GI L1
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
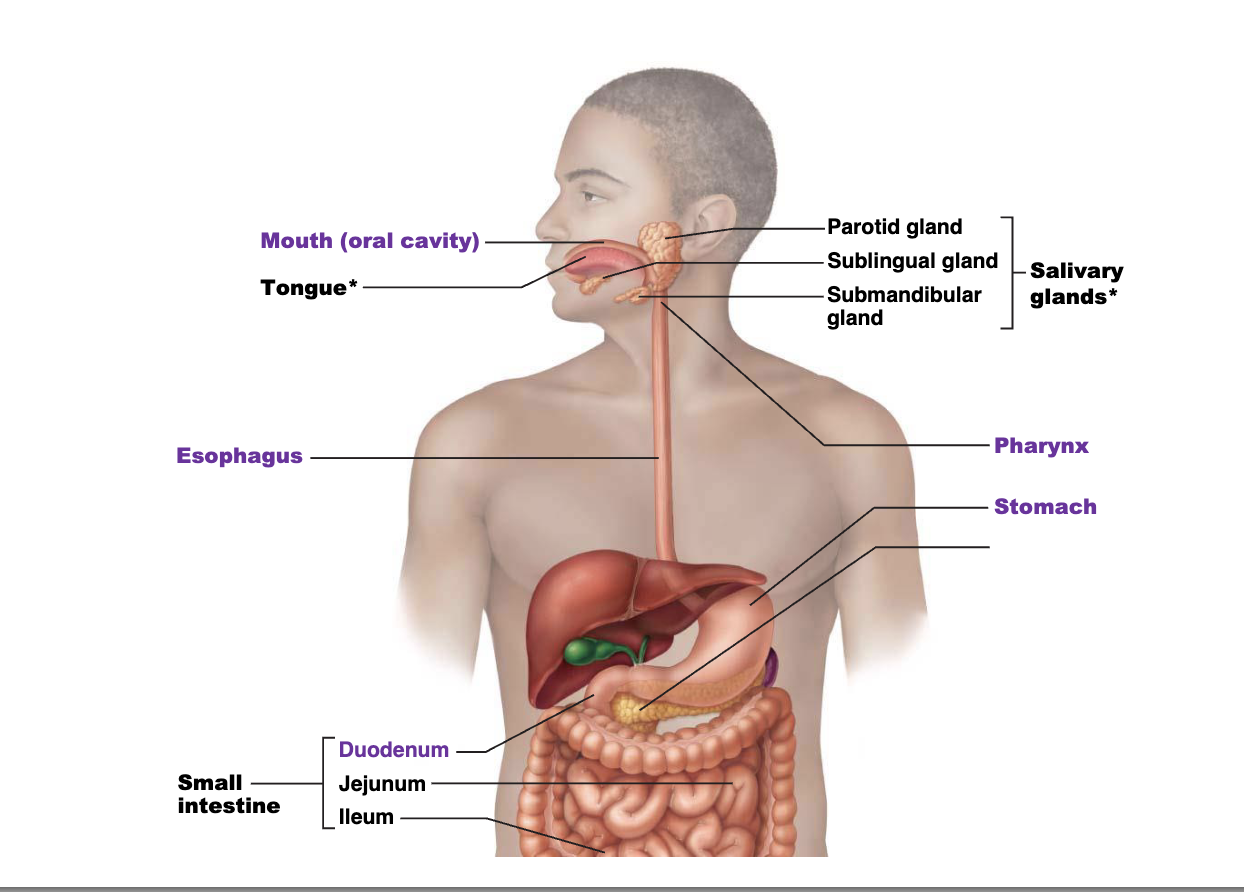
Name the main structures of the upper gi (mouth to small intestine)
Functions of the oral cavity
1. Ingestion
2. Mechanical breakdown
3. Propulsion
4. Digestion
5. Absorption
6. Elimination (defecation)
Where is the oral cavity
oral vestibule- The recess bounded externally by the lips and internally by the teeth is the
The oral cavity proper is behind the teeth
The hard palate sits anteriorly while the soft palate is posterior
What is the function of the tongue
The tongue moves food while chewing and forms a bolus for swallowing
Taste is an important special sense that tells us if something is safe to eat
10000 taste buds on the tongue and a few more on the soft palate, cheeks and back of mouth
Each of the many fungiform papillae have 1-5 taste buds
The few valate papillae have many taste buds
The Foliate papilla have many taste buds during childhood but fewer with age
what is the tongue covered in
The tongue is covered in papillae
Filiform- provide grip, smallest, most numerous
Fungiform- contains taste receptors,intermediate size
Valate- Form a row at back of tongue (8-12 of them- contains taste receptors
Foliate- ridge like folds on side of tongue- contains taste receptors
Desribe tonsils
Tissues for immune surveillance (Lymphatic tissue)
Patches of lymphatic tissue found at the entrance of the pharynx
Protection against ingested and inhaled pathogens
what are the different types of tonsils
•NOSE- Pharyngeal tonsils are in the posterior wall of the nasopharynx (adenoids)
• Palatine tonsils are in the posterolateral region of the oral cavity
• Lingual tonsils are along the posterior one third of the tongue
What are the 6 functions of the salivary glands
Three groups of glands secrete saliva which has 6 key functions
1. Cleanses the mouth (protects the teeth)
2. Dissolves food chemical so they can be tasted
3. Moistens food and helps compact it to a bolus
4. Provides lubrication to protect the mouth/esophagus
5. Contains amylase and lipase to begin digesting carbohydrates and fats
6. Secretes proteins that help digest nutrients (transcobalamin- helps
B12 absorption)
What are the Salivary Glands?
Parotid gland largest salivary gland, secretes into the vestibule near second molar tooth
Submandibular gland runs below the mucosa of the oral cavity and opens at base of lingual frenulum
Sublingual gland Smallest gland, lies anterior to submandibular gland, and opens via 10-20 ducts beneath tongue
what is posterior to the oral cavity
the pharynx, which connects the oral cavity to the esophagus and larynx.
Common passage way for food and air.
what are the three parts of the pharynx
1. Nasopharynx
2. Oropharynx
3. Laryngopharynx
where and what is the function of the epiglottis
The epiglottis projects into the pharynx to protect the larynx from food entering and causing suffocation
When you swallow, the larynx moves up against the epiglottis to close the “wind pipe”
what is the passage of food after swallowed
Propulsion
Once swallowed, food passes into the esophagus which
contracts to move food into the stomach
It passes through the diaphragm (esophageal hiatus)-
Hiatus hernia is when stomach bulges through this opening.
Pharyngo-esophageal (upper) sphincter
prevents air from entering the oesophagus
whats a common Oesophageal disorder
Gastroesophageal (lower) sphincter prevents reflux of stomach content
Weak sphincter - Gastroesophageal Reflux Disease (GERD) leads to erosive oesophagitis - Barrett’s oeosphagus)
• Heartburn – a burning sensation caused by acid reflux
Name and explain the 5 stages of swallowing
Buccal phase: The upper esophageal sphincter is contracted (closed). The tongue presses against the hard palate, forcing the food bolus into the oropharynx
Pharyngeal-esophageal phase begins: the tongue blocks the mouth, the soft palate and its uvula rise, closing off the nasopharynx, the larynx rises so that the epiglottis blocks the trachea, the upper esophageal sphincter relaxes; food enters the esophagus
Pharyngeal-esophageal phase continues (3-5): the constructir muscles of the pharynx contract, forcing food into the esophagus inferiorly, the uper esophageal sphicter contracts after food enters
Peristalsis moves doof through the esophagus to the stomach
The gastroesophageal sphincter surrounding the cardial orifices opens. after food enters the stomach the sphicter closes preventing regurgitation.
what is condition called for difficulty swallowing
dysphagia- common in hospitalised patients, common following stroke and in patients with neurological disorders (major reason for nill by mouth or NPO)
what are the 3 functional departments of the stomach
1. Fundus – dome-shaped region beneath the diaphragm
Cardiac region
• 2. Body (oxyntic mucosa) – mid-portion of the stomach
many gastric glands
• 3. Antrum – the lower part
terminates at the pyloric sphincter (continues into the duodenum)
Characteristic of the stomach
Stomach – a muscular chamber, inferior to the diaphragm.
• The stomach temporarily stores food and begins protein digestion
• The stomach chemically digests food with acid and enzymes while mechanically digesting food be mixing and compressing food→ chyme
• An empty stomach has a volume of about 50 mls but it can be filled with food to hold about 4 liters of food.
When collapsed the mucosa form deep folds known as rugae.
• When full secretes hormones to tell the brain to stop eating
• Weight loss surgery used this fact to its advantage (details to come)
• Specialized cells secrete a range of important factors
what is hiatal hernia
• Hiatal hernia occurs when the cardiac sphincter is weakened and parts of the stomach herniate through
• Can lead to GERD or heartburn
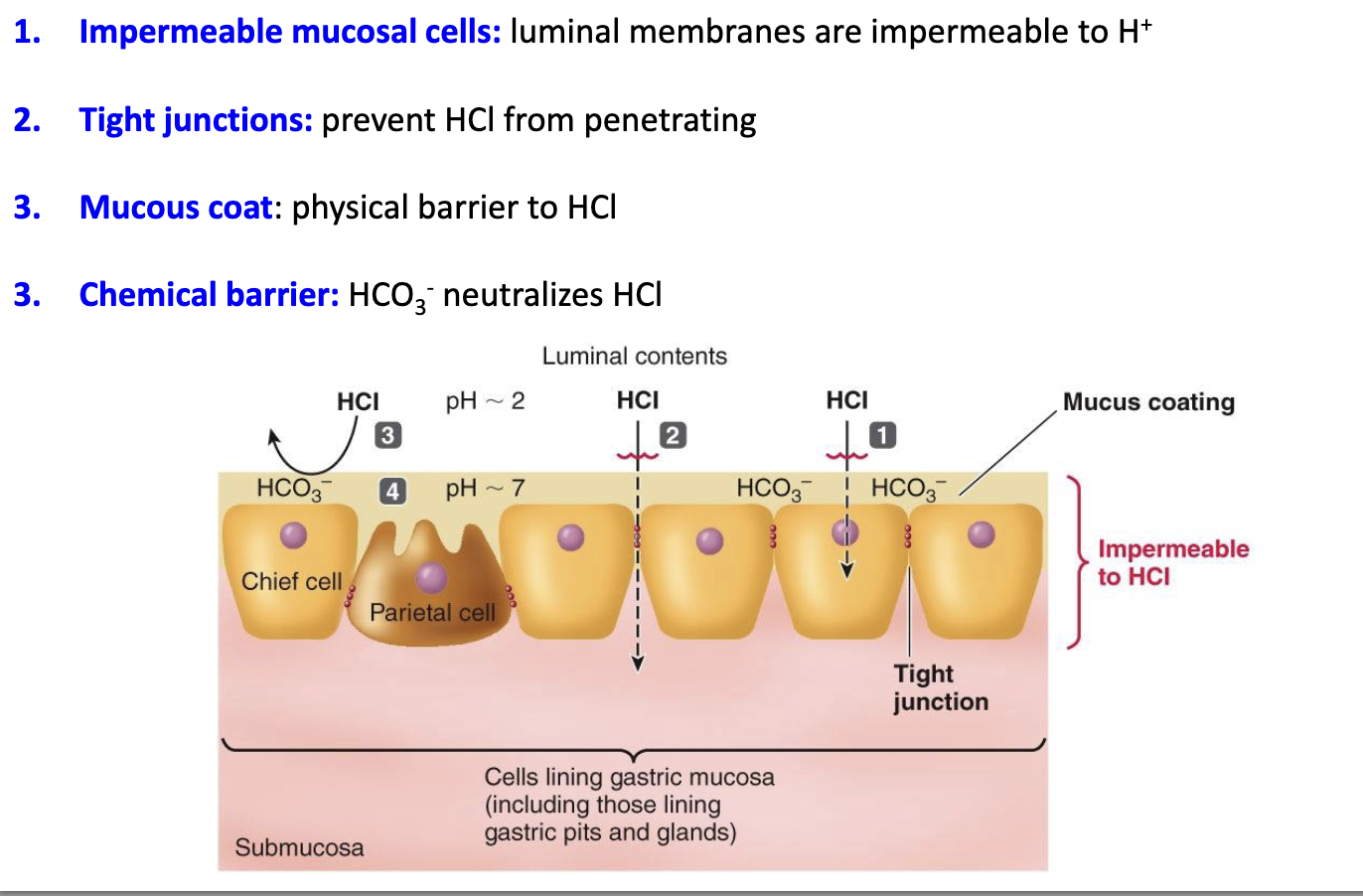
what are the 3 Exocrine cells found in the gastric pits and gastric glands of the stomach
Exocrine cells: release substances into the lumen of the stomach (local action)
Mucous cells (at the surface epithelium and mucous neck):
Secrete mucus
Function: Protect the stomach lining from acid and digestive enzymes
Chief cells (located deeper in the gland):
Secrete pepsinogen (inactive enzyme) and gastric lipase
Pepsinogen is converted into pepsin, a protease, in acidic pH
Gastric lipase helps digest fats
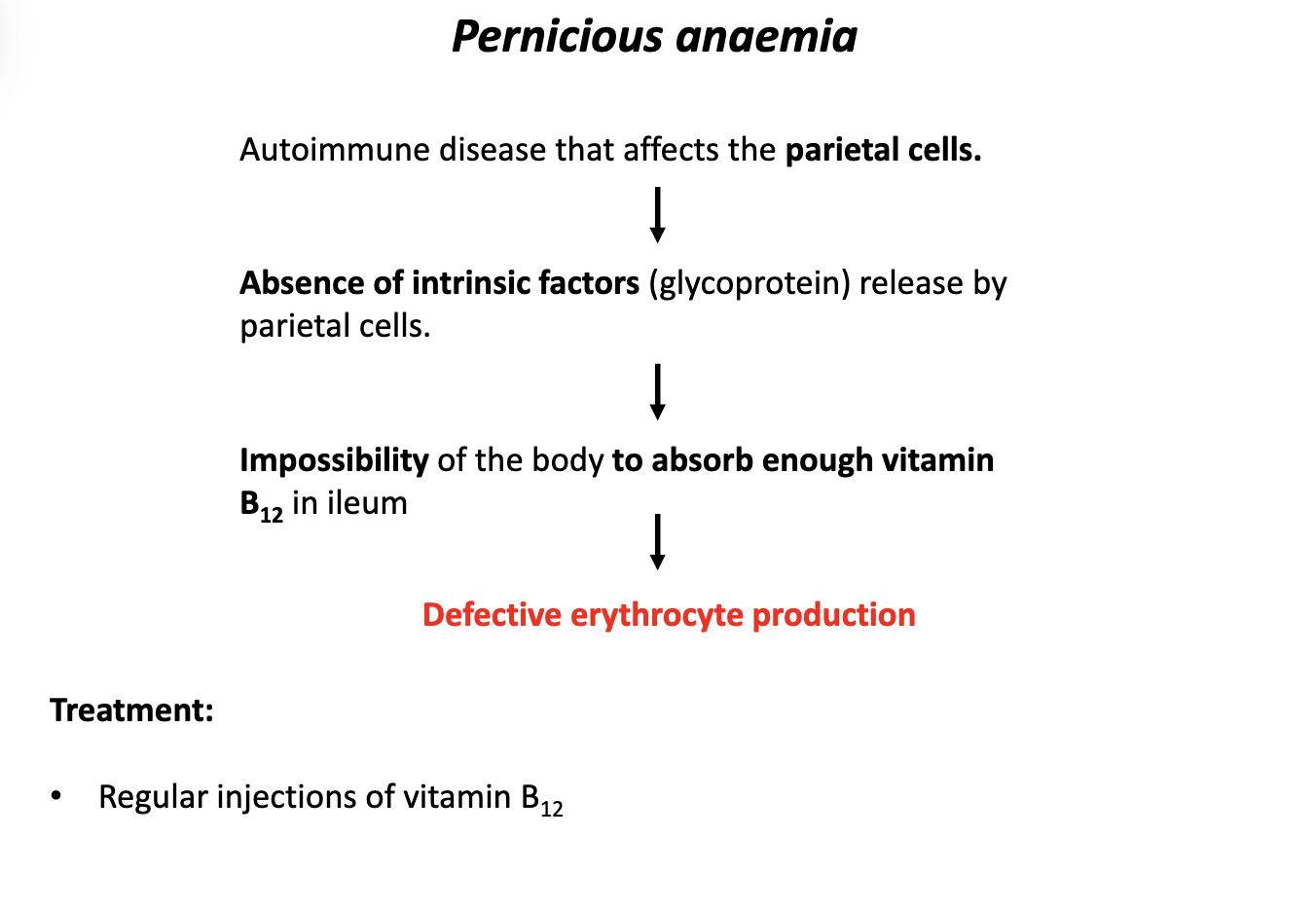
Parietal cells (located in the middle region of the gland):
Secrete hydrochloric acid (HCl) and intrinsic factor
HCl lowers stomach pH (for enzyme activation and pathogen defense)
Intrinsic factor is needed to absorb vitamin B₁₂ in the small intestine
Stem cells:
Responsible for regenerating all the cell types of the gastric lining
what are the 3 Endocrine cells found in the gastric pits and gastric glands of the stomach
Endocrine/Paracrine cells: release hormones into the bloodstream or nearby cells (systemic or local regulatory functions)
These are enteroendocrine cells located at the base of the gastric glands. They secrete hormones into the blood or act locally to regulate stomach function:
Gastrin: Stimulates HCl production and gastric motility
Somatostatin: Inhibits gastrin release, thus reducing acid secretion
GLP-1 (Glucagon-like peptide 1): Enhances insulin secretion and slows gastric emptying
Ghrelin: Stimulates appetite (often called the “hunger hormone”)
what are the 3 main roles of secretion of stomach
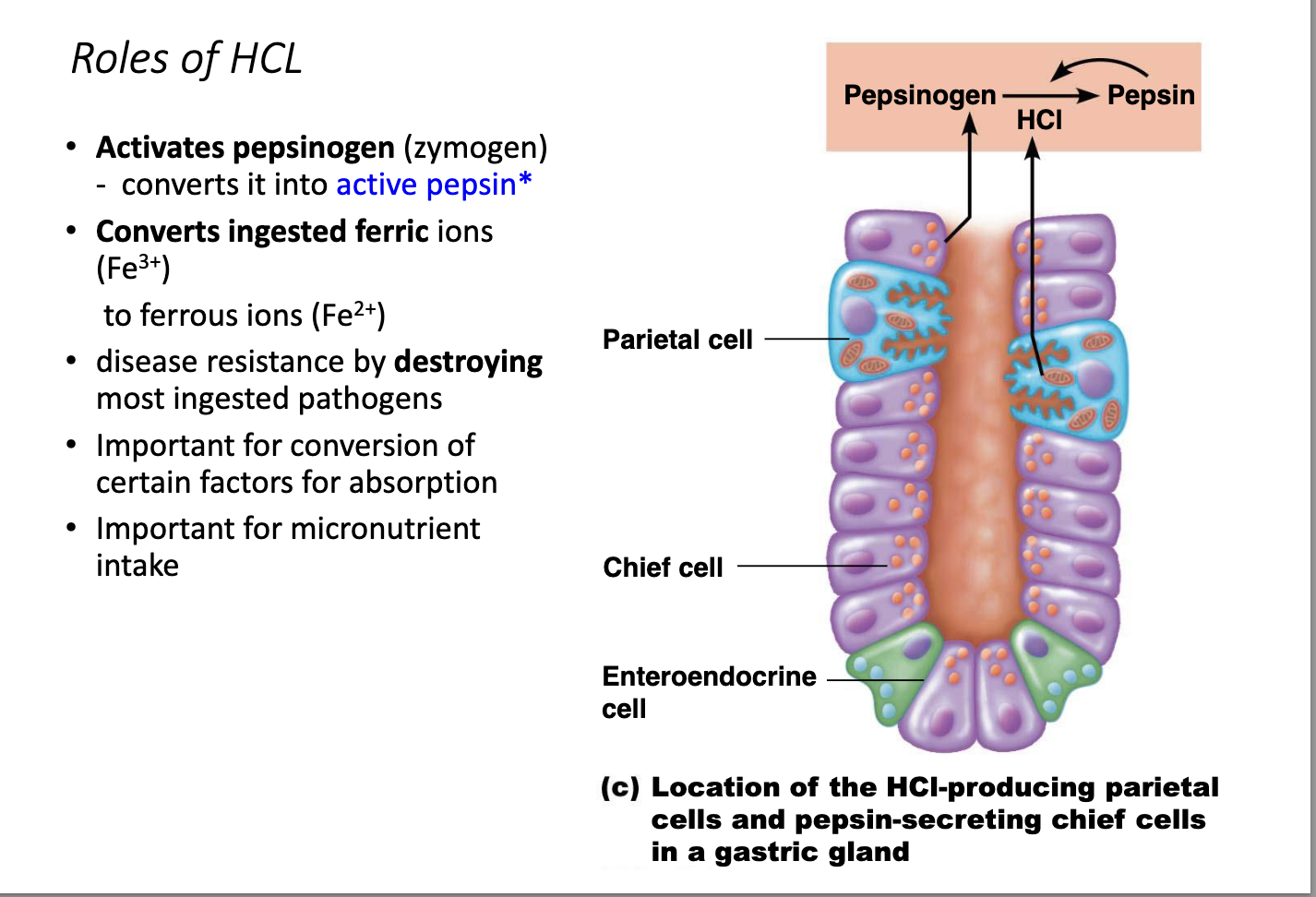
what is the role of HCL
what are the 3 phases of gastric secretion
Cephalic phase – sight and thought of food increase gastric juices.
Gastric phase – begins when food is in the stomach (especially proteins).
Lasts 3–4 hours and provides two-thirds of gastric juice released
Intestinal phase – factor that originates in the small intestine (duodenum).
what is the stomachs regulatory response to the stomach filling
Response of the stomach to filling
Stretches to accommodate incoming food until about 1.5 L of food is ingested.
No change in pressure occurs up to this point due to
When the stomach stretched beyond this capacity, it accelerates stomach motility and emptying
how is gastric contractile activity regulated
The Stomach contracts at a regular interval throughout the day at a rate of 3 contractions per minute.
This rate is set by the enteric pacemaker cells
The frequency of these contractions does not change but a
number of factors increase the force of the contraction
Distension→ stretch receptors→ increase force of contraction
Gastrin increase force of contraction
Therefore the more food in the stomach, the stronger the contractions
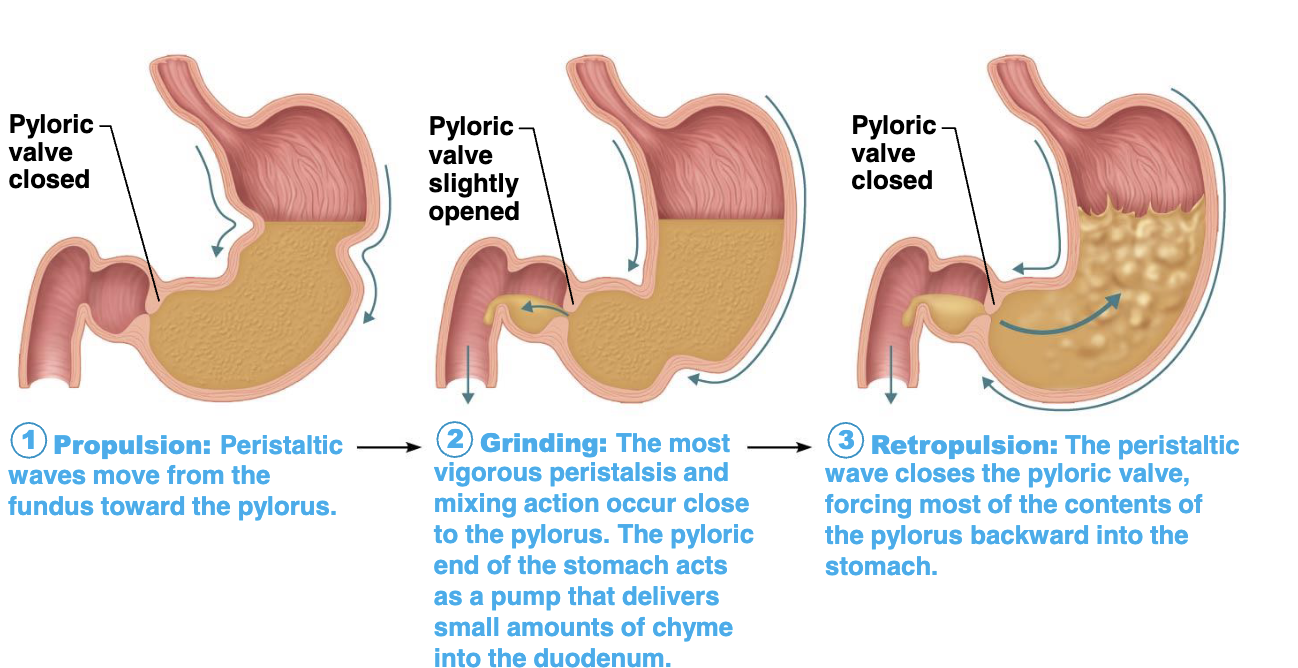
what are the 3 stages of Peristaltic waves of the stomach
Only about 3ml of liquid will normally enter duodenum per
contraction
what is the Regulation of gastric emptying
The stomach usually empties within 4 hours of eating a meal
If more liquid is present, then this will be faster while solids take longer
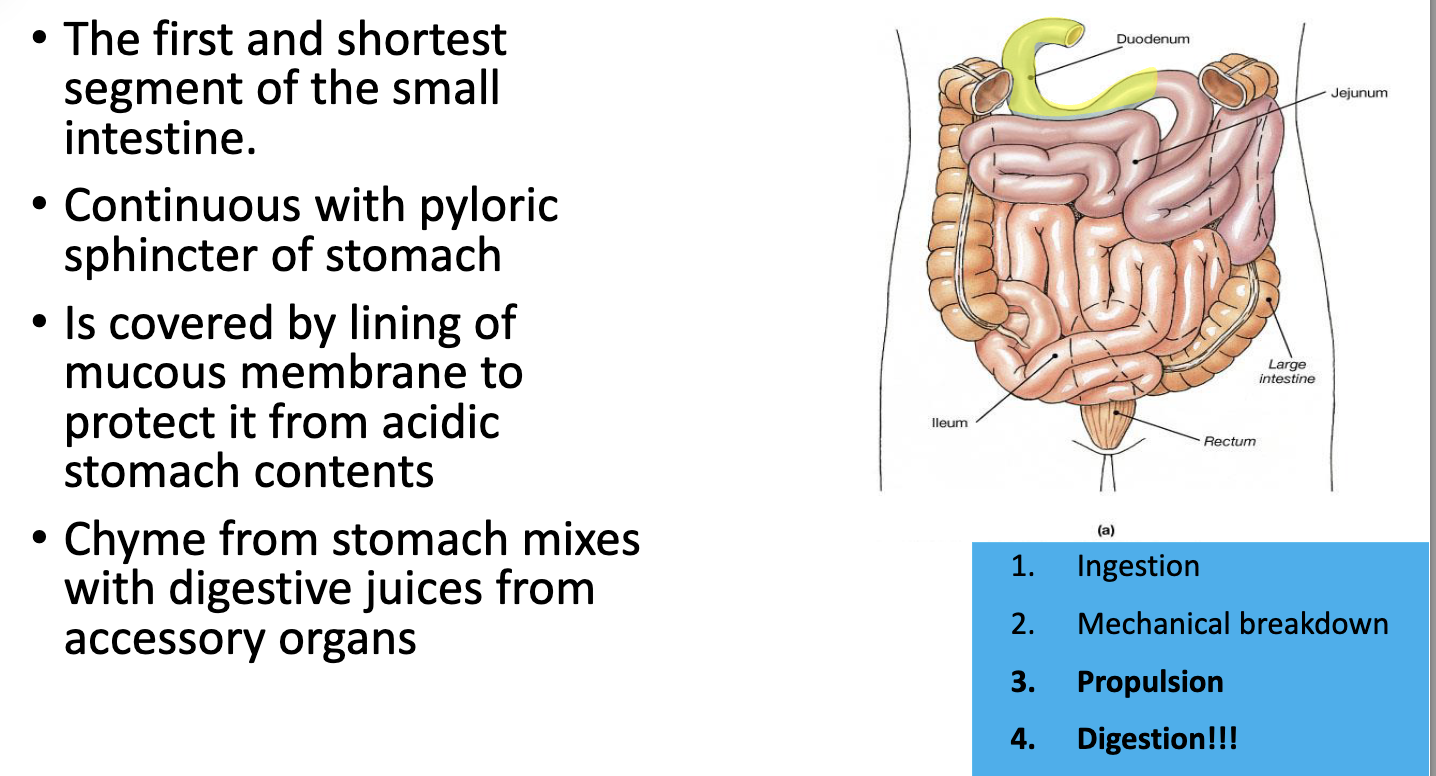
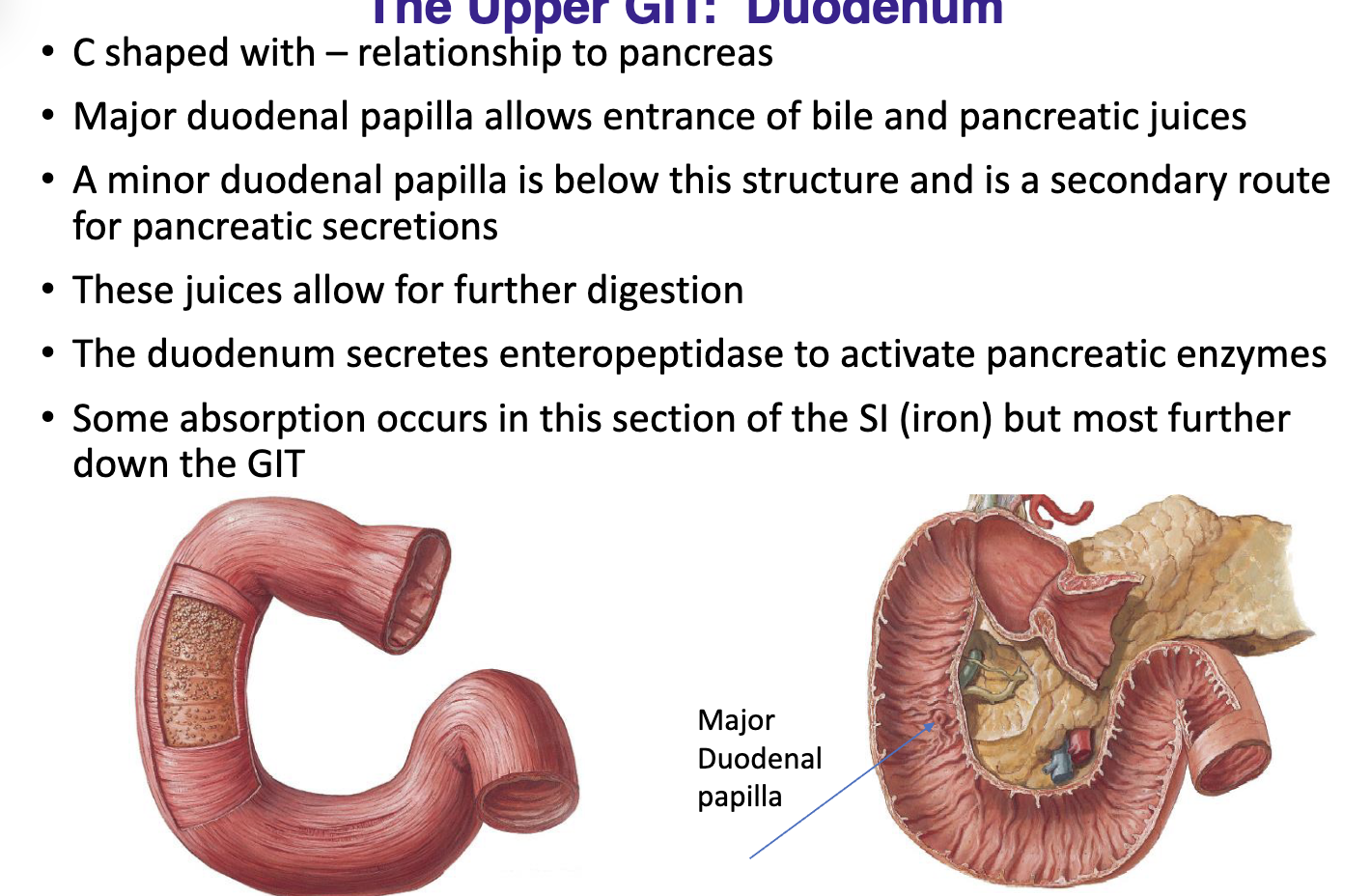
what is the purpose of the Duodenum
Duodenum can prevent overfilling of stomach by regulating how much fluid enters duodenum
Duodenal receptors respond to stretch enterogastrones (duodenal hormones) inhibit gastric secretion and duodenal filling
Carbohydrate-rich chyme moves quickly through duodenum but fatty foods take longer to clear the stomach (6 hours or more)
what is the dueodenum
What protects the stomach lining from acid?
how does the duodenum work
What is Pernicious anaemia and what is the treatment
what is Gastritis and what are treatments

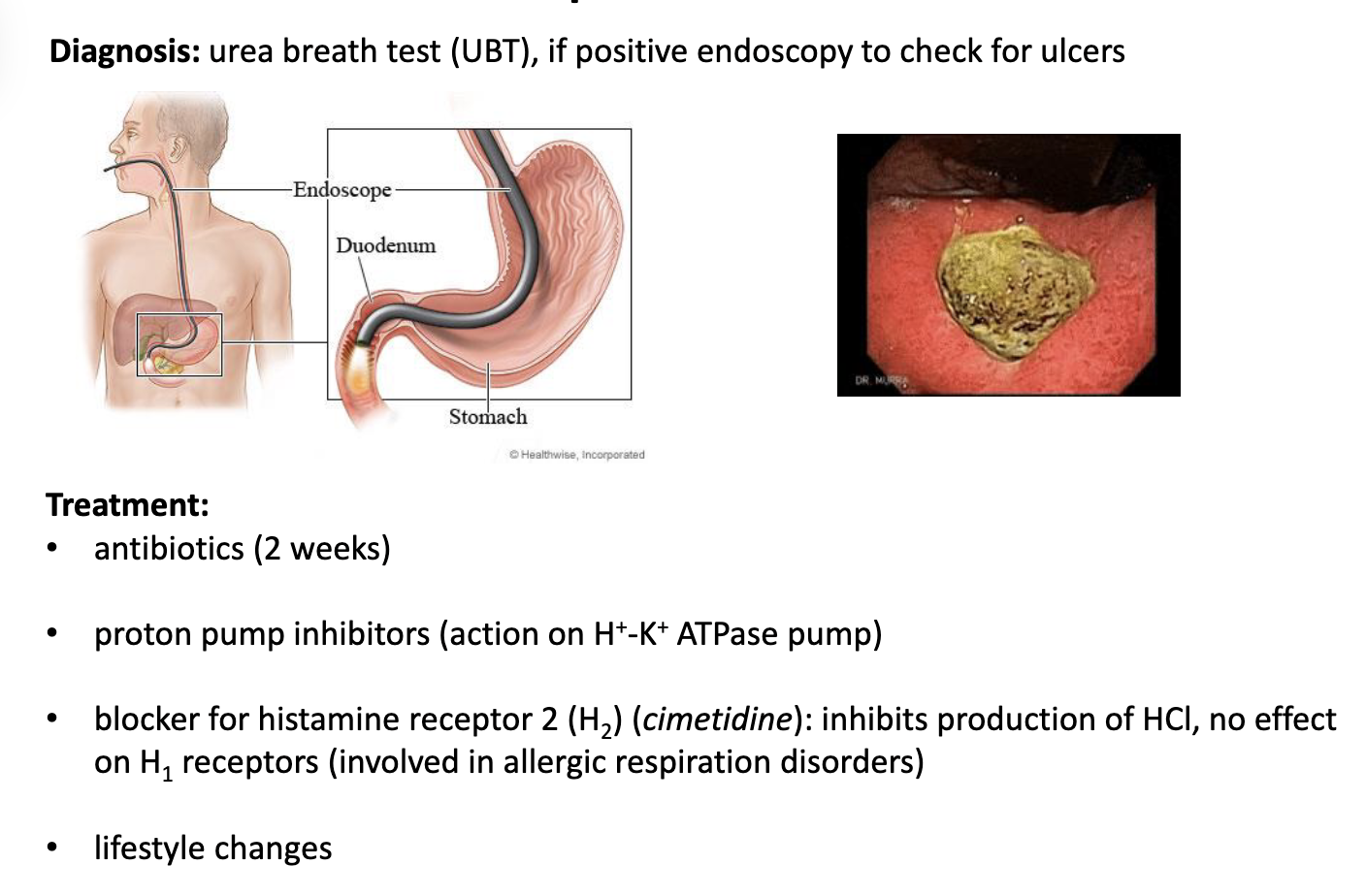
what is Peptic ulcers and what are treatments
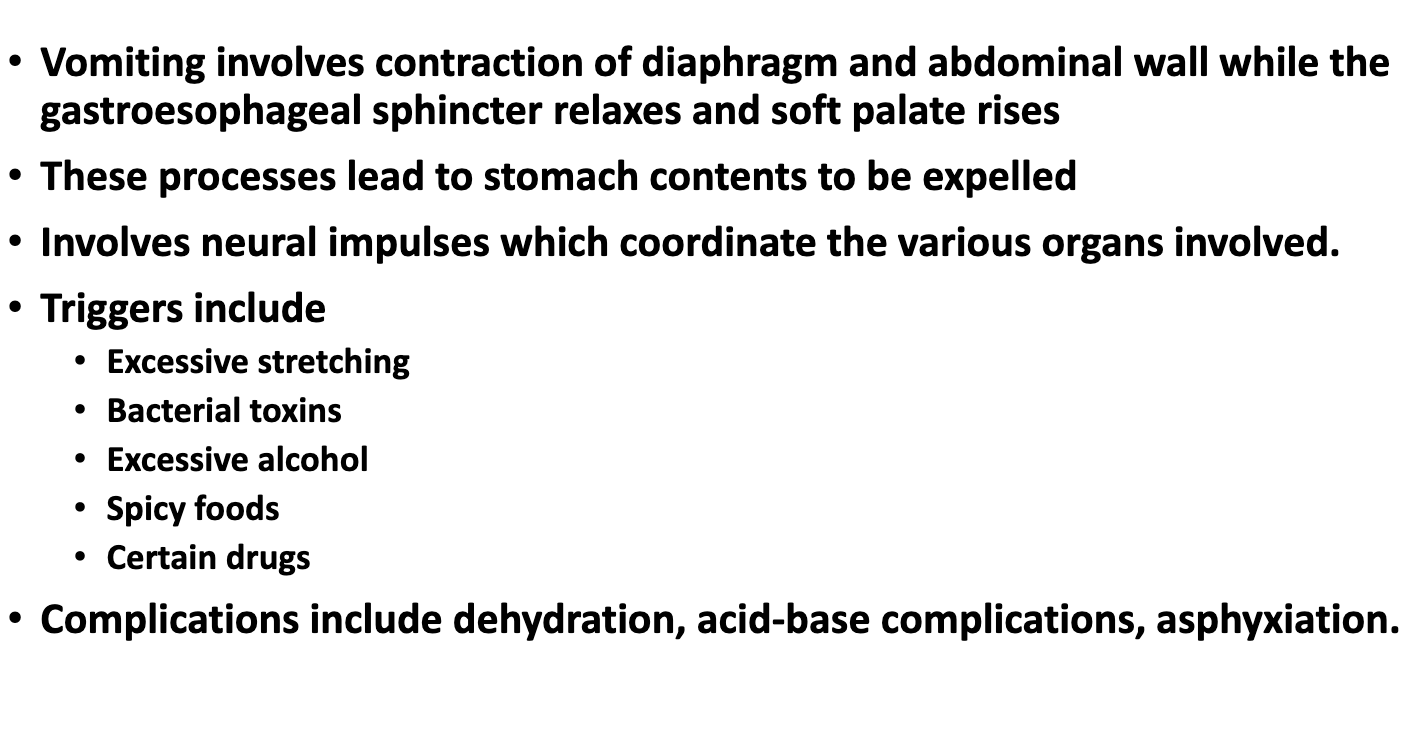
What is EMESIS and what is the treatment