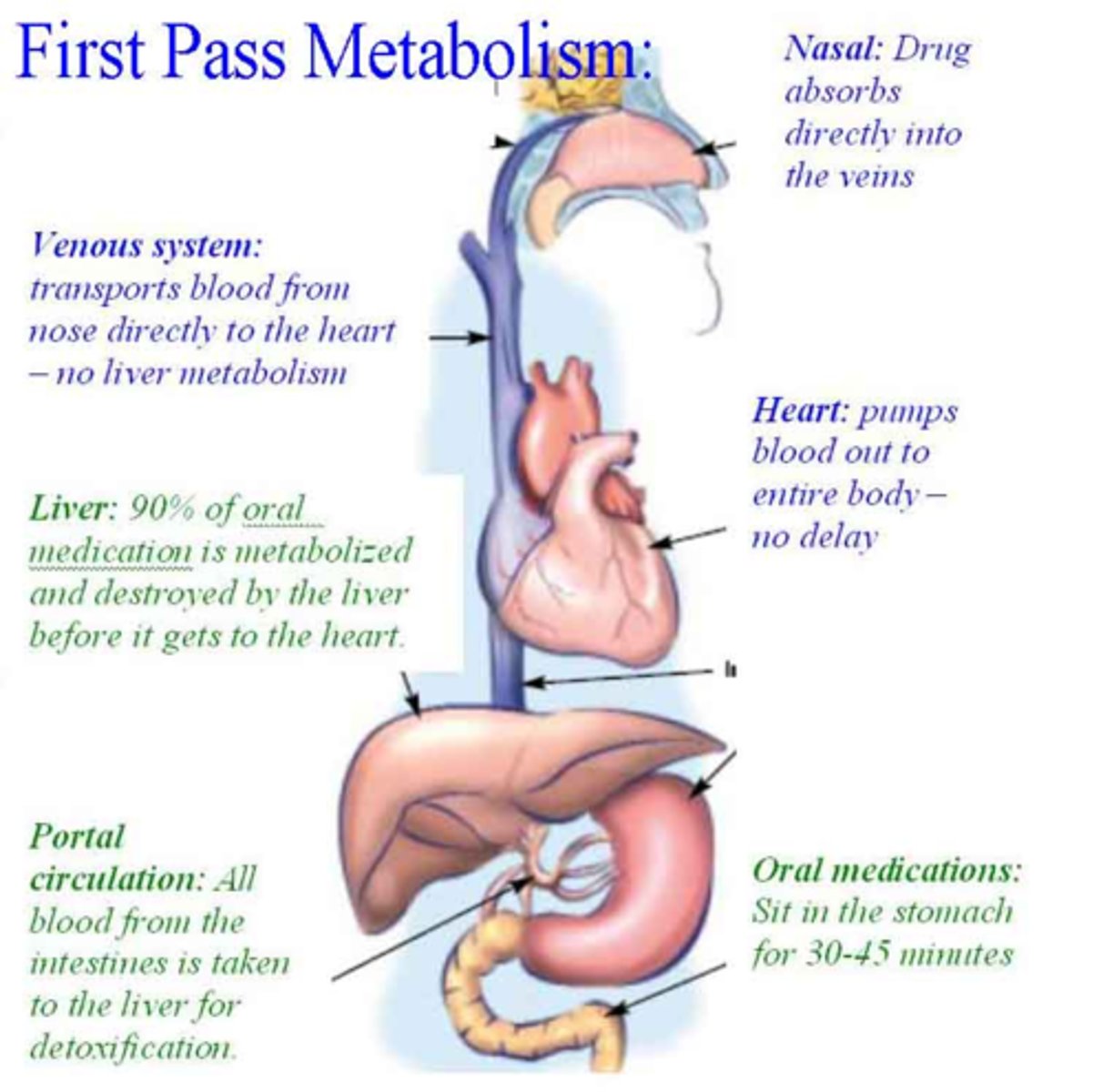
First Pass Effect Example
Any drug taken orally is impacted by the first pass effect since its changed chemically by the liver, leaving a smaller amount of drug available to move into circulation.
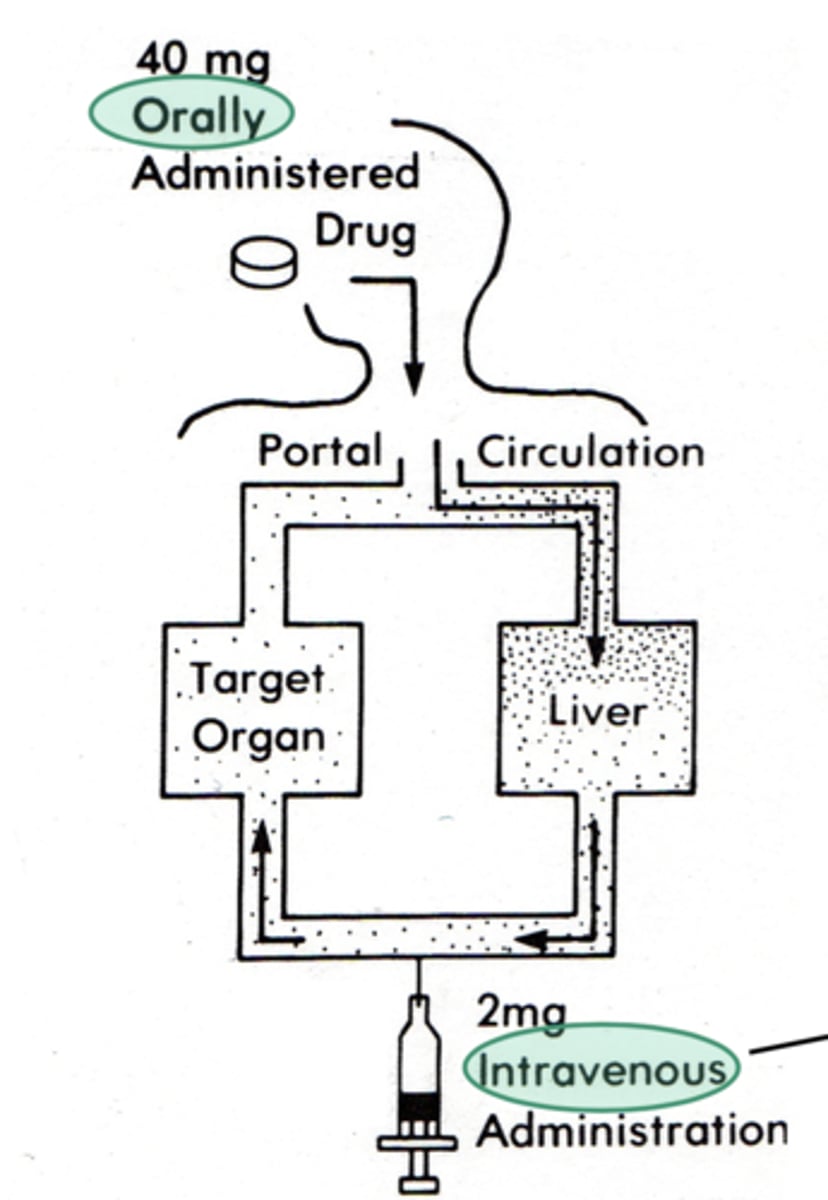
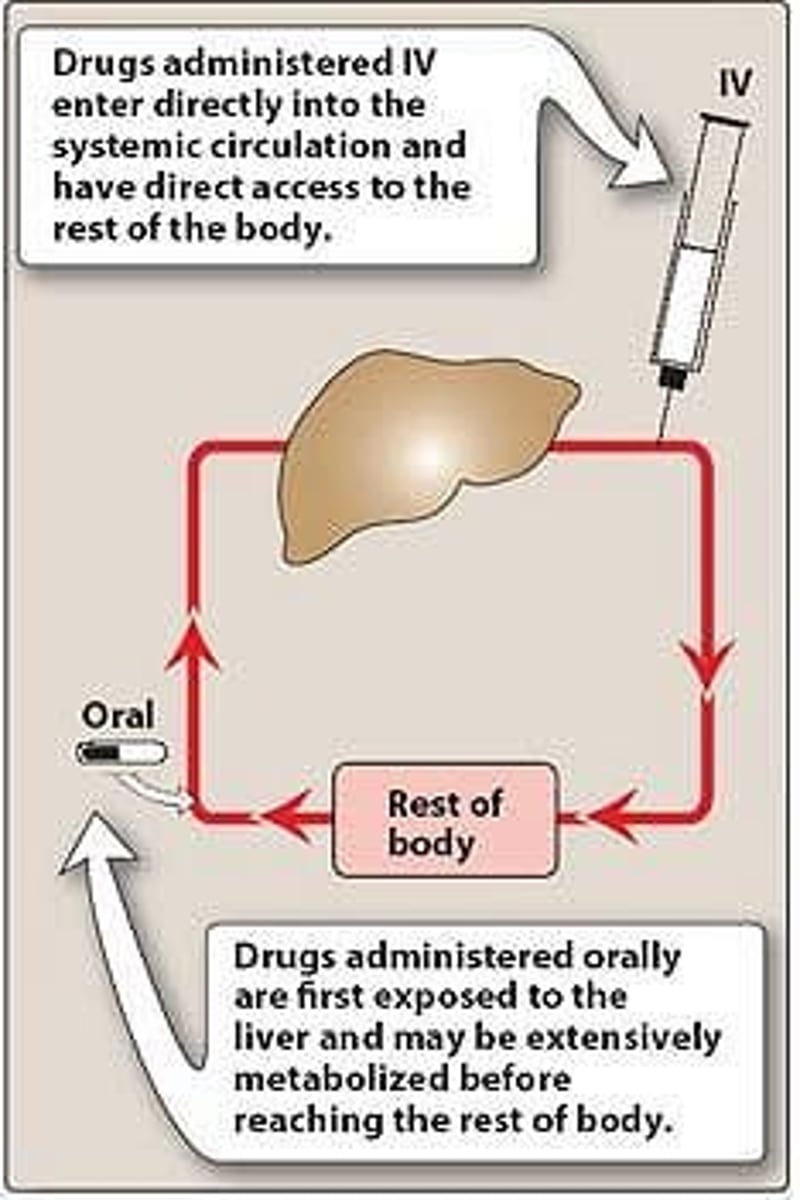
First pass effect and IV's?
IV drugs BYPASS First pass effect
- because it's 100% bioavailable as it's directly injected in the body's circulation through a vein.
Phases of drug activity (Box 2.2)
1. pharmaceutical phase
2. pharmacokinetic phase
3. pharmacodynamic phase
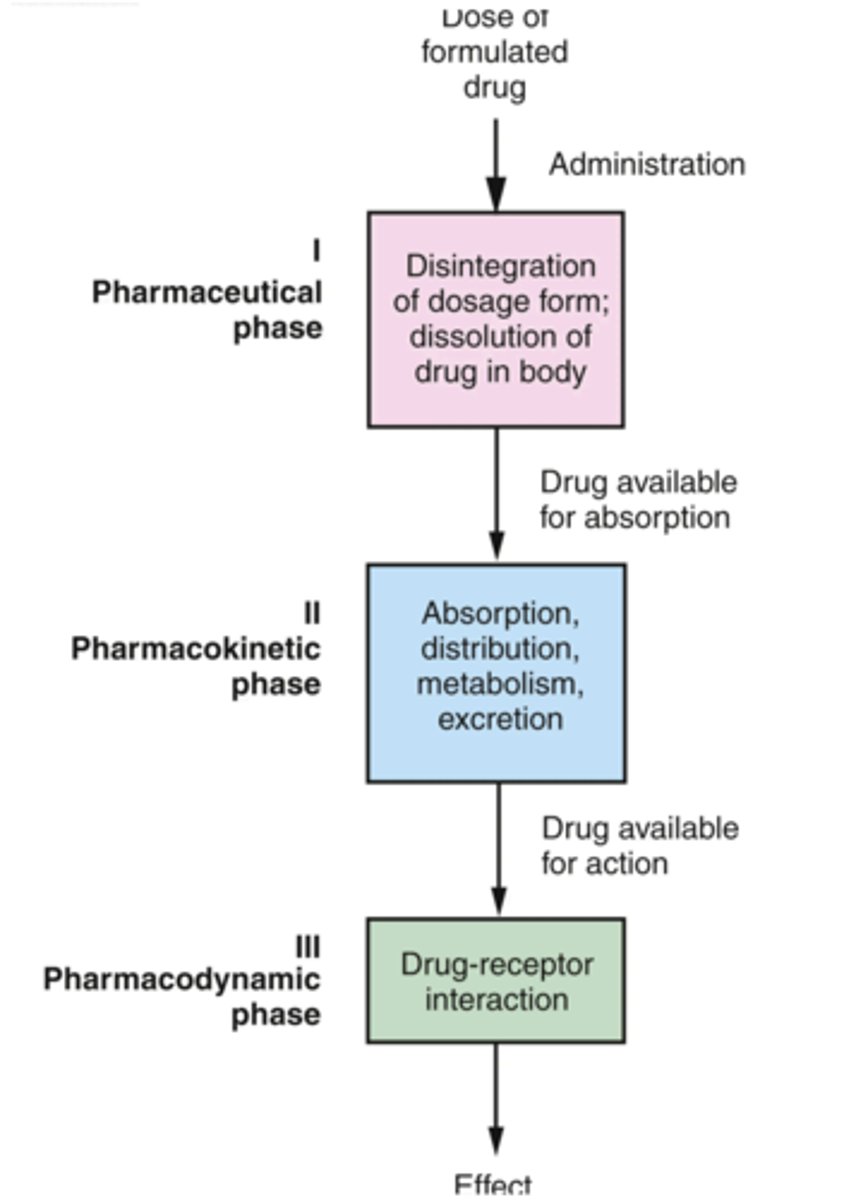
Four phases of Pharmacokinetics
1. Absorption
2. Distribution
3. Metabolism
4. Excretion
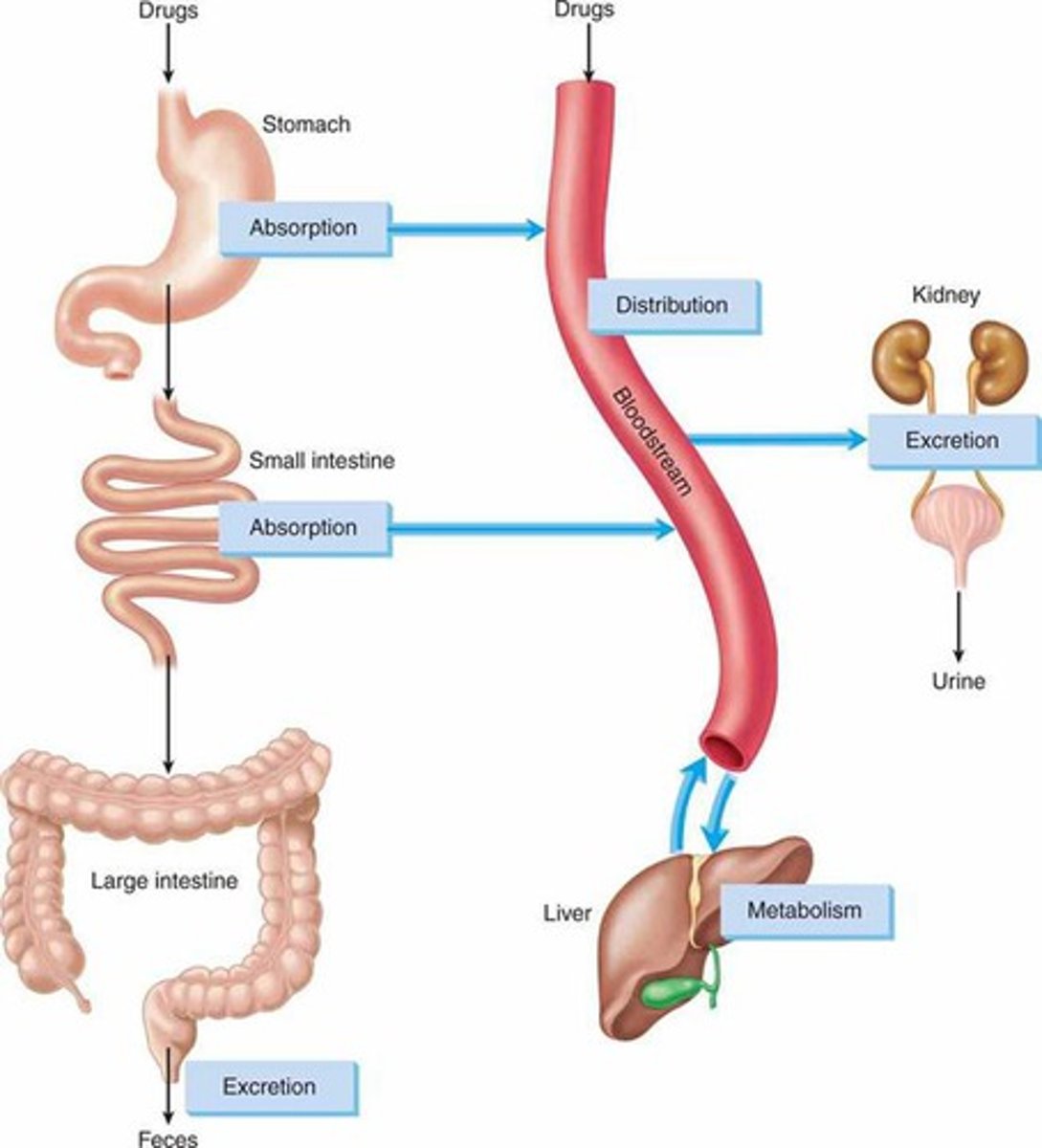
Absorption
Movement of a drug from its site of administration into the bloodstream for distribution to the tissues.
Bioavailability
A measure of the extent of drug absorption for a given drug and route (from 0% to 100%).
Distribution
Transport of a drug by the bloodstream to it's site of action.
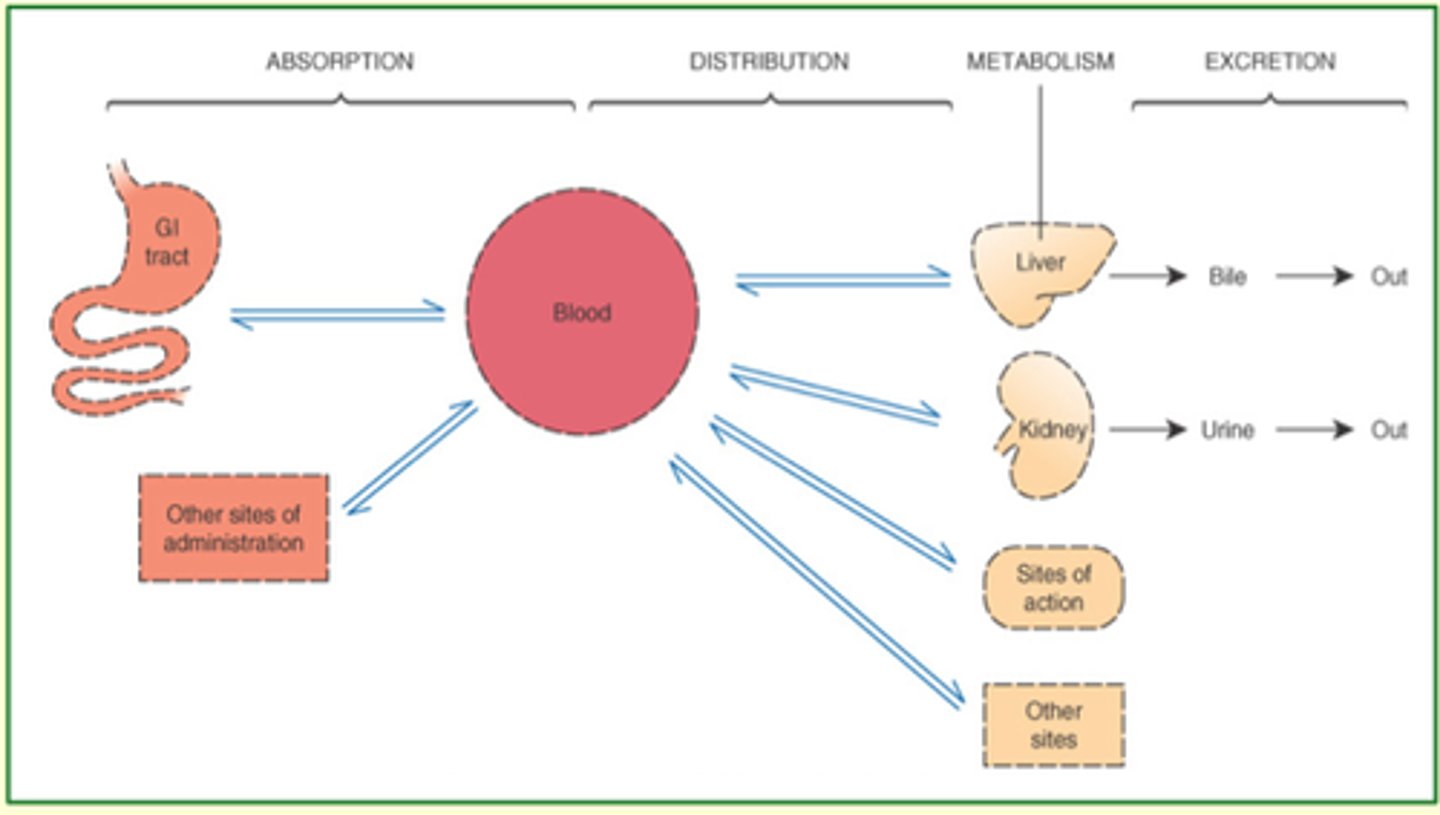
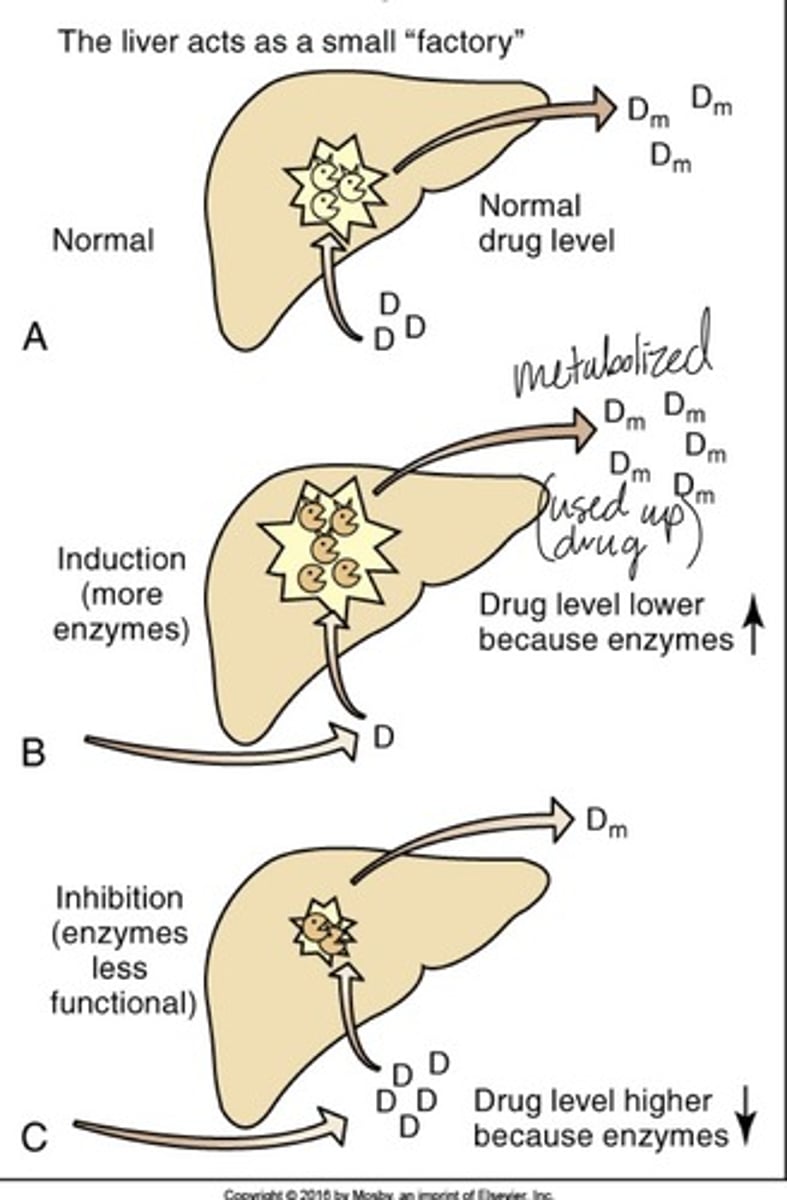
Metabolism
- a.k.a. "Biotransformation"
- Biochemical alteration of a drug into an inactive metabolite, a more soluble compound, a more potent active metabolite, or a less active metabolite.
- Organ (most) responsible: Liver
Excretion
Elimination of drugs from the body.
- Primary organ responsible: Kidney, then liver and bowel.

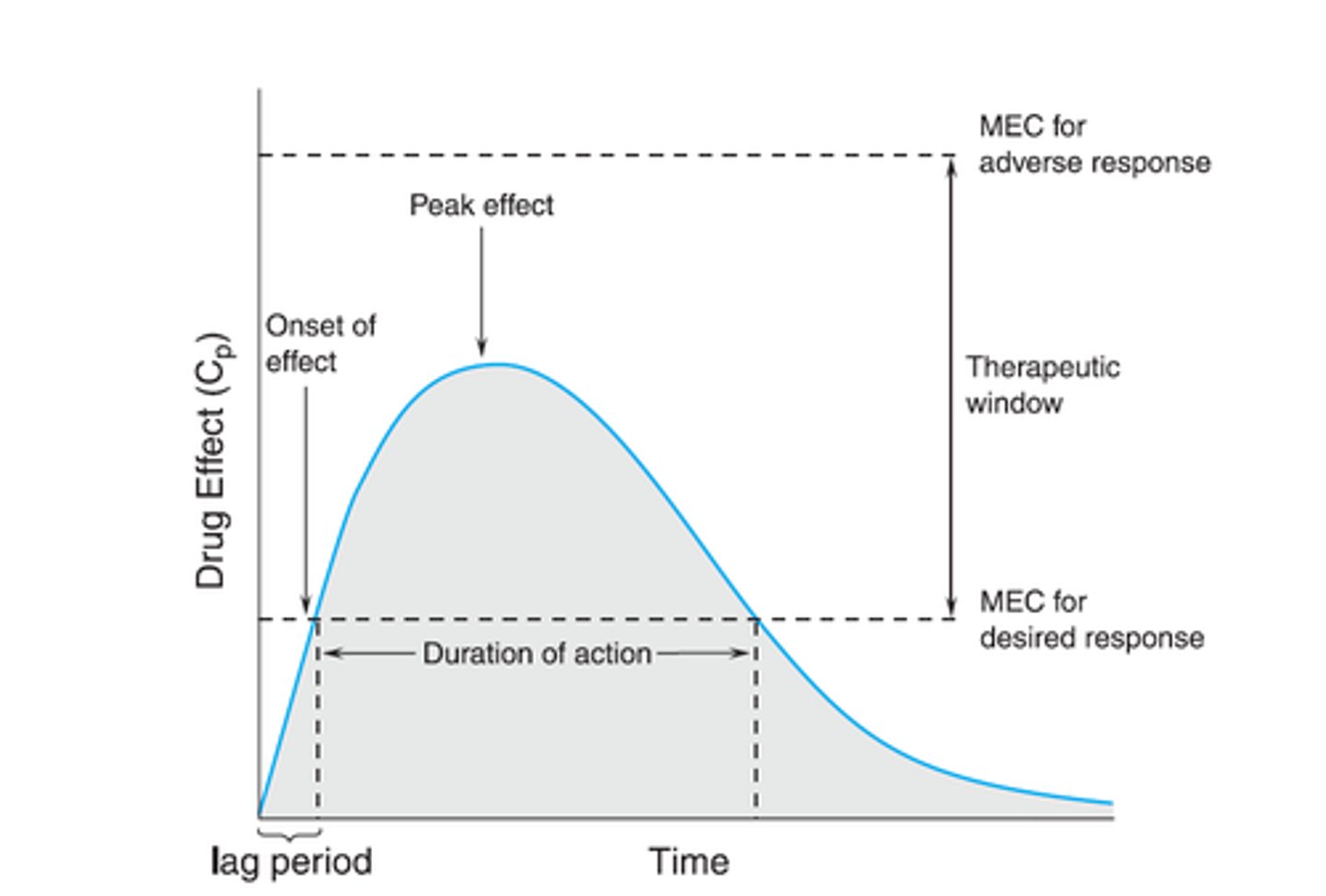
Onset of action
The amount of time from the administration of a medication to the onset of clinical effects.
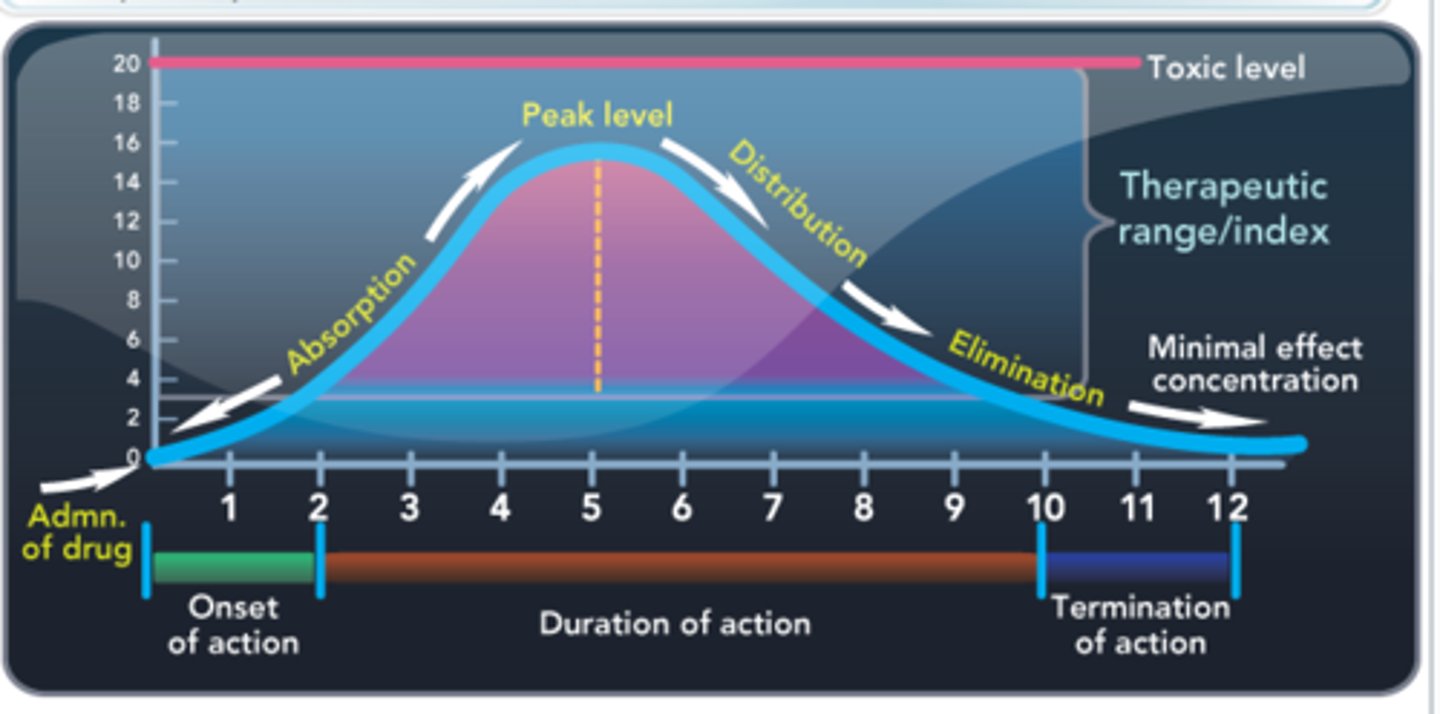
Peak of action
the point in time after administration when a drug exerts its maximal therapeutic effect
Duration of action
how long a drug actively produces a therapeutic effect
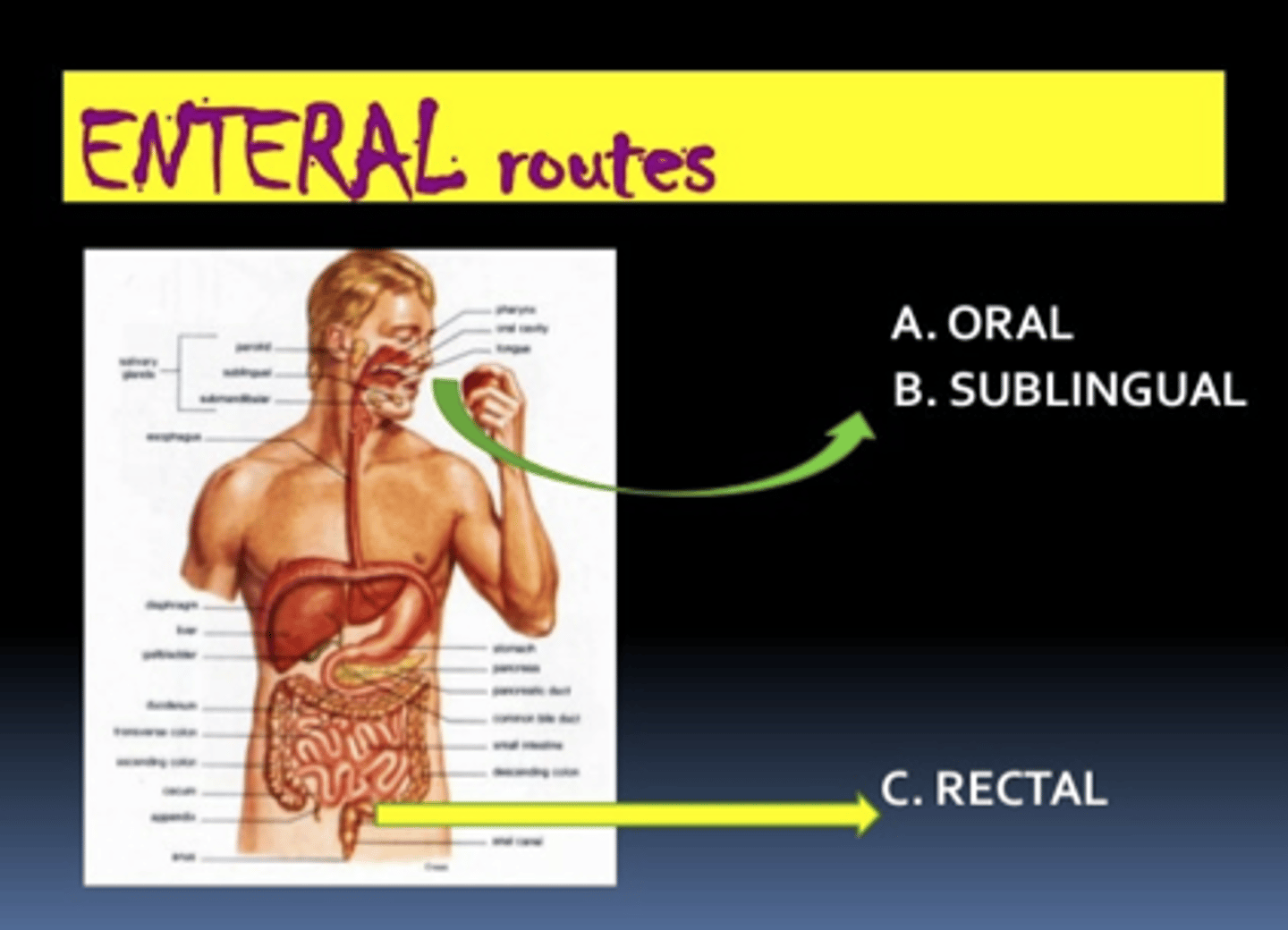
Enteral Drug Route
- Mouth to stomach
- "convenience route"
- Examples: orally, sublingual, NG tube etc.
Parenteral Drug Route
- Any route other than mouth
- Fastest route, 100% available
- Examples: intradermal, subcutaneous, intramuscular, or intravenously (RECTAL! - Prof Ford)
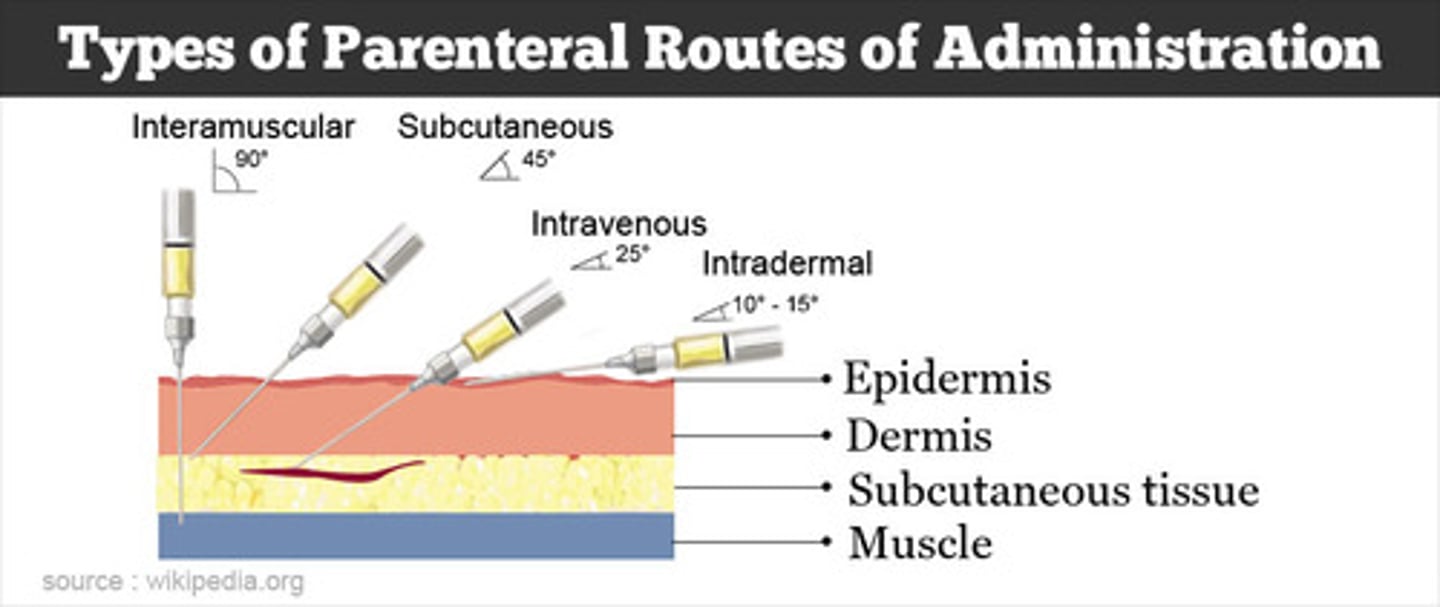
Fastest to Slowest Drug Route Absorption
1. Intravenous (IV)
2. Intramuscular (IM)
3. Oral liquids (solutions, syrups, elixirs)
4. Oral powders
5. Oral tablet & capsules
6. Rectal (suppositories, enemas)
Intravenous Drug Route
absorption
onset
bioavailability
- Absorption: None needed—drug goes directly into systemic circulation.
- Onset: Immediate.
- Bioavailability: 100%.
Intramuscular Drug Route
absorption
onset
bioavailability
- Absorption: Rapid but depends on blood flow to the muscle and the drug formulation (aqueous solutions absorb faster than oil-based suspensions).
- Onset: Minutes.
- Bioavailability: High, but not always complete.
Oral Liquids Drug route
absorption
onset
- Absorption: Faster than solid oral forms because drug is already dissolved.
- Onset: 15–30 minutes typically.
Oral Powders Drug route
absorption
onset
Absorption: Similar to liquids once dissolved, but slightly slower since they need to disperse in GI fluids first.
Oral Tablets & Capsules
absorption
onset
- Absorption: Slowest among oral forms because disintegration and dissolution must occur before absorption.
- Onset: 30–60+ minutes (varies with formulation—enteric-coated or sustained-release delay absorption further).
Rectal Drug Route
absorption
onset
Absorption: Variable and often slower than oral due to irregular blood flow, partial first-pass metabolism (depending on placement), and possible retention issues.
Onset: 30 minutes to several hours. Useful when oral route is not possible
Drug Route Key Contrasts
- IV vs. all others: IV bypasses absorption—instant effect and 100% bioavailability.
- IM vs. oral: IM is faster and avoids first-pass metabolism, but absorption depends on site and formulation.
- Liquids vs. tablets: Liquids are absorbed faster since they don’t require dissolution.
- Rectal vs. oral: Rectal can be an alternative when oral isn’t possible, but absorption is unpredictable.
IV Advantages
- Rapid onset
- Allows more direct control of drug level in blood
- Gives the option of a larger fluid volume, which allows dilution of irritating drugs
- Avoids first-pass metabolism
IV Disadvantages
- Often higher cost
- Requires IV access and not self-administered.
- irreversibility of drug action in most cases
- inability to retrieve meds
- risk for fluid overload
- greater change of infection
- possibility of embolism
Intramuscular(IM) and Subcutaneous (SUBQ) Advantages
- IM injections used with poorly soluble drugs which are given in "depot" preparation and absorbed over Prolonged Period.
- Can give several drugs given simultaneously (if compatible and w/o contraindications)
- IM and SUBQ faster absorption than Oral
Intramuscular(IM) and Subcutaneous (SUBQ) Disadvantages
- Discomfort with injection
- Inaccurate technique or improper landmarking = Risk of damage to blood vessels, nerves, and tissue.
- IM and SUBQ slower than IV
- Only small amounts of drugs may be given (IM up to 3 mL & SUBQ up to 1 mL)
Oral (PO) Advantages
- (Usually) easier, convenient and cheaper
- Safer than injection
- Dosing more likely to be reversible
- No complex equipment required
Oral (PO) Disadvantages
- Variabile absorption
- Slow onset of action
- Inactivation of some drugs by stomach acid or pH
- Problems with First pass effect
- Greater dependence of drug action on pt variables
- Possible nausea and vomiting from local irritation/irritate GI mucosa.
- Patient must be conscious and cooperative
Sublingual (SL) and Buccal Advantages
- Absorbed quicker than oral mucosa, rapid onset of action
- Avoids breakdown of drug by stomach acid
- Avoids first pass metabolism because gastric absorption is bypassed
Sublingual (SL) and Buccal Disadvantages
- Patients may swallow pill instead of keeping under tongue until dissolved
- Pills often smaller to handle
Rectal Advantages
- Relatively rapid absorption
- Good alternative when PO n/a
- Useful for local or systemic drug delivery
- Usually leads to mixed first-pass and non first-pass metabolism
Rectal Disadvantages
- Possible discomfort and embarrassment to patient
- Often higher cost than oral route.
Topical Advantages
- Delivers meds directly to affected area
- decreases likelihood of systemic drug effects
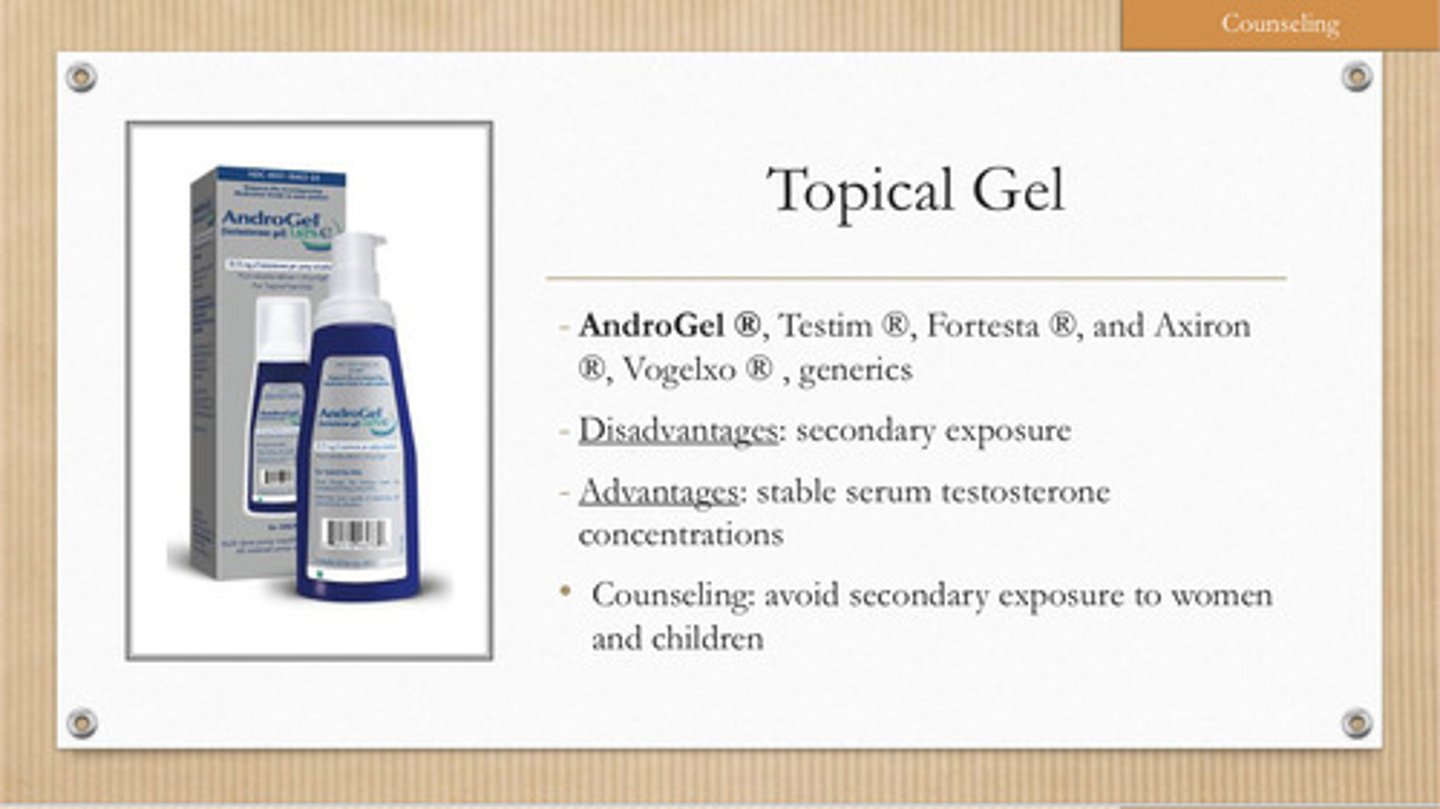
Topical Disadvantages
- Sometimes awkward to self-administer (ex eye drops)
- May irritate skin
- May be messy
- Usually higher cost than PO route
Transdermal (Subtype of topical) Advantages
- Provides relatively constant rate of drug absorption
- One patch lasts 1-7 days, depends on drug
- Avoids first-pass metabolism
Transdermal (Subtype of topical) Disadvantages
- Absorption rate affected by excessive perspiration and body temperature
- Patch can peel off
- Expensive
- Used patches need to disposed correctly.
- May irritate skin
- Drug absorption may be increased if skin is inflamed, abraded, or damaged, leading to systemic side effects
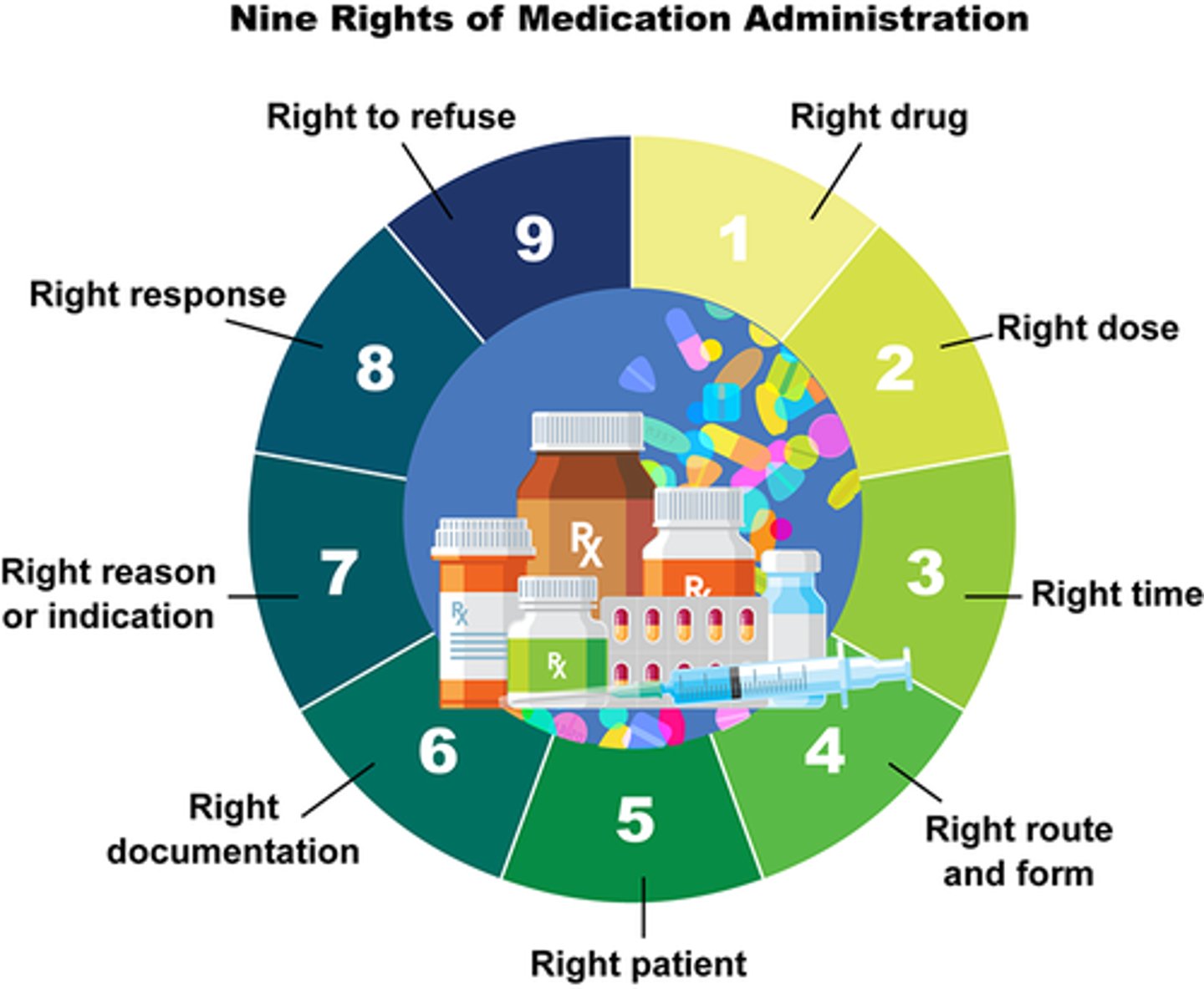
Rights of Medication Administration
1. right DRUG
2. right ROUTE
3. right DOSE
4. right TIME
5. right PATIENT
6. right DOCUMENTATION
7. right REASON
8. right TO REFUSE
9. right RESPONSE
Populations that metabolize drugs differently
- Babies
- Children
- Pregnant/breastfeeding
- Elderly
Why do babies, children, pregnant/lactating women and the elderly metabolize drugs differently?
- Drugs trials focus on adults (ages 18-65 y/o)
- Immaturity of organs
- Elderly have slower systems and aging organs, as well as likelihood of taking multiple drugs
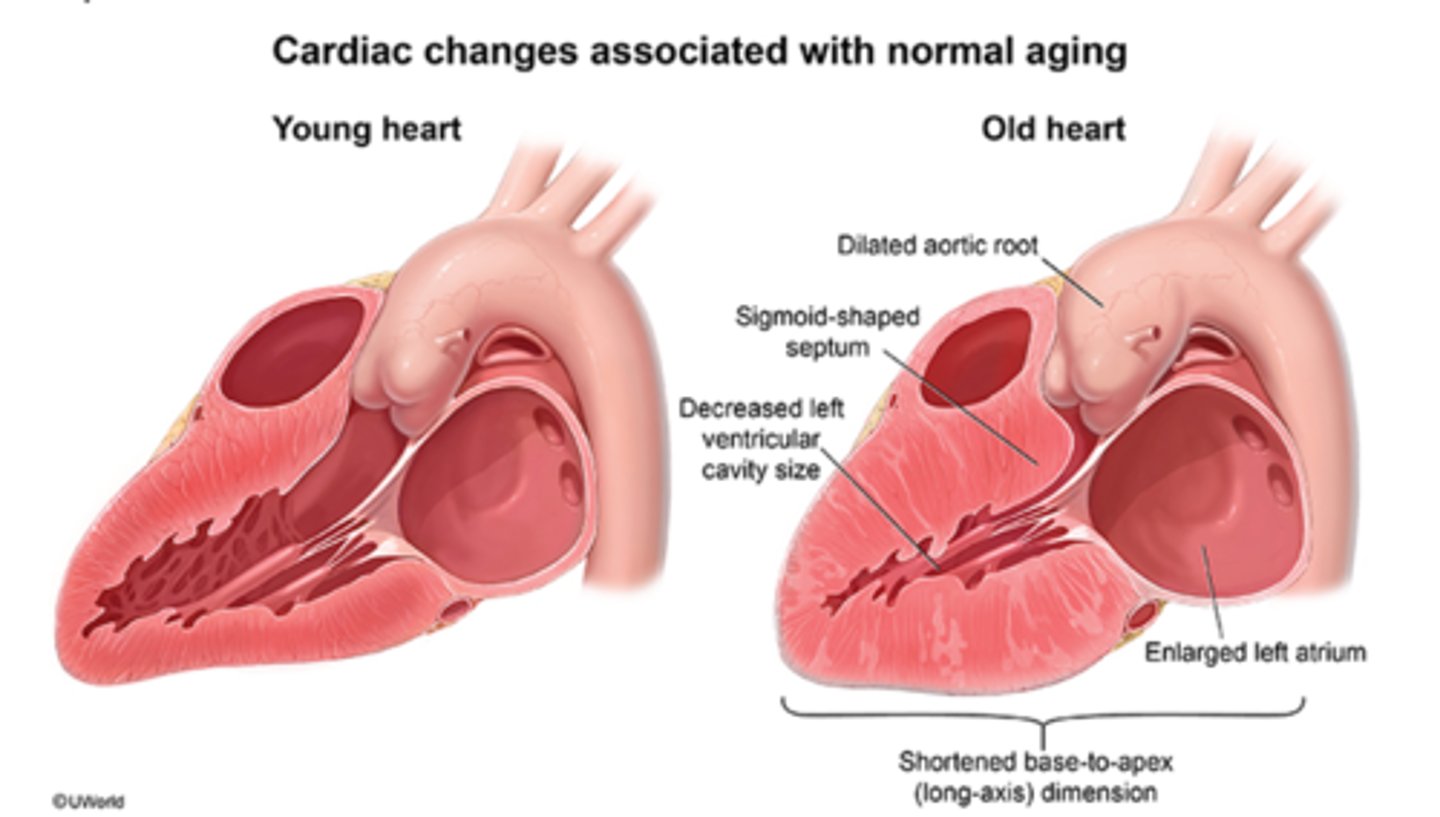
What four major body systems are affected negatively in the elderly?
1. Cardiovascular
2. GI
3. Liver
4. Kidneys
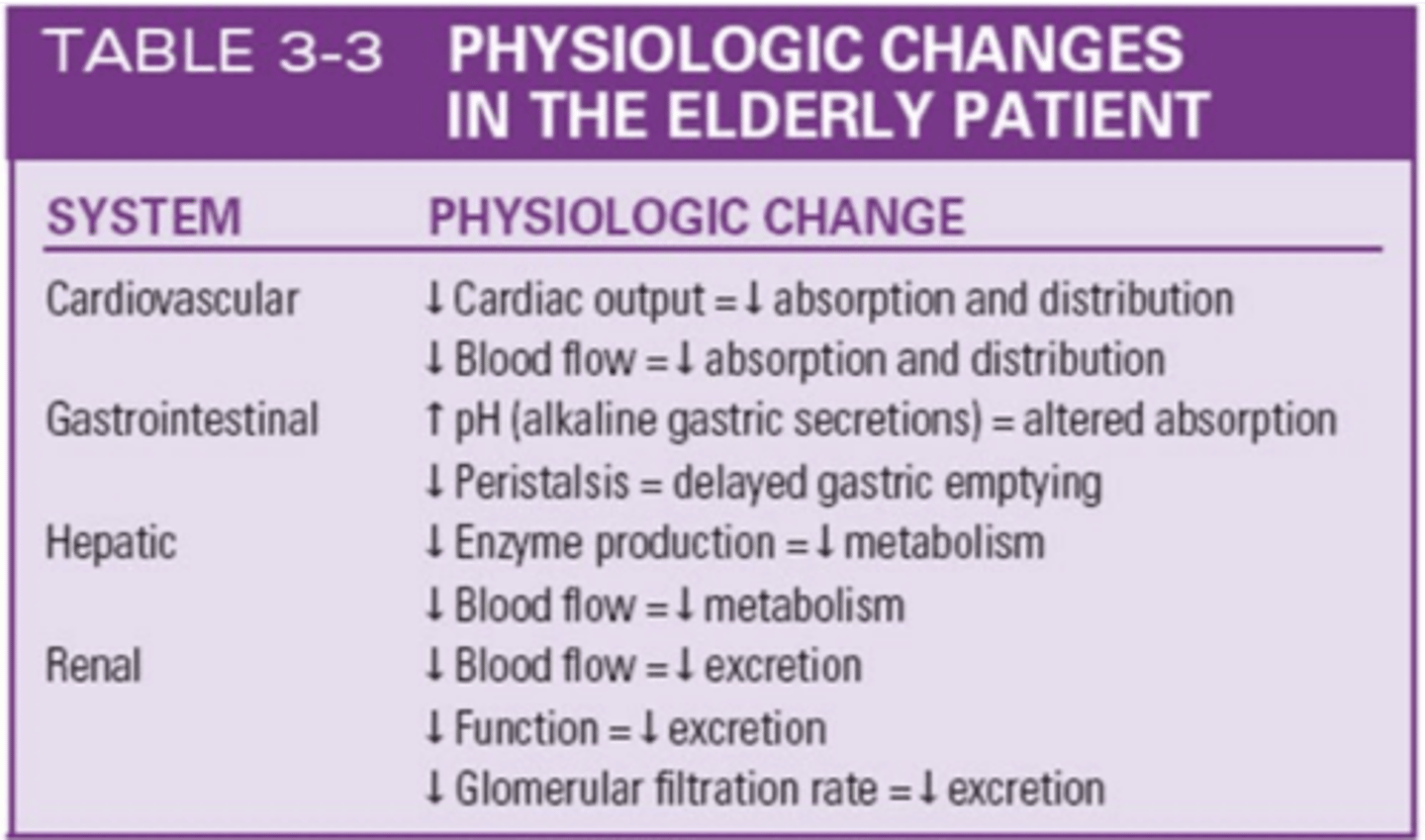
Cardiovascular Changes in Elderly Patient
- Decreased cardiac output = decreased absorption and distribution
- Decreased blood flow = decreased absorption and distribution
GI Changes in Elderly
- Increased pH (alkaline gastric secretions) = altered absorption
- Decreased Peristalsis = Delayed gastric emptying
Hepatic Changes in Elderly
- Decreased enzyme production = decreased metabolism
- Decreased blood flow = decreased metabolism
Monitor AST and ALT
Renal Changes in Elderly
- Decreased blood flow= Decreased excretion
- Decreased function = decreased excretion
- decreased GFR(Glomerular Filtration Rate) = Decreased excretion
Issues in Clinical Drug Use in the Elderly
- Polypharmacy
- Increased risk of drug interactions
- Pill splitting (financial)
- Poor understanding behind medication regimen
- Multiple providers and pharmacies
- increased medications = increased risk of ADRs (adverse drug rxn)
- Noncompliance
Absorption Changes in the Elderly
1. Decreased absorptive surface
2. Decreased splanchnic blood flow (stomach, intestines, liver, spleen, and pancreas)
3. Increased gastric pH
4. Gastric emptying and peristalsis slowed
5. Decreased gastric pH
Distribution Changes in the Elderly
- Decreased TBW (total body water) = decreased distribution of medications = increased risk for toxicity because of higher concentrations of drugs in the bloodstream
- Increased fat content due to lean body mass.
- Reduced protein binding sites (albumin) because of decreased production of proteins by the liver and reduced protein intake, leading to higher amounts of free drug.
Metabolism Changes in the Elderly
- Decrease of microsomal enzymes because of reduced capacity to produce them by the Liver
- Liver blood flow is reduced 1.5% every year after age 25, meaning decreased hepatic metabolism
- Decreased metabolism = potential drug toxicity
Excretion Changes in Elderly Adults
- Decreased GFR by 40-50%, mainly due to decreased blood flow
- Decreased amount of intact nephrons
- Drugs are cleared less effectively due to decreased excretion
- Creatine clearance is an important indicator in renal functioning; if abnormal, drug dosages may need to be adjusted by the provider
Special Consideration MEDICATIONS for Elderly Patients
1. Opioids
2. NSAIDs
3. Anticoagulants (heparin, warfarin)
4. Anticholinergics
5. Antidepressants
6. Antihypertensives
7. Cardiac glycosides (ex digoxin)
8. CNS depressants (ex muscle relaxants and opioids)
9. Sedatives and hypnotics
10. Thiazide diuretics
Common Complications of Opioids in the Elderly
- Confusion
- Constipation
- Urinary retention
- nausea
- vomiting
- respiratory depression
- falls
Common Complications of NSAIDs in the Elderly
- Edema
- Nausea
- Gastric ulceration
- Bleeding
- Renal toxicity
Common Complications of Anticoagulants(heparin, warfarin) in the Elderly
- Major and minor bleeding episodes
- Many drug interactions
- Dietary interactions
Common Complications of Anticholinergics in the Elderly
- Blurred vision
- Dry mouth
- Constipation
- Confusion
- Urinary retention
- Tachycardia
Common Complications of Antidepressants in the Elderly
Sedation and strong anticholinergic adverse effects
Common Complications of Antihypertensives in the Elderly
- Nausea
- Hypotension
- Diarrhea
- Bradycardia
- Heart failure
- Impotence (def: helplessness)
Common Complications of Cardiac Glycosides (ex. digoxin) in the Elderly
- Visual disorders
- Nausea
- Diarrhea
- Dysrhythmia
- Hallucinations
- Decreased appetite
- Weight loss
Common Complications of CNS Depressants (muscle relaxers, opioids) in the Elderly
- Sedation
- Weakness
- Dry mouth
- Confusion
- Urinary retention
- Ataxia (lack of coordination/balance)
Common Complications of Sedatives and Hypnotics in the Elderly
- Confusion
- Daytime sedation
- Ataxia
- Lethargy
- Increased fall risk
Common Complications of Thiazide Diuretics in the Elderly
- Electrolyte imbalance
- Rashes
- Fatigue
- Leg cramps
- Dehydration
Special Consideration CONDITIONS for Elderly Patients
1. Bladder flow obstruction
2. Clotting disorders
3. Chronic constipation
4. Chronic obstructive pulmonary disease (COPD)
5. Heart Failure and Hypertension
6. Insomnia
7. Parkinson's Disease
8. Syncope, falls
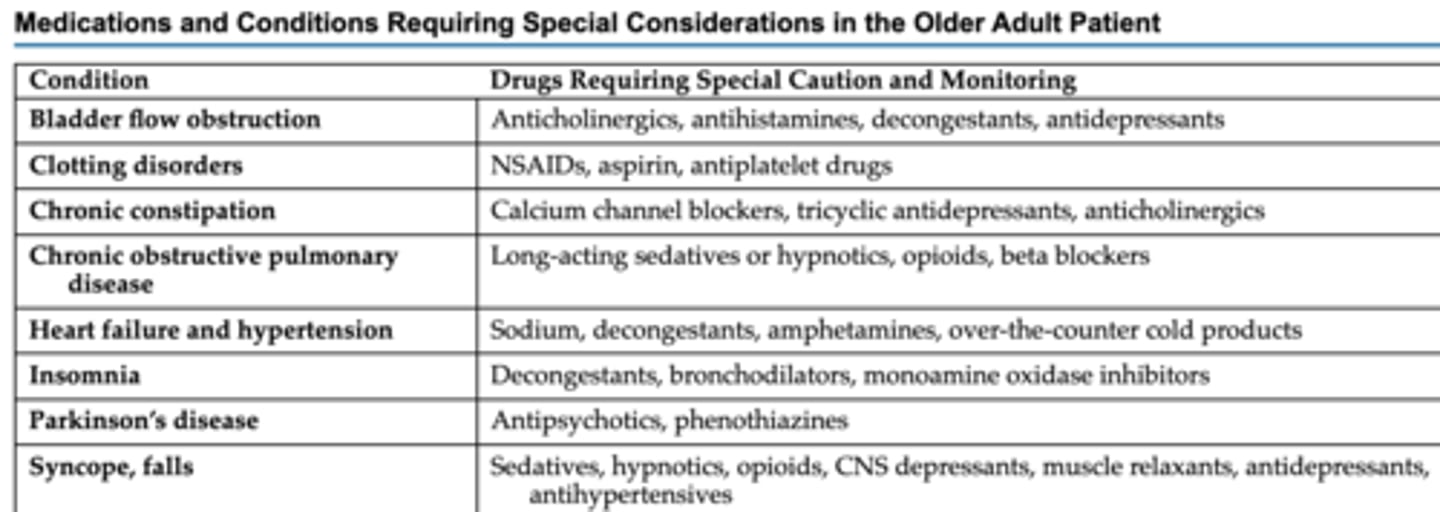
Drugs needing Special Caution/Monitoring for BLADDER FLOW OBSTRUCTION in the Elderly
- Anticholinergics
- Antihistamines
- Decongestants
- Antidepressants
Drugs needing Special Caution/Monitoring for CLOTTING DISORDERS in the Elderly
- NSAIDs
- Aspirin
- Antiplatelet drugs
Drugs needing Special Caution/Monitoring for CHRONIC CONSTIPATION in the Elderly
- Calcium channel blockers
- Tricyclic antidepressants
- Anticholinergics
Drugs needing Special Caution/Monitoring for COPD in the Elderly
- Long-acting sedatives or hypnotics
- Opioids
- Beta-blockers
Drugs needing Special Caution/Monitoring for HEART FAILURE & HYPERTENSION in the Elderly
- Sodium
- Decongestants
- Amphetamines
- OTC Cold medications
Drugs needing Special Caution/Monitoring for INSOMNIA in the Elderly
- Decongestants
- Bronchodilators
- Monoamine oxidase inhibitors
Drugs needing Special Caution/Monitoring for PARKINSONS DISEASE in the Elderly
- Antipsychotics
- Phenothiazines
Drugs needing Special Caution/Monitoring for SYNCOPE/FALLS in the Elderly
- Sedatives
- Hypnotics
- Opioids
- CNS Depressants
- Muscle relaxants
- Antihypertensives
1 kg =
2.2 lbs
Three Factors Contributing to Safety/Potential Harm of Drug Therapy during Pregnancy
1. Drug properties
- ex. dose and duration
2. Fetal gestational age
- 1st Trimester = Greatest risk for drug-induced developmental defects
- 3rd Trimester = Increased risk of drug transfer to fetus
3. Maternal factors
- mom's kidney and liver function
Why do kids not metabolize drugs well?
- Skin is thinner; more permeable (ointment absorbs quickly)
- Stomach lacks acid to kill bacteria
- Lungs have weaker mucus barriers
- Body temp is less well regulated, with potential dehydration
- Liver and kidneys not fully mature, making drug metabolism and excretion impaired
Absorption in Pediatric Patients
• Gastric pH is less acidic because acid-producing cells in the stomach are immature until approximately 1 to 2 years of age.
• Gastric emptying is slowed because of a slow or irregular peristalsis.
• First-pass elimination by the liver is reduced because of the immaturity of the liver and reduced levels of microsomal enzymes.
• Intramuscular absorption is faster and irregular.
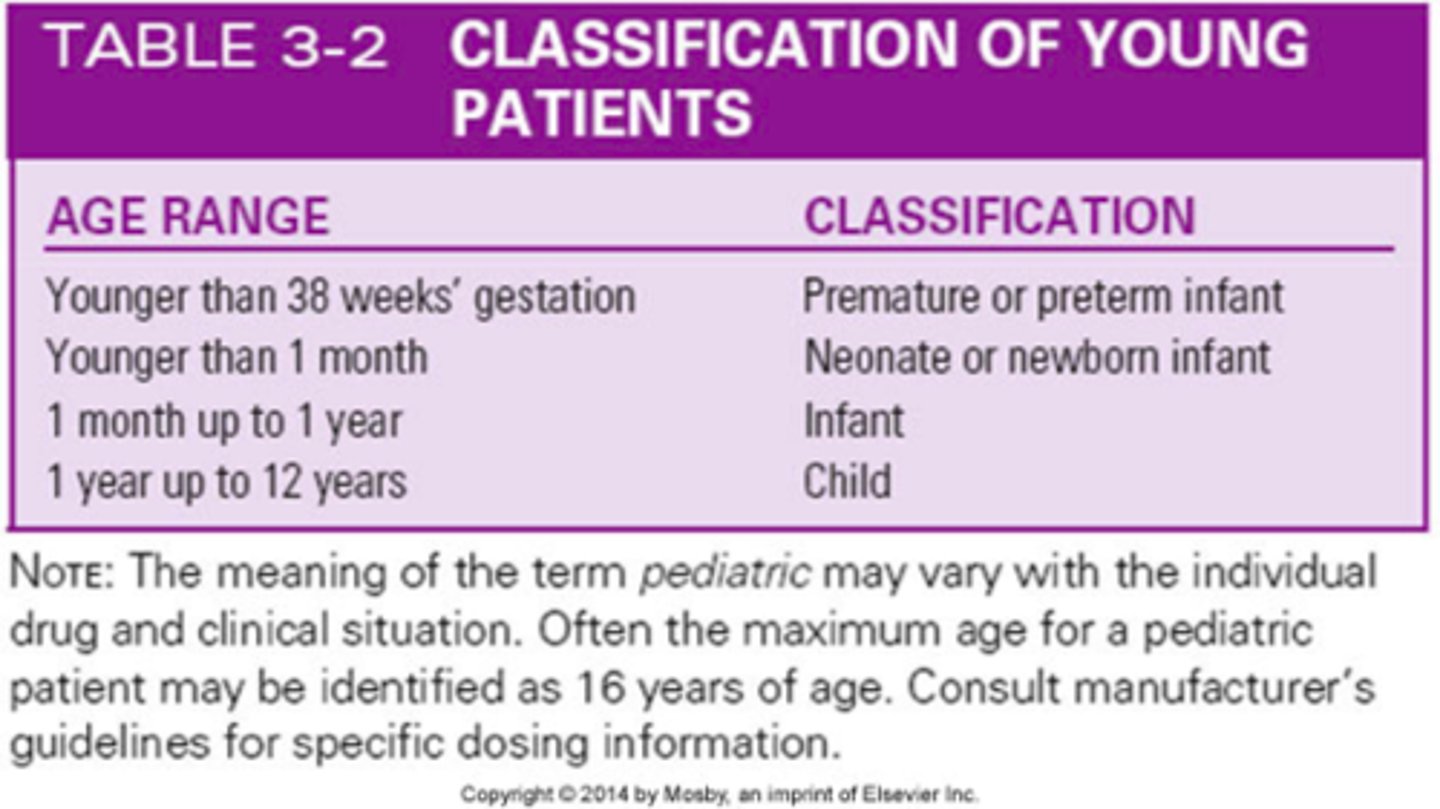
Distribution in Pediatric Patients
• Total body water is 70% to 80% in full-term infants, 85% in premature newborns, and 64% in children 1 to 12 years of age.
• Fat content is lower in young patients because of greater total body water.
• Protein binding is decreased because of decreased production of protein by the immature liver.
• More drugs enter the brain because of an immature blood-brain barrier.
Metabolism in Pediatric Patients
• Levels of microsomal enzymes are decreased because the immature liver has not yet started producing enough.
• Older children may have increased metabolism and require higher dosages once hepatic enzymes are produced.
• Many variables affect metabolism in premature infants, infants, and children, including the status of liver enzyme production, genetic differences, and substances to which the mother was exposed during pregnancy.
Excretion in Pediatric Patients
- Glomerular filtration rate and tubular secretion and resorption are all decreased in young patients because of kidney immaturity.
- Perfusion to the kidneys may be decreased, which results in reduced renal function, concentration ability, and excretion of drugs.
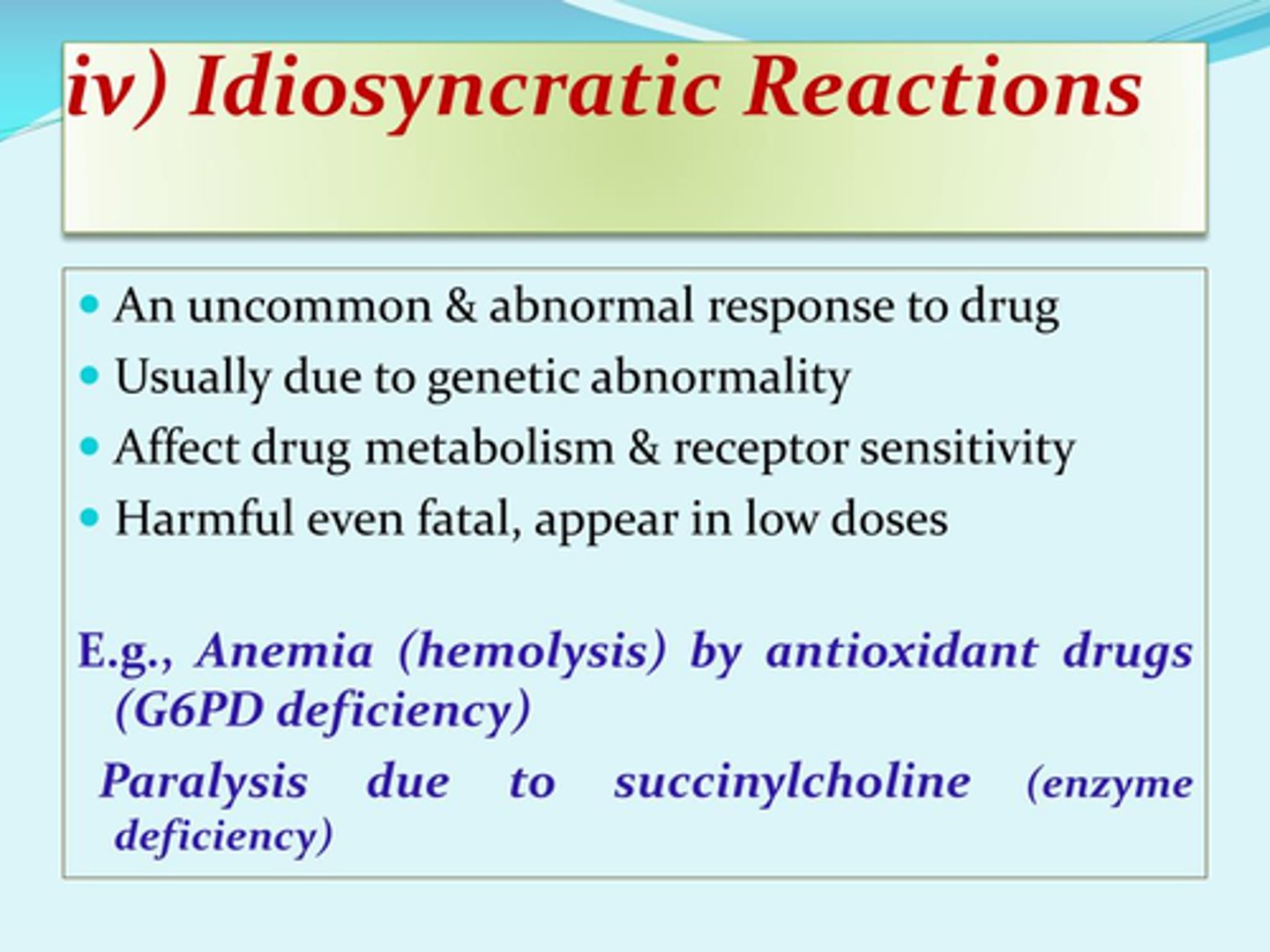
Adverse Drug Event
any undesirable occurrence related to administering or failing to administer a prescribed medication
Adverse Drug Events Include:
1. Medication errors
2. Adverse drug responses (ADRs)
- ex. Allergic rxn
- ex. Idiosyncratic rxn
Adverse Drug Reactions
Unexpected, unintended, or excessive responses to medications given at therapeutic dosages (as opposed to overdose)
- one type of adverse drug event.
Allergic Reaction
An immunologic hypersensitivity reaction resulting from the unusual sensitivity of a patient to a particular medication
- a type of adverse drug event.

Idiosyncratic Reaction
An abnormal and unexpected response to a medication, other than an allergic reaction, that is peculiar to an individual patient.
Medical Errors
A broad term used to refer to any errors at any point in patient care that cause or have the potential to cause patient harm
Medication Errors
any preventable adverse drug events involving inappropriate medication use by a patient or health care professional
- may or may not cause patient harm
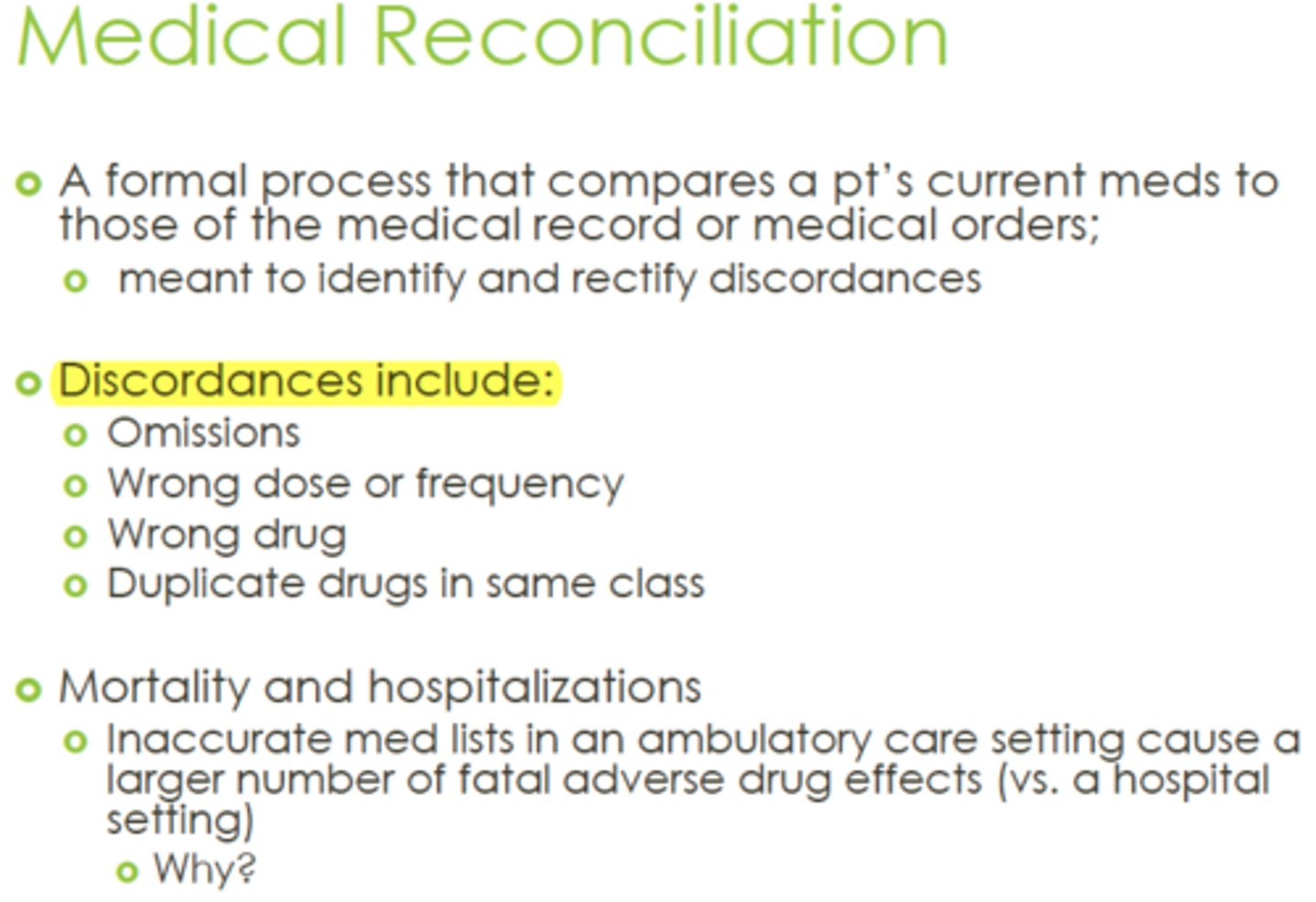
Medication Reconciliation
A procedure to maintain an accurate and up-to-date list of medications for all patients across all phases of health care delivery
Near Miss
- Event or situation that didn't produce patient injury, but only by miracle/by chance
- Must still be reported so that safety can be addressed and future incidents are prevented

Preventing Medication Errors
- Checks medication order THREE times before giving the drug
- Apply "Nine Rights" of Medication Administration
- Use TWO patient identifiers
- Didn't draw it? DON'T give it!
- Minimize verbal or telephone orders.
- List drug indications next to each other
- Learn special administration techniques of certain dosage forms
- Verify new medication administration
- Read labels.
- Use generic names to avoid sound-alike trade names
- Verify allergies
- Listen and honor patients' concerns
- Know where to find info on meds, prep, side-effects; use current sources
- Mandatory 2nd nurse verification for high-risk meds
- Minimize interruptions when prepping medications
Should you use a trailing zero with medication orders? example: 1.0 mg
False (correct 1 mg)
Should you use a leading zero for decimal dosages? example: 0.25mg
True!
- .25 mg incorrect
- 0.25 mg correct!
Reporting Medication Errors
1. Report to prescriber and nursing management
2. Document error per policy and procedure
3. Factual documentation only
--Medication administered
--Actual dose
--Observed changes in patient condition
--Prescriber notified/ follow-up orders
Additional Prevention for Pediatric Med Errors
Obtain and document accurate weight (kg)
OTC Acid-controlling drugs, Antacids, and Proton Pump inhibitors
- famotidine (Pepcid AC)
- aluminum and magnesium-containing products (Maalox, Mylanta)
- calcium containing products (Tums)
- esomeprazole (Nexium 24)
- lansoprazole (Prevacid-24)
- omeprazole (Prilosec-OTC)

OTC Antifungal drugs (topical)
- clotrimazole (Lotrimin)
- miconazole (Monistat)
- terbinafine (Lamisil AT)
OTC Antihistamines and decongestants
- brompheniramine (Dimetapp)
- cetirizine (Zyrtec)
- chlorpheniramine (Theraflu)
- diphenhydramine (Benadryl)
- fexofenadine (Allegra)
- guaigensin (Robitussin)
- loratadine (Claritin)
- pseudoephedrine (Sudafed)

OTC Eyedrops
- Artificial tears (Moisture Eyes)

OTC Hair growth Drugs (topical)
- minoxidil (Rogaine)
OTC analgesics
- acetaminophen (Tylenol)

OTC NSAIDs
- aspirin
- ibuprofen (Advil, Motrin)
- naproxen sodium (Aleve)

OTC Nasal Steroids
-fluticasone (Flonase)
-triamcinolone acetonide (Nasocort)

OTC Smoking Deterrents
- transdermal nicotine patches
- nicotine gum
