Trace Elements
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
Trace Elements
Elements found in very small amounts in body, usually 1 ug per gram of tissue.
Excess conc. of these elements is associated with toxicity
often function as enzyme co-factors
Trace elements significance
An element is considered essential if:
deficiency impairs a biochemical or functional process and replacement of element corrects the impairment.
Trace elements are vital to normal function and health
If depleted secondarily to an illness, further complications may be life-threatening.
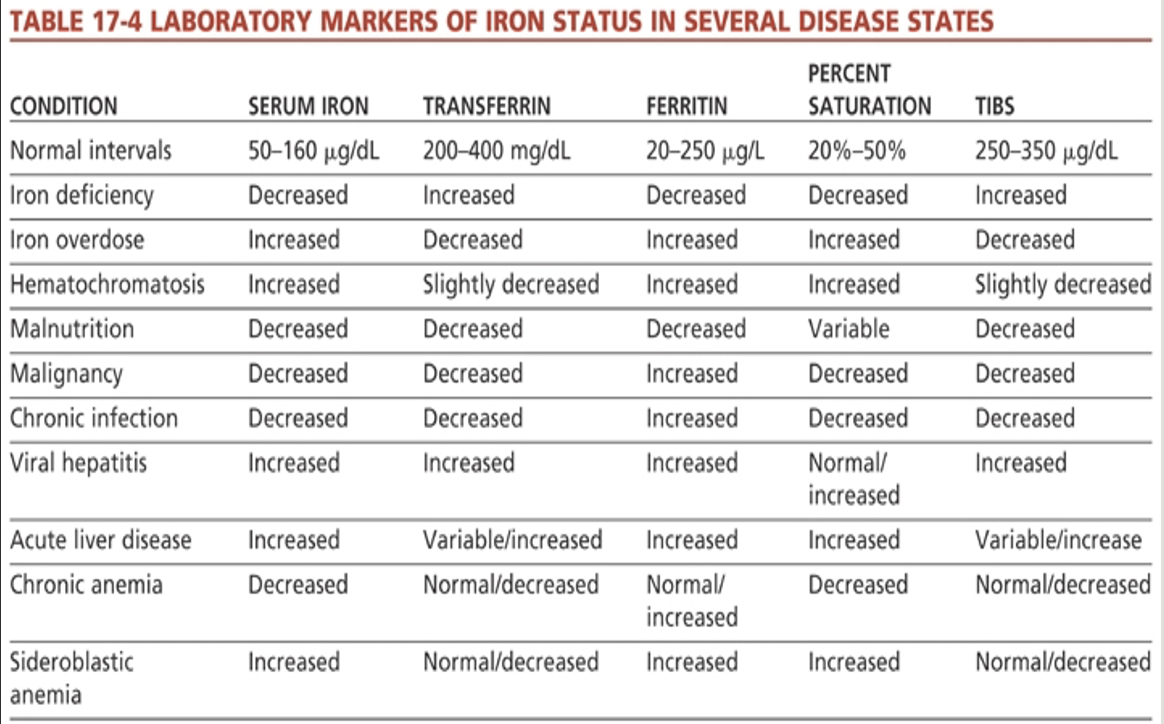
Laboratory Marker of Iron Status on Several Disease States
Iron distribution
Reversible interaction of Fe+ with O2 makes iron physiologically important.
3-5 g of iron in the body
2-2.5 g in hemoglobin
130 mg in myoglobin
8 mg in tissues (bound to enzymes)
3-5 mg found in plasma –bound to transferrin, albumin and free hemoglobin
Also stored as ferritin and hemosiderin in BM, liver and spleen
Trace Element Examples
zinc, copper, selenium, arsenic, cadmium, mercury, lead, iron, manganese, molybdenum and chromium
Iron intake
Dietary intake
avg of 1 mg loss per day in adults must be replaced.
Menstrual cycle drains ~ 30 mg of iron
Pregnant and pre-menopausal women, children and patients with bleeding disorders have greater requirement.
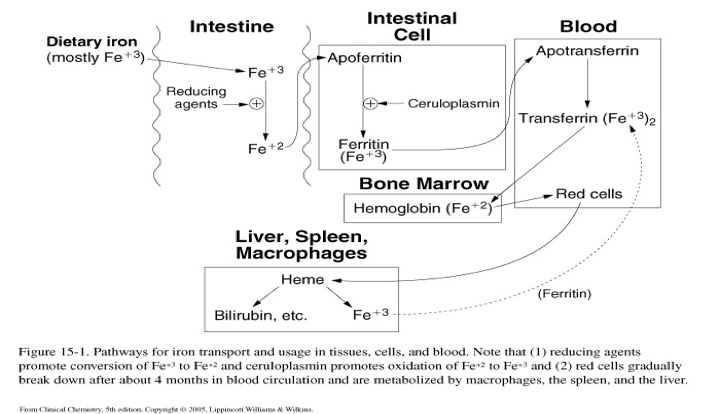
Iron absorption and transport
The process through which iron is taken up from the diet, transported in the bloodstream by proteins such as transferrin, and utilized by the body for various physiological functions, including oxygen transport.
Iron excretion
Small amts are lost in epithelial and red cells excreted in urine and feces each day.
Women lose 20 – 40 mg of iron with each menstrual cycle
600 – 900 mg with each pregnancy.
Iron Clinical Significance Iron
Iron (ferrous) allows hemoglobin to bind reversibly to oxygen and CO2.
Fe deficiency anemia
red. of iron stores
red. in circulating iron
Labs:
dec. RBC, MCH, MCHC and MCV
dec. serum iron and ferritin
inc. transferrin and TIBC (total Iron-Binding capacity)
Iron status determination
Hemoglobin
Serum Iron
TIBC/TIBS
% Saturation (transferrin saturation)
Ratio of serum iron to TIBC => (total iron/TIBC) * 100%
Transferrin and Ferritin
Serum Iron
Measures Fe3+ bound to transferrin
Diurnal variation
Anticoagulants: serum or heparinized plasma
TIBC / TIBS
Amount of iron that could be bound by transferrin and other proteins
TIBC (ug/dL) = serum transferrin (mg/dL) x 1.25
Normal Intervals of Iron
Serum Iron: 50-160 ug/dL
Transferrin: 200-400 mg/dL
Ferritin: 20-250 ug/L
Percent Saturation: 20%-50%
TIBS; 250-350 ug/dL
Iron Deficiency:
Serum Iron: Decreased
Transferrin: Increased
Ferritin: Decreased
Percent Saturation: Decreased
TIBS: Increased
Iron Overdose
Serum Iron: Increased
Transferrin: Decreased
Ferritin: Increased
Percent Saturation: Increased
TIBS: Increased
Hematochromatosis
Serum Iron: Increased
Transferrin: Slightly Decreased
Ferritin: Increased
Percent Saturation: Increased
TIBS: Slightly Decreased
Malnutrition
**Decreased Everything**
Serum Iron: Decreased
Transferrin: Decreased
Ferritin: Decreased
Percent Saturation: Variable
TIBS: Slightly Decreased
Malignancy
Serum Iron: Decreased
Transferrin: Decreased
Ferritin: Increased
Percent Saturation: Decreased
TIBS: Slightly Decreased
Chronic Infection
Serum Iron: Decreased
Transferrin: Decreased
Ferritin: Increased
Percent Saturation: Decreased
TIBS: Slightly Decreased
Viral Hepatitis
Serum Iron: Increased
Transferrin: Increased
Ferritin: Increased
Percent Saturation: Normal/Increased
TIBS: Increased
Acute liver disease
Serum Iron: Increased
Transferrin: Variable/Increased
Ferritin: Increased
Percent Saturation:Increased
TIBS: Variable/Increased
Chronic Anemia
Serum Iron: Decreased
Transferrin: Normal/Decreased
Ferritin: Normal/Increased
Percent Saturation: Decreased
TIBS: Normal/Decreased
Sideroblastic Anemia
Serum Iron: Increased
Transferrin: Normal/Decreased
Ferritin: Normal/Increased
Percent Saturation: Increased
TIBS: Normal/Decreased
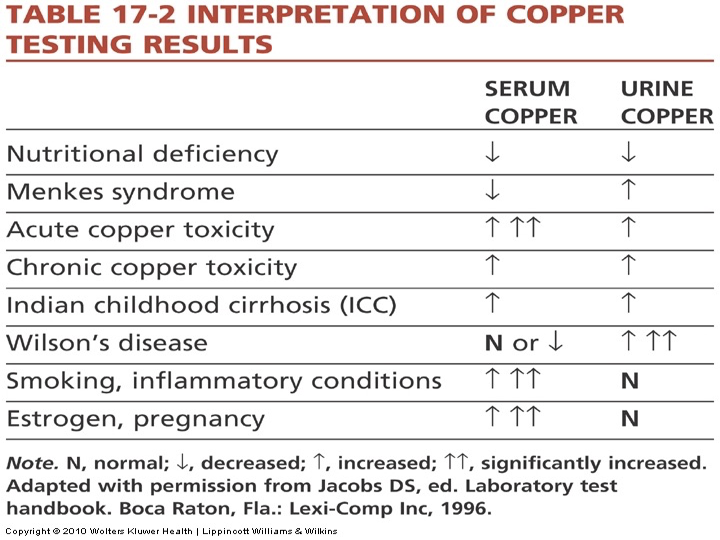
Copper
Absorbed through the intestine from dietary substances.
Travels in blood bound to albumin or histidine to the liver, brain, heart, and kidneys.
Half is excreted in feces.
Most is incorporated as ceruloplasmin, an acute phase reactant.
Deficiency seen in premature infants, malnutrition, and chronic diarrhea.
Results in decreased hemoglobin and collagen production.
Interpretation of Copper Testing Results
Note*
Serum copper: ↑↑↑
Acute copper toxicity
Smoking, inflammatory conditions
Estrogen, pregnancy
Urine copper: ↑↑↑
Wilson’s Disease
Zinc
Second to iron in importance as an essential trace element.
Absorbed through the intestine from dietary nutrients.
Transported in blood with albumin or alpha 2 macroglobulin carriers.
Excreted in feces or pancreatic secretions.
Higher conc. in RBCs than in plasma or serum.
Lead
Heavy metal commonly found in the environment.
Present in batteries, ammunition, foil, petrol, household paints, and toys.
Exposure is primarily respiratory or gastrointestinal.
94% of lead is transported to RBCs (bound to hemoglobin); 6% is in plasma.
Half-life in whole blood is 2 to 3 weeks.
Stored in soft tissues (~5%) and bones (~95%); excreted in urine, feces, and other routes.
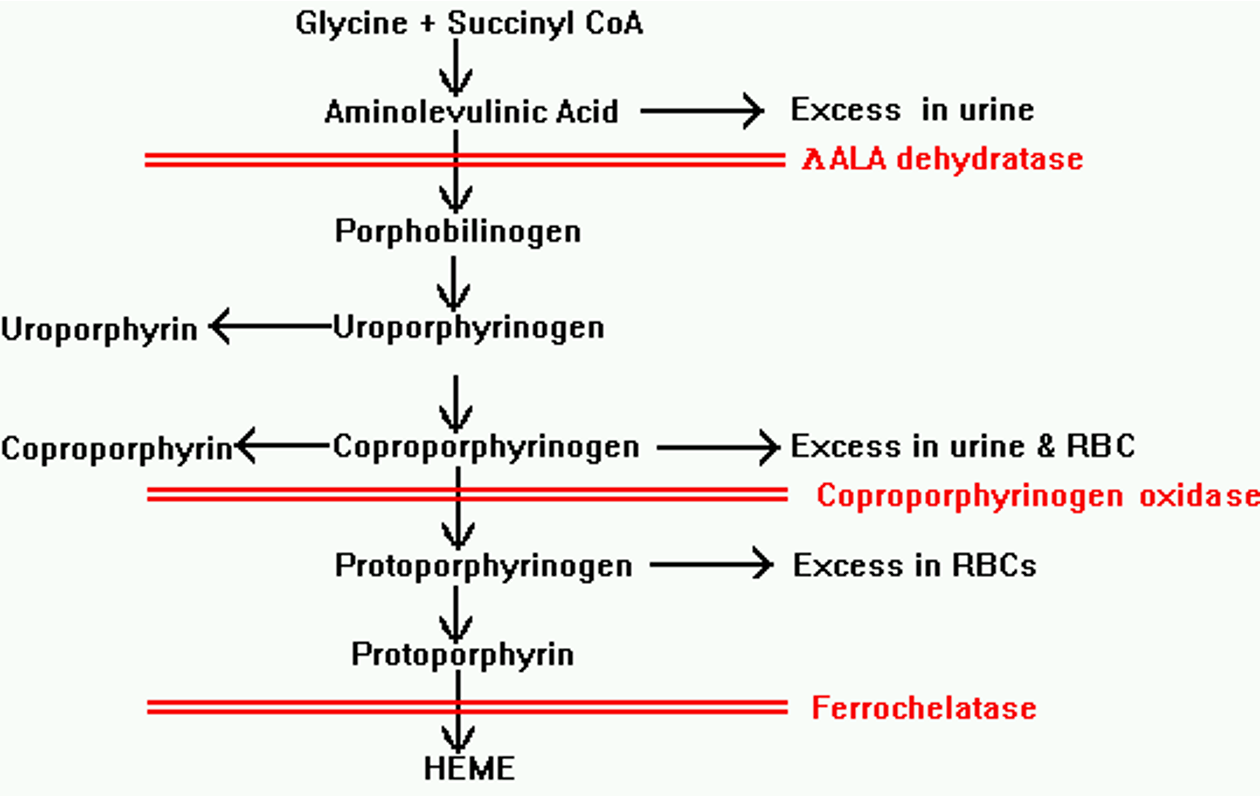
Lead Poisoning
Build-up of lead in the body over months or years.
Interferes with bodily processes, particularly heme synthesis → anemia.
Negative effects: cognitive deficits, developmental delays in children, peripheral neuropathy, hypertension.
Can damage organs such as the kidneys and liver.
Lead poisoning pathway
The biosynthesis of heme starts with the amino acid glycine and succinyl-CoA, leading to the formation of porphyrin, which in the presence of iron, is transformed into heme.
Specimen for Lead Testing
Avoid contamination due to small difference between normal and elevated lead levels.
Collect whole blood with:
Lead-free needle
Royal blue top tube (metal-free)
EDTA is commonly used.
Urine plastic container that is acid-washed to remove surface lead.
Capillary Blood for Lead Testing
not recommended for lead testing due to contamination risks. If capillary samples are used, results must be confirmed with venous blood for accuracy in diagnosing lead exposure.
Lead Testing - Whole Blood
Whole blood lead measurement: best for detection of lead exposure.
Elevated lead level: >3.5 mcg/dL
Lead level standards lowered over 20 years: from 10 mcg/dL to 5 mcg/dL, now 3.5 mcg/dL due to child development concerns.
Significant brain development damage: >30 mcg/dL in adults.
Lead Testing Lab Tests
Free erythrocyte protoporphyrin assay (EPP) levels
Zinc protoporphyrin (ZPP)- considered a supplemental lead test
Arsenic
both metallic and nonmetallic properties.
Nonessential but can be toxic.
Currently, main use is as a wood preservative (profession → poisoning)
Main routes of exposure are ingestion from contaminated food, water, beverages or inhalation of contaminated air
Selenium
Component glutathione peroxidase and tetraiodinothyronine-5’-deiodinase
Enters food chain via plants
Organ meats and seafood, cereals, grains, dairy products, fruits and vegetables are sources of dietary selenium
Low Selenium content seen in parts of China resulting in Keshan disease or Kashin-Bek disease
Keshan disease or Kashin-Bek disease
A selenium deficiency-related disease characterized by cardiomyopathy and joint issues, prevalent in areas with low selenium levels. Seen in parts of China
Specimen considerations for analysis
Avoid contamination; use trace metal-free equipment and royal blue tubes for blood collection. Ensure high sensitivity and specificity in methodology. Elements must be stable; atomic absorption spectroscopy is the most precise method.