Electrons Quiz
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
How are electrons commonly used clinically?
6-20 MeV
superficial tumors: skin, lip, boosting lymph nodes
What is an inelastic collision?
Kinetic energy is converted from one form to another
with electrons: ionization and excitation (low Z material)
with nuclei: Bremsstrahlung (high z material)
What is an elastic collision?
with electrons: electron scattering
with nuclei: Coulomb scattering
KE not lost, redistributed
What is linear energy transfer?
rate of energy loss per unit path length in collisions
energy is locally absorbed, not carried away by secondary electrons
What is electron scattering?
Columb forces between electrons and nuclei of the medium cause electrons to scatter
Z²/KE²
What type of material is used to construct scattering foil?
High Z materials to spread out beam that emerges from accelerator tube
What is the electron beam kept thin?
to minimize X ray contamination
minimize energy degrading
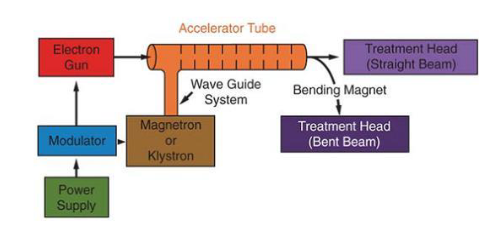
Beam journey
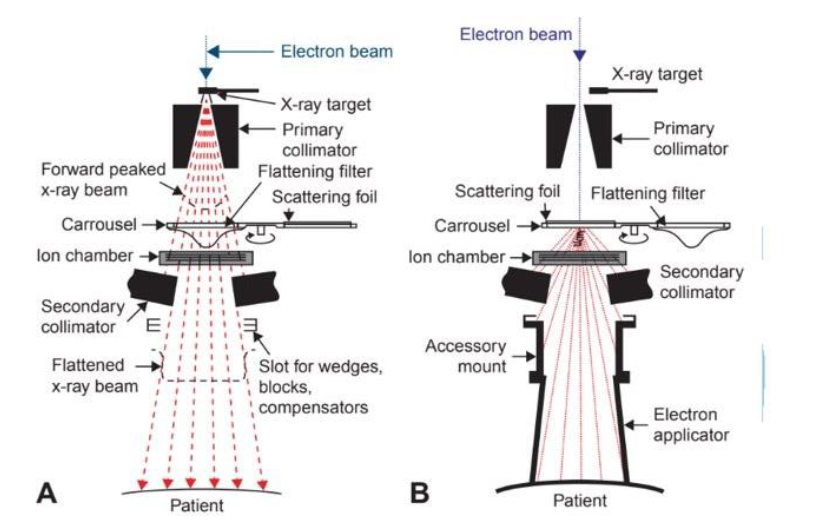
Linac elements
How are electron beams named?
by most probable energy at the body surface
beam starts monoenergetic but gets degraded by the time it reaches phatom surface
What is (Ep)o?
most probable energy, defined at the phantom surface
What is mean energy (E0)?
related to the depth at which dose is 50% of max dose
2.4(MeV/cm for water) x R50
What is energy at depth?
The most probable energy and mean energy decreases linearly w/ depth Z
How can depth dose distribution be determined?
ion chamber
diode
film
What is an ionization chamber?
determines absorbed dose
What are the advantages of silicon diodes?
no corrections needed
small
high sensitivity
What are the disadvantages of silicon diodes?
suffer from energy and temperature dependence
damaged by radiation
measurements must be backed up with ionization chamber (2x more work)
cannot be used for absolute dosimetry
What are the pros and cons of films?
Pros: useful for determining the electron beam dose distributions, practical range, isodose curves, and beam flatness
cons: cannot be used for absolute dosimetry
What are phantoms typically made of?
water or water equivalent density
need to make correction if not water
At what rate do electrons lose energy?
2MeV/cm of water
What is the formula for depth of the 90% isodose?
D90=E/3.2
D90 is the most useful treatment depth
also called therapeutic range (Rt)
What is the formula for depth of 80% isodose?
E/2.8
What contributes to dose beyond the max range of electrons?
x-ray contamination
What is x-ray contamination?
dose contributed by bremsstrahlung interactions w/ scattering foil
In 6-12 MeV, how much dose is due to x-ray contamination?
0.5-1%
In a 12-15 MeV beam, how much dose is due to x-ray contamination?
1-2%
In a 15-20 MeV beam, how much dose is due to x-ray contamination?
2-5%
What is x-ray contamination a concern?
total skin electron therapy b/c entire body is irradiated from 6 directions, so contamination increased 6x
How is dmax related to energy?
dmax increases with energy
at lower energies, electrons will scatter more easily and through larger angles
so dose builds up more rapidly over a shorter distance
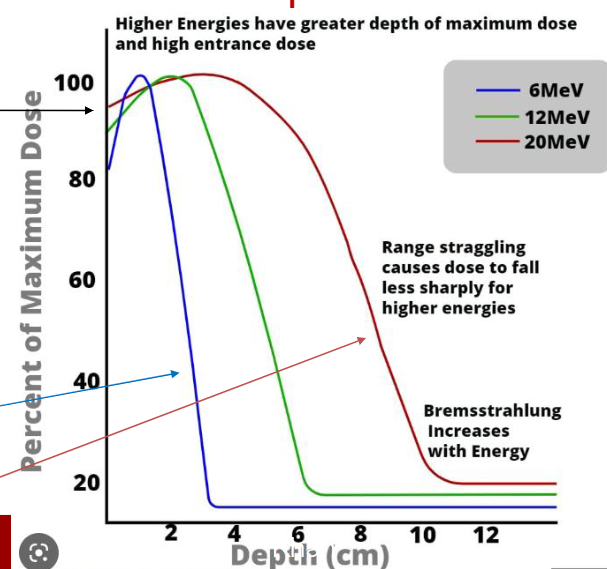
How is percent surface dose related to energy?
increases w/ energy
Why is there a more rapid dose buildup in lower energy electron beams?
in low energy, more scatter through larger angles, bigger difference between surface dose and max dose
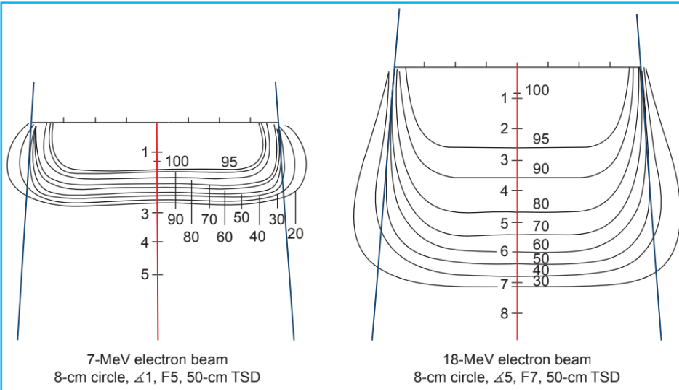
How are isodose curves shaped?
electron scattering causes low E curves to bulge out
In high E electrons, low dose levels bulge out
high E electrons show lateral constriction
What is beam flatness and symmetry?
dose at any point should not exceed 103% of central axis dose
What is the AAPM recommendation for field flatness?
perpendicular to CAX at 95% isodose depth
dose variation should be ±5%
What is the AAPM recommendation for field symmetry?
evaluated from measured cross beam profile
comapres teh dose profile on one side of CAX to the other
pair of points same distance on either side of the CAX should not differ by 2%
How is dose related to field size?
dose increases with field size
more scatter from collimator and phantom
How is PDD related to field size?
increases w/ field size until it exceeds lateral range of electrons
after, PDD is almost consistent w/ field size
How is depth of dmax related to field size?
increases w/ field size until lateral range is reached
dmax shifts toward surface for smaller field sized b/c less scatter, so Dmax is reached faster
How is output impacted by small FS?
decreased output, more MUs
What is the electron source?
electrons do not follow inverse square law
there is no target, so there is no “source”
we use imaginary source = virtual source point
virtual source point: intersection point of back-projections along the most probable directions of electron motion
How can virtual source point be determined?
geometric method: take films at different SSDs, measure reduction in FS, project back to 0 FS
effective SSD method: dose measured in phantom at Dmax w/ phantom in contact w/ cone, then at various distances
Do electron cases typically use SSD or SAD setup?
SSD set up
isocenter maybe center of the lesion or scar
may or may not use bolus
What is an SSD setup?
100cm to skin surface
typically single field b/c have to move the patient between fields
iso is on area we are treating
How are electrons set up at MSH?
typically for primary or metastasis, a template created during sim and then used daily for treatment
What is the electron set up method at MSW?
breast boosts
sim in decubitis if patient is prone
What is the electron setup method at MS chelsea
keloid
skin lesions
sarcomas
How are electron cases planned?
typically single field
if surface is not flat, isodose charts are more complex
TPS accounts for this
How is energy chosen in electron cases?
chosen by depth of target, minimum target dose required, and dose to OARs
If no OARs, typically treat so PTV is within 90-95% isodose line
What isodose line is used when treating chest wall?
80%
What is the purpose of a bolus?
shifts dose upstream
shift is equal to thickness of bolus
ex: 1cm thick bolus, dmax shifts up 1 cm
Why is bolus used with electrons?
fix surface irregularities, flatten
decrease electrons penetrating certain areas
increase skin dose
What is the density of bolus?
should be that of tissue
1g/cm2
superflab, wax
What are decelerators?
low Z material to reduce energy of electron beam
should not be placed close to patient surface
How to relate dose to a point that is not dmax
Ddmax = Drx/%D
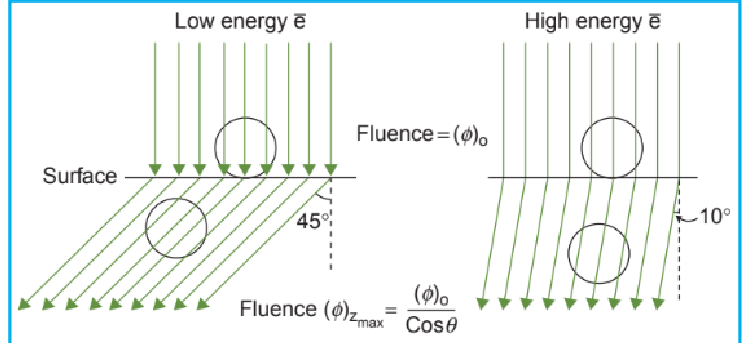
What is beam obliquity?
when you don’t have a flat surface or the beam is not en face
How does beam obliquity change depth dose?
increase max dose (hotter hotspot)
increases side scatter at dmax
shifts dmax towards surface
D90 is reduced
x ray contamination is increased
How do surface irregularities impact dose?
can create hot or cold spots in different areas
can compensate with bolus
taper edges of bolus
How is the beam shaped?
lead blocks on skin
need to be thick enough to reduce beam to <5% transmission
place on skin b/c penumbra
How to calculate the minimum thickness of lead for blocking
energy/2
for cerrobend x1.2
How do 2 electron fields impact skin surface?
hotspot near skin
What happens if a photon and electron field abut?
electrons scatter laterally, so cold spot will be on electron side, and hotspot on photon side
How to account for inhomogeneities
(thickness of tissue x density) + thickness of tissue x density)