Hair, Nails, and Pigmentation Disorders
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Alopecia
absence of hair from where it normally grows
-termed effluvium or defluvium
Scarring Alopecia
a type of alopecia where inflammatory disorders lead to permanent hair loss and follicle destruction
-aka cicatricial
-subtypes include lymphocytic, neutrophilic, and mixed
Non-Scarring Alopecia
a type of alopecia that lacks inflammation and there is no destruction of the follicle
-aka non-cicatricial
-subtypes include focal, patterned, diffuse
-androgenic alopecia, alopecia areata, telogen effluvium
Structural Alopecia
a type of alopecia due to brittle or fragile hair from abnormal hair formation or external insult
-patient is doing something to make their hair fall out
Androgenic Alopecia
most common type of alopecia, hair transitions from terminal to vellus hair
-more common in males

Alopecia Areata
alopecia with an onset usually prior to 30 years
-men and women are equally affected
-causes bald spots

Scarring Alopecia
very rare
-inflammatory disorder leads to permanent, centrifugal destruction of follicle
not, premature, telogen, growth
Pathophysiology of Non-scarring Alopecia
-Hair follicle is ___ damaged
-T cell mediated inflammation resulting in _________ transition to catagen and _______ phases
-Shortens opportunity for hair ________
progressive, DHT
Pathophysiology of Pattern Hair Loss
-Most common type of _________ balding
-___ is the key androgen involved in androgenic alopecia, which is where the hair transitions from terminal to vellus hairs
-Drugs
Trichotillomania
intentional pulling of hair from the scalp
-see broken hair of varying lengths on physical exam
Diffuse Alopecia
hair loss all over the body
Telogen effluvium
sudden shift of many follicles from anagen to telogen phase resulting in decreased hair density but not bald areas (thinning)
-can follow major stressors 2-3 months after event, chronic with illness
Anagen effluvium
interruption of the anagen phase without transition to telogen phase
-chemotherapy is the most common trigger
inherited, chemical, processing
Pathophysiology of Structural Hair Disorders
-_________ disorders
-Can also be due to _______/heat damage due to hair __________ treatments like straightening, curling, perms, and keratin treatments
genetic, stress, chemotherapy, extensions
Risk Factors of Alopecia
-__________ predisposition
-Chronic illness
-Physiologic _______ like pregnancy or birth
-Poor nutrition
-Medications, __________, radiation
-Hair chemical treatments, braids, weaves, and hair _________
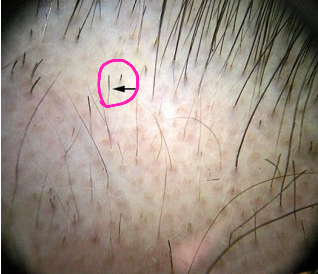
Exclamation point
On physical exam, a patient with alopecia areata would present with __________ ______ hairs, which is where a short hair breaks off with tapering down toward the proximal hair shaft
thinning, loss, normal, abnormalities
Clinical Manifestations of Alopecia
-Varying degrees of hair ________ and/or hair ______ with/without scarring
-Generalized, patterned, or focal
-Non-scarring alopecia demonstrates ________ skin
-Scarring alopecia can demonstrate skin ____________ like erythema, scaling, and edema
Hair Pull Test
test for alopecia, where you pinch 50-60 hairs between thumb and forefinger with gentle traction while pulling up
-more than 6 hairs is abnormal result
medication, hair care, psychological, underlying
General Treatment for Alopecia
-Discontinue ___________, usually resolves most cases of telogen effluvium
-Traction alopecia, change ______ ______ practices
-Trichotillomania, often requires _____________ intervention
-Treat _________ medical condition if indicated
Minoxidil, finasteride, pregnancy
Treatment of Androgenic Alopecia
-Topical _________ 2% is the DOC, works in 60% of cases. Can cause skin irritation
-Oral __________ 1 mg/day, contraindicated in __________ and has an increased risk of prostate cancer
-Spironolactone is an alternative, as is Ketoconazole
corticosteroids, systemic, transplant
Treatment for Alopecia Areata
-No FDA approved treatment
-Intralesional ___________ have been shown to have good results
-_________ glucocorticosteroids, prescribe only if you would have to inject a lot of the intralesional corticosteroids
-Hair ________, wigs, hair pieces, skin grafts, laser therapy, and plasma therapy are other treatment options

T. Rubrum
Dermatophytes are the most common cause of onychomycosis, and _.________ is the leading causative agent
Onychomycosis
fungal nail infection
-toenails are more commonly affected
-can also be due to yeasts and non-dermatophyte molds
-more common in elderly males

age, pedis, diabetes, smoking, trauma
Risk Factors of Onychomycosis
-Older ____
-Tinea ______
-Occlusive footwear
-Cancer/_________/psoriasis
-Peripheral vascular disease
-Cohabitation with others with onychomycosis
-Immunodeficiency
-___________
-History of nail ________
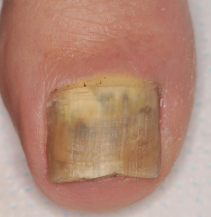
thickened, destruction
Clinical Manifestations of Onychomycosis
-Nail is opaque, _________, discolored and/or cracked
-Subungual hyperkeratinization
-Nail plate ___________
lateral, spots, proximal
Clinical Manifestations of Onychomycosis Due to Dermatophytes
-Distal _______, most common
-Superficial white, hallux preferentially affected with white _____ on nail plate
-Proximal, begins are _______ part of nail plate

hands
Clinical Manifestations of Onychomycosis Due to Candida Infection
-Affects the _______, especially the dominant hand
-About 70% of cases involve the middle finger

KOH, PAS, culture
Diagnosis of Onychomycosis
-Confirmation of fungal infection is essential, this cannot be a clinical diagnosis
-___ prep: only 30-60% sensitive, rapid
-Periodic acid-Schiff test (___): go-to test for onychomycosis, most sensitive, rapid
-Fungal _______: very specific, not sensitive, time consuming. Identifies causative organism
cellulitis, DM, infected, immunosuppressed
Provide treatment for onychomycosis in the following patients:
-Patients with history of ________ of the lower extremity or who have ipsilateral toenail onychomycosis
-Patients with __ with additional risk factors for developing cellulitis
-Patients with discomfort/pain with _________ nails
-______________ patients, like HIV/AIDS
-Patients who desire treatment
systemic, Terbinafine, topical, Ciclopirox, surgical
Treatment of Onychomycosis
First Line
__________ antifungals (most effective)
DOC is _________ 250 mg QD (6 weeks for fingernails, 12 weeks for toenails)
Itraconazole is another potential treatment
Second Line
_________ antifungals
__________ 8% nail lacquer, Efinaconazole, amorolfine, tavaborole
Alternative Treatments
Laser therapy, photodynamic therapy, _______ nail removal
Onycholysis
distal or distal-lateral separation of the nail plate from underlying nail bed and/or lateral supporting structures
-predisposing condition for secondary subungual infections from dermatophytes, yeast, or bacteria

underlying, dry, cold, trimmed
Management of Onycholysis
-Treat __________ condition
-Nail care measures: avoid trauma, avoid contact irritants, keep nails _____, avoiding nail cosmetics, protect hands from _____/windy weather, keep nails ______ short
Paronychia
superficial inflammation of the lateral and posterior nail folds surrounding the fingernails or toenails
-acute is less than 6 weeks, typically bacterial infection (Staph Aureus)
-chronic is longer than 6 weeks or recurrent episodes (candida)
-usually involves one finger

Staph Aureus and Strep Pyogenes
What are the most common causative organisms or paronychia?
trauma, manicured, sucking, water, diabetes
Risk Factors of Paronychia
Acute: direct or indirect ______ to cuticle or nail fold, _________ or sculptured nails, nail biting, thumb _________
Direct: frequent immersion of hands in ______, _________, immunosuppression, and medications
trauma, exposure, short, control
Prevention of Paronychia
-Avoid _______ such as nail biting or manipulating nail folds
-Avoid __________ to allergens and contact irritants
-Keep nails ______, avoid manicures, apply moisturizer after washing hands
-Glycemic _______ in patients with diabetes mellitus
painful, red, cuticle, swollen, Beau, elevation, drainage, Felon
Clinical Manifestations of Paronychia
-Acute: ________, ___, warm, swollen area around the proximal/lateral nail folds at the _______. +/- abscess
-Chronic: initially appears as ________ tender, boggy nail fold +/- abscess. Later appears as a retracted nail fold, thickened nail plate with _____ lines and discoloration
-Occasional _________ of nail bed or separation of nail fold from nail plate
-Purulent __________ or material at the nail margin
-If left untreated, it can progress to _______

severe, recurrent, MRSA, KOH, culture
Diagnosis of Paronychia
Testing is indicated in _______ infections, ________ infections or if ______ is suspected:
-Gram stain
-Culture and sensitivity
-___ prep
-Ultrasound
-Biopsy
-Viral ________

mild, soaks, Mupirocin, moderate, Cephalexin, MRSA, steroids
Treatment for Paronychia
_____ infection without abscess
-Warm water/antiseptic _____
-Topical antibiotics: _________, Bacitracin to cover MRSA
-+/- topical steroid
Mild Infection without abscess (not responding to treatment) / _______ infection
-_________ 500 mg QID
-Dicloxacillin 250-500 mg QID x 5-7 days
-Amoxicillin Clavulanate if the patient bites their nails
______ Infection
-Bactrim, Clindamycin, Doxycycline
Chronic
-Topical high potency _______, like betamethasone 0.05%

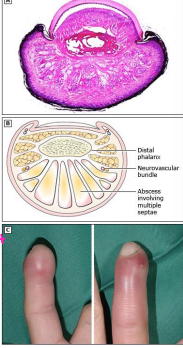
Felon
abscess and infection of the fingertip pulp space
-S. Aureus is the most common organism
-most commonly occurs after penetrating skin trauma
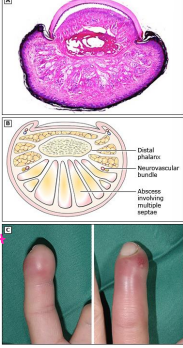
fingertip pad, I&D, Cephalexin
Physical Exam Findings and Treatment of Felon
-Pain, erythema, swelling, and fluctuance to the ________ ___
-_&_ procedure, oral antibiotics (_________ 500 mg QID)
hyperpigmentation, hyper functional, melanin, women, sunlight, hormonal
Epidemiology, Pathophysiology, and Risk Factors for Melasma
-Common, chronic, and recurring disorder of ____________ of skin
-Arises from _____ __________ melanocytes that deposit excessive amounts of ________ in the epidermis and dermis
-Usually _________ of reproductive age are most often affected, late 20s - early 30s
-Risk Factors: genetic predisposition, exposure to ________, skin phototype, and _________ factors (pregnancy, oral contraceptives, hormone therapy)
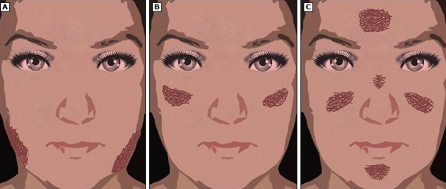
macules, patches, symmetric, centrofacial, cheek, jawline
Clinical Manifestations of Melasma
-Irregular, light-brown to gray-brown _________ and ________ on sun exposed skin
-Lesions are usually __________ and may affect face and neck, spare the lips/ears/periorbital skin
-____________: affects the forehead, cheeks, nose, upper lip, and chin
-Malar: involves lateral _______ areas
-Mandibular: affects lower __________
clinical, Woods, histology
Diagnosing Melasma
-Usually based on ________ presentation
-_______ lamp may assist in identifying the location of pigment
-Dermascopy could aid in diagnoses and identify levels of pigment deposition
-__________ testing causes increased melanin deposition in all layers of the epidermis

standard, photoprotection, Hydroquinone, combination
Melasma Treatment
-No _________ therapy, tough to treat due to recurrence rate
-Therapies that target photo-damage, inflammation, aberrant vascularity, and abnormal pigmentation provide best outcomes
-_____________ is key: avoid the sun, wear UV protection
-Mild melasma can be treated with _____________ 4% cream or BID x 2-4 months
-Moderate to Severe melasma can be treated with triple _________ cream, flucinolone acetonide + hydroquinone + tretinoin

pigmentation, macules, depigmentation, melanocytes
Epidemiology, Etiology, and Pathogenesis of Vitiligo
-Common acquired disorder of ___________
-Characterized by development of well-defined white ________ on the skin
-Most frequent cause of ___________, worldwide prevalence of 0.5-1%
-Males and females are equally affected
-Autoimmune destruction of __________ → skin depigmentation
Vitiligo
asymptomatic depigmented macules and patches, milk or chalk white in color that lack clinical signs of inflammation
-lesions appear anywhere on the body, varying in size from a few mm to many cm
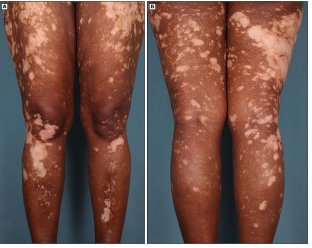
clinical, corticosteroids, re-pigmentation
Diagnosis, Treatment, and Prognosis of Vitiligo
Diagnosis
-Usually based on _______ appearance
-Woods lamp
-Histology evaluation
Treatment
-Based on disease severity, disease activity, patient preference, response evaluation
-Phototherapy + topical or oral ____________, Calcineurin inhibitors, vitamin D analogues
Prognosis
-Highly unpredictable course
-Most patients experience alternating periods of pigment loss and disease stability their entire life
-Occasionally some patients experience spontaneous __-___________