38. Antimicrobial Therapy: Overview and Agent Classification
1/7
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
8 Terms
Overview of Microbiology: Pathogenic Organisms
pathogens cause infection
Infectious disease is a process of when an organism causes tissue damage which can lead to impairment of body function.
The following microorganisms are involved in the initiation and spread of human disease:
Bacteria: treated with antibiotics
Fungi
Viruses
Protozoa
Antibiotics: Route of Administration
Topical antibiotic eye drops or ointments are indicated for most ocular surface infections, such as blepharitis or conjunctivitis..
Oral antibiotics may be more effective for some infections of the adnexa, such as hordeolum and preseptal cellulitis.
Injections into or around the eye (e.g., periocular, intracameral, and intravitreal injections) and/or intravenous antibiotics may be indicated for acute conditions (endophthalmitis, retinitis, orbital cellulitis)
Patients with acute conditions (endophthalmitis, retinitis, orbital cellulitis) or other complicated inflammatory or infectious diseases may need an immediate referral.
Antibiotics: General Warnings and Precautions
Allergic cross-sensitivity reactions are possible within the same or similar classes of drugs.
Cross-sensitivity is likely between all members of a drug class
Cross-sensitivity is possible between similar classes.
~3-5% of patients with a penicillin allergy may cross-react with a cephalosporin due to the structural similarity of having a beta-lactam ring.
Antibiotic use, may result in bacterial or fungal overgrowth of non-susceptible organisms which may lead to secondary infection or superinfection.
Culture and sensitivity (susceptibility) testing is recommended as needed to confirm a diagnosis or when therapy is not progressing.
Topical antibiotics should not be used in non-superficial, or deep- seated infections or in infections likely to become systemic.
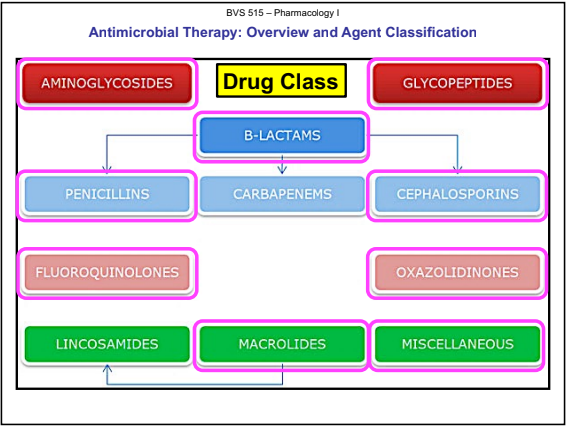
Drug Class
Mode of Action: Bactericidal or Bacteriostatic (Killing Power)
Bactericidal
Aminoglycosides
Polypeptides: Bacitracin, Polymyxins, and Colistin
B-Lactam antibiotics
Bacteriostatic
Tetracyclines
Macrolides
Linzeolid (Zyvox) - Oxazolidinones
can be either bactericidal or bacteriostatic depending on the organism
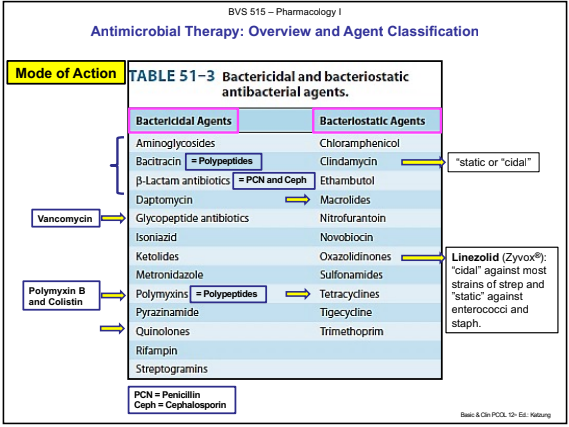
Mode of Action: Bactericidal or Bacteriostatic (Killing Power)
Antibiotic killing properties based on:
Mechanism of action
Achievable serum, tissue, or body fluid concentration with respect to the site of infection
Minimum Inhibitory Concentration (MIC)
The lowest concentration of an antimicrobial that will inhibit the visible growth of a microorganism after overnight incubation. (MICs are used by diagnostic laboratories mainly to confirm resistance)
Bacteriostatic: Limits the spread of infection.
Limits the spread of infection by slowing the growth and replication of bacteria while the body’s immune system attacks and eliminates the pathogens
Bactericidal: Kills bacteria.
Kills bacteria which results in a decrease in the total number of viable organisms.
not using the body as much; better for those with immune system issues
Spectrum of Activity: Narrow vs Broad
Spectrum of coverage for antibiotic selected.
Broad Spectrum Coverage: Antibiotics which halt the growth of, or eradicate a wide range of bacteria
Narrow Spectrum Coverage: Antibiotics which halt the growth of, or eradicate a more specific or narrow range of bacteria
Propensity to induce resistance
Description of Antimicrobial Resistance
Is the broader term for resistance in different types of microorganisms and encompasses resistance to antibacterial, antiviral, antiparasitic and antifungal drugs.
Antimicrobial resistance occurs when infectious microbes develop or acquire the ability to survive exposures to clinically relevant concentrations of antimicrobial drugs that would kill otherwise sensitive organisms of the same strain.
Resistance is also used to describe any pathogen that is less susceptible
Antimicrobial resistance occurs naturally but is also facilitated by the inappropriate use of antibiotics.
The appropriate use of antibiotics or antimicrobial stewardship is a major initiative to reduce antimicrobial resistance.
When microorganisms become resistant to most antibiotics, they are often referred to as “superbugs” or multi-drug-resistant organisms (MDROs).