2.0 DEEP VEIN THROMBOSIS
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
Deep Vein Thrombosis (DVT)
occurs when a blood clot forms in a deep vein,
most commonly in the lower leg, thigh, or pelvis or arms.
If the clot breaks off and travels through the bloodstream, it can lodge in the lungs,
causing a potentially life-threatening condition called a pulmonary embolism (PE).
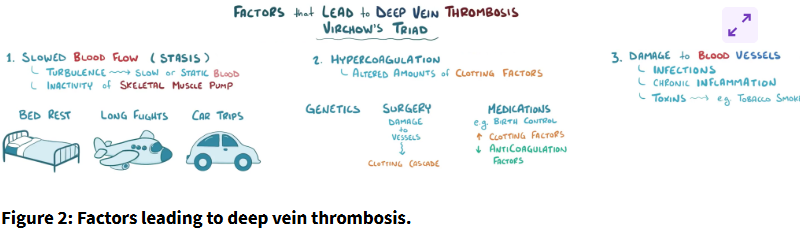
the pathophysiology of Deep Vein Thrombosis (DVT)
lead to clot formation, the coagulation cascade, and potential complications like pulmonary embolism or embolic stroke.
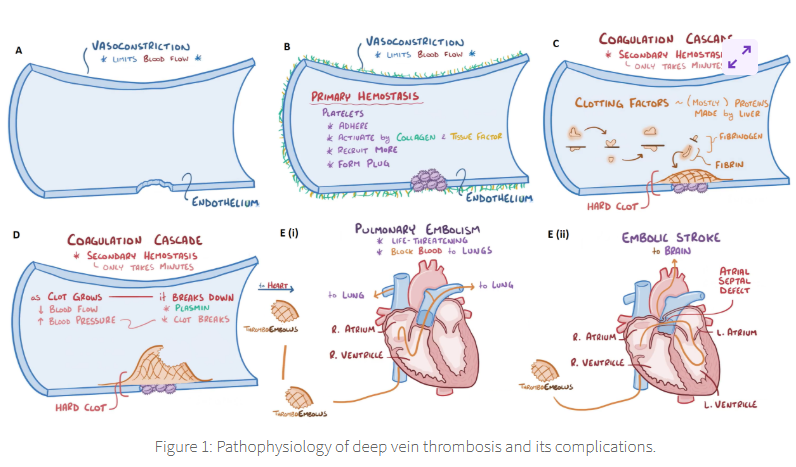
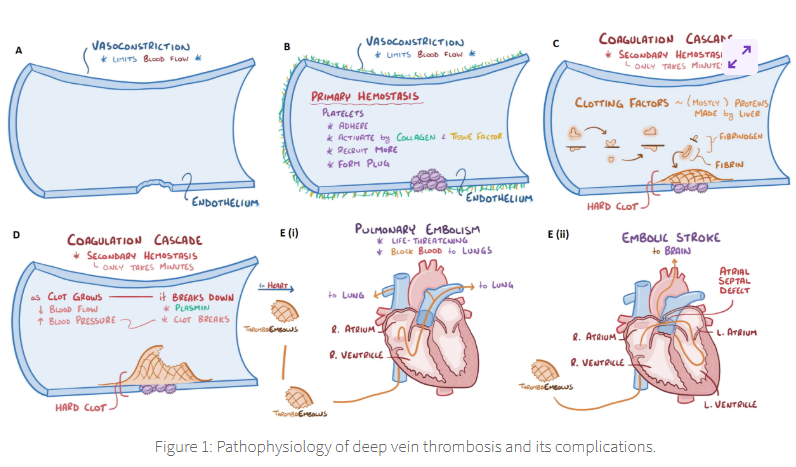
Vasoconstriction
refers to the narrowing of blood vessels, which limits blood flow to the injured area
When damage occurs to the blood vessel like the break in the endothelial lining
vasoconstriction is the body’s first response to reduce blood flow and prevent excessive bleeding
Primary haemostasis begins when platelets adhere to the site of endothelial injury
which becomes activated by the collagen and tissue factor.
Activated platelets recruit additional platelets to the site of injury
forming a platelet plug.
Platelets play a critical role in the early stages of clot formation
by temporarily stopping blood loss, while serving as a platform for subsequent clot stabilization.
Secondary haemostasis involves the coagulation cascade,
a series of biochemical reactions that further stabilize the initial platelet plug by forming a fibrin clot.
Clotting factors, primarily produced by the liver, are activated sequentially,
resulting in the conversion of fibrinogen into fibrin.
Fibrin forms a mesh-like structure around the platelet plug, resulting in a stable hard clot.
This process generally takes only a few minutes after the injury and provides stronger protection against further bleeding.
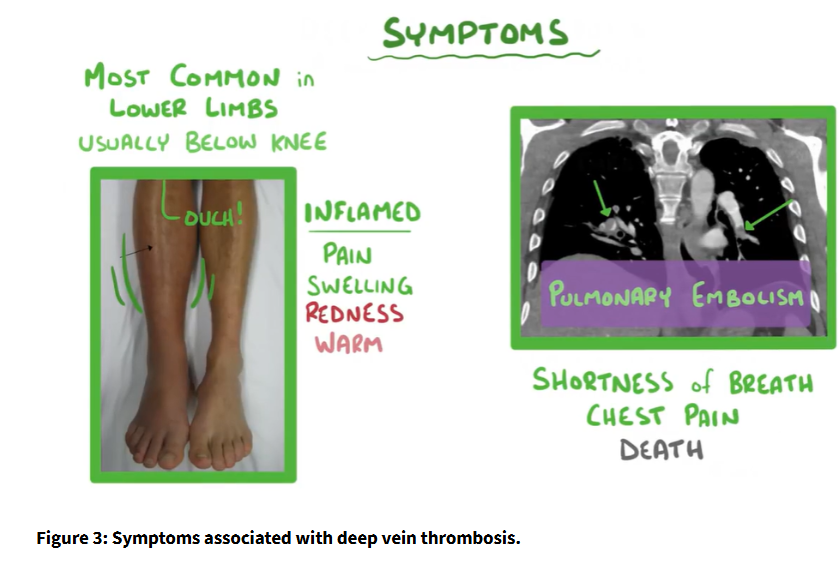
As the clot grows, it can restrict blood flow through the affected blood vessel,
especially in the context of DVT, where clots form in the deep veins of the legs or pelvis.
The restriction of blood flow in the affected area can lead to swelling and pain,
but it doesn't typically cause a decrease in blood pressure. Rather, there can be an increase in venous pressure due to the pooling of blood behind the clot.
The body has mechanisms to break down clots after they have served their purpose.
The enzyme plasmin breaks down fibrin and dissolves the clot, a process known as fibrinolysis.
Proper clot breakdown prevents complications like embolism,
where part of the clot can dislodge and travel through the bloodstream.
In some cases, part of the clot (known as a thromboembolus) can break off from the deep veins (often from the legs in cases of DVT)
due to the high blood pressure and travel to the lungs, causing a pulmonary embolism (PE).
PE is a life-threatening condition where the embolus blocks the blood vessels in the lungs,
preventing proper oxygen exchange.
In the figure, the embolus travels from the right atrium and right ventricle of the heart into the lungs,
where it obstructs blood flow. This can result in respiratory distress and, if severe, can be fatal.
Another potential complication is an embolic stroke,
where the clot (thromboembolus) travels to the brain.
In this case, the embolus passes through a septal defect (a hole between the left and right sides of the heart) into the left atrium and left ventricle,
from where it is pumped into the arteries supplying the brain.
This blockage of blood flow to the brain causes an embolic stroke,
a dangerous condition that can result in neurological damage, loss of function, or even death.