Adult Echo 2 finalA connective tissue disorder that often affects the elderly causes swelling and loss of mobility in the body's joints. Scimitar syndrome Rheumatoid arthritis Systemic lupus erythematosus Erhlers-Danlos syndrome
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
102 Terms
A connective tissue disorder that often affects the elderly causes swelling and loss of mobility in the body's joints.
Scimitar syndrome
Rheumatoid arthritis
Systemic lupus erythematosus
Erhlers-Danlos syndrome
Rheumatoid arthritis
Non primary cardiac tumors are how many more times as likely to occur than primary cardiac tumors?
5 times
10 times
20 times
50 times
20 times
Amyloidosis involves improperly folded _________ that infiltrate the myocardium.
DNA
Glucose
Proteins
Lipids
Proteins
Secondary metastatic tumors, frequently travel:
To the pericardium, myocardium and then to the endocardium
From the IVC to the right atrium and then to the right ventricle
From the pulmonary veins into the left atrium
All of the above
All of the above
A skin lesion that develops in late stage AIDS infections is called
Ulcerations
Pustules
Angiosarcoma
Kaposi's sarcoma
Kaposi's sarcoma
A dumb-bell shaped configuration of the inter-atrial septum often mistaken as cardiac mass is associated with:
Amyloidosis
Lipomatous hypertrophy
Sarcoidosis
Sarcoma
Lipomatous hypertrophy
A common cardiomyopathy that develops in patients with chronic HIV infections is:
Dilated cardiomyopathy
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
Constriction
Dilated cardiomyopathy
Kawasaki's disease is an inflammatory illness that affects children. A cardiac manifestation of Kawasaki's disease is:
Dilated coronary arteries
Dilated ventricular chambers
Cardiac thrombus formation
Mitral regurgitation
Dilated coronary arteries
The most common primary malignant intracardiac tumor in adults is which of the following?
Myxoma
Papillary fibroelastoma
Angiosarcoma
Fibroma
Angiosarcoma
A cardiac manifestation of carcinoid is
Restricted TV leaflet motion
Restricted MV leaflet motion
PHTN
Aortic stenosis
Restricted TV leaflet motion
A well-encapsulated, small tumor composed of fat cells is named____________.
Fibroelastoma
Mesothelioma
Angiosarcoma
Lipoma
Lipoma
The following is true of rhabdomyomas:
Found in the ventricular walls
Most common cardiac tumor in children
Often obstruct the conduction pathways in the myocardium
All of the above
All of the above
The improper retention and storage of iron particles in the body is called:
Sarcoidosis
Carcinoid
Scleroderma
Hemachromatosis
Hemachromatosis
An arteritis that presents with intimal thickening of the aorta and it's major branches is called:
Takotsubo
Fibromuscular dysplasia
Buerger's disease
Takayasu's arteritis
Takayasu's arteritis
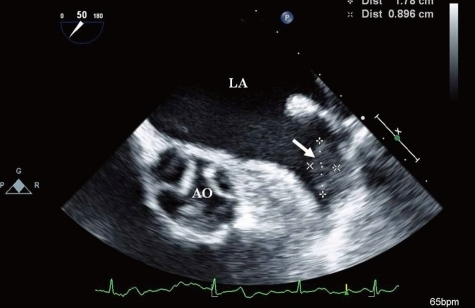
The TEE image of the left atrial appendage revealed:
A normal LAA
A LAA clot
A double lobed LAA
None of the above
A LAA clot
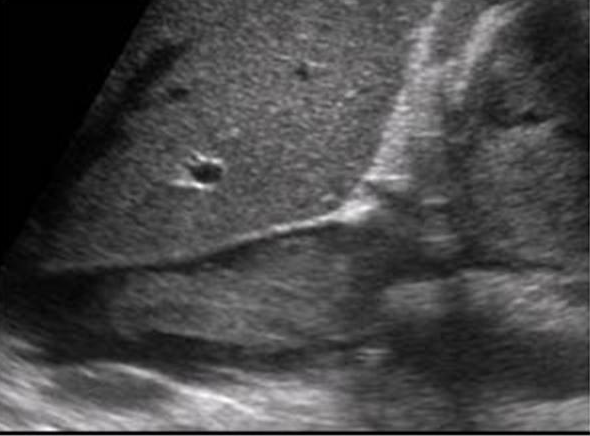
The mass in the IVC on the image above is most likely consistent with which of the following diagnoses?
Rhabdomyosarcoma
Myxoma
Infiltrative renal cell carcinoma
Angiosarcoma
Infiltrative renal cell carcinoma
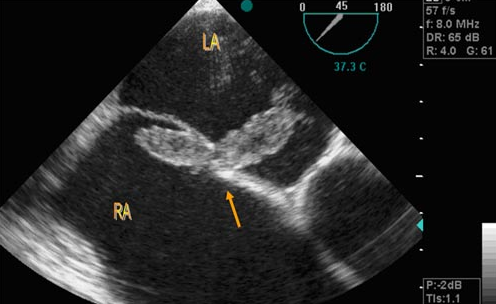
A patient is referred to the echo lab because of symptoms of TIA's. The patient had an echo previously which showed a small patent foramen ovale. A TEE is performed and reveals the above diagnosis.
Normal inter-atrial septum
Catheter protruding through the intra-atrial septum
A large clot lodged in the patent foramen ovale
An ASD closure device
A large clot lodged in the patent foramen ovale
In cases of secondary metastatic tumors in the heart, a common echocardiographic finding is
Pericardial effusion
Well-circumscribed mass with definitive borders
Thickening of the interatrial borders
Cystic space in the pericardium
Pericardial effusion
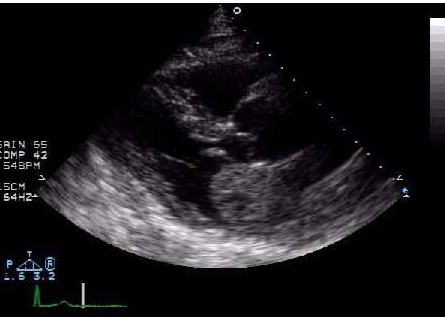
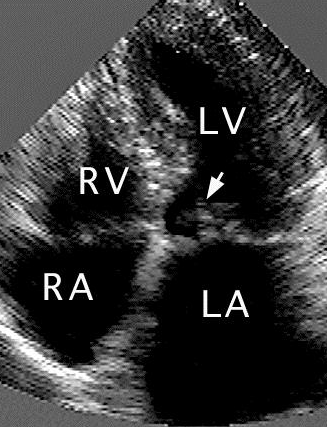
The image above demonstrates a benign primary cardiac tumor. The most likely diagnosis is which of the following?
right atrial myxoma
left atrial myxoma
right atrial hemangioma
left atrial hemangioma
left atrial myxoma

This was taken on a patient who has been diagnosed with postpartum cardiomyopathy and who currently has an ejection fraction of 20%. What is the most likely diagnosis?
left atrial myxoma
left mitral valve vegetation
left ventricular thrombus
right atrial myxoma
left ventricular thrombus
A 34 year old man with lymphoma presents with a 3 week history of decreased exercise tolerance. Physical exam reveals a diaphoretic man with a BP of 90/60, HR of 120 and respiratory rate of 24/min. Lungs are clear, heart sounds are distant. Echo reveals a large, circumferential pericardial effusion with RV diastolic collapse. The most appropriate next step in treating this patient is which of the following?
Evaluate for RA systolic collapse
Record Doppler filling velocities with a respirometer
Insert a Swan-Ganz catheter
Perform a pericardiocentesis
Perform a pericardiocentesis
Etiological possibilities for the development of constrictive pericarditis include which of the following?
cardiac surgery
viral
bacterial
all of the above
all of the above
When evaluating a patient for cardiac tamponade, the echo helps determine the size, location and hemodynamic effects of the pericardial effusion on the heart. Cardiac tamponade is a diagnosis made by which of the following?
Cardiac catheterization
Electrocardiogram
Tamponade is a clinical diagnosis
Thoracotomy
Tamponade is a clinical diagnosis
Classic clinical signs and symptoms of constrictive pericarditis include which of the following?
pericardial knock
murmur
none of the above
Ewart's Sign
pericardial knock
the physiologic severity of a pericardial effusion largely depends on which of the following?
volume and rate of fluid accumulation
volume and presence or absence of loculations in the fluid
rate of accumulation and fluid composition
fluid composition
volume and rate of fluid accumulation
A small posterior echo-free space is detected during the systolic phase only by M-mode/2D echo. This is considered a:
Cardiac tamponade
Normal finding
Moderate pericardial effusion
Large pericardial effusion
Normal finding
In order to be considered full blown tamponade physiology, which of the following must be present?
right ventricular systolic collapse and right atrial diastolic collapse
right ventricular diastolic collapse and right atrial systolic collapse
left atrial systolic collapse and right ventricular diastolic collapse
left ventricular collapse and right atrial collapse throughout systole and diastole
right ventricular diastolic collapse and right atrial systolic collapse
A 10 mmHg decrease in systemic blood pressure with inspiration associated with cardiac tamponade is referred to as which of the following?
Beck's triad
precordium
orthostatic hypotension
pulsus paradoxus
pulsus paradoxus
Which of the following is a component of Beck's Triad?
Bradycardia
Muffled heart sounds
Decreased venous pressure
Hypertension
Muffled heart sounds

What diagnosis can be made from this echo image?
Normal parasternal long axis
Pericardial effusion
Pericardial and pleural effusion
Pleural effusion
Pericardial and pleural effusion
A 45-year old female presents to her doctor with complaints of increasing dyspnea on exertion for three months. Her physical exam reveals jugular venous distention, ascites and a pericardial knock. What is the most likely diagnosis?
constricitve pericarditis
amyloid heart disease
ihss
endocarditis
constricitve pericarditis
Constrictive pericarditis is best defined as which of the following?
a condition in which a pericardial effusion results in tamponade physiology
a condition in which the patient develops an outflow tract obstruction
a condition in which the pericardium becomes thickened and fibrotic
none of the above
a condition in which the pericardium becomes thickened and fibrotic
The best way to differentiate constrictive pericarditis from restrictive cardiomyopathy is by determining if respiratory variation is present.
True
False
True
Which of the following does not present the possibility for development of constrictive pericarditis?
cardiac surgery
Viral infection
Bacterial infection
Aortic dissection
Aortic dissection
Pulsed-wave Doppler evidence of cardiac tamponade includes:
Systolic flow reversal in the pulmonary veins
Systolic flow reversal in the hepatic veins
Inspiratory increase in peak velocity across the mitral valve with an inspiratory decrease in the tricuspid valve
Inspiratory decrease in peak velocity across the mitral valve with an inspiratory increase in peak velocity across the tricuspid valve
Inspiratory decrease in peak velocity across the mitral valve with an inspiratory increase in peak velocity across the tricuspid valve
One of the physical findings seen in constrictive pericarditis is Kussmaul's sign. Which of the following is the correct definition?
Severe shortness of breath
A paradoxical rise in venous pressure with distension of the jugular veins during inspiration
A loud murmur caused from a stiff pericarium
Dissassociation between intrathoracic pressure and intracardiac pressures
A paradoxical rise in venous pressure with distension of the jugular veins during inspiration
A 68 year old woman presents with a two month history of increasing dyspnea, chest pain and decreased exercise tolerance. Her past medical history is remarkable for rheumatoid arthritis, HTN and a coronary bypass 10 years ago. BP is 138/86, HR, 88 and respirations 14/min. On inspiration, a friction rub is noted. Echo reveals normal LV size and function, no significant pericardial effusion. Doppler shows a restrictive physiology, but respiratory variation is noted with the use of a respirometer. What is the most likely diagnosis in this patient?
Pericardial tamponade
Constrictive pericarditis
Restrictive cardiomyopathy
Dilated cardiomyopathy
Hypertensive heart disease
Constrictive pericarditis
A pericardial effusion that is composed of several separate compartments of fluid would be correctly described as which of the following?
loculated
complex
simple
purulent
loculated
Pericardial brightness by echocardiography is diagnostic for pericardial disease.
True
False
False
What would be a primary concern for the patient with pericarditis in the photo above?
developing a pleural effusion
myocardial infarction
developing tamponade
developing an outflow tract obstruction
developing tamponade
A 45 year old patient comes to the lab as a referral from his doctor. He has had elevated blood pressure that has not responded to traditional medications. When performing his echo, you attempt to CW the MV to evaluate for any MR. You get the resulting waveform. What do we see here?
Artifact with mitral regurgitation
Mid cavity obstruction
LVOT outflow waveform
LVOT obstruction
Mid cavity obstruction
According to the AHA, Stage 1 hypertension is defined as:
130/80
140/90
150/95
Over 100mmHg diastolic pressure
130/80
You bring your patient back to the exam room. Upon taking his blood pressure, you note it is 155/92. You become concerned and check his chart and see his blood pressure has been elevated for at least 5 years. Even before scanning, we would expect to see:
Aortic valve sclerosis due to high blood pressure
Elevated aortic valve velocities
Increased LV wall thickness
Significant MR
Increased LV wall thickness
The first line therapy to treat hypertensive heart disease is to reduce the afterload the heart has to pump against. This is initially achieved by:
Statins only
Beta blocker and diuretics
Vasoconstricting medications
Warfarin/heparin
Beta blocker and diuretics
LV mass is an important indicator of disease prognosis with hypertensive heart disease. We can obtain this value 2 ways:
PLAX LV dimensions and automated LV quantification programs
automated LV quantification programs and tracing the LV in the apical window
Apical biplane Simpsons method of discs and PLAX LV dimensions
Apical biplane Simpsons method of discs and automated LV quantification programs
PLAX LV dimensions and automated LV quantification programs
HFpEF is a term used to describe
Diastolic dysfunction
Systolic dysfunction
Reduced EF
Hypertension
Diastolic dysfunction
Although 90-95% of systemic hypertension is idiopathic, there are many secondary reasons. Which of the following ARE NOT a secondary cause of hypertension?
Sleep apnea
Renal artery stenosis
Aortic coarctation
Coronary artery disease
Coronary artery disease
What is the final stage of hypertensive heart disease
Diastolic dysfunction
LV Failure and dilation
Systolic dysfunction
Severe coronary artery disease
LV Failure and dilation
Severe pulmonary hypertension by echocardiography is considered
40-69mmHg
>120mmHg
>70mmHg
>75mmHg
>70mmHg
Although hypertensive heart disease has deleterious effect on the heart, hypertension can cause serious systemic pathologies. Which of the following is an immediate, not a complication of hypertension?
Stroke
Dissection
Aortic dilatation
Reduced cardiac output
Reduced cardiac output
You go to the emergency department to scan a recent arrival. Before leaving you note he had a positive DVT study earlier in the week. Upon entering the room you observe he is significantly short of breath with O2 saturations in the mid 80's. While scanning the apical 4 chamber, you note hyper-contractility of the RV apex (apical wink). Based on these findings, you would expect this patient has experienced a/an
Acute on chronic pulmonary hypertension
Stroke
Pulmonary embolism
Asthma attack
Pulmonary embolism
Pulmonary hypertensive heart disease can be caused by left sided pathology, such as mitral stenosis or aortic insufficiency.
True
False
True
One way to treat pulmonary hypertensive heart disease is to give the patient:
Beta blockers
Warfarin
Vasodilators
Antiarrythmic medications
Vasodilators
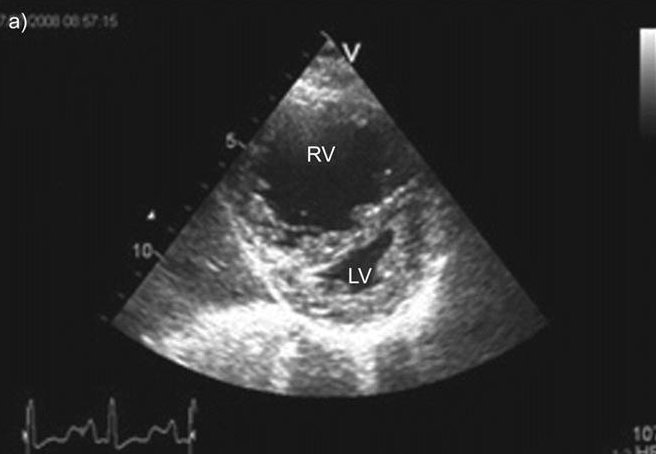
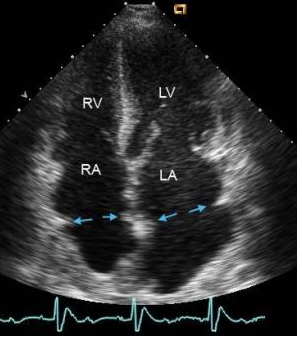
You scan a patient and in the PSAX view we see this image in both systole and diastole. We would expect this patient to be experiencing
Tricuspid stenosis
RVH
Volume overload
Pressure overload
Pressure overload
With pulmonary hypertensive heart disease, the vessels in the lungs harden and are unable to dilate. Due to the stiffness of these vessels we see that the RVOT spectral Doppler exhibits changes. This change is described as:
Longer acceleration time
Flow reversal
Mid systolic notching
Severe PR
Mid systolic notching
Although we can measure RVSP by echocardiography using TR, what measurement of pulmonic flow do we use to evaluate mean pulmonary artery pressure (MPAP)?
PR peak velocity
PR end diastolic velocity
PR VTI
PR acceleration time
PR peak velocity
The ASE defines normal RV basal (or annular) dimension as:
<25mm
15-25mm
30-40mm
25-41 mm
25-41 mm
All of the following are causes of pulmonary hyptertensive heart disease through parenchymal disorders EXCEPT:
Lupus
COPD
Obesity
Emphysema
Obesity
A patient that is short of breath comes to the echo lab for an echocardiogram. The peak TR velocity is 4 m/s with an IVC that measures 2.8cm and does not collapse with a "sniff". You would calculate the RVSP as:
116mmHg
100mmHg
79mmHg
89mmHg
79mmHg
A 41-year-old female presents with a history of an ASD Shunt. The right ventricle demonstrates characteristics of pressure and volume overload. There is a right-to-left shunt noted at the atrial level. Which of the following is the most likely cause of these findings
Ebstein anomaly
Eisenmenger physiology
Endocarditis
Rheumatic heart disease
Eisenmenger physiology
A 44-year-old male presents with dyspnea, no history of smoking or cardiac disease and significantly increased pulmonary artery pressures. The most likely explanation is
Tricuspid regurgitation
Pulmonary regurgitation
Grade 1 Diastolic dysfunction
Primary pulmonary hypertension
Primary pulmonary hypertension
This aortic valve M-mode is consistent with which of the following?
Bicuspid aortic valve
Mid-systolic closure of the aortic valve
Premature opening of the aortic valve
Eccentric closure of the aortic valve
Mid-systolic closure of the aortic valve
The most serious complication that could arise from undiagnosed hypertrophic obstructive cardiomyopathy is which of the following?
hypertension
sudden death
syncope
dyspnea with exertion
sudden death
The progressive replacement of RV myocardium with fatty and fibrous tissue is called:
HCM
ARVD
IHSS
Sarcoidosis
ARVD
A common late complication associated with dilated cardiomyopathy is:
Infective endocarditis
Aortic Regurgitation
Systemic emboli
Ventricular gallop
Systemic emboli
Hypertrophic cardiomyopathy is considered obstructive when the gradient reaches
>25mmHg with valsalva
>25mmHg
>30mmHg
>35mmHg
>30mmHg
Cardiomyopathies are divided into which of the following categories, based on physiologic characteristics?
restrictive, hypertrophic, dilated
constrictive, restrictive, hypertrophic
hypertrophic, dilated, symmetric
symmetric, restrictive, dilated
restrictive, hypertrophic, dilated
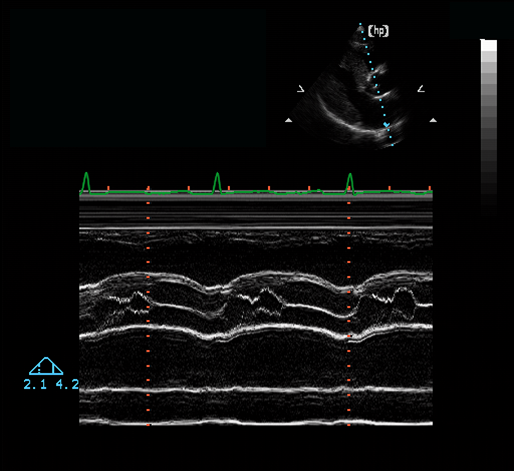
A mitral valve E-point to septal separation of 4.0 cm is an indication of:
Severe dilatation of the left ventricle
Mild left ventricular dilatatoin
Normal LV size
None of the above
Severe dilatation of the left ventricle
Amyloidosis will most likely result in the development of which of the following types of cardiomyopathy?
restrictive cardiomyopathy
dilated cardiomyopathy
hypertrophic cardiomyopathy
amyloidosis probably will not cause cardiomyopathy
restrictive cardiomyopathy
Eddie is a 85 year old male in for a follow-up echocardiogram. His previous echo noted a dilated left atrium at 56ml/m2 and a right atrial volume of 108ml. Diastolic dysfunction was grade III with noted left ventricular hypertrophy. His current echo still shows dilated atria, but now both ventricles are dilated with thin walls. His EF is now reported as 25%.
Eddie likely has ___________ that has progressed to end stage and now looks like _____________.
Restrictive/infiltrative cardiomyopathy
Restrictive/dilated cardiomyopathy
Dilated/restrictive cardiomyopathy
Hypertrophic/dilated cardiomyopathy
Restrictive/dilated cardiomyopathy
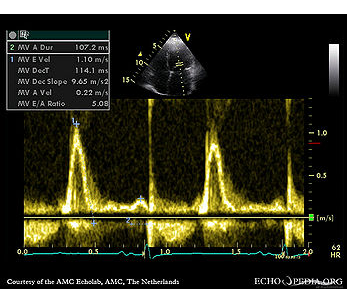
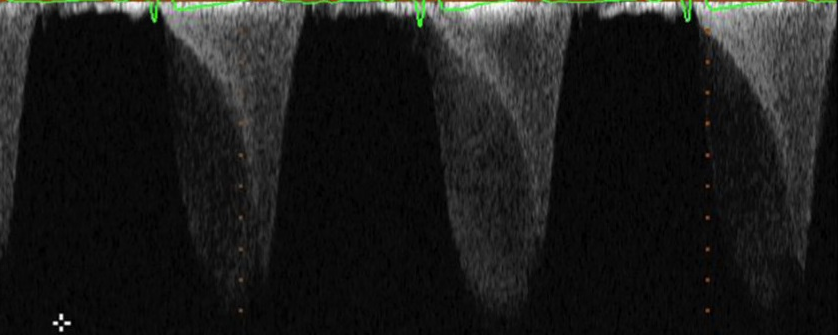
This Doppler inflow image of the mitral valve is consistent with:
Restrictive physiology
Dilated cardiomyopathy
Hypertrophic cardiomypathy
Pericarditis
Restrictive physiology
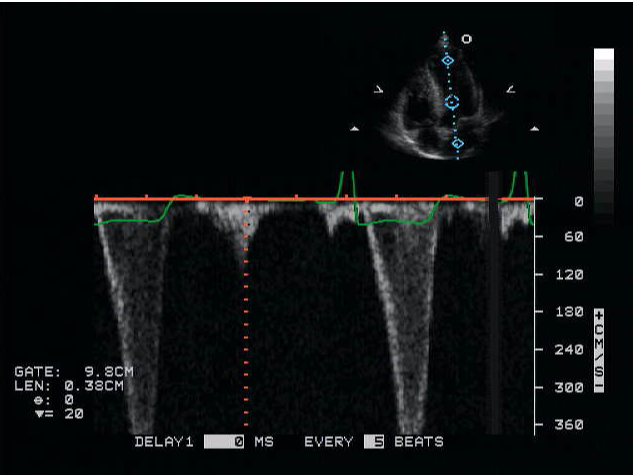
This image was obtained by using which type of Doppler?
Continuous wave
High PRF
Pedoff
None of the above
High PRF
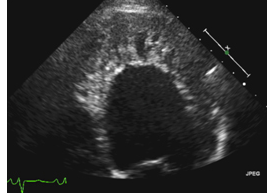
This image is an example of:
Dilated Cardiomyopathy
Restrictive cardiomyopathy
Noncompaction cardiomyopathy
Hypertrophic cardiomyopathy
Noncompaction cardiomyopathy
Carcinoid is a disease that primarily affects which valve?
Tricuspid
Mitral
Aortic
Pulmonic
Tricuspid

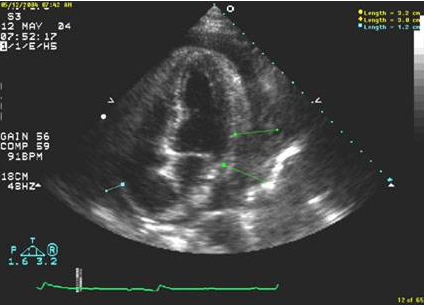
The image above is a parasternal long axis view and MOST likely represets which of the following pathologies?
dilated cardiomyopathy
hypertrophic cardiomyopathy
hypertrophic obstructive cardiomyopathy
restrictive cardiomyopathy
dilated cardiomyopathy
The patient in the apical echocardiographic view above is a 20 year old male with a history of unexplained deaths due to cardiac arrest in his family. He has no history of hypertension. What is the most likely diagnosis?
constricitve pericarditis
restrictive cardiomyopathy
dilated cardiomyopathy
hypertrophic cardiomyopathy
hypertrophic cardiomyopathy
Echocardiographic signs of outflow tract obstruction in hypertrophic cardiomyopathy include all of the following except which?
assymetric septal hypertrophy
left ventricular dilation
systolic anterior motion of the mitral valve
high systolic velocity in the left ventricular outflow tract
left ventricular dilation
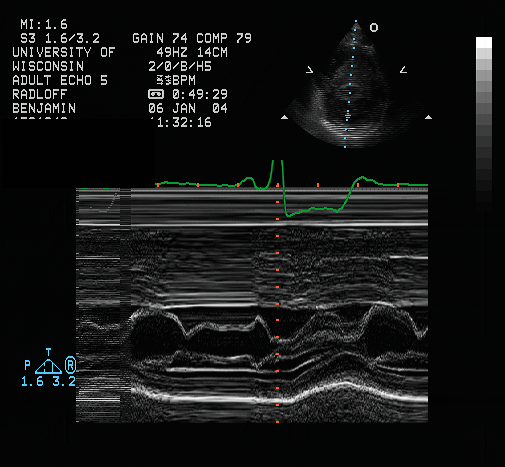
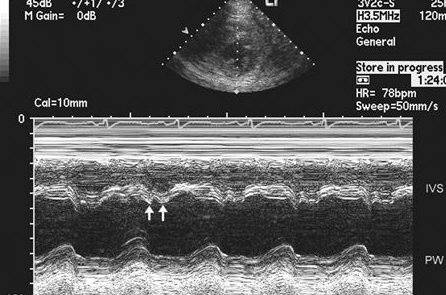
The M-Mode tracing above was done at the level of the mitral valve leaflets in the parasternal short axis on a patient that has documented hypertrophic cardiomyopathy. What critical finding does this M-Mode illustrate?
aortic valve flutter
increased A wave inflow
systolic anterior mitral leaflet motion
systolic posterior mitral leaflet motion
systolic anterior mitral leaflet motion
Asymmetric septal hypertrophy (ASH) is associated with which of the following myopathies.
Dilated
Restrictive
Hypertrophic
None of the above
Hypertrophic
Stress Echo can provoke LVOTO
True
False
True
Which of the following is strongly associated with Syncope
left ventricle outflow obstruction
VSD
rheumatic fever
Did Josie cover this?
both A and D
both A and D
When performing an echocardiogram on a patient with an LVAD, we want to evaluate the frequency of AV opening. This is best accomplished by:
Observe blood flow through the valve with color Doppler
Use Definity or another UCA (ultrasound contrast agent)
Pulsed Doppler of the LVOT in the apical view
Using a low sweep speed with M-mode imaging in the PLAX view
Using a low sweep speed with M-mode imaging in the PLAX view
You are scanning a patient and notice an odd portion of the image in the apical 4 chamber atria. What could it be?
Grating lobe artifact
Transplant suture lines
Thrombus
This is an image of normal atria
Transplant suture lines
There are 2 main categories of heart transplants, orthotopic and heterotopic. A heterotopic heart transplant refers to:
The native heart is removed and replaced with an total artificial heart
A genetically similar heart is taken from an animal and replaces native heart
Native heart is removed, donor heart placed back into chest cavity
Donor heart is "piggybacked" onto a native heart
Donor heart is "piggybacked" onto a native heart
A common hemodynamic condition seen with transplanted hearts is:
Pulmonic regurgitation
Aortic regurgitation
Tricuspid stenosis
Tricuspid regurgitation
Tricuspid regurgitation
Why is dobutamine stress echocardiography used when evaluating post-transplant patients?
Due to deinnervation, the heart has a delayed response to exercise
Posttransplant patients typically cannot exercise well
Due to deinnervation, the heart has no response to exercise
Due to pretransplant cardiac conditions, we do not want to exercise them posttransplant
Due to deinnervation, the heart has a delayed response to exercise
A common early postoperative complication after heart transplant is
Anastomotic stenosis/scarring
Anastomotic leak
Pericardial effusion
Diastolic dysfunction
Pericardial effusion
Although we serially evaluate a transplanted heart for any changes with echocardiography, patient will also have serial:
Anti rejection blood concentration tests
RV biopsies
Cardiac catheterizations to evaluate left sided heart pressures
Exercise stress echos
RV biopsies
A RAMP study is used to evaluate and optimize:
VAD power consumption
VAD function
VAD speed settings
The patients mean arterial pressure (MAP)
VAD speed settings
The inflow cannula of an LVAD is placed at the:
Atrial appendage
Ascending aorta
Lateral wall
Apex
Apex
A patient with a transplanted heart may not feel any pain during a severe heart attack.
True
False
True
VADs are only used to support the failing left ventricle
True
False
False
For a patient waiting for a heart transplant, their placement of a VAD would be considered:
Destination therapy
Bridge to transplant
Permanent
Medically necessary
Bridge to transplant
Although patients with VADs are anticoagulated, ___________ remains a serious complication.
Exercise
Electrical shorts
Thrombosis
Lack of electrical outlets
Thrombosis
During a heart transplant, what important nerve connection is severed?
Vagus
Sciatic
Median
Subcostal
Vagus
With a properly adjusted LVAD, we will not be able to use the LVOT VTI to calculate the cardiac output as the aortic valve only opens intermittently. What is the most common way to evaluate cardiac output in these patients?
RVOT VTI and diameter
PV VTI and RVOT diameter
Mitral valve inflow VTI and LVOT diameter
TR peak velocity + RAP
RVOT VTI and diameter
A patient arrives to the cardiac ICU presenting with acute shock and are expected to recover with few days. However, their cardiac output is reduced with an estimated EF of 25%. We would typically see a/an ________used.
LVAD
RVAD
IABP
Impella
Impella
When performing a dobutamine stress echo on a patient with a heart transplant, if the target heart rate is not achieved, atropine can be used to augment the heart rate.
True
False
False
Aortic coarctation occurs most commonly near the ductus
True
False
True
There are how many different locations for VSD?
4
7
3
5
5