Embryology 2 | Weeks 1 and 2 of Development
1/18
Earn XP
Description and Tags
https://youtu.be/g7FExgKr-x4
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
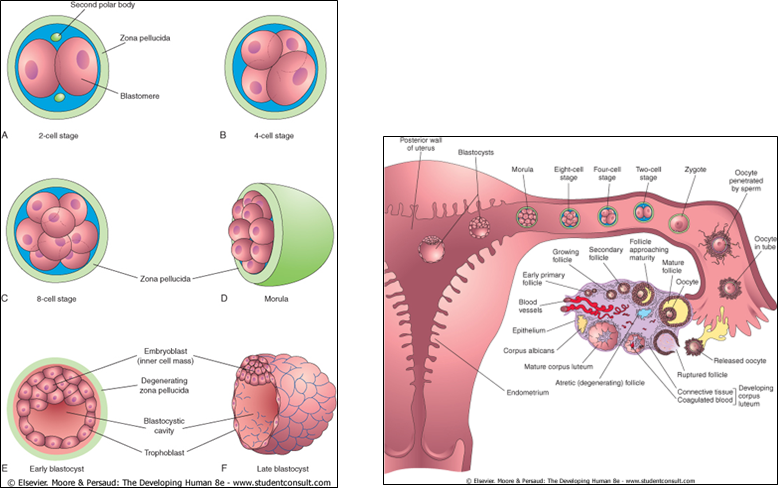
What is cleavage of the zygote?
A series of repeated cell divisions that occurs as the zygote travels down the oviduct.
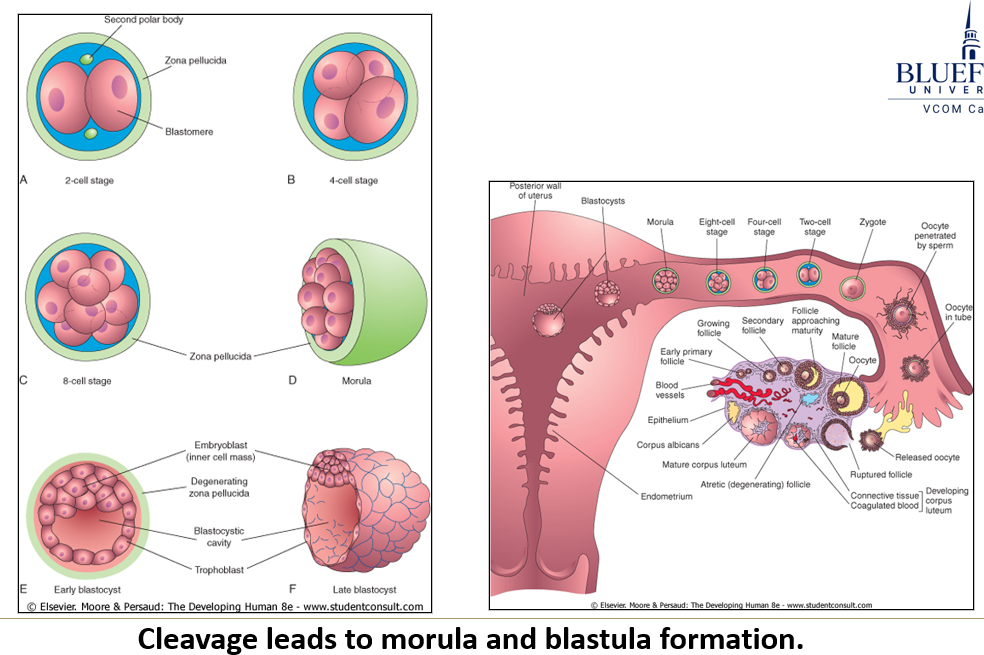
What are the resulting cells from cleavage of the zygote called, and what happens to them?
The resulting cells are called blastomeres, and they become progressively smaller since they don’t grow in size during interphase.
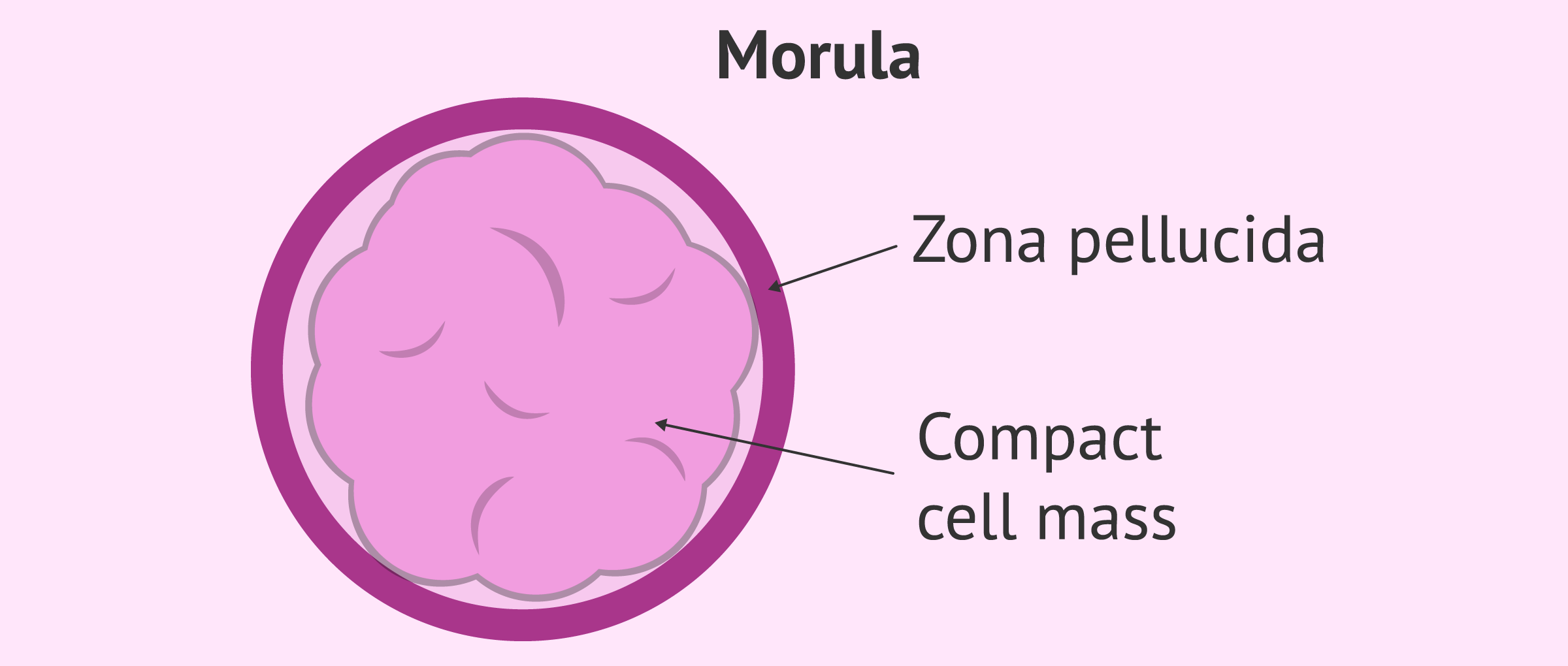
What is the morula?
The morula is a solid mass of 16–32 blastomeres, the typical stage that enters the uterus. It is still surrounded by the zona pellucida.
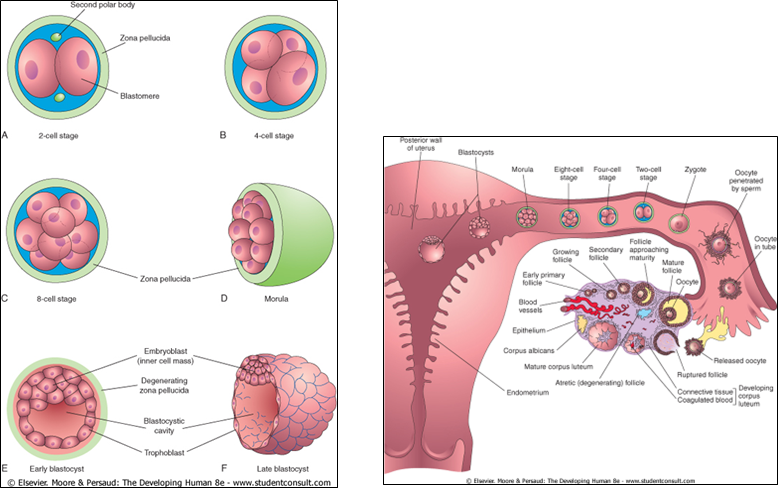
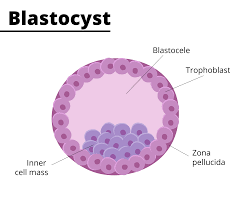
What is a blastocyst?
The blastocyst is a fluid-filled hollow structure with an inner cell mass (called the embryoblast) at one pole.
The outer layer of cells, the trophoblast, secretes early pregnancy factor - EPF, an immunosuppressant detectable in maternal blood within 24–48 hours, forming the basis for early pregnancy tests.
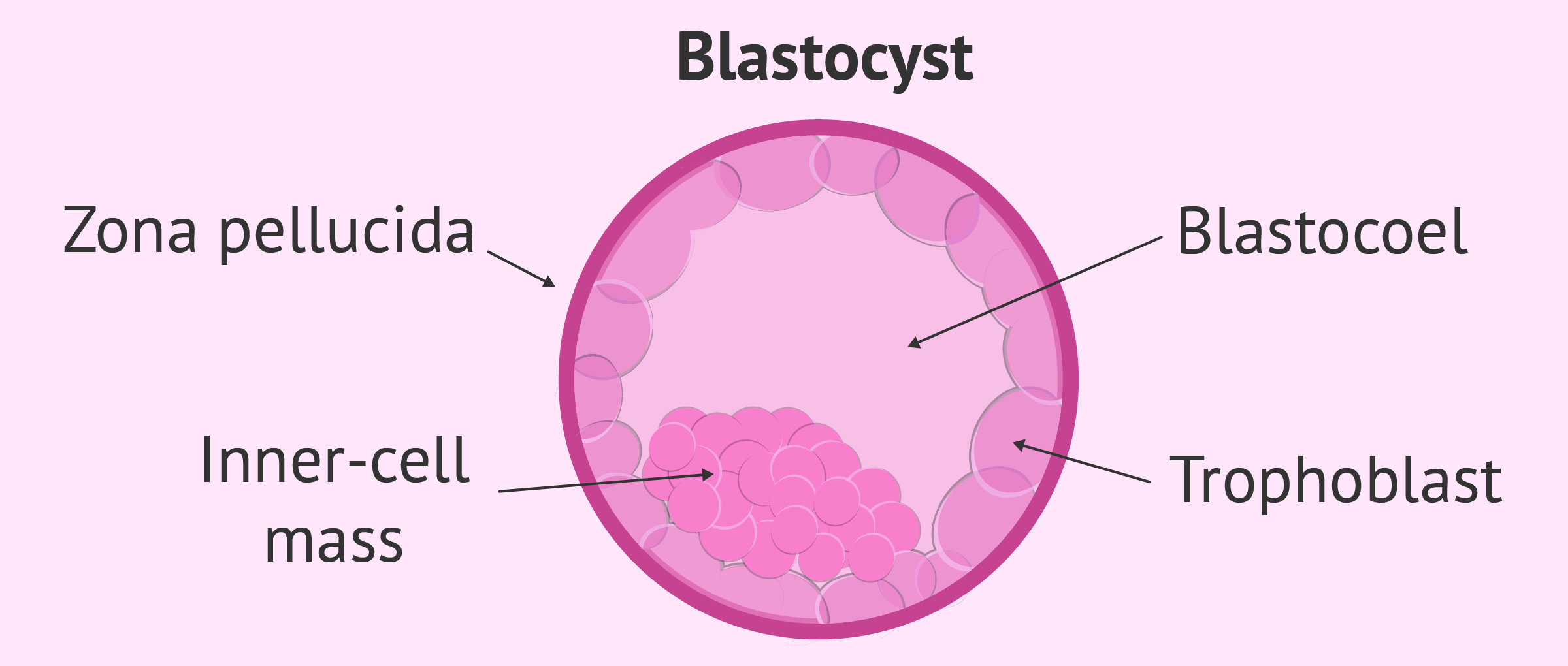
What happens to the zona pellucida in the late blastocyst stage?
The late blastocyst loses the zona pellucida.
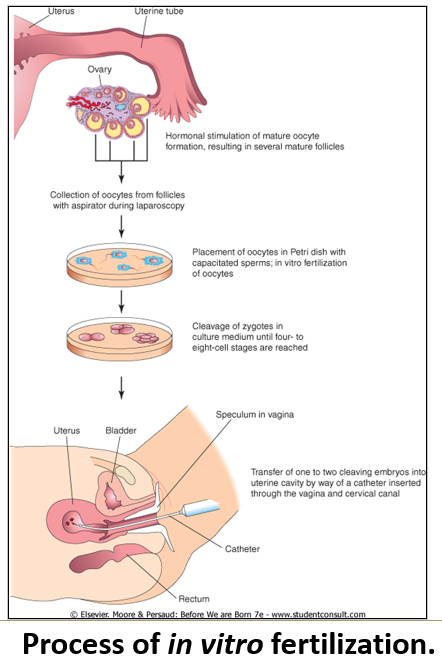
How is in vitro fertilization performed?
Hormonal stimulation triggers ovulation to capture multiple oocytes.
Fertilization and early cleavages occur in a petri dish. A single blastomere may be removed for genetic testing.
The embryo is placed into the uterus at the 4–8 cell stage, and two embryos are often used to increase the chances of implantation.
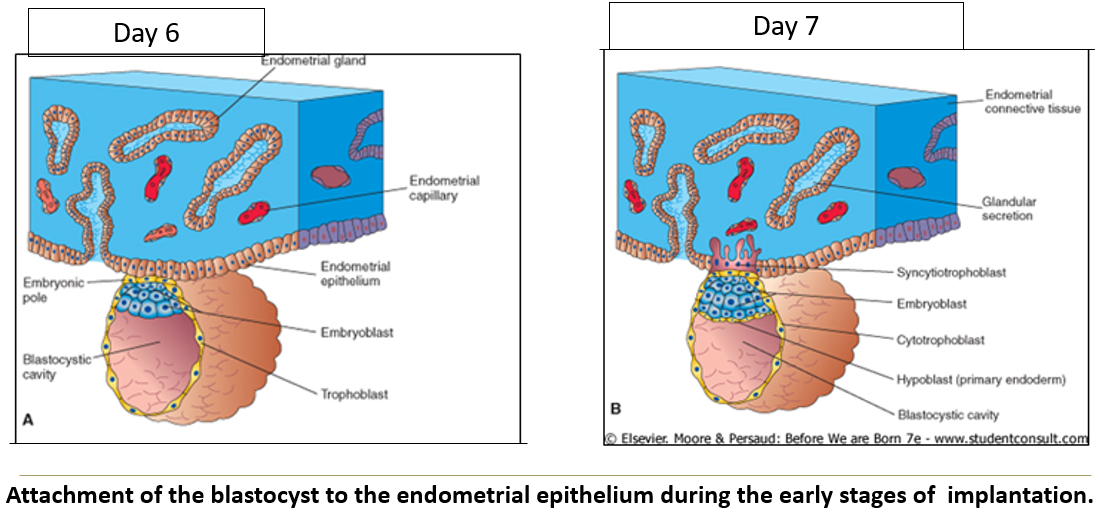
What is implantation?
The attachment and burrowing of the blastocyst into the uterine lining, taking about 2 weeks.
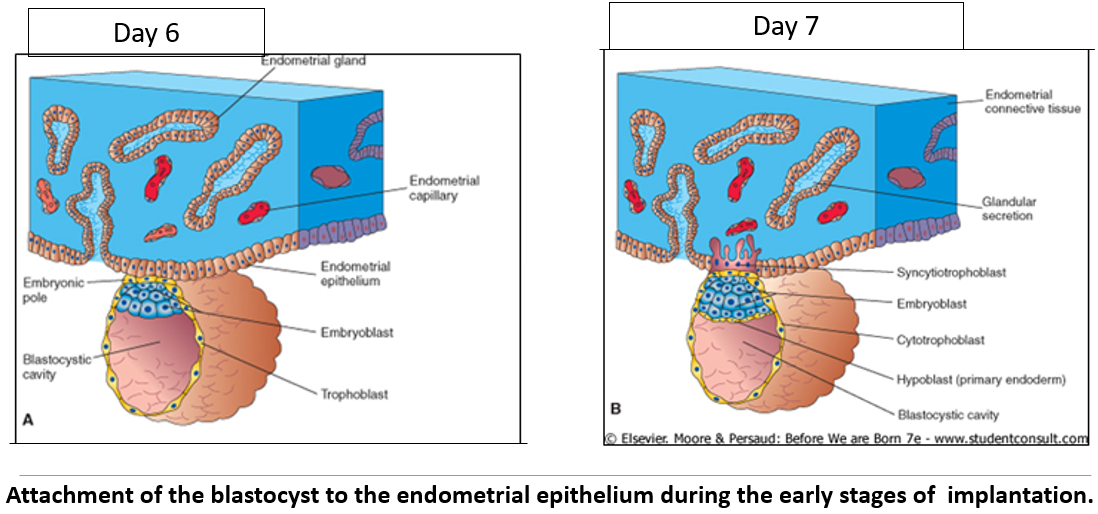
What does the trophoblast differentiate into, and what does it do?
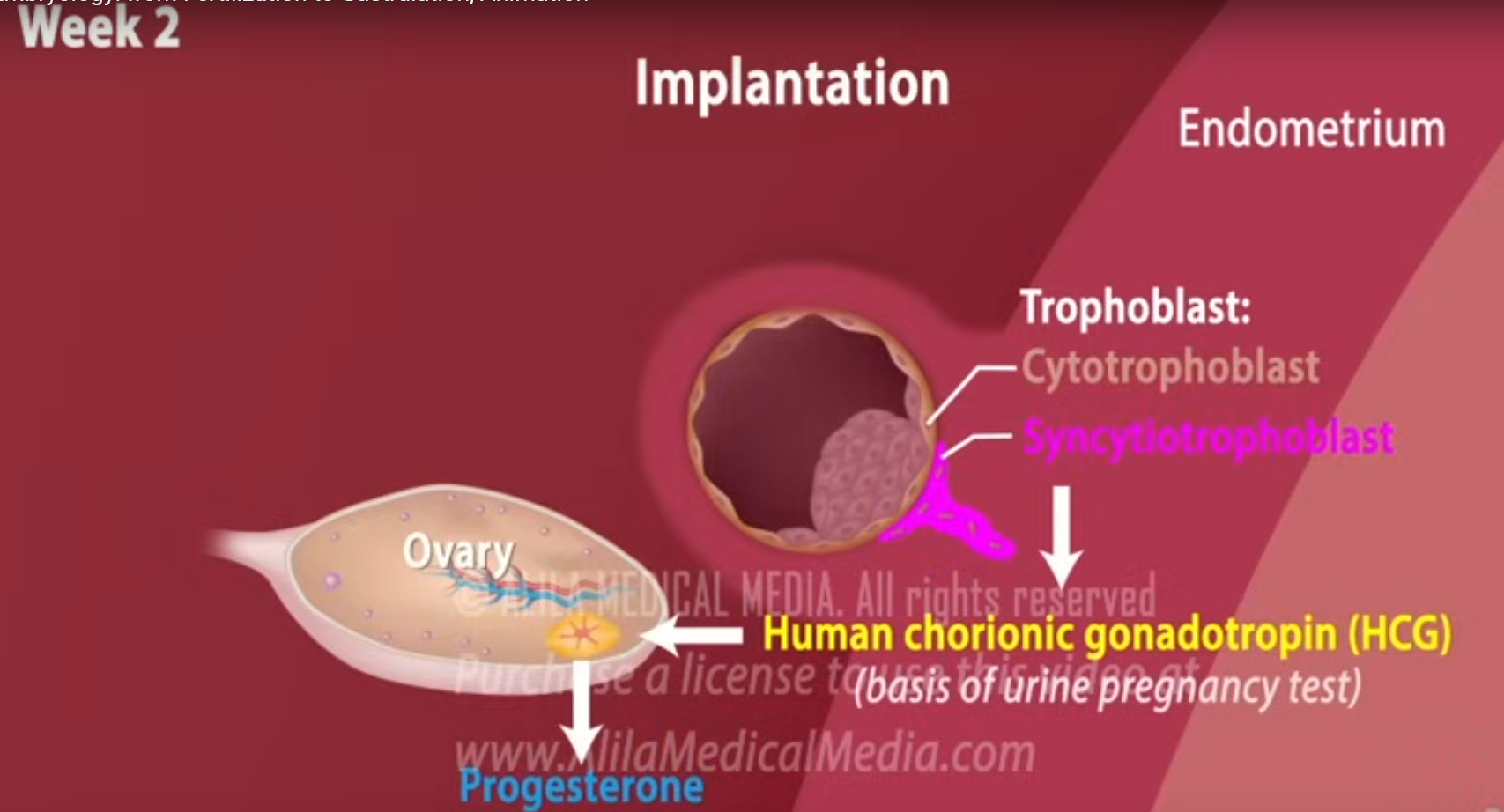
The trophoblast becomes the syncytiotrophoblast, the outer layer of cells in the placenta that that burrows into the uterus to help the embryo implant and enables the exchange of nutrients, gases, and waste between mother and baby.
It produces hCG to maintain progesterone secretion by stimulating the corpus luteum.
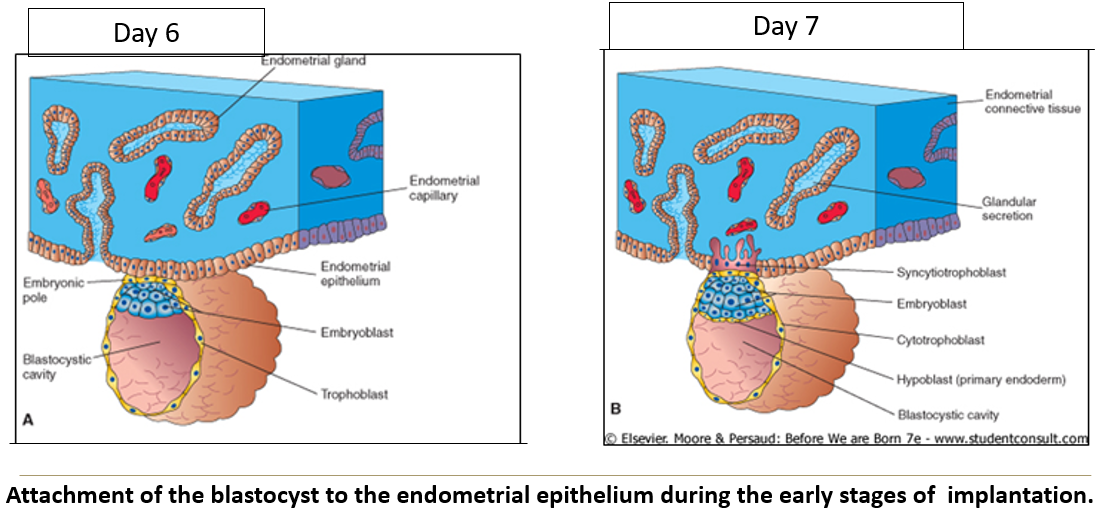
What hormone does the syncytiotrophoblast produce and when?
It produces human chorionic gonadotropin - hCG by the end of week 2, which is used in pregnancy tests.
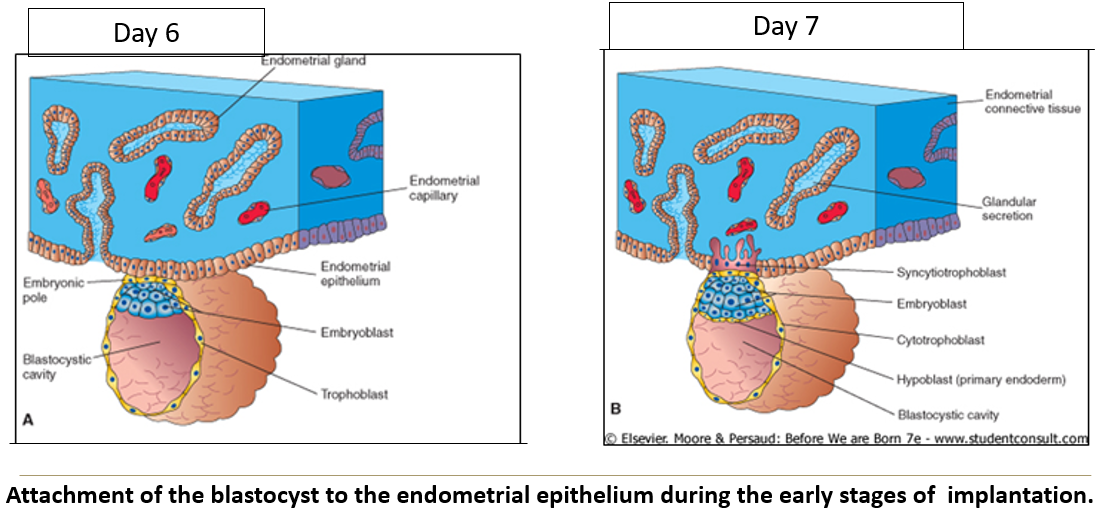
What are the functions of the syncytiotrophoblast?
It enables burrowing into the uterine lining and provides nutrition by invading glands and blood vessels. It also engulfs decidual cells, which are connective tissue cells rich in carbohydrates and lipids.
What percentage of implantations fail, and what might it be mistaken for?
About 45% of implantations fail, often resulting in early spontaneous abortion mistaken for a late, heavy period.
What factors contribute to failed implantation?
It may be due to
estrogen/progesterone sensitivity or
chromosomal abnormalities.
What is ectopic pregnancy?
It’s when an embryo implants outside the uterus, most commonly in the oviduct, causing abdominal pain early in pregnancy.
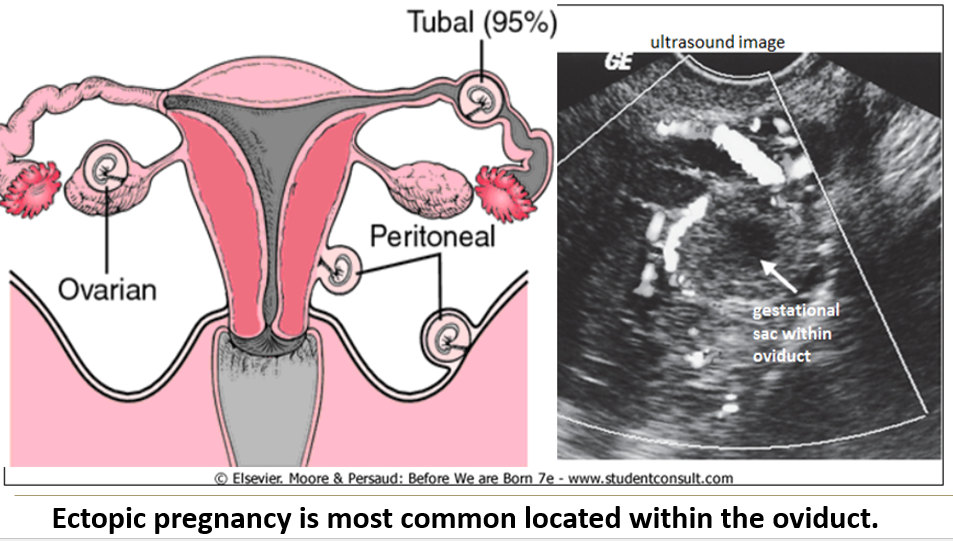
What is a tubal pregnancy and its main cause?
A tubal pregnancy occurs in the oviduct, usually due to scarring of the uterine tubes, but other causes are possible.
Most common location of an ectopic pregnancy?
Oviduct
What is the most common cause of tubal pregnancy?
Caused by scarring of the uterine tubes
How is a tubal pregnancy often resolved?
About 50% resolve naturally through tubal abortion into the pelvic cavity.
Patients may be treated with methotrexate, which prevents cell division, after ultrasound confirmation.
When is surgical removal of a tubal pregnancy necessary?
If the oviduct is at risk of rupture or the implantation is near a major blood vessel, surgery is needed to prevent hemorrhage and maternal death.
Can intra-abdominal pregnancies result in live births?
Rarely, yes, but most require surgical or methotrexate intervention especially if the mother starts bleeding internally.