Integration of Metabolism: Insulin and Glucagon Effects
1/253
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
254 Terms
Insulin
A polypeptide hormone produced by the β cells of the islets of Langerhans in the pancreas, which coordinates the use of fuels by tissues and promotes anabolic processes.
Glucagon
A peptide hormone secreted by the α cells of the islets of Langerhans that stimulates the release of glucose into the bloodstream, particularly during fasting or low-energy states.
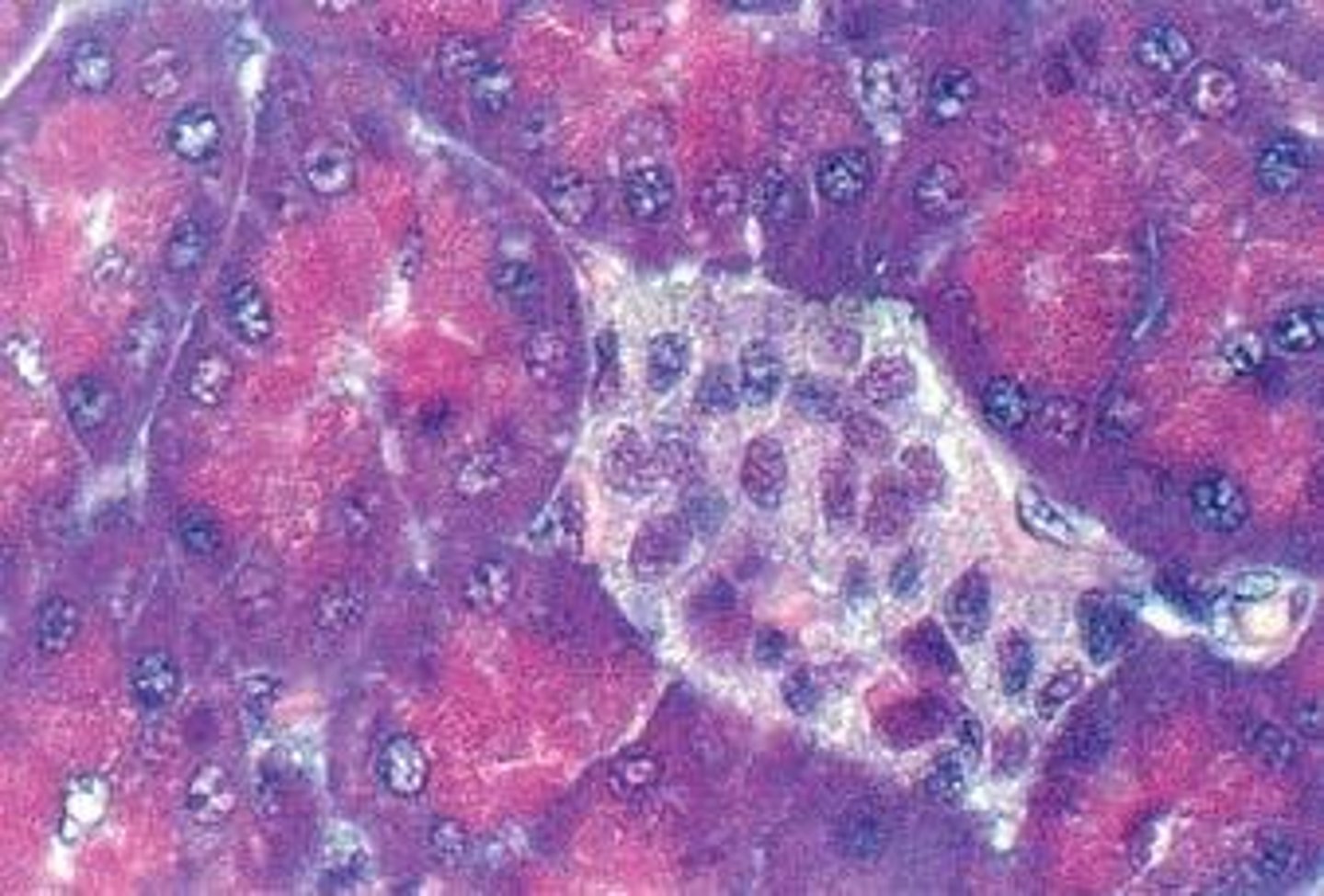
Islets of Langerhans
Clusters of cells in the pancreas that contain insulin-producing β cells and glucagon-producing α cells, playing a crucial role in regulating blood sugar levels.
Anabolic
Referring to metabolic processes that build larger molecules from smaller ones, such as the synthesis of glycogen, proteins, and lipids.
C-peptide
A connecting peptide released during the conversion of proinsulin to insulin, which serves as a marker for insulin production.
Epinephrine
A catecholamine hormone released by the adrenal glands that increases heart rate and energy availability, often involved in the 'fight-or-flight' response.
Insulinase
An enzyme that degrades insulin, primarily found in the liver and kidneys, responsible for regulating insulin levels in the bloodstream.
Plasma half-life
The time it takes for the concentration of a substance in the blood to reduce to half its initial value, indicating the duration of a hormone's action.
Energy metabolism
The biochemical processes that convert food into energy, involving the storage, utilization, and generation of energy substrates in the body.
Circulating substrates
Nutrients and metabolites present in the bloodstream that can be utilized by tissues for energy production and metabolic processes.
Nucleus
The membrane-bound organelle that contains the genetic material of a cell and is responsible for regulating gene expression.
Translation
The process by which ribosomes synthesize proteins using the information encoded in messenger RNA (mRNA).
Signal Sequence
A short peptide sequence that directs the transport of a protein to its proper location within the cell.
Rough Endoplasmic Reticulum (RER)
A type of endoplasmic reticulum studded with ribosomes, where protein synthesis and folding occur.
Proinsulin
An inactive precursor of insulin that is processed in the endoplasmic reticulum and Golgi apparatus to form active insulin.
Golgi Apparatus
An organelle that modifies, sorts, and packages proteins and lipids for secretion or delivery to other organelles.
Secretory Granules
Membrane-bound vesicles that store hormones and neurotransmitters, releasing their contents through exocytosis.
Insulin Secretion
The release of insulin from pancreatic beta cells in response to elevated blood glucose levels.
Incretins
Gastrointestinal hormones that enhance insulin secretion in response to food intake.
Glucose Sensing
The ability of pancreatic beta cells to detect and respond to changes in blood glucose levels.
Calcium Influx
The entry of calcium ions into cells, which triggers various cellular processes, including the release of insulin.
ATP-sensitive Potassium Channels
Ion channels in the cell membrane that regulate the flow of potassium ions and are involved in insulin secretion.
Sulfonylureas
A class of oral medications used to treat type 2 diabetes by stimulating insulin secretion from pancreatic beta cells.
Glycogenolysis
The process of breaking down glycogen into glucose, primarily occurring in the liver and muscle.
Gluconeogenesis
The metabolic process of generating glucose from non-carbohydrate substrates, mainly in the liver.
Glucose Transporter (GLUT-4)
A protein that facilitates the transport of glucose into cells, particularly in muscle and adipose tissue, in response to insulin.
Adipose Tissue
Body fat that stores energy in the form of triacylglycerols and plays a role in metabolism.
Triacylglycerol
A type of fat found in the body, composed of glycerol and three fatty acids, which serves as a major form of energy storage.
Hormone-sensitive Lipase
An enzyme that breaks down stored fat (triacylglycerols) into free fatty acids and glycerol, regulated by hormones.
Insulin Receptor
A specific receptor on cell membranes that binds insulin and initiates a signaling cascade to promote glucose uptake and metabolism.
Insulin Receptor Substrate (IRS)
Proteins that are phosphorylated by the insulin receptor and mediate various biological effects of insulin.
Protein Synthesis
The process by which cells build proteins, stimulated by insulin through the uptake of amino acids.
Lipoprotein Lipase
An enzyme that hydrolyzes triglycerides in lipoproteins into free fatty acids, facilitating their uptake by tissues.
Dephosphorylation
The removal of phosphate groups from proteins, often leading to a decrease in activity, as seen in hormone regulation.
Biologic Actions of Insulin
The diverse effects of insulin on glucose uptake, glycogen synthesis, lipid metabolism, and protein synthesis.
Sympathetic Nervous System
A part of the autonomic nervous system that prepares the body for stress-related activities, influencing hormone release.
Blood Glucose Concentration
The level of glucose in the bloodstream, which is tightly regulated by hormones such as insulin and glucagon.
Metabolic Effects of Insulin
The various physiological changes induced by insulin that promote energy storage and utilization in the body.
Signal transduction
The process by which a cell converts an external signal, such as hormone binding, into a functional response.
Autophosphorylation
The process by which a kinase enzyme adds a phosphate group to itself, often leading to activation of signaling pathways.
Endosome
An organelle formed by the fusion of vesicles that transport materials within the cell, including insulin and its receptors.
Ketogenesis
The process of producing ketone bodies from fatty acids, typically occurring in the liver during low carbohydrate intake.
Lipolysis
The breakdown of fats and other lipids to release fatty acids, often stimulated by hormones like glucagon.
Receptor internalization
The process by which a cell takes in a receptor-ligand complex, often leading to receptor degradation or recycling.
Down-regulation
The process by which a cell decreases the quantity of a cellular component, such as receptors, in response to an external signal.
Facilitated transport
A process of passive transport that uses specific transport proteins to move molecules across a cell membrane.
Active transport
The movement of molecules across a cell membrane against their concentration gradient, requiring energy.
Skeletal muscle
A type of muscle tissue that is under voluntary control and is responsible for movement and glucose uptake in response to insulin.
Insulin-sensitive tissues
Tissues that require insulin for glucose uptake, such as skeletal muscle and adipose tissue.
Insulin-insensitive tissues
Tissues that can uptake glucose without the need for insulin, such as the brain and liver.
α Cells
Cells in the pancreatic islets of Langerhans that secrete glucagon in response to low blood glucose levels.
Preproglucagon
The large precursor molecule from which glucagon is synthesized through proteolytic cleavage.
Counter-regulatory hormones
Hormones that oppose the actions of insulin, including glucagon, epinephrine, cortisol, and growth hormone.
Amino Acids
Organic compounds that stimulate the release of both glucagon and insulin, particularly after protein-rich meals.
G protein-coupled receptors
Receptors on the cell membrane that glucagon binds to in order to exert its biological effects.
cAMP
Cyclic adenosine monophosphate, a secondary messenger involved in the signaling pathway activated by glucagon.
Hypoglycemia
A condition characterized by abnormally low blood glucose levels, which stimulates glucagon secretion.
Proteolytic cleavage
The process of breaking down proteins into smaller peptides or amino acids, crucial for converting preproglucagon to glucagon.
Adenylyl Cyclase
An enzyme that converts ATP to cyclic AMP, playing a crucial role in signal transduction pathways.
Adrenergic Symptoms
Physical responses such as anxiety and palpitations that occur due to the release of epinephrine in response to low blood sugar.
Neuroglycopenia
A state of impaired brain function due to insufficient glucose supply, resulting in symptoms like confusion and seizures.
Cortisol
A steroid hormone released by the adrenal cortex that helps regulate metabolism and the body's response to stress.
ACTH
Adrenocorticotropic hormone, which stimulates the adrenal cortex to produce cortisol in response to stress.
Growth Hormone
A hormone that stimulates growth and cell reproduction, also playing a role in increasing blood glucose levels by promoting lipolysis and reducing glucose uptake in tissues.
Insulin-induced hypoglycemia
A type of hypoglycemia that occurs in patients with diabetes who are receiving insulin treatment, often requiring immediate carbohydrate intake or glucagon administration.
Postprandial hypoglycemia
A form of hypoglycemia that occurs after meals due to excessive insulin release, leading to transient low blood sugar levels.
Fasting hypoglycemia
A rare condition where blood glucose levels drop significantly during fasting, potentially due to liver dysfunction or excessive insulin production.
Alcohol-induced hypoglycemia
A condition where alcohol consumption leads to low blood sugar levels, particularly in fasting individuals, due to impaired gluconeogenesis.
Ethanol
A type of alcohol that, when consumed, affects metabolic pathways in the liver, leading to increased NADH levels.
NADH
A reduced form of nicotinamide adenine dinucleotide, which acts as an electron carrier in cellular respiration and is increased during ethanol metabolism.
Disulfiram
A medication that inhibits aldehyde dehydrogenase, leading to increased acetaldehyde levels and unpleasant reactions when alcohol is consumed.
Lactic Acidosis
A condition characterized by the accumulation of lactic acid in the body, often resulting from increased NADH levels and the conversion of pyruvate to lactate.
Acetaldehyde
A toxic intermediate produced during ethanol metabolism that accumulates when disulfiram is used.
Alcoholic Fatty Liver
A condition resulting from chronic alcohol consumption, characterized by the accumulation of fat in liver cells due to disrupted lipid metabolism.
Ketone Bodies
Metabolic products formed from the breakdown of fatty acids, which can be produced when acetyl CoA is diverted away from the citric acid cycle.
Acetyl CoA
A central metabolite in energy metabolism that can enter the citric acid cycle or be converted into ketone bodies.
Triacylglycerols
A type of fat found in the body, which can accumulate in the liver due to increased lipogenesis associated with ethanol metabolism.
Cirrhosis
A late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases, including chronic alcohol consumption.
IRS proteins
A family of proteins that mediate the signaling pathways activated by insulin receptor phosphorylation.
Adenylate cyclase
An enzyme activated by glucagon that converts ATP to cyclic AMP, a secondary messenger in cellular signaling.
Gene transcription
The process by which genetic information is copied from DNA to RNA, influenced by insulin and glucagon.
Phosphorylation
The addition of a phosphate group to a protein, which can activate or deactivate its function, often mediated by insulin and glucagon signaling.
Liver
An organ that plays a crucial role in glucose metabolism, responding to both insulin and glucagon.
Central nervous system symptoms
Symptoms such as confusion and aberrant behavior that can occur during hypoglycemia.
Immediate secretion of glucagon
The rapid release of glucagon in response to low blood glucose levels to restore glucose homeostasis.
Oral glucose administration
The method of treating hypoglycemia in conscious patients by providing glucose to rapidly increase blood sugar levels.
3-Hydroxybutyrate
A type of ketone body produced in the liver during periods of low insulin levels, serving as an alternative energy source.
Absorptive state
The metabolic state occurring shortly after eating, characterized by increased insulin levels and the use of glucose for energy.
Anabolic period
A phase of metabolism where the body builds complex molecules from simpler ones, such as synthesizing glycogen and fat.
Chylomicrons
Lipid transport particles synthesized in the intestinal mucosa that carry dietary lipids into the bloodstream.
Insulinoma
A rare tumor of the pancreas that produces excessive amounts of insulin, leading to hypoglycemia.
Elevated insulin to glucagon ratio
A condition that promotes anabolic processes in the body, such as glycogen and fat synthesis.
Liver glycogen
Stored glucose in the liver that can be mobilized to maintain blood glucose levels during fasting.
Triacylglycerols (TAG)
The main form of stored fat in the body, composed of glycerol and three fatty acids.
Metabolite
A substance formed in or necessary for metabolism, often serving as an intermediate in metabolic pathways.
Allosteric Regulation
A form of enzyme regulation where the binding of a molecule at one site affects the activity at a different site, often altering enzyme shape and function.
Covalent Modification
The process of altering enzyme activity through the addition or removal of chemical groups, such as phosphate, which can activate or deactivate the enzyme.
Induction
The process of increasing enzyme synthesis in response to specific signals, leading to a greater number of active enzyme molecules.
Repression
The process of decreasing enzyme synthesis, resulting in fewer active enzyme molecules available for metabolic reactions.
Glycogen Synthase
An enzyme that catalyzes the formation of glycogen from glucose, primarily active in the presence of insulin.