2 - Tubular Mechanisms, Renal Clearance, Micturition
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
61 Terms
How much filtrate is produced a day?
180 liters
How much urine is produced day
1-2 Liters
What type of substances are reabsorbed? (1)
Water
Good solutes – eg ions (Na+, K+, Cl-, Ca++)?
Nutrients – eg glucose, amino acids?
Waste produces – eg creatinine or urea?
Water - Yes, up to 99%
Good solutes – eg ions (Na+, K+, Cl-, Ca++)? - Yes, up to 99% Na+
Nutrients – eg glucose, amino acids? - Yes, 100%
Creatinine - None
urea? - Yes, 50%
Nutrients and waste products are not under physiological control
Basic mechanisms of tubular reabsorption (2)(1)
• Diffusion (passive)
• Mediated transport (active)
NOT bulk flow
What are the two main pathways substances use to move from the tubular lumen to the blood?
Paracellular and transcellular pathways
Paracellular pathway
Substance X moves between cells via tight junctions.
Transcellular pathway
Substance Z moves through the tubule cell, crossing both the luminal and basolateral membranes.
After passing through the tubule cell or tight junctions, where do substances go next?
Into the interstitial fluid, then into the peritubular capillary by bulk flow.
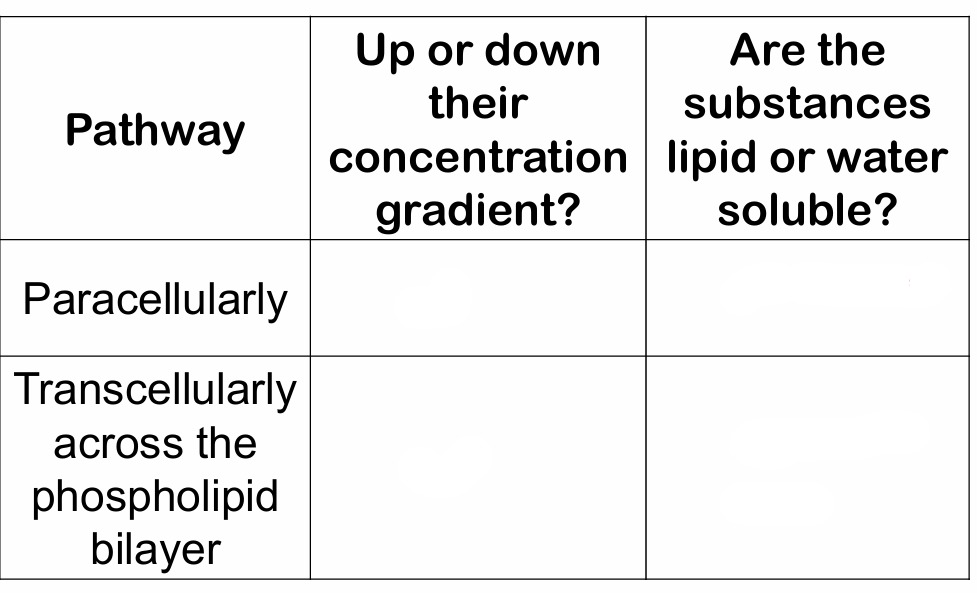
How can substances move by diffusion across the tubular epithelium?
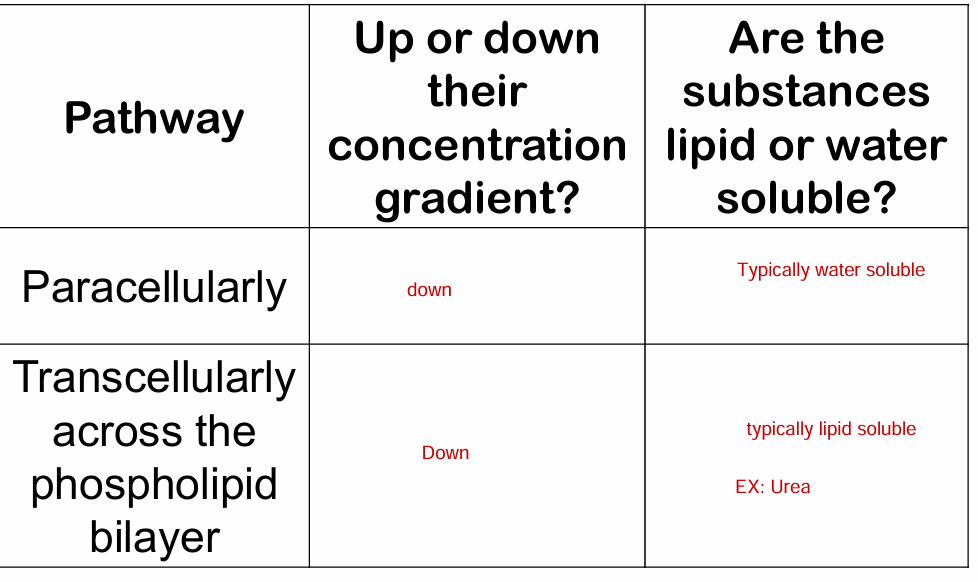
Will urea be reabsorbed under these condition?
Since concentration is the same, there will be no net movement of urea. No reabsorption
If the solute concentration is the same between the filtrate and interstitial fluid, how can there be transepithelial movement of substances by diffusion?
A concentration gradient needs to be established
This concentration gradient is established by the reabsorption of water
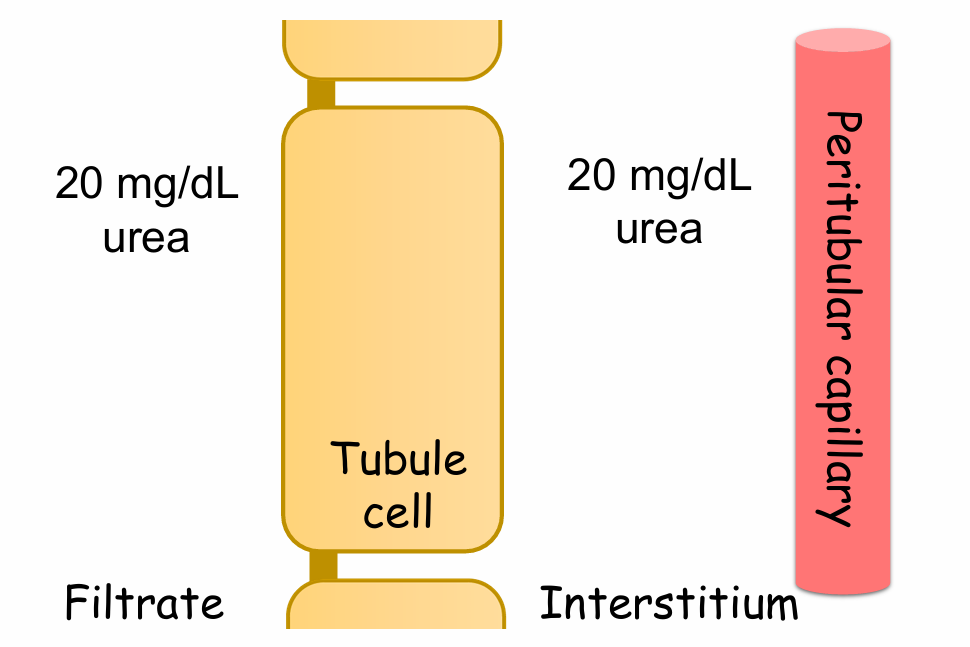
Reabsorption of urea by diffusion (5)
If there are aquaporin (water) channels on both the luminal and basolateral membranes of tubular cells, the tubular cell is permeable to water
Water moves by osmosis from the lumen, through the tubular cell, to the interstitial fluid
This causes a concentration gradient for urea.
Urea moves down its concentration gradient from the lumen, through the tubular cell, to the interstitial fluid
Water and urea then move by bulk flow from the interstitial fluid into the blood and hence both are reabsorbed
How does a ‘concentration or diffusion gradient’ for water occur????
by reabsorption of Na+ via mediated transport. Second basic mechanism of tubular reabsorption.
Mediated transport (3)
Uses energy at some point
Many substances are coupled to reabsorption of Na+ by mediated transport
Secondary active transport
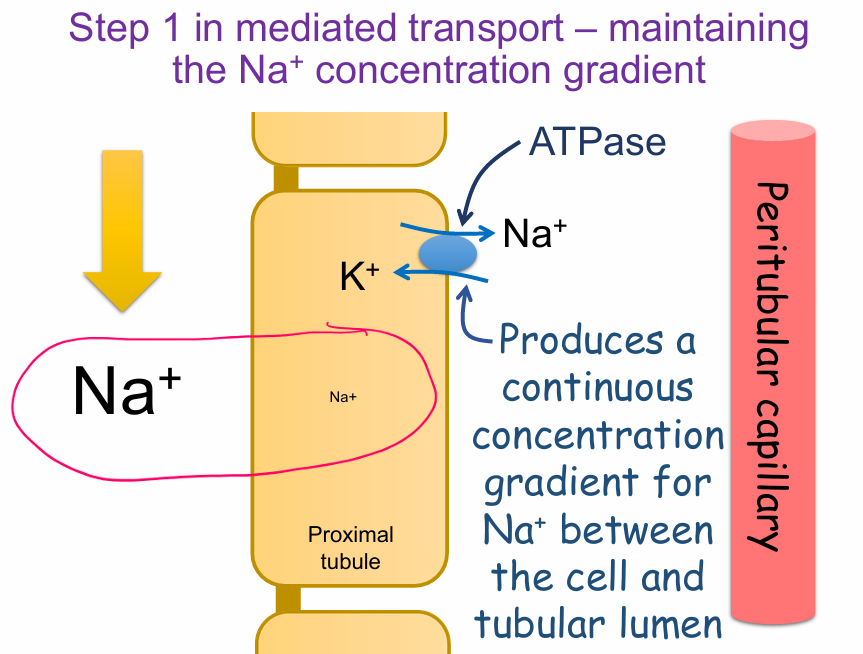
Step 1 in mediated transport (1)(5)
maintaining the Na+ concentration gradient
Na⁺/K⁺ ATPase pump uses ATP to actively transport Na⁺ out of the proximal tubule cell into the peritubular capillary.
K⁺ is transported into the cell in exchange for Na⁺.
This maintains a low intracellular Na⁺ concentration.
Creates a continuous Na⁺ concentration gradient between the tubular lumen and the cell.
This gradient drives mediated transport processes, such as Na⁺-glucose cotransport.
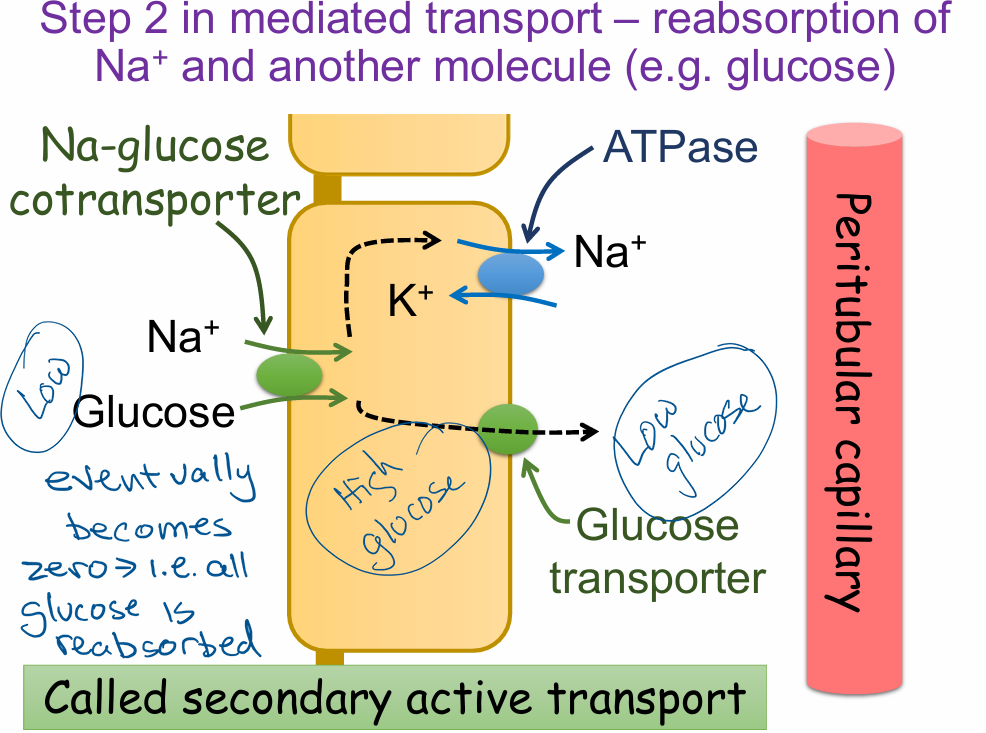
Step 2 in mediated transport (1) (7)
reabsorption of Na+ and another molecule (e.g. glucose)
Na⁺-glucose cotransporter on the apical membrane moves both Na⁺ and glucose into the cell from the tubular lumen.
Na⁺ moves down its concentration gradient, driving glucose against its gradient into the cell.
Na⁺/K⁺ ATPase pump maintains the Na⁺ gradient by exporting Na⁺ and importing K⁺.
Glucose builds up to a high concentration inside the cell.
Glucose exits into the peritubular capillary through a glucose transporter on the basolateral membrane.
Eventually, all glucose is reabsorbed from the tubular lumen.
This process is secondary active transport – it indirectly uses energy via the Na⁺ gradient.
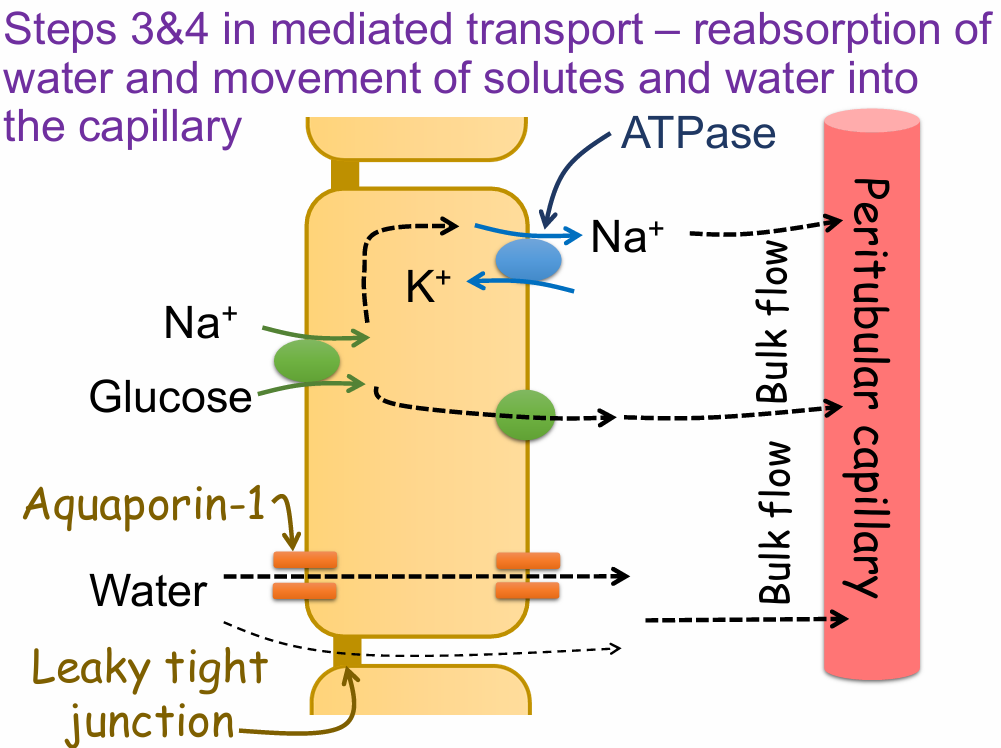
Steps 3&4 in mediated transport (1)(6)
reabsorption of water and movement of solutes and water into the capillary
After glucose and Na⁺ enter the cell, they are transported into the peritubular capillary via bulk flow.
Na⁺/K⁺ ATPase continues to maintain the Na⁺ gradient by pumping Na⁺ into the interstitial space.
Water follows solute reabsorption (especially Na⁺ and glucose) by osmosis.
Water enters through Aquaporin-1 channels in the cell membrane.
Additional water reabsorption occurs through leaky tight junctions between cells.
Solutes and water move together into the capillary via bulk flow, driven by osmotic and hydrostatic pressure.
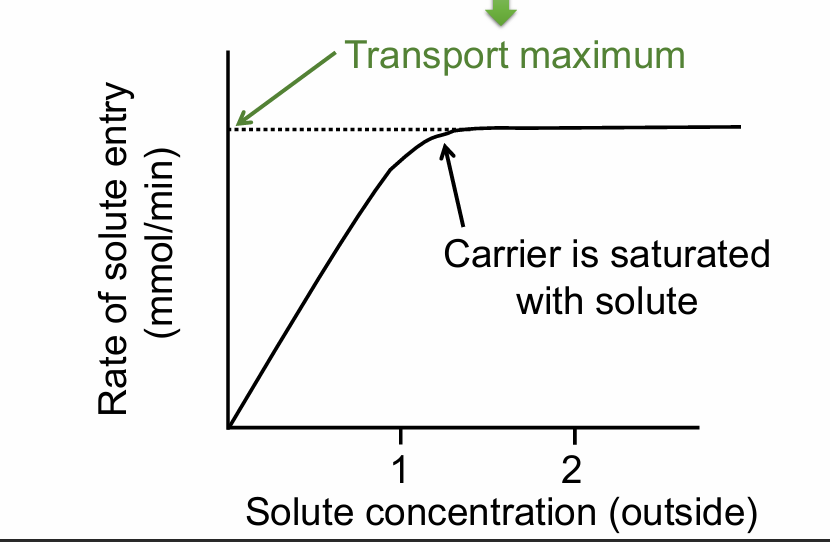
Remember with transport by carriers
There is a limit on the rate of solute entry
Because of secondary active transport, how much filtered glucose and amino acids are normally reabsorbed in the proximal tubule?
All of them
A person with diabetes mellitus has a urinalysis performed and there is glucose in their urine. How can this be????
A. Glucose is transported across the luminal membrane down its concentration gradient so there normally is glucose in the urine
B. Blood glucose levels were too high which caused the filtered load of glucose to exceed the transport maximum of the Na glucose cotransporter
B. Blood glucose levels were too high which caused the filtered load of glucose to exceed the transport maximum of the Na glucose cotransporter
Why is there net movement of water and solutes from the interstitial space to the peritubular capillary via bulk flow?
A. The Starling forces (hydrostatic and oncotic pressures) favor absorption
B. The Starling forces (hydrostatic and oncotic pressures) favor filtration
A. The Starling forces (hydrostatic and oncotic pressures) favor absorption
Only need to know starling forces in glom
In summary, what does reabsorption of Na+ accomplish?(4)(1)
Reabsorption of other solutes by facilitated transport (transcellular epithelial transport)
Glucose, Amino acid, Phosphate, Cl-
Reabsorption of water
Reabsorption of urea (because of the reabsorption of water)
Reabsorption of K+, Ca++, Cl- (because of paracellular movement of water – solvent drag)
Tubular secretion (2)
This is another way to get substances from the blood into the tubule!
Often coupled somehow with reabsorption of Na+
Renal Clearance (2)(1)
Volume of plasma cleared of a substance per unit time
VOLUME per unit TIME
Not amount that is cleared
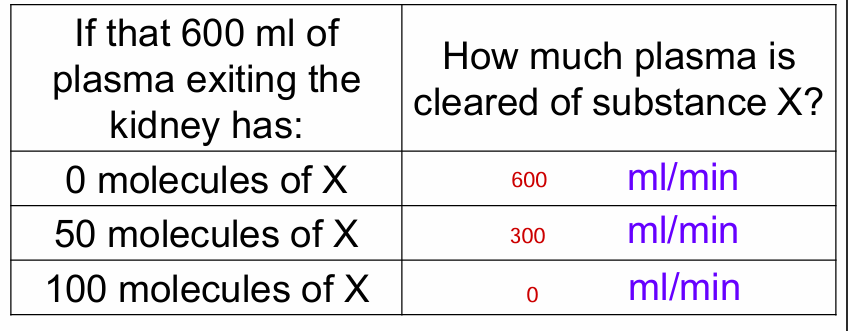
What does that mean, volume of plasma cleared of a substance per unit time? (2)
•Let’s say 600 ml of plasma (blood) is going through the kidney in 1 minute
•That 600 ml of plasma entering the kidney has 100 molecules of substance X
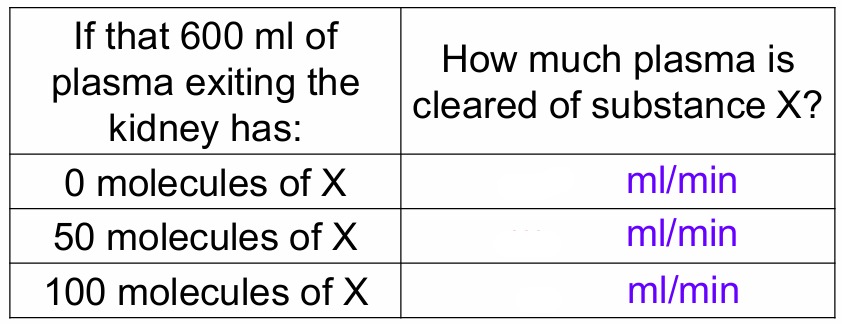
Fill in table
How can a substance be cleared by the kidney?
By being filtered
But if the substance is filtered, how can none of it be cleared?
By also be reabsorbed
But only about 20% of the blood that goes through the kidney is filtered. So how can all of a substance be cleared?
By also be secreted
GFR value
125 ml/min
If GFR = 125 ml/min, how much plasma is cleared of substance X, if it is freely filtered, and not reabsorbed nor secreted?
A. 50 ml/min
B. 125 ml/min
C. 175 ml/min
D. I need more information
B. 125 ml/min
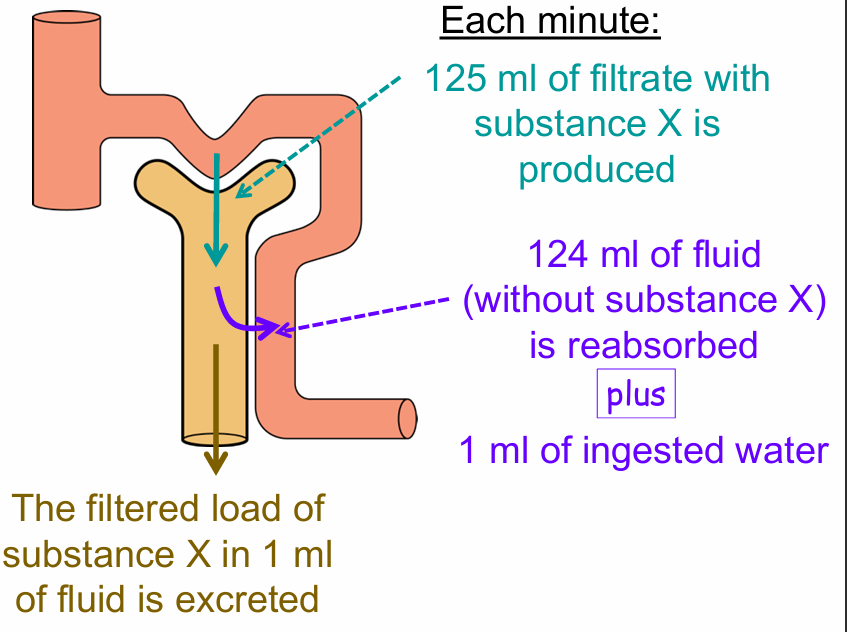
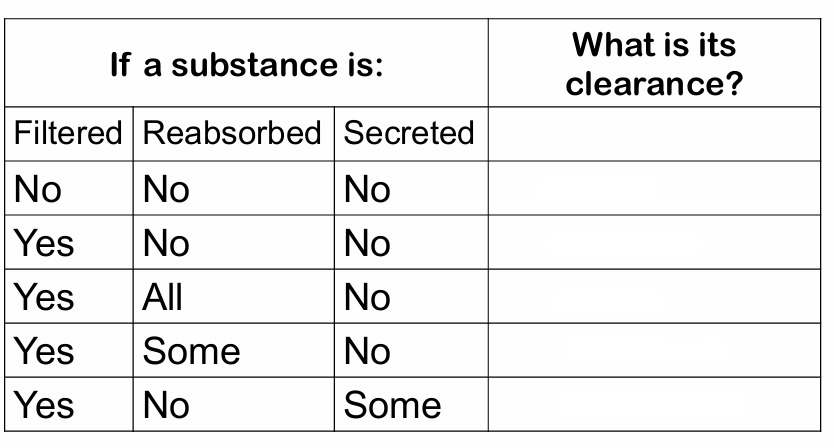
Figure out the clearance of a substance
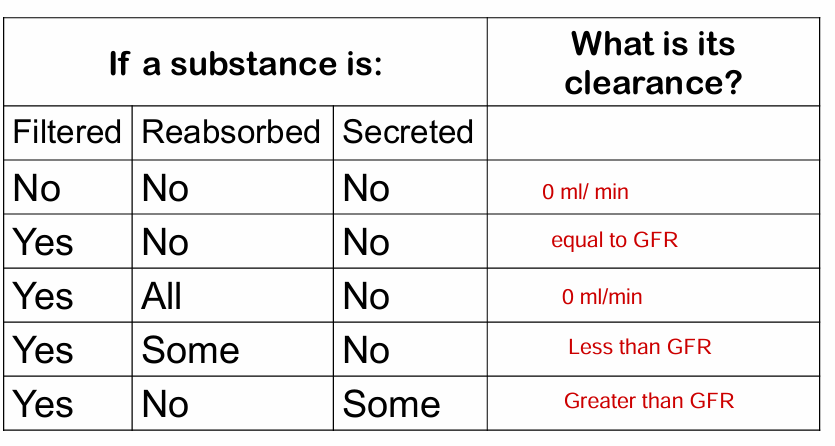
If a substance has a clearance that is greater than GFR, what does that mean?
A. There is no net reabsorption or secretion
B. There is net reabsorption
C. There is net secretion
C. There is net secretion
Calculation of renal clearance
DO NOT MEMORIZE THIS. JUST KNOW TABLE. KNOW THAT THIS CAN CALCULATE GFR
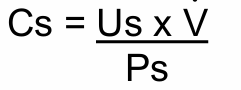
How do you use the clearance equation to calculate GFR?(1) Example(1)
Measure the clearance of a substance that is freely filtered, not reabsorbed and not secreted
EX: insulin, but not normally in blood. Administer IV
Practical method of measuring GFR
Use the clearance of creatinine
Creatinine information (4)
Endogenous substance
End product of creatine metabolism
Continuously exported to blood by skeletal muscle
If muscle mass is constant, creatinine
Creatinine production is constant
Is Creatinine freely filtered? Is Creatinine reabsorbed? Is Creatinine secreted?
Is Creatinine freely filtered? Yes
Is Creatinine reabsorbed? No
Is Creatinine secreted? Only a small amount
Ways to use creatinine to measure or estimate GFR (2)(1)
24 hour urine collection
Measure clearance of creatinine → GFR
Measure the amount of creatinine in serum and use a formula (e.g. Cockcroft Gault) to estimate GFR (eGFR)
A 65-year-old male with a history of hypertension and type II diabetes has a serum creatinine of 1.8 mg/dL (normal 0.6 1.2 mg/dL). What does this mean?
D. GFR is lower than normal
E. GFR is higher than normal
D. GFR is lower than normal
The higher the blood or serum creatinine the lower the GFR and vice versa
A 55-year-old male presents to his physician with knee pain for which he has been taking large amounts of a nonsteroidal anti-inflammatory drug. At his last visit (6 months ago) his blood pressure was 130/75 and his serum creatinine was 1 mg/dl. Now, his blood pressure is 155/85 and his serum creatinine is 2.5 mg/dl. Which of the following best explains his increased serum creatinine?
A. Increased GFR from an increased permeability of the filtration membrane
B. Increased GFR from an increased blood pressure
C. Reduced secretion of creatinine into the tubule
D. Reduced GFR from an increased efferent arteriolar resistance
E. Reduced GFR from an increased afferent arteriolar resistance
E. Reduced GFR from an increased afferent arteriolar resistance
What is the effect of prostaglandins (PGs)
PGs dilate the afferent arteriole.
How do NSAIDs affect prostaglandins?
NSAIDs inhibit prostaglandin (PG) production.
What happens to the afferent arteriole when PGs are inhibited (e.g. by NSAIDs)?
The afferent arteriole constricts
How does PG inhibition affect glomerular filtration rate (GFR)?
PG inhibition decreases GFR due to reduced afferent arteriole dilation.
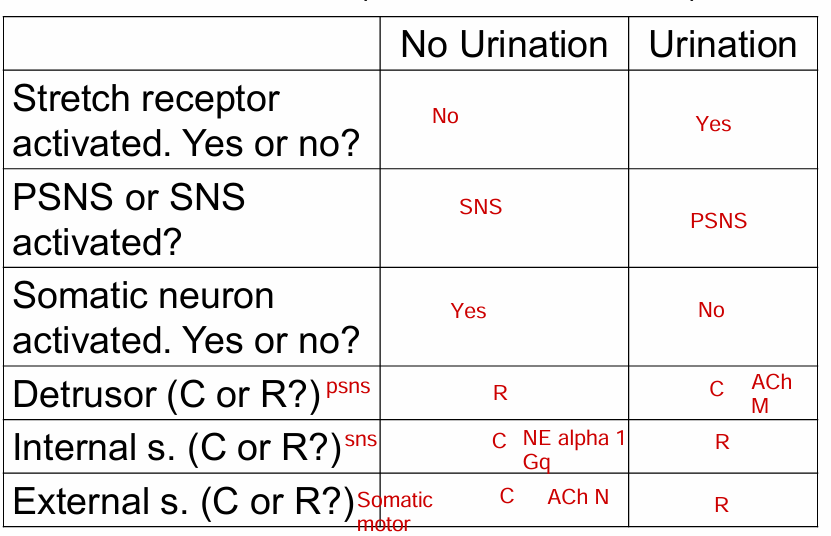
Muscles of the urinary bladder (3)
Detrusor (smooth muscle)
Internal urethral sphincter (smooth muscle)
External urethral sphincter (skeletal muscle)
When is each muscle contracted and why is it contracted?
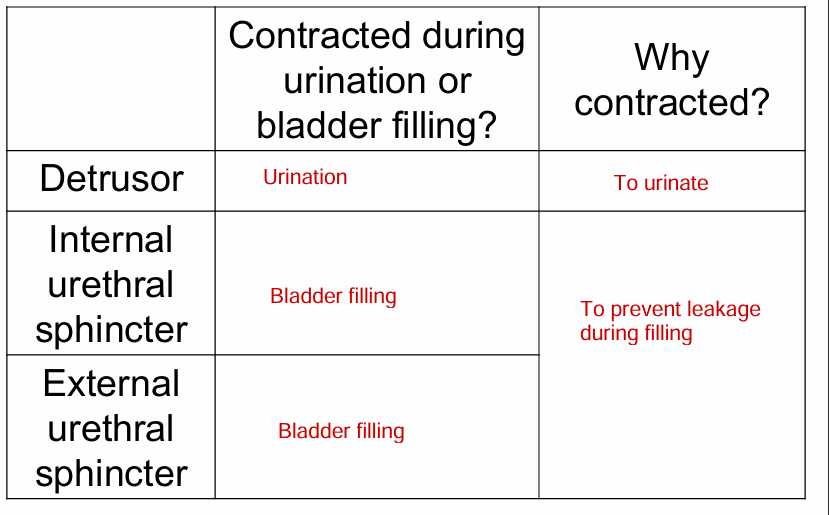
What detects bladder filling?
Stretch receptors in the bladder wall.
What type of neuron carries information from the stretch receptor to the spinal cord?
Sensory neuron.
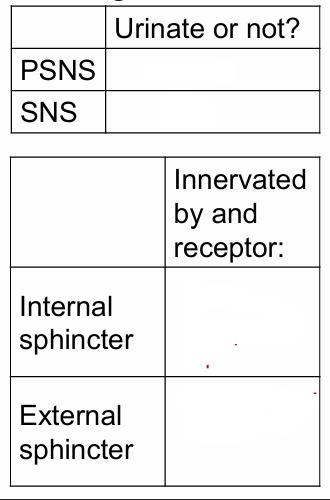
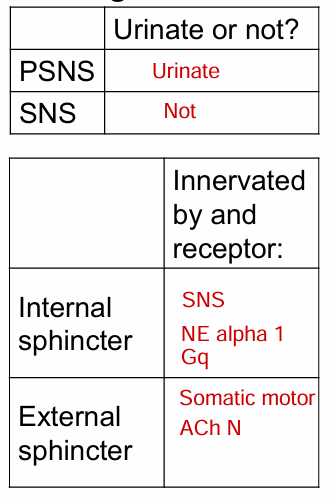
What nervous system activates bladder contraction?
Parasympathetic nervous system.
What type of receptor is on the bladder smooth muscle?
Muscarinic receptor (M rec).
Which nervous system controls the internal urethral sphincter?
Sympathetic nervous system.
What receptor is found on the internal urethral sphincter?
Alpha-1 adrenergic receptor (α₁ rec).
What type of neuron controls the external urethral sphincter?
Somatic motor neuron.
What receptor is found on the external urethral sphincter?
Nicotinic receptor (N rec).
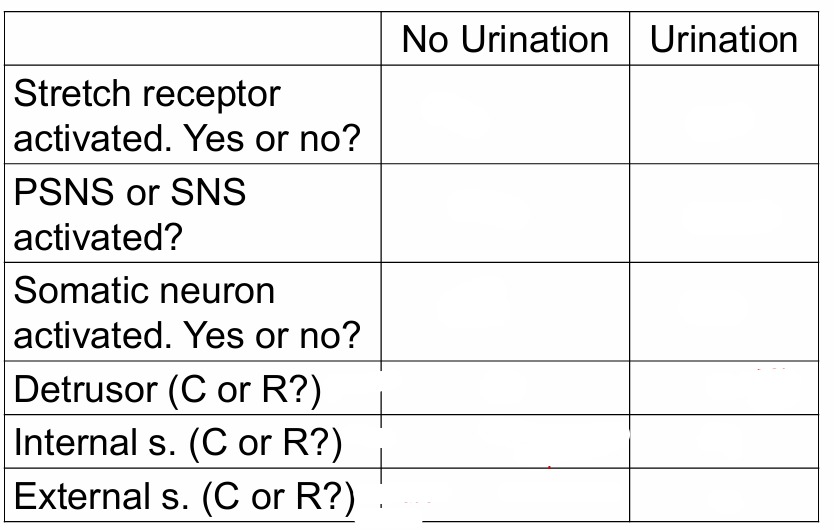
Identify what happens during bladder filling and urination (Micturition reflex)
Descending pathways function
Either inhibit or facilitate the reflex
Males after prostate surgery may become incontinent. One possible cause is that the surgery damaged the:
A. Parasympathetic neurons that innervate the internal urethral sphincter
B. Parasympathetic neurons that innervate the external urethral sphincter
C. Sympathetic neurons that innervate the internal urethral sphincter
D. Sympathetic neurons that innervate the external urethral sphincter
C. Sympathetic neurons that innervate the internal urethral sphincter
Urge incontinence results from detrusor overactivity, leading to uninhibited detrusor muscle contractions during bladder filling. Which of the following is the most useful treatment of urge incontinence?
A. Activate muscarinic receptors
B. Inhibit acetylcholinesterase
C. Block nicotinic receptors
D. Block a1 receptors
E. Block muscarinic receptors
E. Block muscarinic receptors