unit 2 vasculature
1/101
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
102 Terms
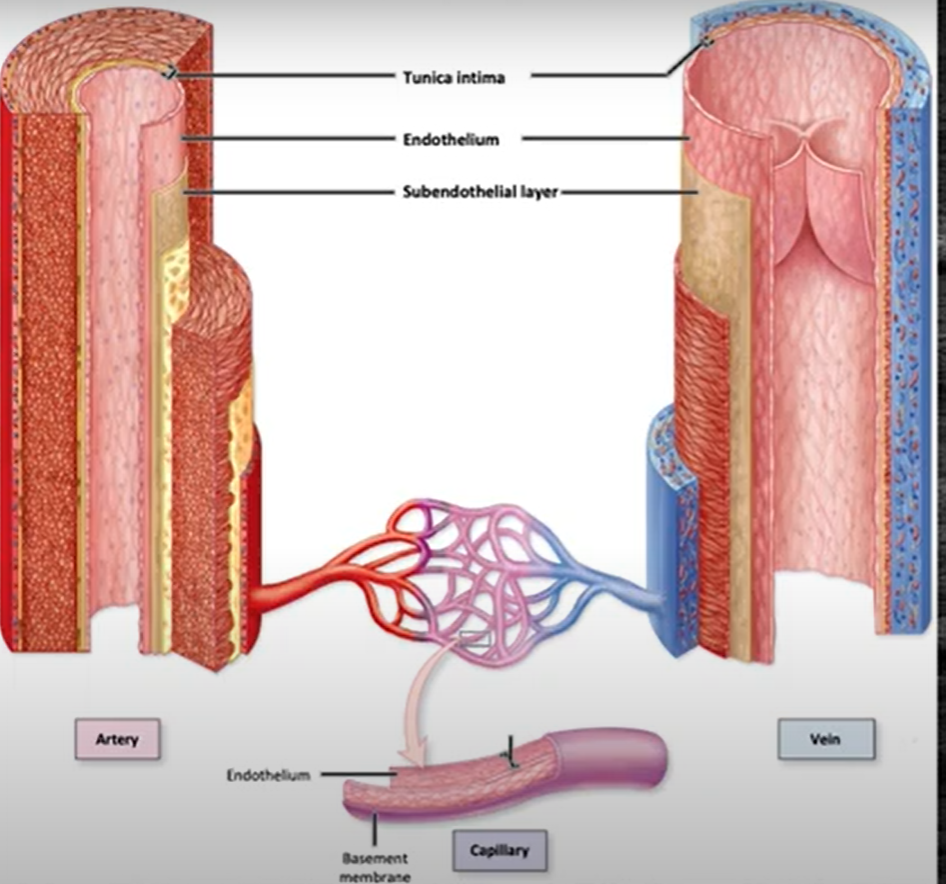
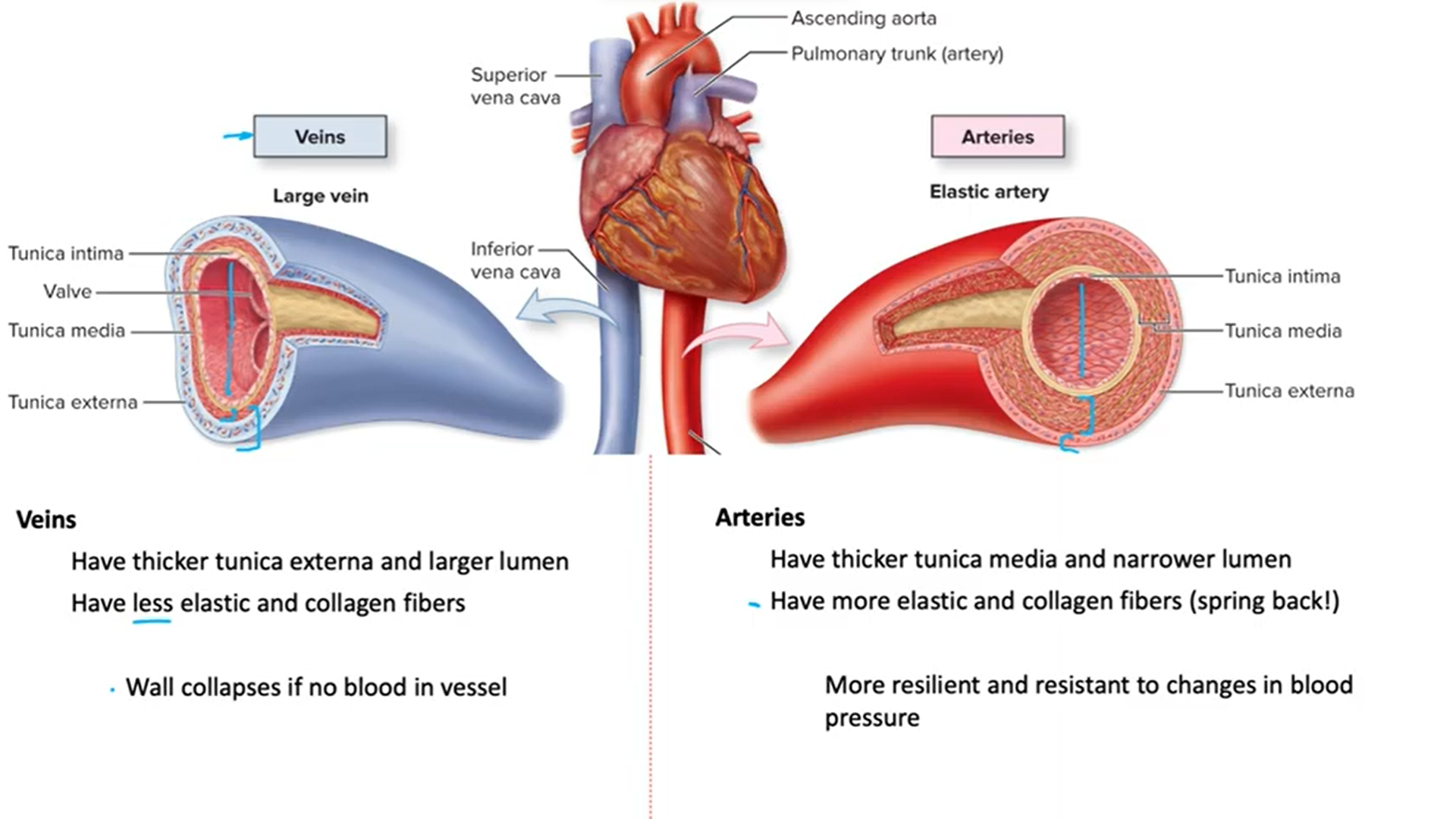
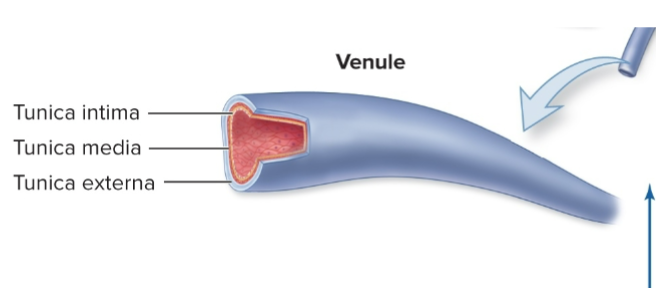
blood vessel anatomy
lumen = hollow space in middle (where blood goes)
-3 layers called tunics
tunica intima = closest to lumen
tunica media = in middle
tunica externa = outside part
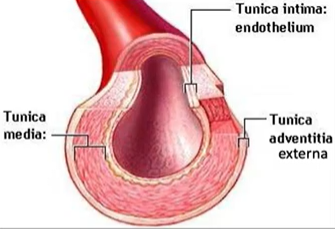
BV artery and vein diagram
tunica intima
-inner most BV layer
-closest to tunic
-endothelium of simple squamous endothelium
-subendothelial layer of areolar CT
epithelial tissue
functions: exchange (permeability), barrier, secretion, sensation, form glands
2 types:
-epithelial sheets = boundaries
-secretory glands = secrete products
simple vs stratified epithelial layers
simple = only 1 layer of epithelial cells
stratified = more than 1 layer
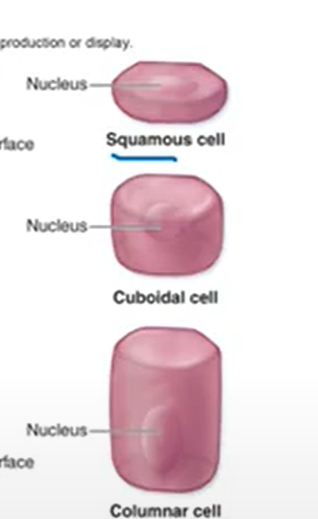
epithelium classified by shapes
tunica media
-middle layer of BV
-functions: vasoconstriction and vasodilation
-circularly arranged layers of smooth muscle cells w/ elastic fibers → circular is bc contraction can cause vasoconstriction of lumen, relaxation cause vasodilation
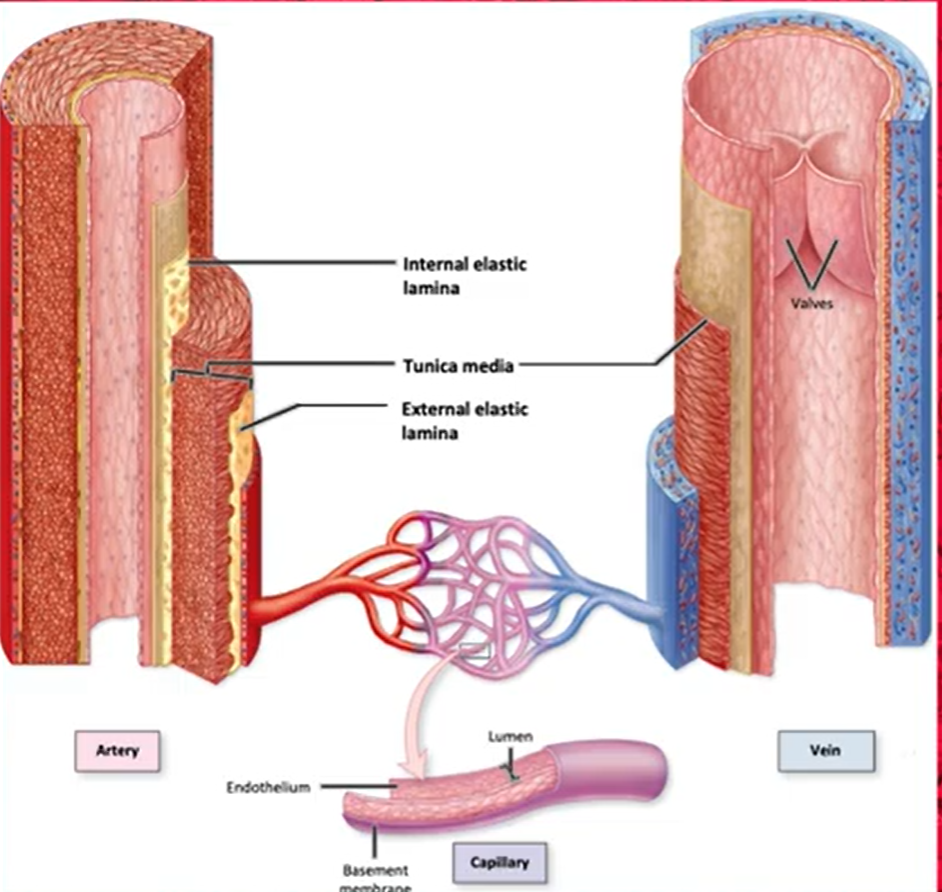
tunica externa
-outer BV layer
-made of areolar CT w/ elastic and collagen fibers
-may contain vasa vasorum = small arteries required to supply very large vessels
functions: help anchor BV to other structures in body

connective tissue (CT) functions
-transport fluids/material
-structure/support
-energy storage
-protect organs
areolar CT
-contains all cells/fibers found in other CTs (elastic, collagen, macrophage fibers)
-extensive blood supply
-found underneath epithelial layer → provides cushioning & elasticity
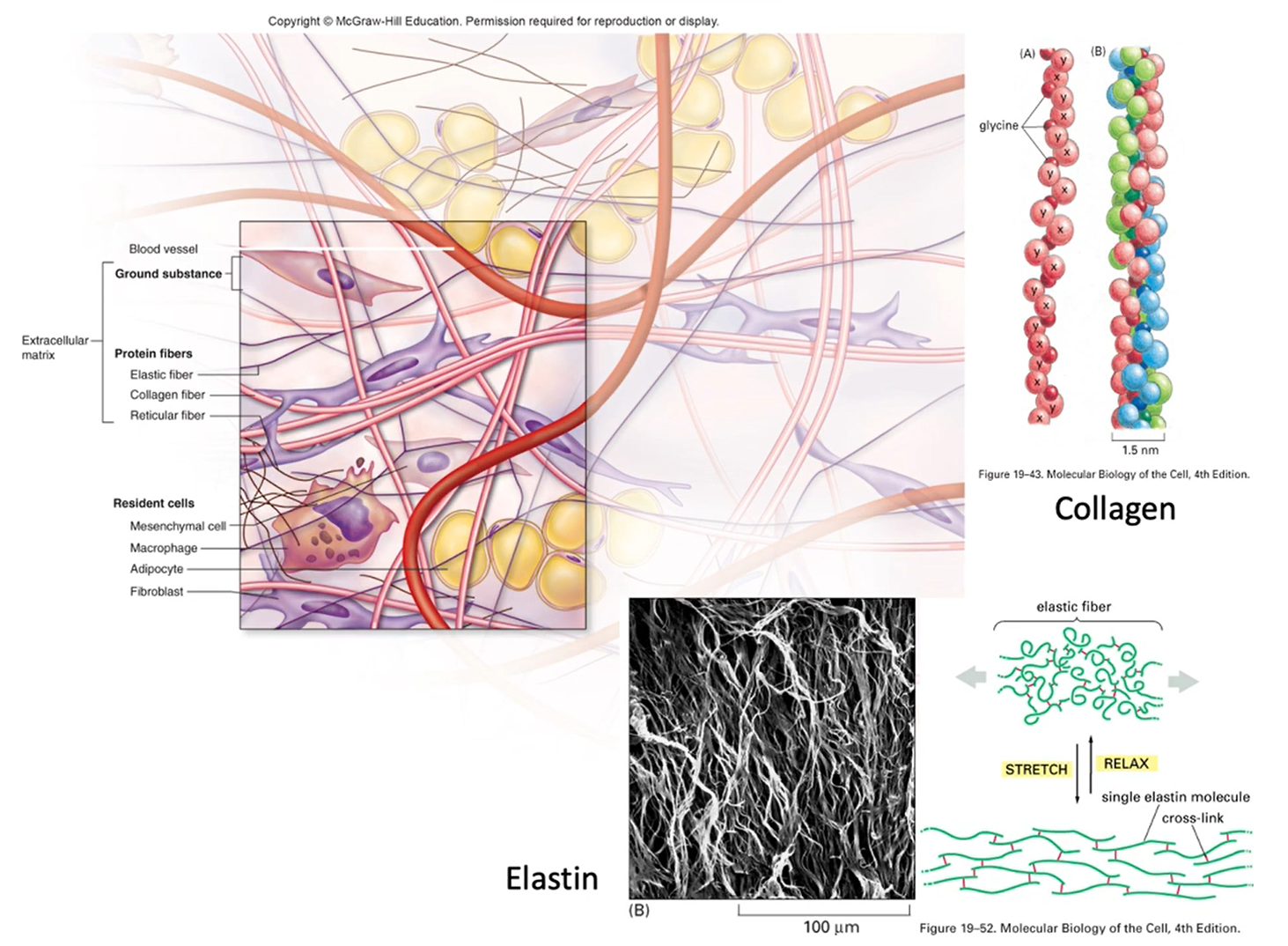
collagen and elastin
elastin = makes things elastic → stretch and flex
collagen = structural support
companion vessels
artery and vein that lie next to each other, serve same body region

what are the anatomical/structural differences btwn veins and arteries?
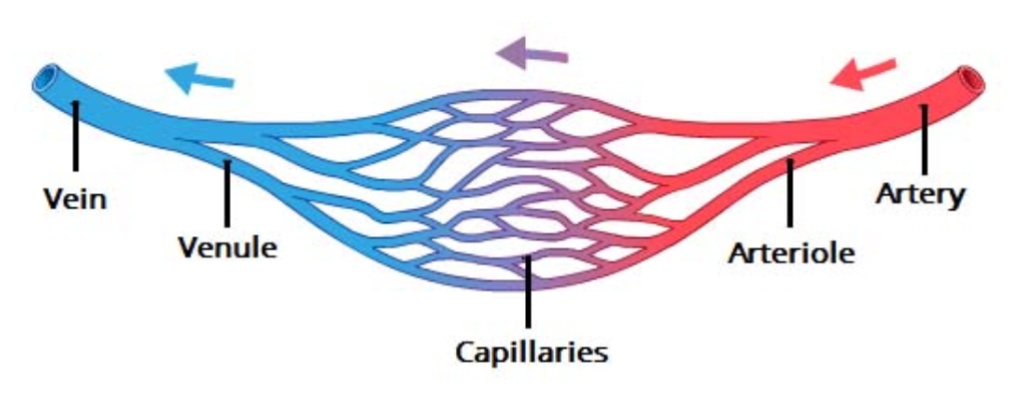
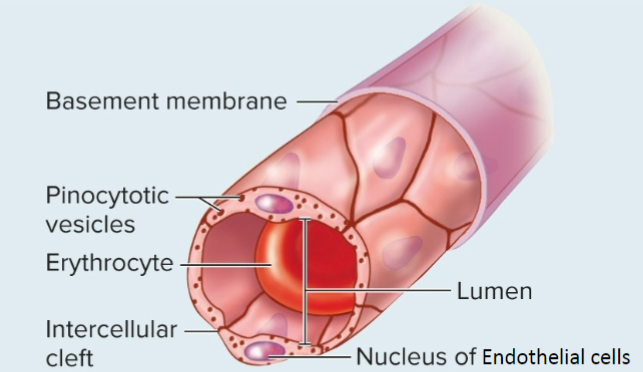
differences btwn capillaries and other BVs
-capillaries are the smallest
-exchange btwn artery and vein
-only have a lumen and tunica intima
-thin wall allows for rapid gas & nutrient exchange
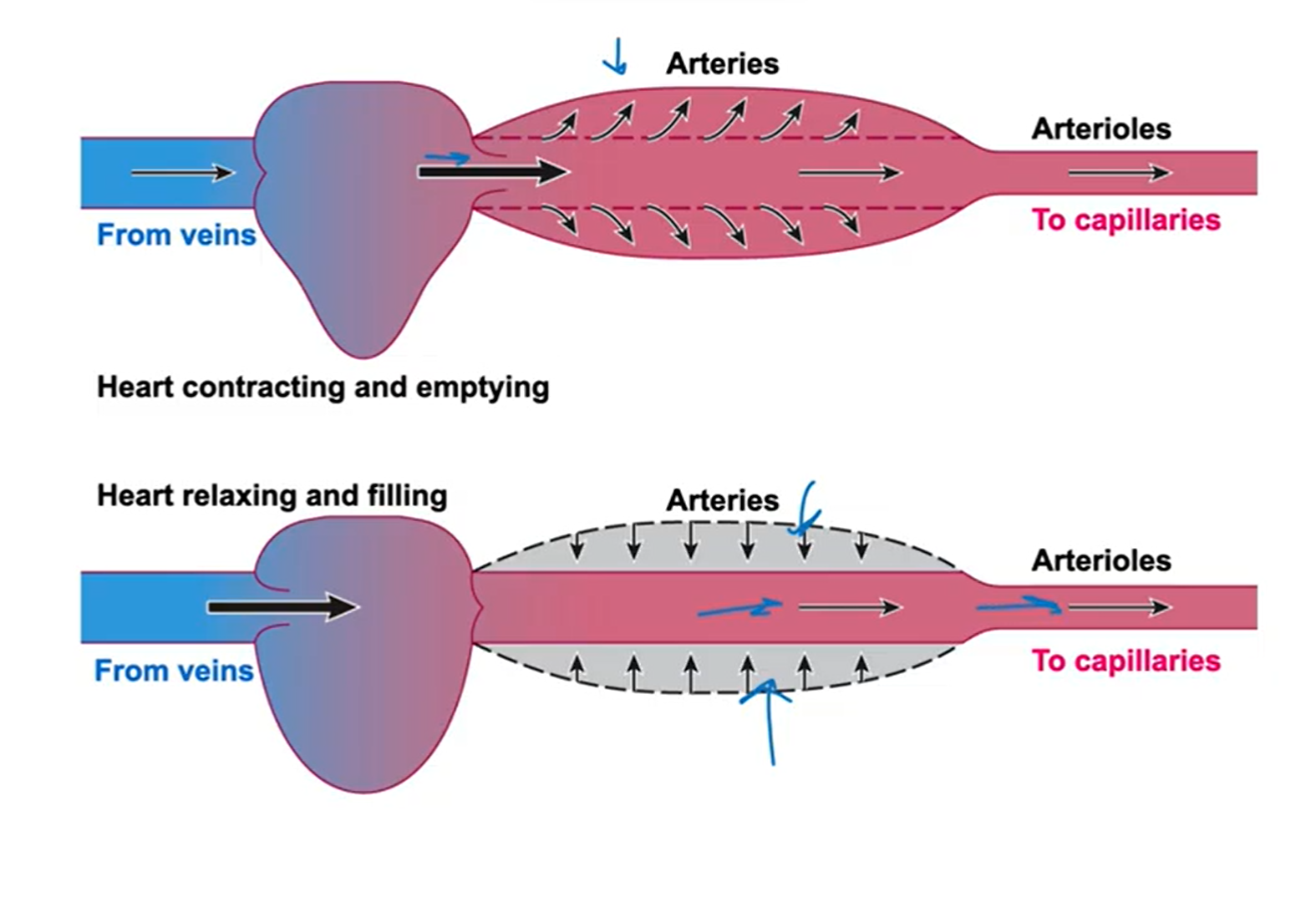
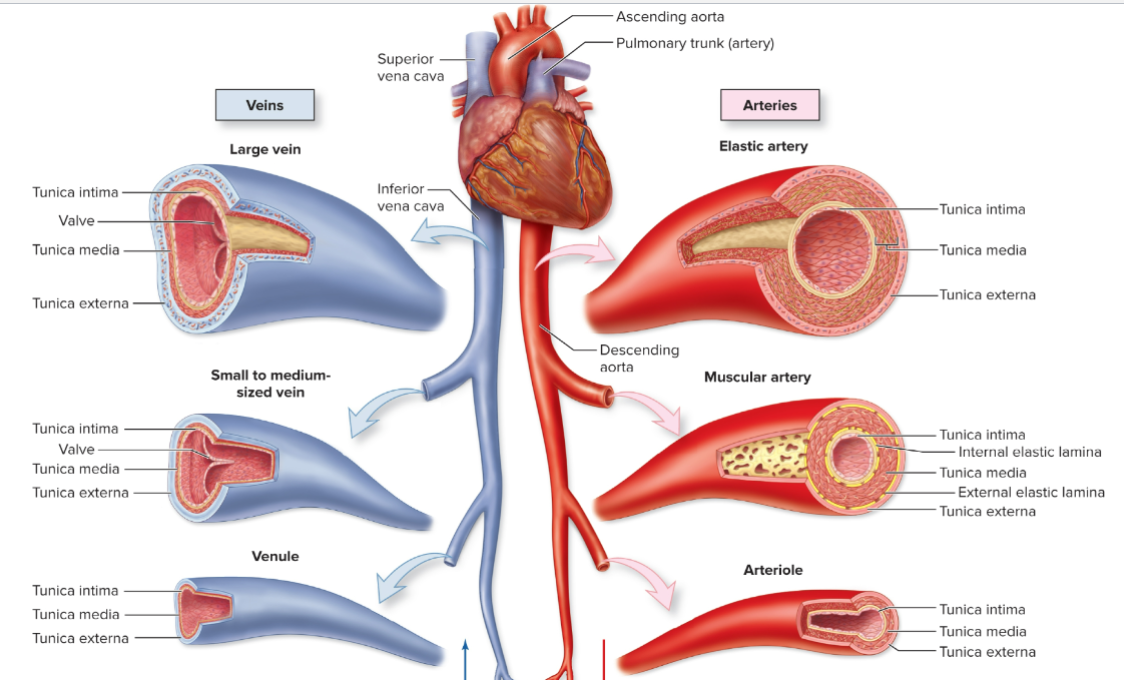
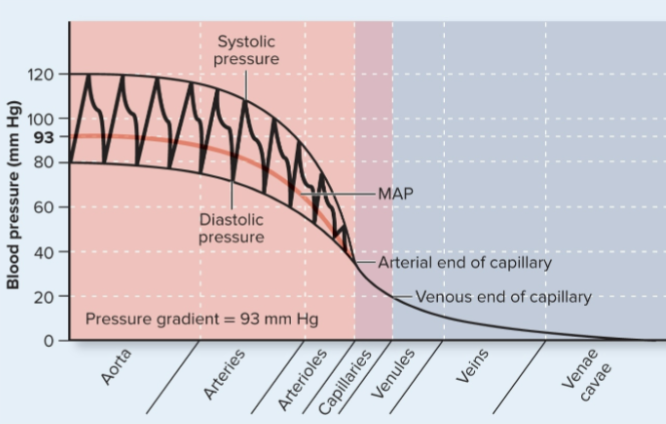
arteries
-AWAY from heart → O2 rich blood to organs
-continue to exert pressure to drive blood even during diastole
-arterial CT contains collagen for tensile strength & elastin for elasticity
-branches into 3 types = elastic, muscular, arterioles
-as move farther from heart, decrease diameter & elastin, while increase smooth muscle
elastic artery
-largest arteries
-have large proportion of elastic fibers → helps propel blood thu arteries during diastole
-examples: aorta, common iliac arts.
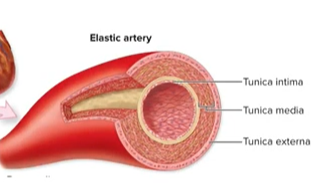
How does an elastic artery push blood forward during diastole?
-during systole the walls of the lumen are blown up like a balloon, filled w blood
-when diastole happens, the smooth muscle in the tunica media contract, and it pushes the blood forward even when the heart is relaxed
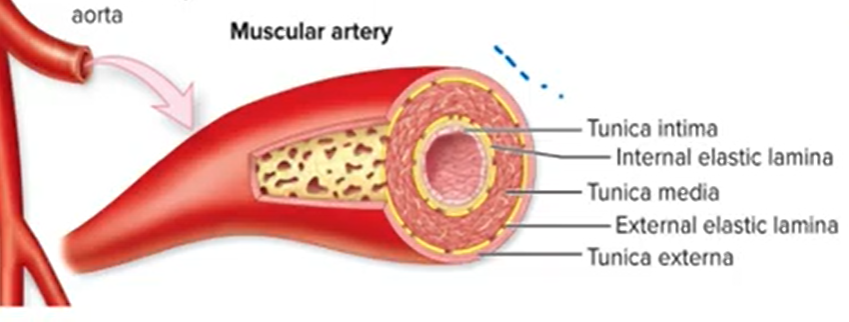
muscular arteries
-branch from the elastic arteries
-medium sized
-better vasoconstriction & dilation ability
-examples: brachial art., coronary arts.
-elastic tissue is confined to 2 layers:
→ internal elastic lamina - btwn tunica intima and media
→ external elastic lamina - btwn tunica media and externa
arterioles
-branch from muscular arts.
-smallest. they don’t have individual names bc of how small they are
-regulate systemic BP and blood flow
-smooth muscle usually somewhat constricted → called vasomotor tone
Coronary artery disease (CAD) and myocardial ischemia
CAD = damage or disease in the heart’s major BV (on outside of heart)
-can cause myocardial ischemia = coronary blood flow can’t keep up with O2 needs, heart can’t contract as much as needed
-occlusion due to plaque buildup → can cause heart attack (myocardial infarction)
atherosclerosis
progressive, degenerative arterial disease
-plaque builds up (occlusion) in BV blocking lumen
-can lead to stroke or heart attack → if plaque breaks off it can deposit somewhere else and block blood flow to another area in body (brain or heart)
causes/risk factors and treatment of atherosclerosis
causes/risks = hypercholesterolemia (high cholesterol), smoking, hypertension, male
treatments = angioplasty or coronary bypass surgery
coronary angiogram
type of x-ray that shows coronary heart arteries, can see if they’re blocked
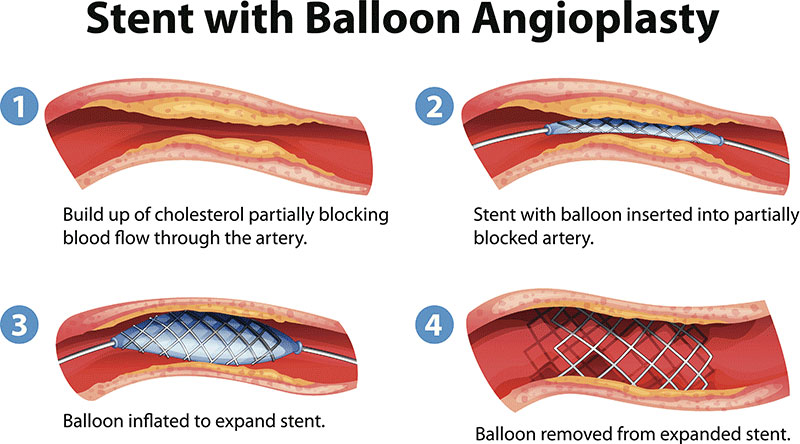
angioplasty
-procedure to treat atherosclerosis
-balloon goes into artery and inflates, then a stent is placed in the artery to keep it expanded
-patient goes home w/in a few hrs
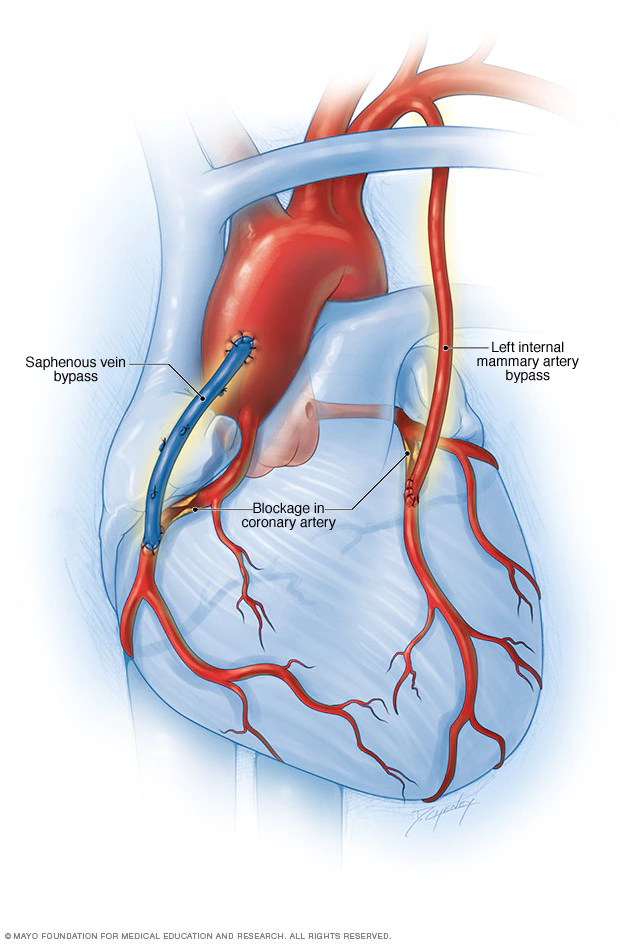
coronary bypass surgery
-treat atherosclerosis of coronary vessel blockage
-blockage is not cleared, instead a detour is created for blood to travel instead
-use mammary artery, radial artery, or saphenous vein for bypass
-not a permanent solution
capillaries
-small vessels connect arterioles to venules
-only as wide as 1 RBC, so cells must travel single file (rouleau)
-small radius and very porous = large surface area ratio, good for exchange
2 types of passive exchanges for capillaries
1: diffusion = down concentration gradient
2: bulk flow = relies on pressure gradient, move water and solutes from high to low pressure
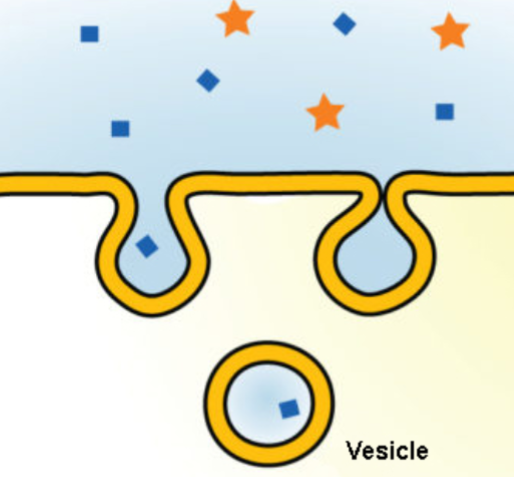
pinocytosis
cellular drinking
-intake droplets of fluid that contain solutes
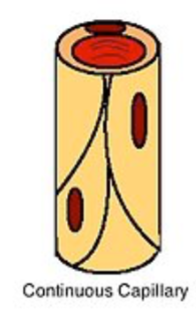
continuous capillary
-least permeable, less gaps
-endothelial cells form a continuous lining
-connected by tight junctions
-intercellular clefts = spaces along the wall where molecules can pass
-smaller molecules (glucose and gas) can pass thru walls
-ex. lungs
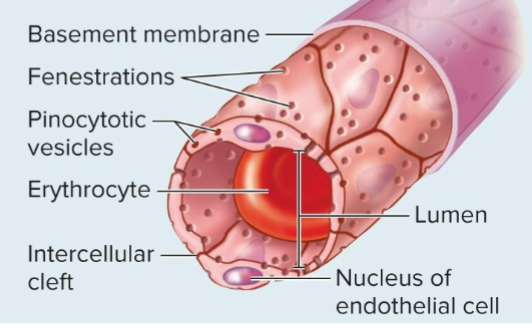
fenestrated capillary
-good for fluid exchange (plasma proteins)
-continuous lining but the cells have fenestrations (pores)
-ex. kidneys
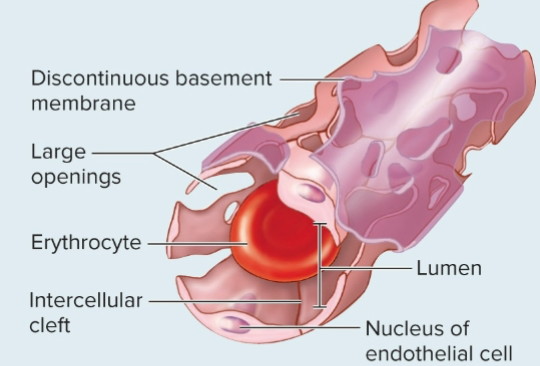
sinusoidal capillary
-biggest holes, easiest to transport
-basement membrane is incomplete or absent
-red in color bc of the blood being visible, can turn tissue of organs red if there’s a lot of them (ex. liver)
-move large substances, formed elements (blood cells or platelets)
-ex. liver, bone marrow
capillary diagram
capillary beds = groups of capillaries functioning together
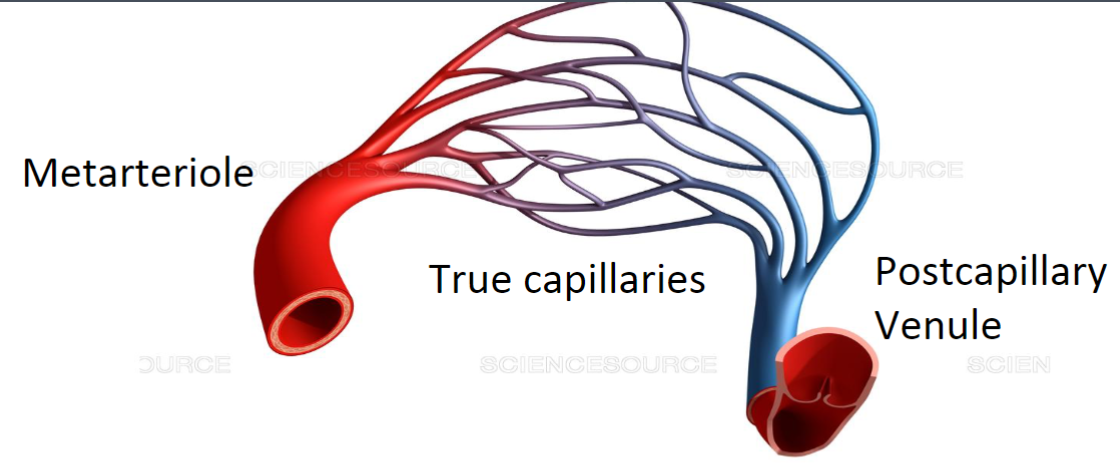
vasomotion
process of venules and arterioles contracting and relaxing to channel blood flow
-75% of capillaries are closed at once, bc we don’t have enough blood to fill all at once
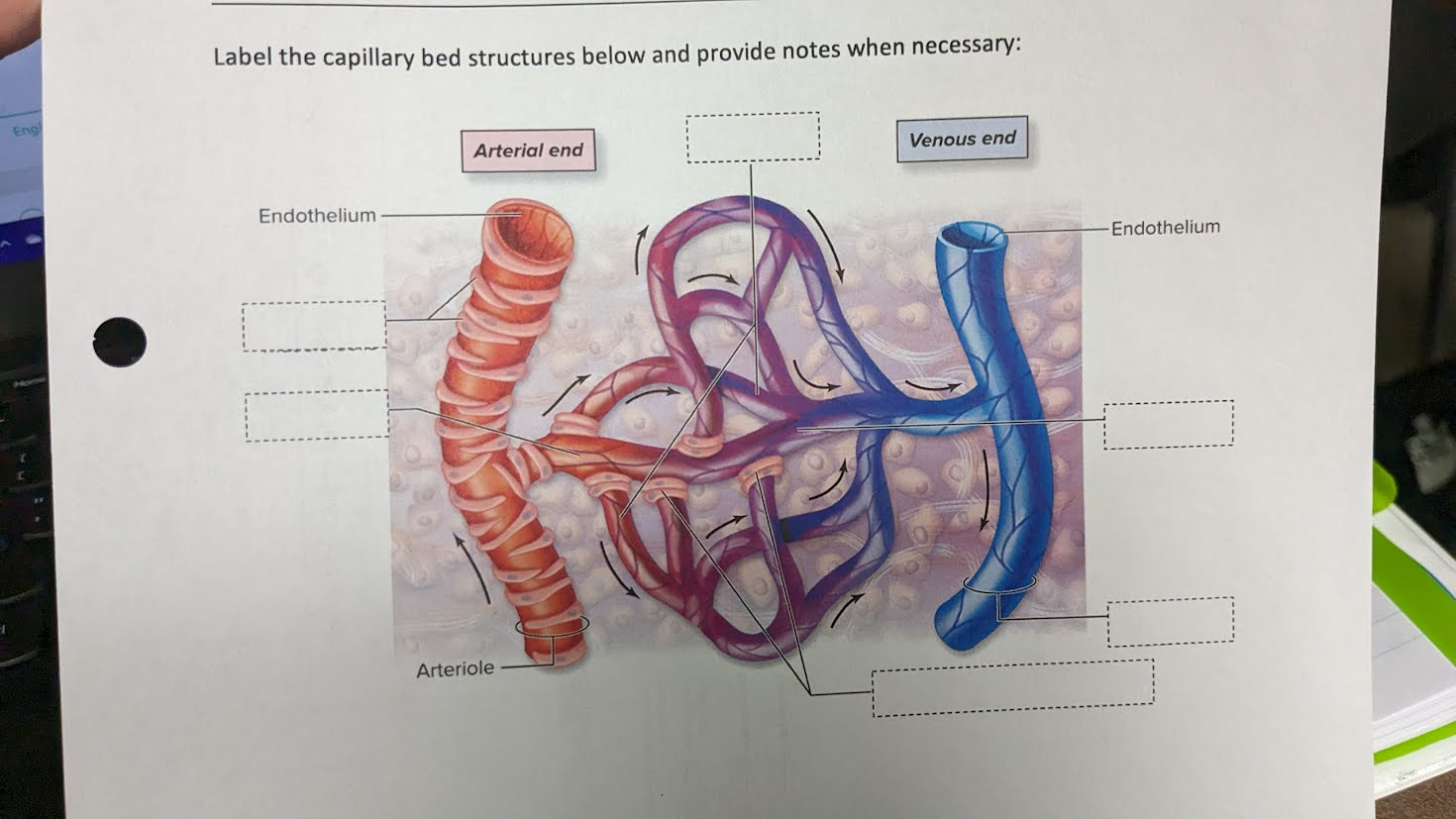
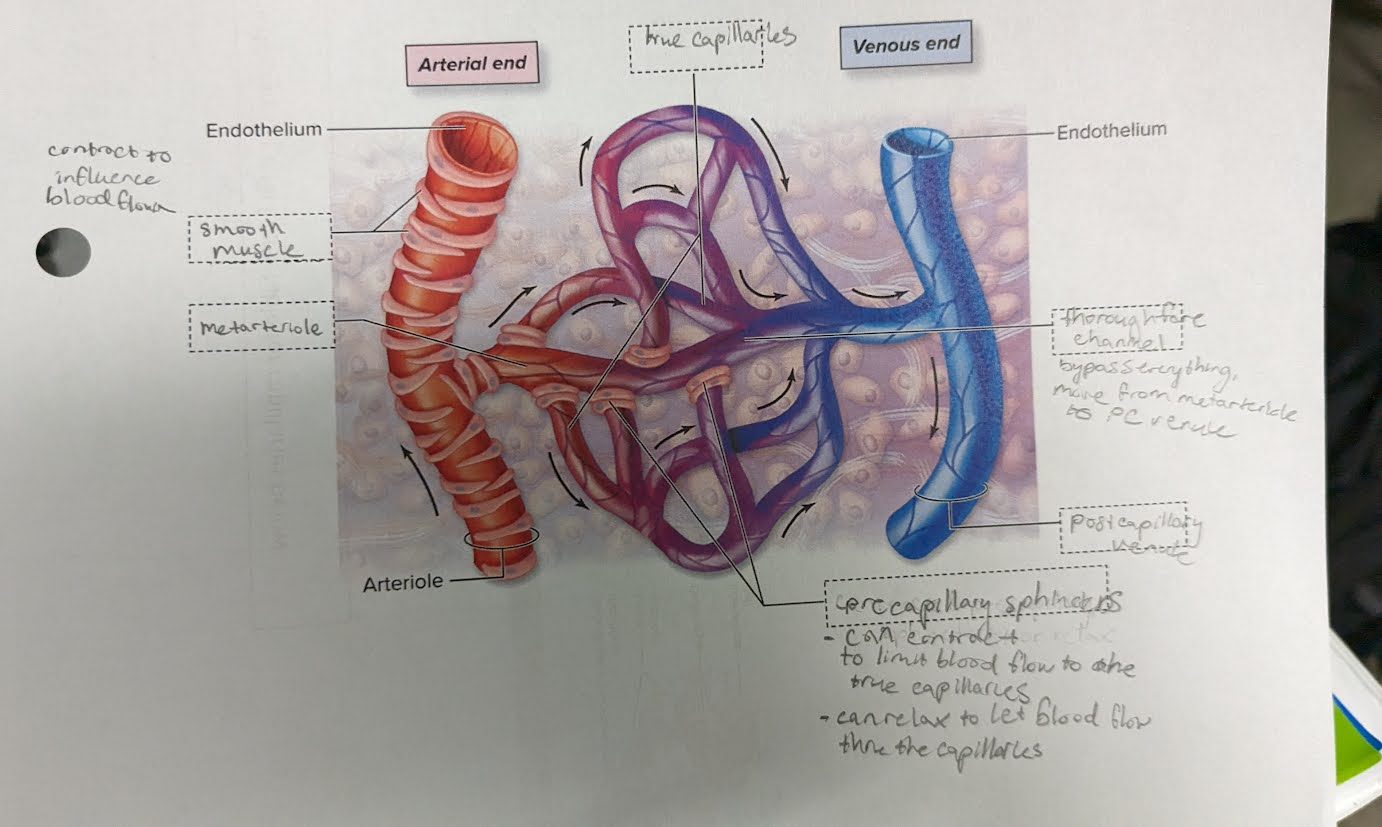
venule
-smallest veins
-companion vessels to arterioles
-smallest venules are postcapillary venules
-large ones have all 3 tunics
-merge to form veins
small & medium veins. large veins
-middle size veins companion vessels w/ muscular arts
-large companion to elastic arteries
-have many valves
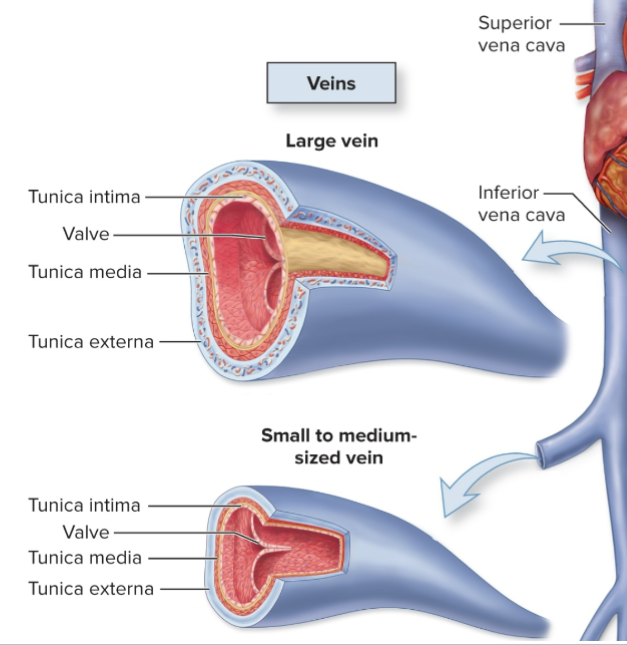
do veins and/or arteries have valves? why?
veins do, arteries do not.
veins need it to prevent backflow since pressure is lower
-made of tunica intima and elastic and collagen fibers
varicose vein
-blood pools in veins causes veins to bend
-this opens the valves and blood backflow happens

artery and vein types full diagram
blood reservoir
-veins store extra blood when not needed
-vasoconstriction moves it to circulation when needed, vasodilation relaxes blood back into veins when not needed
blood in body at rest: 18% pulmonary circ, 12% heart, 70% systemic circ
in systemic circ: 10% art, < 5% cap, 55% veins
deep vein thrombosis
blood clot forms in the vein (usually in legs)
-can dislodge and move to other parts of body, cause pulmonary embolism (blockage)
-compression socks and meds can treat
-has hereditary component → if you have less antithrombin protein, your blood is more likely to clot
pulmonary embolism
a sudden blockage in your pulmonary arteries
-usually happens when DVT blood clot dislodges from leg and moves up to heart
hematoma
A pool of mostly clotted blood that forms in an organ or tissue
-usually caused by broken BV
why is warfarin prescribed for DVT
-it thins blood so blood can flow thru the veins easier
-it also blocks an enzyme that uses vit K to clot blood → leads to slower blood clotting
venous stasis
when veins have problems moving blood back to the heart → blood backflow
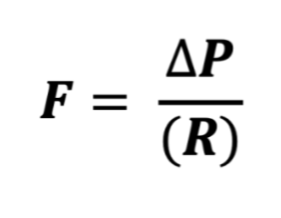
blood flow (perfusion) equation
F = blood flow (L/min)
∆ P = pressure gradient (mmHg). find by subtracting high minus low ends of vessel
R = resistance. find by mmHg x L^-1 x min^-1
blood pressure, BP gradient
BP = force of blood against a vessel wall
BP gradient = change in P from beginning to end of a vessel (high - low = P) → propels blood thru vessels
→ BP is highest in arteries and lowest in veins
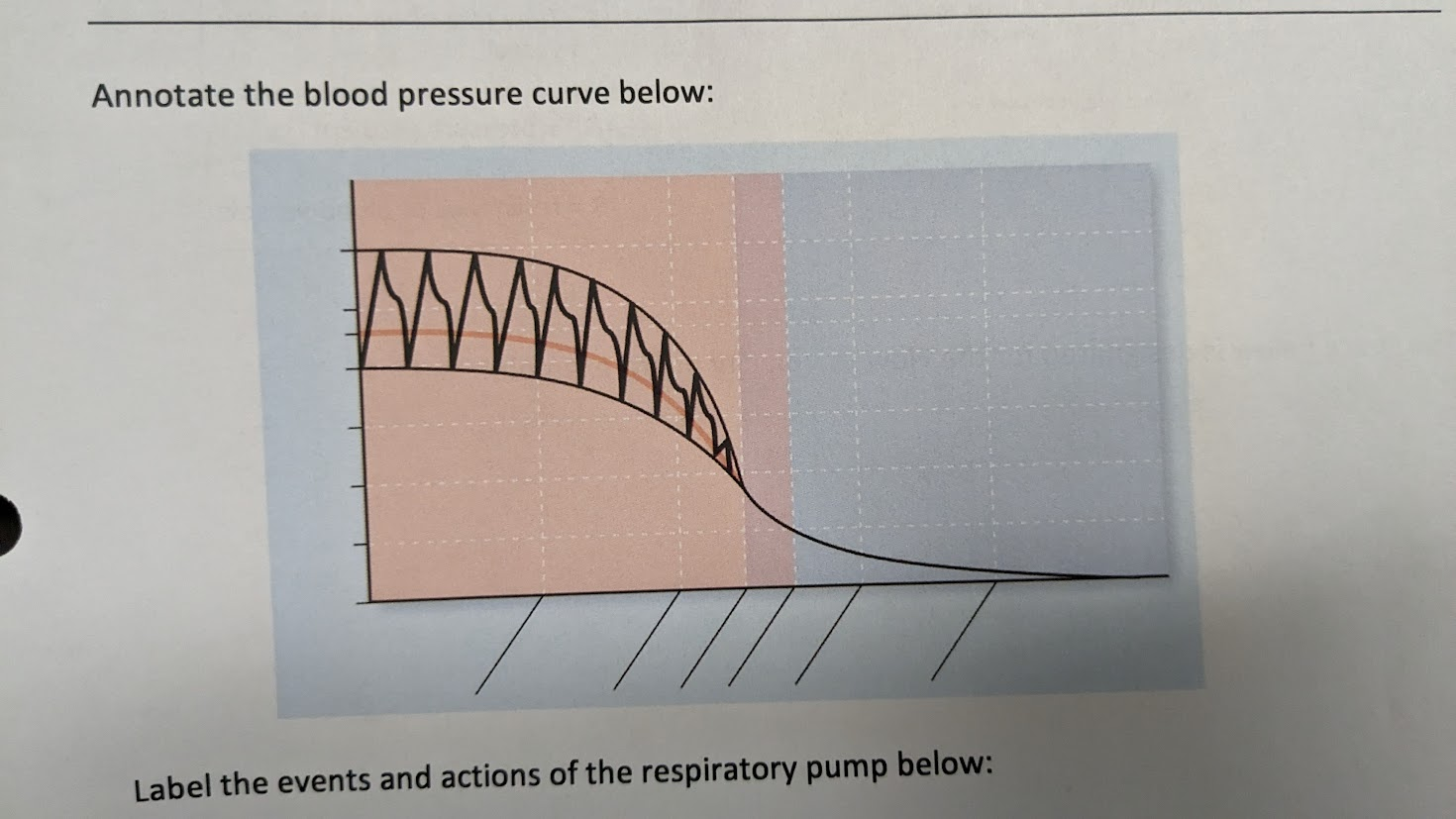
What does it mean to be pulsatile? Are arteries, veins, or both pulsatile?
Moving up/down or expand/contract with heart beat
-only in arteries, not veins
-this is why we only take BP for arteries bc veins are not pulsatile
-this means veins and capillaries also don’t have a pulse pressure
pulse pressure
additional pressure placed on arteries from when heart is resting to when heart contracting
-gives idea of how elastic arteries are
-measured by systole - diastole
→pulse pressure of image shown is 40 mmHg
How does age affect pulse pressure?
It increases with age
-less elasticity in BV, don’t expand as easily
-this means there is more pressure in vessel wall, so pulse pressure increases
-systolic vol increases, diastolic remains the same
MAP
Mean arterial pressure = avg art. BP across entire cardiac cycle
70-110 mmHg = healthy
MAP = diastolic + (1/3) pulse pressure
( e.g. if BP is 120/80
80 + (1/3) 40 = 93 )
also MAP = CO X R
(CO = SV x HR)
why is capillary BP range so important?
-need to be high enough velocity for exchange of substances
-needs to be low enough V to not dmg vessels
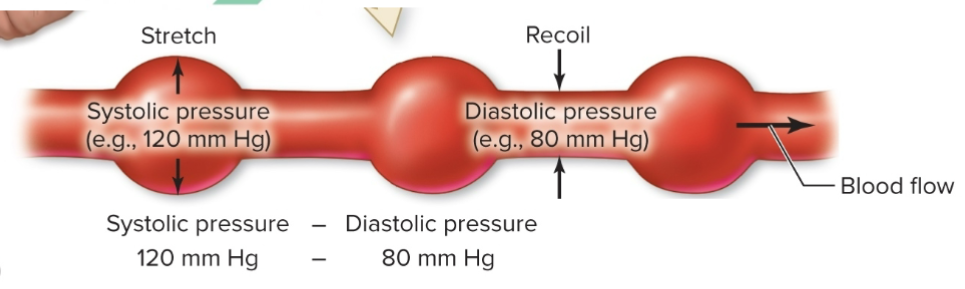
flow, linear velocity of flow
-Flow (L/min) = identical through all vascular segments; dictated by pressure and resistance across individual vessels
-Linear Velocity of Flow = How quickly a given volume of blood passes through vessel (cm / sec); how far blood travels per unit time
(CSA = cross-sectional area)
V = flow/CSA
How does CSA affect velocity and flow?
CSA = cross-sectional area. total area of blood to flow all over (add the area of all the capillaries together)
→ more area/CSA = more room to flow, not as much pressure so the velocity slows down in capillaries. in arteries and veins it’s much faster since all of the blood goes only along one path
**however flow itself does not change, since it’s the same # of blood being used at once. But velocity changes
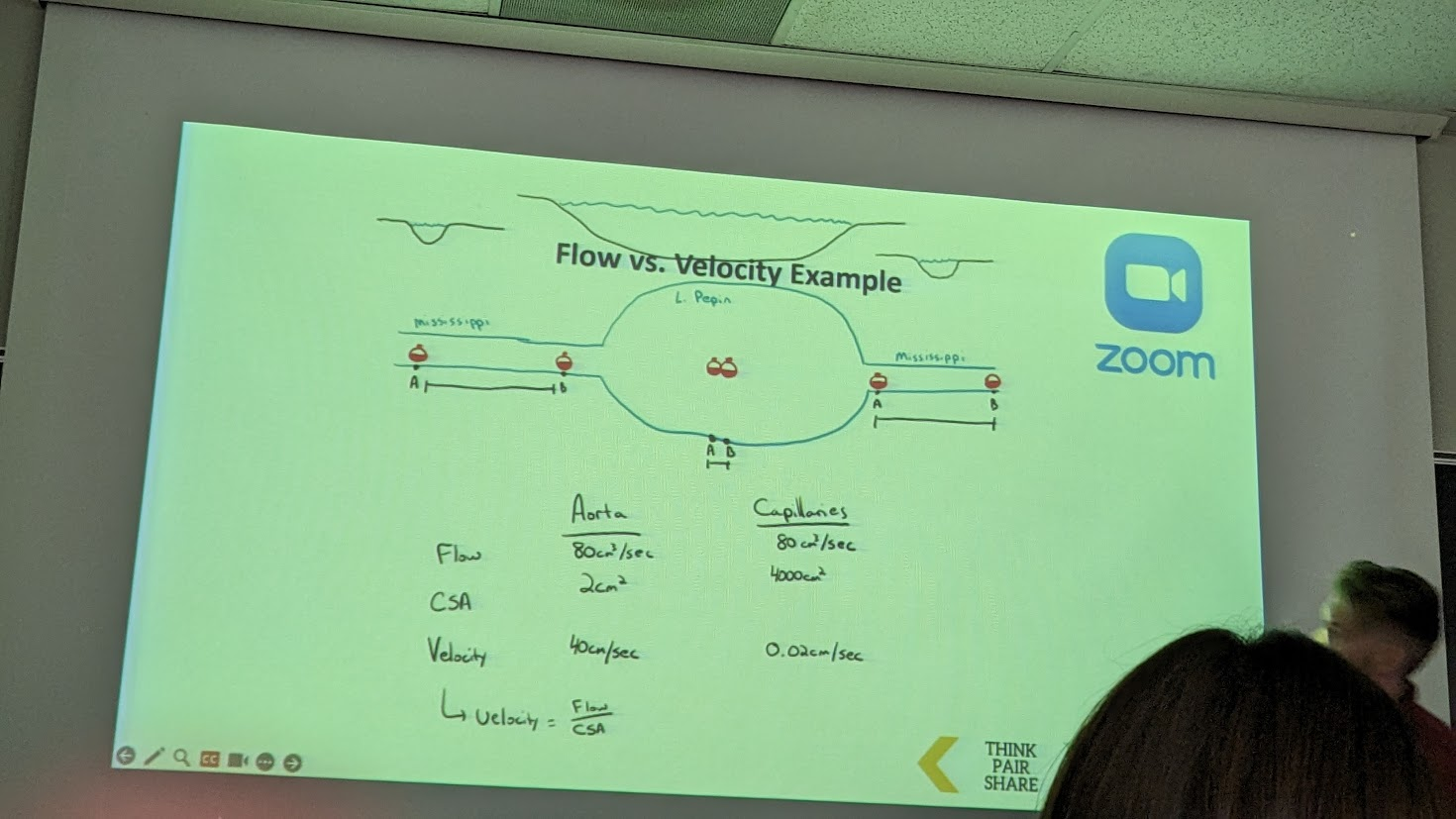
calculate the flow for the aorta vs the capillaries
V = flow/CSA
aorta = 80/2 = 40cm/sec
capillaries = 80/4000 = 0.02 cm/sec
skeletal muscle pump
→ clusters of muscles that surround deep veins and helps squeeze veins. Assists venous return from limbs
• As muscle contracts, veins are squeezed
• Blood is pushed and valves prevent backflow
• Blood is moved more quickly during exercise
-this is what helps prevent varicose veins to prevent blood pooling in legs
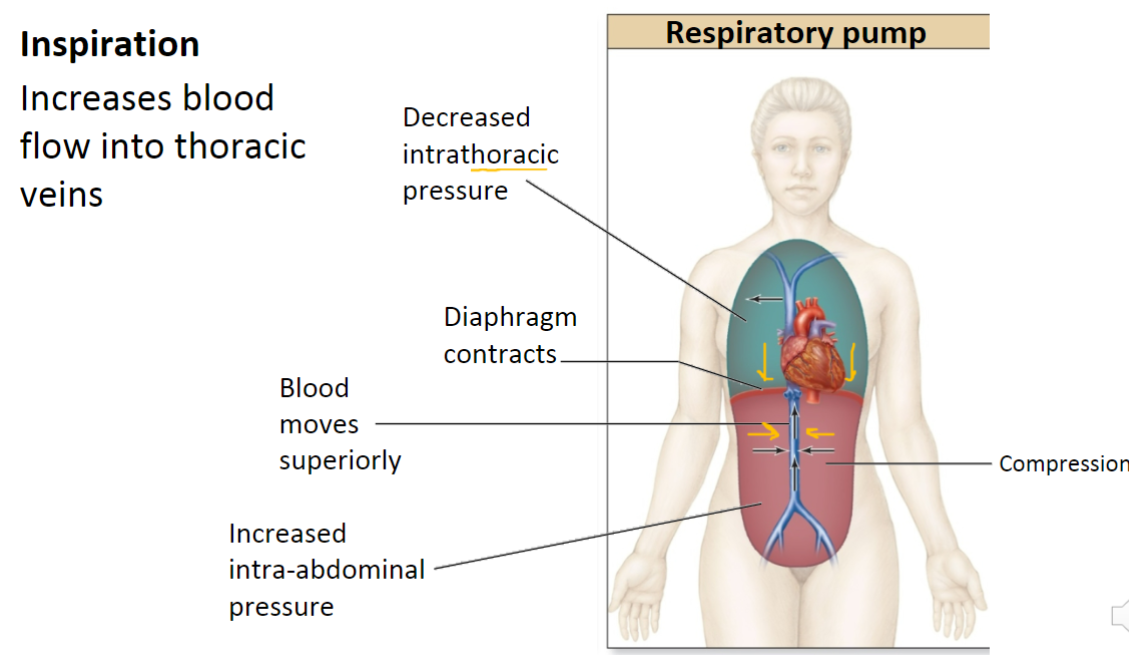
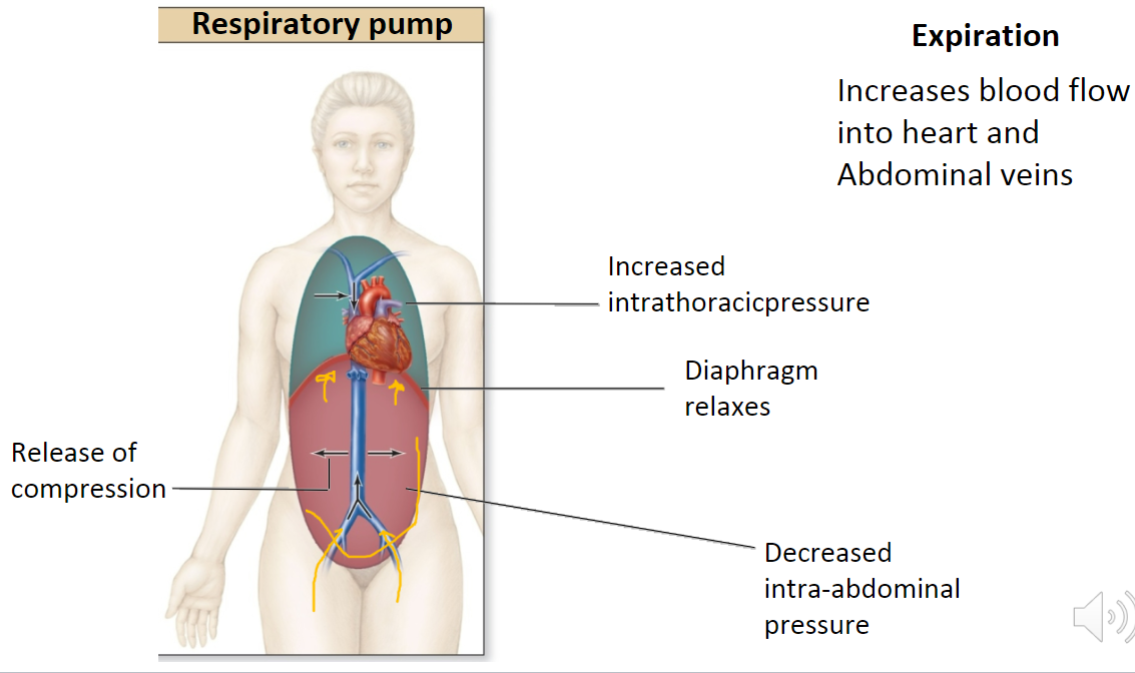
respiratory pump
Assists venous return in the thorax
• Both inspiration and expiration cause P gradient changes that will help venous return
• Increased breathing rate facilitates blood mvmt
how does inspiration affect respiratory pump?
how does expiration affect respiratory pump?
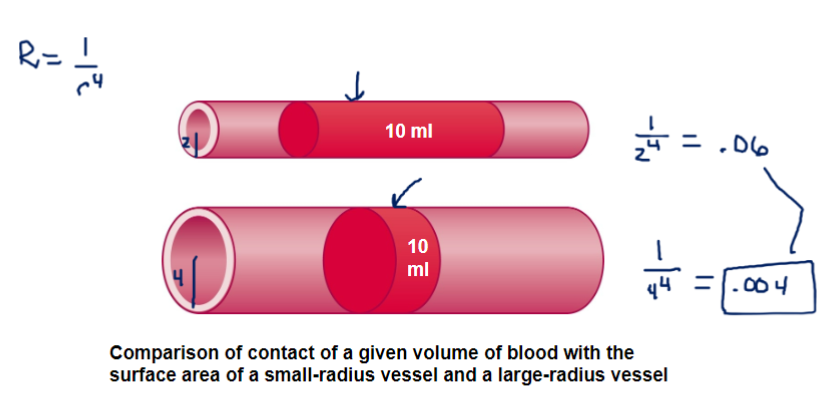
peripheral resistance (R)
-measure opposition of blood flow as it moves thru vessel
depends on:
1) viscosity
2) BV length
3) BV radius (r). slight radius change produces significant resistance change
R = 1/r^4
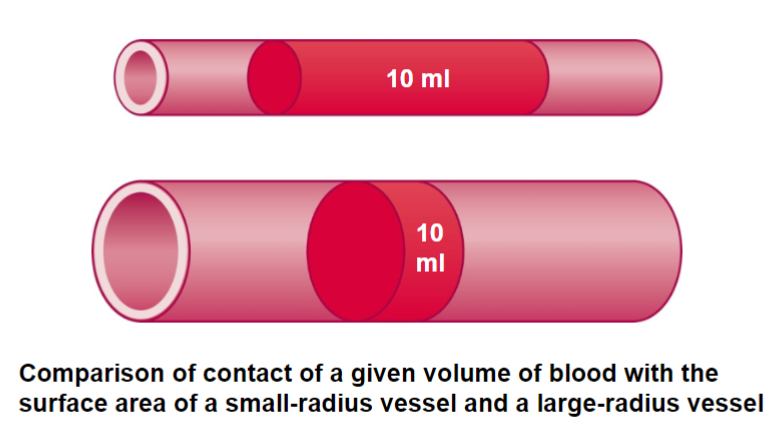
Find the resistance of each. Which one has less resistance?
top BV r = 2mm
bottom r = 4mm
R = 1/r^4
→ bigger one has lower resistance
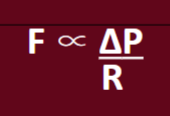
How is F flow related to P and R?
-directly proportional to pressure (↑ P ↑ F)
-inversely proportional to resistance (↑ R ↓ F)
local blood flow
blood delivered locally to capillaries of a tissue
-measured in mL/min
dependent upon
1) tissue degree of vascularization
2) myogenic response
3) local regulatory factors affecting blood flow
4) total blood flow
Degree of vascularization
the extend of vessels in a tissue
-metabolically active tissues have higher vascularity (need more O2) ex. brain, heart, liver
-low vascularity includes connective tissue, does not need O2
angiogenesis
form new BV over weeks to months
Stimulated by:
-increased aerobic training in skeletal muscle
-in adipose tissue with weight gain
-in coronary vessels in response to blockage
-cancer growth
**vessel regression can occur if inverse (go to sedentary lifestyle SM or lose weight adipose)
myogenic response
smooth muscle in BV wall keeps local flow constant
-contract and relax blood vessels in response to changes in stretch of vessel wall
myogenic response to high BP
increased arterial pressure
stretch BV walls
mechanically gated Ca channel opens
Ca rush into BV
muscle contracts more (vasodilation)
BP lowers
sympathetic and parasympathetic effects on myogenic response
sympathetic brings more blood flow, increase BP , so wall stretches → smooth muscle response will contract the BV to normal size
parasymp brings less blood flow, decrease BP, so wall has no stretch → smooth muscle relaxes to return blood flow to original
autoregulation positive feedback (molecules that are vasodilators)
when inadequate perfusion (BV too constricted), the tissues release substances that can act as vasodilators to bring in more blood
during vasoconstriction:
→ O2 and nutrient levels decline
→ Co2, lactic acid, H+ increase
concentrations of these particles will signal vasodilation
autoregulation negative feedback → reactive hyperemia
increase in blood flow after it is temporarily disrupted
-additional blood required to resupply O2 & nutrients, get rid of waste products
-example: cheeks flush after being outside in the cold. they flush due to increased blood as your BV are playing catch up trying to remove waste from the previously-constricted areas
Why does swelling happen in an immune response?
-Histamine and bradykinin release, cause vasodilation of arterioles → edema
-may also stimulate release of nitric oxide (another vasodilator)
-this helps immune cells arrive to area quickly to help eliminate possible pathogens (ex. in case of bee sting)
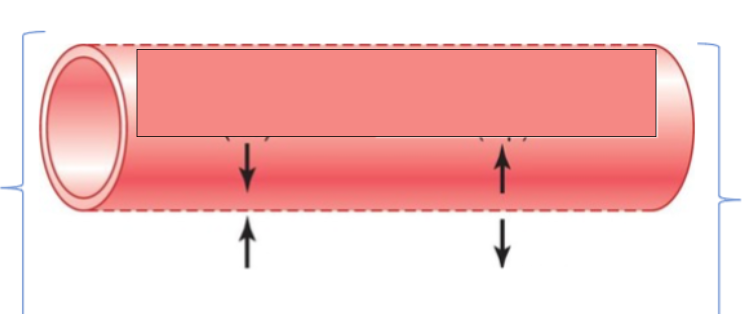
bulk flow
how capillaries do fluid exchange (ISF fluid and plasma) → fluid leaves and returns capillaries
-filtration = fluid moves out of blood
-reabsorption = fluid back into blood
**when BP low, caps. retain more fluid (less filtration) to raise blood vol and BP
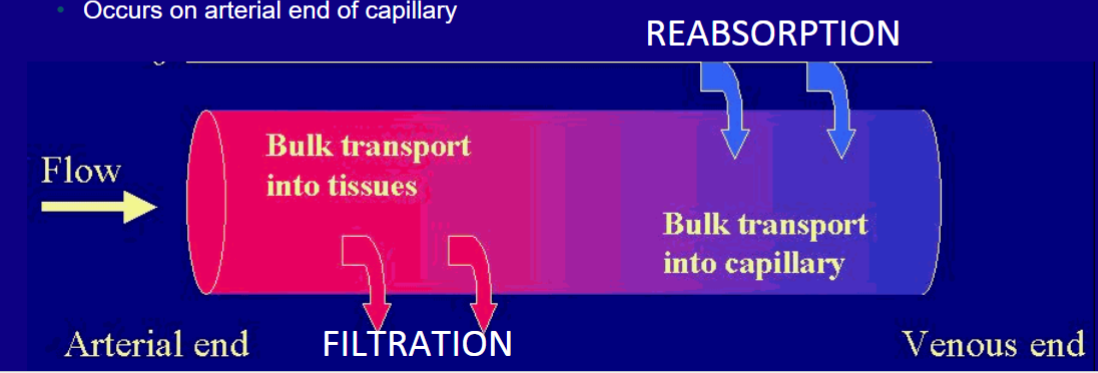
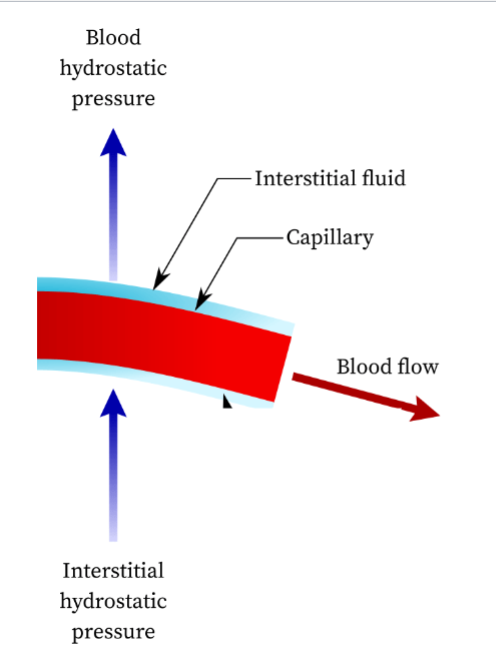
blood hydrostatic pressure (HPb)
• Force exerted per unit area by blood on BV wall (blood pushing inside BV)
• Promotes filtration (blood out of cap.)
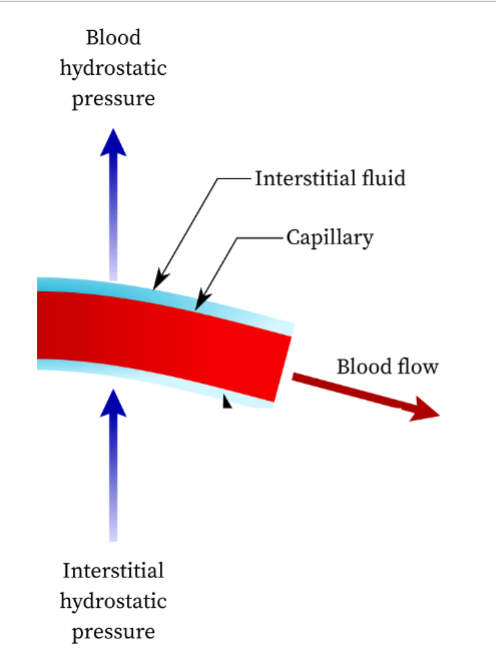
Interstitial fluid hydrostatic pressure (HPif)
• Force of interstitial fluid on outside of BV (IF pushing outside BV)
• Close to zero in most tissues
Colloid osmotic pressure (COP)
the pull on water due to the presence of proteins (colloid)
** “solutes suck” → water goes to where more proteins/solutes are
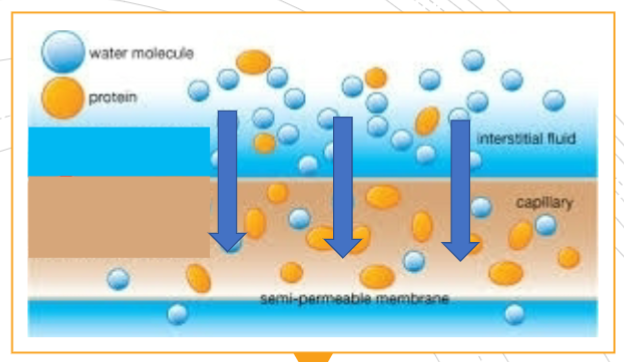
Blood colloid osmotic pressure (COPb)
• Draws fluid into blood due to blood proteins (e.g., albumins) → proteins are in the capillary which draws water in
• Promotes reabsorption (blood in)
• opposes the dominant hydrostatic pressure (HPb)
Interstitial fluid colloid osmotic pressure (COPif)
• Draws fluid into interstitial fluid → proteins are outside capillary which draws water out
• Since few proteins present in IF, this is relatively low (0 to 5 mm Hg)
label the capillary with the 2 HP types and 2 COP types

Net filtration pressure (NFP)
net hydrostatic P - net colloid osmotic P
*to get net HP and COP, subtract to find the difference of each
NFP = (HPb - HPif) - (COPb - COPif)
if end result positive = favors filtration
end result negative = favors reabsorption
**however, if at any time a number is negative, take the absolute value (turn it positive)
role of lymphatic system in circulation
pick up excess fluid that is not reabsorbed at venous capillary end (15% of fluid)
-also filters fluid before returning it
Hypertension effects
1. Endothelial damage: High BP damages endothelium, creates sites where cholesterol accumulates
2. Increased LDL: LDL penetrates the damaged endothelium & accumulates in broken arterial wall
3. Inflammation: inflammation promotes the recruitment of WBC which are key components of plaque.
4.Oxidative stress: High BP increases oxidative stress in the arteries, which can further damage the endothelium and promote the formation of plaque.
5. Smooth muscle cell proliferation: Hypertension stimulates proliferation of smooth muscle cells in the arterial wall.
6. Platelet activation: High BP leads to increased platelet activation, which can promote formation of blood clots that can further narrow the artery & contribute to plaque buildup.
BP regulation - pressure depends on
cardiac output (CO) (SV and HR)
resistance (R)
→ these can bechanged nervous and endocrine factors
cardiovascular center
combo of cardiac center and vasomotor center (in medulla)
MAP = CO x R
cardiac center = influence CO to change BP (HR and SV)
vasomotor center = influence R to change BP (vessel diameter)
cardioacceleratory center
-part of cardiac center
-origin of sympathetic pathways → paths go to SA & AV node and heart
-activity increases HR and SV → increase CO
cardioinhibitory center
-part of cerdiac center
-origin of parasymp pathways → paths go to SA and AV nodes only
-activity decrease HR (but not SV) → decrease CO
vasomotor center
-origin of sympathetic pathways (no parasymp in vasomotor)
-pathways go to BV where they release norepinephrine (NE)
-symp. activation also releases EPI and NE as hormones from adrenal gland from kidney
EPI and NE receptors on BV
-both activated by vasomotor, but BV dilation or constriction depends on what receptor. this differs based on where BV is in body
-α1 = constrict (in other areas)
-β2 = dilate (in SM and heart)
→ receptors located in tunica media smooth muscle
-overall effect is vasoconstriction bc we have much more A1 receptors in body
sympathetic activation will cause
1 - increase or decrease in peripheral resistance?
2 - more or less total blood circulation? (flow)
3 - more or less blood flow to skeletal muscle and heart?
1 - increase R (more blood flow and more constriction due to more α1 receptors)
2 - greater F (vasoconstriction pushes blood stored in veins to body, so increasing blood vol and P)
3 - more (these areas have the B2 receptors)
baroreceptors, baroreflex
-detect BP by detecting BV stretch
-firing rate changes w BP changes → send signal to brain which can change BP
-located in tunica externa of aortic arch and carotid sinuses
aortic arch baroreceptors
-go to brain via vagus nerve
-monitor systemic BP (whole body BP)
carotid sinus baroreceptors
-go to brain via glossopharyngeal nerve
-monitor BP in head and neck
-more sensitive to changes than the baroreceptors in aorta
How does your body compensate when your BP drops? Name all the mechanisms that happen
-baroreceptors (aortic & carotid) detect less stretch, send signal to brain
-signal sent via vagus & glossopharyngeal nerves to cardiac and vasomotor centers → sympathetic response
-VM = release NE. A1 constrict, B2 dilate. Overal constriction. ↑ R
-C = stimulate SA/AV node and contractile cells. ↑ HR ↑ SV
↑ CO and ↑ R means ↑ MAP. BP increases
How does your body compensate when your BP rises? Name all the mechanisms that happen
-baroreceptors (aortic & carotid) detect more stretch, send signal to brain
-signal sent via vagus & glossopharyngeal nerves to cardiac center (NOT vasomotor) → parasympathetic response
-C = stimulate SA/AV node ↓ HR. No effect on SV
-↓CO means ↓ MAP. BP lowers
name all the hormones that regulate BP
EPI, NEP, Aldosterone, Angiotensin II (AT2), Atrial natriuretic peptide, Antidiuretic hormone (ADH)
→ they all work by modifying resistance, blood volume, or both
how to modify blood volume?
-intake of fluids
-modify urine output
→ more urine retained and drink more = higher BV
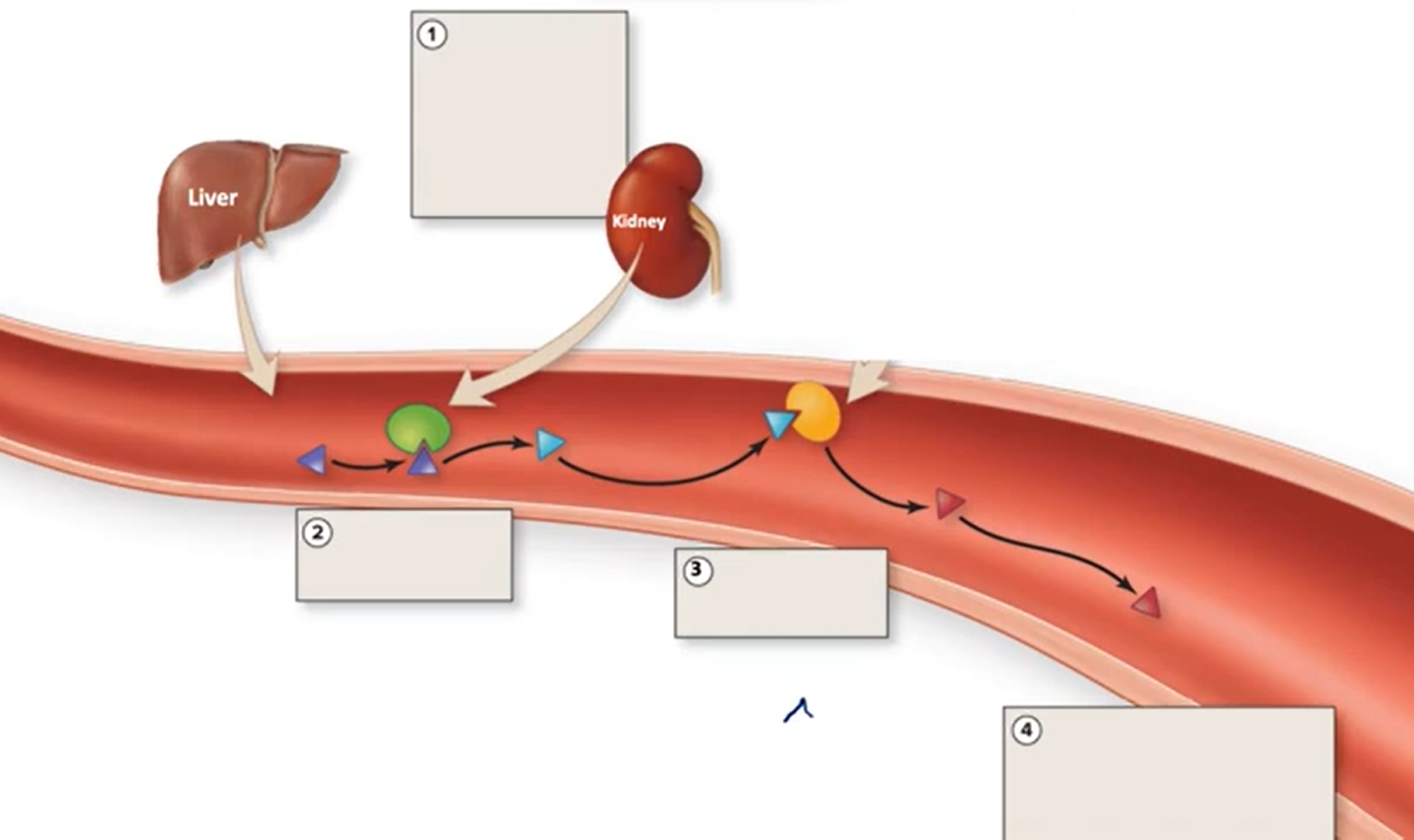
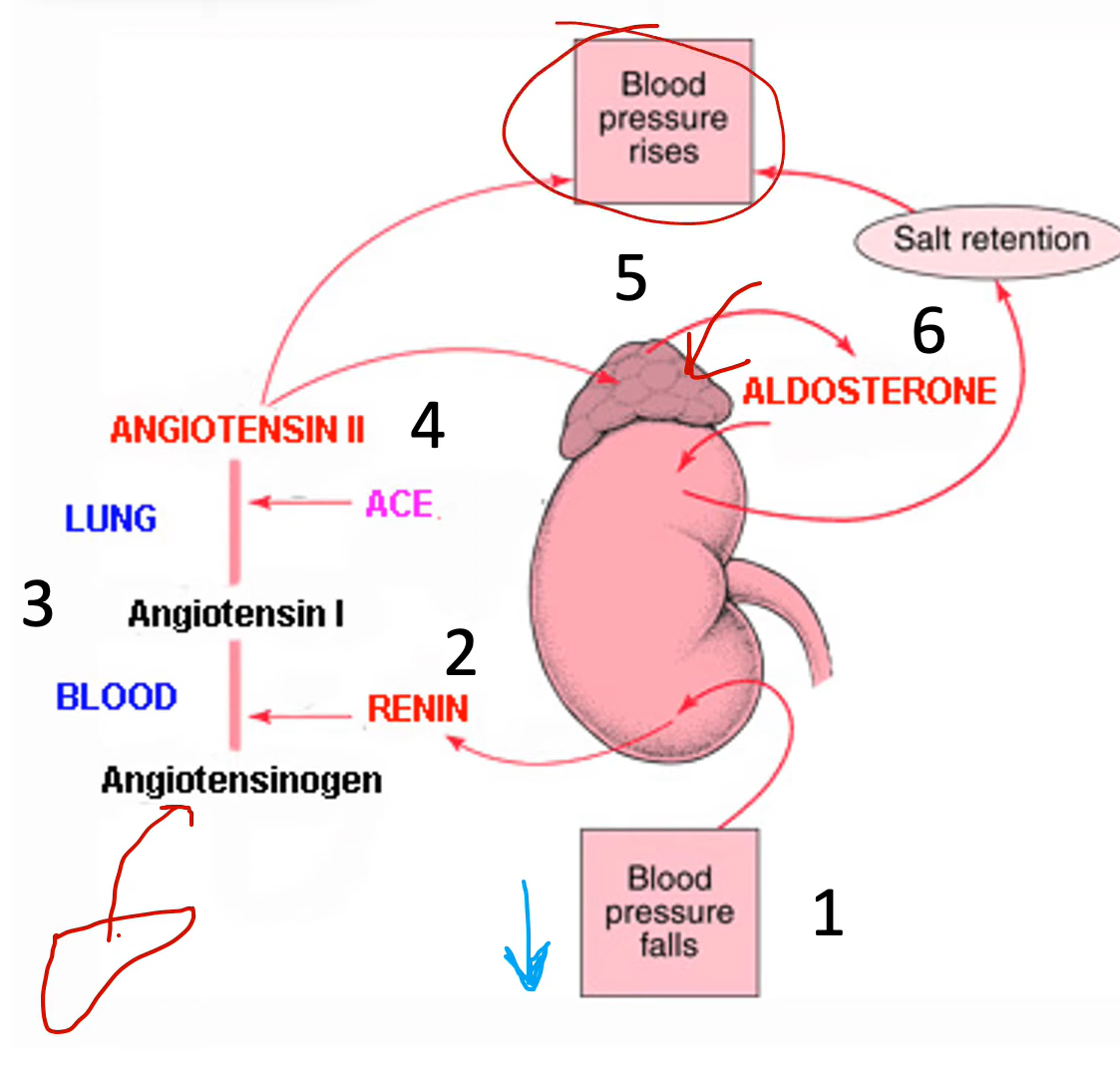
renin-angiotensin system (RAS) → how is AT2 produced?
-liver continuously produces angiotensinogen, an inactive hormone, and puts into blood
-during low BP or a symp. response, kidney will release renin into blood
-renin converts angiotensinogen into angiotensin I (AT1), but AT1 is still inactive
-AT1 goes to pulmonary capillary endothelium (lungs), where angiotensin-converting enzyme (ACE) turns AT1→AT2
-now AT2 is active
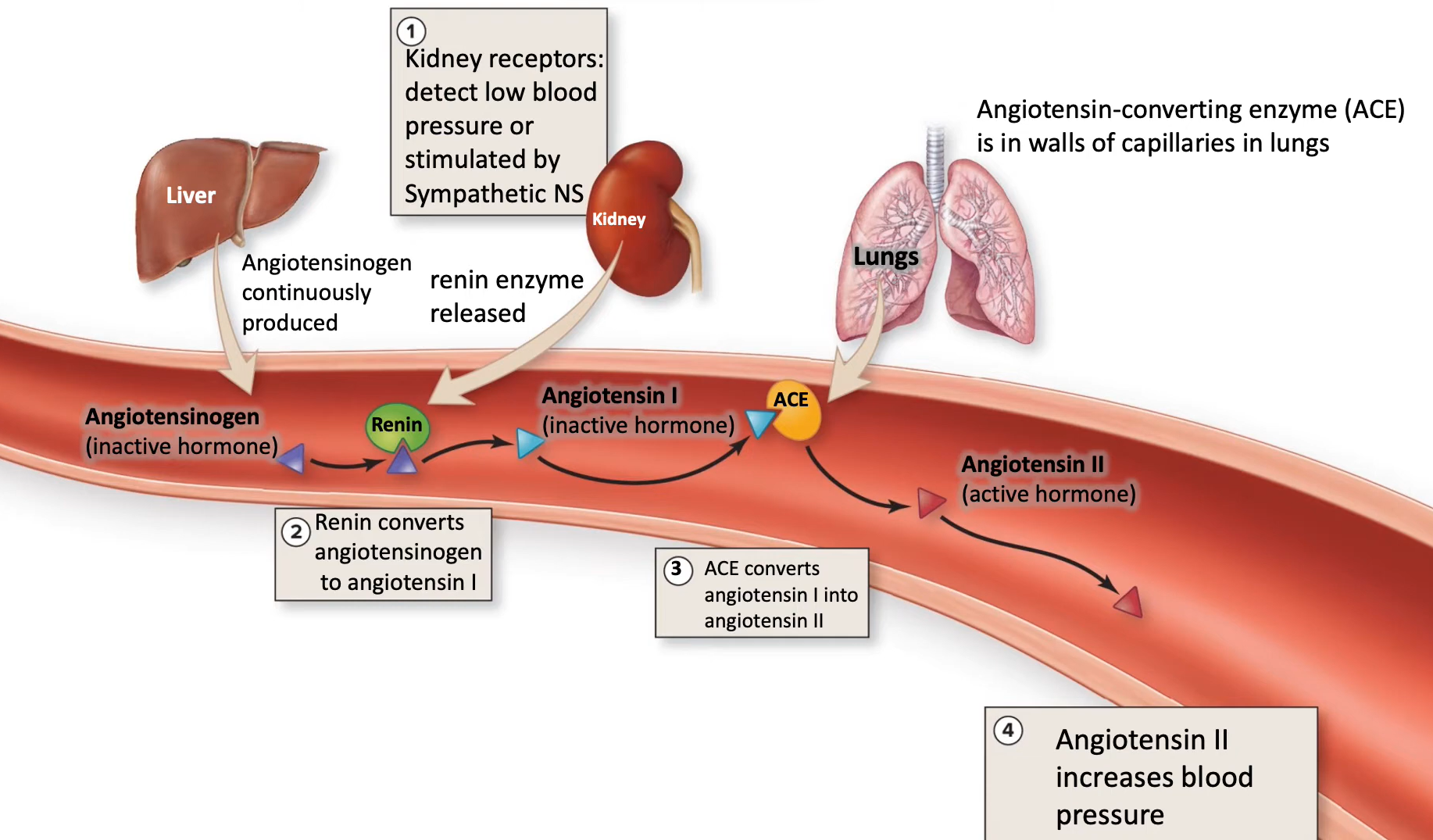
why does AT2 conversion happen in the lungs?
all blood in body eventually ends up in lungs, so having conversion in lungs mean it maximizes contact btwn AT1 and ACE
How does AT2 affect BP?
1) vasoconstrictor (effect greater than NEP) → raise resistance
2) stimulate thirst center in hypothalamus → fluid intake raise BV
3) act on kidneys to decrease urine output → stimulate aldosterone and ADH release
→ all of these raise BP
aldosterone
-maintain BV and BP
-released from adrenal cortex (kidney)
-triggered by several stimuli, including AT2
-increase absorption of sodium ions and water in kidney → decrease urine output