Integrative physiology (The Cardiovascular System: The Heart)
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
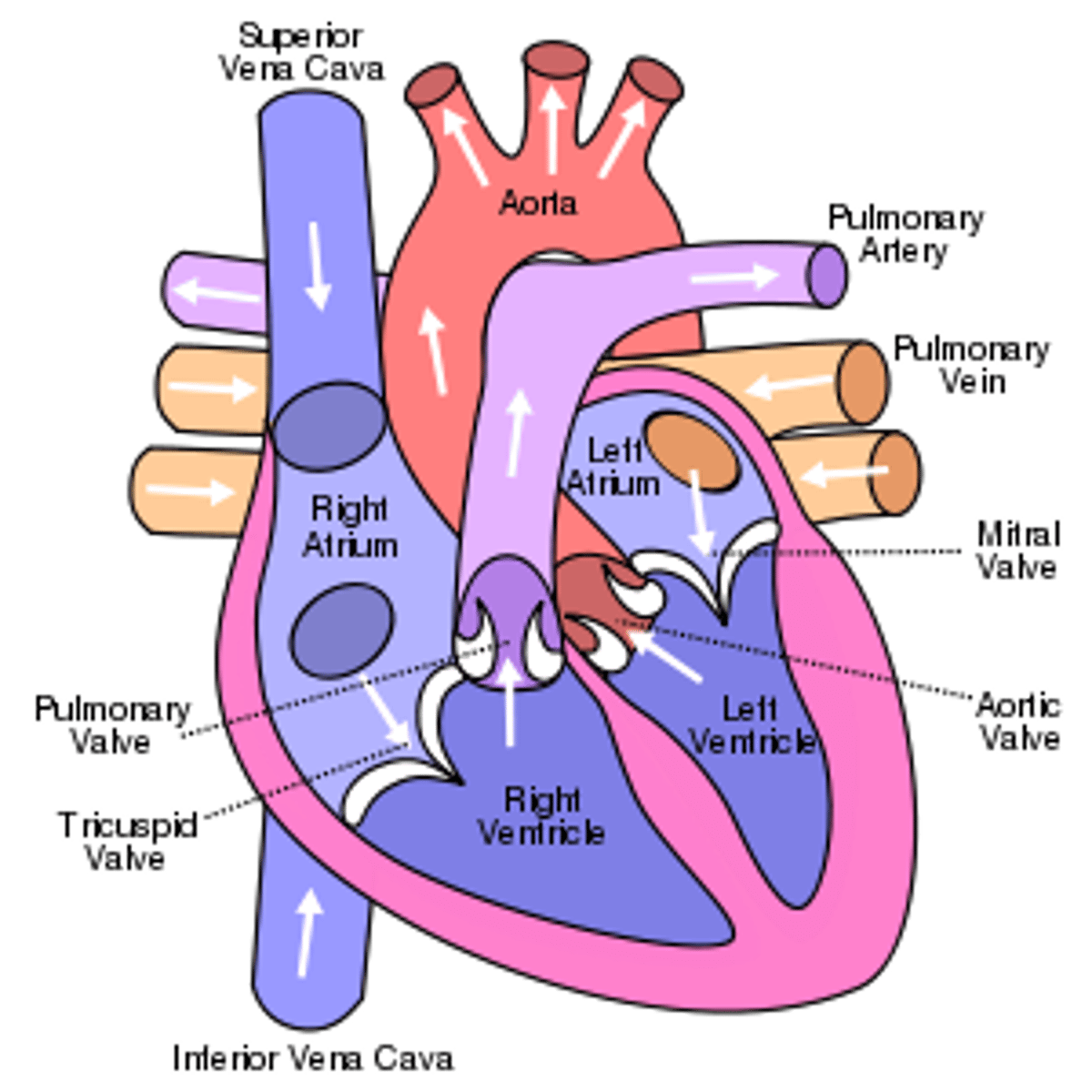
pulmonary and systemic circulation
Pulmonary circulation - for oxygenation of the blood. Right ventricle to pulmonary artery to lungs to pulmonary vein to left atrium.
Systemic circulation - to supply cells with oxygenated blood and remove waste. Left ventricle to aorta to body to vena cave to right atrium.
heart
hollow organ about the size of a fist
located in thoracic cavity
lies mostly to the left
pericardium
protects and anchors the heart
heart chambers
right atrium, right ventricle, left atrium, left ventricle
can be divided into right and left:
2 atria
2 ventricles
right side of the heart function:
serves pulmonary circuit
left side of the heart function:
serves systemic circuit
top two chambers of the heart
atria
bottom 2 chambers of the heart
ventricles
atria
great vessels leading blood to the atria
right atria contains...
superior vena cava
inferior vena cave
left atria contains...
pulmonary veins
ventricles
great vessels leading blood away from ventricles
right ventricle
pulmonary trunk
left ventricle
aorta
heart valves
ensure one way blood flow
righ heart valve
tricuspid atrioventricular valve (AV)
pulmonary semilunar valve
left heart valve
bicuspid valve antroventricular valve (AV)
aortic semilunar valve
valves have a fibrous skeleton that prevents
them from stretching
Blood flow though the heart
1. right atrium (deoxygenated blood)
2. rigth ventricle
3. pulmonary trunk and pulmonary arteries
4. in pulmonary capillaries, blood loses CO2 and gains O2
5. pulmonary veins (oxygenated blood)
6. left atrium
7. left ventricle
8. aorta and systemic arteries
9. in systemic capillaries, blood loses O2 and gains CO2
cardiac muscle tissue structure
interconnected cells act as a functional syncytium:
1. all cells depolarize and contract at the same time
2. connected via intercalated disks
conduction system functions:
- ensures coordinated contraction
- collection of modified muscle cells (pacemaker)
- initiate action potentials
- conduct action potentials to other heart cells via gap channels
- do not contribute significantly to contractile forces
conduction system process
starts at the superior wall of the rigth atrium
continues through the apex of the heart and myocardium of the ventricles
see slide 51 for visual
conduction system structures
1. sinoatrial (SA) node
2. atrioventricular (AV) node
3. antroventricular (AV) bundle: bundle of HIS
4. rigtht and left bundle branches
5. purkinje fibers
pacemaker potentials- nodal cells
during first half of pacemaker potential, voltage- gated K+ channels close and F-type Na+ channels are open; during second half of pacemaker potential, T-type voltage-gated Ca2+ channels open
1. depolarizing phase
2. repolarizing phase
nodal cells
responsible for establishing the rate of cardiac contraction
contractile cells
- produce force
- do not spontaneously depolarize
- contract in a similar fashion to skeletal muscle
- produce action potentials only in response to signals from the nodal cells
contractile cell action potential
- Rapid depolarization phase
- Initial repolarization phase
- Plateau phase
- Repolarization phase
excitation-contraction coupling
events that link the action potentials on the sarcolemma to activation of the myofilaments, thereby preparing them to contract
electrocardiogram
records electrical signals of the heart
consists of waves, intervals and segments that
can be read to provide clues for abnormalities
P wave
represents the depolarization of the atria
P-R interval
represents the AV node delay
QRS complex
represents ventricular depolarization
S-T segment
depolarized state of the ventricular muscle
T wave
represents ventricular repolarization
ECG and heart action potentials
1. depolarization of atrial contractile fibers produces P wave
2. atrial systole (contraction)
3. depolarization of ventricular contractile fibers produces QRS complex
4. ventricular systole (contraction)
5. repolarization of ventricular contractile fibers produces T wave
6. ventricular diastole (relaxation)
cardiac cycle
1. passive ventricular filling
2. atrial contraction
3. isovolumetric ventricular contraction
4. ventricular ejection
5. isovolumetric ventricular relaxation
heart sounds
first sound: S1
second sound: S2
S1
- sound of Lubb
- louder and a bit longer
- caused by vibrations associated with closure of the AV valves
S2
- sound of Dubb
- shorter and not as loud
- caused by vibrations associated with closure of the SL valves
cardiac output
the amount of blood ejected per minute
cardiac output= stroke volume (left ventricle contracting and ejecting blood) X heart rate (SA node generating an action potential)
stroke volume
Amount of blood pumped by one ventricle during a contraction
stroke volume= EDV-ESV
EDV
end diastolic volume
ESV
end systolic volume
stroke volume increases as _______ increases
EDV
EDV is affected by __________ return
venous
venous return is affected by...
- Skeletal muscle pump
- Respiratory pump
- Sympathetic innervation
force of contraction is affected by ...
- Stroke volume
- Length of muscle fiber and contractility of heart
stroke volume regulated by:
preload
contractility
afterload
contractility
inotropic agents (ex. sympathetic nervous system)
change intracellular Ca2+ concentrations
inotropic agents- effects on contractility
increase the stroke volume and EDV (increase contraction) --> positive inotropic effect
decrease the stroke volume and EDV (decrease contraction) --> negative inotropic effect
inotropic agents (positive)
increases stroke volume by increasing cardiac contraction
makes your heart muscle contractions stronger, raising your cardiac output to a normal level and increasing the amount of blood your heart can pump out. This helps your organs get the blood and oxygen they need to keep working.
agents: Dopamine, epinephrine, norepinephrine
inotropic agents (negative)
decreases stroke volume by decreasing cardiac contraction
keeps your heart muscles from working too hard by beating with less force. This is helpful when you have high blood pressure, chest pain, an abnormal heart rhythm or a disease like hypertrophic cardiomyopathy.
agents: flecainide, verapamil
autonomic regulation
Cardiovascular Control Center in brain, releases epinephrine which circulates throughout system & binds B1 receptors, increasing heart rate and contractility
sympathetic regulation
faster rate of spontaneous depolarization
1. norepinephrine attaches to receptor
2. This activates the Gs protein
3. this activates ATP from Adenylyl cyclase into cAMP
4. the cAMP binds to the F-type Na+ channel which causes the channel to stay open longer, increasing Na+ flow
5. increased rate of spontaneous depolarization of SA node cell
parasympathetic stimulation
slower rate of spontaneous depolarization
1. ACh attaches to Muscarinic receptor
2. The Gi protein is activated
3. The activation of the Gi protein opens the K+ channel, which increases the K+ flow, which hyperpolarizes the cell membrane
4. cAMP production decreases which accelerates closure of F-type Na+ channel, reducing Na+ flow
5. both the reducion in Na+ and the hyperpolarization of the cell membrane due to the increases K+ flow decreases the rate of spontaneous depolarization of SA node cell
exercise and the heart
cardio fitness can be improved at any age
aerobics
- any exercise that works a large muscle group for 20 mins or more
- after several weeks of training, maximal cardiac output increases
- training will lead to hypertrophy of the heart
- well trained individuals can have resting bradycardia
40-60 bpm