Chapter 14, Psychological Disorders
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
What is abnormal: The role of culture
Cultural concepts of distress:
A pattern of mental illness, distress, and/or symptoms that is unique to a specific ethnic or cultural population
Does not conform to standard classifications of psychiatric disorders
Some behaviours are not culturally specific
Ex. Schizophrenia, bipolar disorder, panic disorder - biological bases
(May have different meanings across cultures)
Koro:
An episode of sudden illness and intense anxiety that the genitals recede into the body and possibly causes death
(Chinese, Malaysian, and Indonesian)
Amok Syndrome:
Period of brooding followed by a sudden outburst of indiscriminate murderous frenzy, sometimes provoked by an insult, jealousy, or a sense of depression
(Brunei, Singapore, Malaysia, Indonesia, Philippines, Timor-Leste)
4 D’s (actually 5 lol)
Deviance
Departure of what is normal/usual
Refers to behaviours, thoughts, and feelings that are not in line with generally accepted standards
Culturally - based
Distress
Behaviors, thoughts, and feelings that are upsetting and cause pain, suffering, or sorrow
Dysfunctional
Behaviors, thoughts, and feelings are disruptive to one’s regular routine or interfere with day-to-day functioning
Dangerous
Behaviors, thoughts, and feelings may head to harm or injury to self or others
Duration
The interval between the onset of a psychiatric disorder and the administration of the first pharmacological treatment
(to get a diagnosis, the abnormal behaviours need to persist for a specific amount of time)
Psychological disorder:
Patterns of deviant and dysfunctional behaviors, thoughts, and/or feelings that cause significant dishes, and may even be dangerous, and last for a specific amount of time.
History of Psychiatry: 1840
First attempt in the US to gather info. about mental health (ideas of idiocy and insanity)
History of Psychiatry: 1883
Emil Kraplin
Published a system of psychological disorders centered around a pattern of symptoms
7 categories:
Mania
Melancholia
Monomania
Paresis
Dementia
Dipsomania
Epilepsy
History of Psychiatry: 1918
America Medico-Psychological Association changed its name to the American Psychological Association (APA)
Issued the statistical manual for use of institutions for the insane
(Beg. of Diagnostic Materials)
First Diagnostic Manuals
1921: Americana Medical Association’s standard Classification Nomenclature of Disease
22 different categories, 21 psychotic conditions
History of Psychiatry: 1946
US army psychiatrists following WW2
High proportion of soldiers in combat suffered psychiatric breakdowns
Kinds of breakdowns they had (clearly response to stressful experiences) weren’t encompassed by existing manual (in-patients)
Model for first DSM
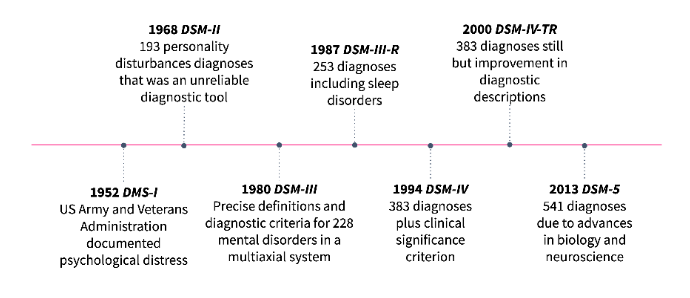
Diagnostic and statistical manual for mental disorders (DSM-I) 1952
Combined 2 major influences:
Adolf Meyer → emphasized how most mental disorders represented personality reactions to psychological, social, and biological factors
Sigmund Freud → general underlying processes rather than outward symptoms
- Unreliable diagnostic tool, but the first tool to focus on clinical use
- Concepts had not been scientifically tested
- 10 Categories for psychoses and psychoneuroses
- 7 Categories for disorders of character, behavior, and intelligence
Diagnostic and statistical manual for mental disorders (DSM-II): 1968
193 personality disturbance
Based on psychoanalytic theory
Unreliable diagnostic tool - didn’t pay a lot of attention to symptoms of some conditions, much more general in their outlook
Eliminated the term reaction but kept the term neurosis
Increased attention to children and adolescents is not seen in the previous version
Diagnosis of homosexuality renamed “sexual orientation disturbance”
Diagnostic and statistical manual for mental disorders (DSM - III): 1980
Why?
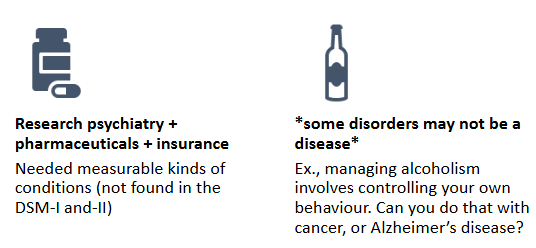
Research psychiatrists
Consistent diagnostic criteria across different clinicians
Pharmaceutical industry
Products originally marketed for general conditions, not particular diagnoses
This changed in the 1970s, when the FDA (US regulatory board) could no longer advertise their products for the “stress of life” (common marketing technique)
Needed to prove effectiveness with particular conditions (Concrete, measurable
Third-party health insurance
In the 50’s, most patients paid out of pocket for therapists
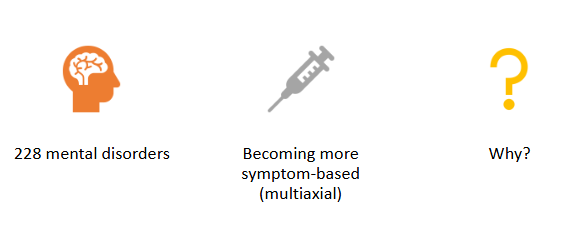
Diagnostic and Statistical manual for mental disorders (DSM-III): 1980
Included explicit diagnostic criteria
Goal: standardized diagnostic reliability (better treatment, randomized clinical trials became easier)
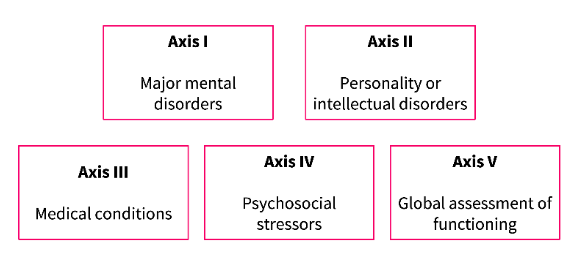
Becoming multiaxial
Multiaxial: a system/method of evaluation, grounded in the biopsychosocial model of assessment that considers multiple factors in mental health diagnoses
Responsible for the shift to biological psychiatry
Medical model
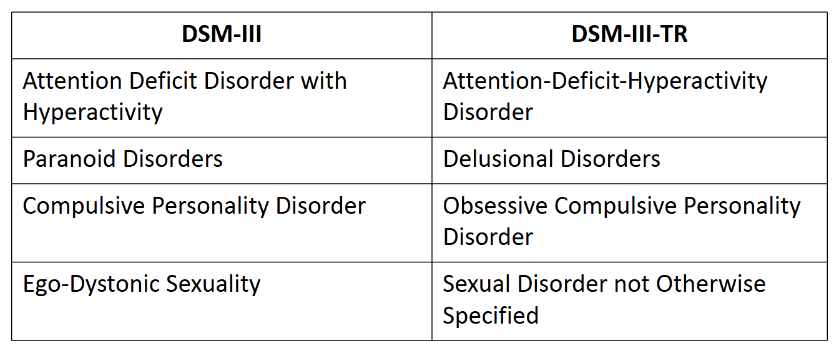
Diagnostic and statistical manual for mental disorders (DSM - III - R): 1987
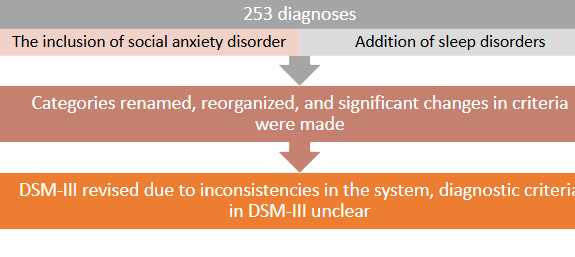
DSM-III to DSM-III-TR
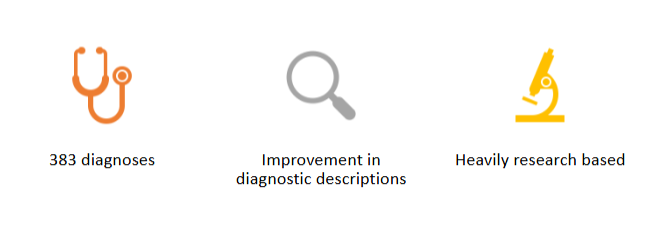
Diagnostic and statistical manual for mental disorders (DSM-IV): 1994
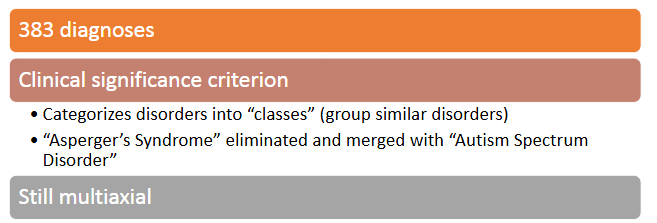
Diagnostic and statistical manual for mental disorders (DSM-IV-TR): 2000
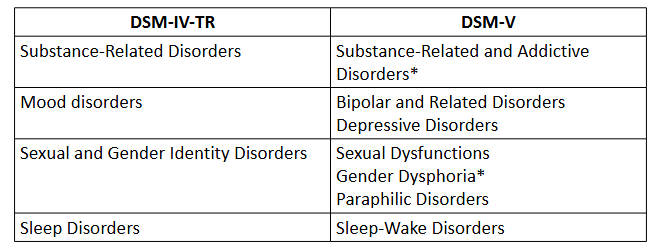
Diagnostic and statistical manual for mental disorders (DSM-V): 2013
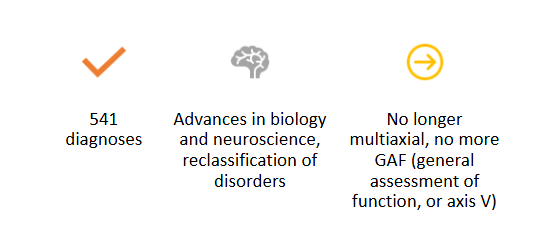
DSM-IV-TR to DSM-V
Diagnostic and statistical manual for mental disorders (DSM-V-TR): 2022
Identified out-of-date information in the DSM-V
Clarified certain diagnostic criteria
Ensured appropriate attention to risk factor (racism, discrimination)
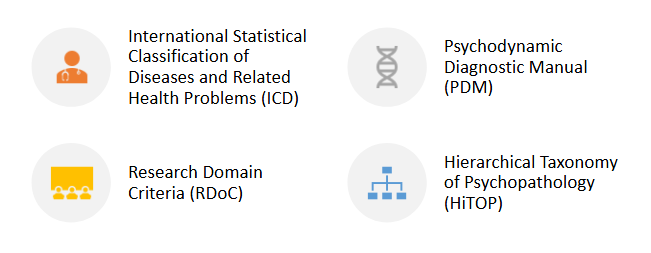
Other diagnositc manuals
Anxiety Disorders
Fear and anxiety are adaptive reactions to threats
Ex. It is typical to be fearful of a hungry lion or anxious about an upcoming exam
Estimated 30% of Canadians experience one pathological anxiety, although only about 5% of people are ever diagnosed.
DSM-5 recognizes 12 types of anxiety disorders:
Generalized Anxiety Disorder (GAD
An anxiety disorder in which worries are not focused on any specific threat - GAD is used as a case study for examining the different parts of the DSM
In the population, levels of anxiety are constant throughout the lifespan - the content of worries changes
Diagnostic Criteria:
Excessive anxiety and worry, occurring more days than not for at least 6 months, about more than one event/stressor
The individual finds it difficult to control the worry
Three or more of these symptoms:
a) Restlessness
b) Fatigue
c) Concentration deficiency
d) Irritability
e) Muscle tension
f) Sleep disturbanceCauses significant distress/affects functioning
Cannot be attributed to substance use or other medical condition
Cannot be better described by another DSM diagnosis
Onset:
Median age for diagnosis is 30, but many patients report having anxiety symptoms for a long time before reporting them
In the population, the level of anxiety is constant throughout life spans
The content of worries changes
Prognosis: In individuals, the severity of symptoms waxes and wanes across the lifespan (remission is rare)
Phobic Disorders
A more specific type of anxiety disorder (characterized by marked, persistent, excessive fear of specific objects, activities, or situations)
Usually, the person recognizes the irrationality of their fear but can’t control it
Specific phobias: Have 12% prevalence
Animals
Natural environment
Situations
Medical events
Other
Social phobia - maladaptive fear of being publicly humiliated or embarrassed (13% prevalence)
Why are phobic disorders so common? Preparedness Theory
We may be evolutionarily adapted to fear certain types of stimulus
Evidence for this hypothesis comes from conditioning
Monkeys can easily be conditioned to fear snakes, but not flowers
These fears may be overdeveloped in some individuals
Panic Disorder
Sudden occurrence of multiple psychological and physical symptoms typically associated with terror
Shortness of breath
Heart palpitations
Sweating
Dizziness
derealisation (feeling that the world is unreal)Fear of death/”losing one’s mind?
Panic episodes are common (1/3 Canadian experience a panic attack once or more per year)
Diagnosis:
Recurrent, unexpected attacks
Significant fear of another attack
Moods
A sustained emotional state
Emotions
reactions to significant events, involving feelings, physiological changes, and behaviors.
Emotional states:
Long-lasting
Non-specific
Mood disorders
Mental disorders that have mood disturbance as their prominent feature
Manic episode
A distinct period of high energy and increased activity
Depressive Episode
A distinct period of sad mood and loss of interest or pleasure
Depressive Disorders
Present in 22% of the female Canadian population and 14% of the male Canadian population
Due to:
Hormonal differences
Higher diagnoses
Difference in coping strategies (sharing and co-rumination)
About 1 in 12 Canadians will experience major depression in their lives
Major Depressive Disorder/Unipolar Disorder (Most well known)
Severely depressed mood and/or inability to experience pleasure that lasts two or more weeks and is accompanied by feelings of worthlessness, lethargy, sleep disturbance, and/or appetite disturbance
Diagnostic Criteria:
Five or more of the following symptoms in the same 2-week period
Depressed mood
Diminished interest
Significant weight loss/gain
Insomnia or hypersomnia
Psychomotor agitation, retardation (anxiety/restlessness or intellectual disability)
Fatigue
Feelings of worthlessness/guilt
Diminished concentration/decisiveness
Recurrent thoughts of death/suicidal ideation
No evidence of a manic episode
Symptoms cause clinically significant distress/impairment
Not better described by another DSM disorder
Not attributable to another medical condition or physiological effects of substance use
Onset:
It may appear at any age, but is most likely to appear in the 20s
Prognosis:
2/5 of individuals recover within 3 months
4/5 of individuals recover within 1 year
1/5 of individuals do not experience remission
Bipolar Disorders
Mood disorders are not unipolar
Bipolar Disorders are characterized by cycles of abnormal, persistent high mood (mania) and low mood (depression)
→ Bipolar I Disorder - At least one manic episode, possibly with hypomanic and depressive episodes as well
→ Bipolar II Disorder - Presence of both hypomanic and depressive episodes; no manic episodes
Criteria:
1. Distinct period of abnormal, persistently elevated mood; increased activity or energy; lasting at least 1 week (manic episode)
2. 3 or more of the following:
- Inflated self-esteem
- Decreased need for sleep
- Talkative
- Racing thoughts
- Distractibility
- Increase in Goal-Directed Activity or Psychometer Agitation
- Excessive Involvement in Activities with a high potential for painful consequences
3. Symptoms cause clinically significant distress/impairment
4. Not better described by another DSM disorder
5. Not attributable to another medical condition or physiological effects of substance use
Prevalence:
1 in 40 individuals
No differences between women and men (1:1)
Onset:
Mean age of first episode = 18 years
Onset can occur for the first time in the 60s or 70s
Prognosis:
90% of individuals who experience a manic episode will experience more of them throughout life
Full remission is very rare
Risk Factors
Temperamental (particularly neuroticism, or negative affect)
Environmental (childhood experiences, stressful life events)
Biological (neurotransmitter imbalance)
Genetic (family members of individuals with MDD are 2-4 times more likely to be diagnosed with MDD; 40% heritability)
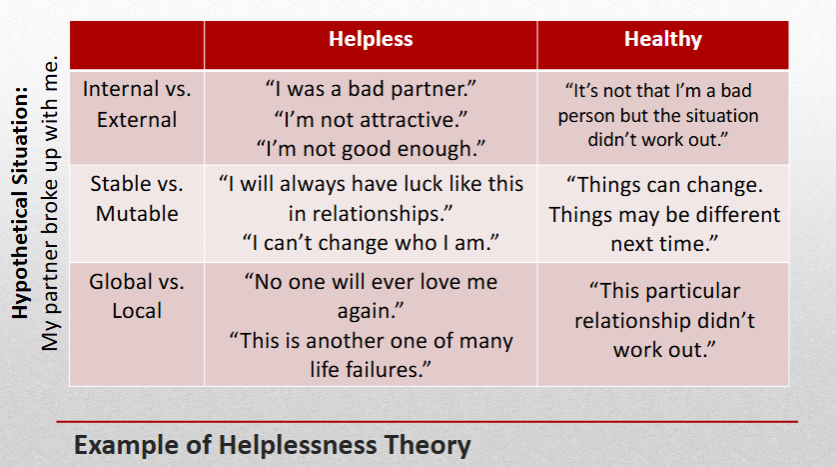
The Helplessness Theory
It argues that the way a person thinks about failure makes them more or less likely to be depressed
Attribute failures to internal characteristics
Believes that failures are permanent (stable)
Believes that failures are global (apply to many areas of life)
Dysthymia or Dysthymic Disorder
Moderate depressive symptoms that last for more than 2 years
When dysthymia is punctuated by an episode of major depression, it is called Double Depression
Obsessions
Recurrent, unwanted, and intrusive thoughts, fears, urges, or images
Ex. Fear of germs
Compulsions
Behaviors in response to obsession
Ex. Repetitive handwashing
Hoarding Disorder
Difficulty getting rid of useless possessions
results in excessive accumulation of items
areas in living space become unusable and hazardous
Trauma
An emotional response to something shocking or dangerous
Stress
A reaction to life demands
Post-traumatic stress disorder (PTSD)
Experiencing or witnessing a traumatic event
Ex. war, natural disasters, and /or violent crime
Addiction
Repeated and compulsive engagement in rewarding activities
disregard for negative, long-term outcomes
addictions can be substance-related or behavioral
Substance use disorder/ Substance induced disorders
Substance-related disorders lead to physiological dependence and tolerence
Gambling Disorder
Repeatedly placing bets to risk some money to gain even more (chasing a feeling of euphoria)
- this is a behavioral addiction
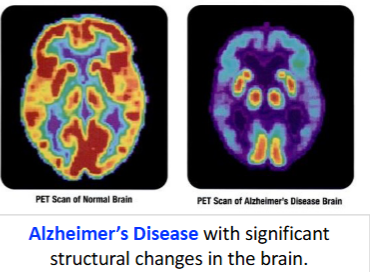
General Neurocognitive Disorders
Neurocognitive disorders are acquired (cognitive deficit was not present at birth)
Attributed to:
Brain injury
Disease
substance/Medication use
General Personality Disorder
Drastically different characteristics, beliefs, and behaviors
3 Categories of behavior:
Cluster A: odd and eccentric
Cluster B: dramatic, emotional, and erratic
Cluster C: anxious and fearful
Borderline Personality Disorder
Instability in interpersonal relationships, self-image, and emotion
Intense emotions that quickly change
Thinking in absolutes of all good or bad