UNC BIOL252 EXAM 3 STUDY GUIDE
1/145
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
146 Terms
Path of Blood Through The Double Circuit
Vena cava —> Right Atrium —> Right Ventricle —> Pulmonary Trunk (deoxygenated artery) —> Pulmonary Capillaries —> Pulmonary Veins (oxygenated) —> Left Atrium —> Left Ventricle —> Aorta —> Arteries —> Systemic Capillaries —> Veins
Heart, lungs, heart, body
Aorta
The main artery of the body, supplying oxygenated blood to the circulatory system. In humans it passes over the heart from the left ventricle and runs down in front of the backbone.
Vena cava
very large veins that bring deoxygenated blood to your heart to get oxygen
Right Heart
Received deoxygenated blood from the body and sends it to the lungs
Left Heart
Receives oxygenated blood from the lungs and sends it to the body
Diaphragm
Muscle responsible for quiet breathing and separates the thoracic and abdominal cavities. It flexes during inspiration and relaxes during expiration.
Pericardium
A double-layered membrane that surrounds and protects the heart. The outer layer is fibrous and the inner layer is serous.
Fibrous pericardium
the tough outer layer that limits the expansion of the heart, anchors it in place, and prevents it from overfilling with blood
Serous pericardium
Produces pericardial fluid and contains the pericardial cavity. This inner layer consists of 2 parts:
Parietal layer: lines the inside of the fibrous pericardium
Visceral layer: also called the epicardium, covers the heart’s surface
Pericardial cavity
The fluid-filled space between the visceral and parietal pericardia
Pericardial sac
The two outer layers that hold the pericardial cavity and the heart
Myocardium
The innermost muscular layer that makes the heart beat. It is responsible for the contraction of the heart, which pumps blood throughout the body.
Layers of Tissue Surrounding the Heart
Fibrous pericardium (outermost)
Parietal pericardium (serous)
Pericardial cavity
Visceral pericardium (serous)
Myocardium (innermost)
Intercalated discs
Specialized cardiac muscle junctions that connect individual cardiac muscle cells (cardiomyocytes) to one another: they contain desmosomes and gap junctions
Desmosomes
hold cardiomyocytes together during strong muscle contractions (located inside of intercalated discs)
Gap junctions
allow ions and electrical signals to pass quickly between cells, enabling the heart to contract as one coordinated unit (located in intercalated discs)
Sinoatrial (SA) Node
Establishes the frequency of action potentials through pacemaker cells. It is located in the right atrium near the superior vena cava
Atrioventricular (AV) Node
A cluster of pacemaker cells located posterior and medial to the tricuspid valve. It receives the electrical impulse from the SA node, briefly delays it to allow the ventricles to fill completely, and then passes the signal to the bundle branches and through the Purkinje fibers to trigger ventricular contraction.
Sinus rhythm
A normal heartbeat set by the SA node
Bundle branches
Carry the electrical impulse from the atrioventricular (AV) node down toward the apex of the heart, directing the signal to each ventricle.
The right bundle branch sends impulses to the right ventricle.
The left bundle branch sends impulses to the left ventricle.
Purkinje fiber system
The slowest group of pacemaker cells, only depolarize about 20 times per minute. Sometimes called atypical pacemakers because their action potentials rely on different ion channels and they function in a slightly different way.
Pacemaker cells
Specialized cardiac muscle cells found mainly in the SA node that generate their own electrical impulses without external stimulation. These cells set the rhythm of the heartbeat by repeatedly depolarizing and repolarizing, initiating the electrical signals that spread through the heart.
HCN Channels (“Funny Channels”)
Nonspecific cation channels unique to pacemaker cells that open when the cell membrane becomes hyperpolarized (more negative). They allow Na⁺ and K⁺ ions to flow slowly, creating the “funny current” that gradually depolarizes the membrane until it reaches threshold and triggers an action potential
Hyperpolarizes at -60 mV
Ca2+ voltage-gated channel opens at -40 mV and Na+ closes when depolarized
Pacemaker Phsyiology
Slow Initial Depolarization Phase: Funny channels open when membrane is hyperpolarized at -60 mV, and Na+ enters the cell
Full Depolarization Phase: Funny channels close when the cell becomes depolarized. Voltage-gated Ca2+ channels open at threshold (-40 mV), Ca2+ enters the cell, depolarization occurs
Repolarization Phase: Voltage-gated Ca2+ channels close at peak depolarization. Voltage-gated K+ channels open, K+ leaves cell, repolarization occurs.
Cycle Repeats: Voltage-gated K+ channels remain open and depolarization continues. Funny channels will reopen when membrane is hyperpolarized again
How do pacemaker cells increase their pace?
By increasing the membrane’s permeability to Ca2+
How do pacemaker cells decrease their pace?
By increasing the membrane’s permeability to K+
How could you turn a normal neuron membrane channel into a pacemaker cell?
By adding HCN channels
You engineer a cell that has twice as many Na+ funny channels. What effect would this have on the resting membrane potential (RMP)?
It would become more positive as more Na+ travels into the cell
Phases of Contractile Cell Action Potential
Rapid depolarization: Voltage-gated Na+ channels open, Na+ enters the cells, membrane depolarizes
Initial repolarization: Voltage-gated K+ channels open, K+ exits the cell, membrane begins repolarizing. Voltage-gated Na+ channels inactivate.
Plateau Phase: Voltage-gated K+ channels remain open and K+ exits the cell. Voltage-gated Ca2+ channels open and Ca2+ enters the cell. Both channels are open at the same time, causing very little change in voltage.
Repolarization: Voltage-gated K+ channels remain open and K+ exits the cell. Voltage-gated Ca2+ channels inactivate, causing repolarization to intensify.
Significance of the Plateau Phase
Ensures the heart has enough time to slowly relax and refill with blood before the next contraction
Influx of Ca2+ results in…
Release of sarcoplasmic reticulum (SR) Ca2+ (calcium-induced calcium release)
Binding of Ca2+ to troponin
Calcium-induced calcium release
The mechanism where a small calcium influx from outside the cell triggers a larger release of calcium inside the cell, amplifying the signal for heart muscle contraction.
How does calcium return to the extracellular matrix?
P wave
Atrial depolarization // atrial systole
Pacemaker cells are firing action potentials
Represents the SA node action potential
QRS complex
Atrial repolarization and ventricular depolarization // ventricle systole
AV node fires action potentials
T wave
Ventricular repolarization // ventricular diastole
AV node fires action potentials
Pulmonic Semilunar Valve (pulmonary valve)
Located between the right ventricle and the pulmonary trunk.
It opens when the right ventricle contracts, allowing blood to flow into the pulmonary arteries and toward the lungs. It closes when the ventricle relaxes to prevent backflow of blood into the right ventricle.
AV Tricuspid Valve
Located between the right atrium and right ventricle.
It has three cusps (flaps) and opens to allow blood to flow from the right atrium into the right ventricle during relaxation. It closes during ventricular contraction to prevent backflow into the atrium.
Aortic Semilunar Valve
Located between the left ventricle and the aorta.
It opens when the left ventricle contracts to pump oxygenated blood into the aorta and closes when the ventricle relaxes to prevent blood from flowing back into the heart.
AV Bicuspid Valve (Mitral valve)
Located between the left atrium and left ventricle.
It has two cusps (flaps) and opens to let blood flow from the left atrium into the left ventricle. It closes during ventricular contraction to prevent backflow into the left atrium.
Phases of Blood Flow Through the Cardiac Cycle
Ventricular Filling Phase: Ventricles are relaxed (diastole). Change in pressure moves blood to the ventricles.
Isovolumetric Contraction Phase: Atria relax (diastole). Ventricles contract (systole). Blood pushes the AV valves closed. Both sets of valves are closed and ventricular volume does not change.
Ventricular Ejection Phase: Ventricles continue contracting (systole). Semilunar valved are pushed open, and pressure increase moves blood out of the ventricles. Blood enters the aorta and pulmonary trunk.
Isovolumetric Relaxation Phase: Ventricles relax (diastole). Blood pushes semilunar valves closed. Both sets of valves are closes and ventricular volume does not change.
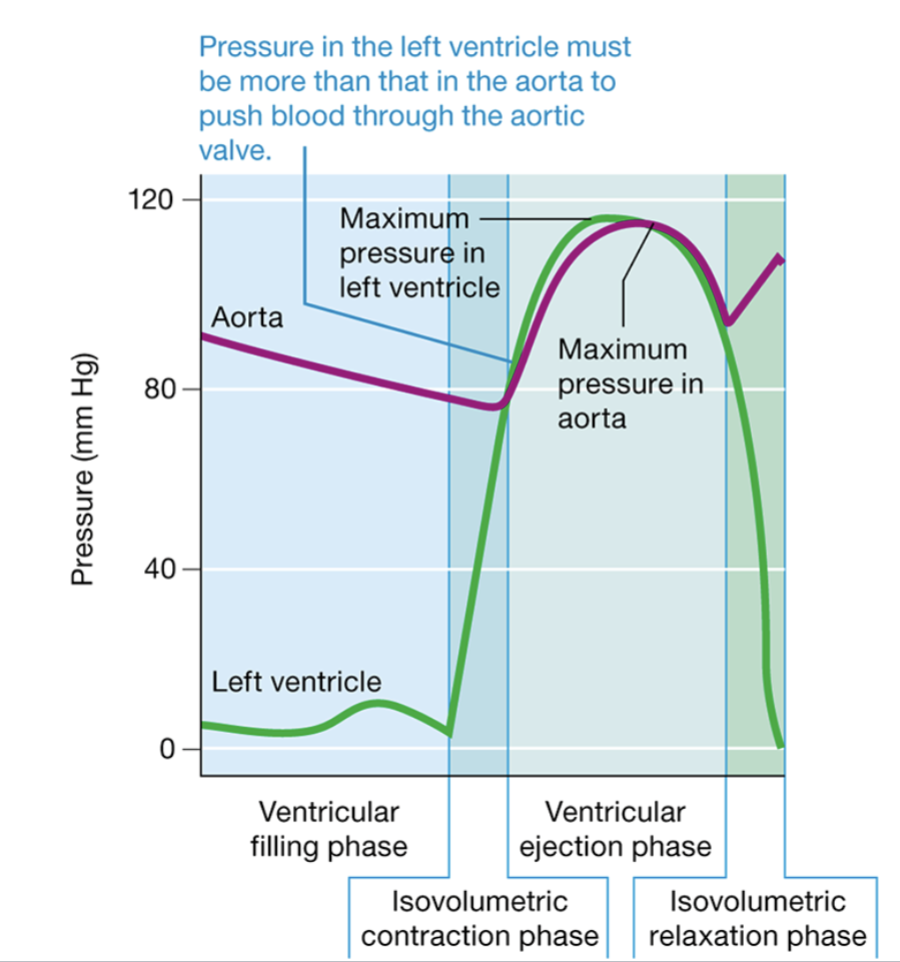
During which phase(s) of the cardiac cycle is no blood moving in the heart?
Isovolumetric contraction and relaxation phases. Prefix “iso” means “same,” so the volume of blood doesn’t change.
During which phase(s) of the cardiac cycle is blood moving from the atria to the ventricles?
Ventricular filling phase
During which phase(s) of the cardiac cycle is blood moving from ventricles to the aorta and pulmonary trunk?
Ventricular ejection phase
During which phase(s) of the cardiac cycle is pressure in the left ventricles greater than the pressure in the aorta?
Ventricular ejection phase
During which phase(s) of the cardiac cycle is pressure in the aorta greater than in the left ventricle?
Ventricular filling phase, isovolumetric contraction phase, isovolumetric relaxation phase
S1 Heart Sound
Heard as the AV valves close (tricuspid and bicuspid valves)
S2 Heart Sounds
Heard as the SL valves close (pulmonary and aortic valves)
Stroke Volume (SV)
The amount of blood pumped by the left ventricle in one heartbeat
Calculation: SV = EDV - ESV
End-Diastolic volume (EDV)
Amount of blood in the left ventricle after it has filled. Affected by 2 variables:
The length of time the ventricle spends in diastole
The amount of blood returning to the right atrium from the systemic circuit
End-Systolic volume (ESV)
amount of blood in the left ventricle at the end of a contraction
Cardiac Output (CO)
The amount of blood pumped out of the heart per minute. It is the same for both sides of the heart.
Calculation: CO = HR x SV
Each side of the heart has the same…
Stroke volume, heart rate, and cardiac output
Factors the Influence Stroke Volume
Preload
Afterload
Contractility
Preload
Refers to the degree to which the sarcomeres in the ventricular cells are stretched before they contract. When venous pressure rises, and more blood flows into the ventricle, the ventricular wall is stretched. Enhances contractility and stroke volume.
Frank-Starling Law
The greater the end-diastolic volume (EDV), the greater the stroke volume (SV)
Situations that Increase Preload
Exercise: muscle contractions push more blood back to the heart, increasing venous return
Increased blood volume: conditions like excessive IV fluid administration or kidney disease lead to higher blood volume, increasing venous return
Lying down: Gravity no longer pulls blood down into the lower extremities, so more blood returns to the heart
Afterload
The blood pressure in the aorta and the pulmonary trunk that resists the ejection of blood from the ventricles during systole. It opposes ventricular ejection and reduces the stroke volume.
High afterload causes a weak heart and low contractility
Situations that Increase Afterload
Hypertension: Increased arterial pressure makes it harder for the heart to eject blood
Aortic Stenosis: A narrowed aortic valve increases resistance, requiring more forceful contractions
Vasoconstriction: Conditions like stress or cold exposure can cause blood vessels to narrow, increasing resistance to blood flow
Contractility
The intrinsic strength of the cardiac muscle contraction, independent of preload and afterload
Inotropic agents
Affects contractility
Norepinephrine increases contractility
Acetylcholine decreases contractility (small effect)
Chronotropic agents
Affects heart rate
Sympathetic NS (NE) = positive agent, regulated by cardiac nerves
Thyroid Hormones E & T3 = positive agents
Parasympathetic NS (ACh) = negative agent, regulated by CN X, perform action on pacemaker cells
Baroreceptors
Provide information on blood pressure and respond to changes in blood pressure. Contained in carotid sinuses.
Chemoreceptors
Respond to changes in blood chemistry. Contained in carotid and aortic bodies.
In cases of hypotension, baroreceptors would tell the cardiac centers to stimulate the heart with the _____ nervous system. Heart rate would _____, and the CO would _____, returning BP to normal.
Sympathetic, increase, increase
In cases of hypertension, baroreceptors would tell the cardiac centers to stimulate the heart with the _____ nervous system. Heart rate would _____, and the CO would _____, returning BP to normal.
Parasympathetic, decrease, decrease
Structure of Blood Vessels
Tunica intima
Tunica media
Tunica externa
Echocardiogram (ECG)
A graphic depiction of the electrical activity occurring in all cardiac muscle cells over a period of time. They can only show electrical changes that occur in contractile cells, so it appears flat when the pacemaker cells have their action potentials.
R-R Interval
entire duration of a cardiac action potential, determines heart rate
P-R interval
duration of atrial depolarization and AV node delay
Q-T interval
entire duration of ventricular action potential
S-T segment
ventricular plateau phase
Diastole
a period of relaxation
Systole
a period of contraction
Arteries
The distribution system of the vasculature: they travel away from the heart, branching into vessels of progressively smaller diameter.
Pulmonary circuit: transport deoxygenated blood
Systemic circuit: transport oxygenated blood
Capillaries
The exchange system of the vasculature: they are vessels of very small diameter that form branching networks called capillary beds. Gases, nutrients, wastes, and other substances are quickly exchanged between cells and the blood through the walls of these vessels.
Contain only tunica intima
Has porous intercellular connections and fenestrations
Veins
The collective system of the vasculature: they drain blood from capillary beds and return it to the heart. These vessels become progressively larger as they get closer to the heart.
Pulmonary circuit: transport oxygenated blood
Systemic circuit: transport deoxygenated blood
Tunica intima
The innermost layer of tissue composed of ENDOTHELIUM: consists of a sheet of simple endothelium and its basal lamina.
Endocardium
The inner lining of the heart, which is also composed of endothelium
Tunica media
The middle layer of the blood vessel wall. The smooth muscle cells control the diameter of the blood vessel and so the amount of blood flow to the organs. It has 2 layers:
A layer of smooth muscle cells arranged in a circular manner around the lumen
A layer of elastic filaments called external elastic lamina
Tunica externa
The outermost layer of tissue composed of dense irregular collagenous connective tissue that supports the blood vessel and prevents it from overstretching.
Vaso Vasora
“vessels to the vessels” —> tiny vessels supplying the tunica media and tunica externa. They supply O2 and nutrients to the outer layers of larger blood vessels, whose cells are too far away from the lumen to receive O2 and nutrients by diffusion alone.
Elastic arteries
High blood pressure vessels closest to the heart. They have the largest diameter and have very extensive elastic lamina.
Ex. Aorta
Muscular arteries
Have extremely thick tunica media, and are responsible for controlling blood flow to organs and consist of smooth muscle. Major site of vasodilation and vasoconstriction. They make up the smaller branches of the aorta.
Ex. renal artery
Aterioles
Thin-walled (1 layer of endothelial cells) vessels that contain smooth muscle and control blood flow to tissues. They are also major sites of vasodilation and vasoconstriction, and exchange materials.
Fenestrations
Holes in the plasma membrane allowing easy movement of materials through
Venules
The smallest veins which drain blood from capillary beds. Consists of thin walls and little smooth muscle. Some exchange continues here, and there is little tunica media/externa
Venous and Arterial Anastomoses
Connection between two veins or two arteries allowing blood to reroute in case of a blockage
Ateriovenous anastomosis (shunt)
A direct connection between an artery and a vein, bypassing capillaries to regulate blood flow as in thermoregulation
Factors that Influence Blood Pressure
Cardiac output (CO): blood flow into the vessels
Blood volume: total volume of the circulatory system
Resistance: prevention of flow
Compliance: stretchiness of vessels
Factors Determining Peripheral Resistance
Vessel radius (smaller radius = more resistance)
Blood viscosity (higher viscosity = more resistance)
Blood vessel length (longer length = more resistance)
Obstructions in vessels
Mean arterial pressure (MAP)
diastolic pressure + 1/3(systolic pressure - diastolic pressure)
Which two values account for the pressure change that drives blood flow?
Cardiac output and peripheral resistance
How does venous blood get into the heart?
Venous valves that dictate one direction of flow
The muscular pump
The respiratory pump
Venoconstriction (smooth muscles in vein walls)
Baroreceptor reflex
When MAP is low, the sympathetic neurons increase heart rate and contractility, which increases cardiac output, leading to increased MAP. Sympathetic neurons also cause vasoconstriction of arterioles, which increases peripheral resistance, leading to increased MAP and BP.
When MAP is high, parasympathetic neurons decrease the heart rate and contractility, which decreases cardiac output, leading to decreased MAP. Sympathetic neurons are inhibited, but there is no parasympathetic innervation to blood vessels. If there is no sympathetic stimulation, the vessels naturally dilate.
Chemoreceptors
Located around the great vessels (the aorta and carotid arteries), and also in the medulla. The carotid bodies sense changes in the blood’s gasses and accompanying pH changes. Low O2/high CO2 result in sympathetic activation of the heart and blood vessels that lead to increased MAP.
ADH
Stimulated by high Na+ levels. Response is thirst, water retention, and vasoconstriction.
Aldosterone
Stimulated by low Na+ levels. Response is Na+ retention.
Angiotensin-II
Powerful hormone stimulated by low blood volume. The response is thirst, Na+ retention, and vasoconstriction.
Promotes vasoconstriction of efferent arterioles (keeps kidneys working properly with low BP)
Promotes vasoconstriction of systemic blood vessels (arterioles have receptors for this hormone)
Promotes reabsorption of Na+ and Cl- from the proximal tubule (region of kidney that gets H2O back into circulation) and H2O follows
Promotes aldosterone release, leading to increase Na+ and H2O reabsorption
Stimulates thirst center in hypothalamus, which may increase fluid intake.
ANP
Hormone stimulated by high blood volume. Response is Na+ and H2O excretion and vasodilation.