Lecture 2 - pigs and poultry
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
Cystoisospora suis
Trichuris suis
Oesophagostomum spp
Stephanurus dentatus
Metastrongylus spp
Pig coccidiosis
Trichurosis
Oesophagostomosis
Stephanurosis
Metastrongylosis
Pig coccidiosis: Cystoisospora/Isospora suis
Location: small intestine
Cystoisospora (Isospora) suis: proven pathogenic;
Infected animals shed in the environment unsporulated oocysts;
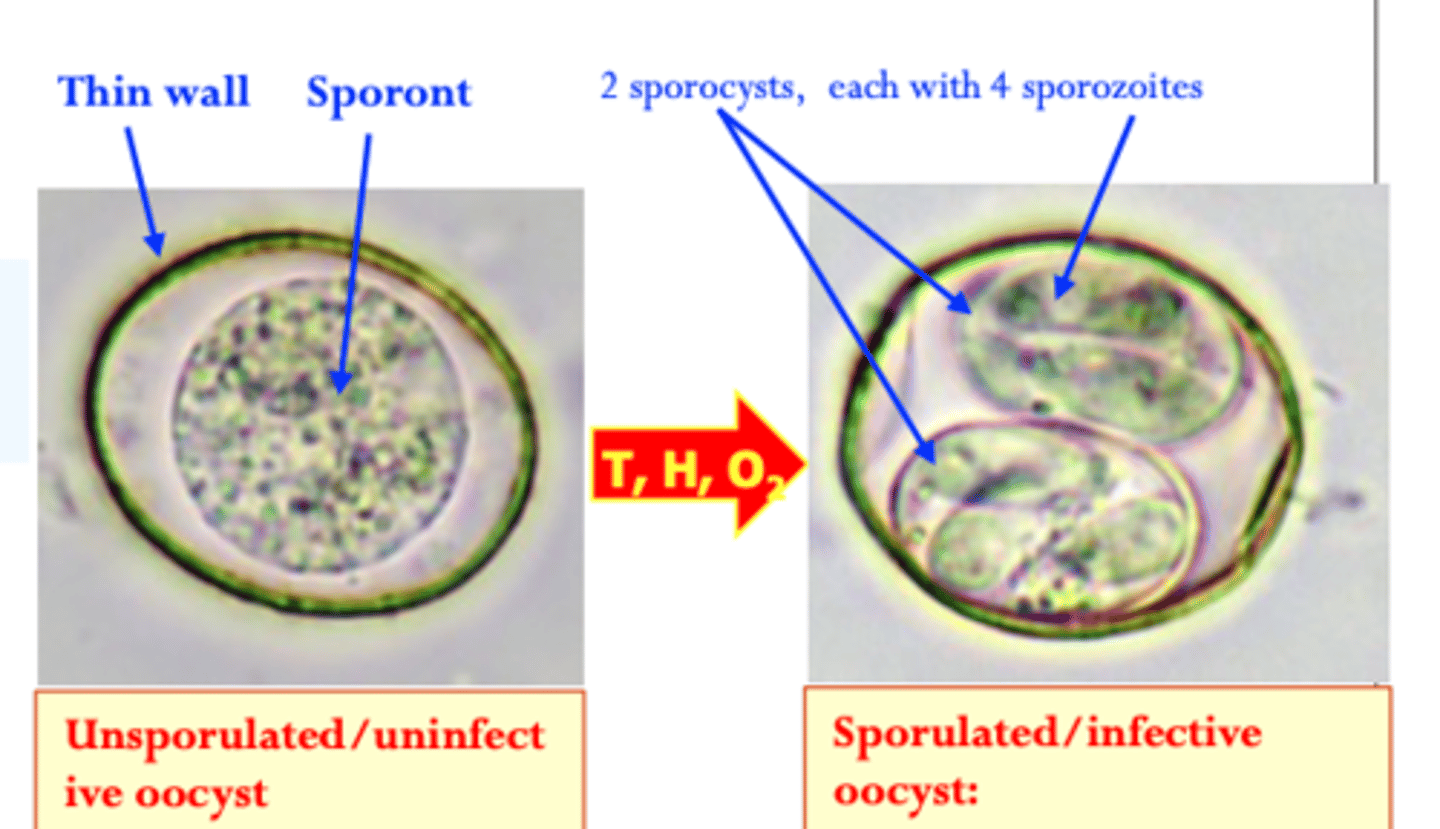
Sporulation/sporogony: the oocysts require
• Humidity;
• Proper temperature:
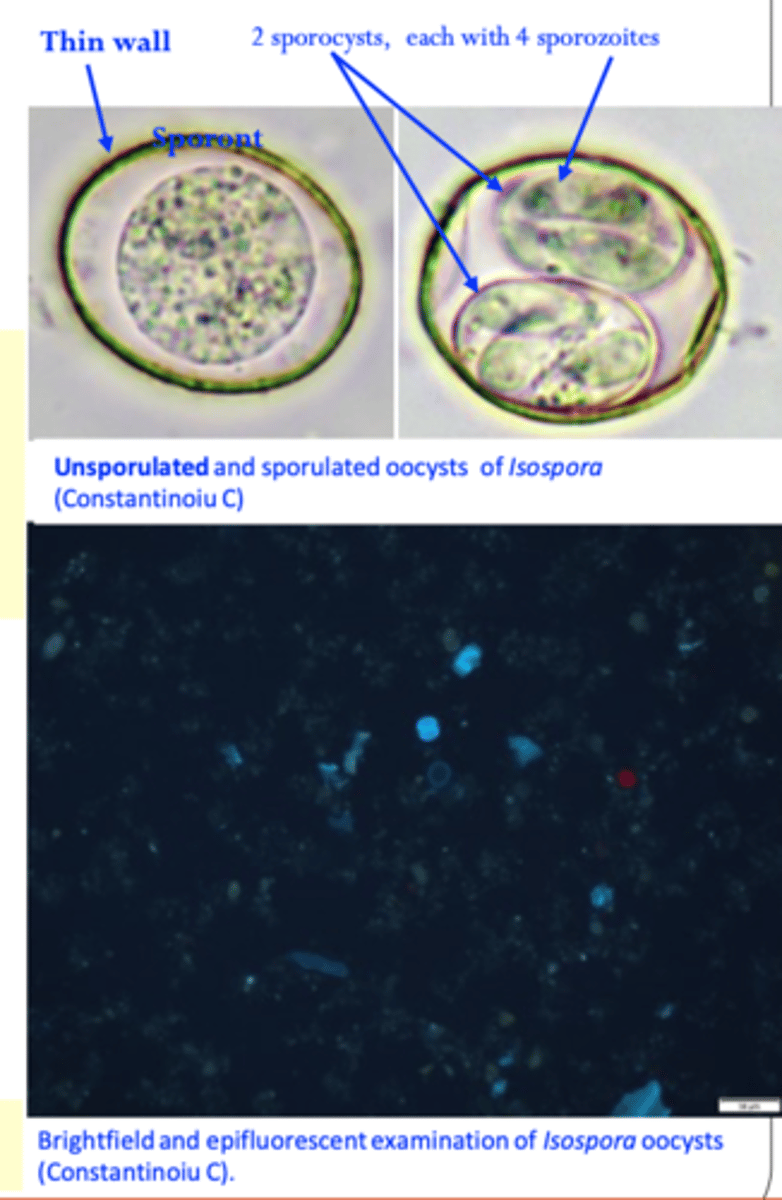
Sporulated oocysts contain two sporocysts each with four sporozoites;
Infection of the host: ingestion of sporulated oocysts;
Cystoisospora/Isospora suis
Morphology/life cycle
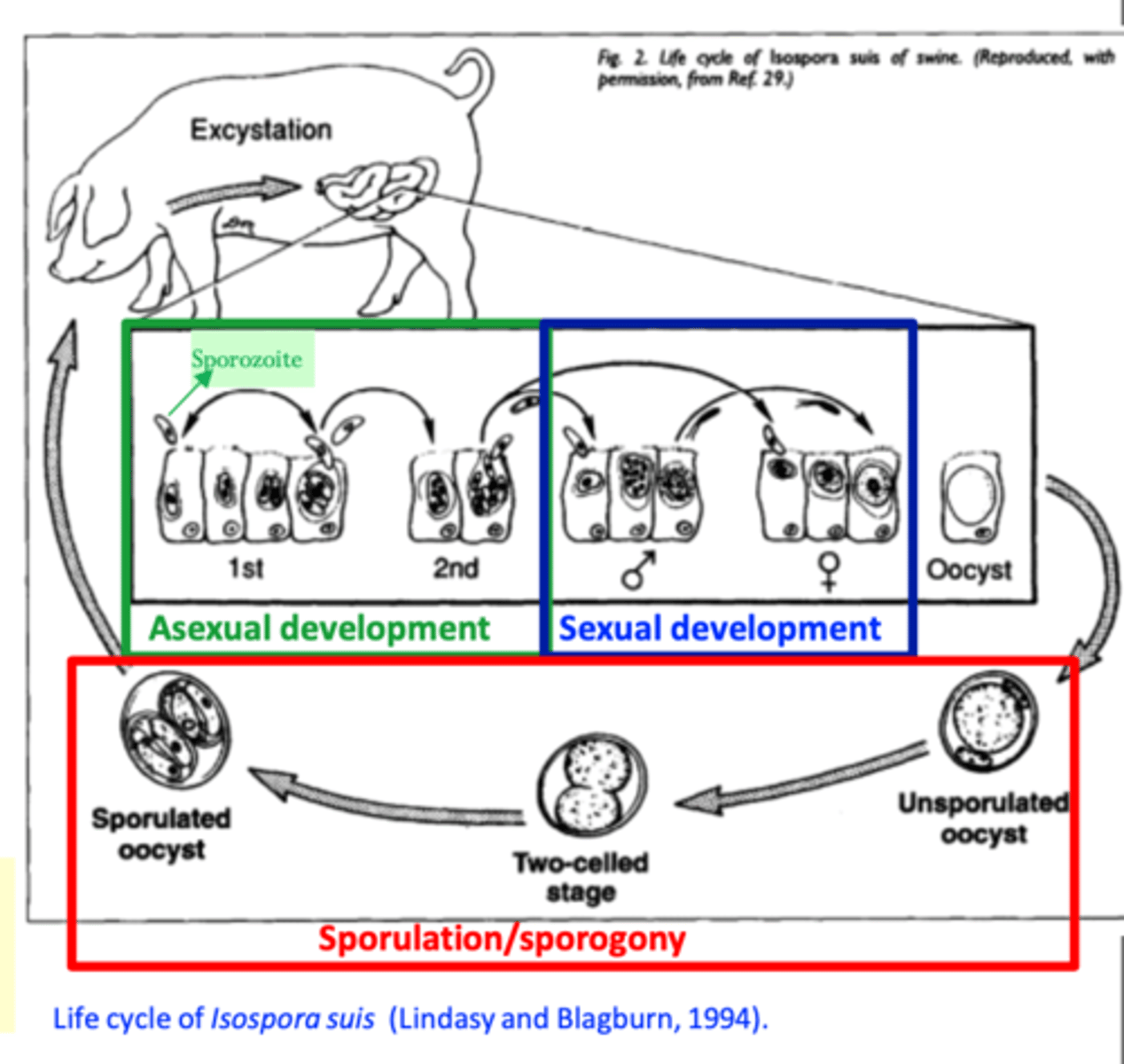
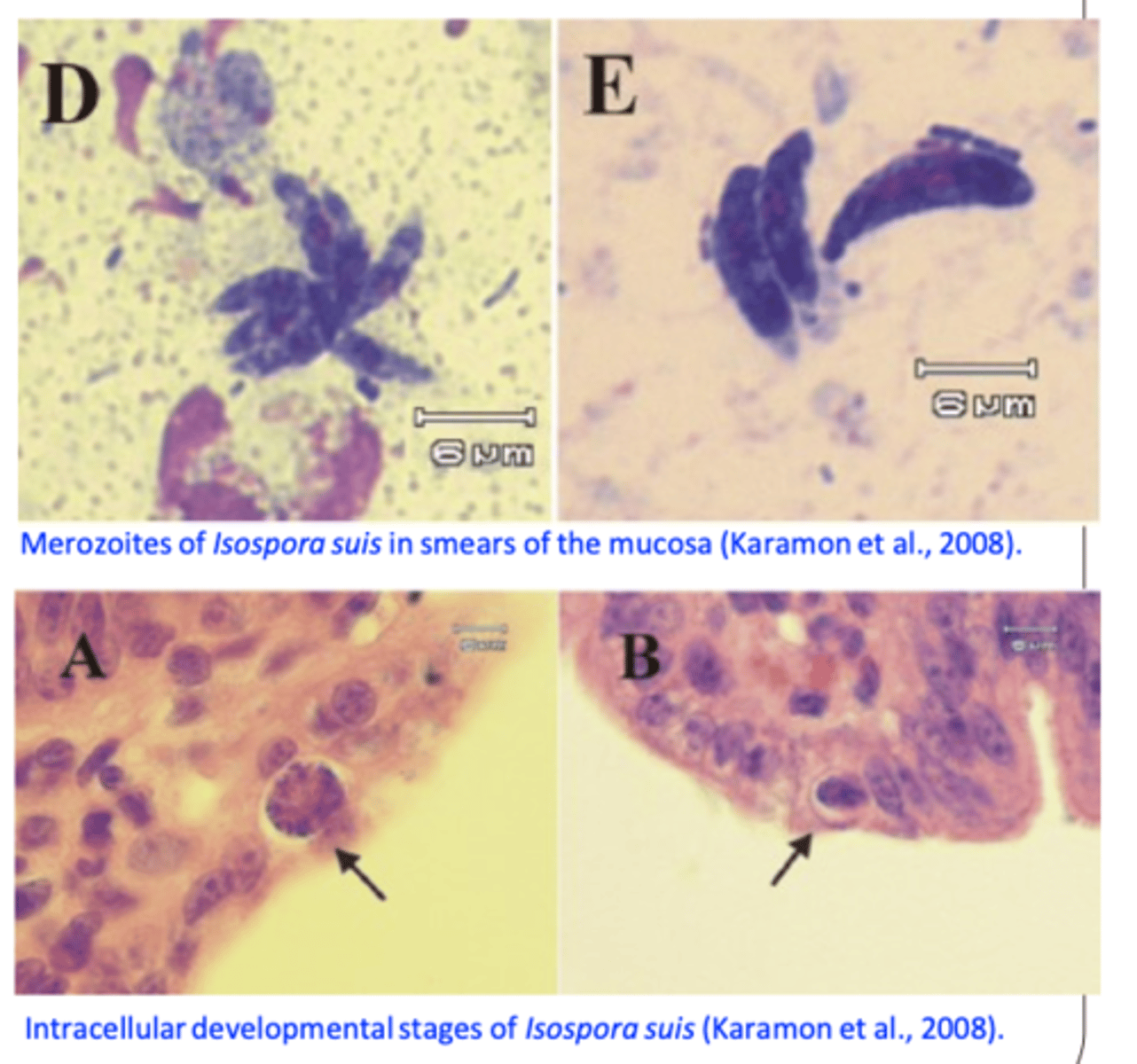
• Oocysts excyst in the small intestine sporozoites are released and invade the epithelial cells;
• Asexual (merogony) and sexual (gamogony) development occurs in the enterocytes of the
small intestine
• Oocysts are shed in the faeces 4-5 days post infection in several peaks (each phase lasts for 2-3 days) for up to 2 weeks
Short PPT (4-5 days) and short sporulation time (12 h - 2 days);
Cystoisospora/Isospora suis
EPIDEMIOLOGY
Infections occur all over the world in both indoor and outdoor systems (does not seem to be associated with a particular season);
Pigs younger than 2 - 3 weeks more susceptible (most susceptible in the first 3 days of life) age resistance develops
Infections of piglets older than 3 weeks are asymptomatic
Pigs that recover from infection are resistant to challenge infections;
Sows are not the source of infection for piglets
Oocysts shed by previous piglets in the farrowing pen and that survived on floor and walls seem to be the source of infection --> management/cleaning of the farrowing pen is essential in prevention;
Sporulated oocysts can survive for months in the environment and are resistant to most disinfectants
Cystoisospora/Isospora suis
Pathogenesis/Pathology
Depends on the age of the pigs and infective dose:
Pathogenesis is caused by both asexual (meronts) and sexual (gamonts) stages
Cystoisospora suis
Clinical signs
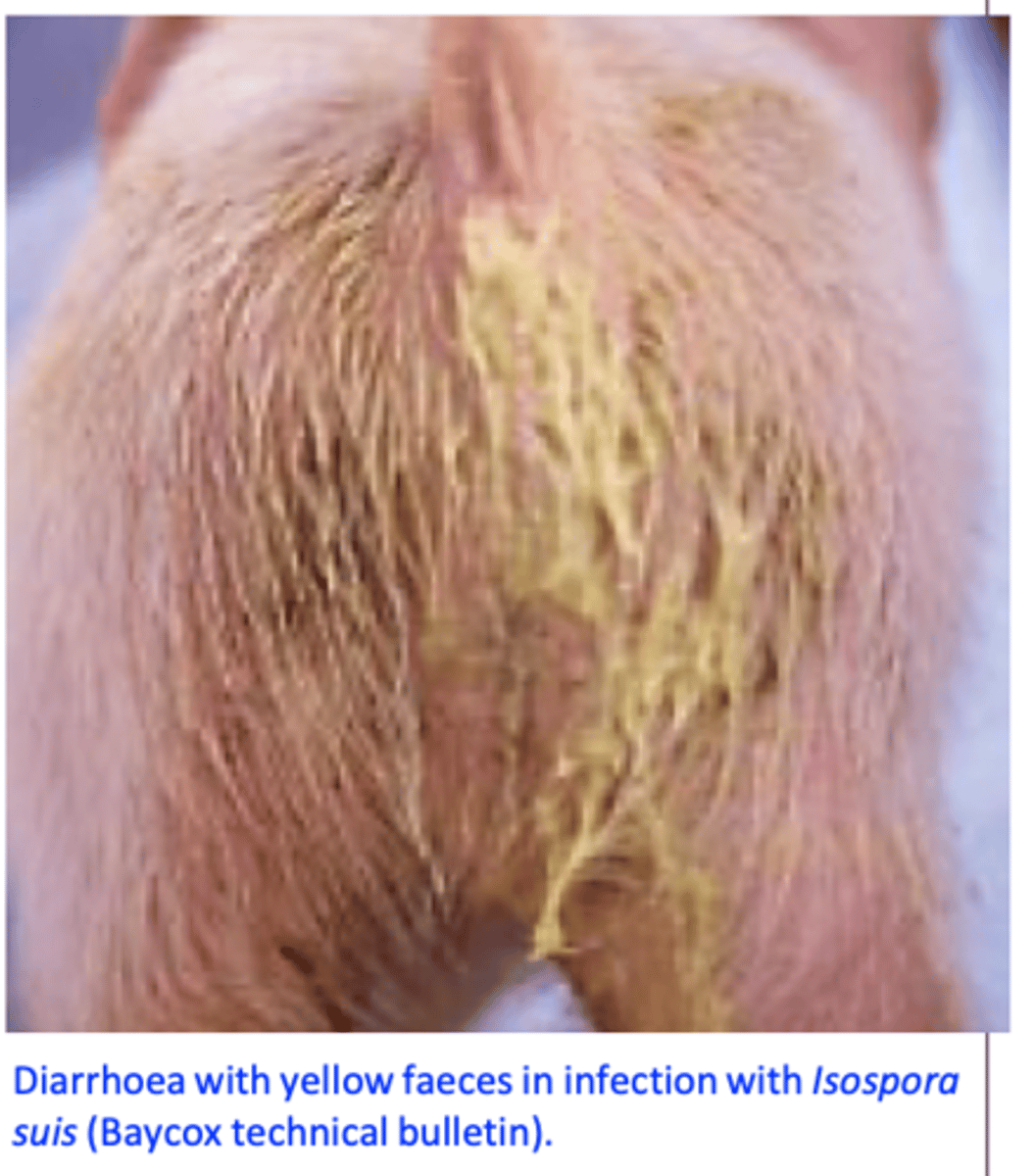
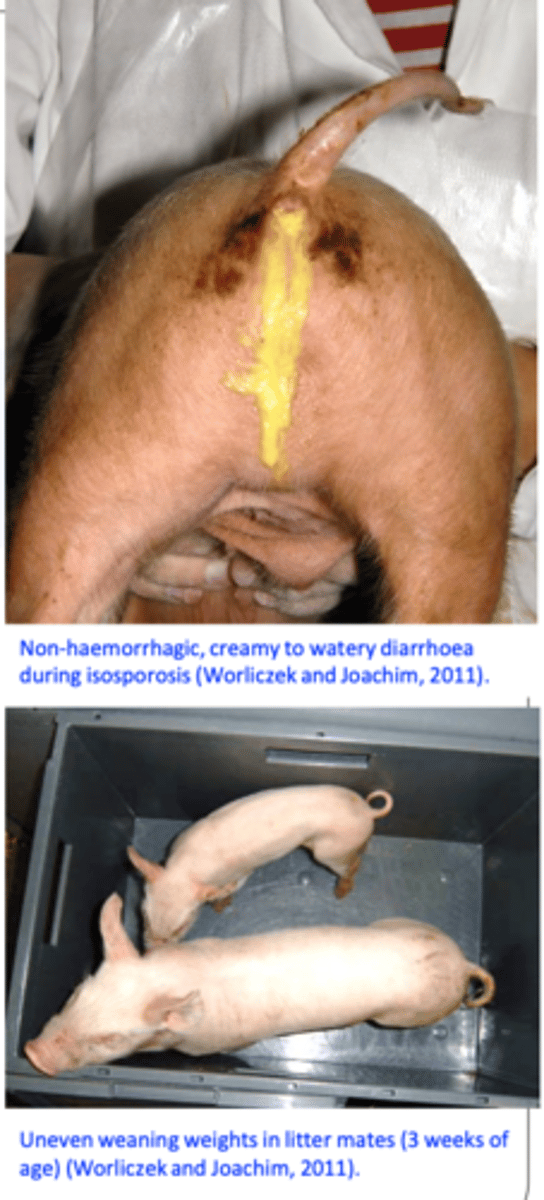
Commonly occur in pigs of 1-2 weeks of age;
Appear 3-5 days after infection (associated with the asexual stages) and last 3-7 days;
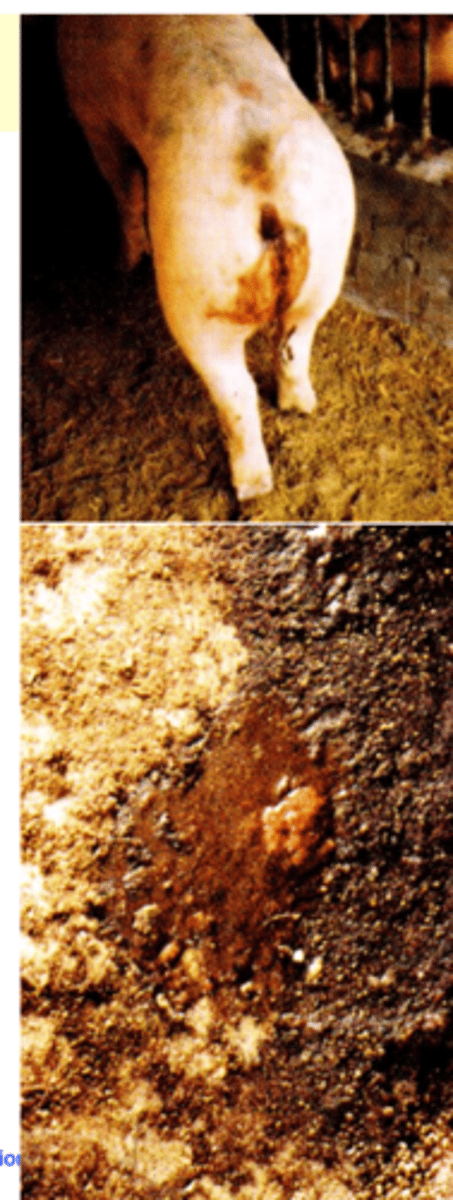
Yellowish/grayish diarrhoea, (non-haemorrhagic), liquid to pasty, foul smelling, that stains the perineum;
Dehydration, pigs are less active and depressed;
Reduced weight gains, weight loss not all the piglets in the litter are equally affected uneven weight gain and stunted growth;
Cystoisospora/Isospora suis
Diagnosis - LIVE ANIMALS
Live animals
History & clinical signs: diarrhoea in 1-2 week pigs that does not respond to antibiotics is suggestive;
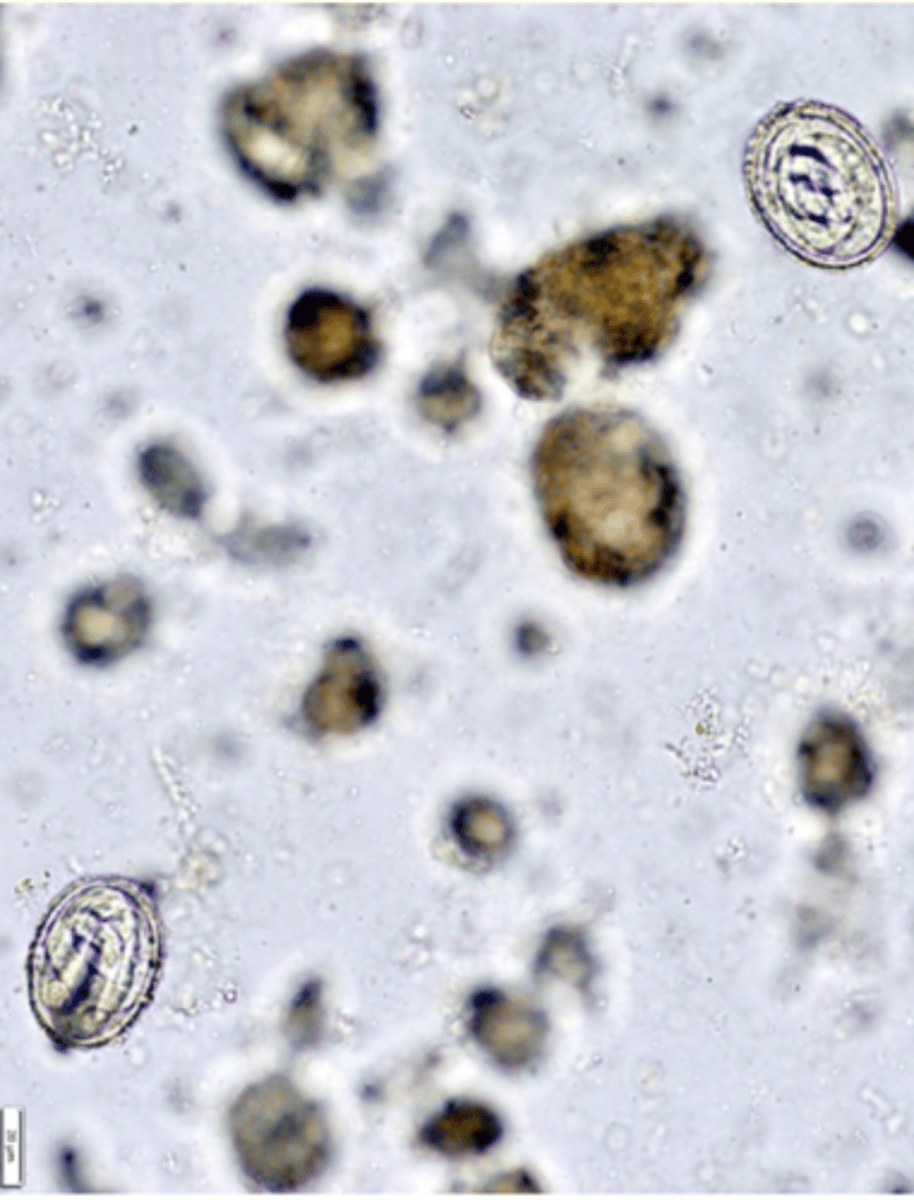
Identification of oocysts in the faeces: faecal flotations or direct smears;
High fat content of the faeces detection of oocysts is sometimes difficult epifluorescence might help visualization of oocysts (oocysts show autofluorescence);
PCR seems to be the most sensitive method
Cystoisospora/Isospora suis
Diagnosis - DEAD ANIMALS
Dead animals
Gut scrapings endogenous stages (the amount of endogenous stages might be low relative to the pathological effects);
Histopathology:
Differential diagnosis
Enteropathogenic E. coli, Clostridium perfringens type 3, Strongyloides ransomi, rotivirus etc.
Cystoisospora/Isospora suis TREATMENT
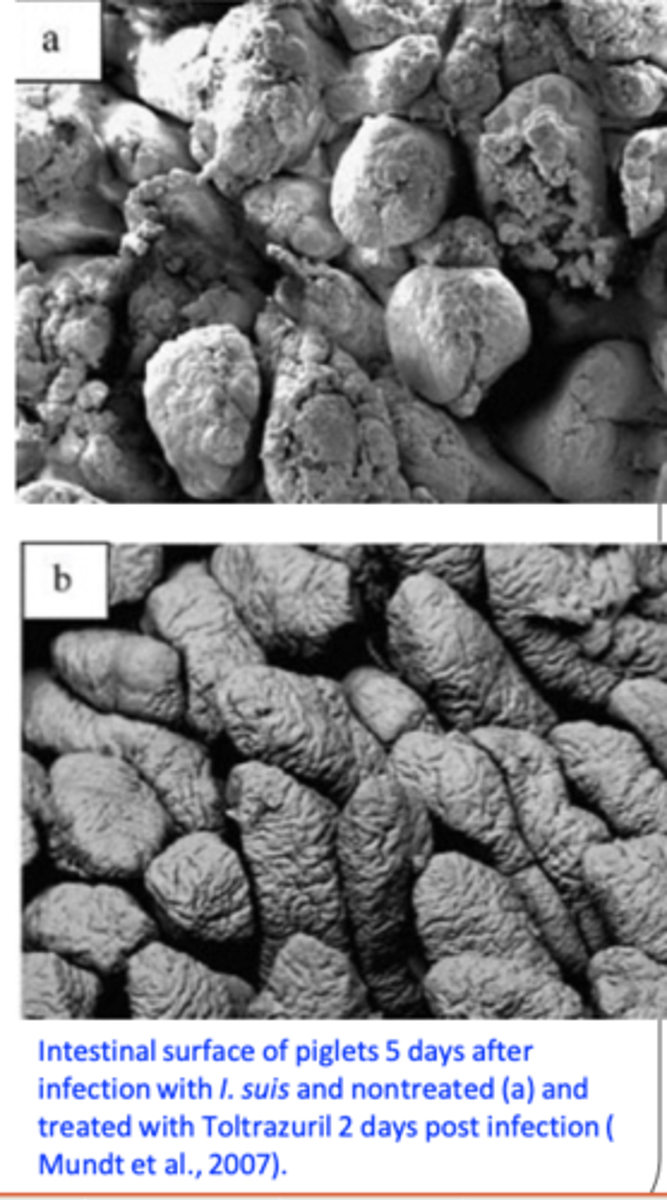
Toltrazuril (Baycox) (oral and injectable formulations)
Treat all the piglets in a litter, all infected and ‘at risk’ litters in the farrowing house.
• In stocks at risk treat metaphylactically when pigs are 3-5 days of age (this treatment prevent deaths and reduce losses);
Chemoresistance has developed

Cystoisospora/Isospora suis
Management and hygiene
All-in all-out, optimum stocking density;
Clean and disinfect the entire farrowing room after all the litters are weaned (use steam, burners etc);
Keep the farrowing rooms/pens dry and clean;
Disinfection with:
Bleach (at least 50%) or ammonia compounds for several hours or overnight; Neopredisan 135-1: associated with good results (availability in Australia?).
Trichuris suis
Location: caecum and colon:
may infect humans
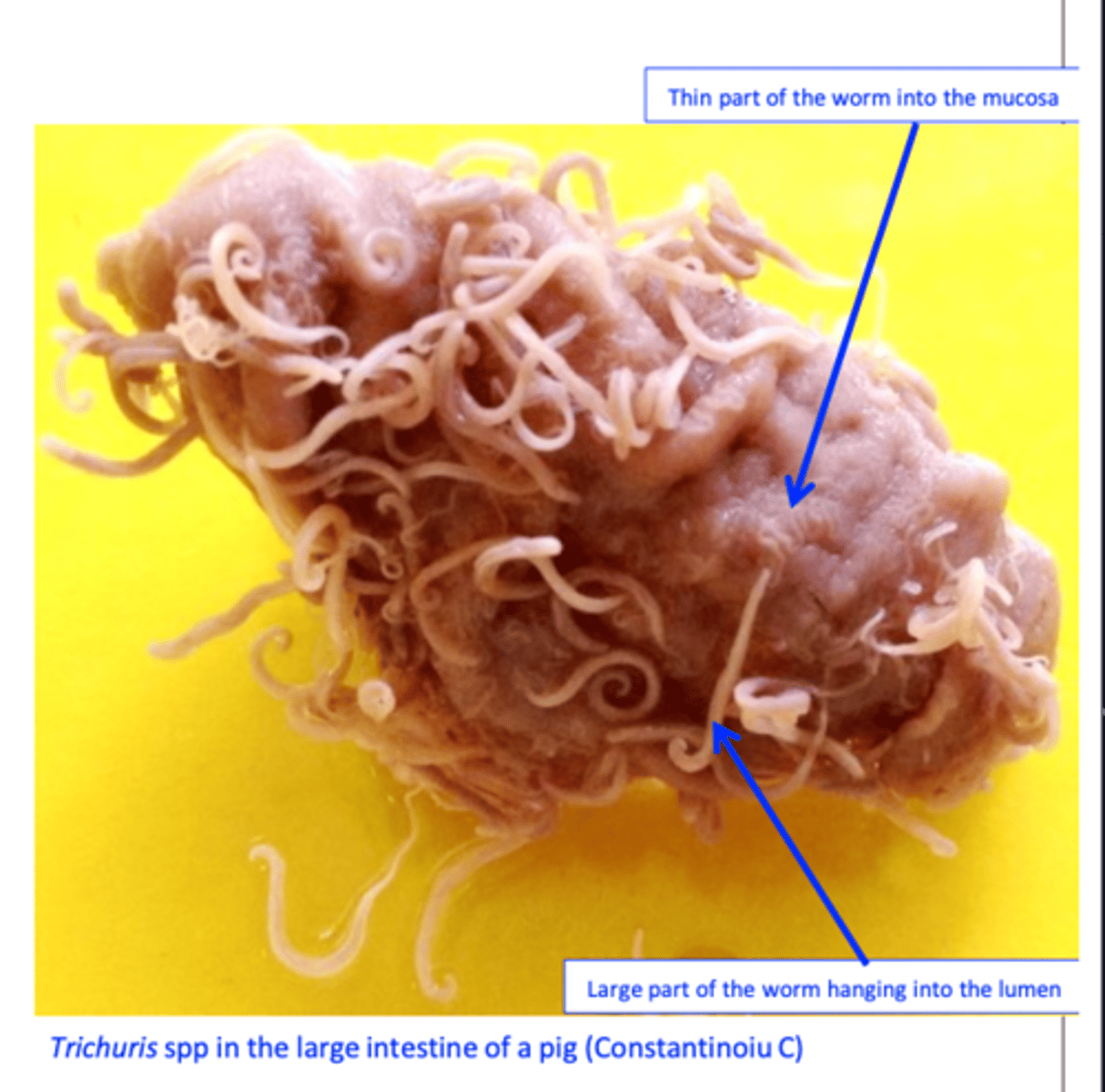
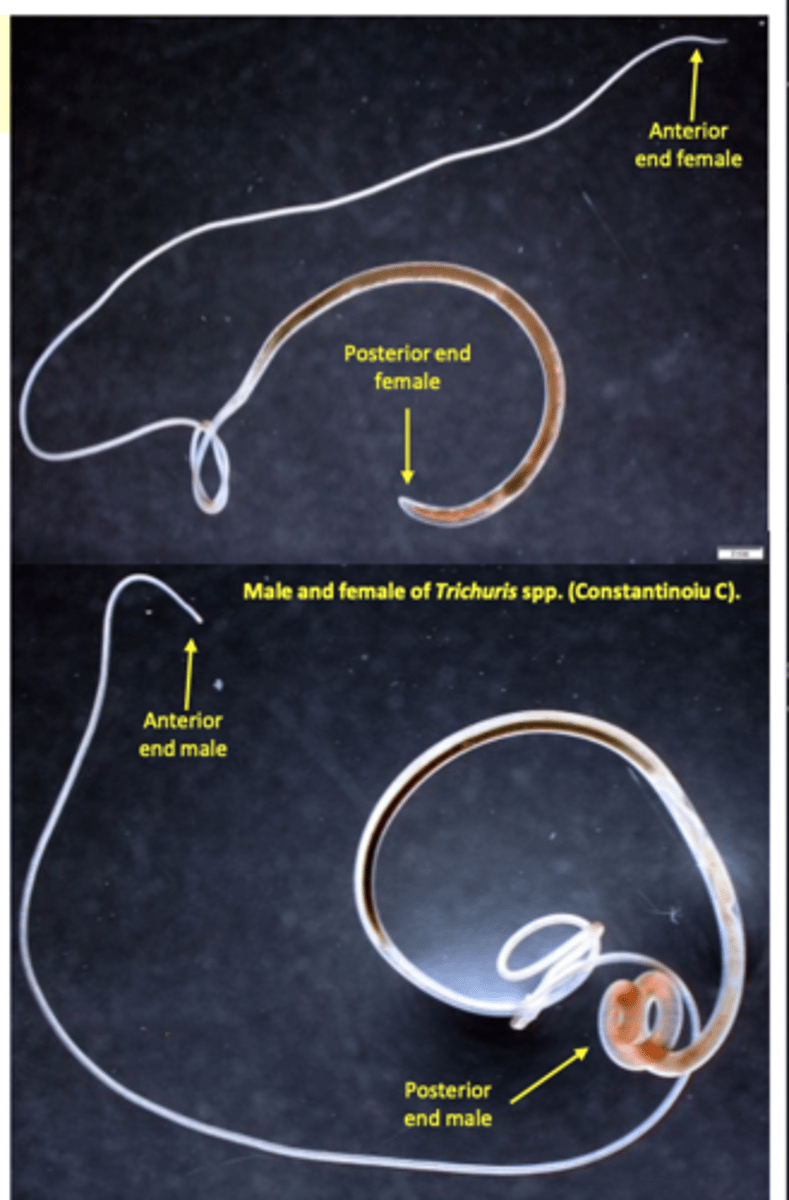
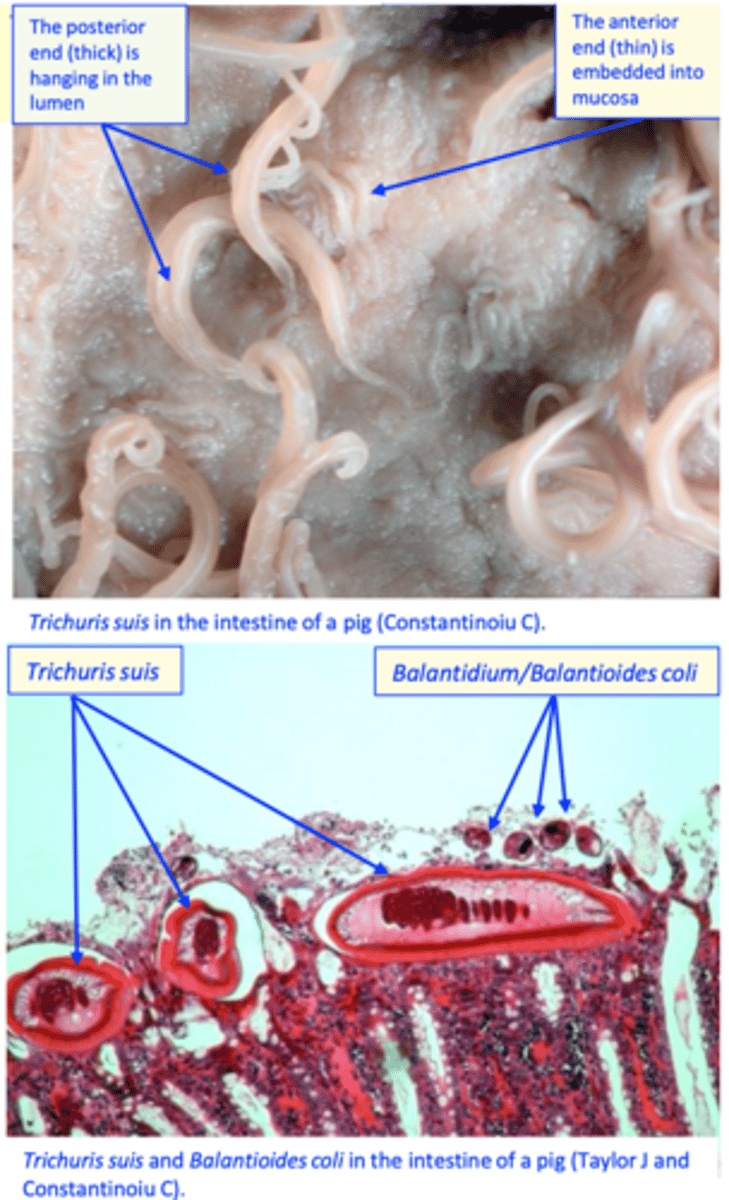
Trichuris morphology
Adult worms
Length: 6-8 cm female worms;
Body made up of two parts, slender, anterior one (2/3 of the body length) and a thick, posterior part;
Posterior end of the male: coiled, with one spicule;
Posterior end of the female: curved;
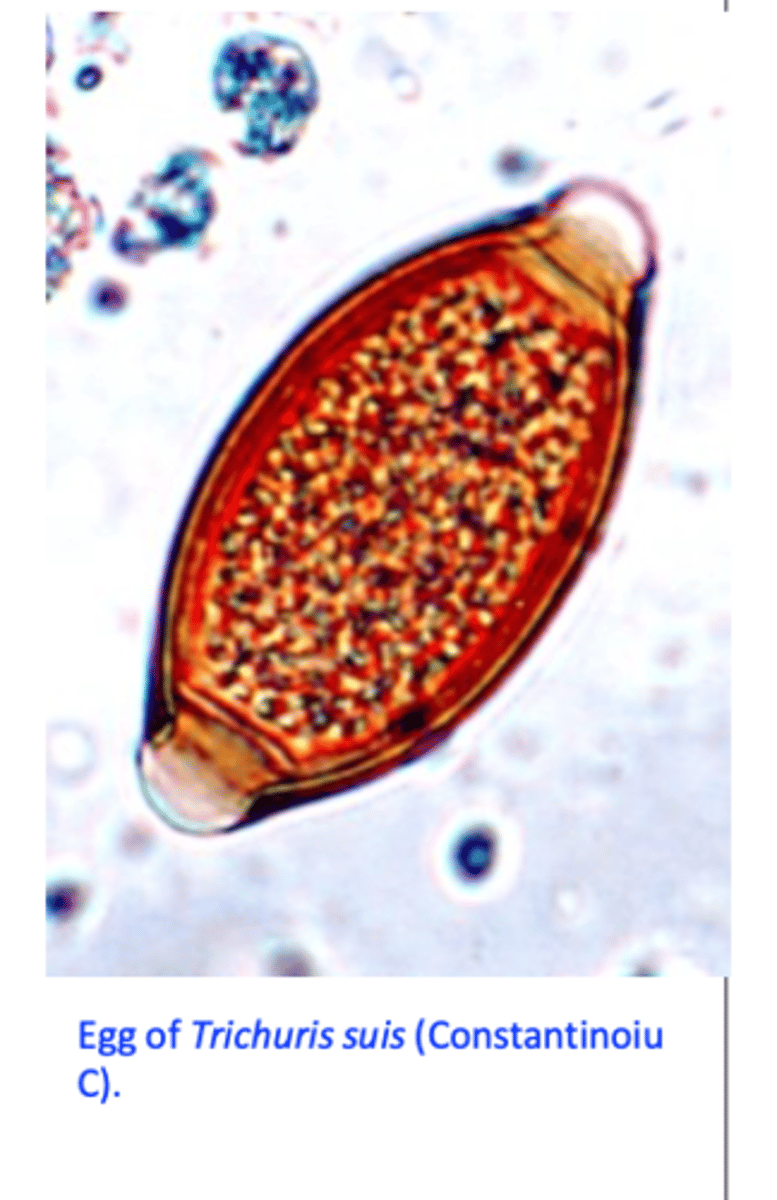
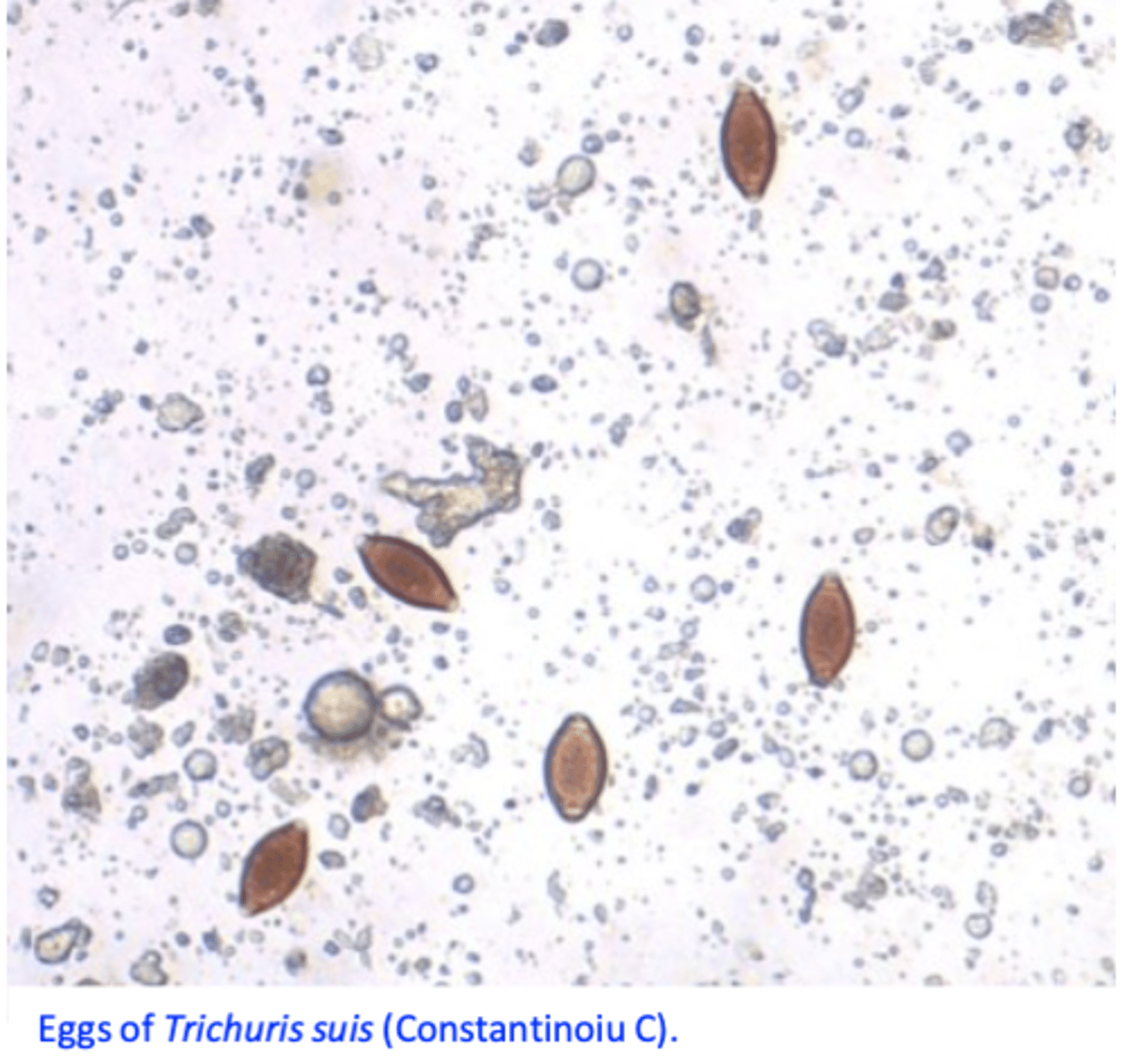
Trichuris eggs
Eggs
• 50-70 μm;• Lemon shaped;• Thick & smooth shell, yellow-brown; • Plugs at poles,• One cell inside;
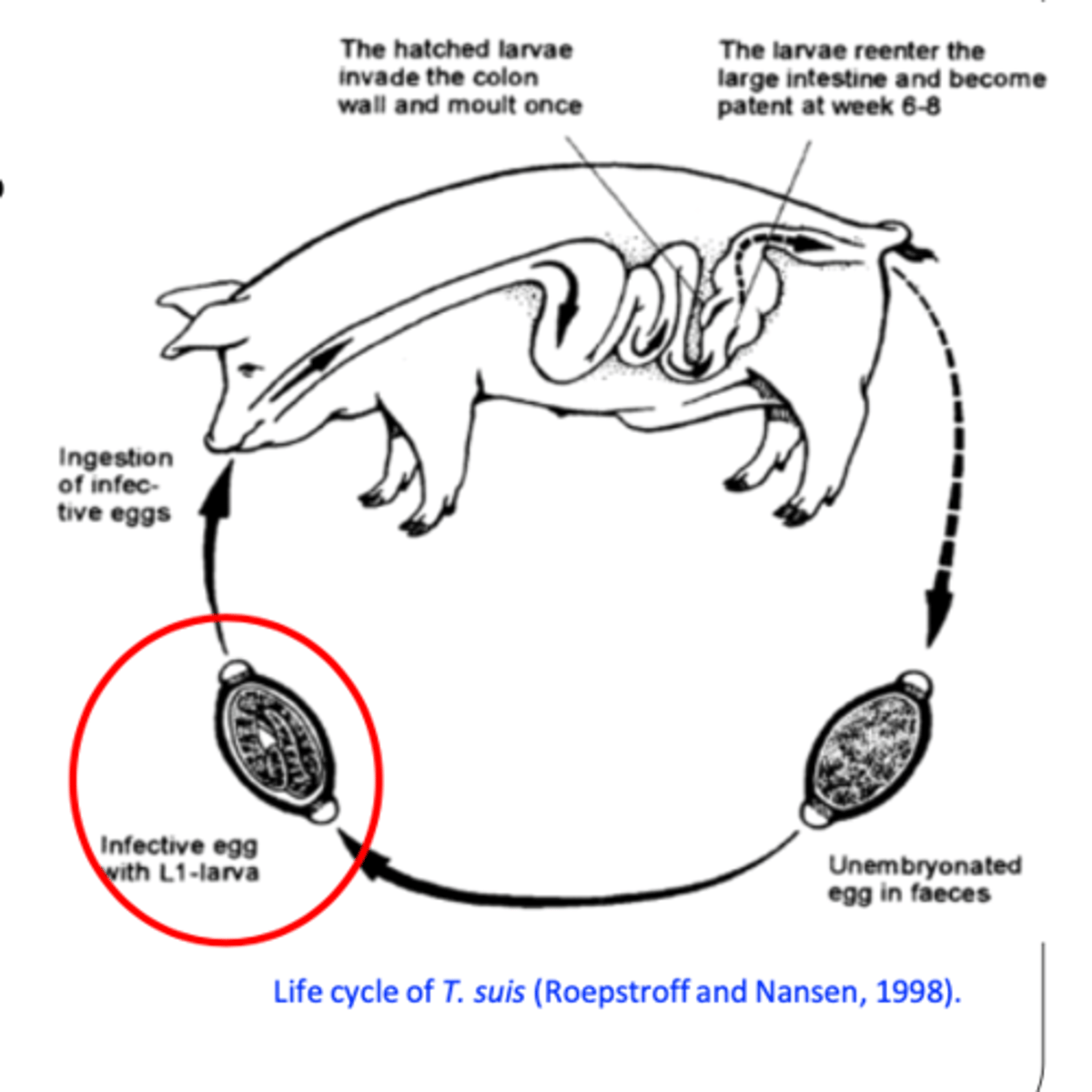
Trichuris suis
Life cycle
Eggs are passed in the faeces
infective larva develops slowly inside the eggs in 3-4 weeks (up to 6 months);
Infection: ingestion of embrionated eggs;
PPT: 6-8 weeks, life span: 4-5 months.
Trichuris suis
Epidemiology
Prevalence higher in free range/organic farms;
Eggs develop/become infective very slowly and in the intensive systems they are eliminated by cleaning/disinfection before they get infective
Common in herds housed on dirt lots/inadequate drainage of stagnant water etc (less common in pigs housed on concrete);
Growers and finisher (2-6 months of age) pigs are generally the most (heavily) infected - sows and boars have the lowest levels of
infection
Infection: ingestion of embrionated eggs
Eggs are very resistant in the environment (up to 6-11 years)
Trichuris suis
Pathogenesis/pathology
• Cause enterocyte destruction, ulcers --> secondary bacterial (Serpulina (Treponema) hyodysenteriae, Campylobacter and Pseudomonas aeruginosa) and Balantidium/Balantioides coli infections -> infections with T. suis might mimic swine dysentery
Erosion of the dilated blood vessels and mucosa -> hemorrhage, anemia and hypoalbuminaemia;
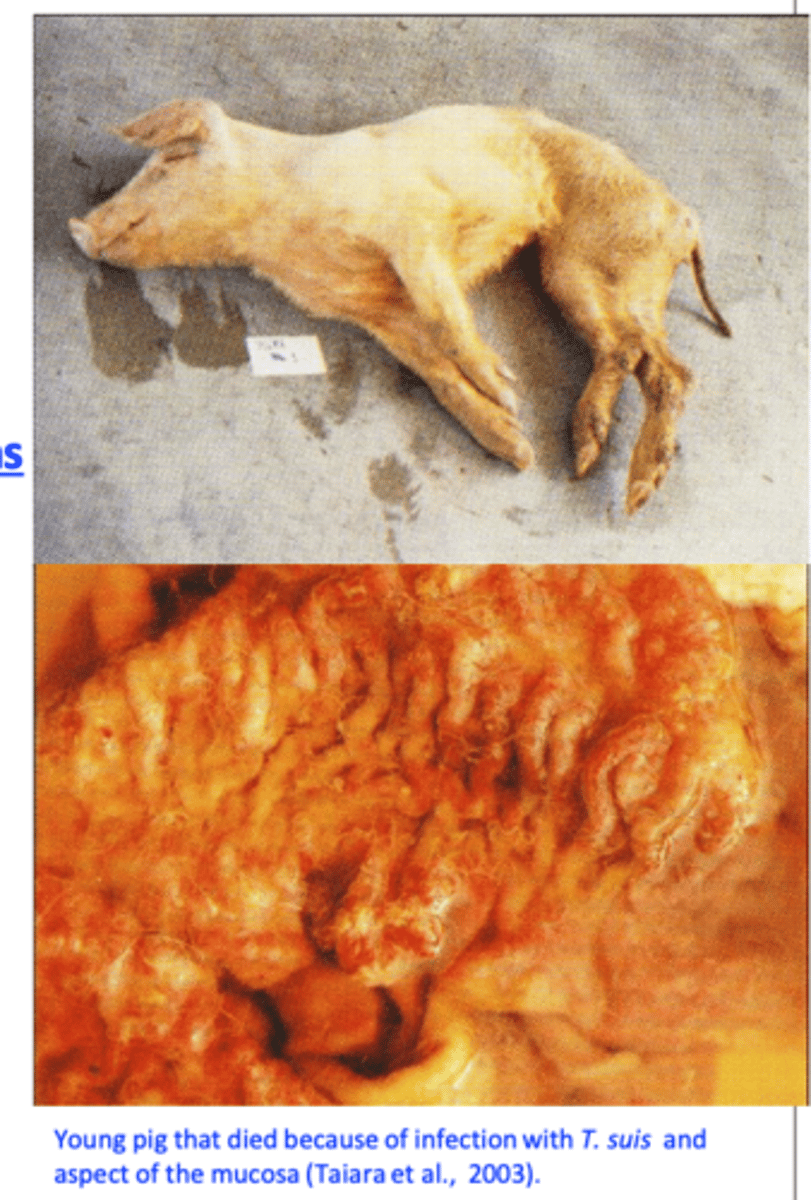
Trichuris suis
Clinical signs
• Light infections: no clinical signs;
• Massive infections (hundreds/thousands of parasites): anorexia, anemia, mucoid to bloody diarrhea, dehydration, retarded development and death;
Trichuris suis
Diagnosis LIVE animals
Clinical signs and history are not specific;
Detection of eggs in the faeces:
Clinical signs caused by larval stages;
Intermitent egg layers;
Eggs do not float easily;
Trichuris Suis
Diagnosis DEAD animals
• Visualization of the worms is relatively easy; • Histopathology;
Trichuris suis
Treatment
Benzimidazoles
- Fenbendazole (Safe-guard), flubendazole (Flubenol) and oxibendazole
Macrocyclic lactones
- Doramectin
Imidazothiazoles & tetrahydropyrimidines
- Levamisole
- Pyrantel: not active.
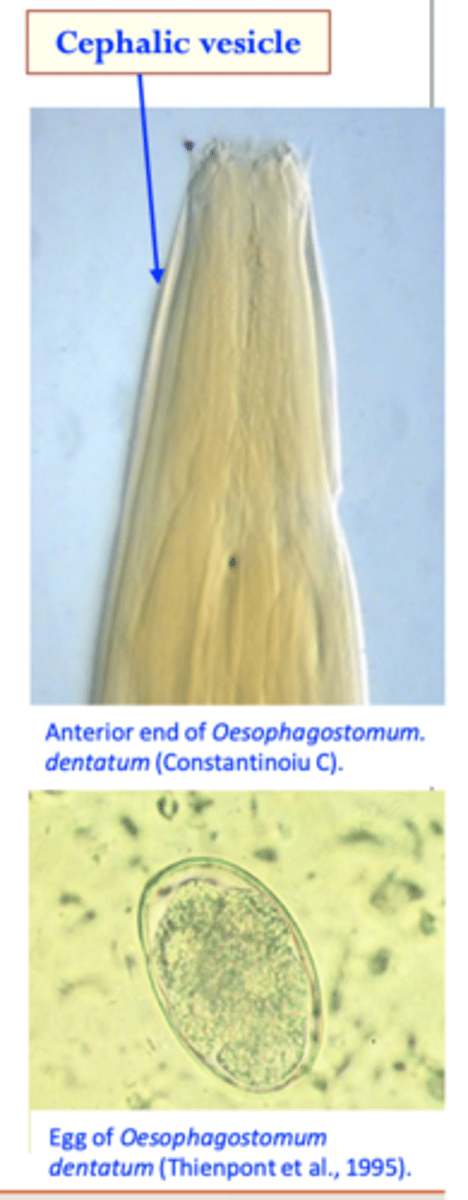
Oesophagostomum spp. (nodular worms)
Oesophagostomum dentatuum
Adult worms
Stout, whitish body;
Anterior end: cephalic vesicle present;
Posterior end: bursa in males;
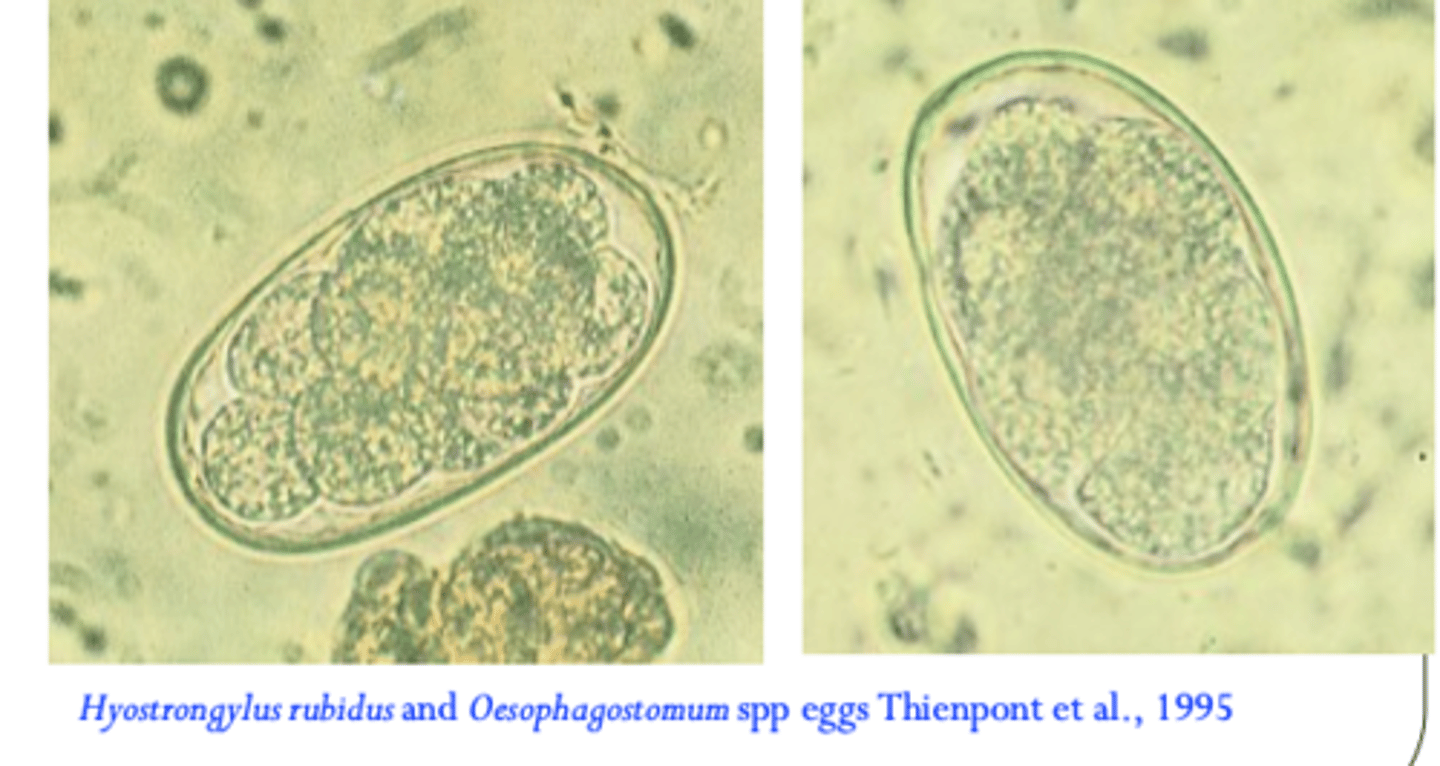
Eggs
• Ovoid;
• Thin shelled, morula stage;
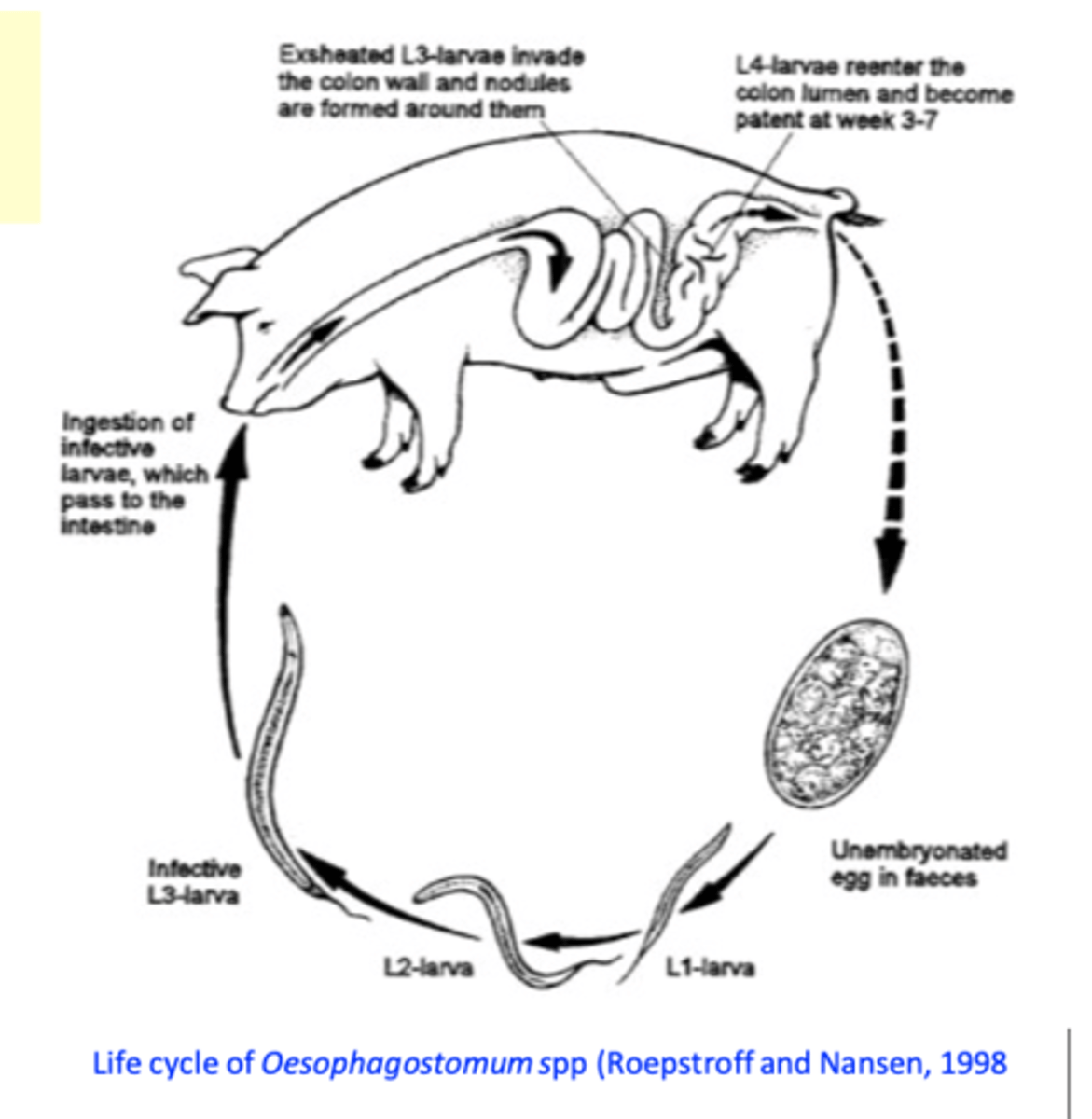
Oesophagostomum dentatuum: Life cycle
• Eggs are shed in the environment;
Egg -> L1 -> L2 -> L3: 7 days at 25-26C;
After ingestion L3s enter the submucosa of the large intestine and molt to L4 (cause nodules);
L4s return to the lumen and molt into adults;
Infection by ingestion of L3 L3 can survive one year outdoors
PPT: as short as 18-21 days
Oesophagostomum dentatuum: Epidemiology
Common in indoor and outdoor systems;
Low immunogenicity -> may accumulate in time -> infections are common in adult animals (breeding stock);
Pigs’ diet and age can have a significant influence on establishment and fecundity:
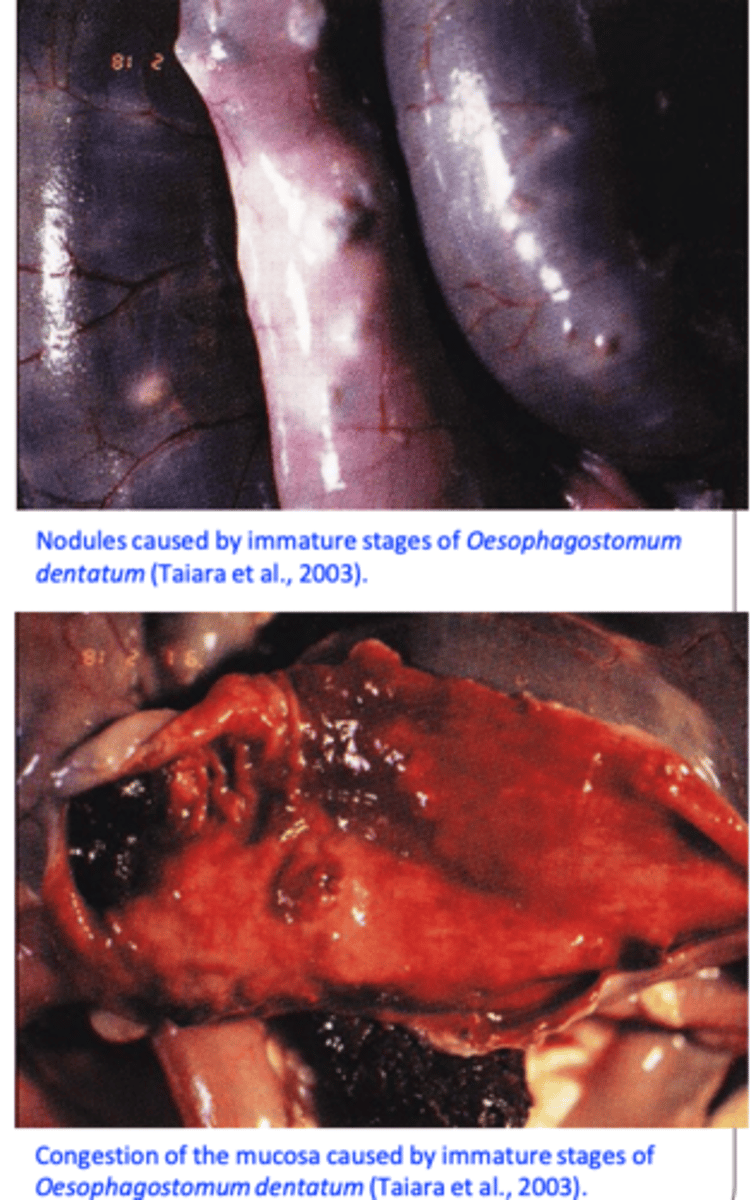
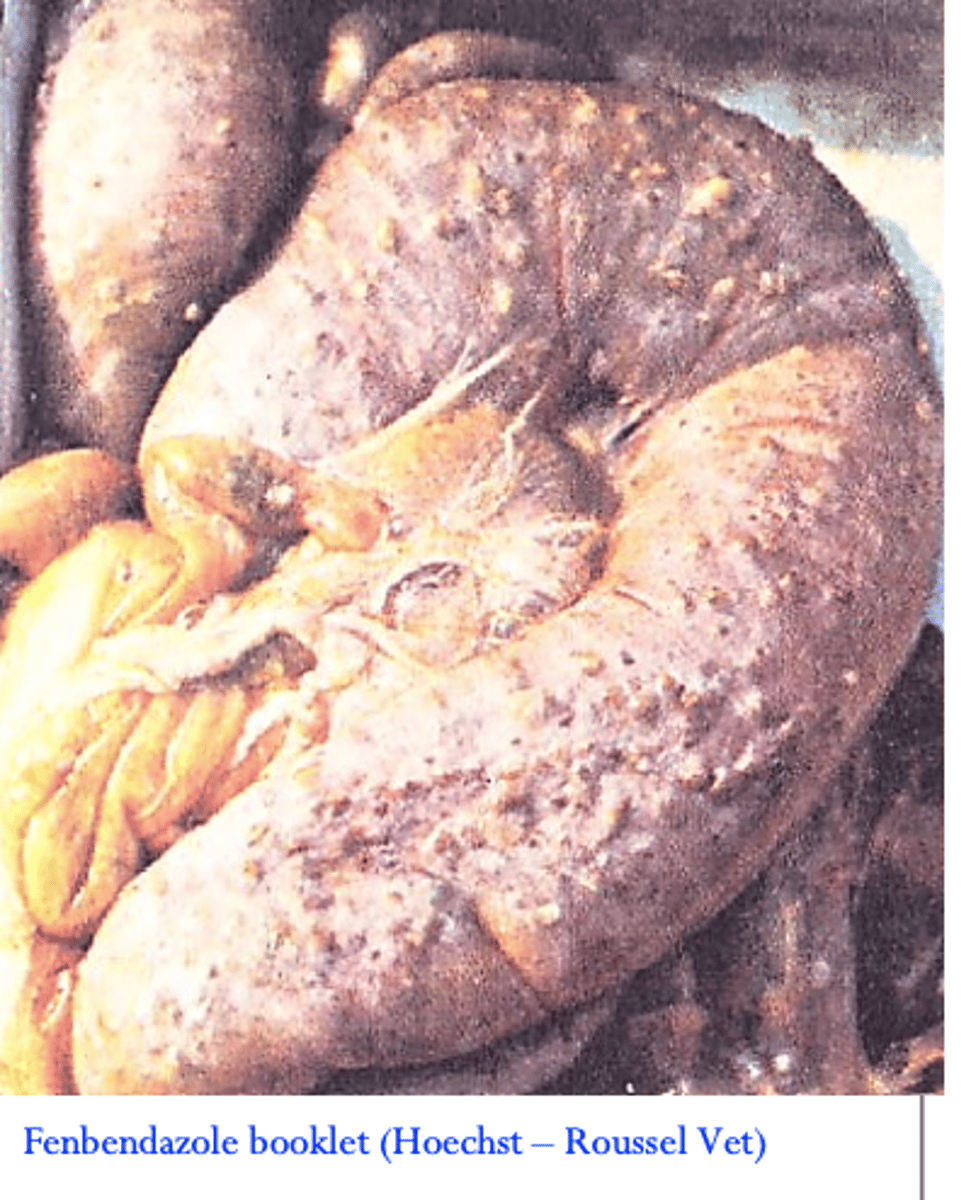
Oesophagostomum dentatuum: Pathology
• Adult worms cause minimum damage to the mucosa
of the large intestine;
L3 enters the mucosa of the caecum and colon -> the host responds by forming a nodule (hypersensitivity reaction) up to 5 mm in diameter;
Pathology caused by:
• Inflammation and nodular reaction induced by
invasion of the mucosa by larvae;• Emergence of the larvae from mucosa;
Heavy infections =congestion of the mucosa
O. dentatuum: Clinical signs
In pigs Oesophagostomum spp. seem to be less pathogenic
than in ruminants;
Infections with up to 5000 parasites per sow -> usually subclinical, greater burdens -> inappetence, weight loss (thin sow syndrome), reduced litter size and weaning weight;
O. dentatuum: DIAGNOSIS
•Finding eggs in the faeces (patent infections);
Thin shell, morula stage;
Oesophagostomum dentatuum: Treatment
Tetrahydropyrimidines: Pyrantel
Imidazothiazoles: Levamisol
Benzimidazoles: Fenbendazole, Flubendazole
Macrocyclic lactones (MLs): Abamectin, Ivermectin, Doramectin
Anthelmintic resistance to Pyrantel and Levamisole mentioned in the past;
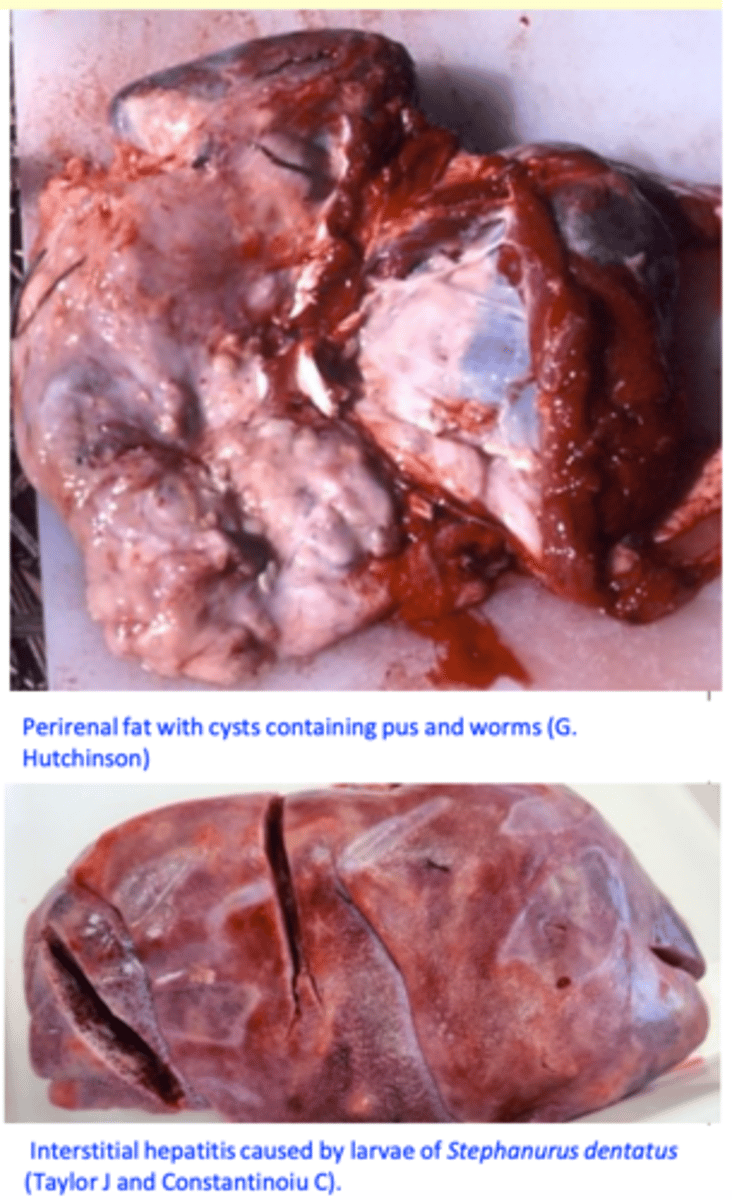
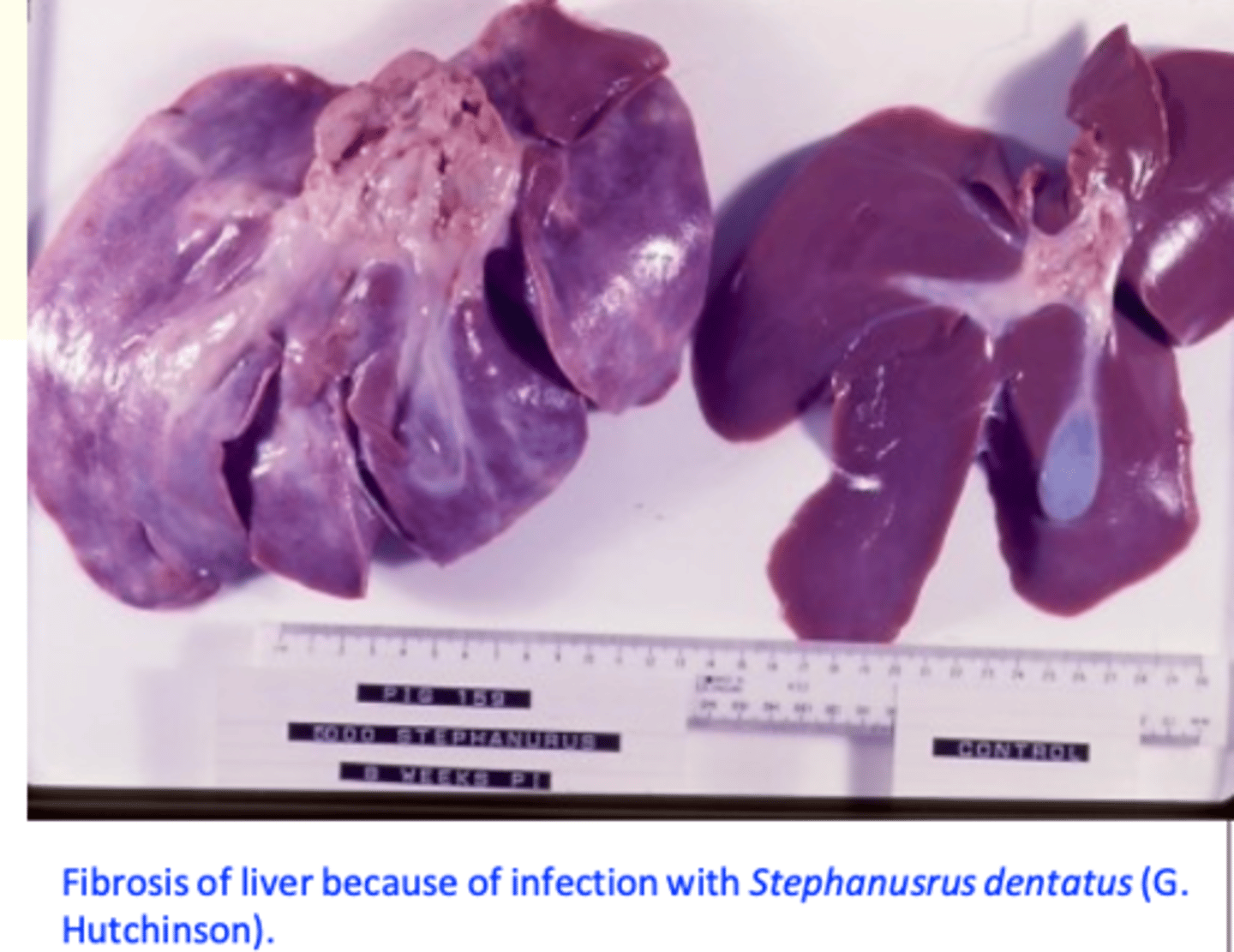
Stephanurus dentatus (Kidney worm of the pig)
Adults worms
Perirenal fat in cysts that are connected to the pelvis of the kidney or to the ureters;
Pelvis of the kidney;
Walls of ureters;
Larvae
• Liver, peritoneal cavity and other organs.
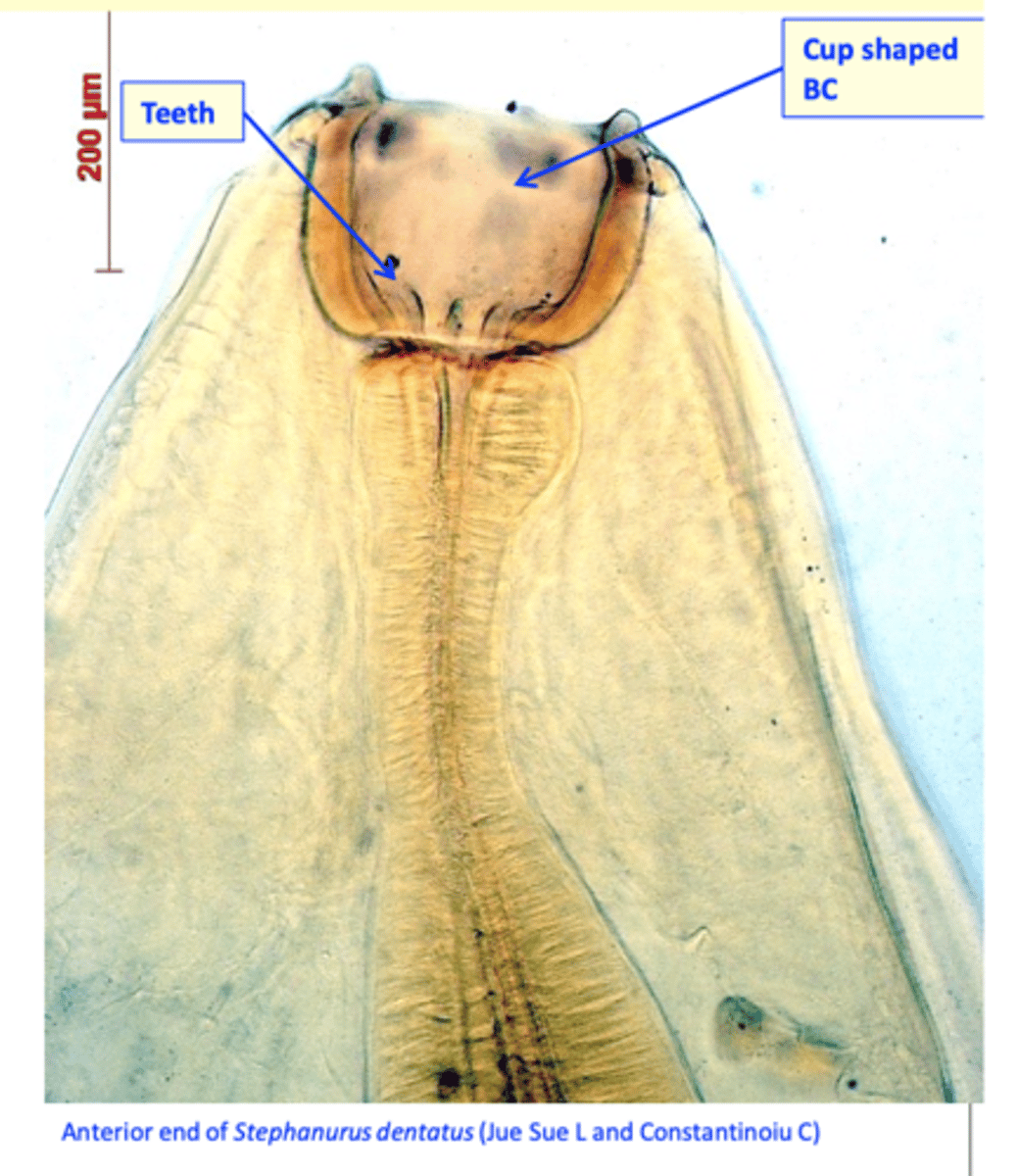
Stephanurus dentatus (Kidney worm of the pig)
Morphology
Adult worms
Stout worms, males up to 3 cm and
females up to 4.5 cm;
The cuticle is rather transparent internal organs are easily seen in fresh specimen;
The buccal capsule is cup shaped and thick walled, small leaf crown; triangular teeth at base of buccal capsule;
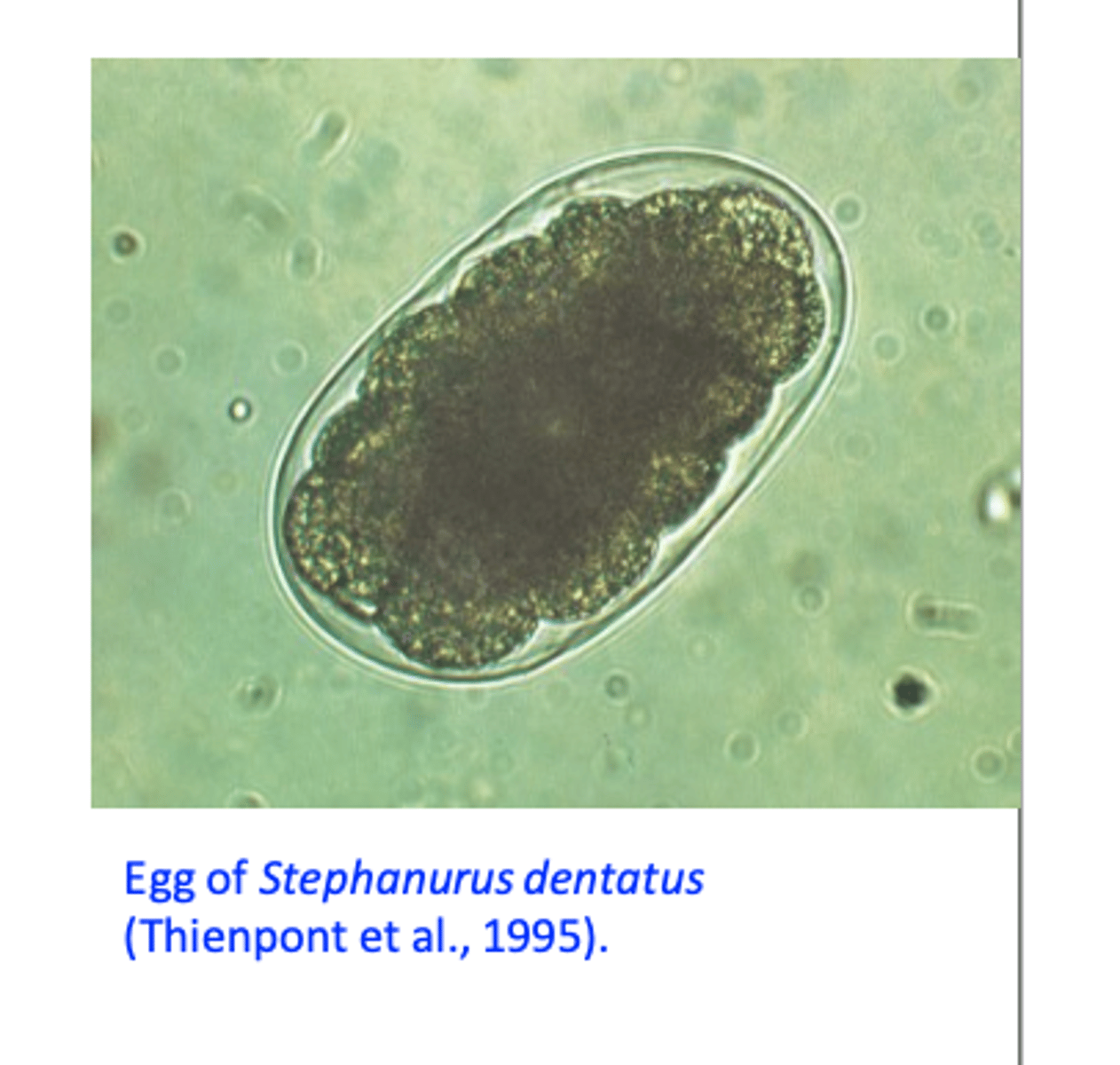
Stephanurus D EGGS
Thin shelled, morula stage (32-64 cells);
Passed in the urine.
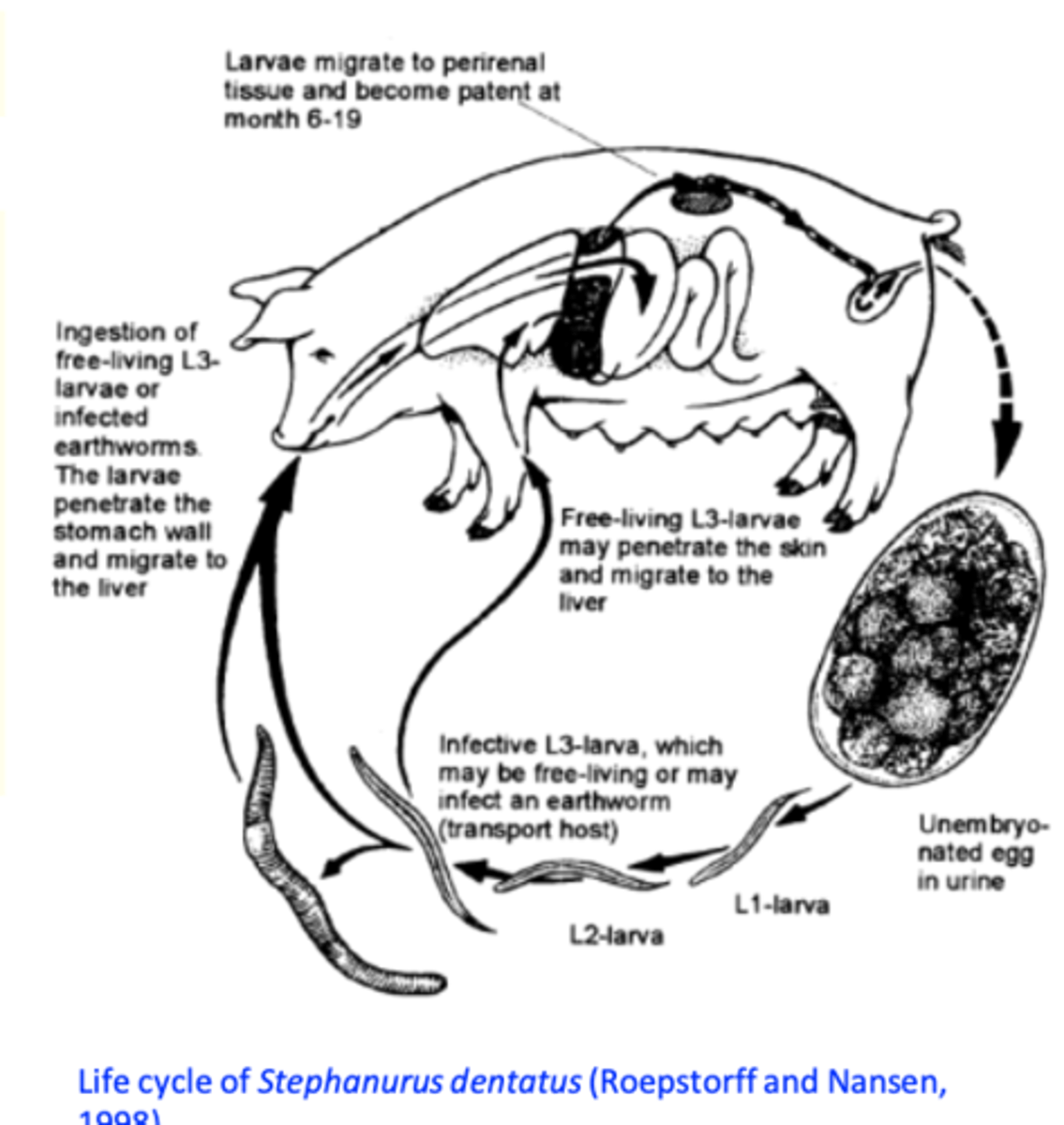
Stephanurus dentatus: Life cycle
Eggs are passed in the urine;
L1 -> L2 -> L3 in the environment; Earthworms may serve as transport hosts;
Infection of the host:
Ingestion of L3
Ingestion of transport hosts
Transcutaneously
- Larvae develop in the liver and migrate through peritoneal cavity to the perirenal region but they can migrate anywhere in the body;
PPT 6-11 months.
Stephanurus dentatus EPIDEMIOLOGY
Common in feral pigs (N Qld)
Limited to warm, moist areas in Australia (L3 are highly susceptible to desiccation);

Stephanurus dentatus - effect on host + DIAGNOSIS
Fibrosis in liver, abscesses in carcases -> organs condemned at slaughter;
Weight loss;
Diagnosis
• Detection of eggs in the urine sediment;
Stephanurus dentatus - TREATMENT + PREVENTION
Treatment
MLs: Ivermectin and Doramectin;
Imidazothiazoles: Levamisol;
Benzimidazoles: Fenbendazole (yes), Flubendazole (?);
Prevention
-Avoid exposure to L3 in wet/muddy conditions;
-House on concrete or slats;
-Separate young pigs from those >9 mos. which shed eggs (long PP).
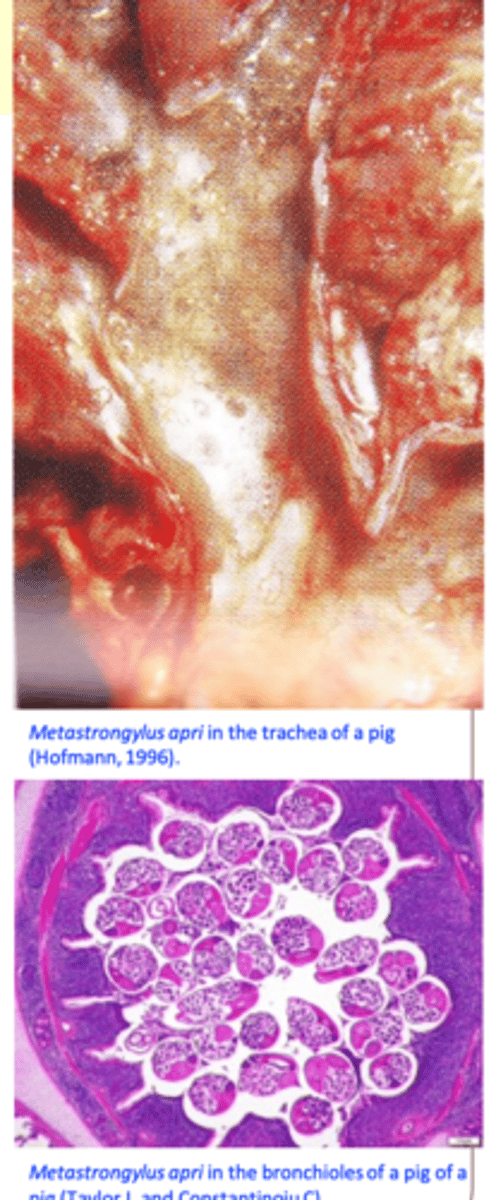
Metastrongylus spp.
Location: bronchi, bronchioles
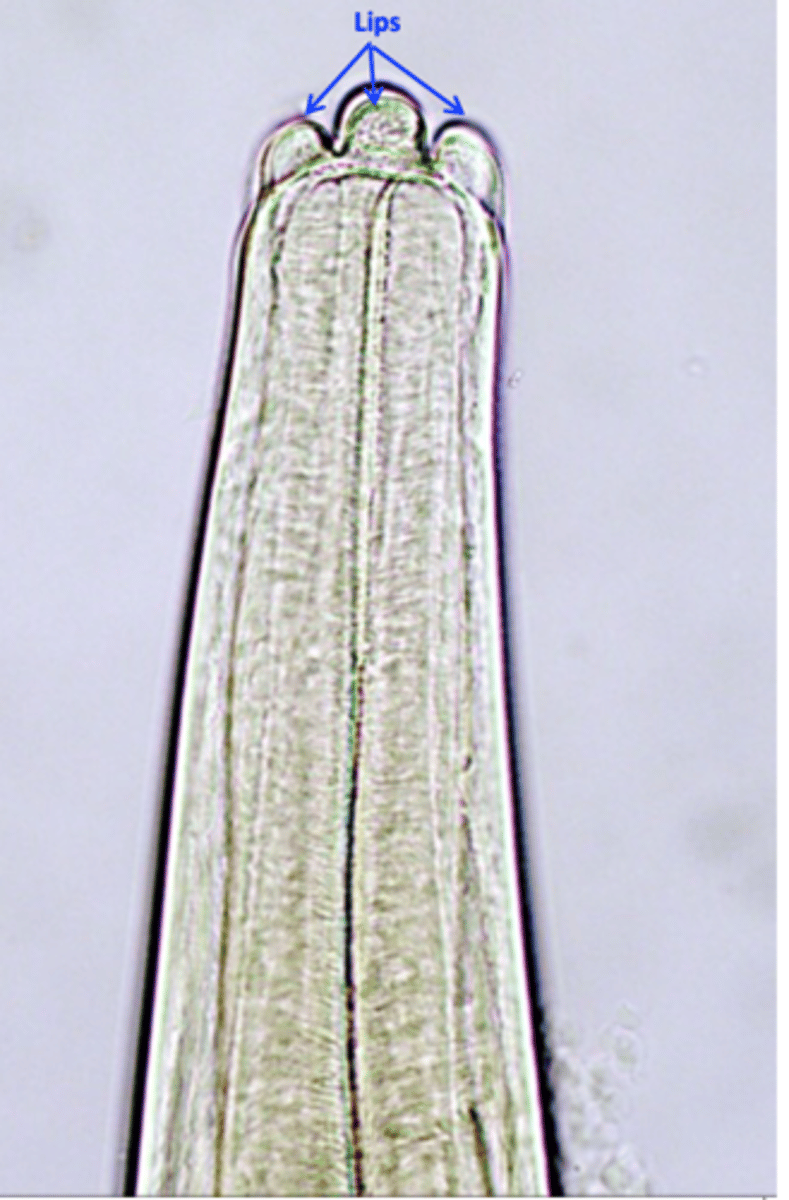
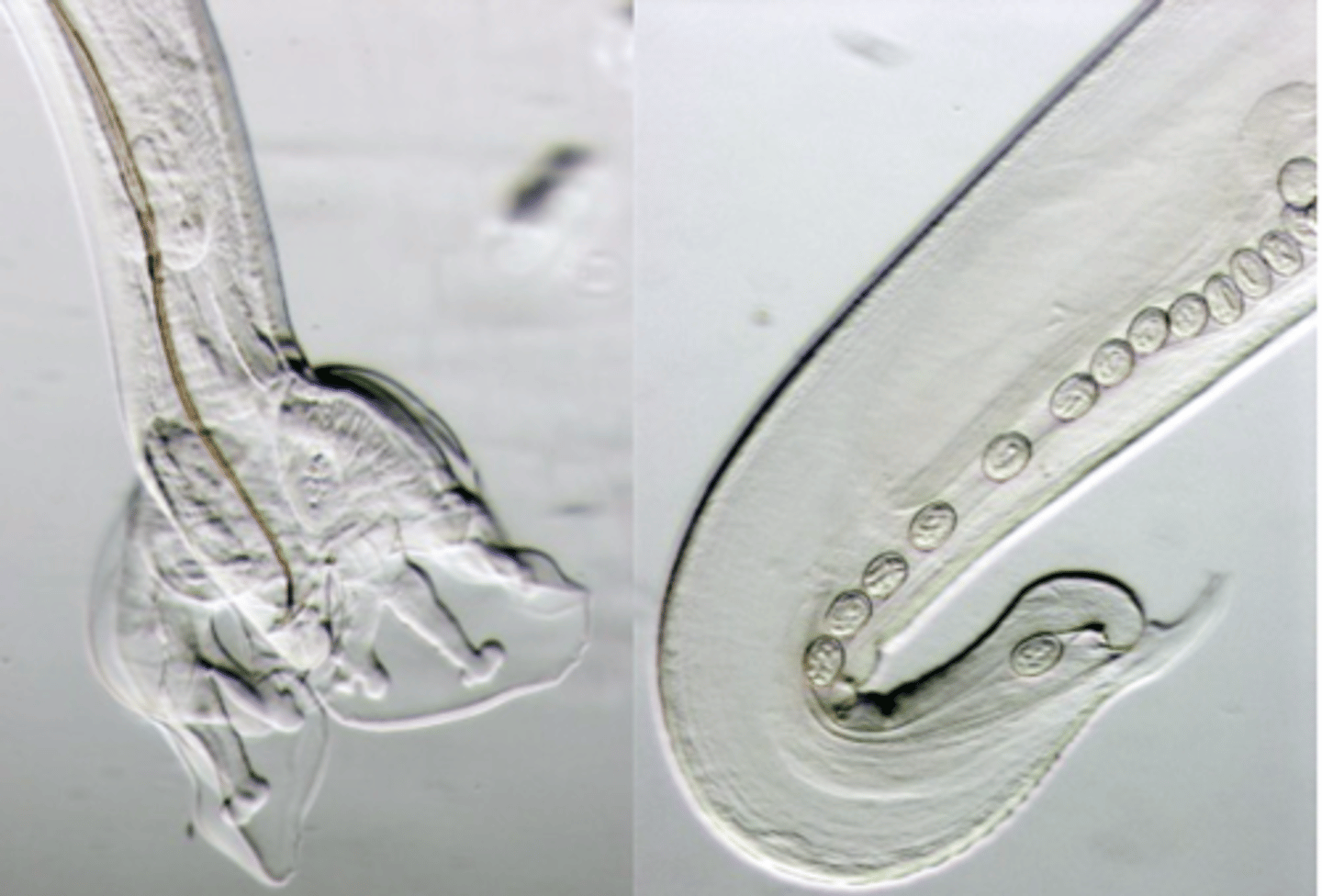
Metastrongylus MORPHOLOGY
Adult worms
White, filiform body;
Mouth with 2 trilobed lips;
Bursal rays of specific shape (some end in swellings);
The spicules are long and transversally striated;
The posterior end of the female appears digitiform (prevulvar swelling);
Metastrongylus EGGS
Have a corrugated surface and are embryonated when
laid.

Metastrongylus spp. Life cycle
Intermediate hosts: earthworms -> outdoor systems;
Pigs become infected after ingestion of earthworms that have in their body infective larvae;
Metastrongylus spp. Clinical signs
• Pigs 4 - 6 months old usually affected: coughing, dyspnoea, unthriftiness;
Metastrongylus spp. Diagnosis
Clinical signs, outdoor systems, age;
Identification of the eggs in the faeces
Metastrongylus spp. Treatment
Benzimidazoles
Fenbendazole
Flubendazole
MLs
ivermectin
doramectin
Imidazothiazoles
levamisole