Subjective Assessment
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
68 Terms
Present Complaint
Specific areas
Type, depth, quality and intensity
Is it Intermittent or constant pain?
Easing or aggravating factors?
Abnormal sensations?
24-hour pattern of symptoms.
Physical Limitations.
SIN Factor) Severity-Irritability-Nature
History of Present Complaint
How Long?
Initial cause (do they know)
Have the symptoms changed since?
Relationship of symptoms.
Previous episodes .
Past medical history
Tyroid, Heart, Rheumatoid arthritis, Epilepsy, Asthma, Diabetes, Steroids
Recent X-rays or investigations
Unexplained weight loss
Fainting, dizziness, visual disturbances
Cauda equina symptoms
Other relevant previous/existing conditions?
Potential treatment contraindications?
Drug History
Dosage & frequency.
Perceived effect.
Any meds for a different condition?
When was the prescription started?
Dosage & frequency.
Any Side effects?
Social History
Age & gender.
Home situation.
Dependents.
Occupation – Specific duties.
Leisure activities.
Functional limitations/activities to return to.
Goals- where do they want to get back to
SALTAPS
See - See the mechanism of the injury
Ask - Consent & find out what happened via the athlete. What they felt/feel, pain and symptoms.
Look - Appearance of the injury. Bleeding, Swelling, Bruisin,g Discolouration, Bone/joint deformity
Touch - Palpate the injury gently. Note the patient’s responses.
Active ROM - Assess active movement ofthe injured
site. Can they move the area through full ROM - Pain free?
Passive ROM - If Active ROM is Ok, assess passively. Can the joint be moved (Via therapist
input) full range?
Strength - Can the patient apply force & move against resistance? Walk or stand unaided. Progress to functional tests - like running.
Cryotherapy
Commonly used to manage acute soft tissue injuries
Management of acute injuries / Recovery from exercise
Cooling of tissues
Reduce to 10 – 15 °C
Cryotherapy applications
Ice: Chips / Crushed / Wetted
Ice baths / immersion
Gel packs
Ice Massage
Cold sprays
Cryo cuffs
Contrast bathing
Phase Change Material
Cryotherapy Chambers
Cryotherapy Contradictions and cautions
Excessive local cooling (ice burn)
Conditions altering cold sensitivity
Raynauds phenomenon /cold urticaria / cryoglobinaemia
Sensory deficits
Cardiac disease
High (or low) blood pressure
Psychological associations with cold
NEVER APPLY ICE DIRECTLY
TO THE SKIN
CHECK PATIENT’S SKIN REGULARLY
Cryotherapy protocols
Treatment explained and contraindications checked
Patient is comfortable with the treatment area appropriately exposed & well supported
Dry towel (& plastic sheet) under the treatment area
Prepare ice pack: a bag of ice wrapped in a damp towel
Apply ice pack to area & secure with a dry towel
Check patient comfort & skin every 3 - 5 mins
If there are any concerns, stop treatment immediately
Cryotherapy: Cryo cuffs
Ice application with compression
Specialised equipment
• Gravity device
• Electric pump
Different cuffs for different areas

Cryotherapy: Instructions
Prepare cooler: Fill to line with water
Add ice to the top
Position EMPTY cuff with straps (not too tightly)
Attach pipe and open valve using gravity to fill the cuff
Close valve & detach pipe
Complete Treatment
Empty cuff before removing:
Connect tube and open valve to cooler
Position cooler below the cuff (i.e. use gravity)
Clean cuff between uses
Superficial Heat application
Clay hot packs
Wheat bags / Gel packs
Paraffin wax
Warm water immersion (whirlpool / hydrotherapy)
Heat sprays / gels
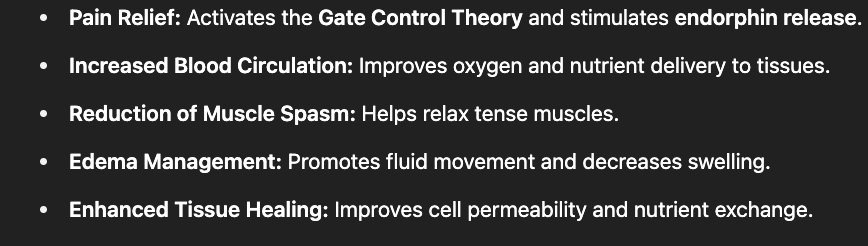
Superficial Heat Therapeutic effects
Tissue Healing
Pain Relief
Sedative Effect
Increased Joint RoM
Superficial Heat Physiological effects
Metabolic activity increased
Increased blood flow & tissue fluid exchange
Stimulation of sensory nerves
Immediate skin arteriole vasodilation
Softening of collagen
Fluid viscosity reduced
Superficial Heat Contraindications & Precaution
Skin checks required (test tubes)
Patients with:
Cognitive impairment (e.g. dementia)
Circulatory insufficiencies (e.g. DVT, peripheral vascular disease)
Treatment should not be applied over:
Areas of malignancy
Active bleeding sites
Active epiphysis plates
Metal implants
Eyes
Superficial Heat Practical Applications
2 x towels
1 x appropriately sized hot pack
Preparation table
Towels folded in half lengthways
Towels laid over each other at 90°
Clay pack placed in centre of the ‘cross’
Towels folded in (bottom towel first
Hot pack wrapped in towels placed on pt
8 towel layers between pt andhot pack
i.e. ‘folded in’ side against pt skin
Proposed Mechanisms for Effects of US
Stable Cavitation: tiny gas bubbles formed by the dissolving of gas in the
medium enabling acoustic streamingAcoustic Streaming: circulatory flow, eddying of fluids near vibrating
structure i.e. cell membrane or gas bubbles – causes increase in cell
membrane permeability potentially enhancing healing processMicromassage: Oscillatory movement of tissue (Compression and
Rarefaction) is proposed to have an effect but there is less evidence
Ultrasound Contraindication
Uterus during pregnancy
Malignant tissue
Open wounds / bleeding tissues
Significant vascular abnormalities
(e.g. DVT, emboli, arteriosclerosis / atherosclerosis)Haemophillia (not covered by factor replacement)
Application over: active epiphyses in children / eyes / stellate ganglion/heart with
pacemaker or heart in advanced heart disease/genitals / metal implants
CAUTIONS
Always use the lowest therapeutic intensity/dosage
Always keep the applicator moving throughout treatment
How does Ultrasound work?
The transducer probe generates and receives sound waves using a principle called the Piezoelectric Effect (ability of certain materials to generate an electric charge)
Ultrasound concepts and terma
Attenuation: Reflection, Refraction and Absorption
BNR: Variability of beam intensity (lower = better)
Effective Radiating Area: Area of US head producing US
Frequency
This determines depth of penetration
Increased frequency = increased absorbency
1 MHz = Deep
2 to 5cm depth
3 MHz = Superficial
Up to 2cm depth
Intensity
This is the rate at which energy is being is being delivered to the tissue
Measured in Watts per cm2 (W/cm2)
Always use the lowest dose to achieve the desired therapeutic effect
Pulse ratio
Ratio of ultrasound machine producing US and rest periods in between
Expressed as a percentage or a ratio
time on : time off e.g. 1:4 or 20%
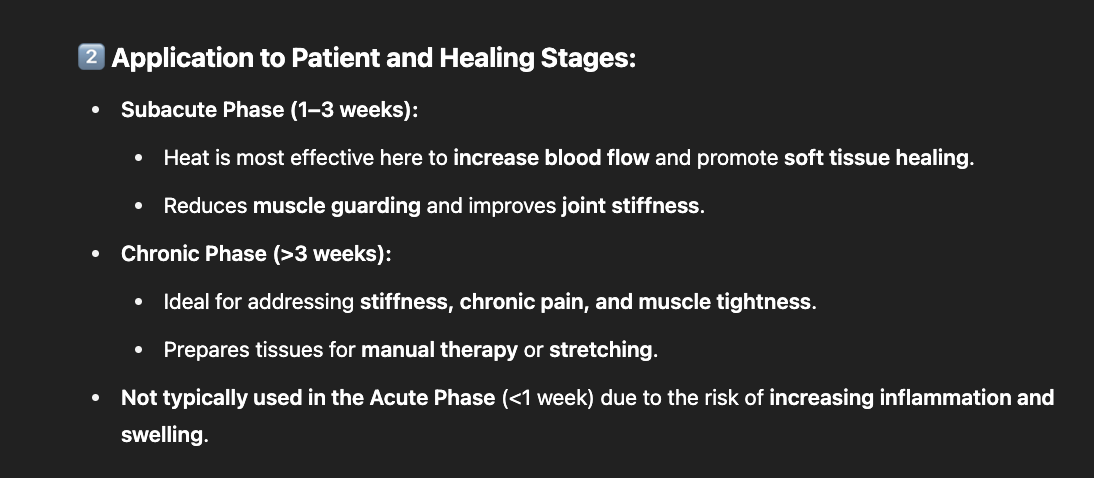
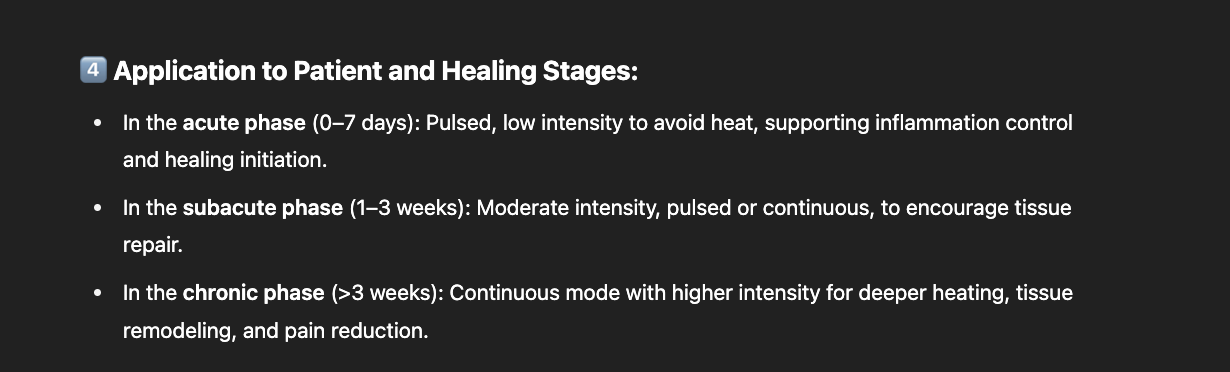
Treatment parameters
Lesion depth:
1Mhz = Deep (2 - 5cm)
3Mhz = Superficial (< 2cm)Pulse Ratios:
Acute 20 – 25%
Sub-Acute 25 – 50%
Chronic 50 – 100%Intensity:
Acute 0.1 – 0.3 w/cm2
Sub-Acute 0.2 – 0.5 w/cm2
Chronic 0.3 – 0.8 w/cm2
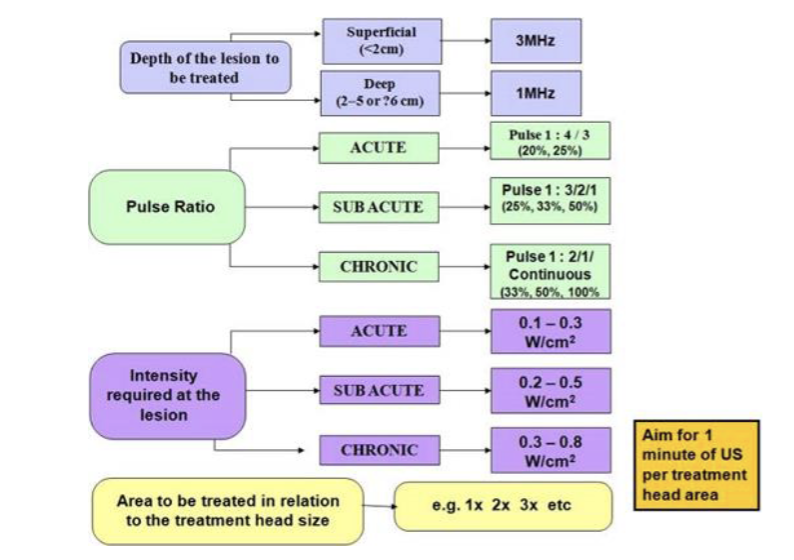
Treatment time calculation
Select a treatment head applicator appropriate to size of area
(e.g. 1cm, 2cm, 5cm)How big is the treatment are compared to the size of the applicator (e.g. x1, x2, x3)
Calculate your pulse factor (add pulse ratio numbers together)
(e.g. a 1:4 ratio would be 1 + 4 = 5)Number of heads x pulse factor x 1 min = total minutes
(e.g. 2 heads area at 1:4 ratio = 2 x 5 x 1 = 10 mins treatment)
Ultrasound protocol
Treatment explanation & contraindication check
Treatment consent gained from patient
Hot & cold sensory check (test tubes)
Applicator size selected
Treatment parameters selected (lowest therapeutic dose)
Time calculated (pulse factor x applicator heads on area)
Coupling gel applied to applicator
Applicator applied to skin and movement started
Remind Pt they must inform you if they feel abnormal
sensations during treatment (e.g. warming of tissues)
Treatment commences (applicator moved continuously)
Treatment completes applicator and skin wiped clean
Post treatment observations and patient subjective
Treatment parameters & details recorded in patients notes
Clinical Indications
Pain Relief (pain gate / opioid mechanism)
Muscle Stimulation (twitch to tetanic)
Increase Local Blood Flow
Reduce Oedema
IFT Principles
Low frequency current offers potential
therapeutic effects2 x medium carrier frequencies
Carrier Frequency
This is the medium frequency current applied to the body
Amplitude Modulated / Beat
The frequency created via the out of sync carrier frequencies
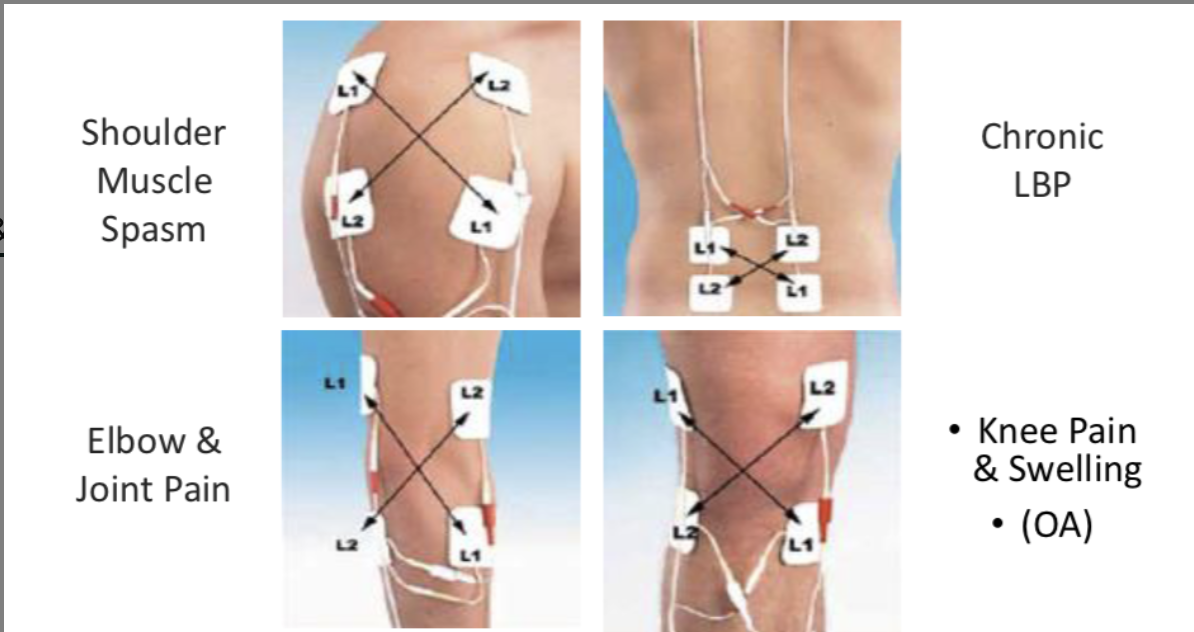
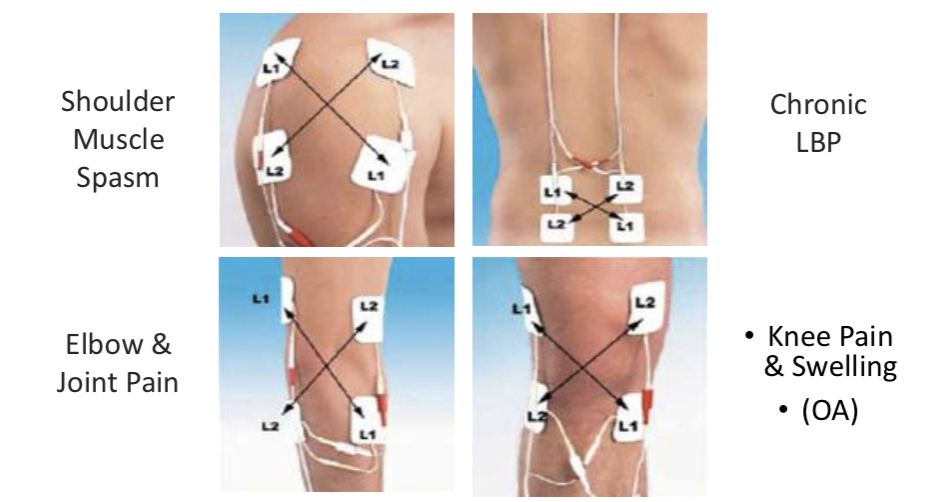
IFT Electrodes & Area of Stimulation
Bipolar electrodes (2).
Quadripolar electrodes (4)
Co-planar
Contra-planar
Disposable / Single use
Suction / Vacuum
Reusable pads
IFT Treatment Parameters
Bipolar / Quadripolar (2 or 4 electrodes)
Electrode Type (pads, suction, disposable)
Carrier Frequency (1kHz – 10kHz)
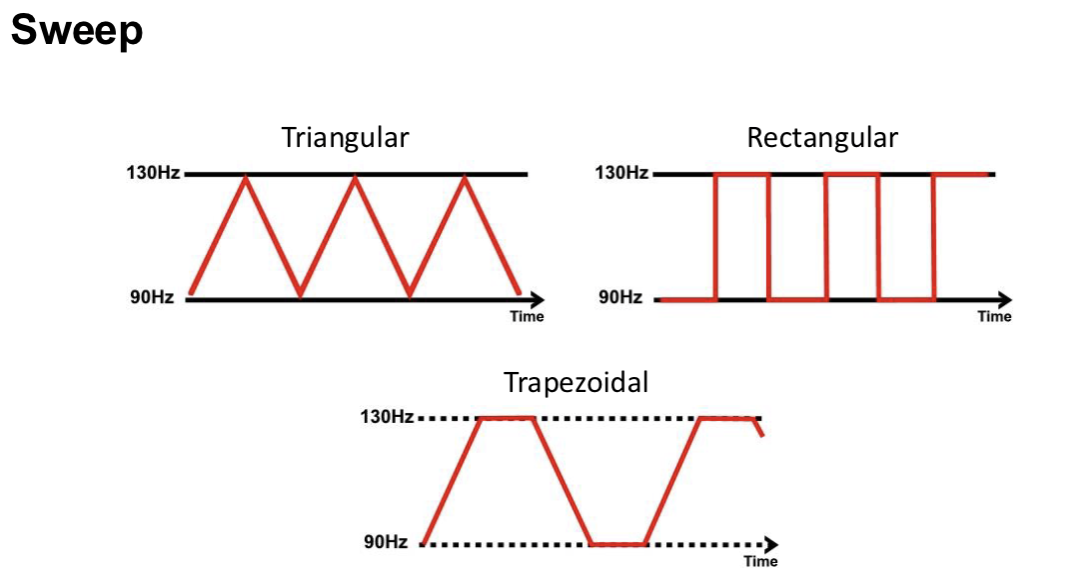
Beat Frequency / AMF (sweep / constant, 0 – 150Hz)
Sweep Mode (rise and fall of beat frequency)
Surge Mode (rise and fall of intensity)
Intensity (strong but comfortable)
Treatment Time (acute / chronic)
Treatment Time (acute / chronic)
Total treatment time usually 15-20 mins
(This may be constructed of different modes)
Acute = Shorter treatment times - 5-10 mins
IFT Beat Frequency
Muscle stimulation 10 - 20Hz (sweep)
Pain Gate 100 - 130Hz (constant)
Promote Healing 25 - 50Hz (sweep)
Reduce Swelling 10 - 100Hz (sweep)
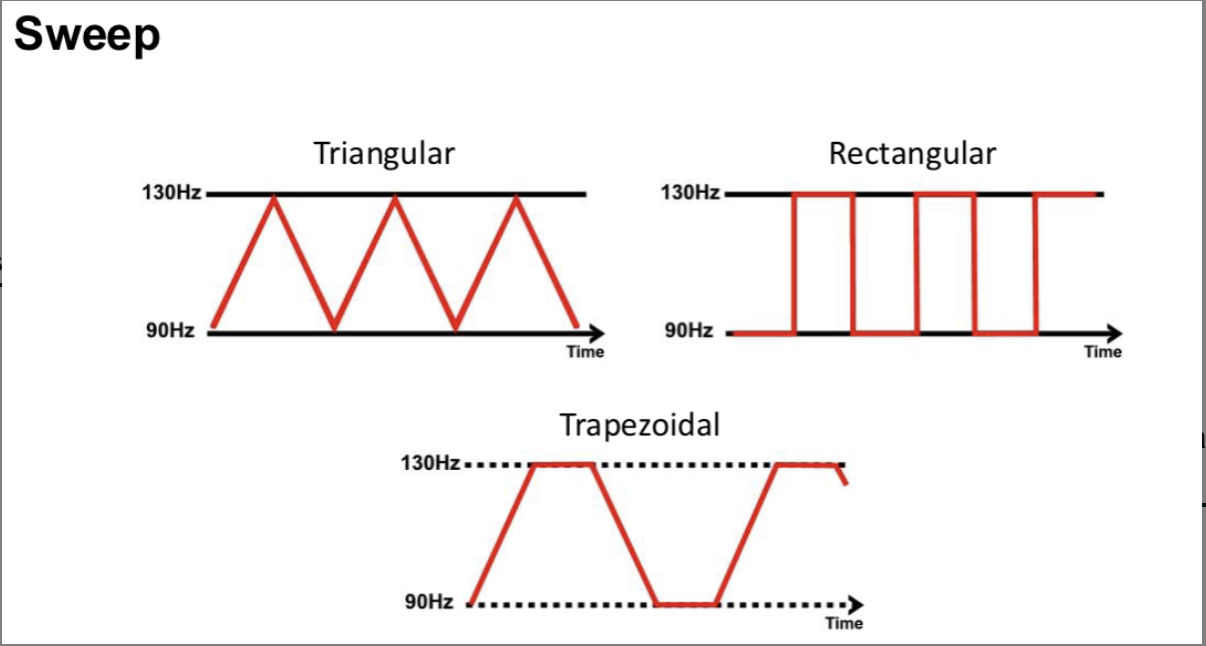
IFT Constant and sweep cycles
Constant – frequency stays the same
Body may begin to accommodate
Sweep – Freq changes gradually
Attempt to reduce the accommodation
Wide sweeps seen to be ineffective & may be counterproductive
IFT Treatment Protocol
Contraindications & skin sensation check (sharp / blunt)
Treatment explanation and pt consent
Ensure patient comfort and appropriate positioning
Electrodes placed & secured around treatment area (sponges must be damp)
Input IFT treatment settings
Begin treatment and slowly turn up intensity to be ‘strong but comfortable’
After a few mins the intensity can be increased a little (only do this once)
Complete treatment time
Remove pads and check treatment area (observations)
Record pt subjective feedback & observations and full treatment settings
IFT Contraindications
Pacemaker
Advanced cardiovascular conditions
Epilepsy
Active / suspected malignancy
Patients who cannot comprehend Rx
Anticoagulation therapy / history of embolism
Do not place pads over:
Trunk / pelvis during pregnancy
Carotid sinus & Anterior neck region
Areas of reduced/altered sensation or circulation
Dermatological lesions e.g. dermatitis
Over metal implants
Bleeding tissues
Close to the eyes or in mouth
Varicose veins
Anterior chest wall
Over a joint replacement
Treatment Record
Treatment area and aim of treatment
Number of electrodes
Placement of electrodes
Frequency applied & sweep
Treatment Intensity (& / or pt subjective feedback)
Treatment duration
What is TENS
Electrical stimulation of nerves
Used for pain relief
TENS Theoretical Principles
Reduce pain through stimulation of sensory nerves
Proposed to relieve pain through:
Pain gate mechanism (A Beta fibres)
Opioid system stimulation (A Delta fibres)
Good evidence to suggest provides pain relief
What is TENS used for
Regularly used in practice for chronic pain
Research also supports use for acute p
Patients are encouraged to explore the settings
(within boundaries & guidance)
TENS Contraindications
Cancer
Pregnancy
Pacemaker
Metal implants
Epilepsy
Do not place the pads:
Over a pregnant uterus (womb)
Carotid sinus (Anterior neck) region
Areas of reduced or altered sensation
On dermatological lesions e.g. dermatitis
TENS Directins step by step
Test the machine by holding the pads between your fingers &
carefully increase the intensity to feel a tingling sensation
Check contraindications & complete skin sensation test completed before application
Area of skin where electrodes are to be placed must be clean. No cuts, grazes or skin irritation
Place the pads around the area of pain at least an inch apart (e.g. above and below)
Select treatment parameters (see other slides)
Switch the machine on slowly & turn up gradually until patient feels strong but comfortable
sensation
After a few mins the sensation will reduce slightly (accommodation) at this point turn the machine
up slightly
Do not turn the machine up too high as can cause over stimulation which may increase pain
There should be NO muscle contraction
Hi TENS Treatment Settings
High Frequency 80 – 130 hz (or pps)
Stimulates A-beta fibers, blocks pain signals through the Gate Control Theory.
Narrow pulse width ~ 100 micro seconds
30 minutes +
shorter pulse width for superficial pain relief).
Good acute pain relief
Lo TENS Treatment Settings
Lower frequency 2 – 5 hz
Targets A-delta fibers, stimulates endorphin release for long-lasting relief.
Longer pulses 200 – 250 micro seconds
Longer pulse width for deeper tissues
For chronic pain and deeper tissue relief.
Brief Intense TENS Settings
Aims to provide quicker pain relief
High pulse frequency (90 – 130 Hz)
High pulse width (200 micro sec +)
15 – 30 mins
Burst Mode TENS Settings
raditional / Hi TENS settings
…but with burst mode so current is interrupted
2 – 3 burst per second
Intensity can be slightly higher than Hi TENS (but lower than brief)
Please explain the therapeutic effects of ultrasound?
How do these relate to our patient and the stages
of healing?
Non-Thermal Effects: (Pulsed Mode)
Enhances cell membrane permeability
Stimulates tissue repair and protein synthesis
Reduces inflammation
Promotes angiogenesis and wound healing
How would you explain the US treatment to a patient?
I’m going to use an ultrasound device to help reduce pain and improve healing in your [injured area]. This will send sound waves into the tissue, promoting blood flow and cellular repair. You might feel a gentle warmth or nothing at all, but it’s working to speed up your recovery. I’ll keep the device moving to make sure it’s comfortable and effective.
What should the patient feel during the US treatment?
hermal Mode: Mild warmth, comfortable sensation.
Non-Thermal Mode: Likely nothing noticeable; sometimes a slight tingling.
Abnormal Sensation: Sharp pain, burning, or discomfort should be reported immediately.
How would you explain the TENS treatment to a patient?
I’m going to use a TENS device, which sends small electrical impulses to your skin. These impulses block pain signals from reaching your brain and help your body release natural painkillers. You might feel a gentle tingling or pulsing sensation, and I’ll adjust it to keep it comfortable. The goal is to reduce your pain so you can move more easil
What should the patient feel during the TENS treatment?
Conventional TENS: A mild tingling or buzzing sensation—should not be uncomfortable.
Low-Frequency TENS: A stronger pulse with muscle twitching, but still comfortable.
Burst Mode: More intense, rhythmic pulses—strong but not painful.
Please explain the therapeutic effects of Cryotherapy?
Vasoconstriction: Reduces blood flow, minimizing swelling and edema.
Decreased Metabolic Rate: Slows cellular metabolism, reducing tissue damage and oxygen demand.
Reduced Nerve Conduction Velocity: Slows down nerve signals, leading to pain relief.
Muscle Spasm Reduction: Lowers muscle spindle activity, decreasing spasticity.
Anti-Inflammatory Effects: Limits the release of inflammatory mediators.
What would you expect to see post cryo treatment?
Decreased Swelling: Observable reduction in localized edema.
Reduced Pain and Spasm: Patient reports less pain and muscle tension.
Improved Range of Motion: Less stiffness, easier joint movement.
Possible Temporary Numbness: Reduced sensation in the treated area for a short time.
How long would you apply the CRYO treatment for?
Typical Application: 10–20 minutes, depending on the thickness of the tissue and depth of the injury.
For superficial areas (like fingers or toes): 10–15 minutes.
For deeper muscles or joints: 15–20 minutes.
Should be applied every 2–3 hours during the acute phase of injury
How would you explain the CRYO treatment to the patient
I’m going to apply a cold pack to your [injured area] to help reduce swelling and numb the pain. You might feel it go through stages: cold, burning, aching, and then numbness. It’s important for the cold to reach the deeper tissues to be effective, but I’ll make sure it’s comfortable for you. Let me know if it gets too intense."
What Should the Patient Feel During CRYO Treatment?
Cold Sensation: Immediate feeling of coolness.
Burning or Aching: After 2–3 minutes, a deep ache or burning sensation.
Numbness: After 5–7 minutes, the area should feel comfortably numb.
If pain or discomfort increases instead of decreasing, the treatment should be stoppe
Expected outcome of post SH treatment
creased Range of Motion: Muscles and connective tissues are more flexible.
Reduced Pain and Stiffness: Patients report feeling looser and more comfortable.
Improved Circulation: Area may look red and warm due to increased blood flow.
Reduced Muscle Spasm: Less tightness in the affected area.
How long should SH be applied for
15–20 minutes is typical for moist heat packs, heating pads, or warm water immersion.
This duration is sufficient to achieve therapeutic tissue temperatures (104°F–113°F or 40°C–45°C).
Should be applied 2–3 times daily depending on patient tolerance and clinical goals.
How would you explain the SH treatment to the patient
I’m going to apply some gentle heat to your [affected area] to help relax the muscles, reduce stiffness, and improve blood flow. This will make it easier for you to move and reduce your discomfort. You should feel a warm, soothing sensation—not too hot. Let me know if it gets uncomfortable."
How should PT feel during SH treatment
Comfortable Warmth: A gentle, soothing heat sensation.
Mild Muscle Relaxation: A feeling of loosening in the targeted area.
No Pain or Burning: If it becomes too hot or uncomfortable, the application should be stopped immediately.
Reccommended IFT settings
IFT Treatment Duration
Explaining the IFT Treatment to the Patient
I’m going to apply some small electrical currents to your [injured area] using four pads. These currents work together to block pain and promote healing. You might feel a gentle tingling or pulsing sensation—it should be comfortable, not painful. We’ll adjust it to your comfort level and let it work for about 15–20 minutes."
What should PT feel during IFT sensation
Tingling or Pulsing Sensation: A comfortable, rhythmic feeling under the pads.
Mild Muscle Twitching: Sometimes noticeable, especially at lower frequencies.
No Pain or Burning: If it becomes sharp or painful, the intensity should be adjusted.
herapeutic Effects of Interferential Therapy: