CH 24 ADAPTIVE IMMUNITY
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
What is the difference between adaptive and innate immunity?
Innate immunity: first line of defense, works immediately, non-specific (doesn’t target a specific pathogen)
Adaptive immunity: THIRD LINE. slower, develops after exposure, highly specific to the pathogen, creates memory for faster future response
👉 Innate = instant general defense; Adaptive = learned, specific defense.
Differentiate humoral from cell-mediated immunity.
Humoral immunity: involves B cells → become plasma cells and memory cells → plasma cells make antibodies (IgA, IgG..)→ fight extracellular pathogens (outside cells)
Cell-mediated immunity: involves T cells → become cytotoxic T cells (kill infected cells) or T helper cells(activate other immune cells) → fight intracellular pathogens (inside cells)
👉 B cells make antibodies; T cells kill infected cells and help other immune cells.
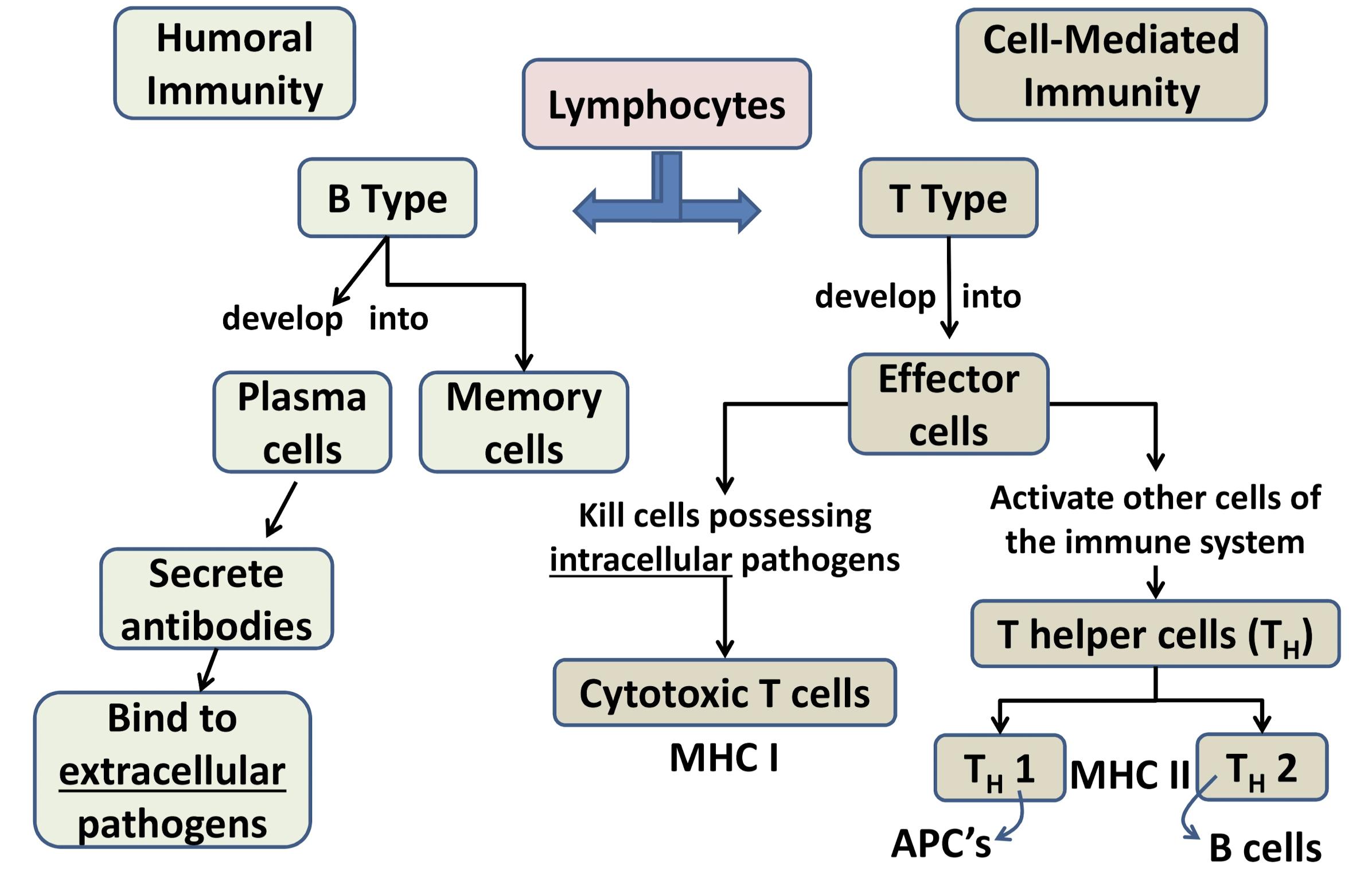
Which T helper cell recognizes APCs like macrophages and dendritic cells?
T helper 1
Which T helper cell recognizes B cells?
T helper 2
Define antigen. What type of molecules can they be?
- a molecule in the body that triggers the immune system
- can be a protein, lipid, nucleic acid, or complex carb
cause antibodies to be made
a molecule that triggers the immune system to respond
Can be: proteins, lipids, nucleic acids, or complex carbohydrates
👉 Antigen = anything the immune system can recognize as “foreign.”
Which molecule acts as the best antigen and why?
Proteins → most diversity in shape → immune system can recognize many different ones
How do B cells and T cells interact with antigens?
B cells: use antibodies on their surface to bind antigens directly
T cells: use T cell receptors to bind antigens presented by MHC molecules
👉B cells grab antigens themselves; T cells need help from MHC “presentation.”
What is an epitope?
epitopes on antigen
The specific part of an antigen that an antibody or T cell receptor binds to
can be made of: Proteins, Peptides (small pieces of proteins), Complex sugars (polysaccharides)
When your immune system detects an epitope, it triggers an immune response.
👉 Epitope = “target spot” on an antigen.
What is the function of an antibody?
Recognize antigens
Trigger immune responses like phagocytosis, complement activation, and neutralization
👉 Antibodies = immune system’s “flags” to attack invaders.
Describe an antibody’s structure.
Shape = Y
Chains: 2 heavy (long, inside) + 2 light (short, outside)
Variable region: top of Y, binds antigen
Constant region: bottom of Y, binds host cell receptors
👉 Antibody = Y-shaped flag: top grabs invader, bottom signals immune cells.
Where is the antigen-binding site on an antibody?
Located on variable regions (two tops of Y)
👉 Top tips of the Y = grab the target.
How do variable regions differ across antibodies?
Different amino acid sequences → bind different epitopes/antigens
👉 Each antibody top is unique to its target.
Which part of the antibody binds to host cell receptors?
Stem of heavy chain constant region (bottom of Y)
👉 Bottom of Y = connects to immune system.
Host cell receptors = proteins on your cells that pathogens can attach to in order to infect you. They act like "locks," and pathogens have the "keys."
What are the five classes of antibodies?
IgG
IgA
IgM
IgD
IgE
Which three antibody classes are in a monomer form? Which two form polymers?
- IgG, IgD, and IgE are monomers form
- IgA and IgM form polymers (2 or more monomers)
What is an antibody isotype?
Antibodies have a constant region on their heavy chains.
If the amino acid sequence in this constant region is different, the antibody is a different class.
Isotype tells us:
➡ Which antibody class it is:
IgG
IgA
IgM
IgD
IgE
Based on constant region differences.
What is an antibody idiotype?
Idiotype = what antigen the antibody binds.
What it means:
Two antibodies can have the same constant region (so they are the same class).
But if the antigen-binding sites (the variable regions) are different, they will bind different epitopes.
Based on variable region differences.
Tells you: what exact epitope the antibody binds.
Characteristics of IgG antibody
Monomer form (single Y)
Most abundant in blood and tissues @ 75%
Functions: opsonization (tagging), complement activation, virus neutralization
👉 IgG = main antibody in blood, tags invaders for attack.
Characteristics of IgA antibody
Dimer form (two Ys joined) 15%
Found in mucosal surfaces (saliva, mucus, breast milk)
Functions: neutralize pathogens at surfaces and prevent pathogen attachment
👉 IgA = guards surfaces like mouth, nose, and gut.
Characteristics of IgM antibody
Pentamer form (5 Ys linked) 10%
Usually stays in blood vessels
First antibody produced in immune response
Effective at clumping pathogens (agglutination) and activating complement
👉 IgM = first responder, clumps germs together.
Characteristics of IgD antibody
Monomer form (single Y) 0.2%
Only binds antigen when attached to a B cell
Found in blood and lymph
👉 IgD = antenna on B cells to detect invaders.
Characteristics of IgE antibody
Monomer form (single Y) 0.2%
Binds antigen when attached to mast cells or basophils
Causes release of histamine → allergy symptoms
Can attract complement proteins and phagocytes
👉 IgE = antenna on mast or basophil triggers allergies and fights parasites.
Five outcomes of antigen-antibody reaction
Agglutination: clumps bacteria together, reduce number of infectious units
Opsonization: coats pathogens to help phagocytes eat them, surrounds the bad
Neutralization: covers pathogen so it can’t infect cells, makes it look spiky so can’t land
Complement activation: triggers inflammation & lysis, drills hole then bursts
ADCC (Antibody-Dependent Cell-Mediated Cytotoxicity): antibodies guide NK cells to kill big parasites, uses macrophage and eosinophils, and NK cells to target cell
Q: What is the humoral immune response and their B cells?
a part of the immune system where B cells make antibodies to fight germs outside cells
most effective against extracellular pathogens
because microbes have many small parts called epitopes, and each B cell recognizes only one epitope—B cells need the help of T helper cells (T dependent antigen)
→The B cell shows the germ piece to the T helper cell using MHC Class II, and the T cell gives the B cell a “go make antibodies!” signal.
Define clonal selection
making B cell babies
B cells that match a specific antigen multiply → make more identical B cells
Some become memory cells (long-term)
Some become plasma cells (antibody factories)
👉 Matching B cells make copies to fight the invader now and later.
with the perfect match, the b-cel will make babies that will then differeiate to plasma or memory
Describe the process of clonal selection.
when a B cell with an antibody binds to its matching antigen, this triggers clonal selection and expansion
this specific B cell and antibody combo will now go through lots of mitosis to make many clones of itself
some of these clones will differentiate into memory B cells and some will differentiate into plasma cells
Difference between plasma and memory B cells
Plasma B cells: secrete antibodies during active infection
Memory B cells: hang around for long-term immunity → respond quickly if antigen comes back
👉 Plasma = fights now; Memory = remembers for later.
Compare and contrast T-dependent and T-independent antigens.
T-dependent:
binds to the B cell, required
T helper 2 cell recognizes antigen on MHC II → activates B cell
B cell goes through clonal selection → makes plasma & memory B cells
T-independent:
not required by B cells
large antigens cluster the B cell
Difference between primary and secondary immune response
Primary Response (first time you see the pathogen):
Happens after the first infection or first vaccine
Slow – antibodies take several days to appear
Starts with IgM first, then switches to IgG
B cells become:
Plasma cells (make antibodies)
Memory B cells (saved for next time)
Secondary Response (second exposure or booster shot):
Triggered by memory B cells
Very fast and much stronger
Mostly IgG made
This is the reason vaccines work (booster = bigger response)
Which MHC class do cytotoxic T cells recognize? Which co-receptor do they use (CD4 or CD8)?
MHC I
they use CD8
Which MHC class do helper T cells recognize? Which co-receptor do they use (CD4 or CD8)?
MHC II
they use CD4
Where does the cell-mediated immunity happen?
it uses T cells, recognizing antigens infected with intercellular pathogens
What is the function of T helper cells?
Activate macrophages, dendritic cells, and B cells.
Cause release of cytokines to direct immune response.
👉 T helpers are “immune coaches,” telling cells how to fight.
What is the function of cytotoxic T cells?
Recognize intracellular antigens (from viruses, bacteria inside cells, or cancer cells).
Via MHC I and CD8 co receptor
Kill these infected or abnormal cells by releasing:
Perforins → make holes in the target cell’s membrane.
Granzymes → enter cell and trigger apoptosis (programmed cell death).
Result: the infected cell is destroyed, stopping the infection.
👉Cytotoxic T cells = “cell assassins,” killing infected cells.
What is the function of T helper 1 cells?
Recognize antigens presented by dendritic cells and macrophages (APCs).
Via MHC II and CD4 co recep
Release cytokines to:
Activate these APCs
Promote complement activation
Stimulate inflammation
Help opsonization
Help cytotoxic T cell differentiation
👉 boosts attack on infected cells and inflammation.
What is the function of T helper 2 cells?
Recognize antigens presented by B cells.
Via MHC II and CD4 co recep
Release cytokines to:
Stimulate B cells to make antibodies
Focuses on humoral (antibody) immunity, especially against extracellular pathogens.
👉helps B cells make antibodies
How are T helper cells and cytotoxic T cells different from each other?
T helper cells: do not kill. They activate other immune cells like B cells, macrophages, and dendritic cells.
Cytotoxic T cells: can kill infected or cancerous cells directly to cause lysis or apoptosis.
Define antigen-presenting cell (APC).
Immune cell that processes antigens and displays them on MHC II molecules.
Purpose: activates T helper cells to start the adaptive immune response.
Examples: macrophages, dendritic cells, B cells.
👉 APC = “flag bearer” showing antigens to T helper cells.
What is the role of natural killer (NK) cells in antibody-dependent cell-mediated cytotoxicity (ADCC)?
Bind to antibody-coated target cells.
Release cytotoxic granules containing:
Perforins → make holes in target cell membrane
Granzymes → trigger apoptosis
Purpose: destroy large targets (like virus-infected cells or parasites) flagged by antibodies.
List and describe the four types of adaptive immunity.
Active natural: body encounters antigen naturally → makes antibodies
Ex: getting COVID
Passive natural: antibodies pass from mother to child
Ex: through placenta or breastfeeding
Active artificial: vaccines give antigens → body makes antibodies
Ex: flu shot
Passive artificial: inject pre-made antibodies
Ex: antivenom or immunoglobulin therapy
👉 Super simple: Active = body makes antibodies; Passive = gets antibodies from outside.
Do vaccines provoke a primary or secondary immune response?
Vaccines cause a primary immune response first (slow, initial antibody production).
Memory B cells are formed → next exposure triggers secondary response (faster, stronger, mostly IgG).
Define herd immunity
Most of a population is immune, so disease spreads slowly or not at all.
👉 Herd immunity = “group protection.”
Define R0 value.
Average number of people one sick person infects in a susceptible population.
👉 R0 = “contagion score.”
Why are disease outbreaks sporadic?
Not everyone is susceptible, so outbreaks stop when few susceptible hosts remain.
⭐ Front: Define and describe live attenuated vaccines.
Back:
Vaccine uses a weakened pathogen (virus or bacteria)
Still has antigens and can replicate a little in the host
Weakened by:
Mutating virulence genes
Growing in cell culture or non-human host
Advantages:
Mimics natural infection closely
Strong, long-lasting immunity (both cellular and humoral)
Example: Measles, Mumps, Rubella (MMR)
👉 Super simple: Live vaccine = “tiny live germ” that trains immune system.
⭐ Front: Define and describe inactivated (killed) vaccines.
Back:
Vaccine uses dead pathogen
Cannot replicate in host
Safer than live vaccines
Usually requires booster shots to maintain immunity
Mainly stimulates humoral (B cell/antibody) response
Example: Inactivated polio vaccine (IPV)
👉 Super simple: Dead vaccine = “non-living germ” teaches antibodies.
⭐ Front: Define toxoids.
Back:
Inactivated toxins produced by pathogens
Cannot cause disease, but still trains immune system to fight the toxin
Example: Tetanus vaccine
👉 Super simple: Toxoid = “neutralized poison” for immunity.
⭐ Front: Define subunit vaccines.
Back:
Use only pieces of the pathogen (antigens)
Stimulate immune response without whole germ
Example: Hepatitis B vaccine
👉 Super simple: Subunit = “just part of germ” trains immunity.
⭐ Front: Define recombinant vaccines.
Back:
Subunit vaccine made by genetic engineering
Antigens are produced by modifying DNA in lab organisms
Example: Hepatitis B recombinant vaccine
👉 Super simple: Recombinant = “lab-made germ pieces.”
⭐ Front: Define and describe virus-like particle (VLP) vaccines.
Back:
Mimic whole virus shape but no viral genome
Cannot infect cells
Present antigens to immune system
Stimulate B cells for antibody production
Example: HPV vaccine
👉 Super simple: VLP = “fake virus shell” that teaches immune system.
⭐ Front: Define and describe outer membrane vesicle (OMV) vaccines.
Back:
Made from outer membrane of bacteria
Contain pathogen antigens to stimulate immune system
Mimics the natural pathogen without causing infection
Example: Some meningococcal vaccines
👉 Super simple: OMV = “bacterial pieces” for safe training.
⭐ Front: Define and describe polysaccharide vaccines.
Back:
Made from sugar capsule of bacteria
Stimulates immune response poorly in children
Not very immunogenic by itself
Example: Pneumococcal polysaccharide vaccine
👉 Super simple: Polysaccharide = “sugar coat” of bacteria.
⭐ Front: Define and describe protein-polysaccharide conjugated vaccines.
Back:
Polysaccharide linked to a protein
Produces stronger immune response, especially in children
Example: Haemophilus influenzae type b (Hib) vaccine
👉 Super simple: Conjugate = “sugar + protein” = stronger vaccine.
⭐ Front: Define and describe nucleic acid vaccines.
Back:
DNA vaccines: inject naked DNA plasmid encoding viral antigen → host makes antigen → stimulates immune response
RNA vaccines: inject naked mRNA encoding viral antigen → host makes antigen → stimulates immune response
Stimulates both humoral (B cells) and cell-mediated (T cells) immunity
Example: Pfizer/Moderna COVID vaccines (RNA)
👉 Super simple: Nucleic acid = “DNA/RNA instructions” → body makes viral protein → trains immune system.
⭐ Front: Define and describe viral vectored/recombinant vector vaccines.
Back:
Use harmless virus or bacteria as a delivery vehicle
Carries genes that encode pathogen antigens
Vectors are genetically modified
Example: Johnson & Johnson COVID vaccine
👉 Super simple: Viral vector = “delivery truck carrying antigen genes.”
⭐ Front: What type of vaccine is Pfizer/Moderna COVID vaccine?
Back:
Nucleic acid vaccine (RNA)
RNA instructs cells to make viral spike protein
Trains immune system without infecting cells
👉 Super simple: Pfizer/Moderna = “mRNA instructions” → body makes harmless spike → immunity.
⭐ Front: What type of vaccine is Johnson & Johnson COVID vaccine?
Back:
Viral vector vaccine
Harmless virus carries gene for spike protein
Trains immune system to recognize SARS-CoV-2
👉 Super simple: J&J = “virus delivery truck” → teaches immune system.