Exam 1- IRA 1-3 Skin and Cardio
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
Please complete the table below.
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
IV isotonic saline (NaCl) | increase | increase | no change | no change |
Diarrhea (isotonic loss) | decrease | decrease | no change | no change |
Excessive NaCl intake (without drinking any water) | no change | ? | ? | ? |
A.
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
Excessive NaCl intake (without drinking any water) | no change | increase | decrease | increase |
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
Excessive NaCl intake (without drinking any water) | no change | decrease | decrease | decrease |
C.
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
Excessive NaCl intake (without drinking any water) | no change | decrease | decrease | increase |
D.
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
Excessive NaCl intake (without drinking any water) | no change | increase | increase | increase |
E.
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
Excessive NaCl intake (without drinking any water) | no change | decrease | increase | increase |
A.
Condition | Total Body Water | ECF Volume | ICF Volume | ECF Osmolarity |
Excessive NaCl intake (without drinking any water) | no change | increase | decrease | increase |
How does facilitated diffusion differ from active transport?
A. Active transport uses ATP, while facilitated diffusion does not.
B. Active transport uses a transporter protein, while facilitated diffusion does not.
C. Active transport exhibits chemical specificity, while facilitated diffusion does not.
D. Active transport exhibits saturation, while facilitated diffusion does not.
E. Active transport uses aquaporin channels, while facilitated diffusion does not.
A. Active transport uses ATP, while facilitated diffusion does not.
Which of the following statements regarding the distribution of water in the body is most accurate?
A. Approximately 2/3 of the total body water is in the interstitial fluid (ISF).
B. Approximately 3/4 of the total body water is in the extracellular fluid (ECF).
C. Approximately 2/3 of the total body water is in the intracellular fluid (ICF).
D. Approximately 1/12 of the total body water is in the interstitial fluid (ISF).
E. Approximately 1/3 of the total body water is in the intravascular fluid (IVF).
C. Approximately 2/3 of the total body water is in the intracellular fluid (ICF).
In what way does cardiac muscle differ from skeletal muscle?
A. The regulation of contraction in cardiac muscle is mediated by the thick filaments.
B. The regulation of contraction in cardiac muscle is mediated by the thin filaments.
C. Contraction in cardiac muscle is dependent on Ca++ release from internal stores (sarcoplasmic reticulum, or SR).
D. The refractory period of cardiac muscle is almost the same length of time as its action potential.
E. The absolute refractory period during which voltage-gated Na+ channels remain inactivated is much shorter in cardiac muscle.
D. The refractory period of cardiac muscle is almost the same length of time as its action potential.
5. What are the structures indicated on by the black arrows on the following histological images? (these are the same image at different magnifications)
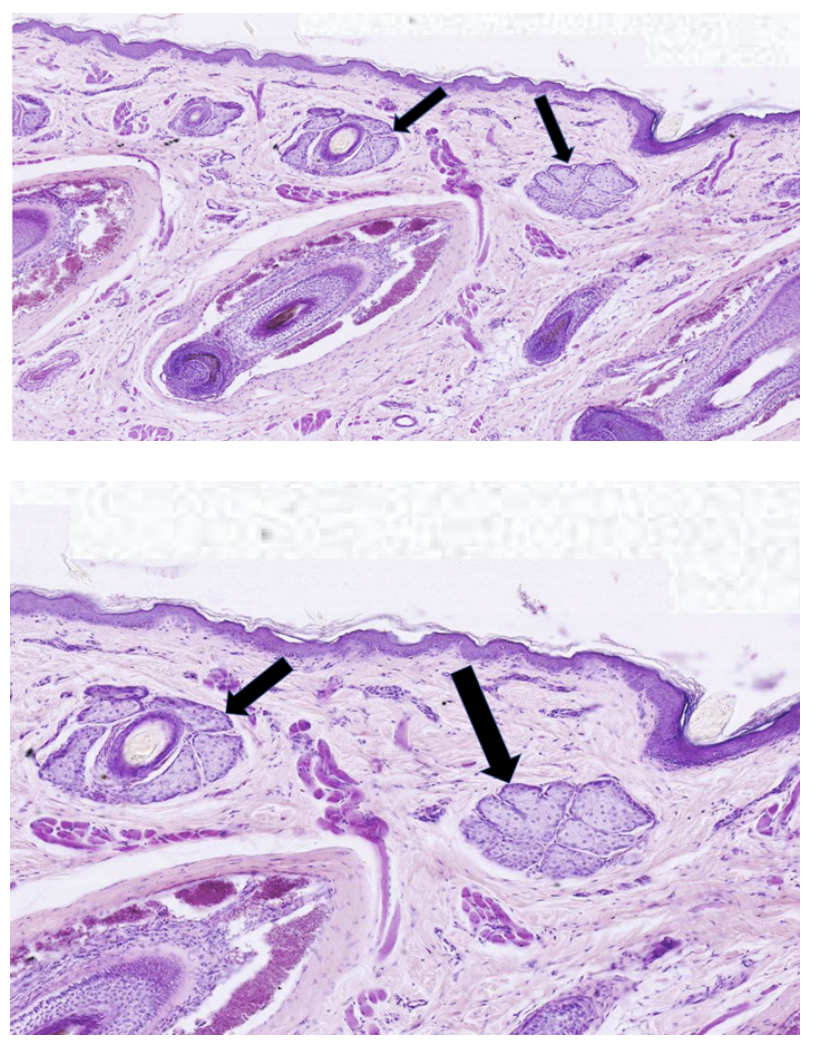
A. eccrine sweat glands
B. free nerve endings
C. hair follicle roots
D. sebaceous glands
E. apocrine sweat glands
D. sebaceous glands
What are structures prominently featured in this micrograph?
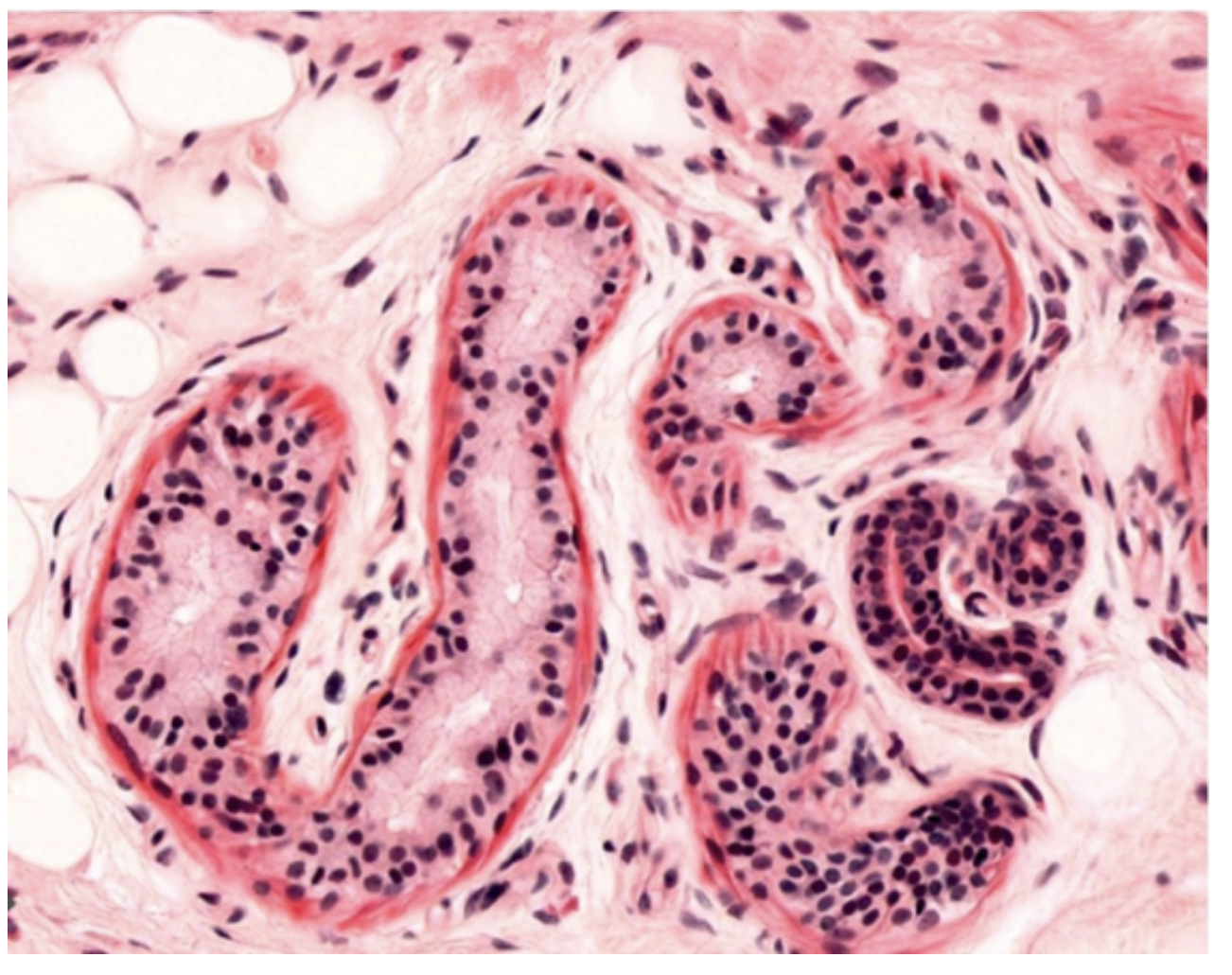
A. Eccrine sweat glands and ducts
B. Pacinian corpuscles
C. Meissner’s corpuscles
D. Apocrine sweat glands and ducts
E. Sebaceous glands and ducts
A. Eccrine sweat glands and ducts
Which of the following statements regarding INTERcellular signaling is most accurate?
A. Neurotransmitters typically signal via very high affinity receptors.
B. All peptide hormones require carrier proteins for transport to target cells.
C. Most hormones are ACTIVE when bound to their carrier proteins.
D. Steroid hormones are packaged in vesicles that are released via regulated secretion.
E. Steroid hormones typically bind cytosolic or nuclear receptors that directly regulate DNA transcription.
E. Steroid hormones typically bind cytosolic or nuclear receptors that directly regulate DNA transcription.
Which of the labeled cells synthesizes and secretes melanin?
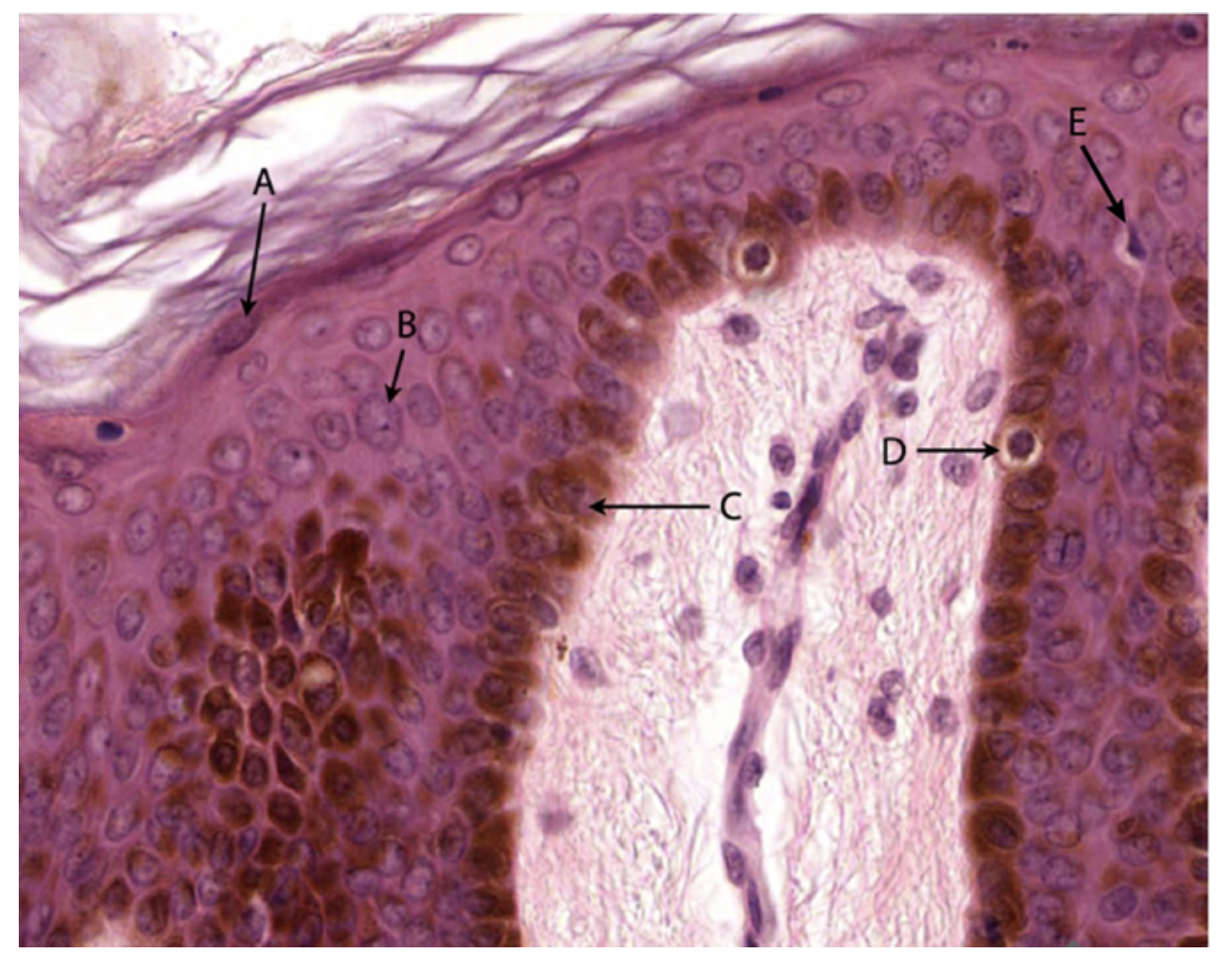
A. A
B. B
C. C
D. D
E. E
D. D
Patients experiencing dehydration often exhibit increased activation of their sympathetic nervous system. Which of the following is a symptom you would expect to see?
A. increased heart rate
B. excessive salivation
C. increased bowel sounds
D. decreased sweating
E. constricted pupils
A. increased heart rate
When does gastrulation occur in the human embryo?
A. during the 3rd week (i.e., days 14-21) following conception.
B. before implantation.
C. before formation of the yolk sac.
D. after generation of the somites.
E. after neural tube closure.
A. during the 3rd week (i.e., days 14-21) following conception.
11. Signaling by acetylcholine via MUSCARINIC receptors occurs at which synaptic junctions?
A. Post-ganglionic parasympathetic neurons on end-organs.
B. Post-ganglionic sympathetic neurons on end-organs.
C. Motor neurons on skeletal muscle.
D. Pre-ganglionic parasympathetic neurons on post-ganglionic parasympathetic neurons.
E. Pre-ganglionic sympathetic neurons on post-ganglionic sympathetic neurons.
A. Post-ganglionic parasympathetic neurons on end-organs.
12. Which of the following structures produces amniotic fluid?
A. yolk sac.
B. fetal kidneys.
C. placenta.
D. fetal heart.
E. maternal kidneys.
B. fetal kidneys.
13. Which of the following is derived from ECTODERM?
A. Stratified squamous epithelial lining of the esophagus
B. Heart
C. Placenta
D. Spinal cord
E. Nephrons of the kidneys
D. Spinal cord
The itching, redness, and swelling characteristic of dermatitis is caused by vasodilation and increased blood vessel permeability in the affected area. What region of the skin would be most responsible for these effects? (i.e. Where do you find the highest concentration of capillaries?)
A. stratum basale
B. dermal papillae
C. stratum corneum
D. hypodermis
E. epidermal ridges
B. dermal papillae
15. Medications best suited to be applied topically (via an ointment or cream) are usually hydrophobic. Which of the following statements best describes why that would be the case?
A. Hydrophobic drugs would also act as emollients to calm skin irritation.
B. Hydrophobic molecules are always small, which makes them easy to mix into a cream.
C. Hydrophobic molecules have a longer shelf-life than hydrophilic molecules.
D. The skin’s keratinized epithelium is water resistant, so hydrophilic drugs would not be able to pass the epithelial barrier.
E. Hydrophobic molecules can freely enter the nuclei of the stratum corneum, allowing for quick drug delivery.
D. The skin’s keratinized epithelium is water resistant, so hydrophilic drugs would not be able to pass the epithelial barrier.
1. You are working for a pharmaceutical company testing if a new birth control medication causes any developmental defects. Your experiments in rats show the medication causes a specific heart defect. Further investigation of the mechanism reveals that the medication does not affect the development of the outflow tract or the AV tissue cushions. However, growth of the heart is arrested. What defect does this medication MOST LIKELY cause?
A. Tetralogy of Fallot
B. Double inlet left ventricle
C. Truncus arteriosus
D. Transposition of the great vessels
E. Persistent A-V canal
B. Double inlet left ventricle
2. During heart development, the septum primum and septum secundum create the division between which two structures?
A. the inferior vena cava and the superior vena cava
B. left and right atrioventricular canals
C. left and right atria
D. left and right ventricles
E. aorta and pulmonary trunk
C. left and right atria
What type of vessel is indicated by the black arrow?
A. capillary
B. arteriole
C. muscular (medium) artery
D. venule
E. medium vein
D. venule
4. During gestation, the fetus receives oxygenated blood from placental circulation and delivers that blood directly into the systemic circuit, bypassing the pulmonary circuit. Which of the following statements best describes the process of bypassing the pulmonary circuit?
A. Oxygenated blood is received by the right atrium from the inferior vena cava, moves into the right ventricles and is then shunted into the left ventricle via the foramen ovale.
B. Oxygenated blood is received by the left ventricle from the pulmonary vein.
C. Oxygenated blood is received by the right atrium from the inferior vena cava, moves into the right ventricle, is pumped into the pulmonary artery, and is then diverted into the aorta via the foramen ovale.
D. Oxygenated blood is received by the right atrium from the inferior vena cava and is then shunted into the left atrium via the foramen ovale.
E. Oxygenated blood is received by the right atrium from the inferior vena cava and is then shunted into the left atrium via the ductus arteriosus.
D. Oxygenated blood is received by the right atrium from the inferior vena cava and is then shunted into the left atrium via the foramen ovale.
5. If there is a malformation of heart valves, it usually affects one or both of the semilunar valves (pulmonary and aortic) OR one or both of the AV valves (bicuspid and tricuspid), but not both semilunar and AV valves. Why might this be the case?
A. The semilunar valves develop days later than the AV valves.
B. The semilunar valves are derived from neural crest tissue and the AV valves are derived from endogenous (mesodermal) heart tissue.
C. Semilunar valve formation is retinoic acid dependent, but AV valve formation is not.
D. The structure of the semilunar valves requires attachment to chordae tendinae, which requires a specific developmental step that is easily perturbed.
E. It is actually equally for a patient to have valve defects in one semilunar and one AV valve as it is to have defects in both semilunar or both AV valves.
B. The semilunar valves are derived from neural crest tissue and the AV valves are derived from endogenous (mesodermal) heart tissue.
The entire venous system develops from three paired veins of the embryo. Which of the following statements is correct regarding this development?
A. Because these embryonic veins are paired and symmetrical, they give rise to the symmetrical venous system that we see in adults.
B. The umbilical veins originally associate with the placenta, and the right umbilical vein completely regresses into a ligament while the left umbilical vein remains open in the adult as the ductus venosus of the liver.
C. The vitelline veins originally associate with the yolk sac, and the right vitelline vein eventually gives rise to the hepatic portal system.
D. The cardinal veins give rise to all of the veins of the body, but not to the veins draining blood from the brain.
E. The patterning of these three paired veins into the adult venous system is highly regulated and does not normally allow for variation between individuals.
C. The vitelline veins originally associate with the yolk sac, and the right vitelline vein eventually gives rise to the hepatic portal system.
Which of the following regions highlights the myocardium of the ventricle?
https://www.digitalscope.org/ViewerUI/?SlideId=ec07dcf4-f848-4b68-9aea-f9e607fbbeac&ann=111000011
A. A
B. B
C. C
D. D
E. E
E. E
Where in the heart should you look to find Purkinje fibers?
A. In the endocardium.
B. In the myocardium, near the junction with the epicardium.
C. In the epicardium.
D. In the myocardium, near the junction with the endocardium.
E. In the middle of the myocardium, generally equidistant to the endocardium and the epicardium.
A. In the endocardium.
Because the brachial artery is considered a muscular artery, all of the following statements are true of the brachial artery except for one. Please identify the FALSE statement.
A. The brachial artery is lined with a simple squamous endothelium.
B. The brachial artery has a relatively thick tunica adventitia, compared to other types of arteries.
C. The brachial artery has many fenestrated sheets of elastic fibers spread throughout its tunica media.
D. The smooth muscle in the tunica media of the brachial artery is capable of causing diameter changes to the vessel.
E. The brachial artery, like all muscular arteries, is a major site of blood pressure regulation.
C. The brachial artery has many fenestrated sheets of elastic fibers spread throughout its tunica media.
Which structure(s) is found in the atria of the heart?
A. trabeculae carnae
B. papillary muscles
C. chordae tendinae
D. SA node
E. the bundle of His
D. SA node
Remember when you could go to a gym and see 10 people running on a treadmill? Those runners were experiencing an increase in venous return (assuming normal heart function). What is the result of this increase?
A. a decrease in cardiac output
B. a decrease in end diastolic volume
C. an increase in end systolic volume
D. decreased release of atrial natriuretic peptide
E. an increase in stroke volume
E. an increase in stroke volume
2. Which of the following enhances stroke volume?
A. increased parasympathetic stimulation to the heart
B. increased end systolic volume in the ventricle
C. increased end diastolic volume in the ventricle
D. decreased epinephrine level in the plasma
E. ALL of the above will enhance stroke volume
C. increased end diastolic volume in the ventricle
3. Per the ACC/AHA 2022 Updated Guidelines, what is the goal blood pressure for most adults, excluding pregnant patients (which of the following blood pressures is not considered to be hypertensive or pre-hypertensive)?
A. <200/100 mmHg
B. <120/90 mmHg
C. <130/70 mmHg
D. <150/95 mmHg
E. <120/80 mmHg
E. <120/80 mmHg
What event occurs in a normal heart during isovolumic contraction?
A. the second heart sound ("dub") is heard
B. the aortic valve opens
C. the atrial-ventricular valves are open
D. the aortic valve is closed
E. the pulmonic valve is open
D. the aortic valve is closed
Why does the greatest pressure drop in the circulation occur across the arterioles?
A. they have the greatest total surface area
B. the velocity of blood through them is lowest
C. they have the greatest total cross sectional area
D. their walls have the most compliance (i.e. easiest to stretch)
E. they have the greatest resistance
E. they have the greatest resistance
How is the function of cardiac pacemaker cells affected by parasympathetic stimulation?
A. Increase in the rate of depolarization to reach threshold
B. Increase in the voltage threshold for action potential firing
C. Increase in the opening of funny Na+ channels
D. Hyperpolarization of the membrane potential
E. Decrease in the K+ efflux after rapid depolarization
D. Hyperpolarization of the membrane potential
In the Pressure-Volume Loop (A,B,C,D) shown below, what does point D to point A represent?
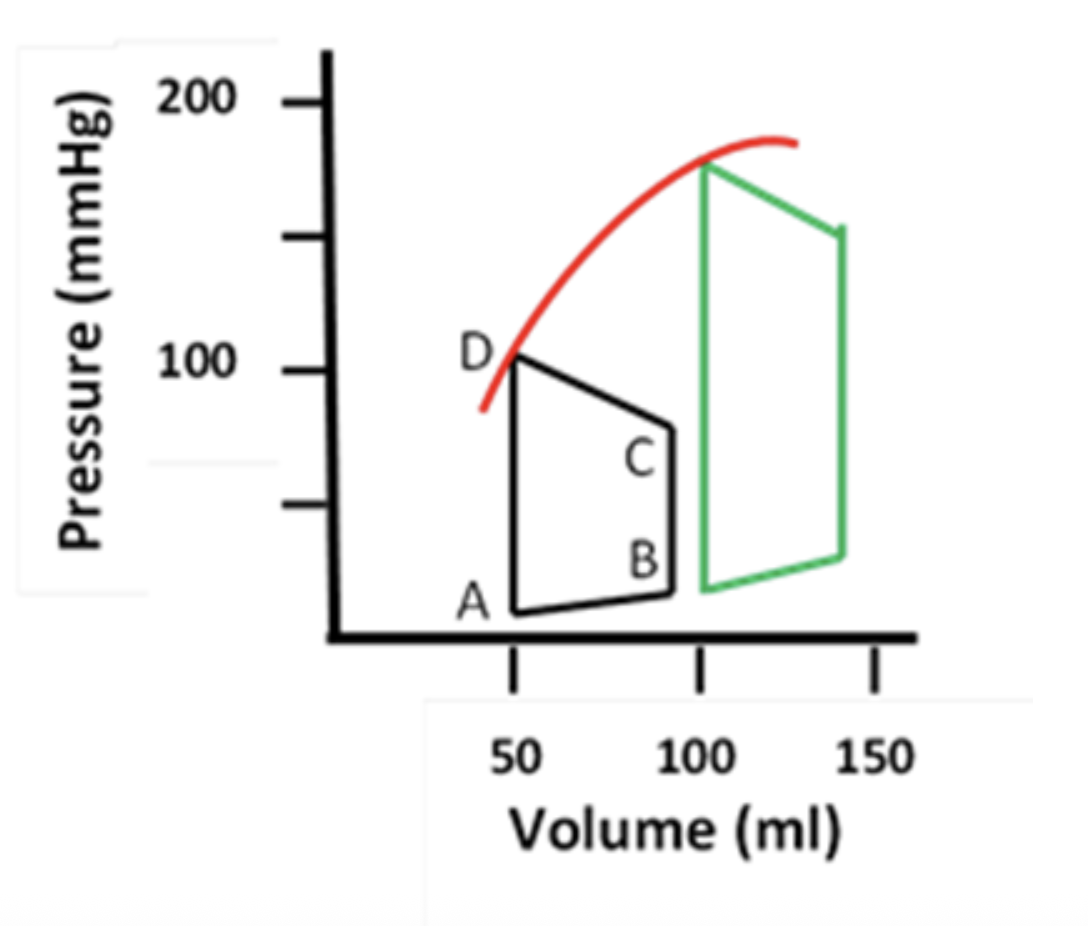
A. isovolumic relaxation
B. isovolumic contraction
C. ejection of blood
D. ventricular filling
E. opening of the aortic and pulmonic valves
A. isovolumic relaxation
Why does blood continue to flow out of the arteries to the remaining systemic blood vessels during diastole?
A. blood is flowing from the pulmonary to the systemic circulatory system
B. the walls of the large arteries recoil from being stretched in systole
C. the arterioles relax to reduce total peripheral resistance
D. the veins contract to maintains arteriole pressure
E. longitudinal bundles of smooth muscle in the adventitia contract to propel blood forward
B. the walls of the large arteries recoil from being stretched in systole
Which of the following statements best describes an aortic dissection?
A. A bulge in the aorta caused by the gradual weakening of the vessel wall
B. A bulge in the aorta caused by a tear in the tunica intima and tunica media, which allowed blood to pool between the tunica media and the tunica adventitia
C. A bulge in the aorta caused by a tear in the tunica intima, which allowed blood to pool between the tunica intima and the tunica media
D. A bulge in the aorta caused by a hemorrhage and formation of a hematoma under the tunica adventitia
E. A true rupture of the aorta at the site of an aneurysm
C. A bulge in the aorta caused by a tear in the tunica intima, which allowed blood to pool between the tunica intima and the tunica media
10. Suppose the Purkinje fibers are the only cells capable of pacemaker function in a heart. What would the heart rate be closest to in this scenario?
A. Zero beats per minute because the Purkinje fibers have no intrinsic pacemaker activity
B. 35 beats per minute
C. 55 beats per minute
D. 70 beats per minute
E. 100 beats per minute
B. 35 beats per minute
ACE inhibitors are a common treatment for heart failure. They act by blocking the formation of angiotensin II, which causes smooth muscle contraction. What is the expected outcome of this drug action?
A. Increasing peripheral resistance
B. Increasing ejection fraction
C. Decreasing peripheral resistance
D. Decreasing ejection fraction
E. Decreasing venous return
C. Decreasing peripheral resistance
Chronic hypertension is a major risk factor for the development of atherosclerosis. Why might this be the case?
A. There is no direct causation between hypertension and atherosclerosis; they are just coincident diagnoses (likely due to modifiable lifestyle choices).
B. Chronic hypertension would increase the amount of cholesterol and LDL in circulation.
C. Chronic hypertension increases the turbulence of blood flow, increasing the likelihood that platelets would adhere and aggregate.
D. Chronic hypertension decreases the rate of smooth muscle proliferation, which allows cells in the tunica media to be replaced by adipose tissue.
E. Chronic hypertension would cause continuous stress to the tunica intima of blood vessels, resulting in chronic endothelial injury.
E. Chronic hypertension would cause continuous stress to the tunica intima of blood vessels, resulting in chronic endothelial injury.
Which of the following statements regarding the distribution of water in the body is CORRECT?
A. Approximately 1/2 of the total body water is in the interstitial fluid (ISF).
B. Approximately 1/3 of the total body water is in the intracellular fluid (ICF).
C. Approximately 2/3 of the total body water is in the interstitial fluid (ISF).
D. Approximately 3/4 of the total body water is in the extracellular fluid (ECF).
E. Approximately 1/12 of the total body water is in the intravascular fluid (IVF).
E. Approximately 1/12 of the total body water is in the intravascular fluid (IVF).
Which of the following statements regarding the concentration of ions in the fluid compartment of the body is CORRECT?
A. The concentration of Ca2+ is higher in the intracellular fluid (ICF) compartment compared to the extracellular fluid (ECF) compartment.
B. The concentration of Ca2+ is lower in the interstitial fluid (ISF) compartment compared to the intracellular fluid (ICF) compartment.
C. The concentration of Na+ is lower in the intracellular fluid (ICF) compartment compared to the extracellular fluid (ECF) compartment.
D. The concentration of K+ is higher in the interstitial fluid (ISF) compartment compared to the intracellular fluid (ICF) compartment.
E. The concentration of K+ is higher in the intravascular fluid (IVF) compartment compared to the extracellular fluid (ECF) compartment.
C. The concentration of Na+ is lower in the intracellular fluid (ICF) compartment compared to the extracellular fluid (ECF) compartment.
3. Which of the following statements regarding intercellular signaling is CORRECT?
A. Endocrine hormones typically signal via low affinity receptors.
B. Steroid hormones typically bind membrane receptors that signal via G-protein second messengers.
C. Peptide hormones typically bind cytosolic or nuclear receptors that directly regulate DNA transcription.
D. Neurotransmitters typically signal via high affinity receptors.
E. Neurotransmitters typically signal via low affinity receptors.
E. Neurotransmitters typically signal via low affinity receptors.
Choking on a piece of food can elicit hyperactivity of the parasympathetic system in some individuals. Which of the following is a symptom you would expect to see in these individuals?
A. decreased bowel sounds
B. decreased salivation
C. increased sweating
D. decreased heart rate
E. dilated pupils
D. decreased heart rate
At which synapse would signaling occur via norepinephrine on alpha-adrenergic receptors?
A. Pre-ganglionic parasympathetic neurons on post-ganglionic parasympathetic neurons.
B. Post-ganglionic parasympathetic neurons on end organs.
C. Motor neurons on skeletal muscle.
D. Pre-ganglionic sympathetic neurons on post-ganglionic sympathetic neurons.
E. Post-ganglionic sympathetic neurons on arteriolar smooth muscle.
E. Post-ganglionic sympathetic neurons on arteriolar smooth muscle.
Channels and transporters are both used to move charged molecules across biological membranes. However, what key feature typically differentiates channels from transporters?
A. Channels transport specific molecules and transporters transport molecules non-selectively .
B. Channels can transport substances against their concentration gradient and transporters cannot .
C. Channels require ATP for transport and transporters do not.
D. Channels have a gating mechanism and transporters do not.
E. Channels exhibit a maximal rate of transport (Tm) and transporters do not have a maximum rate.
D. Channels have a gating mechanism and transporters do not.
Omental fat cells bind peptide Y, which then causes an increase in cell size and the expression of peptide Y receptors on the cell surface. What is this an example of?
A. positive feedback
B. negative feedback
C. antagonistic control
D. tonic control
A. positive feedback
What is the approximate age of the embryo shown in the attached diagram?
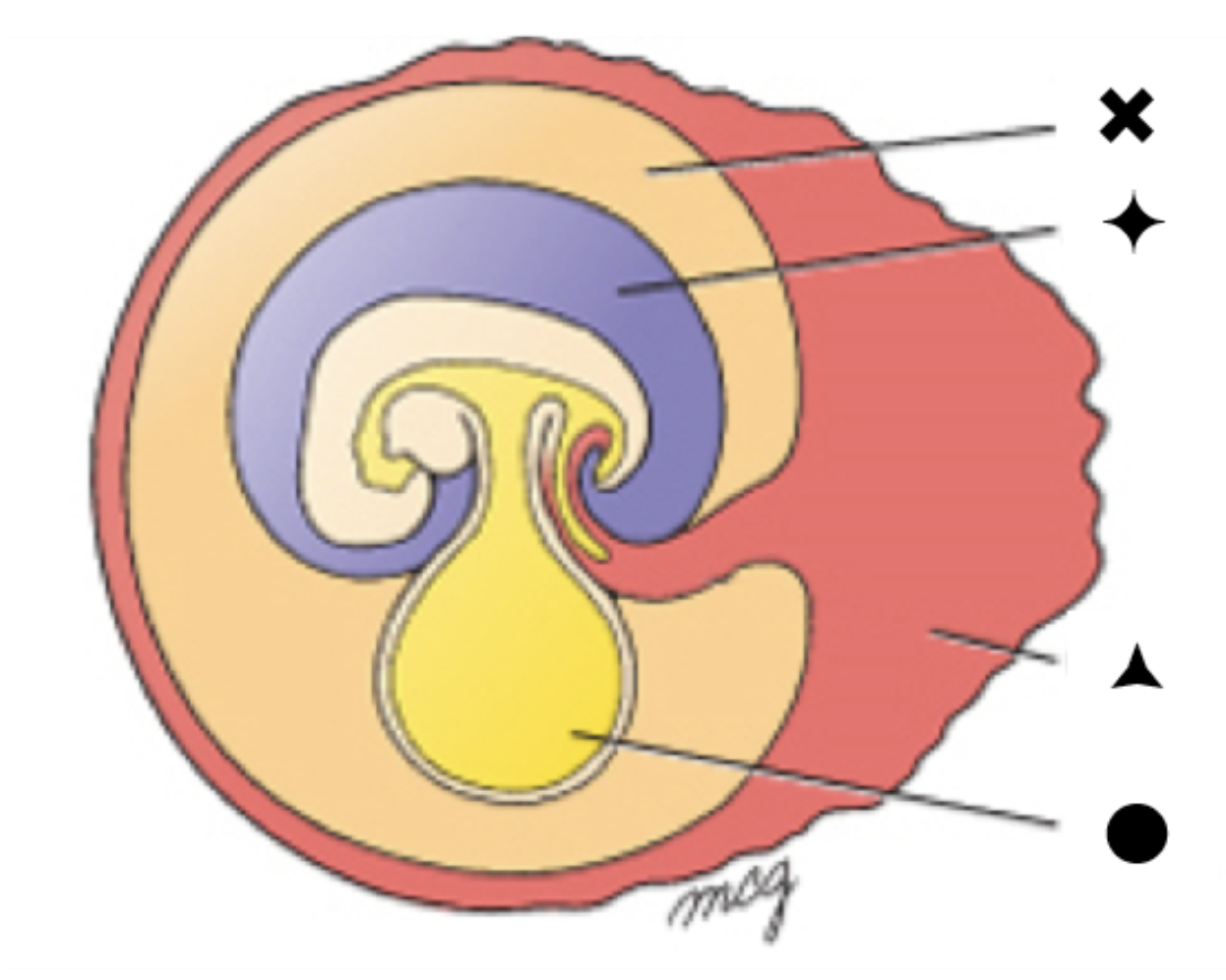
A. 2 weeks
B. 4-5 weeks
C. 8 weeks
D. 12 weeks
E. 18-20 weeks
B. 4-5 weeks
Which label indicates a space lined by endoderm-derived cells?
A. the triangle
B. the diamond
C. the circle
D. the x
C. the circle
Which label indicates a space containing fluid that is produced by the kidneys in the developing fetus?
A. the triangle
B. the diamond
C. the circle
D. the x
B. the diamond
A 9-month-old girl, with a colostomy fashioned at birth for an imperforate anus, was brought into the neonatal GI surgery service for further management and colostomy closure and referral to the orthopedic service for treatment of congenital lower limb defects. There was no other significant history from the pregnancy other than ultrasound examinations at 20 and 36 weeks, both of which indicated oligohydramnios. At birth she had lower limb deformities and imperforate anus, for which the colostomy was performed. On examination she was active and alert, in satisfactory general health, and had passed normal mental milestones. However, she had partially fused and uniformly hypoplastic lower limbs as shown in the image.
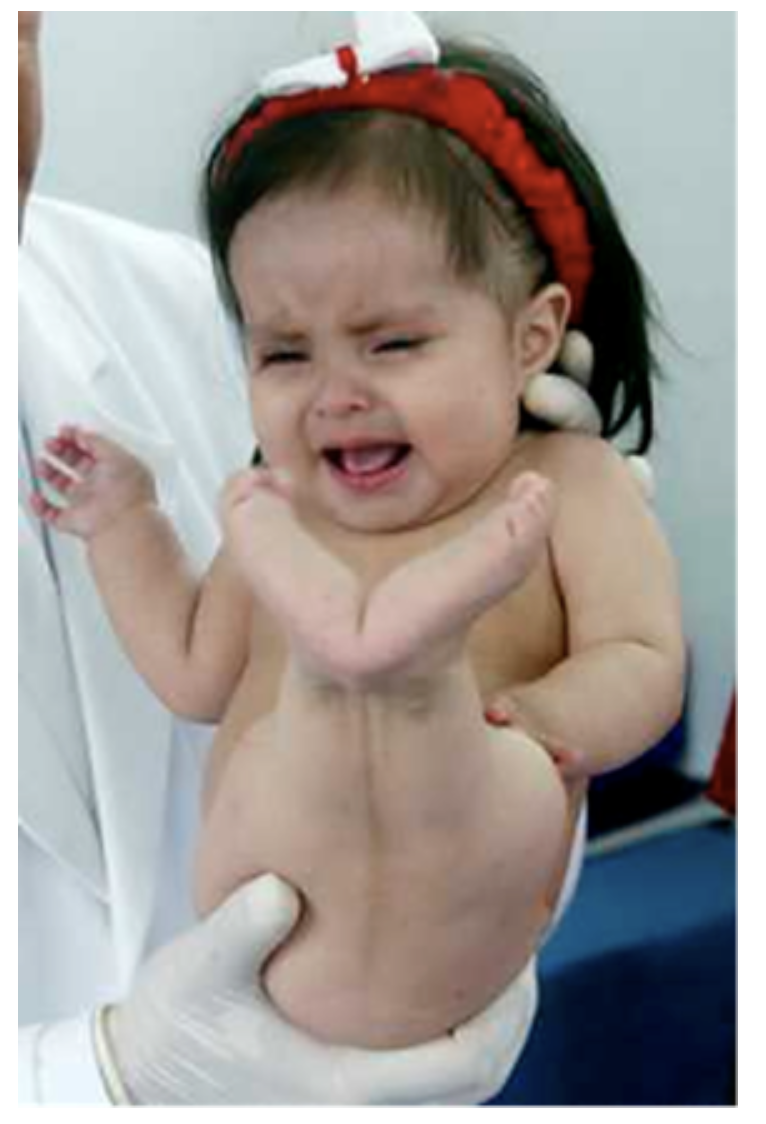
What is the MOST LIKELY cause for this spectrum of congenital defects?
A. failure of trunk neural crest to migrate into the lower limbs
B. premature closure of the posterior (caudal) neuropore.
C. premature regression of the primitive streak during gastrulation.
D. abnormal persistence of primitive streak tissue after completion of gastrulation.
E. abnormal left-right patterning due to ciliary dysfunction.
C. premature regression of the primitive streak during gastrulation.
A 9-month-old girl, with a colostomy fashioned at birth for an imperforate anus, was brought into the neonatal GI surgery service for further management and colostomy closure and referral to the orthopedic service for treatment of congenital lower limb defects. There was no other significant history from the pregnancy other than ultrasound examinations at 20 and 36 weeks, both of which indicated oligohydramnios. At birth she had lower limb deformities and imperforate anus, for which the colostomy was performed. On examination she was active and alert, in satisfactory general health, and had passed normal mental milestones. However, she had partially fused and uniformly hypoplastic lower limbs as shown in the image.
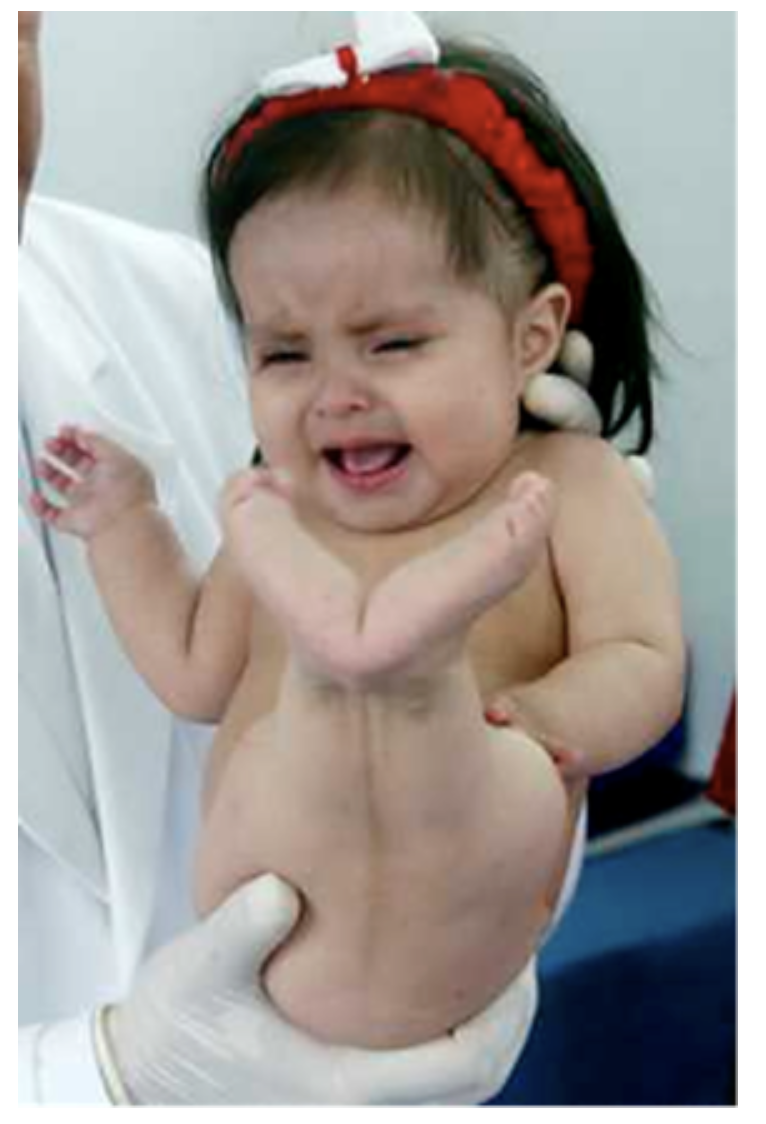
This patient should be screened for other defects. Why is this necessary?
A. The abnormal persistence of the primitive streak may cause the neural plate to expand, which can lead to defects in the nervous system.
B. The dysfunction of cilia at the primitive node may cause production of too little endoderm, causing defects in the lungs and digestive system.
C. Improper migration of neural crest tissue can cause production of too much mesoderm, causing defects in the skeletal muscles.
D. The premature closure of the posterior (caudal) neuropore may prevent development of the anterior visceral endoderm (AVE), which can lead to developmental delays.
E. The premature regression of the primitive streak may impact development of other structures derived from mesoderm, like the kidneys and the heart.
E. The premature regression of the primitive streak may impact development of other structures derived from mesoderm, like the kidneys and the heart.
You are tutoring a fellow student in Histology. The student is struggling to identify the attached image as thick or thin skin. What specific feature would you use to determine that the skin on this slide is thick skin and NOT thin?
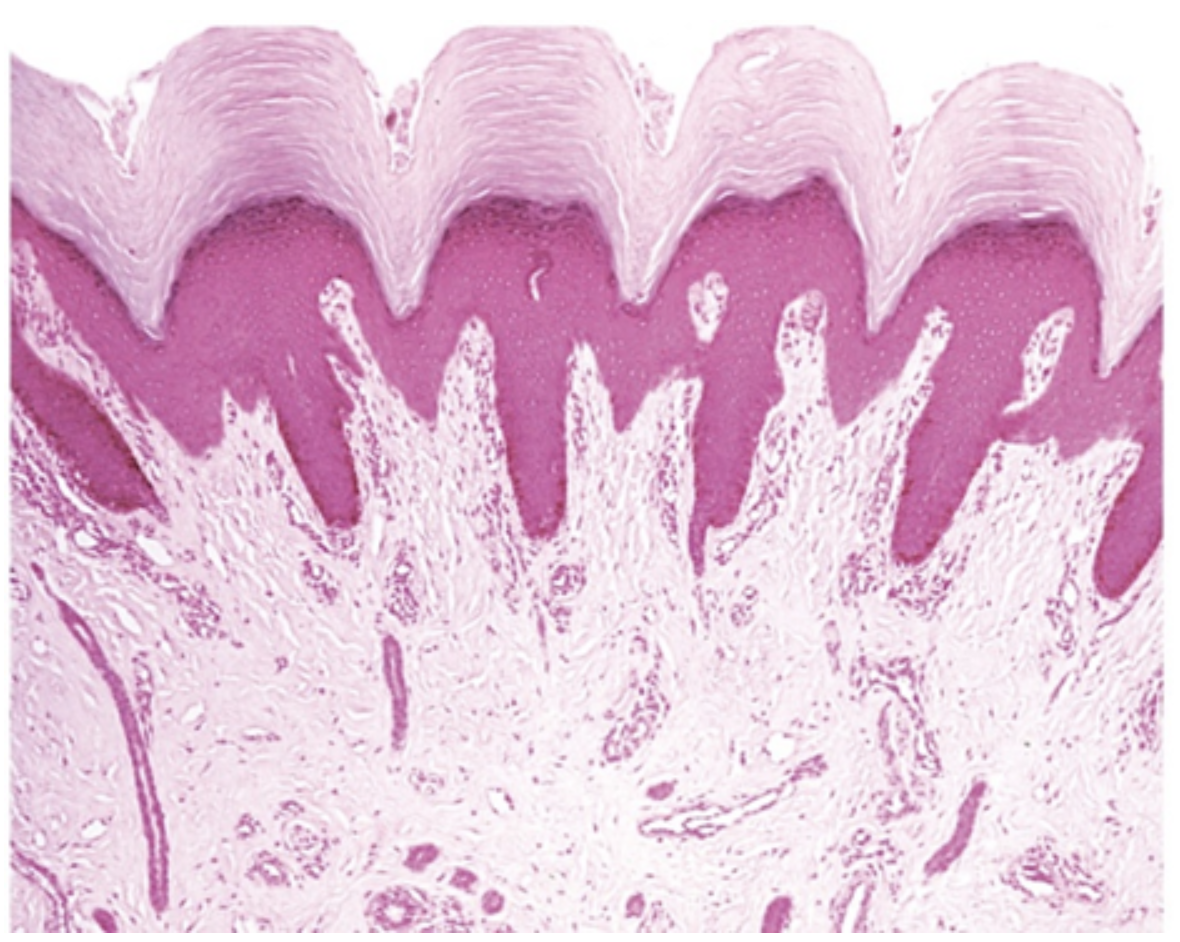
A. a stratum corneum more than 20 layers thick
B. the presence of melanocytes
C. the presence of eccrine sweat glands and ducts
D. the absence of papillary ridges
E. a single layer of cells in the stratum granulosum
A. a stratum corneum more than 20 layers thick
If you go outside on a very hot day, what will eventually happen to blood flow in the dermal papillae?
A. blood flow will remain the same
B. blood flow will decrease because heat causes clot formation
C. blood flow will increase because blood vessels expand to allow heat loss from the body
D. blood flow will increase because heat causes increased vascular permeability
E. blood flow will decrease because blood vessels constrict to conserve heat in the body
C. blood flow will increase because blood vessels expand to allow heat loss from the body
View the glands in the slide linked hereLinks to an external site.. (An image of the glands is also attached.) Under what conditions would these glands become activated? https://www.digitalscope.org/ViewerUI/?SlideId=dc093054-02ed-4912-bdf8-6422eb042d17&X=24059.74910812031&Y=25055.277335969426&Z=23&ann=11100000100000
A. In close proximity to an individual of the same species (for pheromone release)
D. An increase in body temperature
B. Stimulation of the hair follicles by brushing
C. A decrease in body temperature
D. An increase in body temperature
E. In response to having excess oil on the skin
D. An increase in body temperature
Examine the attached image which has the layers of the skin labeled. Which option below correctly identifies the layer of the skin and a unique characteristic of that layer?
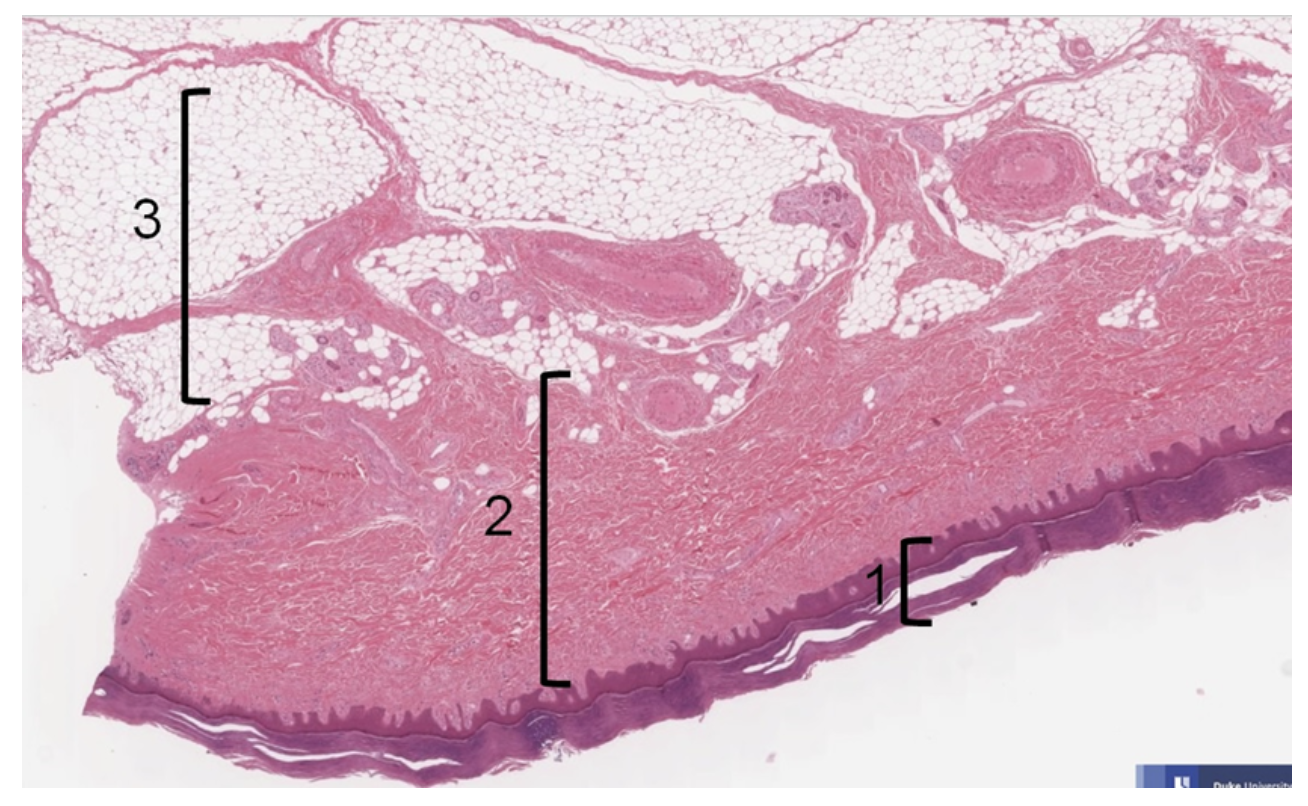
A. Layer 2 contains white adipose tissue and is therefore the dermis.
B. Layer 1 contains no blood vessels and is therefore the epidermis.
C. Layer 3 contains eccrine sweat glands and is therefore the dermis.
D. Layer 1 contains melanocytes and is therefore the hypodermis.
E. Layer 2 contains sensory nerve endings and is therefore the epidermis.
B. Layer 1 contains no blood vessels and is therefore the epidermis.
Because exogenous steroids disrupt cell division, prolonged used of topical corticosteroids can cause skin thinning. Which layer of the skin would be MOST responsible for this adverse drug effect? (i.e. in which layer of the skin do we see the greatest number of mitosis-capable cells?)
A. stratum lucidum
B. stratum basale
C. stratum granulosum
D. stratum corneum
E. stratum spinosum
E. stratum spinosum
In the figure shown, where would you expect to find Langerhan’s cells?
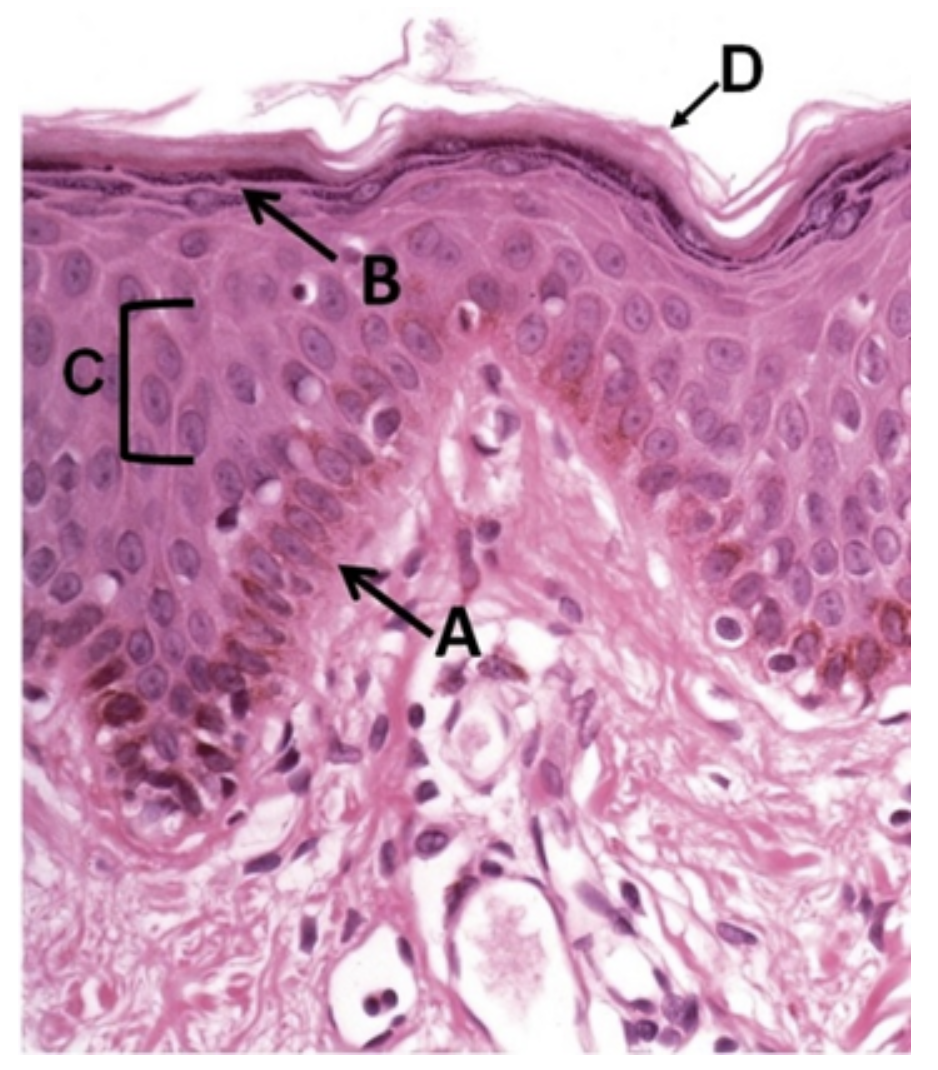
A. A
B. B
C. C
D. D
C. C
Which of the following is a “normal” osmolarity for ECF?
A. 190 mOsM
B. 240 mOsM
C. 290 mOsM
D. 340 mOsM
E. 390 mOsM
C. 290 mOsM
A patient quickly rises from her bed to standing. Under normal conditions, this change in body position will result in:
A. activation of the renin-angiotensin-aldosterone system.
B. widespread vasodilation of arterioles
C. an increase in sympathetic firing
D. an increase in parasympathetic firing
E. a decrease in heart rate
C. an increase in sympathetic firing
In the Pressure-Volume Loop (A,B,C,D) shown, what does point B to point C represent?
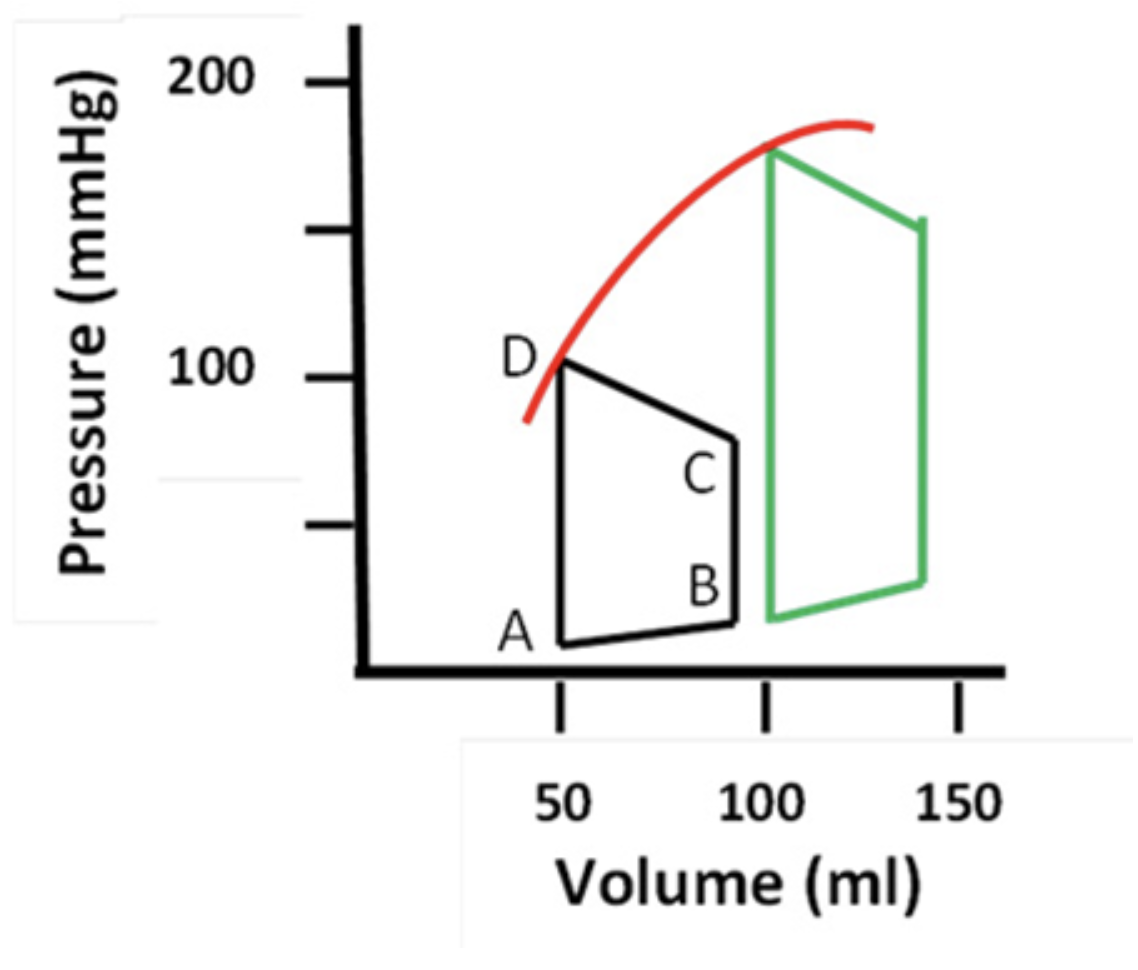
A. atrial ejection
B. isovolumic contraction
C. isovolumic relaxation
D. ventricular filling
E. ventricular ejection
B. isovolumic contraction
The T wave on an electrocardiogram corresponds to electrical current from which layer of tissue shown in this slide? [digital scope]Links to an external site.
https://www.digitalscope.org/ViewerUI/?SlideId=ec07dcf4-f848-4b68-9aea-f9e607fbbeac&ann=111000011
A. A
B. B
C. C
D. D
E. E
E. E
Which of the following are characterized by a thick tunica media containing many elastic lamellae intermixed with layers of circumferentially oriented smooth muscle?
A. Large elastic arteries (such as the aorta)
B. Large veins (such as the inferior vena cava)
C. Muscular arteries
D. Blood capillaries in skeletal muscle
E. Lymphatic capillaries in small intestinal villus
A. Large elastic arteries (such as the aorta)
What is the tissue indicated by the arrow in this slideLinks to an external site. stained with Masson's trichrome?
https://www.digitalscope.org/ViewerUI/?SlideId=35899d00-8a03-4539-bad8-87b183e78f04&ann=111000111
A. cardiac (fibrous) skeleton
B. Purkinje fibers
C. myocardium
D. epicardium
E. endocardium
A. cardiac (fibrous) skeleton
Suppose the SA node is the only source of pacemaker cells in the heart. What would the heart rate be closest to in this scenario?
A. 30 beats per minute
B. 40 beats per minute
C. 60 beats per minut
D. 80 beats per minute
E. 150 beat per minute
D. 80 beats per minute
During cardiac catheterization of a 6-year-old child, the radiologist notes that the contrast medium released into the arch of the aorta is IMMEDIATELY visible in the left pulmonary artery. What is the MOST LIKELY explanation for this finding?
A. Patent ductus arteriosus
B. Patent ductus venosus
C. Ventricular septal defect
D. Atrial septal defect
E. Mitral valve prolapse
A. Patent ductus arteriosus
Which of the following statements is TRUE of the cardiac muscle pacemaker action potential shown in the figure?
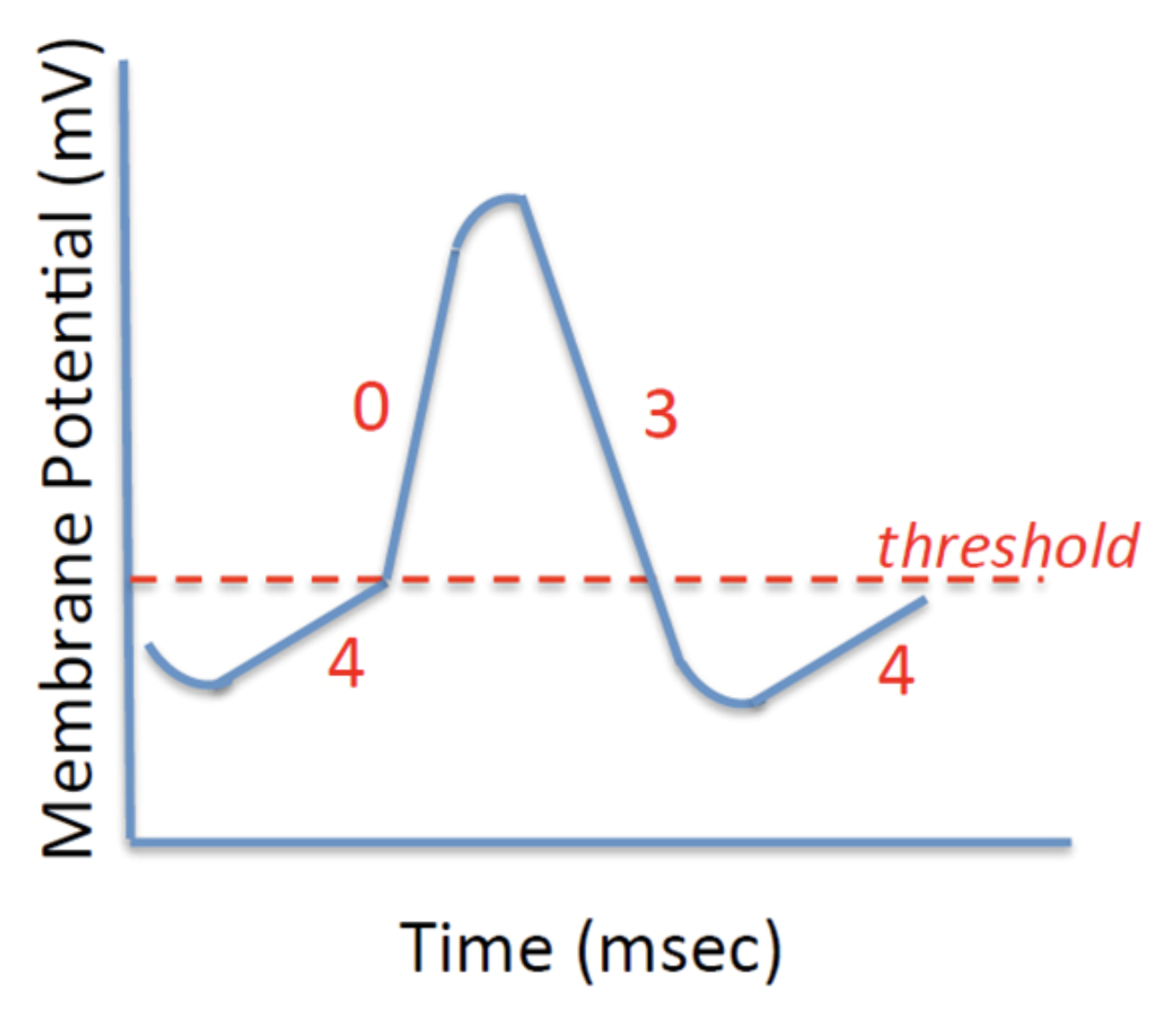
A. Phase 0 is caused by a rapid increase in sodium influx.
B. Slow depolarization in phase 4 is due to sympathetic nerve stimulation.
C. Phase 0 is caused by the opening of voltage gated calcium channels.
D. It is typical of the contractile muscle fibers in the ventricle.
C. Phase 0 is caused by the opening of voltage gated calcium channels.
Examine the structure indicated by the arrow on the slide linked hereLinks to an external site.. What BEST describes the function of this structure?
A. This valve, when closed, prevents blood in the ventricle from flowing back into the atria.
B. This collection of cardiomyocytes, connected by gap junctions, conducts electrical signals to synchronize contractions of the chambers of the heart.
C. This section of the epicardium forms a junction to separate the atrium and the ventricle from each other.
D. This elastic artery, with many layers of smooth muscle and elastin, withstands high blood pressures that leave the heart.
E. This valve remains closed until a buildup of intraventricular pressure forces it open and allows for ejection of blood into an elastic artery.
A. This valve, when closed, prevents blood in the ventricle from flowing back into the atria.
Examine the blood vessel on the slide linked hereLinks to an external site.. How is this vessel BEST categorized?
A. Elastic artery
B. Muscular artery
C. Large vein
D. Medium vein
E. Capillary
C. Large vein
The lighter-staining cells indicated within the bracketed region (toward the top of the slide) are specialized primarily for what function? [virtual slide]Links to an external site. https://www.digitalscope.org/ViewerUI/?SlideId=f5770b3e-c48b-4ed2-8ded-5d5dc2735043&ann=111000101
A. prevent prolapse of atrioventricular valves
B. electrical impulse (action potential) conduction
C. forceful contraction
D. strengthening the cardiac wall
E. elasticity
B. electrical impulse (action potential) conduction
Which of the following is a feature of the sequence of cardiovascular defects known as the “tetralogy of Fallot?”
A. atrial septal defect
B. patent ductus venosus
C. right atrial hypertrophy
D. double aortic arch
E. pulmonary stenosis
E. pulmonary stenosis
If development of the conotruncal endocardial cushions is disrupted, which of the following will not form correctly?
A. mitral valve
B. aortic valve
C. ductus venosus
D. tricuspid valve
B. aortic valve
Imagine (or better yet, sketch) the embryonic heart prior to looping. What BEST DESCRIBES the orientation of the venous input via the atria and output via the outflow tract?
A. Both input and output are cranial (superior or “anterior”)
B. Both input and output are caudal (inferior or “posterior”)
C. Input is to the right of the midline axis and output is to the left of the midline axis
D. Input is cranial and output is caudal
E. Input is caudal and output is cranial
E. Input is caudal and output is cranial
A 45-year-old female is admitted to the hospital with swelling (edema) of the lower limbs. Ultrasound examination reveals an incompetent tricuspid valve. Into which vessel or chamber will regurgitation of blood MOST LIKELY occur in this patient?
A. Ascending aorta
B. Left atrium
C. Right atrium
D. Left ventricle
E. Pulmonary trunk
C. Right atrium
During normal vascular development, what happens to the proximal segment of the 6th aortic arch on the RIGHT?
A. contributes to the right common carotid artery
B. contributes to the proximal right subclavian artery
C. contributes to the ductus arteriosus
D. contributes to the right pulmonary trunk
E. regresses
D. contributes to the right pulmonary trunk
During normal vascular development, what gives rise to the inferior vena cava and azygous veins?
A. subcardinal and supracardinal veins
B. vitelline veins
C. umbilical veins
D. vitelline arteries
E. ductus venosus
A. subcardinal and supracardinal veins
Refer to the image of the electrocardiogram. When does atrial depolarization occur?
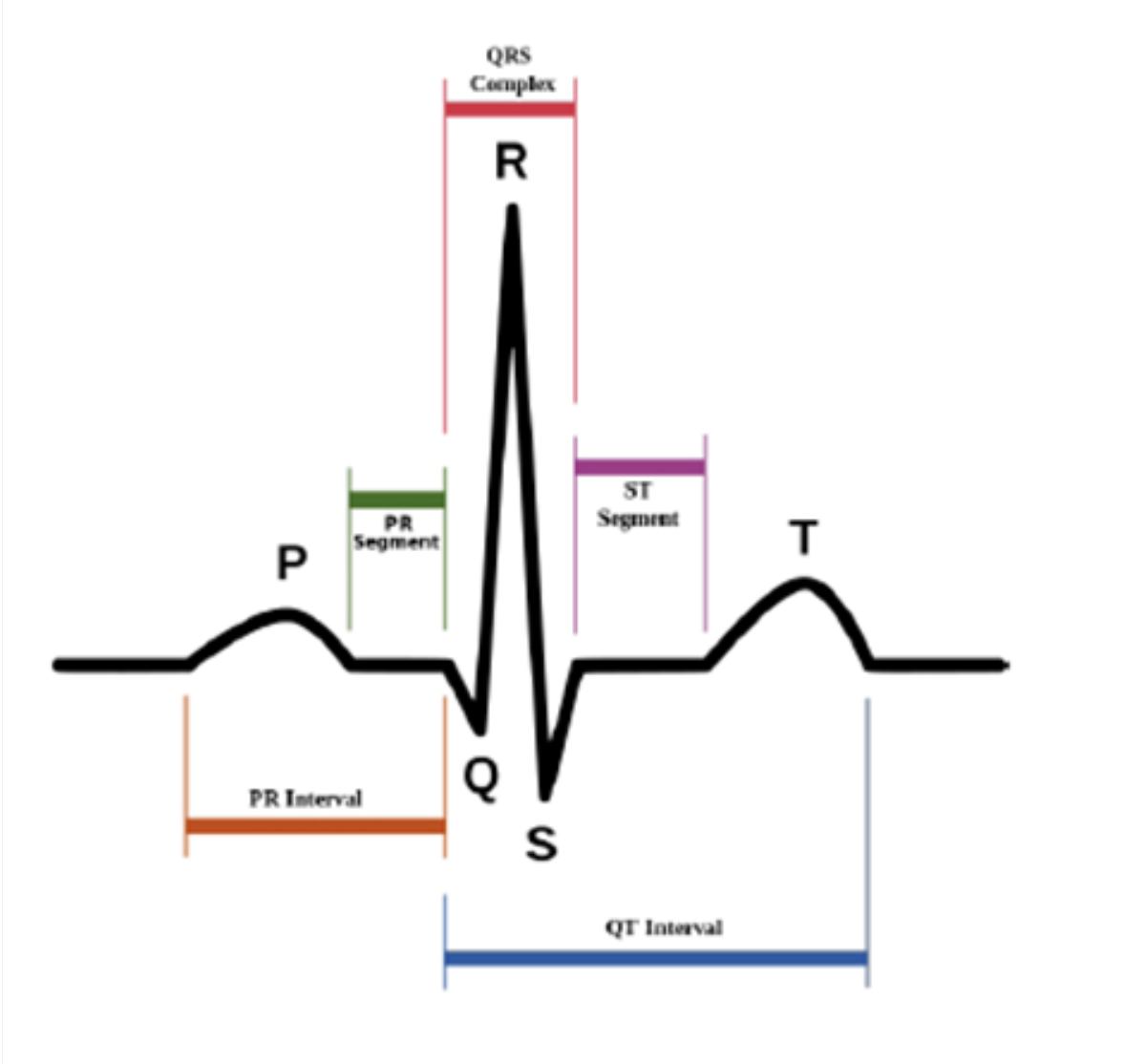
A. P-wave
B. PR segment
C. QRS complex
D. S-T segment
E. T-wave
A. P-wave
Why does the contractile cardiomyocyte NOT exhibit tetanus?
A. Duration of the twitch is too short to allow summation of contractions.
B. Duration of phase 0 of its action potential is too long to allow summation of contractions.
C. There is no absolute refractory period.
D. The absolute refractory period is too long to allow summation of contractions.
D. The absolute refractory period is too long to allow summation of contractions.
You are monitoring the ECG of a patient while shadowing Dr. Cor, a cardiologist. You notice that the Q-T interval has lengthened and report to Dr. Cor that this means the depolarization of the ventricle has slowed. Dr. Cor asks for the physical symptom this causes in the patient. What is your answer?
A. a decrease in heart rate
B. an increase in heart rate
C. arterial vasoconstriction
D. uncontrolled bleeding
E. hyperglycemia
A. a decrease in heart rate
The first heart sound (“lub”) is heard at approximately the same time as which of the following events?
A. closing of the aortic valve
B. diastolic filling of the ventricles
C. P-wave of the electrocardiogram (ECG)
D. QRS complex of the ECG
E. T-wave of the ECG
D. QRS complex of the ECG
Which event is responsible for creating the second heart sound (“dub”)?
A. the closing of the AV valves
B. the opening of the semilunar valves
C. the closing of the semilunar valves
D. isovolumic contraction
E. the end of diastole
C. the closing of the semilunar valves
When the cardiac pacemaker cells are subjected to sympathetic stimulation, what will happen?
A. the heart rate will decrease
B. the membrane potential will hyperpolarize
C. the threshold for action potential firing will increase
D. the rate of depolarization to reach threshold will increase
E. sympathetic stimulation has no effect on these cells
D. the rate of depolarization to reach threshold will increase
Blood flow in the body is regulated via many mechanisms, but dilation and constriction of vessels are key. Changing the diameter of a vessel has effects on pressure and flow in upstream and downstream vessels. Suppose that pressure in a capillary is DECREASED because of a change in another vessel. What event MOST LIKELY caused this drop in pressure?
A. Vasoconstriction of the medium vein downstream of the capillary
B. Vasodilation of the muscular artery upstream of the capillary
C. Vasoconstriction of the venule immediately downstream of the capillary
D. Vasodilation of the arteriole immediately upstream of the capillary
E. Vasoconstriction of the arteriole immediately upstream of the capillary
E. Vasoconstriction of the arteriole immediately upstream of the capillary
Which of the following is TRUE during phase 2 of the contractile cardiomyocyte action potential shown below?
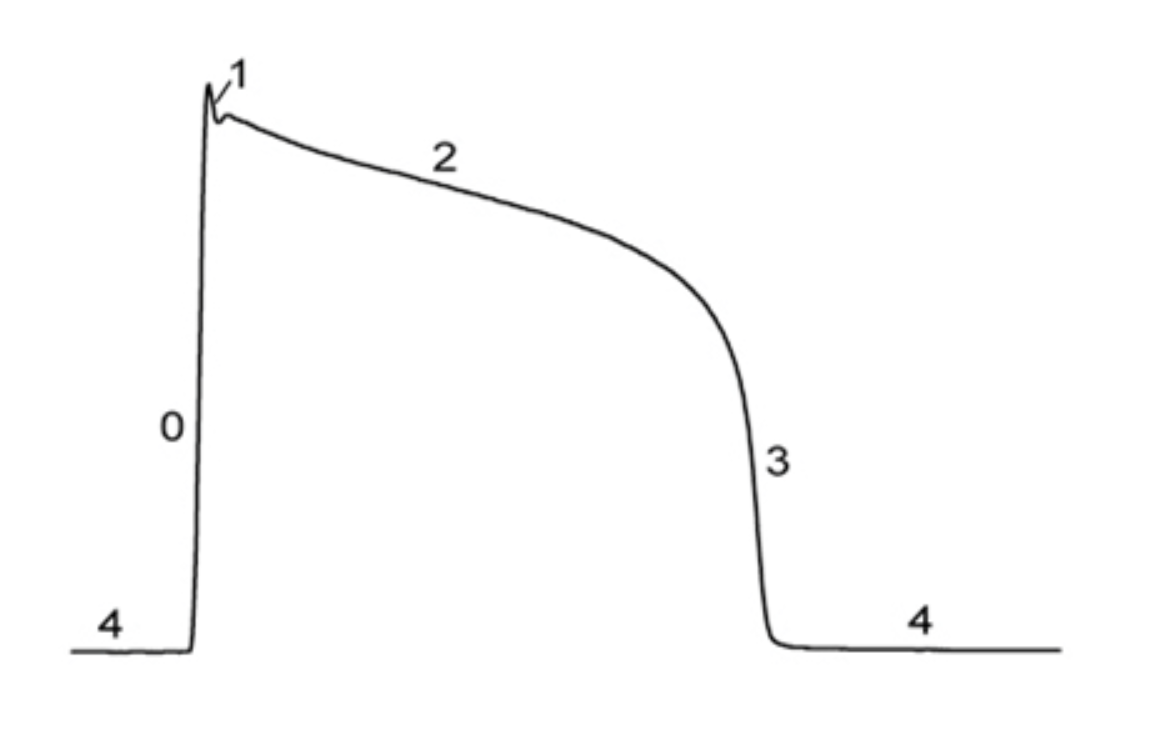
A. Only potassium current is flowing.
B. Inward current is carried by calcium ions.
C. Current from neighboring regions can trigger a second action potential.
D. Potassium current is nearly equal to sodium current.
B. Inward current is carried by calcium ions.
CB is a 65yo patient under the care of a cardiologist for chronic hypertension. After making lifestyle modifications for two years, this patient’s average brachial blood pressure is 135/85.
45. One of CB’s main complaints regarding his chronic hypertension is swelling, particularly in his feet after a long day of standing at work. Why does he suffer from edema?
A. Chronic hypertension causes blood to back up, leading to vessel congestion and subsequent edema.
B. Chronic hypertension increases the capillary hydrostatic pressure, leading to decreased capillary reabsorption.
C. Chronic hypertension causes liver damage, decreasing albumin production, and leading to decreased blood plasma oncotic pressure.
D. Chronic hypertension increases the capillary hydrostatic pressure, leading to increased capillary filtration.
E. Chronic hypertension increases the oncotic pressure of the interstitial fluid, leading to an increase in osmotic movement of water out of the blood plasma and into the interstitial space.
B. Chronic hypertension increases the capillary hydrostatic pressure, leading to decreased capillary reabsorption.
CB is a 65yo patient under the care of a cardiologist for chronic hypertension. After making lifestyle modifications for two years, this patient’s average brachial blood pressure is 135/85.
The cardiologist prescribes an ACE inhibitor (ACEi) to manage CBs hypertension. ACEis act on the RAAS pathway by blocking the conversion of angiotensin I into angiotensin II. Normally, angiotensin II causes vasoconstriction. How do ACEis decrease systemic blood pressure?
A. ACEis increase total peripheral resistance, which decreases blood pressure.
B. ACEis decrease total peripheral resistance, which decreases blood pressure.
C. ACEis increase renin secretion at the kidneys, increasing urine output and decreasing blood volume, which decreases blood pressure.
D. ACEis increase ADH secretion from the hypothalamus, increasing urine output and decreasing blood volume, which decreases blood pressure.
E. ACEis decrease sympathetic stimulation of the heart, decreasing heart rate and cardiac output, which decreases blood pressure.
B. ACEis decrease total peripheral resistance, which decreases blood pressure.
CB is a 65yo patient under the care of a cardiologist for chronic hypertension. After making lifestyle modifications for two years, this patient’s average brachial blood pressure is 135/85.
While the ARBs seem to be generally working, after 6 months CB complains to his partner of occasional dizziness and visual disturbances (blurriness) upon exertion. One night, he experiences severe “ripping” chest pain. He is transported to an ER at her insistence and is eventually diagnosed with an aortic dissection resultant from chronic hypertension.
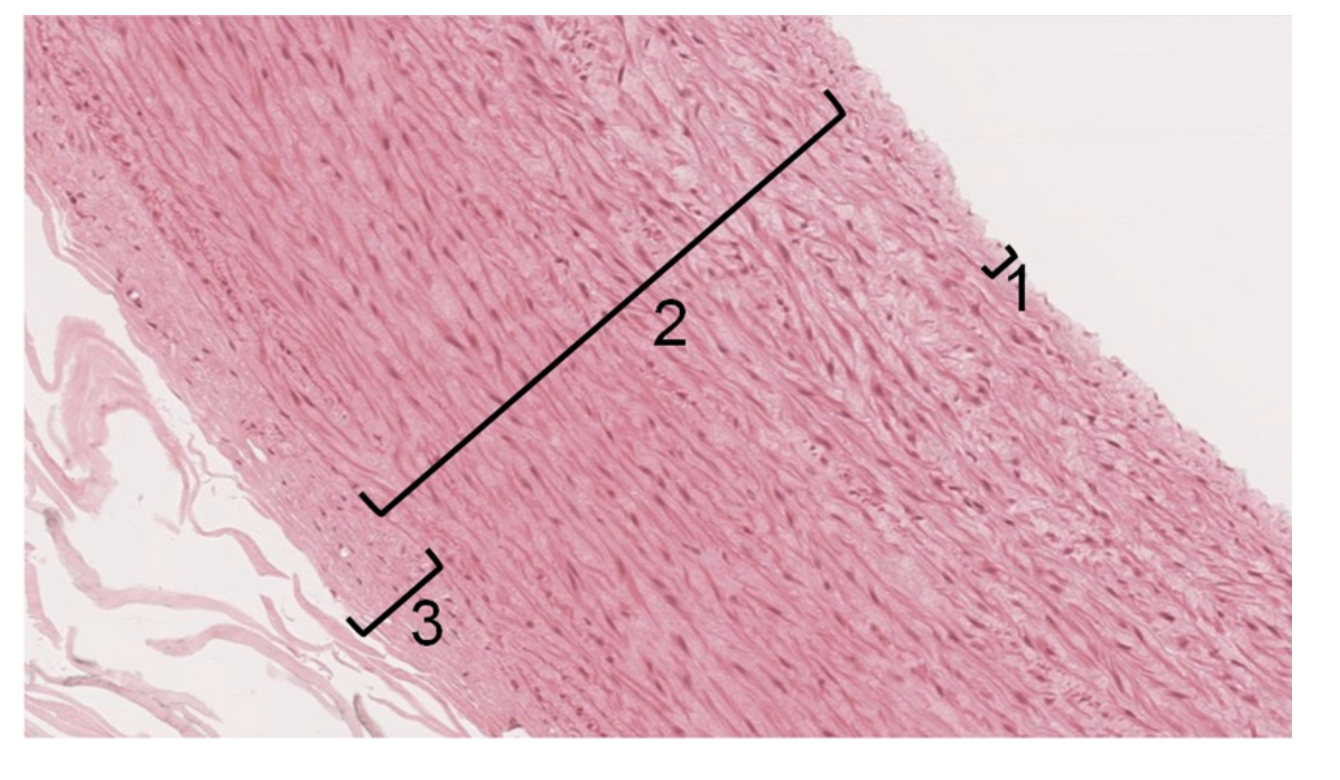
Examine the attached image of an elastic artery. If a dissection were to occur, which layers would be DIRECTLY separated from each other?
Layers 2 & 3; the tunica media separates from the tunica adventitia
B. Layers 1 & 3; the tunica intima separates from the tunica adventitia
C. Layers 1 & 2; the tunica media separates from the tunica adventitia
D. Layers 1 &2; the tunica intima separates from the tunica media
E. Layers 2 & 3; the tunica intima separates from the tunica media
D. Layers 1 &2; the tunica intima separates from the tunica media
CB is scheduled for surgery in the morning to address his aortic dissection. Understandably, he is very worried. He exclaims, “between the high blood pressure and now this aneurysm, it feels like I’m at risk for EVERYTHING!” While you agree that he does have an increased risk for certain conditions, based on his history, there is one condition that he almost certainly currently has. Which condition is he likely to suffer from today?
A. myocardial infarction
B. deep vein thrombosis
C. atherosclerosis
D. pulmonary embolism
E. cystic medial degeneration
C. atherosclerosis
The aortic dissection was repaired, but due to extensive scarring at the repair site, CB’s condition deteriorated and left him in left-sided heart failure within 6 months. Left Heart Failure is marked by a drastic decrease in ejection fraction. Which change in cardiac performance parameters would MOST DIRECTLY lead to a decrease in EF?
A. increased stroke volume
B. decreased heart rate
C. increased end systolic volume
D. increased end diastolic volume
E. increased heart rate
D. increased end diastolic volume
What symptom do you expect to see first in CB, because of left-sided heart failure? (What would a decrease in left ventricle pumping cause, most directly?)
A. Swollen legs, because of congestion of blood in the vena cava.
B. Decreased blood pressure, because of inhibition of the RAAS pathway.
C. Dehydration, because of increased K+ and Na+ loss at the kidneys.
D. Coughing, because of congestion of blood in the lungs.
E. Bradycardia, because of decreased sympathetic stimulation.
D. Coughing, because of congestion of blood in the lungs.