BB Exam 5 Review
5.0(1)
Card Sorting
1/114
There's no tags or description
Looks like no tags are added yet.
Last updated 2:50 AM on 4/14/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
115 Terms
1
New cards
How long is the blood donor deferral for someone with or with a history of Chagas’ Disease?
Indefinite deferral
2
New cards
How long is someone deferred from donating blood if they have CJD, have a blood relative with CJD, had a dura matter transplant, or pituitary-derived growth hormone?
Indefinite deferral
3
New cards
How long is someone deferred from blood donation if they have Zika? Or is it if they travelled to somewhere with a zika endemic?
4 week deferral
4
New cards
How long is a blood donor deferred if they have Hep B IgG?
12 months
5
New cards
How long is a blood donor deferred if they have a new tattoo/piercing?
12 months
6
New cards
How long is a blood donor deferred if they have been exposed to someone else’s blood?
12 months
7
New cards
How long is a blood donor deferred if they have had sexual contact with a person at high risk for HIV?
12 months
8
New cards
How long is a blood donor deferred if they have been imprisoned for more than 72 hours?
12 months
9
New cards
How long is a blood donor deferred after they have returned from a malarial endemic area?
12 months
10
New cards
How long is a blood donor deferred after a post-blood transfusion?
12 months
11
New cards
How long is a blood donor deferred after they have used acutane?
1 month
12
New cards
How long is a blood donor deferred after they have used propecia use?
1 month
13
New cards
How long is a blood donor deferred after a malarial infection?
3 years after becoming asymptomatic
14
New cards
How long is a blood donor deferred if they have taken aspirin and aspirin-containing drugs?
48 hours (2 days)
15
New cards
List some conditions that would meet the criteria for a **permanent deferral**
1. Human pituitary growth hormone injection
2. Taken clotting factors
3. Sexual contact with anyone who used a needle to take illegal drugs
4. AIDS or HIV pos.
5. Males having sex w/ other males (update: 3 mo. from last sexual contact)
6. Had viral hepatitis
7. Positive HBsAg
8. Positive HBc
9. Positive HTLV
10. History of CJD
11. History of Chagas’ or babesiosis
16
New cards
What is the minimum Hgb requirement to donate blood?
12\.5 g/dl
17
New cards
What is the minimum Hct requirement to donate blood?
38%
18
New cards
What is the minimal age *without* parental consent to donate blood?
17
19
New cards
What age must you at least be in order to donate blood *with* parental consent?
16 or older
20
New cards
What is the ideal body temperature to donate blood?
21
New cards
What is the ideal blood pressure you must have to donate blood?
< 180/100
22
New cards
What is the pulse range for blood donation?
50-100 bpm
23
New cards
What is the minimum body weight required for blood donation?
110 lbs
24
New cards
If you decide to take blood from someone who is less than 110 lbs, what must you do first?
Reduce the amount of anticoagulant
25
New cards
What is the standard volume of anticoagulant? (hint: looking for a # not a definition)
63 mL
26
New cards
What is the volume of a standard unit?
450 mL plus or minus 45 mL
27
New cards
How would you calculate the amount of anticoagulant needed, anticoagulant removed, and amount of blood collected for an “underweight” donor?
1. __Reduce Volume Factor (__@@__**A**__@@__)__ = weight (lbs)/ 110 lbs
2. @@**A**@@ x 63 = amount of anticoagulant needed (^^**B**^^)
3. 63 mL - ^^**B**^^ = amount of anticoagulant removed
4. @@**A**@@ x 450 mL = amount of blood collected
28
New cards
How often can you donate **RBCs**?
8 weeks
29
New cards
How often can you donate **Platelets**/**Granulocytes**?
* 48 hours between donations
* No more than 2x a week or 24x per year
* No more than 2x a week or 24x per year
30
New cards
What is the minimum amount of platelets that you need to have in order to donate?
150,000/uL
31
New cards
How often can you donate **plasma**?
* every 4 weeks
* Total protein must be within normal limits (**>6.0 g/dL**)
* Total protein must be within normal limits (**>6.0 g/dL**)
32
New cards
Blood expires in ___ days with the addition of the anticoagulant CPD.
21
33
New cards
Blood expires in ___ days with the addition of the anticoagulant CP2D.
21
34
New cards
Blood expires in ___ days with the addition of the coagulant CPDA-1.
35
35
New cards
Blood expires in ___ days with the addition of AS-1, AS-3, or AS-5.
42
36
New cards
What is the function of the preservative: Dextrose
Supports RBC life by providing energy
37
New cards
What is the function of the preservative: Adenine
Used in ATP synthesis; restores ATP
38
New cards
What is the function of the preservative: Citrate
Chelates calcium to prevent coagulation
39
New cards
What is the function of the preservative: Sodium biphosphate
Buffer to prevent decrease in pH
40
New cards
During storage of **RBC** units, what **increases**?
1. Potassium (K+)
2. Lactic Acid
3. Plasma Hemoglobin
41
New cards
During the storage of **RBC** units, what **decreases**?
1. ATP
2. 2,3 DPG
3. pH
42
New cards
What temperature do you store **PRBCs**?
1-6 C
43
New cards
What temperature do you store **frozen RBCs** and when do they expire?
* ≤ -65 C
* 10 years
* 10 years
44
New cards
What temperature do you store **deglycerolized RBCs** and when do they expire?
* 1-6 C
* 24 hours
* 24 hours
45
New cards
What temperature do you store **irradiated RBCs** and when do they expire?
* 1-6 C
* 28 days *or* originally assigned expiration date (whichever comes first)
* 28 days *or* originally assigned expiration date (whichever comes first)
46
New cards
What temperature do you store **platelets** and when do they expire?
* 20-24 C (room temp.), agitated
* 5 days
* 5 days
47
New cards
What temperature do you store ***pooled*** **platelets** and when do they expire?
* 20-24 C (room temp.), agitated
* 4 hours
* 4 hours
48
New cards
What temperature do you store **apheresis platelets** and when do they expire?
* 20-24 C (room temp.), agitated
* 24-48 hours
* 24-48 hours
49
New cards
What temperature do you store **fresh frozen plasma (FFP)** and when does it expire?
* ≤ -18 C
* 1 year
* 1 year
50
New cards
What temperature do you store **thawed FFP** and when does it expire?
* 1-6 C
* 24 hours
* 24 hours
51
New cards
What temperature do you store **cryoprecipitate** and when does it expire?
* ≤ -18 C
* 12 months
* 12 months
52
New cards
What temperature do you store **granulocytes** and when do they expire?
* 20-24 C (room temp.)
* 24 hours
* 24 hours
53
New cards
What is the guideline in order for a patient to be refractory?
If 10 minute platelet count is less than 50% of that expected on *two* occasions
54
New cards
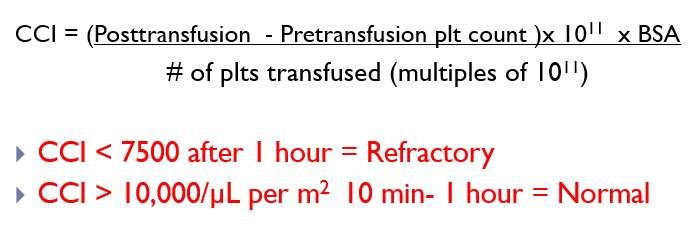
What is the equation to determine platelet refractoriness?
\
55
New cards
If CCI is less than 7500 after 1 hour, the patient is considered ________.
Refractory
56
New cards
If the CCI is greater than 10,000/uL per m^2 after 10 minutes to an hour, the patient is considered _______.
normal
57
New cards
List the most common FDA approved methods for bacterial contamination testing.
1. BacT/ALERT culture system (bioMerieux)
2. Pall eBDS system (Pall Corp)
3. ScanSystem (Hemosystem)
58
New cards
What temperature should **PBRCs** be ***transported*** at?
1-10 C with ice in plastic bags
59
New cards
How should **frozen components** be transported?
With dry ice
60
New cards
Define **Apheresis**
The separation of blood components; removal of desired components and return of remainder of the blood to donor
61
New cards
The **buffy coat** consists of ______ & _______.
leukocytes & platelets
62
New cards
What are the donor requirements for **plateletpheresis**?
* same as whole blood, no aspirin within 3 days
* Pre-platelet count: 150 x 10^9/L
* Pre-platelet count: 150 x 10^9/L
63
New cards
What quality control factors do you need to consider with plateletpheresis?
* 3 x 10^11 in 75% of units tested
* pH > 6.0
* pH > 6.0
64
New cards
\
What is plateletpheresis used for?
What is plateletpheresis used for?
1. Increase platelet counts
2. Prevent HLA alloimmunization
65
New cards
What are the requirements for leukapheresis?
* Same as whole blood donations
* Absolute granulocyte count: 4.0 x 10^9/L
* Absolute granulocyte count: 4.0 x 10^9/L
66
New cards
What quality control factors do you need to consider with leukapheresis?
WBC > 1.0 x 10^10
67
New cards
What is leukapheresis used for?
1. Sepsis
2. Removal of blasts from leukemic patients
3. Neutropenia in cancer patients
68
New cards
What is the purpose of plasmapheresis?
Removal of plasma and returning cellular components to patient
69
New cards
What are the donor requirements for plasmapheresis?
Same as platelet donors
70
New cards
What is plasmapheresis used for?
1. @@**Multiple myeloma**@@ (remove abnormal protein)
2. Lupus (immune complexes)
3. Autoantibodies
4. Toxins (barbiturate poisoning)
71
New cards
What happens in **Intermittent Flow Centrifugation**
1. Blood drawn from donor is anticoagulated with **ACD**
2. Blood pumped into bowl which separates components by specific gravity
3. Desired component is removed into a separate bag and the remaining is returned to donor
72
New cards
What does the list below describe?
* Blood drawn out and put back in “batches”
* **One** venipuncture site
* Repeats 6-8 cycles to obtain therapeutic dose
* Takes longer but more mobile
* Blood drawn out and put back in “batches”
* **One** venipuncture site
* Repeats 6-8 cycles to obtain therapeutic dose
* Takes longer but more mobile
Intermittent Flow Centrifugation
73
New cards
What does the list below describe?
* Blood is spun, separated continuously with desired product being removed, and remaining product returned **uninterrupted**
* **2** venipuncture sites
* Faster
* Blood is spun, separated continuously with desired product being removed, and remaining product returned **uninterrupted**
* **2** venipuncture sites
* Faster
Continuous Flow Centrifugation
74
New cards
What is a major “pro” of Continuous Flow Centrifugation (CFC)?
Reinfuses **simultaneously** (IFC does one cycle before starting the next one) - so it’s a lot faster
75
New cards
If a patient is experiencing tingly/ numb lips during an apheresis treatment, what might be the cause?
Transient systemic hypocalcemia (citrate toxicity) presenting with numbness, tingly lips, cramping, EKC changes, etc… from **ACD** (Acid Citrate Dextrose)
76
New cards
What is **HES** and what is it used for?
* Hydroxyethyl starch
* “Sedimenting agent”
* Promotes rouleaux
* “Sedimenting agent”
* Promotes rouleaux
77
New cards
What is the minimum acceptable platelet count for platelets apheresis?
3 x 10^11
78
New cards
What might donors be given in order to increase the number of granulocytes that can be collected for granulocytes apheresis?
1. corticosteroids
2. growth factors (G-CSF)
3. Precipitating agents (e.g., **HES**)
79
New cards
What is the minimum number of granulocytes per component for granulocytes apheresis?
1 x 10^10
80
New cards
How long should it take to collect a whole blood unit?
15 minutes
81
New cards
When should FFP be separated/frozen?
Within 7 (or 8) hours of collection
82
New cards
When should platelets be separated?
Within 8 hours of collection
83
New cards
You’re gonna ace these finals, pass the BOC with flying colors, and get a job starting off at 70K.
periodt
84
New cards
Quality Control:
In **leukocyte-reduced components**, what is the amount of leukocytes that you must have and what percentage of the original RBC mass should be maintained?
In **leukocyte-reduced components**, what is the amount of leukocytes that you must have and what percentage of the original RBC mass should be maintained?
* 5.5 x 10^6 (leukocytes)
* 85% of original RBC mass should be maintained
* 85% of original RBC mass should be maintained
85
New cards
Quality Control:
How many **platelets** per unit in 75% of units tested? How many platelets per unit in an **apheresis unit**?
How many **platelets** per unit in 75% of units tested? How many platelets per unit in an **apheresis unit**?
* 5.5 x 10^10 platelets/unit in 75% of units tested
* Apheresis unit: 3 x 10^11 platelets/unit
* Apheresis unit: 3 x 10^11 platelets/unit
86
New cards
Do leukapheresis and granulocyte products need to be crossmatched with the patient?
YES! These products still contain a small amount of RBCs that are still in it.
87
New cards
Quality Control:
How much fibrinogen and Factor VIII (8) is needed in order to be considered **cryoprecipitate**?
How much fibrinogen and Factor VIII (8) is needed in order to be considered **cryoprecipitate**?
* 150 mg/dL of fibrinogen
* 80 IU Factor VIII (8)
* 80 IU Factor VIII (8)
88
New cards
Quality Control:
Granulocytes need to be greater than _____.
Granulocytes need to be greater than _____.
greater than 1 x 10^10
89
New cards
In general, what is the function of all RBC components?
Carrying oxygen
90
New cards
Why do we give leukocyte-reduced RBCs?
To reduce **febrile transfusion reactions**
91
New cards
Why do we give irradiated RBCs?
To reduce the chance of **graft-vs-host**
92
New cards
Why do we give washed RBCs?
Given for someone who has an anaphylactic reaction
93
New cards
Why do we use FFP (fresh frozen plasma)?
Replace coag factors
94
New cards
What are platelets used for?
* Used to control bleeding
95
New cards
Contraindications:
You __**DO NOT**__ want to give platelets to patients with which disorders?
You __**DO NOT**__ want to give platelets to patients with which disorders?
1. Uremic patients (HUS)
2. Autoimmune disorders
1. Idiopathic thrombocytopenia (ITP)
2. TTP
96
New cards
What do we use granulocytes for?
1. Septic patients
2. Immunodeficient patients
97
New cards
What do we use cryo for?
1. **Fibrinogen deficiency**
2. Factor XIII deficiency
3. Fibrin sealant (mixed with thrombin)
98
New cards
Contraindications:
When should you __**NOT**__ give a patient RBCs?
When should you __**NOT**__ give a patient RBCs?
1. Compensated/nutritional anemias
2. General fatigue
3. Enhance a patient’s well-being
4. Wound healing
99
New cards
MHC 1 is responsible for which HLA’s?
HLA-…
* A
* B
* C
* A
* B
* C
100
New cards
MHC 2 is responsible for which HLA’s?
HLA-…
* DR
* DP
* DQ
* DR
* DP
* DQ