open ended questions gen path
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
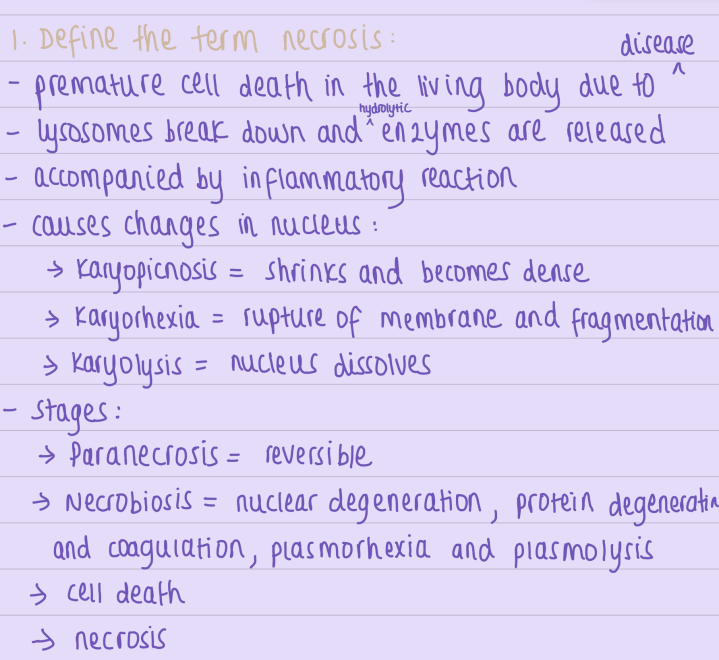
define necrosis, steps
types of necrosis
1. Coagulative ➡ inhibits lytic enzymes in organs with high protein content and low water
Heart, Liver, spleen and Kidneys
organ becomes pale, firm and then becomes yellow
It occurs when blood flow stops
ischemic —> hypoxia —> enzyme and protein denaturation
denatured enzymes —>
The cell has an outline but no nucleus
2. Liquefactive ➡ dissolution of tissue using lytic enzymes
commonly in the brain and forms a pseudocyst
also occurs in purulent inflammation
liquified tissue is soft and made from disintegrated cells and tissue
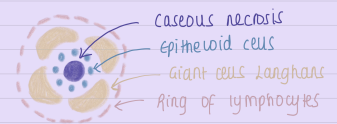
3. Caseous ➡ coagulative and liquefactive necrosis
occurs in the centre of a tuberculous granuloma
white, cheesy centre
Definition of Amyloid - Describe sago spleen and lardaceous spleen:
Here's the text from the image:
3. Definition of Amyloid - Describe sago spleen and lardaceous spleen:
Amyloid refers to an abnormal extracellular deposition of insoluble protein material in tissues.
95% - Fibrillar part = B-pleated sheet
5% - Non fibrillar = P-component
Macroscopically = large, firm, waxy
Microscopically = structureless
Staining = congo red + = orange
Sago's spleen
Translucent, pale, waxy nodules
no splenomegaly
microscopically = Amyloid in walls of arterioles in white pulp
overtime replaces follicles
Lardaceous spleen
Splenomegaly
cut surface shows streaks of Amyloid
microscopically = deposits in CT of red pulp
Kidney
1. Gross Changes
Enlarged, pale, firm, waxy kidneys (early stage).
Shrunken, fibrotic kidneys (late stage).
2. Microscopic Changes
Glomerular deposits → Thickened capillary walls, glomerulosclerosis, proteinuria.
Tubular deposits → Tubular atrophy, protein casts.
Vascular deposits → Thickened vessels, ischemia.
Interstitial fibrosis → Chronic damage and renal dysfunction.
Clinical Consequences
Nephrotic Syndrome (proteinuria, oedema).
Chronic Kidney Disease (CKD) → requiring dialysis.
Hypertension
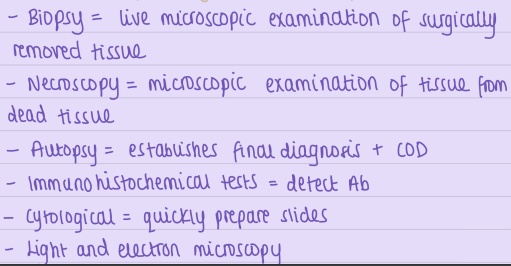
what are the pathological methods of examination?
types of chronic inflammation?
Types:
(1) Non-specific:
= irritant produces non-specific chronic inflammatory response, formation of granulated tissue and healing by fibrosis (e.g. chronic ulcer/lung abscess)
(2) Specific:
= injury causes a characteristic histological tissue response (e.g. TB, leprosy, syphilis)
Hypertrophy- definition
Hypertrophy
Definition - increase in size of parenchymal cells
Enlargement of organ or tissue without changing the number of cells
Hypertrophy- types and examples
- Types: physiological or pathological
Physiological Hypertrophy
Neurohormonal Stimuli:
Female breast: Enlargement during puberty and lactation.
Uterus: Growth during pregnancy.
Prostatic hyperplasia: In elderly men due to hormonal changes.
Working Hypertrophy:
Skeletal muscle in athletes: Increased functional demand leads to the production of more myofilaments, enlarging the muscle fibers.
Pathological Hypertrophy
Neurohormonal Stimuli:
Atrophy of testes: Due to hormonal imbalances or dysfunction.
Hyperfunction of anterior pituitary: Excessive growth hormone production.
Hypertension: Increased workload causes hypertrophy of cardiomyocytes due to the production of more myofilaments.
Working Hypertrophy:
Cardiac muscle hypertrophy: Occurs in hypertension or aortic valve disease.
Smooth muscle hypertrophy: Seen in pyloric stenosis.
Bladder hypertrophy: Due to obstruction caused by an adenoma of the prostate gland.
Compensatory Hypertrophy:
Liver regeneration: Following partial hepatectomy, remaining liver cells grow to compensate for the lost tissue.
Epidermis: Increased thickness following abrasion or injury.
Myocardium: Enlargement after a myocardial infarction as a compensatory mechanism.
Substitutional Hypertrophy:
After nephrectomy: In young patients, the remaining kidney may be replaced by connective tissue as an adaptive response.
Hypertrophic Vegetations:
Chronic inflammation of mucous membranes: Leads to tissue thickening.
Granulation tissue formation: During wound healing.
which organs are most affected by fat degeneration?
Fat degeneration refers to the abnormal accumulation of lipids in cells
1. Liver Causes:
Alcoholic steatosis (chronic alcoholism):
Increased fatty acid (FA) synthesis and reduced FA oxidation due to alcohol.
Diabetes mellitus:
Decreased insulin leads to increased lipid accumulation.
Malnutrition:
Reduced lipoprotein production prevents lipid transport from the liver, causing fat buildup.
Morphological Features:
Macroscopically:
Enlarged, round, pale, greasy, and waxy liver.
Microscopically:
Lipid vacuoles appear in the cytoplasm of hepatocytes.
Vacuoles push the nucleus to the periphery of the cell.
2. Heart (Tiger Heart) Causes:
Fatty degeneration of cardiac muscles occurs due to hypoxia or systemic metabolic disorders.
Morphological Features:
Macroscopically:
Enlarged heart with flabby, stretched chambers.
Striped or “tiger-like” appearance due to fatty streaks in the myocardium.
Microscopically:
Fatty vacuoles are seen in the papillary muscles and trabeculae, giving the myocardium a striped look.
3. Kidney Causes:
Commonly seen in nephrotic syndrome, associated with lipid metabolism abnormalities.
Morphological Features:
Macroscopically:
Enlarged and flabby kidneys.
The cortical substance appears grey with yellow lipid droplets.
Microscopically:
Lipids accumulate in the cytoplasm of epithelial cells in the convoluted tubules.
Microscopic Proof of Fat Degeneration
Light Microscopy (Normal Staining) 🔬
Unfixed or Formalin-fixed tissue: Best observed without alcohol-based fixation since alcohol dissolves lipids.
Cryosectioning (Freezing Microtome): Used to preserve lipids.
Stains Used:
Sudan III → Lipids appear orange-red.
Oil Red O → Lipids appear red.
Hematoxylin and Eosin (H&E) → Shows clear vacuoles (ring-like appearance) since fat dissolves during processing.
Polarized Light Microscopy
Purpose: Detects neutral lipids & cholesterol esters using birefringence (double refraction of light).
Key Finding:
Cholesterol crystals → Show bright birefringence under polarized light.
Electron Microscopy (Ultrastructural Level)
Fixation: Uses osmic acid, which binds lipids and hardens them for detailed observation.
Processing: Tissue is cut into ultrathin sections using an ultramicrotome.
Key Findings:
Lipid droplets → Seen as dark-staining structures.
Membrane-bound liposomes → Abnormal lipid accumulation in organelles.
Morphological Proof of AMYLOIDOSIS
Amyloidosis Overview
Definition: Extracellular accumulation of insoluble amyloid proteins.
Morphological Proof:
Macroscopic Features:
Affected organs are enlarged, firm, and waxy.
Staining Test:
Paint the surface with iodine (I₂), then add sulfuric acid (H₂SO₄):
Positive test: Color changes to yellow, then blue.
Microscopic Features:
Hematoxylin and Eosin (H&E) staining shows a structureless homogenous appearance.
Congo red staining:
Turns amyloid deposits orange-red.
Under polarized light: Exhibits apple-green birefringence.
Distinction Between AA and AL Amyloidosis:
Treat with potassium permanganate, then Congo red:
AA amyloidosis: Congo red becomes negative.
AL amyloidosis: Congo red remains positive.
How many types of hemoglobinogenic pigments do you know? Describe a histochemical reaction which is used to prove them
2 groups of hemoglobinic pigments:
① Non-iron containing : bilirubin
② Iron containing :
➡ Ferritin = blood protein that stores iron, located in the spleen, liver, BM and LN
➡ Hemosiderin = iron storage molecule which contains ferritin in mononuclear phagocytes, looks like golden brown pigment
Stain = prussian blue / Pearls ➡ stained blue
Describe morphologically coagulative, fat and fibrinoid necrosis
Coagulative ➡ inhibits lytic enzymes in organs with high protein content and low water
Heart, Liver, spleen and Kidneys
organ becomes pale, firm and then becomes yellow
It occurs when blood flow stops
The cell has an outline but no nucleus
Fat ➡ occurs in adipose tissue of the pancreas after leakage of the lipase enzyme due to injury or obstruction of the pancreatic ducts
looks like yellow-white deposits in the adipose tissue
microscopically = pale outlines and soap filled cytoplasm
Fibrinoid ➡ in hypertension, the walls of small arteries get damaged which causes deposition of fibrin
Identification = bright eosinophilic hyaline-like deposits in vessel walls
Definition of hemorrhagic infarction. Explain its mechanism and give examples of organs it is seen in:
Hemorrhagic infarction Type I: Occlusion of arteries of organs with double blood flow (lungs, collateral arteries in intestines), necrosis occurs first then hemorrhage
Hemorrhagic infarction Type II: Venous infarction, veins dilate then rupture (intestines), hemorrhage first then necrosis
Describe the structure of granulomas in TB and sarcoidosis
TB has caseous granuloma but sarcoidosis has non-caseous granuloma.
Sarcoidosis has a small amount of lymphocytes and giant cells with no necrosis.
What does the term 'nutmeg liver' mean? What is its morphological appearance:
cyanosis of the liver that turns into nutmeg liver
mottled appearance of liver due to hepatic venous congestion
- 2 types:
① Straight = hypoxia causes cell injury and fatty degeneration of liver around the central vein and middle of sinusoid
② Reverse = peripheral cells are also damaged and have fatty degeneration, causes fibrosis and cardiac cirrhosis because all the hepatocytes die
macroscopically = red and yellow dots on the surface
microscopically = centrilobar hemorrhagic necrosis and fibrosis
How do we form the names of benign and malignant mesenchymal tumors? Give 3 examples:
Benign have suffix 'oma'
Malignant are given 'sarcoma' or 'carcinoma'
Glandular tissue:
Benign = Adenoma
malignant = Adenocarcinoma
Squamous epithelium:
Benign = papilloma
malignant = squamous cell carcinoma
Other:
Benign = fibroma, lipoma, leiomyoma, osteoma
malignant = fibrosarcoma, liposarcoma, leiomyosarcoma
what are exceptions of the tumour naming rule?
Exceptions:
Hepatocellular carcinoma: This is a malignant tumor of the liver, but it ends in "-carcinoma" even though it arises from hepatocytes (liver cells), which are epithelial in origin.
Lymphoma: This is a malignant tumor of the lymphoid tissue, but it doesn't follow the "-sarcoma" rule.
Melanoma: This is a malignant tumor of melanocytes, but it doesn't end in "-sarcoma."
Describe the types of hemorrhages depending on their mechanism of development and give examples
Hemorrhage = bleeding of vessels
According to origin: cardiac, arterial, venous, capillary
According to mechanism of development:
① External
Epistaxis = nose bleed
Hematemesis = vomiting blood
Hematuria = blood in urine
Melena = dark faeces from upper GI bleed
Hemoptysis = coughing blood
Menorrhagia = severe / long menstruation
② Internal
Petechiae = mini puncture hemorrhages, usually on skin or conjunctiva
Purpura = blood accumulation in tissue between cells
Bruise = blood accumulation in skin or mucous membrane (purple -> green -> yellow as bilirubin is oxidised)
Hematoma = blood in soft tissue
Hemothorax = blood in pleural cavity
Hemoperitoneum = blood in peritoneal cavity
Hemopericardium = blood in pericardium
Describe the morphological changes in nutmeg liver. What are the reasons for its development?
Liver is enlarged, tender and tense capsule
The cut surface of the liver shows red and yellow mottled appearance
More severe hypoxia in the centrilobular zone instead of the peripheral zone so more pronounced changes
Shows nutmeg appearance because of dilated central veins and unaffected surrounding tissue
Describe the mechanism of the third type of hypersensitivity reaction?
involves tissue injury mediated by immune complexes ➡ example of immune complex-mediated injury where antigen-antibody complexes
Not normally organ specific and formed in circulation.
IgM / IgG antibodies form complexes with antigens which causes inflammation which attracts more immune cells
➡ by activating complement system
⬇
activates neutrophils and macrophages
⬇
releases inflammatory mediators responsible for injury
18. List at least three types of granulomas containing different types of giant multinucleated cells. Describe
Tuberculosis
granuloma = tubercle
central caseous necrosis surrounded by epithelioid cells, Langhans cells, lymphoid cells + plasma cells
Syphilis
area of gummous (clay-like) necrosis
surrounded by mononuclear inflammatory cells
granulation tissue also forms around the gumma
Sarcoidosis
tissue contains few granulomas made of epithelioid macrophages, a few lymphocytes and giant cells
NO central necrosis
Giant cells
fusion of macrophages or epithelioid cells
20+ nuclei with different arrangements:
➡ at periphery like a horse shoe ring
➡ clustered at 2 poles = Langhans cells
➡ centrally = foreign giant body cells
Which are the reasons for the brown induration of the lungs? Briefly describe the pathological changes
① Right heart Failure
Brown coloured lung and congested
due to enlargement of right ventricle
↑ BP in the lungs caused by chronic lung disease
② Left heart Failure
Aortic Stenosis / weakened left ventricular wall
causes pulmonary oedema due to dilated and congested capillaries
capillaries rupture resulting in small hemorrhages
Hemoglobin is phagocytosed by alveolar macrophages
➡ lysis of heme = bilirubin and iron
➡ stored as hemosiderin
cells uptake hemosiderin pigments in macrophages
converted into 'heart failure cells'
Phagocytes with brown pigment = brown induration
20. List types of exogenous pigments - which pigment is proven by Pearl’s reaction?
Inhaled:
Coal/carbon in alveolar macrophages, looks like black pigment around bronchi = anthracosis
Ingested
Lead in mineralized tissue, looks like blue lines on teeth
Silver in skin/liver/kidneys; causes hemorrhages, ⬇ Erythrocytes and immune dysfunction
Copper in eyes/brain/liver; causes Cu poisoning
Carotenoids in skin, makes skin look orange
Injected
Tattoo ink ➡ in skin macrophages which stay in the CT
can cause LN infection
# Hemosiderin stained in Pearls reaction
. What are the most common source of pulmonary thromboembolism:
Pulmonary thromboembolism ➡ fatal as occludes pulmonary arterial tree, more common in bedridden patients, most fatal from deep veins of lower extremities
causes:
detachment of thrombi which flows through venous drainage and enters right heart side
a large thrombus could lodge at the bifurcation of the pulmonary arteries of the right ventricle
OR could be multiple emboli or a fragmented large one
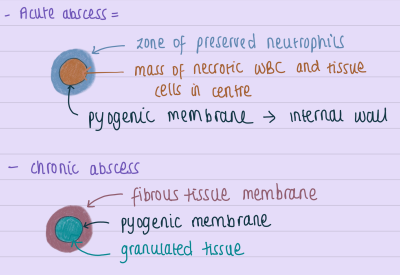
Define an abscess. What form of pathological process is it? Describe an acute and chronic abscess.
Abscess = localized inflammation caused by acute bacterial infection and neutrophils infiltrating the inflamed tissue ➡ causes necrosis
The cavity formed = abscess
➡ contains pus
Benign and malignant tumors of smooth muscle tissue - names, morphology and organ localization:
Tumors are characterised by:
macroscopic features
microscopic features
growth rate
local invasion ➡ lymph nodes
metastasis
Benign tumours:
spherical or ovoid
encapsulated
freely movable
firm structure
malignant tumors:
irregular shape
extend into adjacent tissue
metastasize
sarcomas = flesh like consistency
carcinomas = firm
Names:
CT ➡ fibroma / fibrosarcoma
Fat tissue ➡ lipoma / liposarcoma
Smooth muscle ➡ leiomyoma / leiomyosarcoma
Cartilage tissue ➡ chondroma / chondrosarcoma
Bone ➡ osteoma / osteosarcoma
Blood vessels ➡ hemangioma / hemangiosarcoma
Describe the type of hemorrhages depending on their mechanism of development and give examples
Mechanism of hemorrhage:
Destruction of blood vessel wall
Diapedesis of erythrocytes because of increased permeability of vascular wall
Ulceration of vessel wall
Type depending on location:
Hemothorax = in pleural cavity
Hemoptysis = from lungs
Metrorrhagia = from uterus
Hemoarthrosis = in joint cavity
Hemopericardium = in pericardial cavity
Hemoperitoneum = inside abdominal cavity
Depending on site of origin:
Cardiac = after heart wound
Arterial = due to trauma and rupture of dissecting aneurysm
Capillary = due to vessel wall weakness / trauma
Venous = trauma / surgical procedures
What are benign pigment tumors:
Benign:
Nevi ➡ brown spots of different size, can be flat or elevated or wart like
Junctional nevi ➡ nests of nevus cells on the borders of epidermis and dermis, round or oval, homogenous slightly granular cytoplasm
Compound nevus ➡ Nevus cells are present in both the epidermis and dermis.
Intradermal nevus ➡ Nevus cells located only in the dermis, forming compact nests.
Epitheloid cells ➡ often on the face, flat node
Blue nevus ➡ bluish - Brown/grey spot, round or oval and is not elevated
What are malignant pigment tumors:
Malignant:
Melanoma ➡ one of the most malignant, spreads through lymphatic and blood, 70% on the skin, 4 types:
① Lentigo maligna melanoma: develops from lentigo
② Invasive melanoma: slightly elevated lesion with different colours and ulcerated surface, may not contain pigments, contains haemorrhages and necrosis, localised on: skin, the pigment of the eye, meninges and a medullar layer of the adrenal gland
③ Acral lentigenous melanoma: more common on soles and palms with ulceration
④ Nodular melanoma: elevated and deeply pigmented nodule with rapid growth and ulceration ➡ worst prognosis