TMOD (Choroid)
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms

Choroidal Nevus
Benign
Disappear with red-free filter
Flat, grey-brown-green spot with demarcated borders
Small fraction of nevi can become choroidal melanomas (high risk of melanoma: symptoms, close to optic nerve, change/growth, elevation, orange pigment, subretinal fluid)
Choroidal Nevus Treatment/Management
Monitor with fundus photography
FU within 3 months at first, then 1-12 months depending on risk level

Choroidal Melanoma
Most common primary intraocular malignancy in adults
Most common sites of metastasis include liver, lung, bone, skin, CNS
Dome shaped elevations may or may not be pigmented with overlying yellow/orange lipofuscin, indistinct borders, may have associated serous retinal detachment
Choroidal Melanoma Treatment/Management
Enucleated (leave EOM and orbital content) to prevent metastasis
Refer to oncologist
Choroidal Melanoma prognosis
If metastasizes, 15-45% mortality rate within 10 years
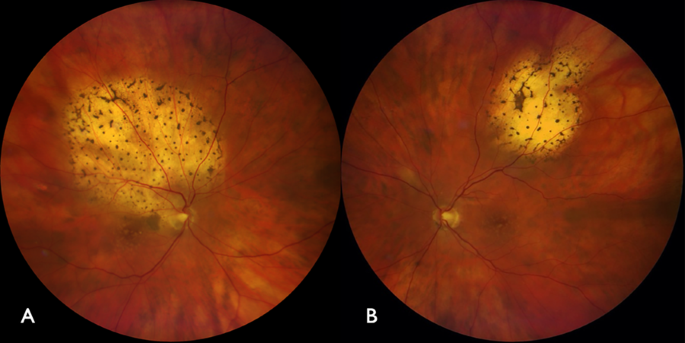
Choroidal Metastasis
Most common intraocular malignancy in adults
When cancer has spread to the eye from another place in the body (#1 primary site is breast in women, lung in men)
Yellow-white elevated lesions with pigmented clumps (leopard spots) and possible overlying serous retinal detachment
Choroidal Metastasis Treament/Management
Refer to oncologist for chemo
Choroidal Metastasis prognosis
Pt will die within 1 year of diagnosis
Choroideremia
X-linked recessive inheritance (men affected, women are carriers)
Bilateral
Presents at 20-30yo and progress to legal blindness by 50-60yo
Nyctalopia, photophobia, peripheral vision loss
Peripheral atrophy of choriocapillaris, revealing choroidal vessels and sclera, spares macula until late stage
Choroideremia Treatment/Management
No tx
Low vision consult may be beneficial

Central Areolar Choroidal Dystrophy
AD inheritance
Shows at age 30-40
Progresses to severe vision loss by 60-70
Blur and central scotoma, bilateral and symmetric, moderate protan-deutan defect
In early stage hypopigmentation of the macula that progress to geographic atrophy that slowly enlarge and show choroidal vasculature
Decrease from 20/25-20/200
Central Areolar Choroidal Dystrophy Treatment/Management
No tx
Low vision consult
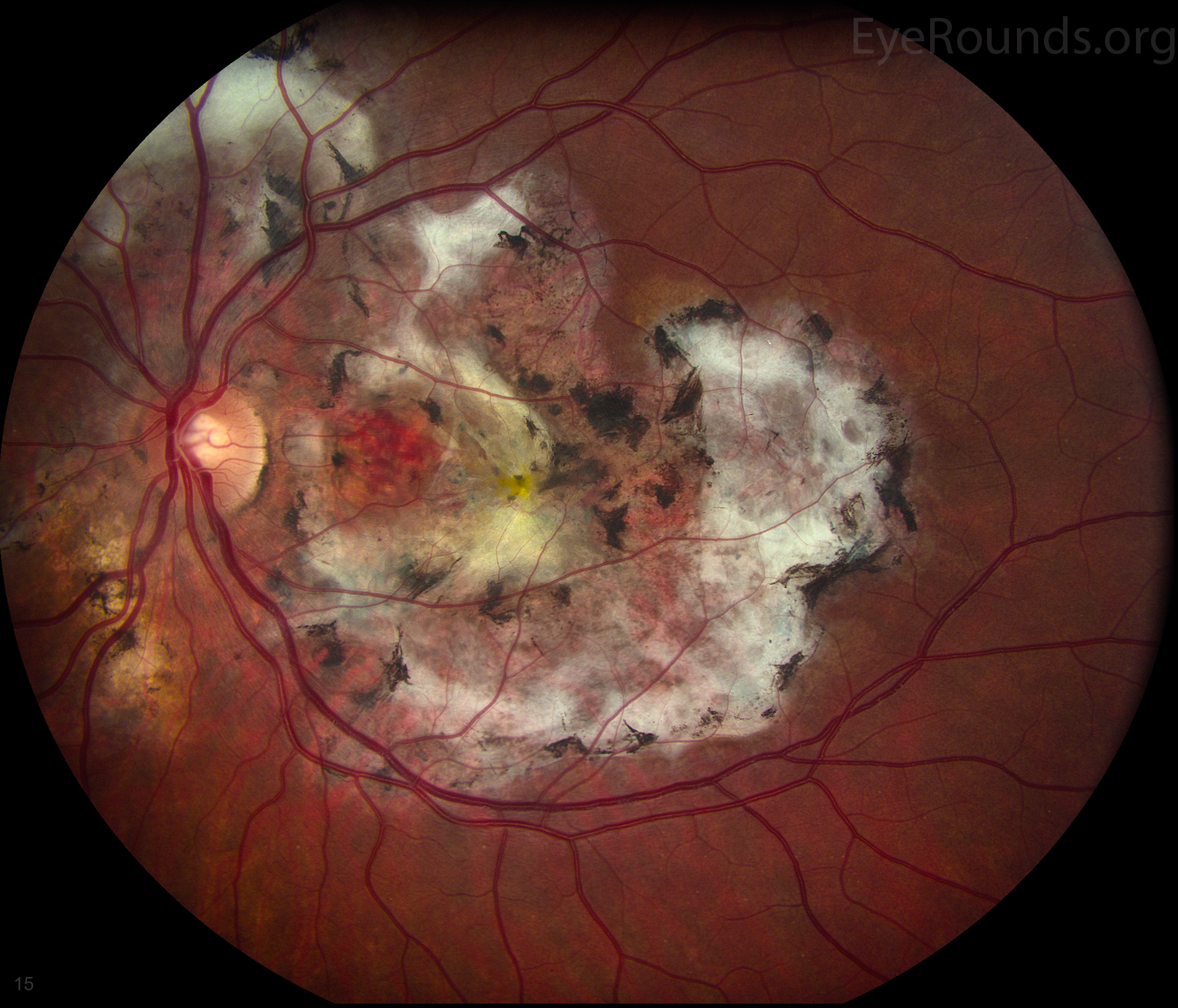
Serpiginous Choroidopathy
HLA-B7
Idiopathic in nature
Presents in 50-60yo men
Central blur, scotoma that is unilateral or bilateral, CNV
Recurrent disease that begins at the optic nerve then grows towards macula
Active - grey-white in color
Dormant - shows atrophy and scar
Serpiginous Choroidopathy Treatment/Management
Poor response to tx
If inflammation, tx with steroids (oral, sub-tenons)
If CNV, laser photocoagulation and anti-VEGF
May benefit from low vision consult
Serpiginous Chroidopathy prognosis
Poor visual outcome

Candidiasis
Fungal infection of Candida and typically seen. in IV drug abusers
Bilateral blur, pain, floaters, RD in late stage
Yellow-white choroidal lesions that progress into a hazy vitritis that looks like “cotton balls”
Candidiasis Treatment/Management
Antifungal (oral or IV)
If vitreous is involved, then do intravitreal injection or vitrectomy if mod to serever inflammation or steroids
May need to monitor daily or hospitalized if pt is noncompliant with tx
Infectious disease specialist should be consulted

Birdshot Retinochoroidopathy (Vitiliginous Chorioretinitis)
HLA-A29
White dot syndrome
Idiopathic, bilateral, chronic, recurrent
Usually seen in white females age 40-60
Floaters, blur
Presents with multiple creamy yellow-white small (1DD) spots (spares macula), mild bouts of recurrent anterior uveitis, vitritis, vasculitis, CNVM, ERM, CME
Birdshot Retinochoroidopathy (Vitiliginous Chorioretinitis) Treatment/Management
Significant inflammation, tx with steroids (oral or sub-tenons)
Vitritis or CME, tx with cyclosporine

Serous Choroidal Detachment (Choroidal Effusion)
Low IOP from puncture wound to the globe
Could also be associated with posterior scleritis, VKH syndrome, trauma, intraocular tumor
WILL transilluminate
Asymptomatic
Choroid separates from sclera (looks the same as hemorrhagic choroidal detachment
Serous Choroidal Detachment (Choroidal Effusion) Treatment/Management
Close wound with bandage CL, suture, cyanoacrylate glue
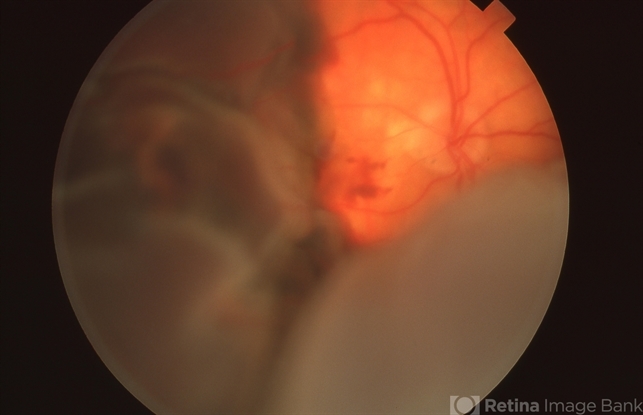
Hemorrhagic Choroidal Detachment
Increased IOP secondary to hemorrhaging during anterior segment surgery
Severe pain, red eye, rapid decreased vision
WILL NOT transilluminate
Hemorrhagic Choroidal Detachment Treatment/Management
Wound should close immediately
Sclerotomy (cutting the sclera)
Cycloplegic to prevent synechiae
Ocular hypotensives to reduce IOP