Exam 4 knes 364
1/47
Earn XP
Description and Tags
TTK
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Pacemaker
Used in patients with sinoatrial node dysfunction or any other problem with the electrical conduction system of the heart.
Additionally, the source states that pacemakers can pace the atria, the ventricles, or both.
Clinical Exercise Tolerance Testing (ETT)
A test to assess the heart's and lungs' response to exercise. Also referred to as Graded Exercise Test (GXT) or Exercise Stress Test. May or may not include additional imaging.
Indications for Clinical Exercise Testing
Diagnosis (determine presence of ischemic cardiovascular disease), Prognosis (risk for future adverse event), Evaluation of physiological response to exercise (e.g., blood pressure response, peak exercise capacity), and developing an accurate/personalized aerobic exercise prescription (prescribing relative intensities).
Graded Exercise Test (GXT)
A type of clinical exercise test. Terms GXT, Exercise Stress Test, and Exercise Tolerance Test (ETT) are often used interchangeably and may or may not include additional imaging.
Cardiopulmonary Exercise Test (CPET)
A clinical exercise test that includes a metabolic cart with gas exchange analysis. Also referred to as an exercise metabolic test.
What can GXTs detect?
Peak exercise capacity, Abnormal hemodynamic response to stress, Arrhythmias, and ST segment changes (myocardial ischemia/infarction). GXTs may also yield false negative or false positive results.
Ischemic Threshold
The intensity of exercise if/when evidence of myocardial ischemia appears. Rate-Pressure Product (RPP) is a repeatable estimate of this.
Rate-Pressure Product (RPP)
Also known as double product. A surrogate for myocardial oxygen uptake, calculated as HR x SBP.
Normal Heart Rate (HR) Response to Incremental Exercise.
Increase of ≈10 beats/min per 1 MET of exercise
Chronotropic Incompetence
Failure to achieve ≥85% of age-predicted HRmax in the presence of maximal effort. Independently associated with increased risk of morbidity and mortality.
Abnormal HR Recovery
Failure of the HR to decrease by at least 12 beats during the first minute or 22 beats by the end of the second minute of active post-exercise recovery is strongly associated with increased mortality risk in patients with ischemic heart disease.
Hypertensive Blood Pressure (BP) Response to Exercise (Abnormal)
SBP >250 mm Hg (relative indication to stop), SBP ≥210 mm Hg in men or ≥190 mm Hg in women (exaggerated response), or peak SBP >250 mm Hg or an increase in SBP >140 mm Hg above resting value (predictive of future resting hypertension).
Hypotensive Blood Pressure (BP) Response to Exercise (Abnormal)
Decrease of SBP below resting value or by >10 mm Hg after a preliminary increase during exercise. Associated with ischemia, LV dysfunction, and increased cardiac event risk.
Diastolic BP Change During Exercise (Abnormal)
A peak DBP >90 mm Hg or an increase in DBP >10 mm Hg above resting value. DBP >115 mm Hg is an exaggerated response and a relative indication to terminate the test.
ST Segment Depression During Exercise (Abnormal EKG Response)
Should be present in at least 3 consecutive cardiac cycles within the same lead. Considered suggestive of ischemia if horizontal or downsloping ≥1 mm at 80 ms (2 small boxes) after the J point. Also if it occurs during post-exercise recovery or at a low workload/RPP.
ST Segment Elevation During Exercise (Abnormal EKG Response)
>1 mm in leads with Q waves is suggestive of ischemia and can indicate myocardial infarction.
J Point or J Junction
The junction between the QRS complex and the ST segment on an EKG.
Lecture 2: 364FalsePosNegSpecialETTs
False Negative Result in Exercise Testing
A GXT and/or EKG result that does not suggest ischemia but CAD does, in fact, exist. Resting and/or exercise ECG may not catch everything.
Potential Causes of False Negative Results in Exercise Testing
Failure to reach an ischemic threshold, monitoring an insufficient number of leads, failure to recognize non-ECG signs/symptoms of CVD (e.g., exertional hypotension), angiographically significant CVD compensated by collateral circulation, musculoskeletal limitations to exercise preceding cardiac abnormalities, technical or observer error.
False Positive Result in Exercise Testing
A GXT and/or EKG result that suggests ischemia, but ischemia does NOT actually exist.
Potential Causes of False Positive Results in Exercise Testing
ST-segment depression >1.0 mm at rest, Left ventricular hypertrophy, accelerated conduction defects (e.g., Wolff-Parkinson-White syndrome), Digitalis medication, Nonischemic cardiomyopathy, Hypokalemia (low potassium levels), Vasoregulatory abnormalities, technical or observer error.
How to Decrease Likelihood of False Positive/Negative Results in Exercise Testing
The inclusion of adjunctive imaging can increase testing sensitivity and/or provide additional information. Examples include Myocardial Perfusion Imaging, Cardiac Computed Tomography (CT), Cardiac Magnetic Resonance Imaging (MRI), and Stress Echocardiography.
Coronary Angiography
Considered the gold standard for diagnosing heart disease. A follow-up test if GXT suggests ischemia.
Myocardial Perfusion Imaging
Uses radioactive isotopes to highlight metabolically active tissue in the heart. Delivery of the isotope is proportional to coronary blood flow. Can detect ischemia and infarction.
Stress Echocardiography
Ultrasound evaluation of wall motion, wall thickness, and valve function immediately after exercise. Deterioration in regional wall motion with exercise suggests myocardial ischemia.
Pharmacological Stress TestENT
Used when a patient cannot exercise. Medication (e.g., Lexiscan, Adenosine) is used to increase blood flow and vasodilation.
Exercise Prescription for Cardiovascular Patients - Intensity
RPE 1-3/10 initially, progressing to 4-7/10; 40-80% of HRR and VO2Reserve in absence of adverse signs/symptoms/EKG changes. If an ischemic threshold exists, the upper HR limit should be 10 bpm below the HR at which ischemia signs/symptoms occur.
Angina Scale
0 = No pain,
1 = Mild, barely noticeable,
2 = Moderate, bothersome,
3 = Moderately severe, very uncomfortable,
4 = Most severe or intense pain ever experienced.
Dyspnea Scale
This specific scale was not provided in the sources. However, monitoring for increased shortness of breath is important in certain populations like CHF.
Claudication Scale
0 = No pain,
1 = Definite discomfort or pain, but only at initial or modest levels,
2 = Moderate discomfort or pain from which the patient's attention can be diverted,
3 = Intense pain from which the patient's attention cannot be diverted,
4 = Excruciating and unbearable pain.
Special Considerations for Exercise in Patients Post-Myocardial Infarction (MI) or Percutaneous Transluminal Coronary Angioplasty/Intervention (PTCA/PTCI)
Resistance training should not start until after 5 weeks (MI) or 3 weeks (PTCA/PTCI). 4 weeks (MI) and 2 weeks (PTCA/PTCI) of supervised aerobic exercise are recommended before resistance training.
Special Considerations for Exercise Post-Coronary Artery Bypass Graft (CABG)
Resistance training is generally not allowed for 10-12 weeks post-surgery.
Special Considerations for Exercise in Patients with Congestive Heart Failure (CHF)
Exercise only for stable CHF. Assess Functional Capacity (>3 METs needed). Medications can affect exercise response (use RPE). Monitor for increased shortness of breath, fatigue, angina, edema, weight gain. Focus on increasing duration/frequency before intensity. Use extended warm-up/cool-down. Main cause of death is cardiac arrest (monitor closely).
Special Consideration for Exercise in Patients with Implantable Defibrillators (AICDs)
Be aware of the device's set upper and/or lower heart rate limits. Do not prescribe exercise that exceeds these rates!.
Special Considerations for Exercise in Patients with Peripheral Arterial Disease (PAD)
Often deconditioned. Walking is the primary aerobic exercise to build collateral circulation. General prescription: "Walk until it hurts. Stop and rest. Walk again." May start with short bouts (<10 min), working up to 30-60 min/day.
American Diabetes Association (ADA) Guidelines for Aerobic Exercise - Starting Blood Glucose
Starting blood glucose must be ≥ 120 mg/dl.
Ending blood glucose must be > 70 mg/dl
If values too low: feed 15g of CHO and recheck blood glucose in 15 min. intervals.
Be aware of insulin-stimulating medications in combination with aerobic exercise – at higher risk for exercise-induced hypoglycemia.
American Diabetes Association (ADA) Guidelines for Aerobic Exercise - Ending Blood Glucose
Ending blood glucose must be ≥ 70 mg/dl.
Safety Precautions/Concerns and Clinical Signs of Concern for Diabetics During Exercise
Monitor for signs/symptoms of hypoglycemia (shakiness, weakness, sweating, etc.) and hyperglycemia (fatigue, headache, thirst, etc.).
Follow ADA guidelines for starting/stopping exercise based on blood glucose.
Be aware of exercise-induced hypoglycemia with insulin-stimulating medications.
Consider peripheral and autonomic neuropathy (balance issues, silent ischemia - use RPE). Monitor foot health and wound healing.
CVA (cerebrovascular Accident or stroke
Sudden numbness or weakness
of the face, arm or leg,
especially on one side of the
bodySudden confusion, trouble
speaking or understandingSudden trouble seeing
Sudden trouble walking,
dizziness or loss of balanceSudden severe headache with
no known cause
Ischemic Stroke
Obstructed cerebral artery limits O2 delivery
Cerebral thrombosis (clot)
Cerebral embolism (blockage)
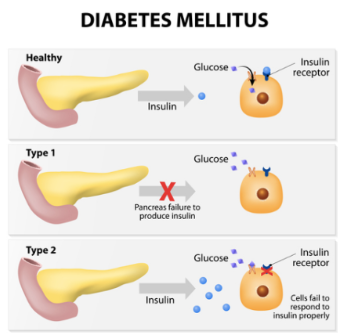
Diabetes Mellitus
Metabolic disease that affects carbohydrate metabolism
Causes hyperglycemia
At risk for ketoacidosis
Diabetic Concerns and Complications
Cardiovascular disease (all forms)
Chronic Kidney Disease
Neuropathy
Eye disorders (blindness/vision changes)
Dental disease
Non-healing wounds/Amputations
Diabetes Mellitus Type 1 (5-10% of cases)
Autoimmune disease
β-cells destroyed, no insulin produced
Sudden onset, often in childhood or young adult
Diabetes Mellitus Type 2 (90-95% of cases)
Insulin insensitivity (resistance), gradual onset
Impaired insulin secretion, action, responsiveness
Result of lifestyle factors, obesity
Hypoglycemia
(BG < 70 mg/dl)
Signsand/symptoms
Shakiness
Weakness
Abnormal sweating
Nervousness
Anxiety
Hunger
Headache
Visual disturbances
Mental dullness
Confusion
Hyperglycemia
(BG > 300 mg/dl)
Fatigue
Headache
Weakness
Increased thirst
Blurred vision
Increased urination (polyuria)
Diabetic Ketoacidosis (DKA)
Acetone or fruity smelling breath
Nausea and vomiting
Shortness of breath
Dry mouth
Confusion
Coma
Abdominal pain
Exercise Considerations for Diabetics
Combination of resistance and aerobic training is optimal
Exercise enhances insulin sensitivity
Muscle contraction mimics insulin action -lowering blood glucose
Decreases insulin requirement due to exercise's effect on lowering blood glucose
Enhances insulin receptor sensitivity for up to 72 hours
Timing of exercise is important in relation to medication effects, meal timing, and current blood glucose levels
Exercise Considerations for Diabetics
Follow ADA guidelines
Monitor for hypo/hyperglycemia symptoms
Peripheral Neuropathy can cause balance and gait issues, and lead to unnoticed wounds
Autonomic Neuropathy can lead to chronotropic incompetence and silent ischemia. Use RPE to judge exercise intensity
Monitor wound healing – address blisters, ulcers, cuts, etc.