1. Endo/Repro Exam 2: Male Reproductive System (Dr. Leavis)
1/95
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
96 Terms
Define the following:
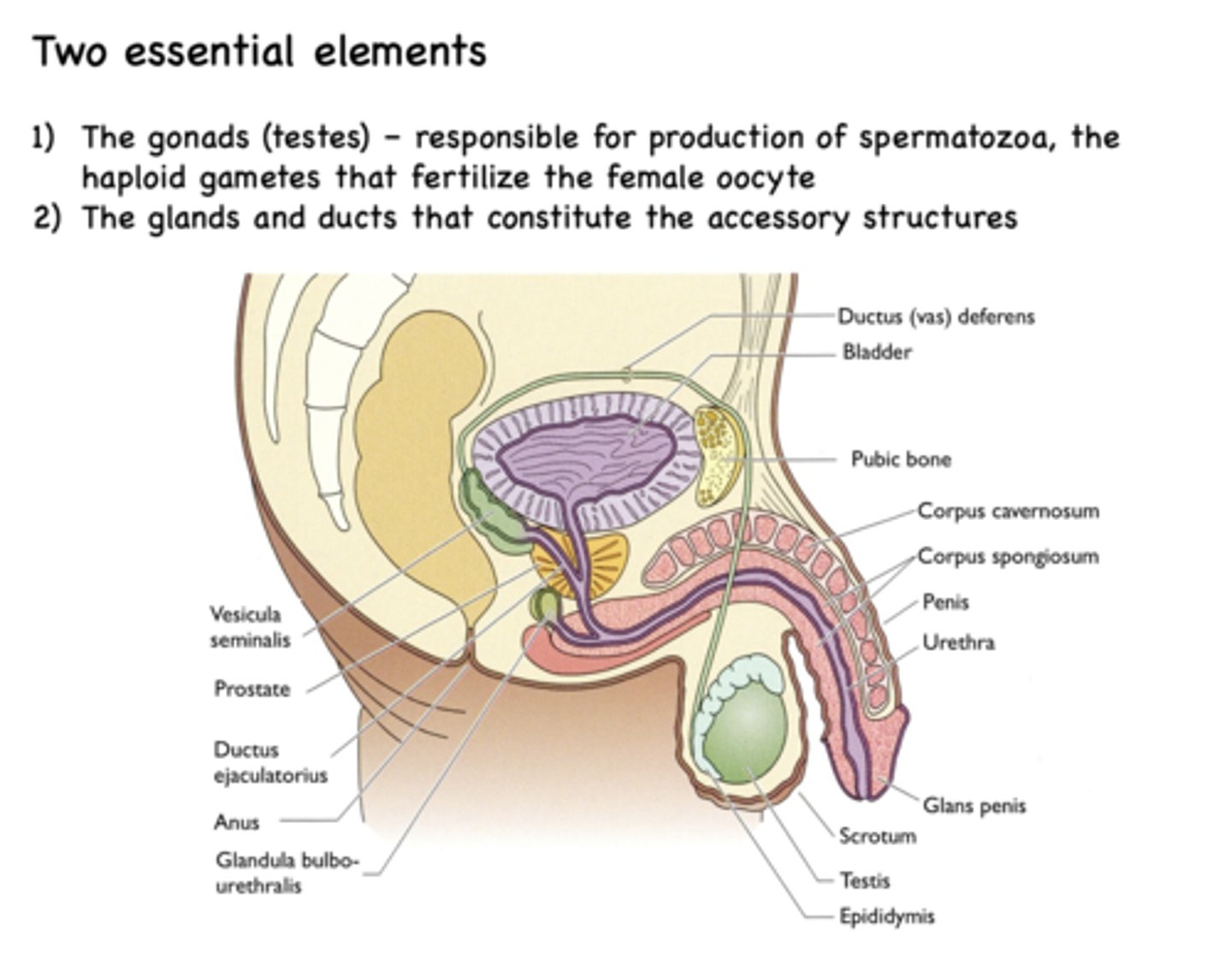
Responsible for production of spermatozoa, the haploid gametes that fertilize the female oocyte
Gonads (testes)
What is the testis largely composed of?
seminiferous tubules
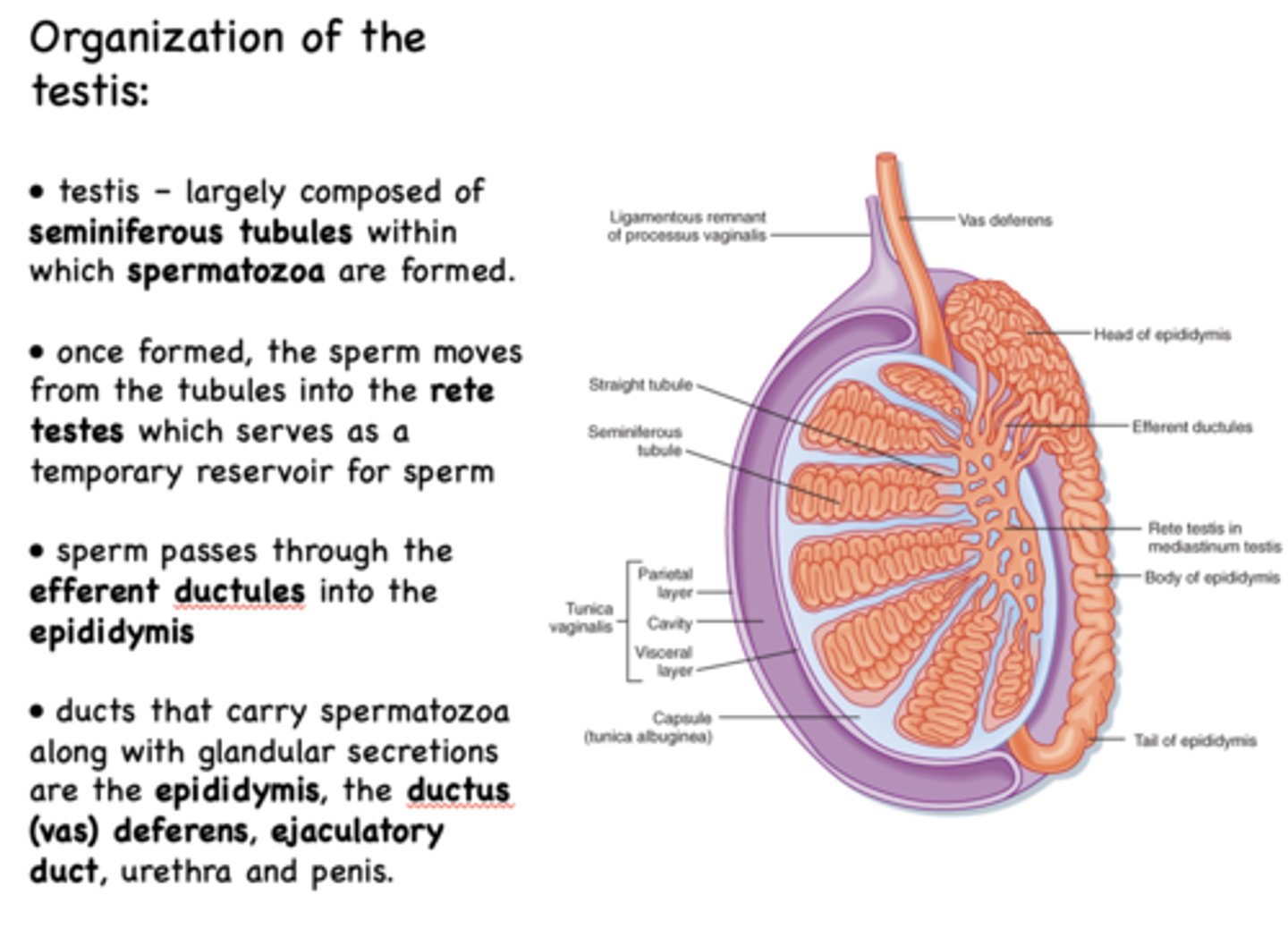
where are spermatozoa made?
seminiferous tubules
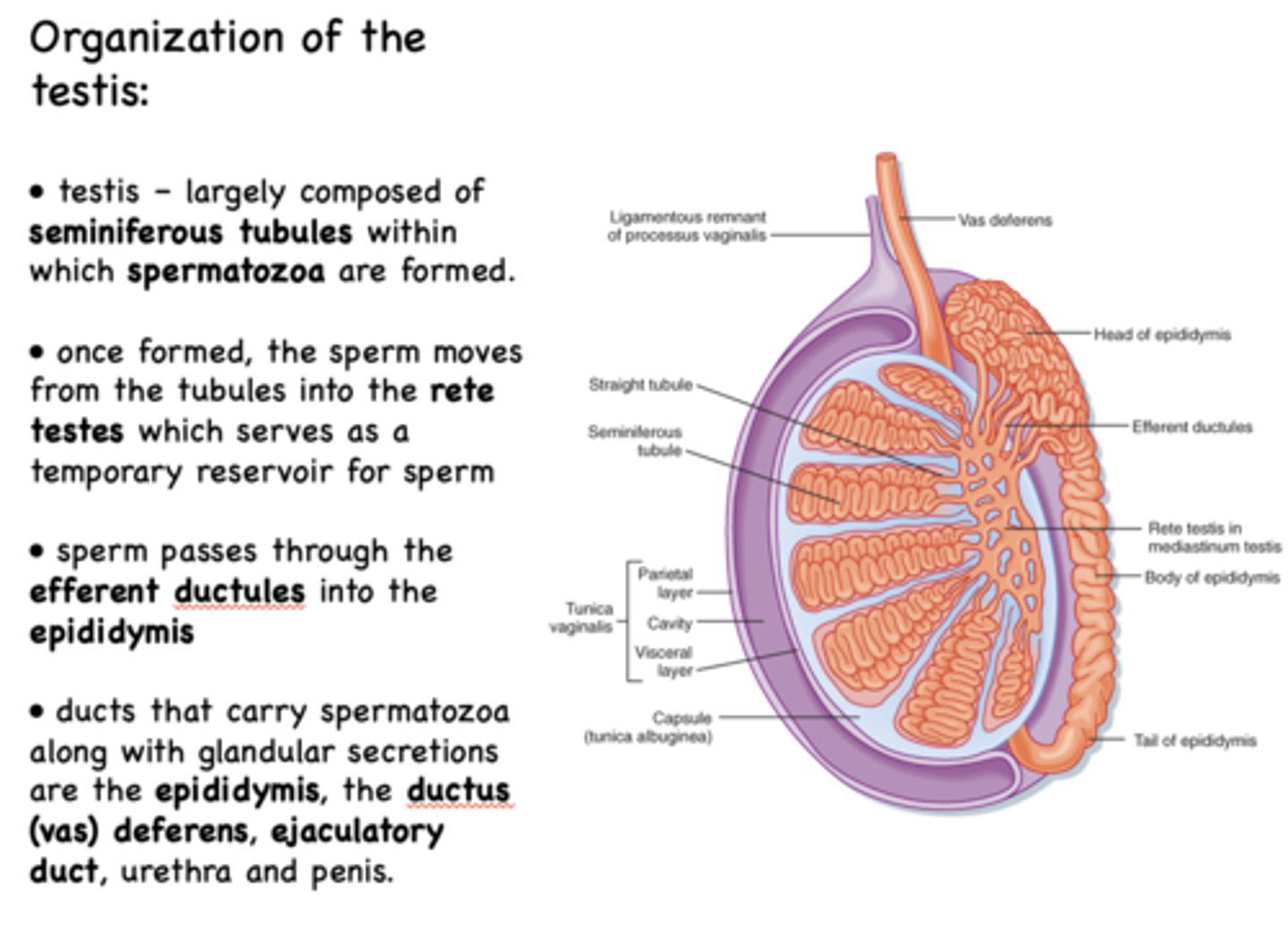
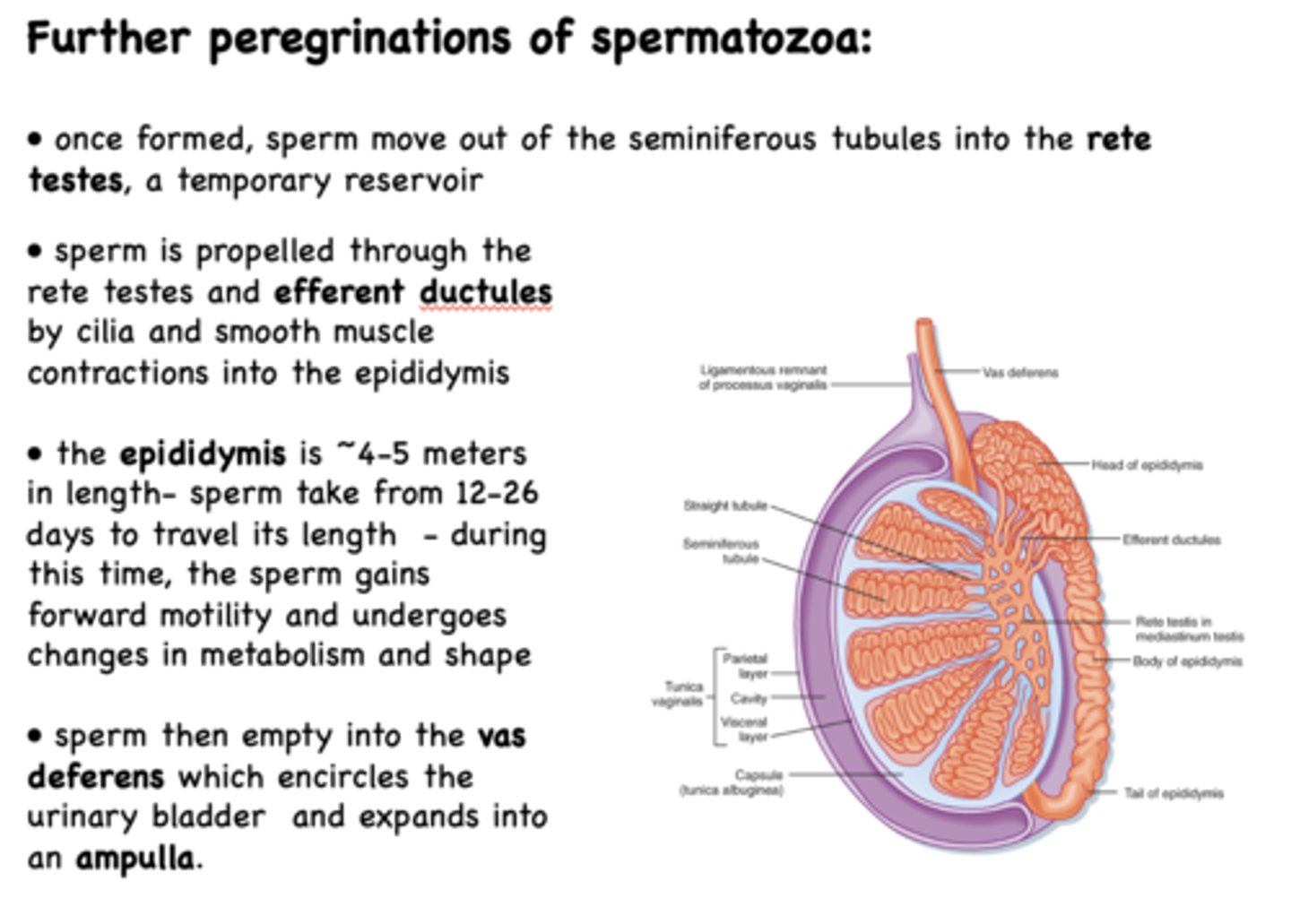
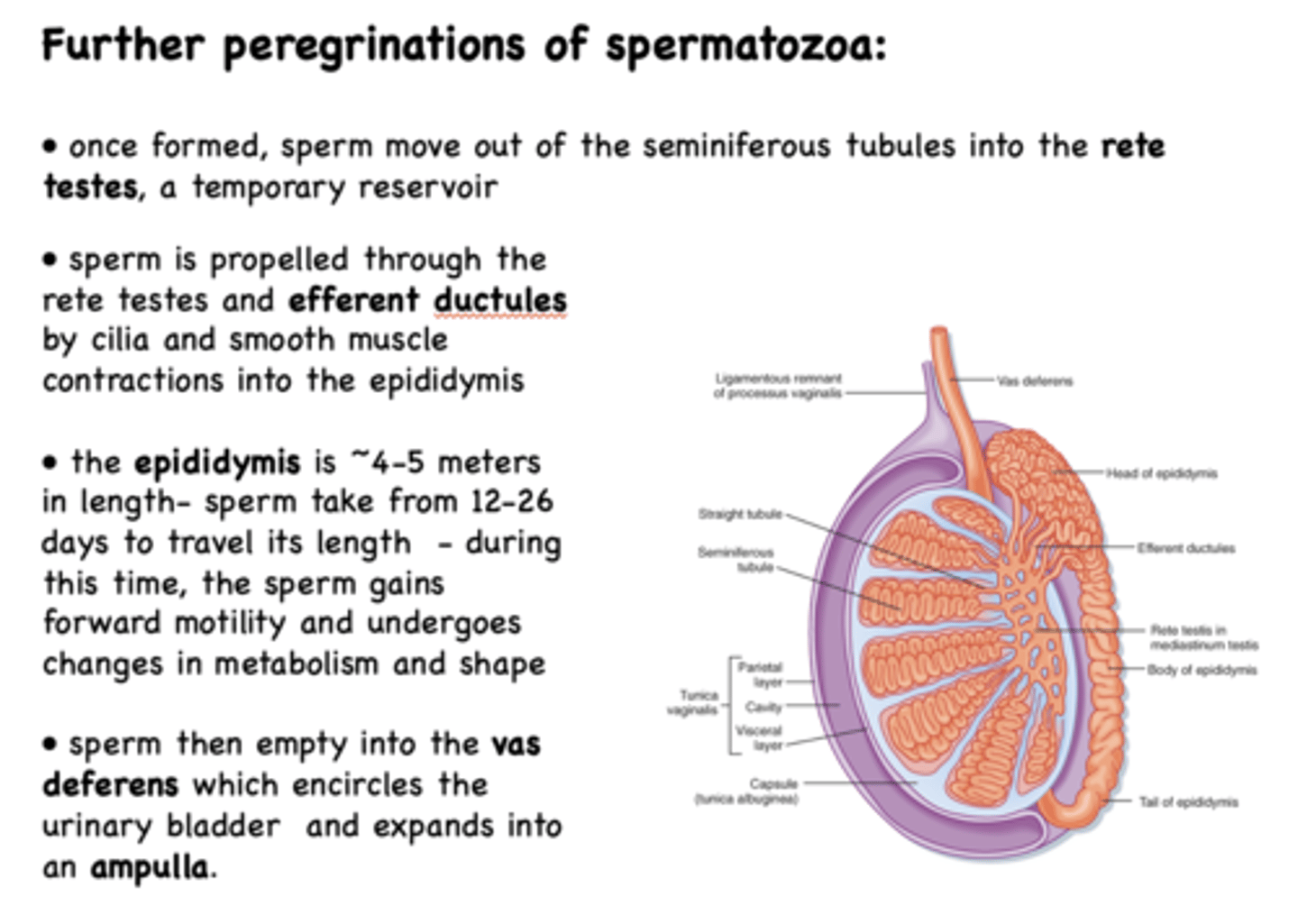
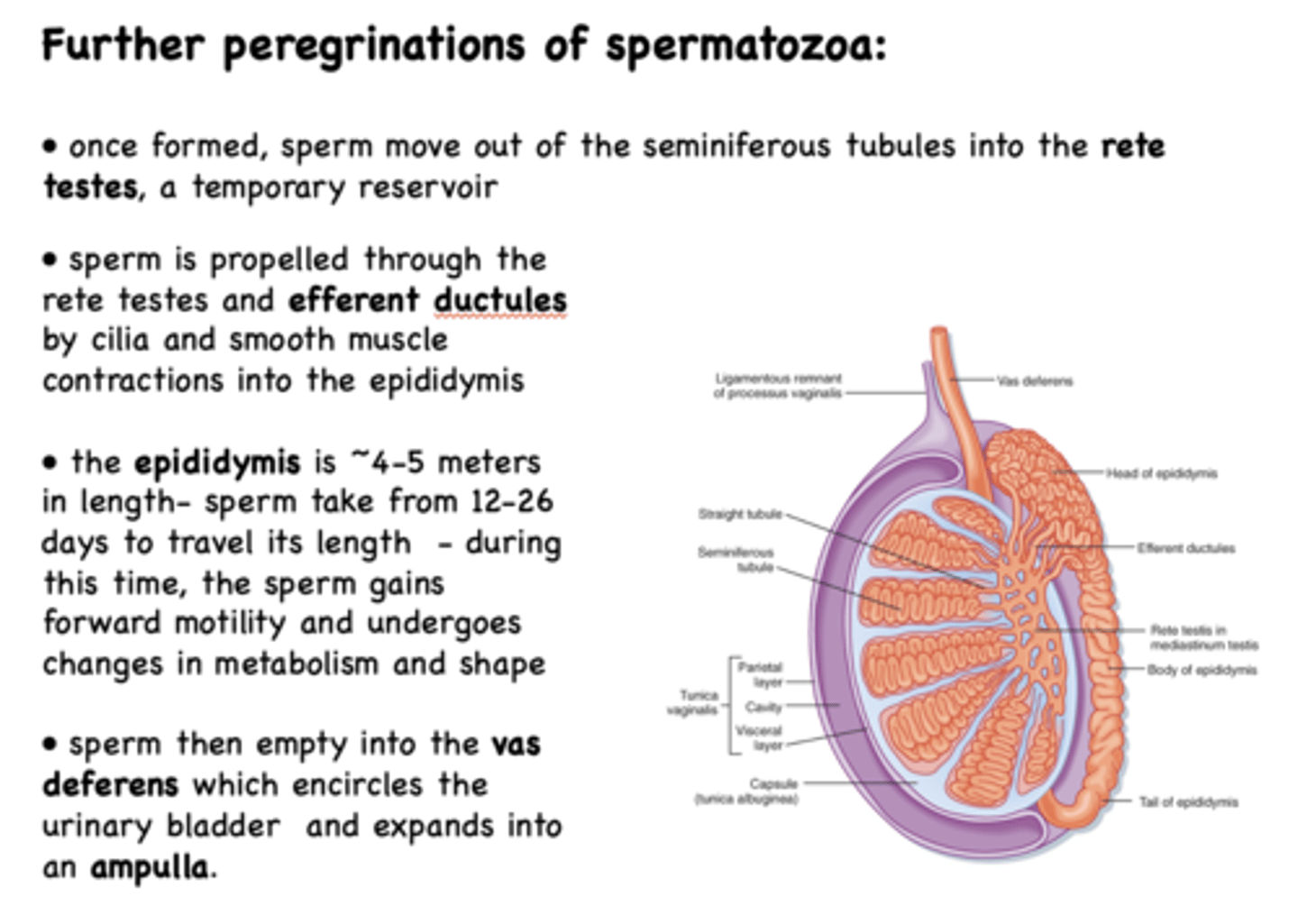
once formed in the seminiferous tubules, the sperm moves from the tubules into the _______ which serves as a temporary reservoir for sperm
rete testes

from the rete testes, sperm moves to the ______
efferent ductules
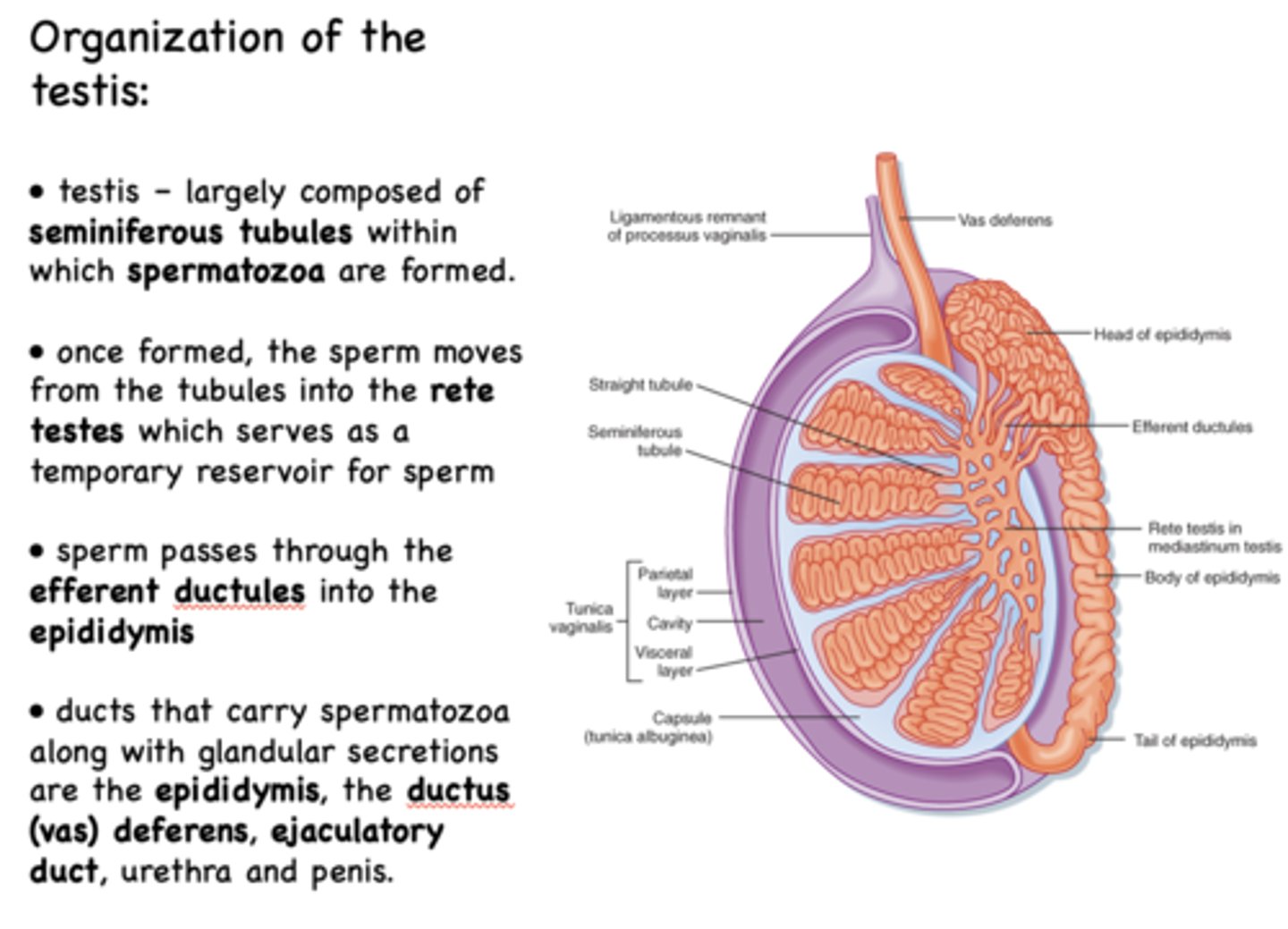
from the efferent ductules, sperm moves to the ______
epididymus
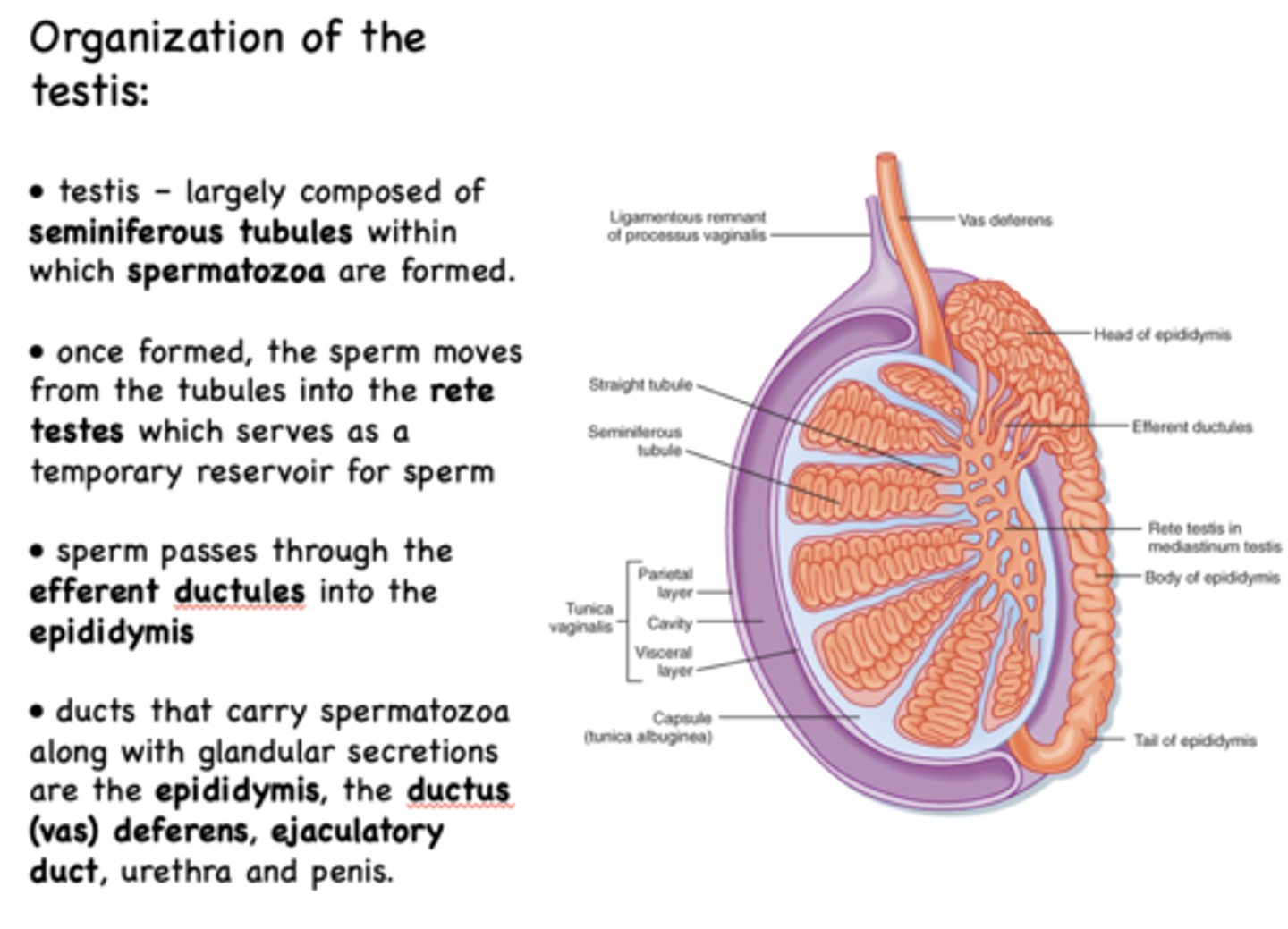
What are the ducts that carry spermatozoa along with glandular secretions?
- Epididymis
- Ductus (vas) deferens
- Ejaculatory duct
- Urethra
- Penis
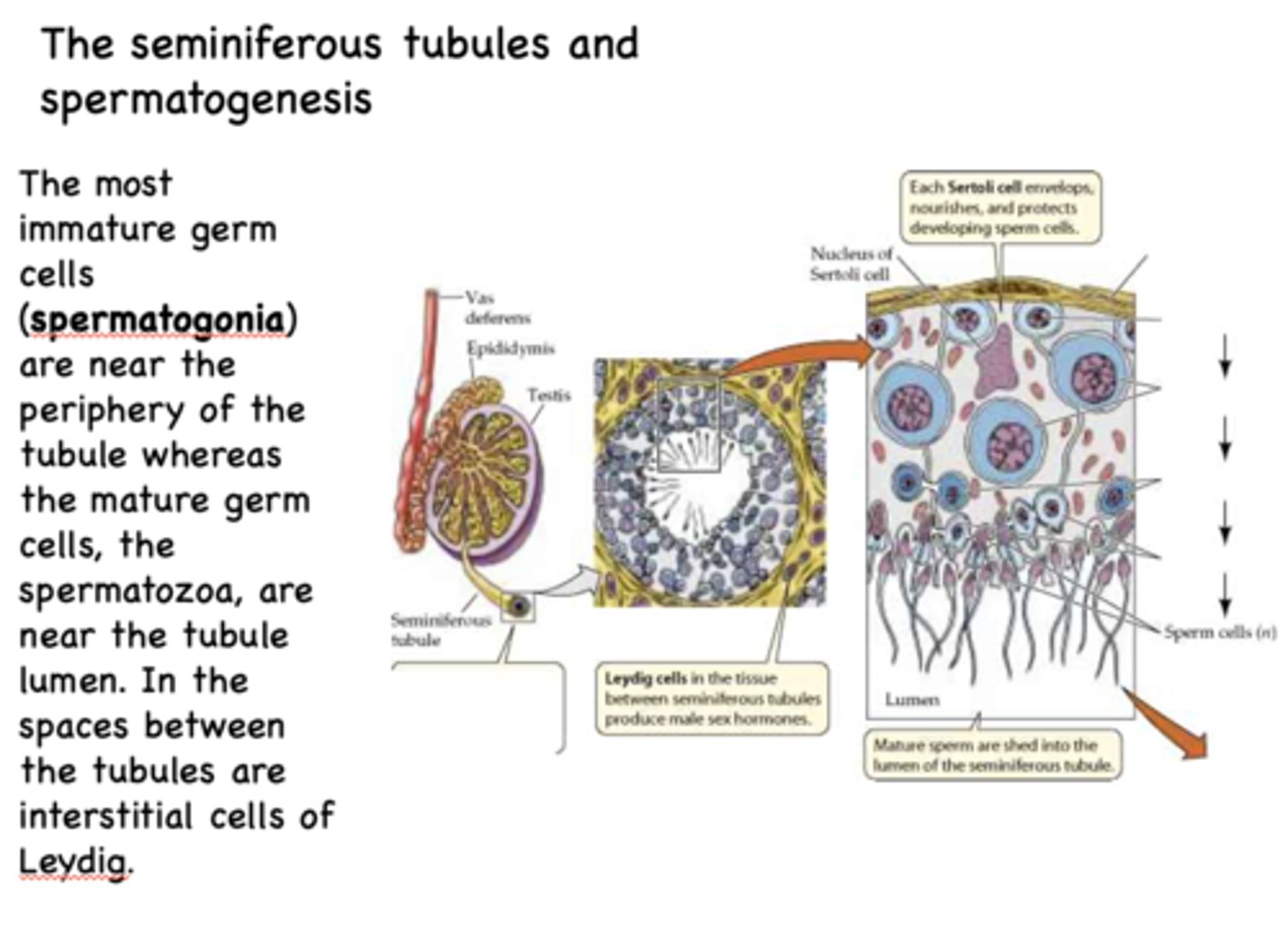
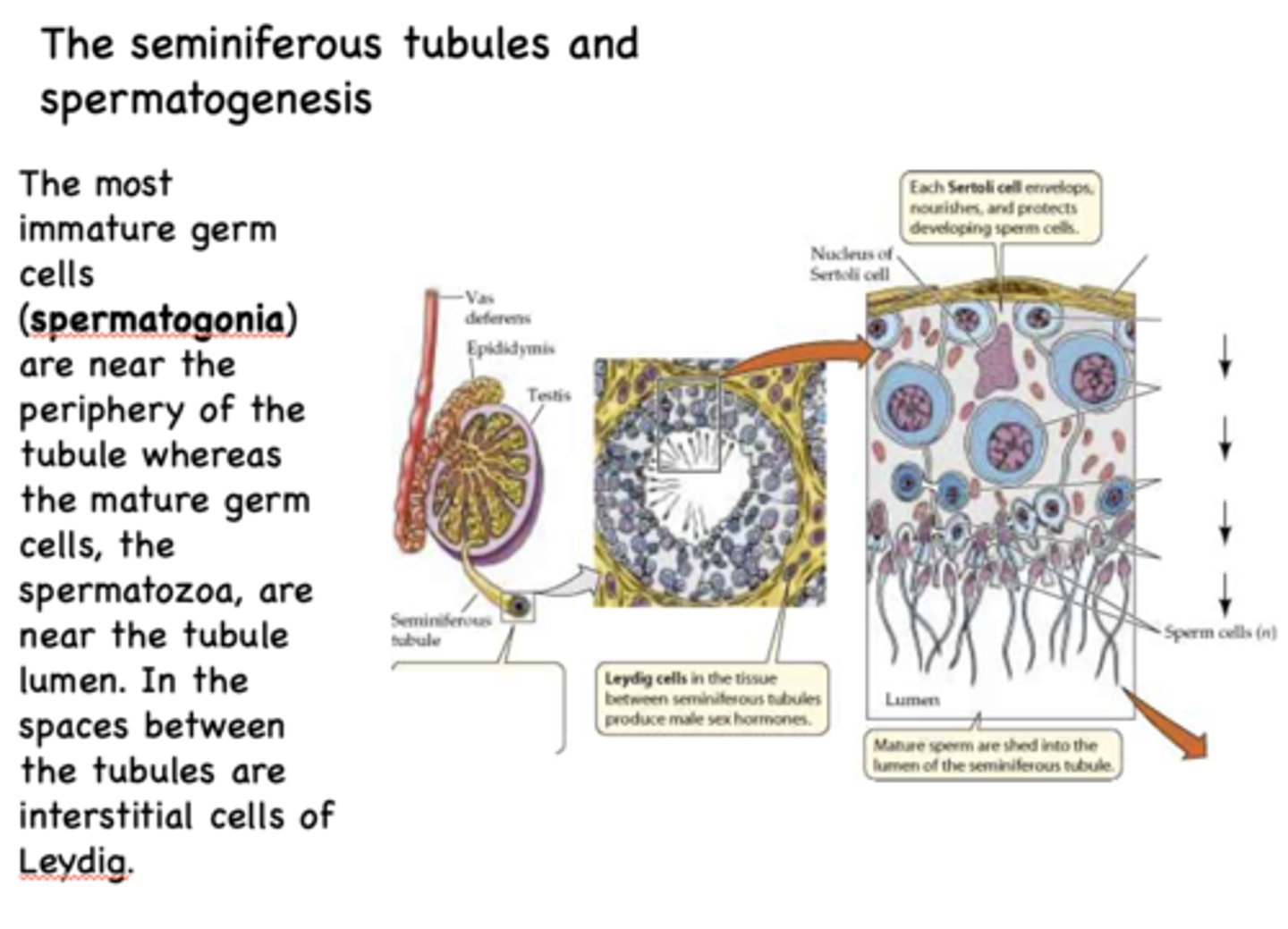
What is the most immature germ cells?
spermatogonia
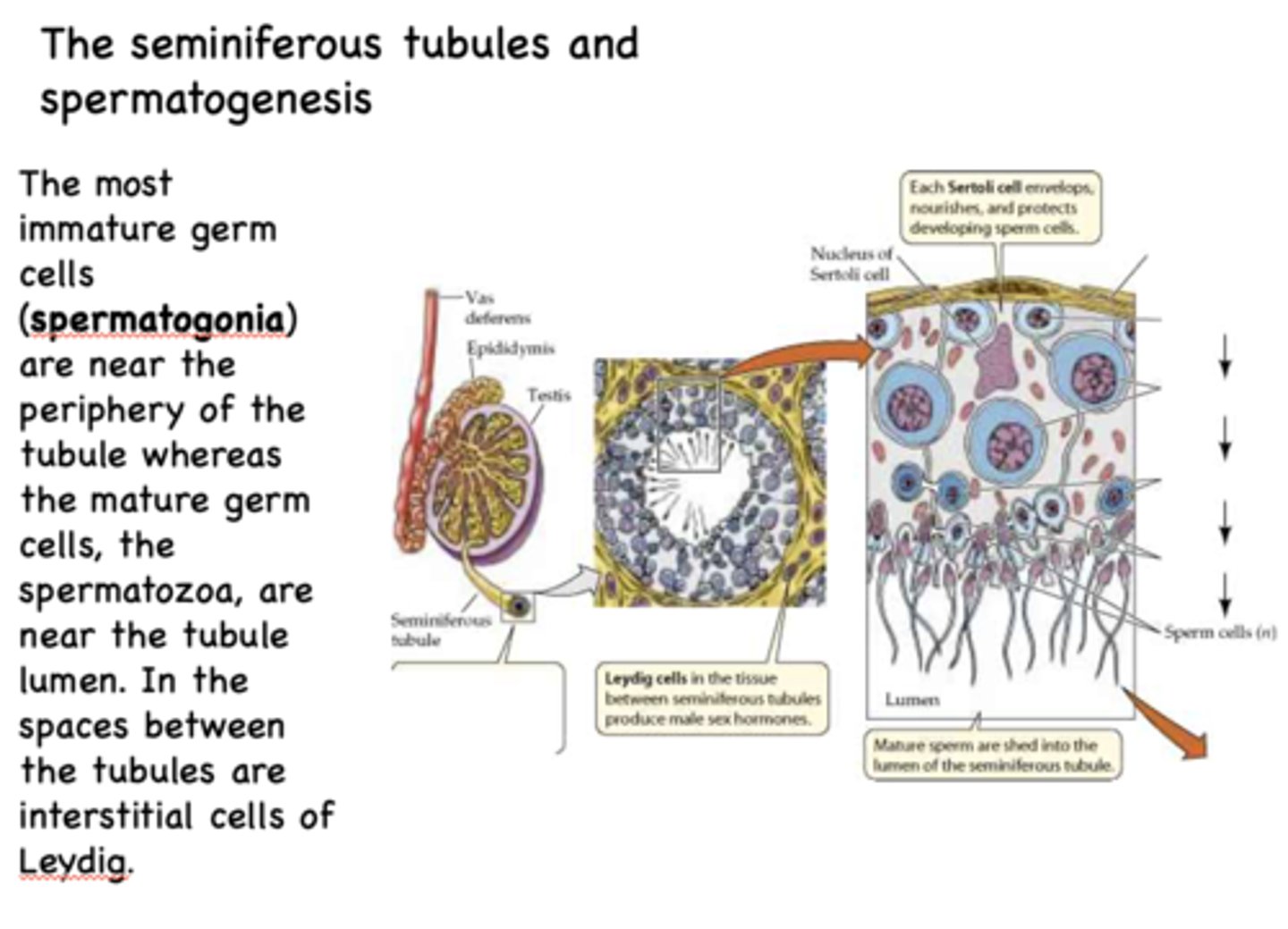
what stage of sperm would you expect to find near the periphery of the seminiferous tubules?
spermatogonia
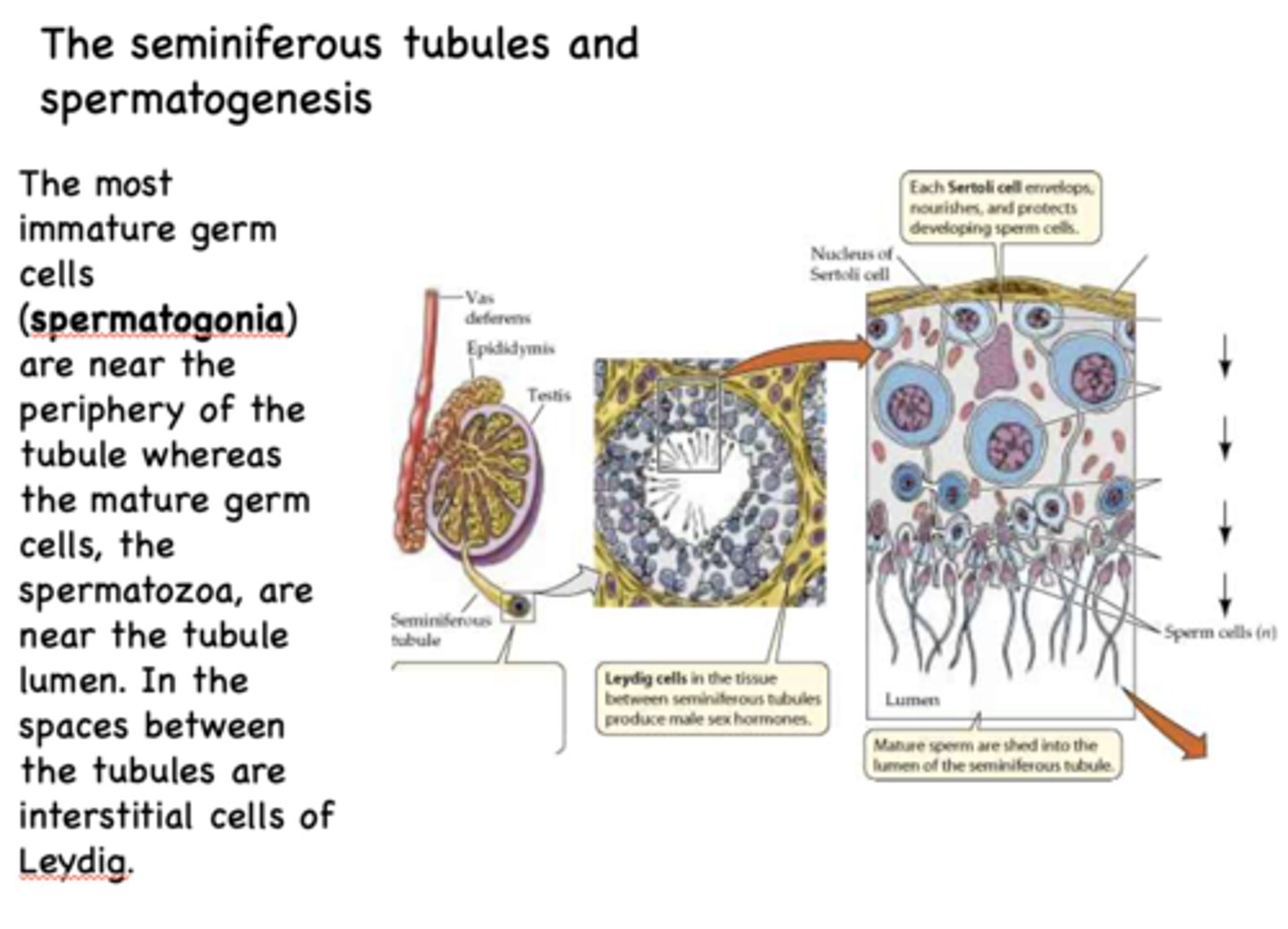
what stage of sperm would you expect to find near the lumen of the seminiferous tubules?
spermatozoa
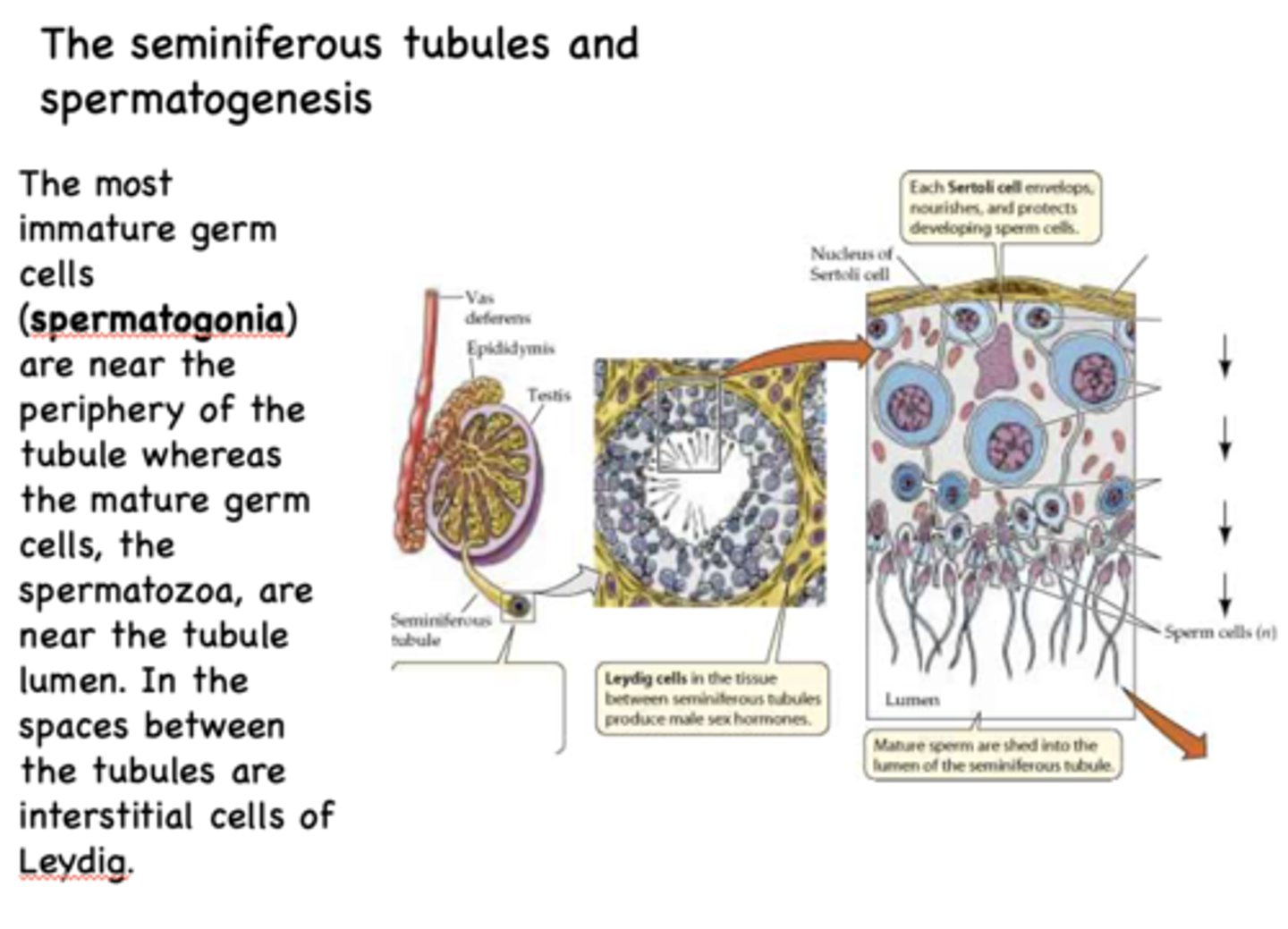
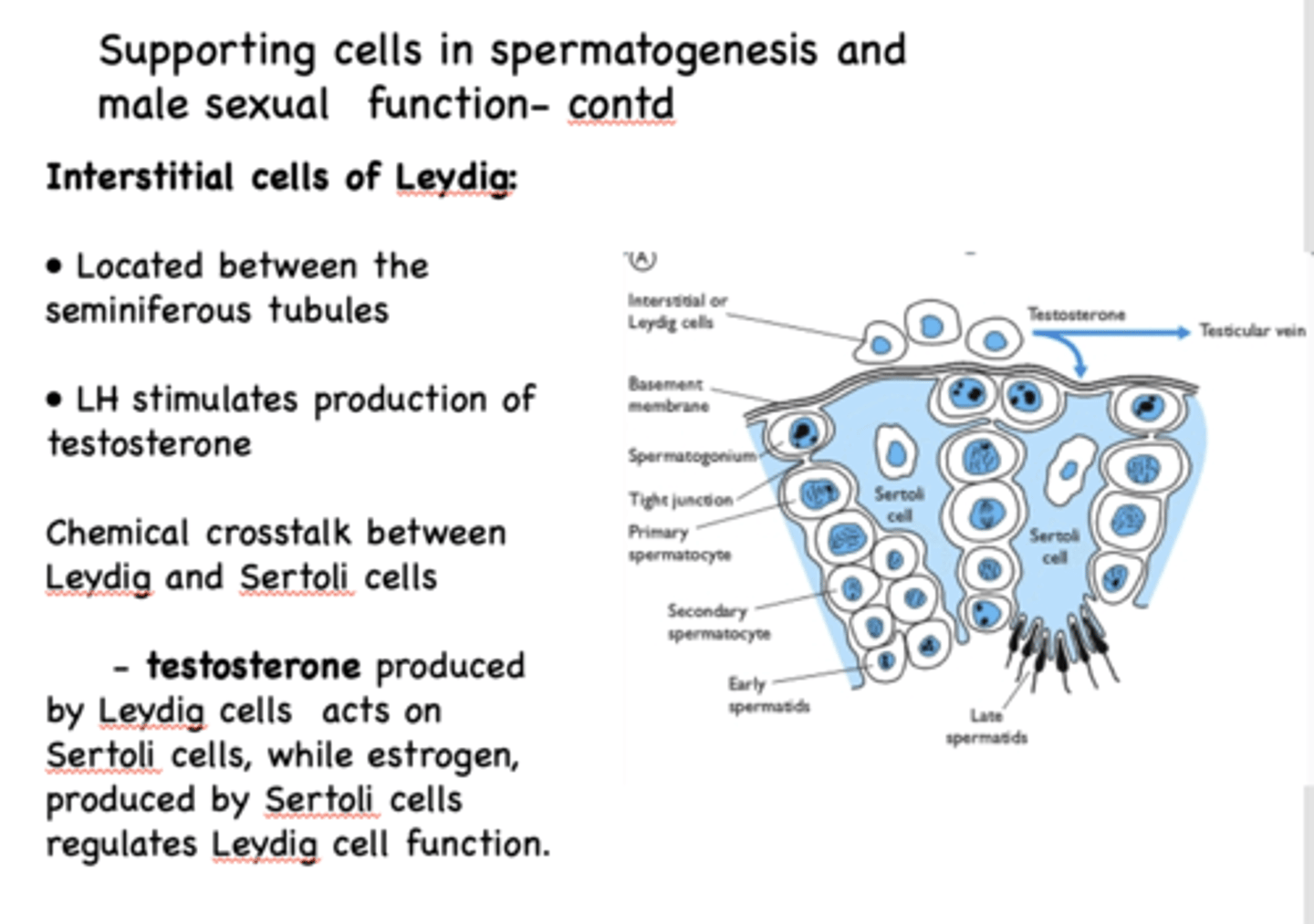
these interstitial cells sit in the spaces between the seminiferous tubules:
Leydig cells
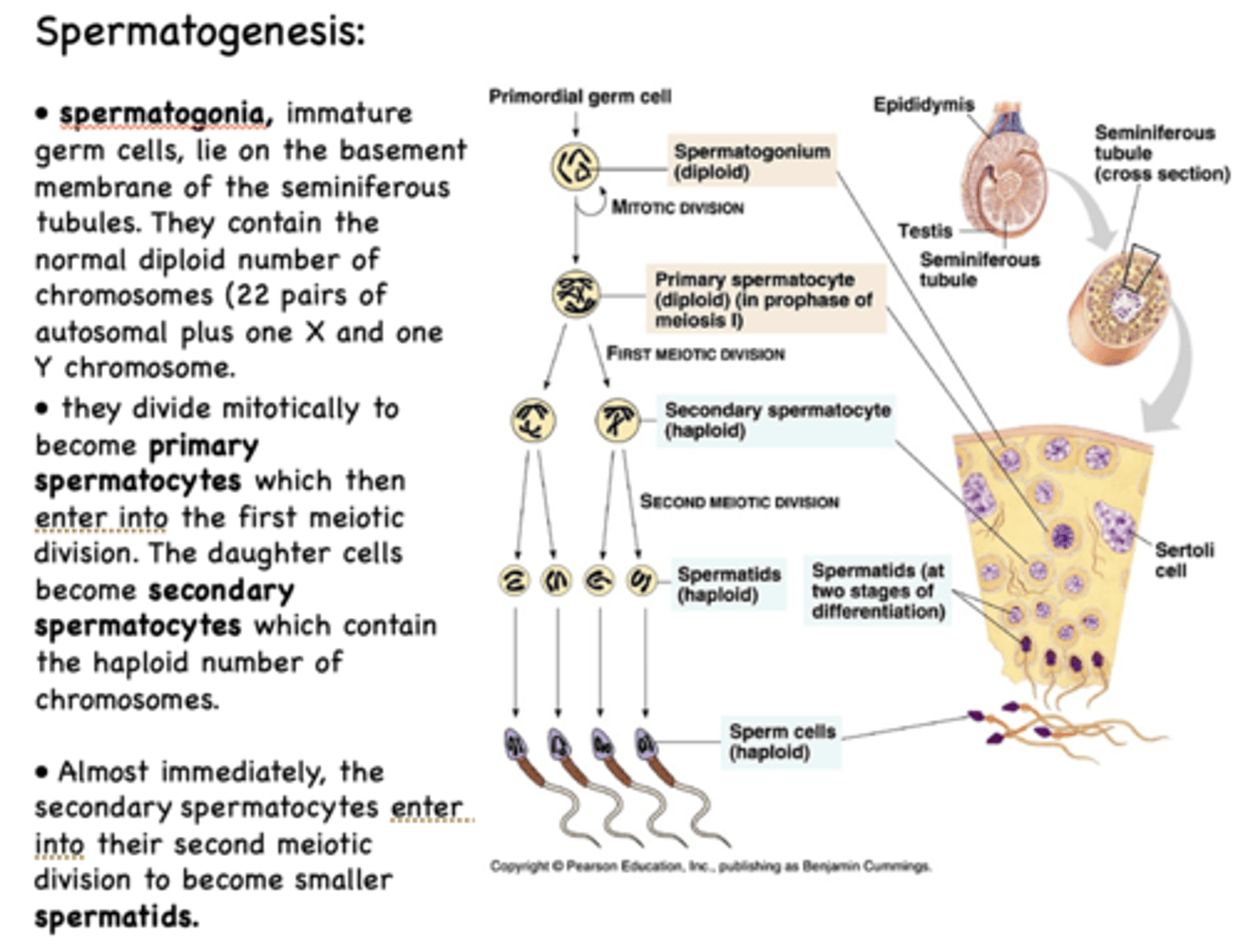
___________ are immature germ cells that lie on the basement membrane of the seminiferous tubules
Spermatogonia
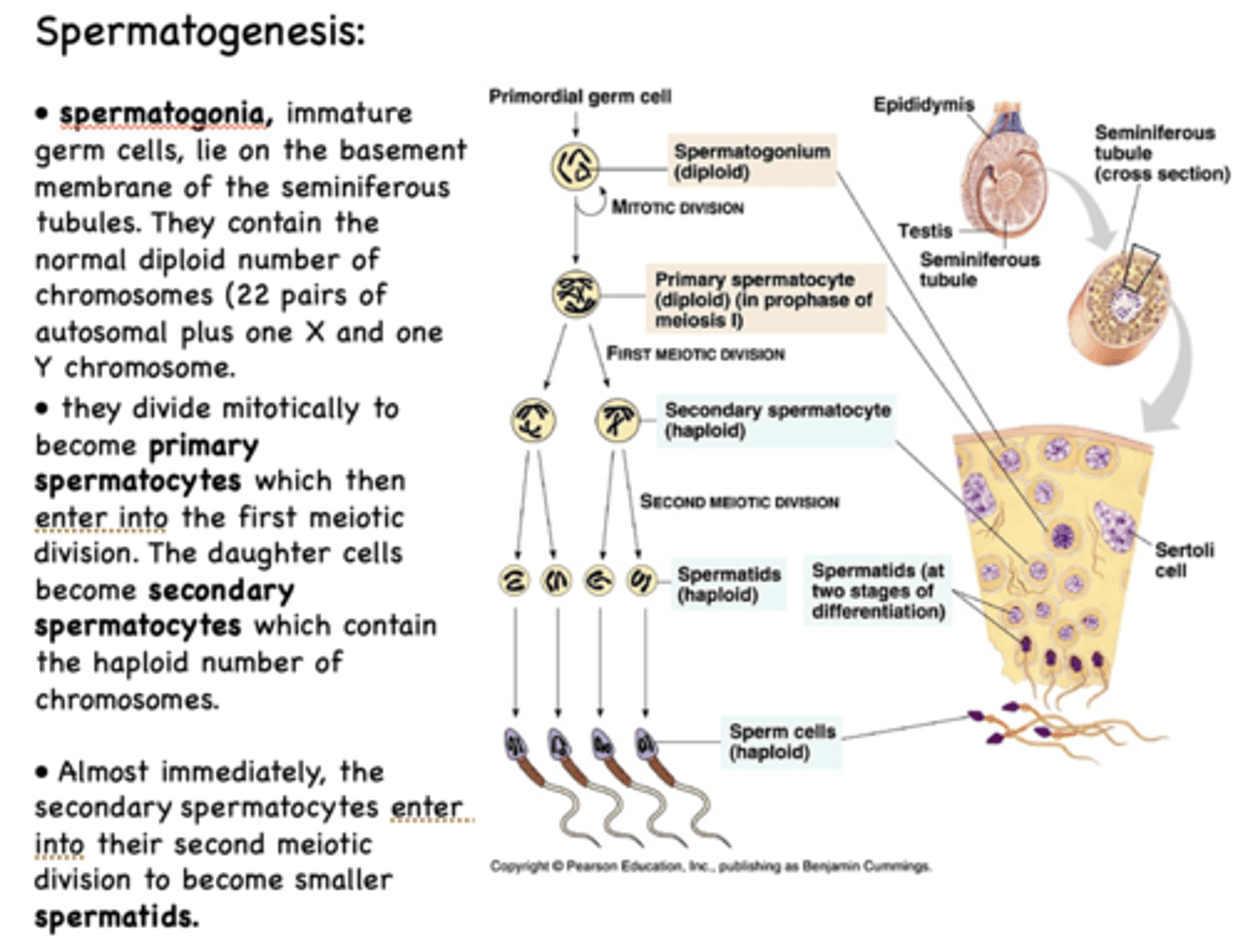
Spermatogonia contain the normal diploid number of chromosomes which is...
22 pairs of autosomal plus one X and one Y chromosome
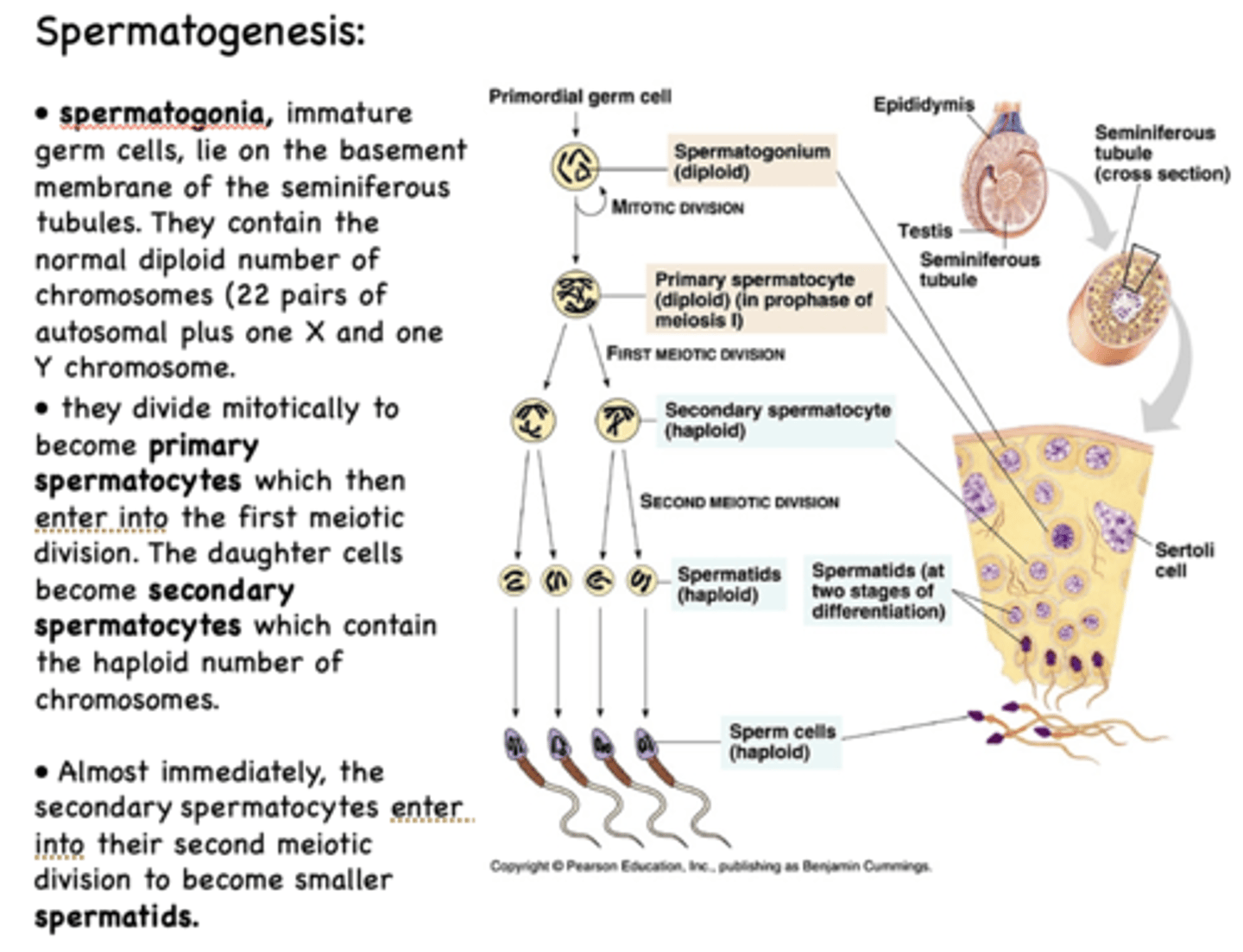
what process allows spermatogonia to become primary spermatocytes?
mitosis
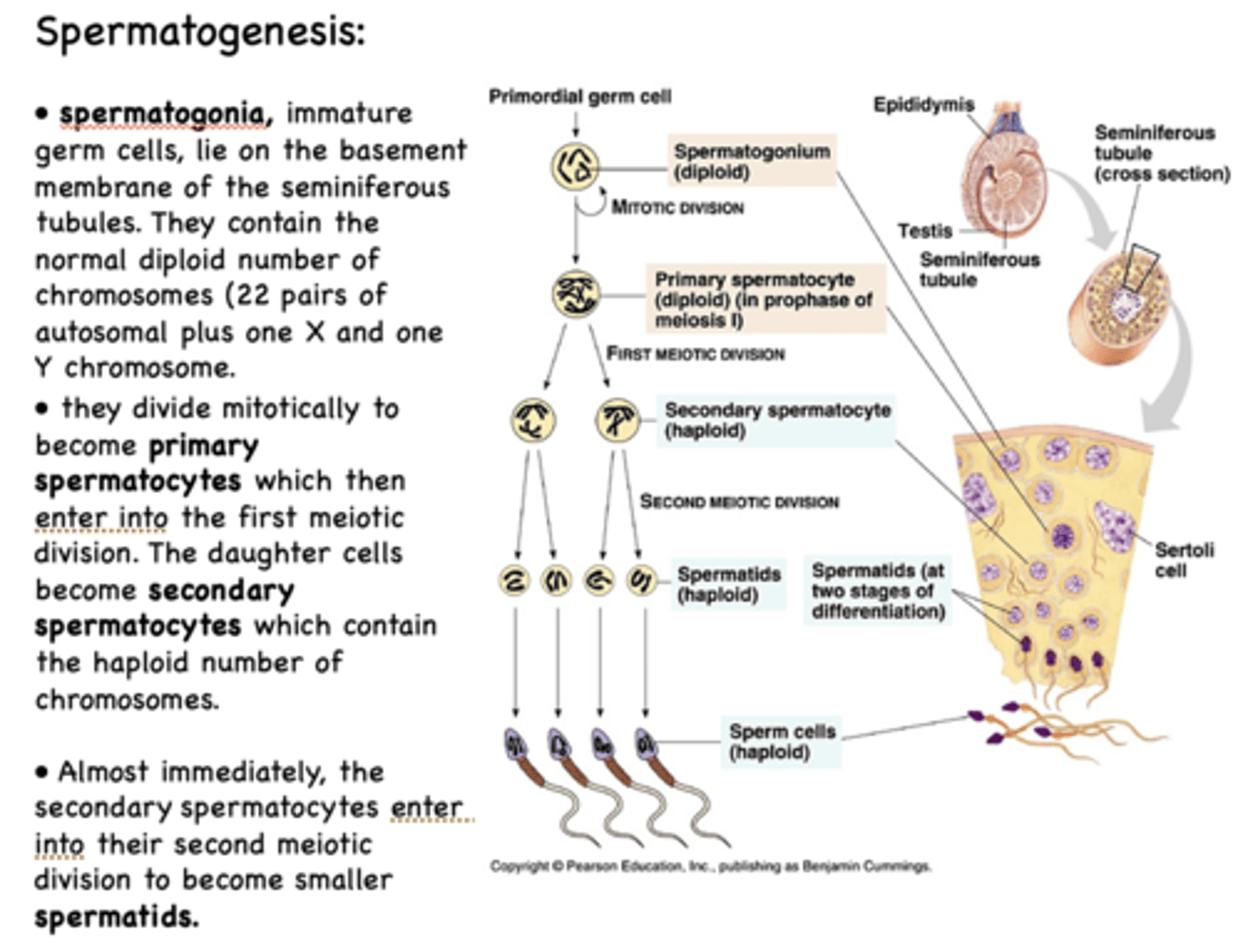
spermatogonia undergo mitosis to become ______________
primary spermatocytes
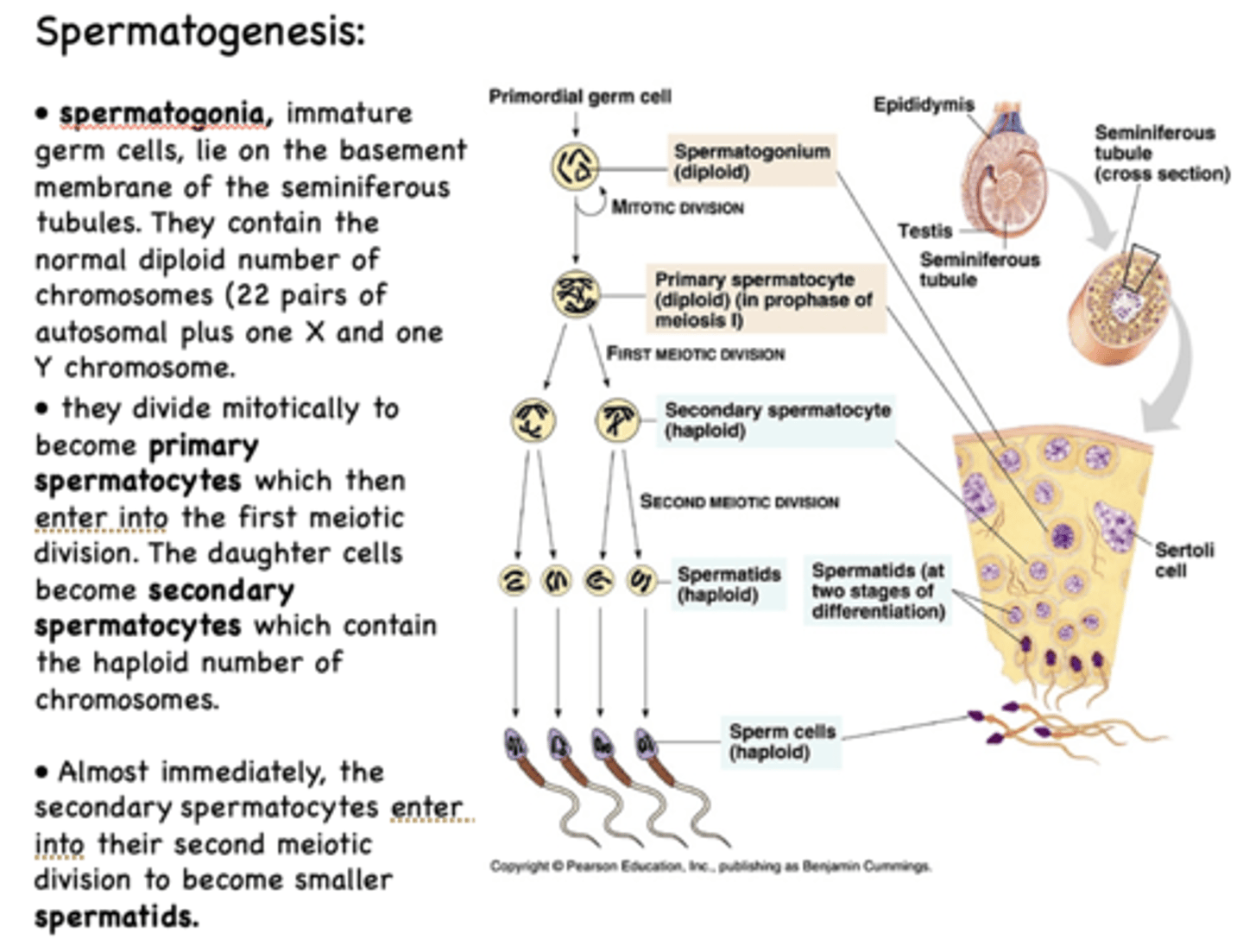
primary spermatocytes undergo ______________ to form daughter cells that are secondary spermatocytes
meiosis I
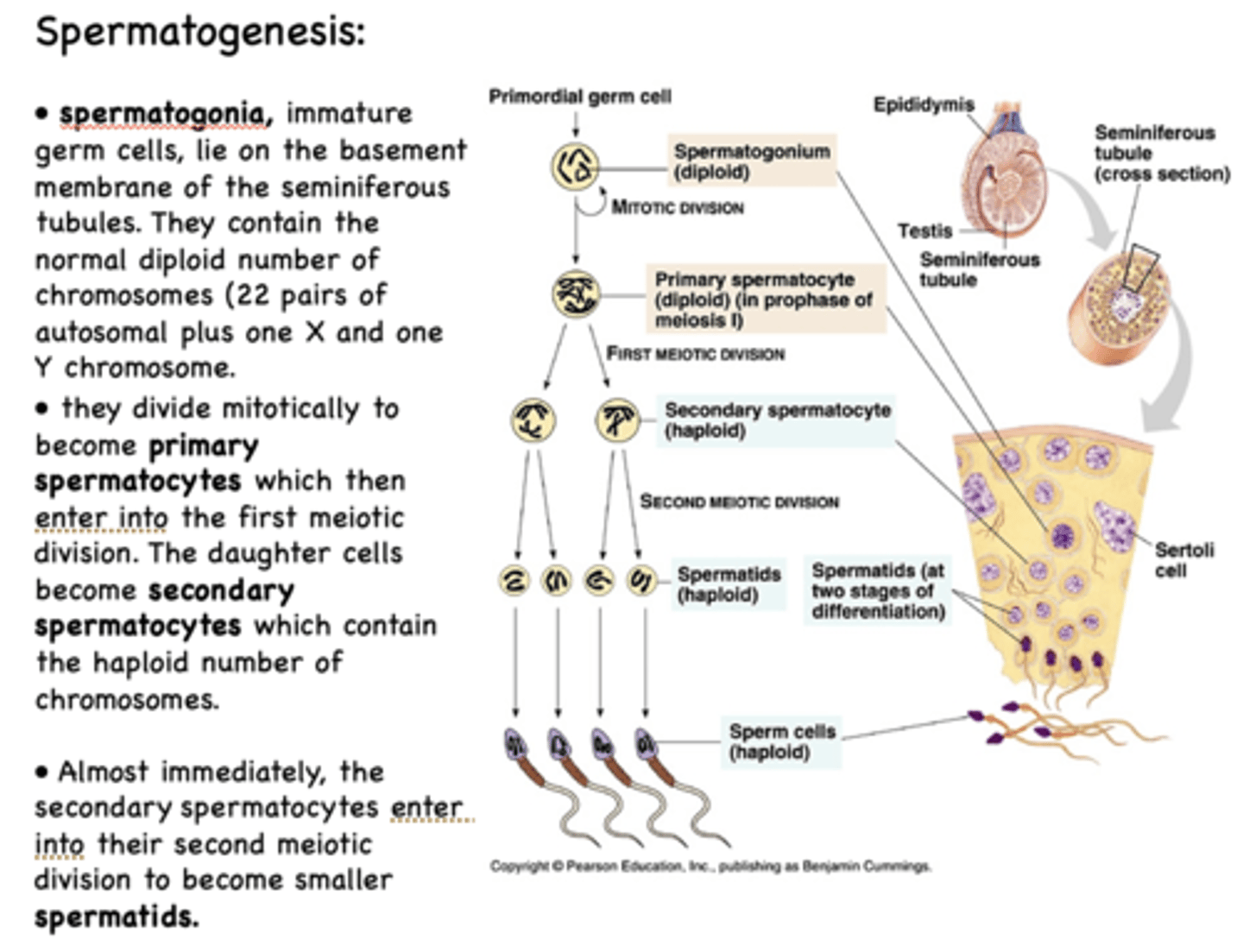
in terms of # of chromosomes, the spermatogonia is a ______________ cell
diploid
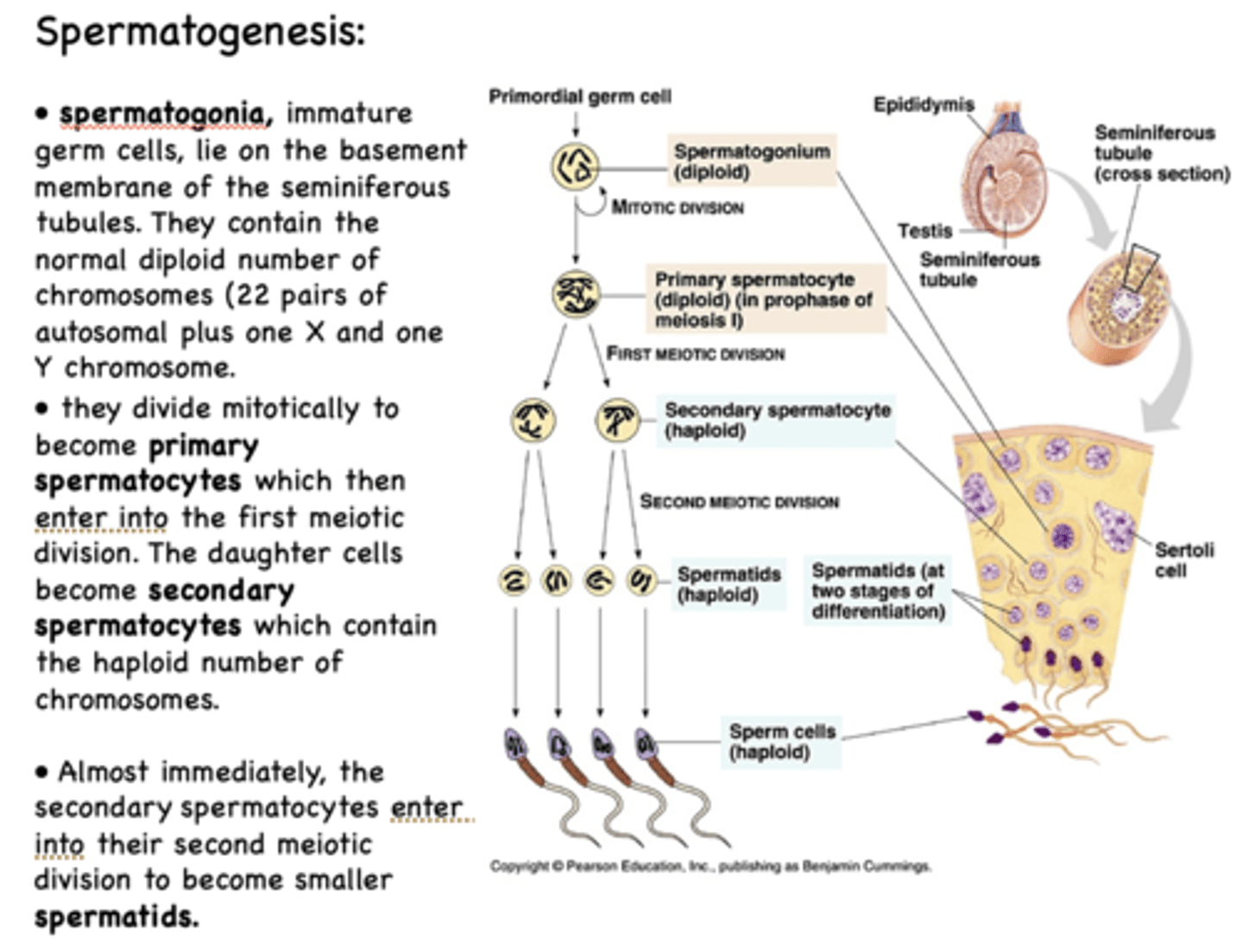
in terms of # of chromosomes, the primary spermatocyte is a ______________ cell
diploid
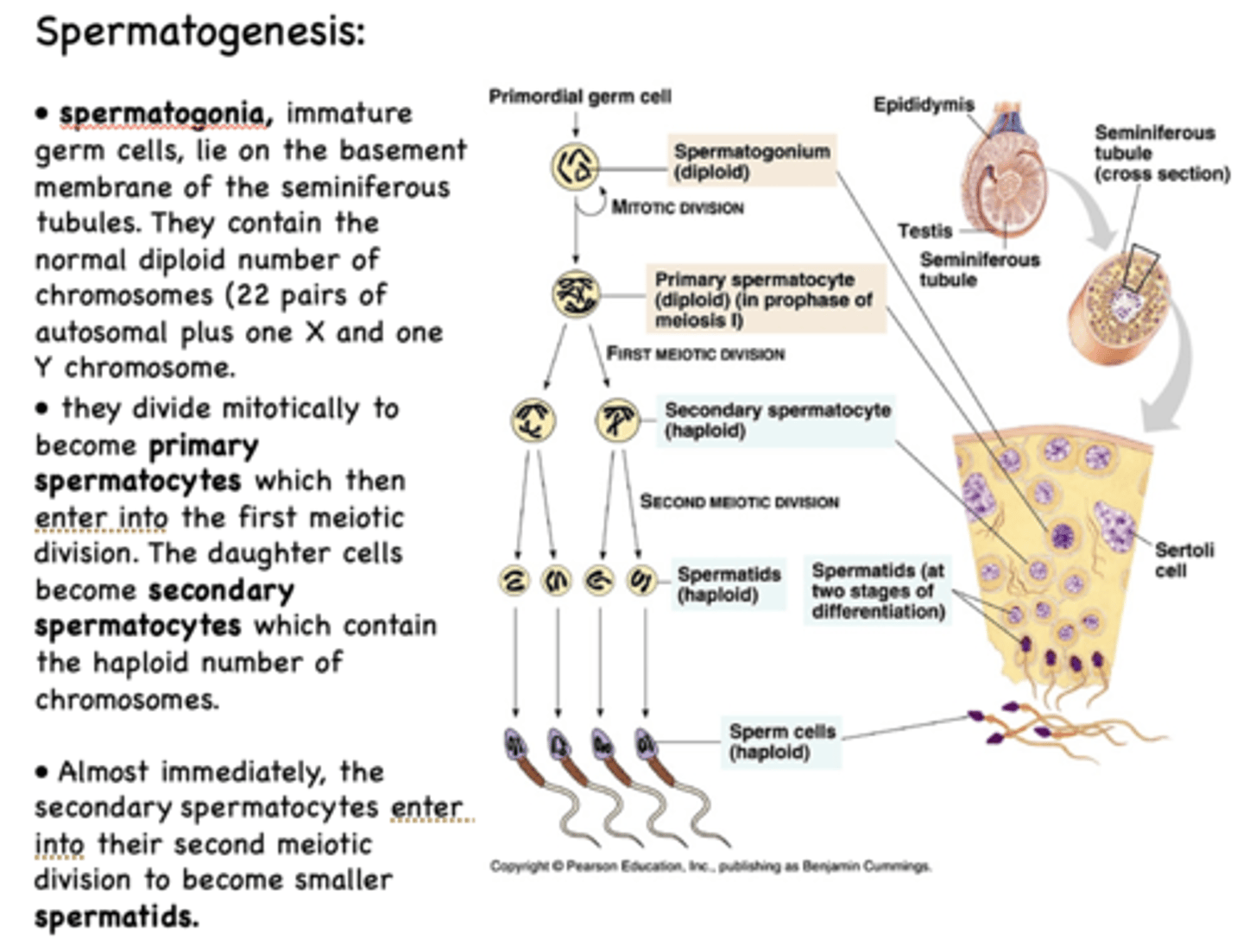
in terms of # of chromosomes, the secondary spermatocyte is a ______________ cell
haploid
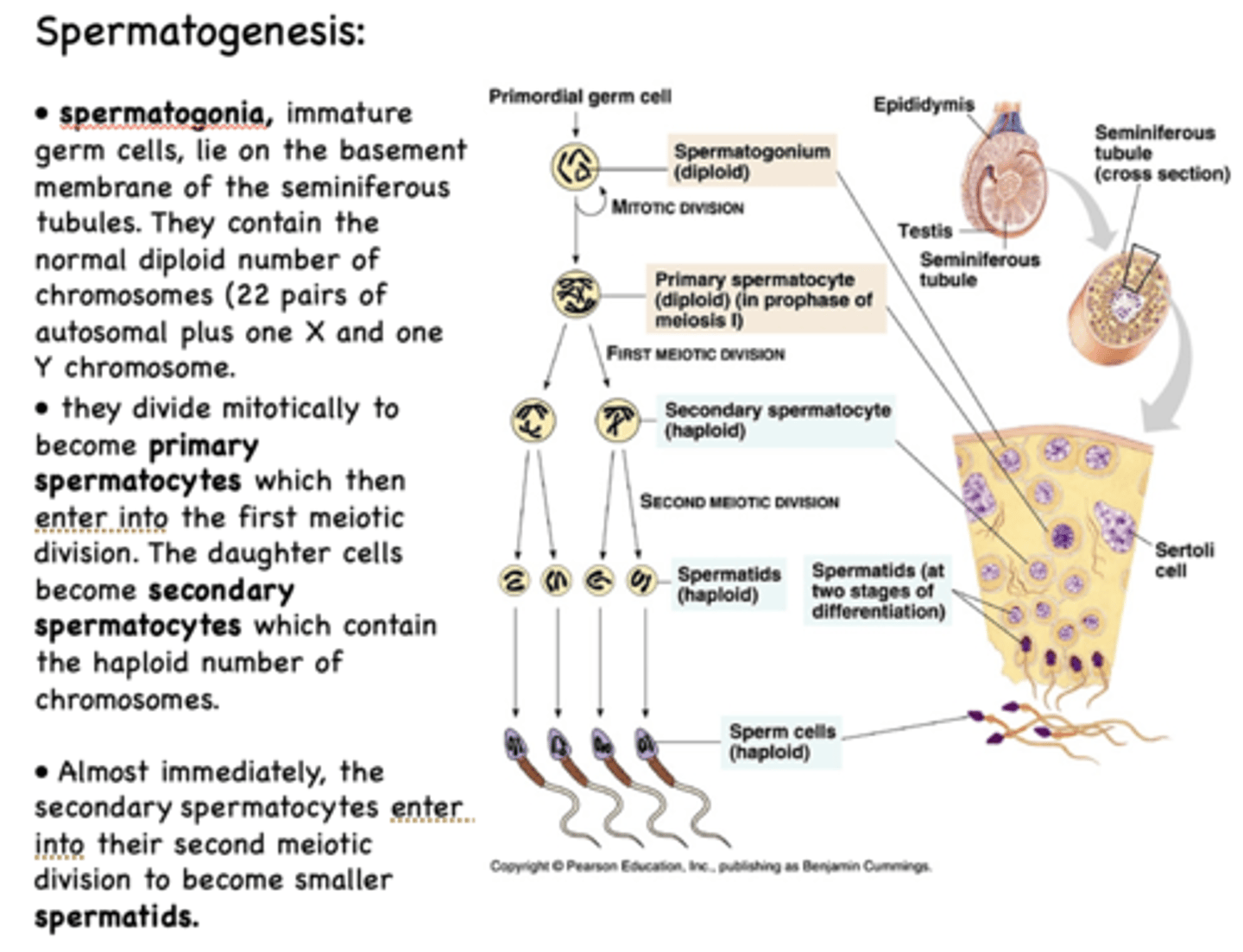
in terms of # of chromosomes, the spermatid is a ______________ cell
haploid
secondary spermatocyte undergo a second round of ______________ to become spermatids
meiosis
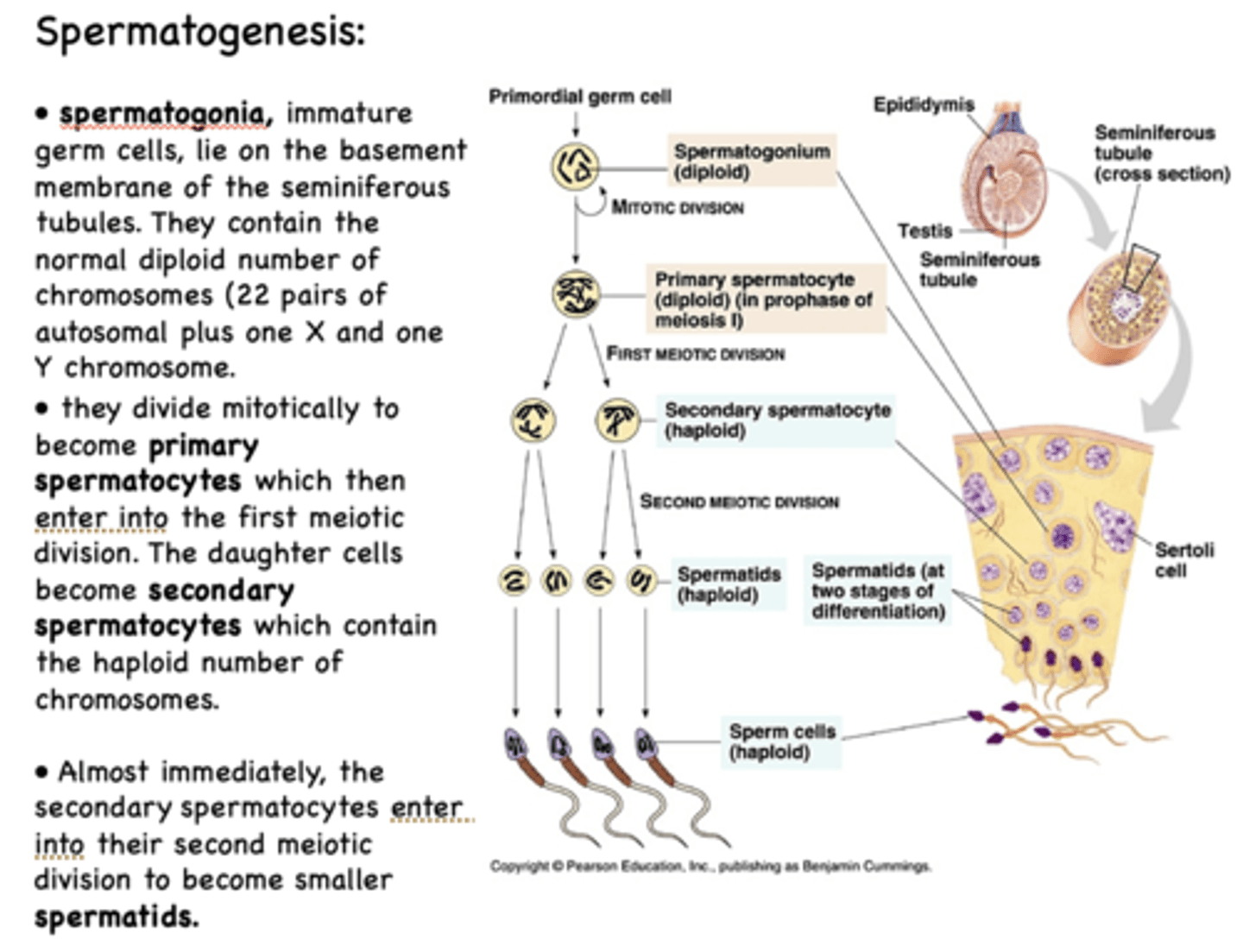
secondary spermatocyte undergo a second round of meiosis to become ______
spermatids
Define the following:
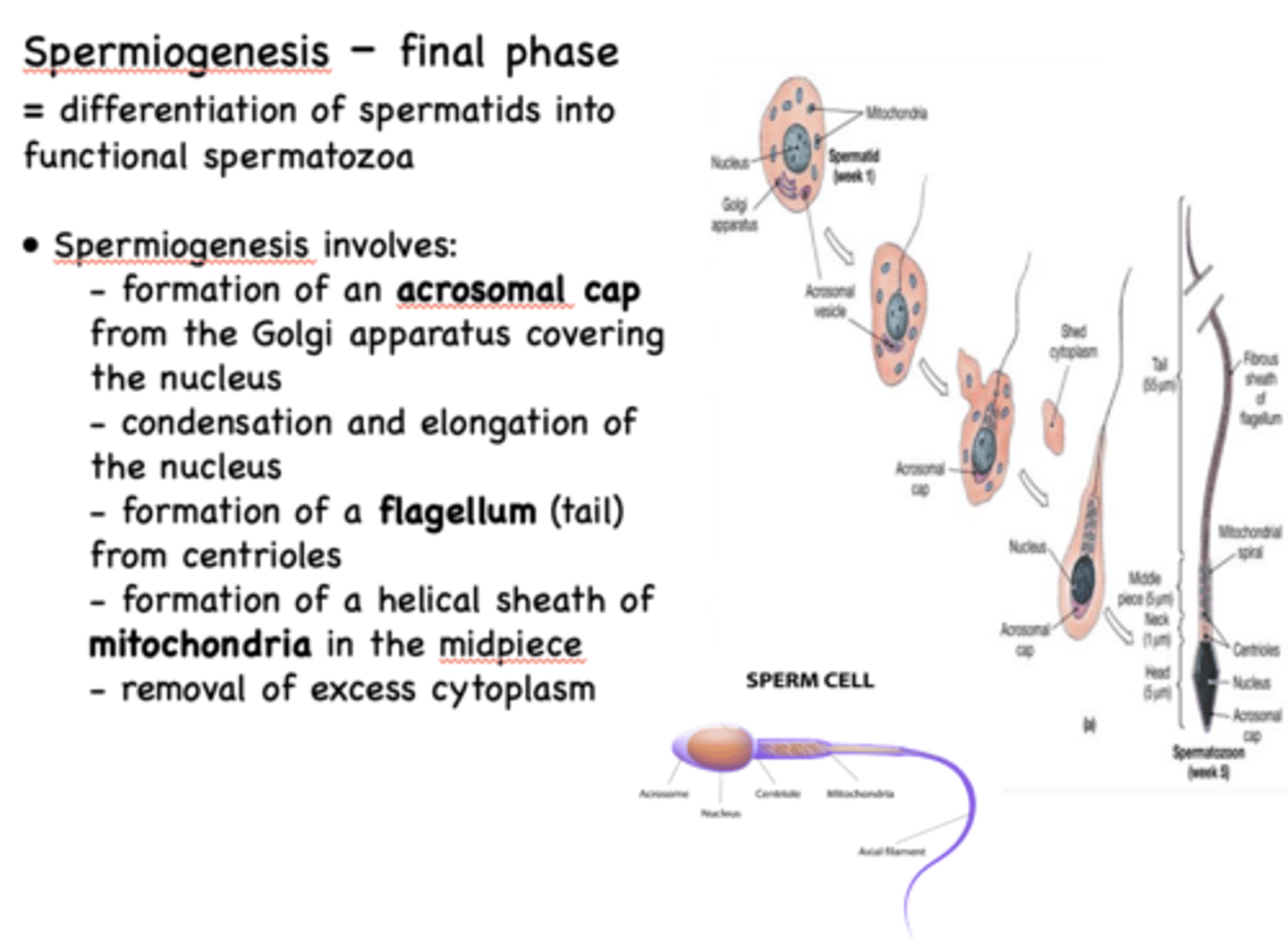
The differentiation of spermatids into functional spermatozoa
spermiogenesis
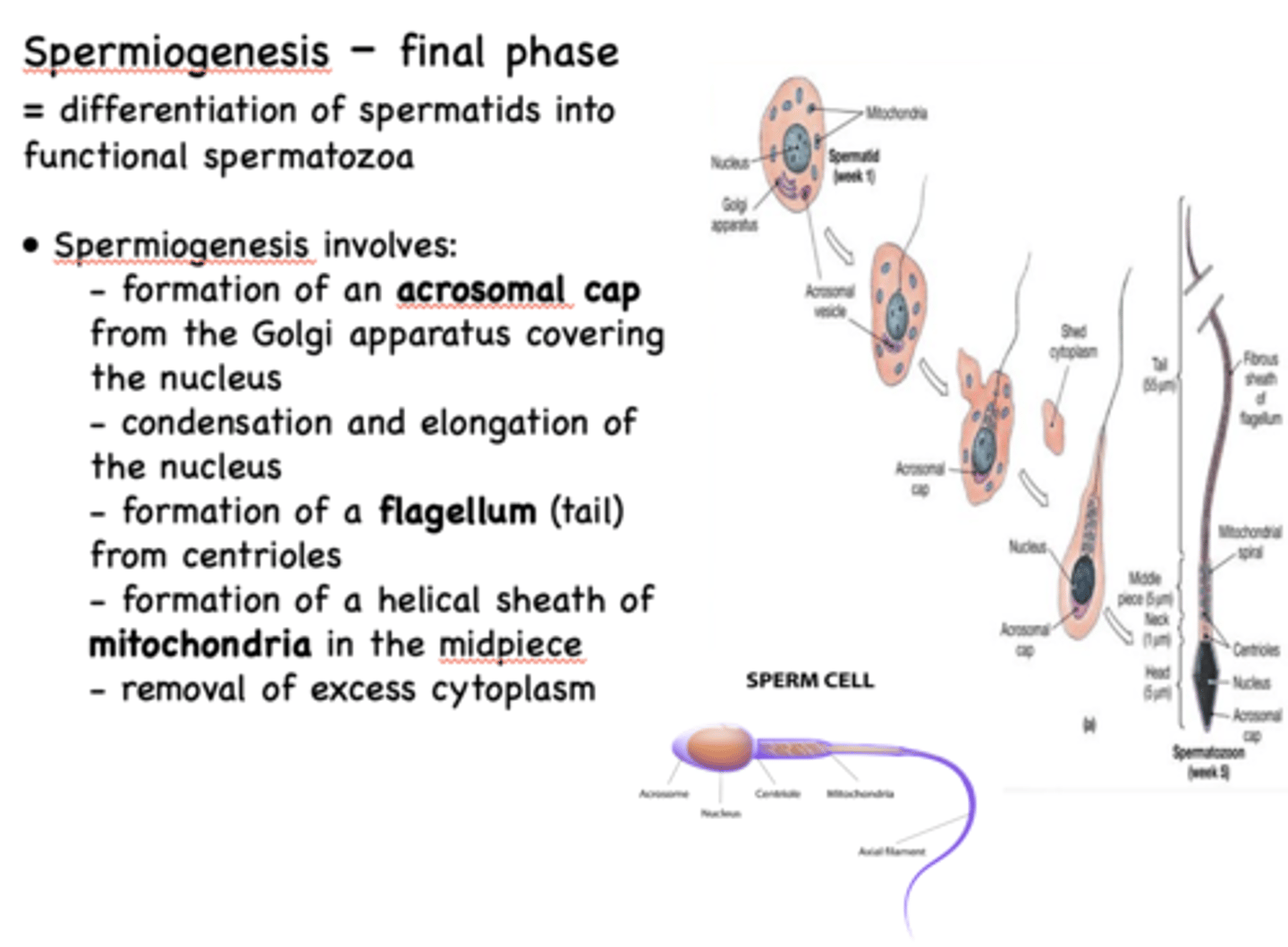
Spermiogenesis involves the formation of 3 main structures:
- Acrosomal cap
- Flagellum
- Helical sheath of mitochondria
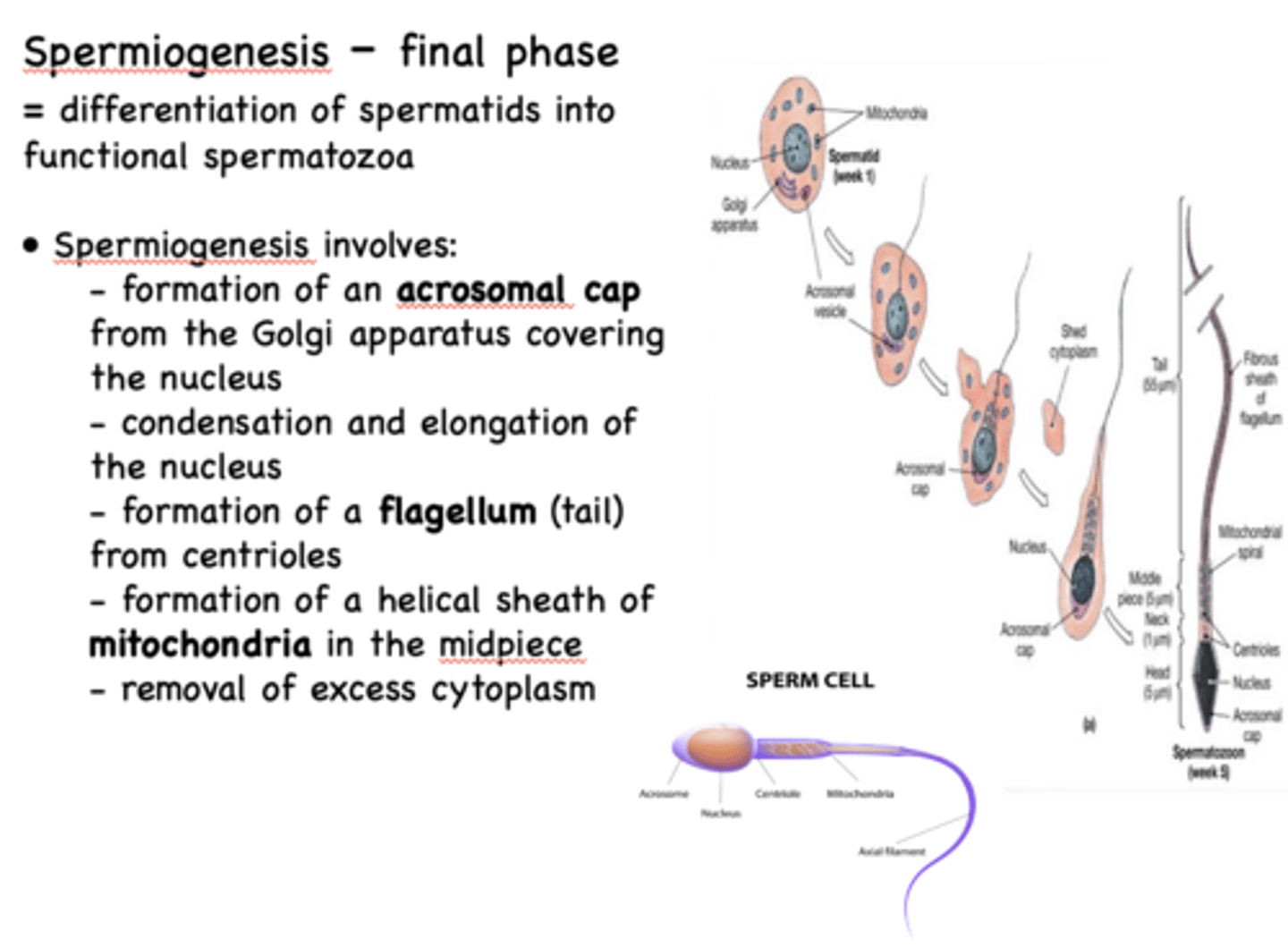
Spermiogenesis involves the formation of an ____________ from the Golgi apparatus covering the nucleus
acrosomal cap
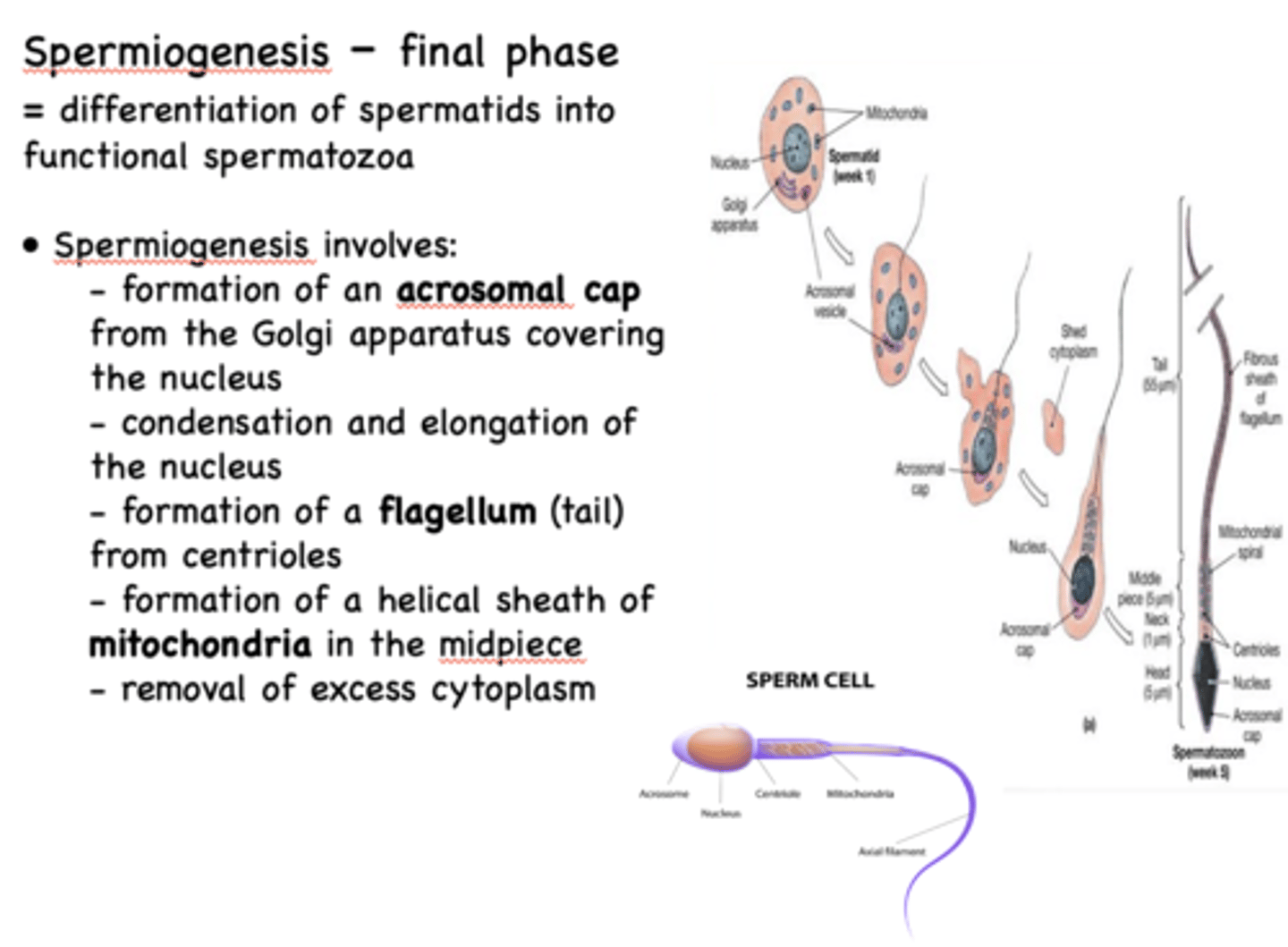
the centrioles from the spermatid develops into the ________ in a spermatozoa
flagellum
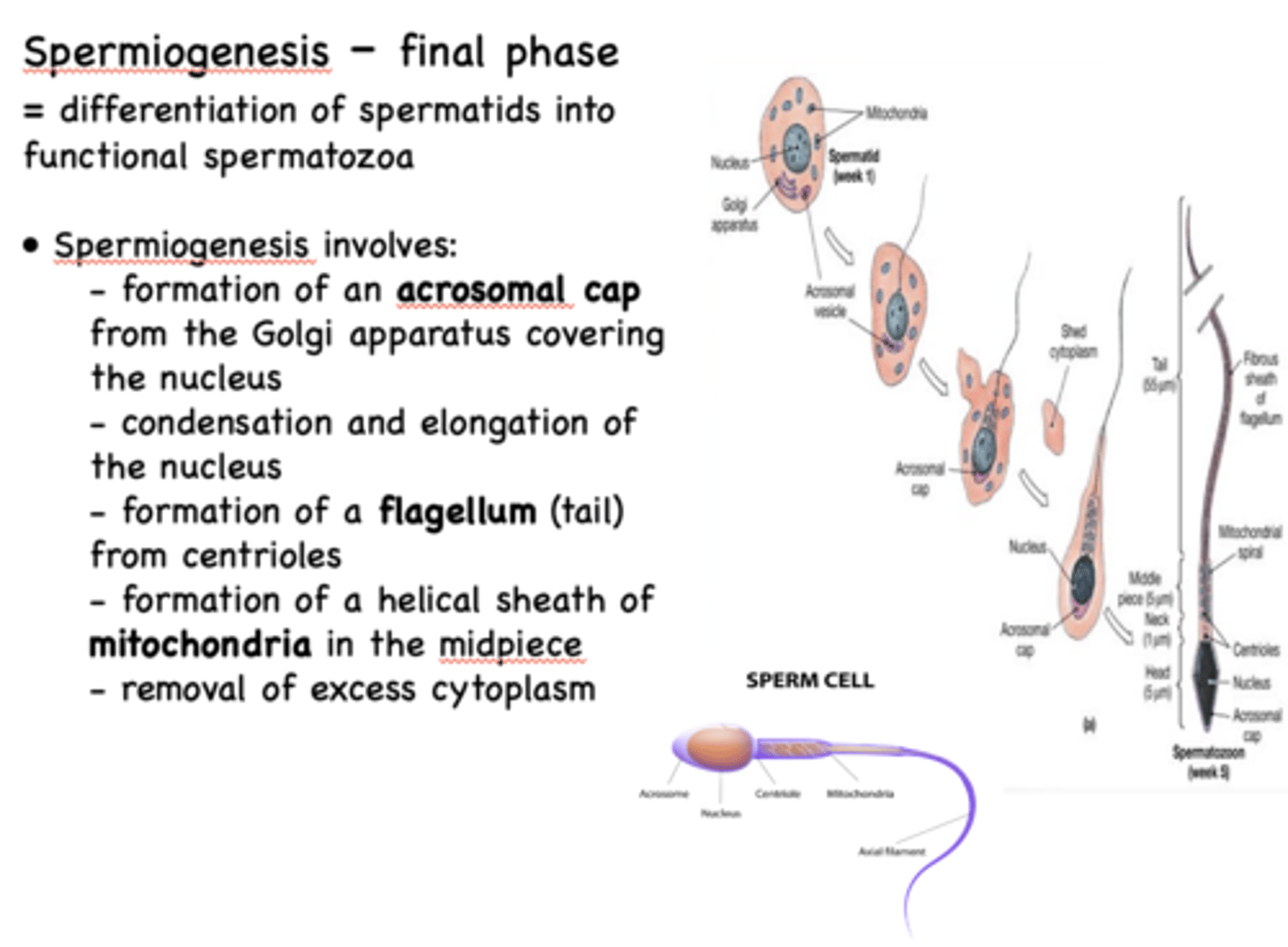
Condensation and elongation of the nucleus removal of excess cytoplasm is part of what process?
spermiogenesis
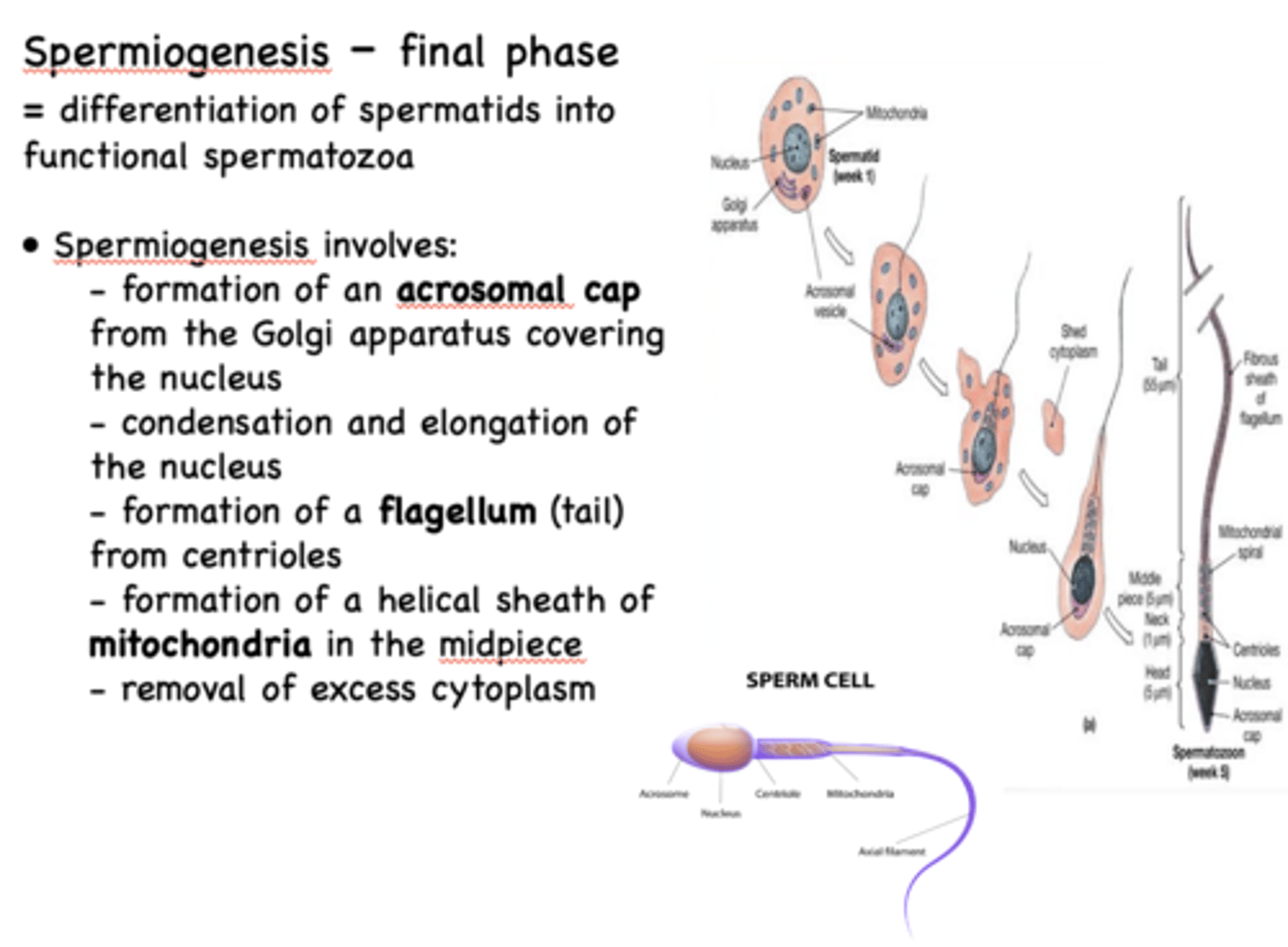
Which structure forms a helical sheath in the midpiece of a sperm cell during spermiogenesis?
Mitochondria
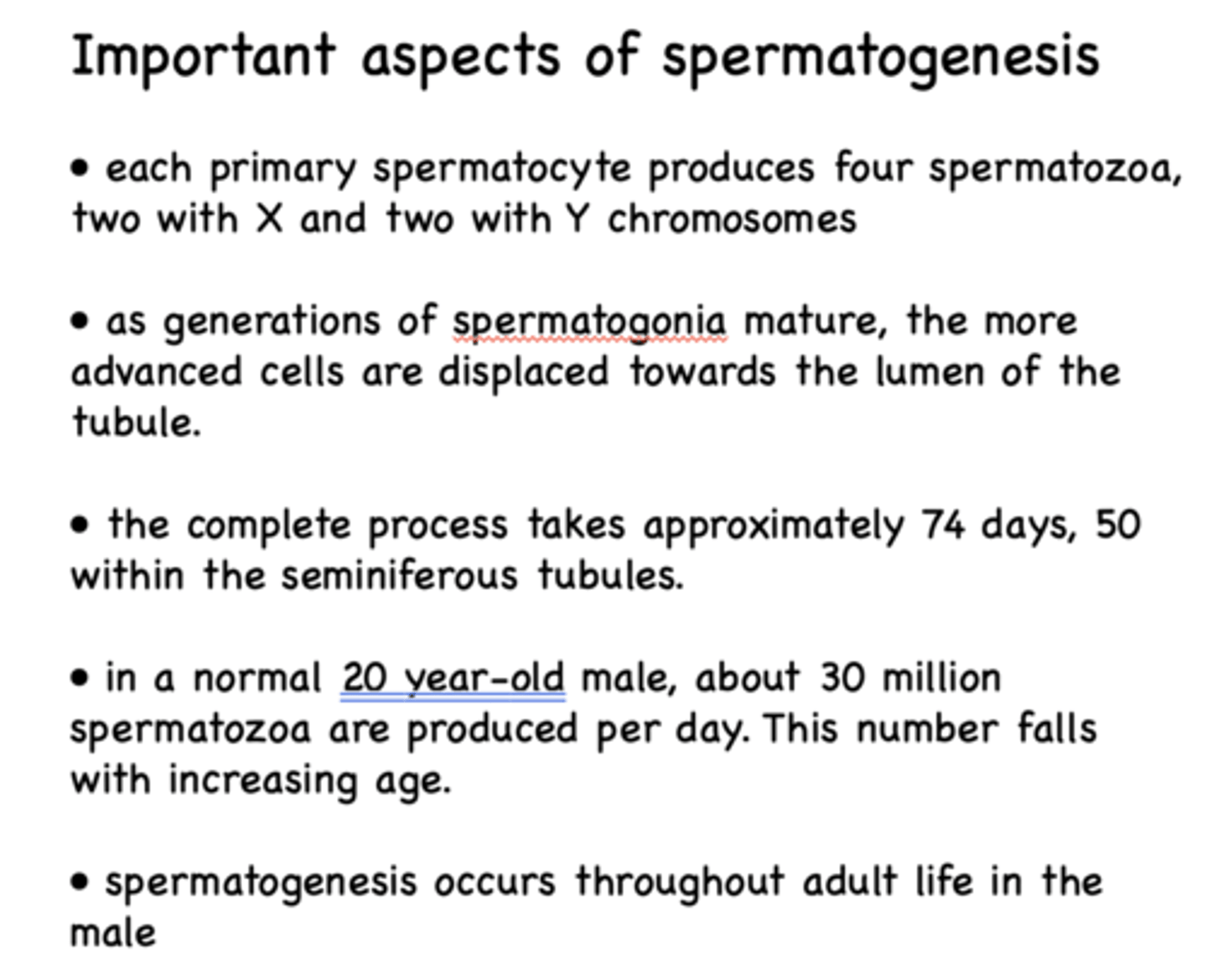
each primary spermatocyte produces __________ spermatozoa
4
as generations of spermatogonia mature, the more advanced cells are displaced towards the ______________ of the tubule
lumen
How long is the complete process of spermatogenesis?
Approximately 74 days (50 within the seminiferous tubules; 12-26 in epididymis)
in a normal 20 year-old male, about _____ million spermatozoa are produced per day
30
T/F: Spermatogenesis occurs throughout adult life in the male. But the number of spermatozoa produced per day falls with increasing age
True
What cells produce and secrete testosterone?
Leydig cells
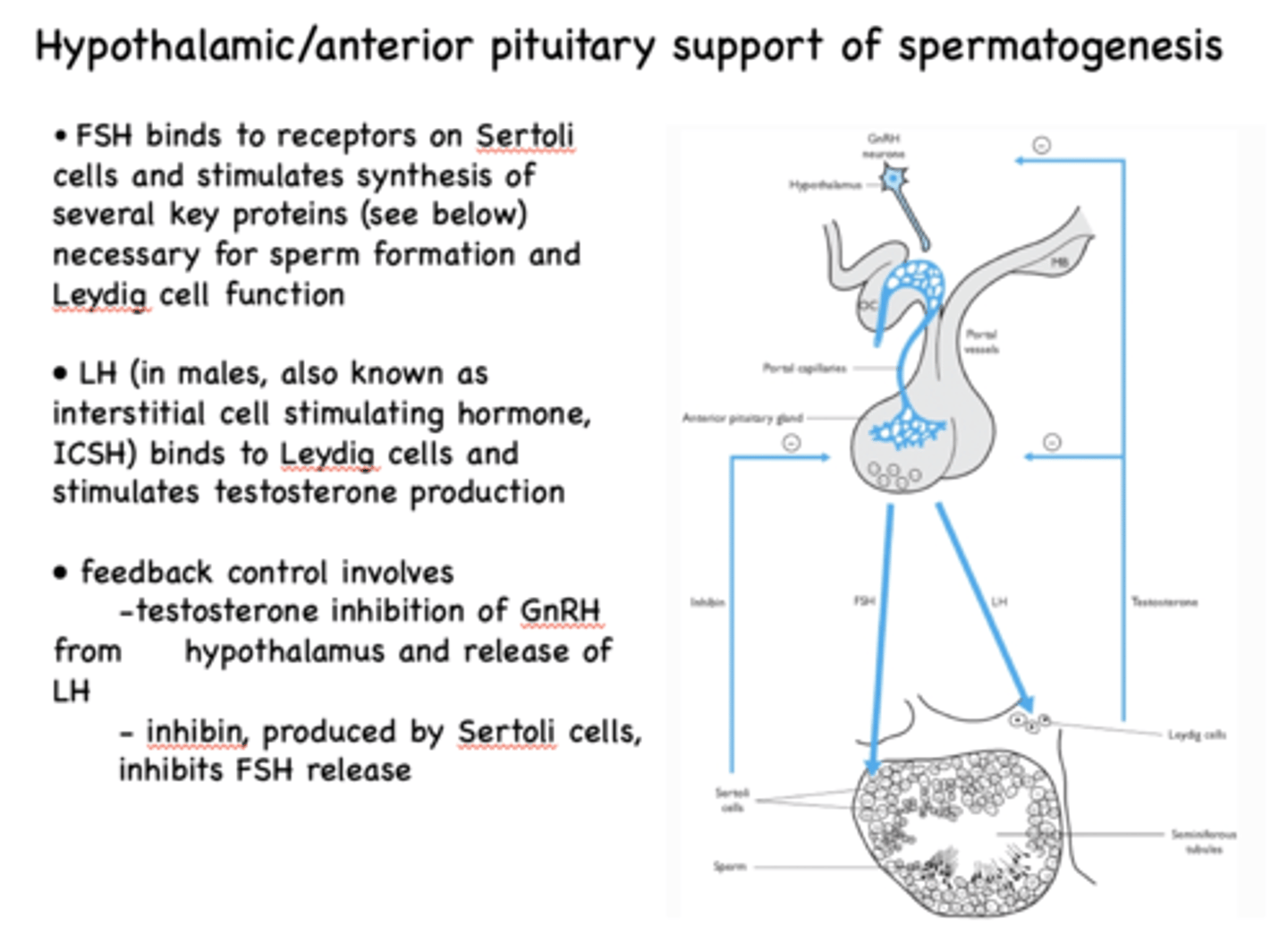
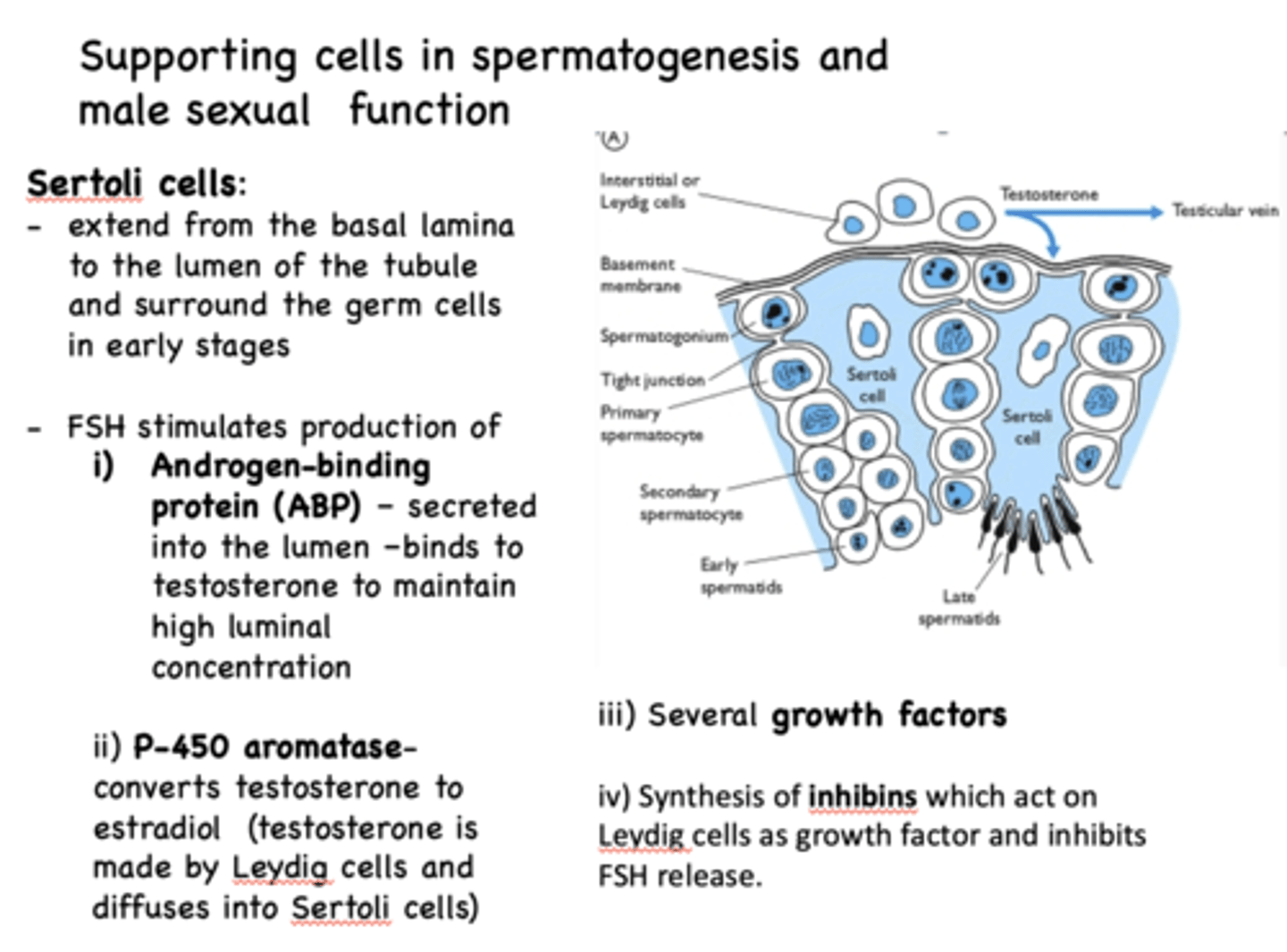
Sertoli cells are activated under ______ stimulation
FSH
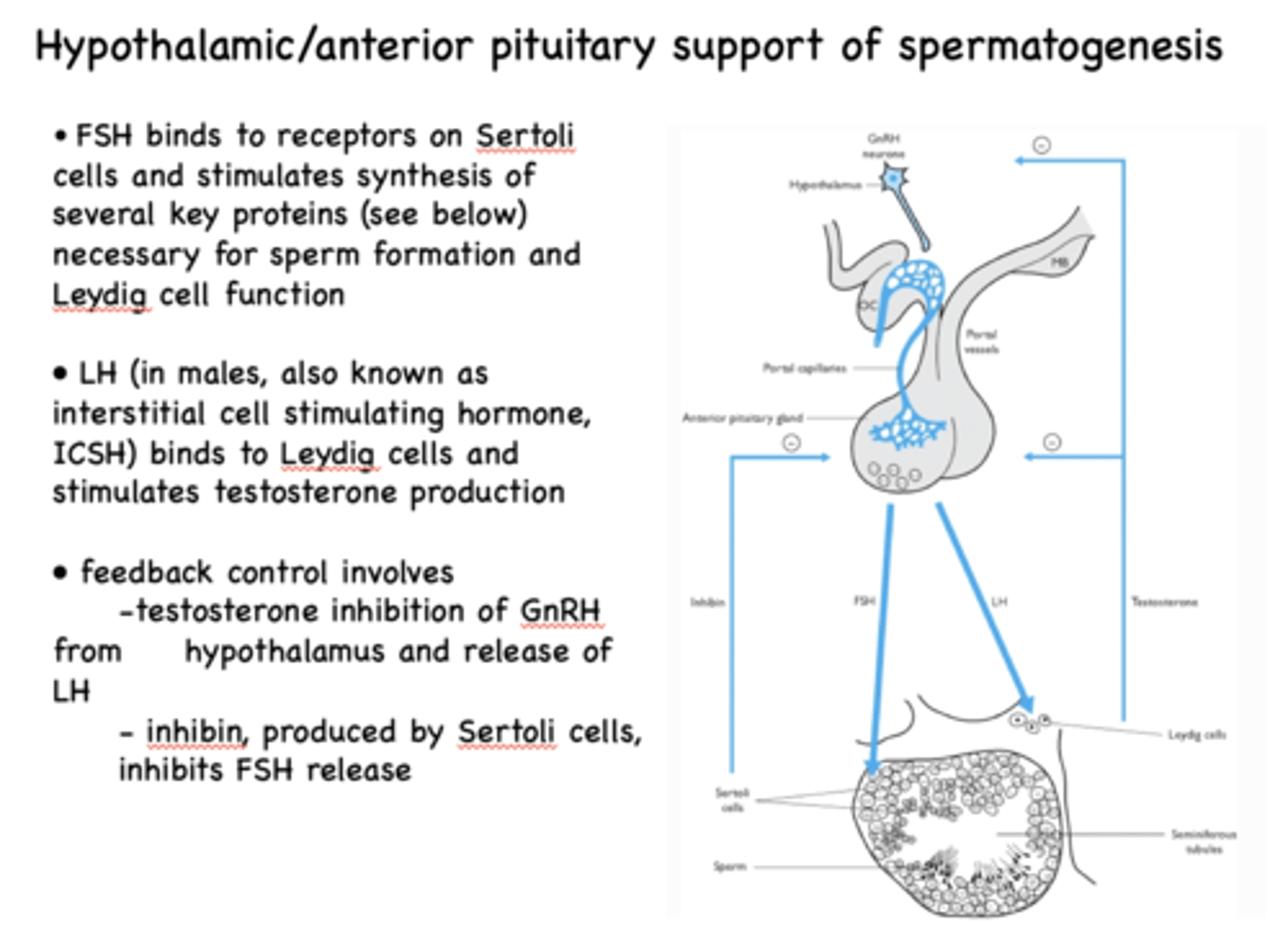
_____________ binds to receptors on Sertoli cells and stimulates synthesis of several key proteins necessary for sperm formation and Leydig cell function
FSH
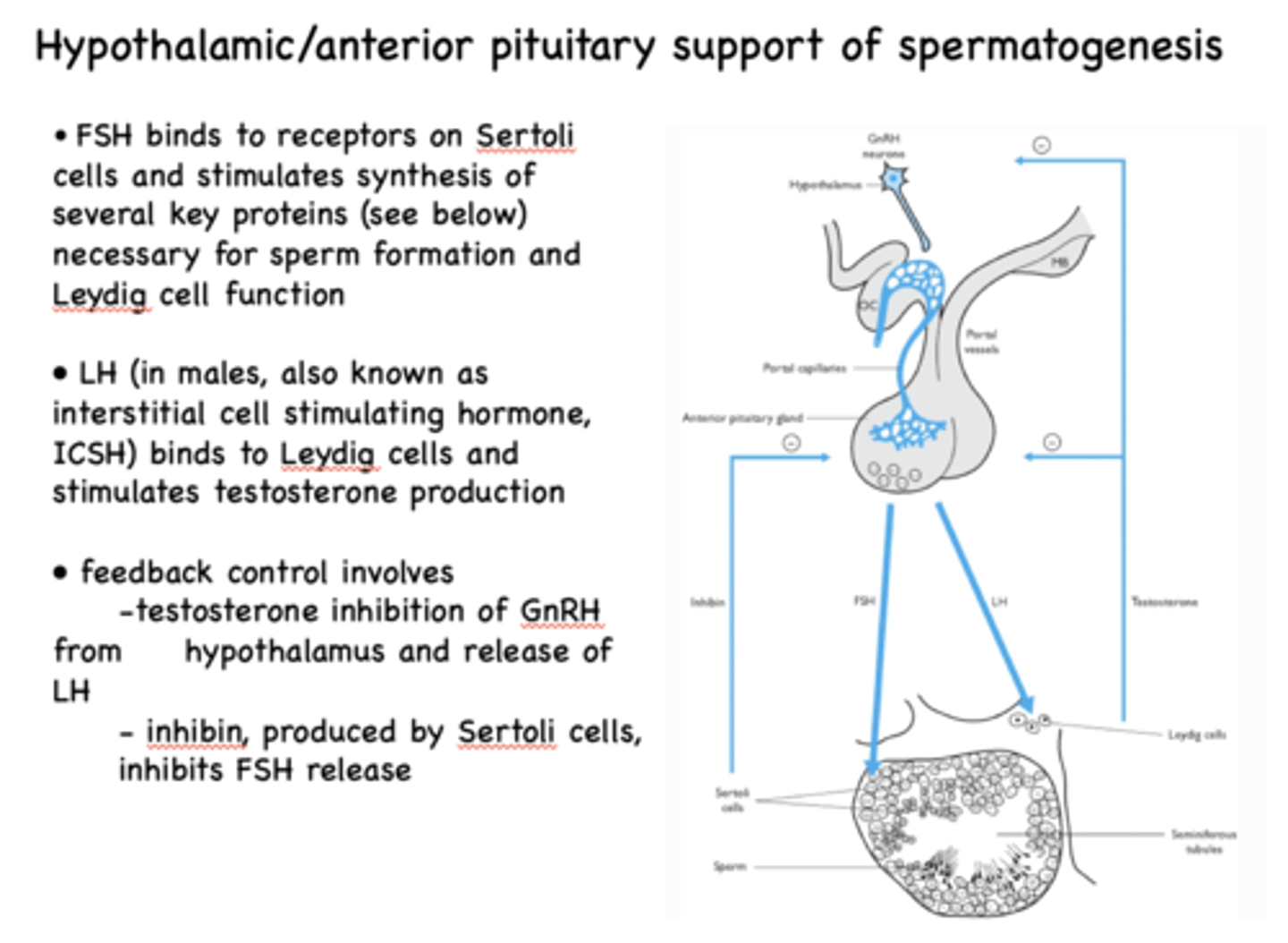
Leydig cells produce and secrete testosterone under ______ stimulation
LH (ICSH in males)
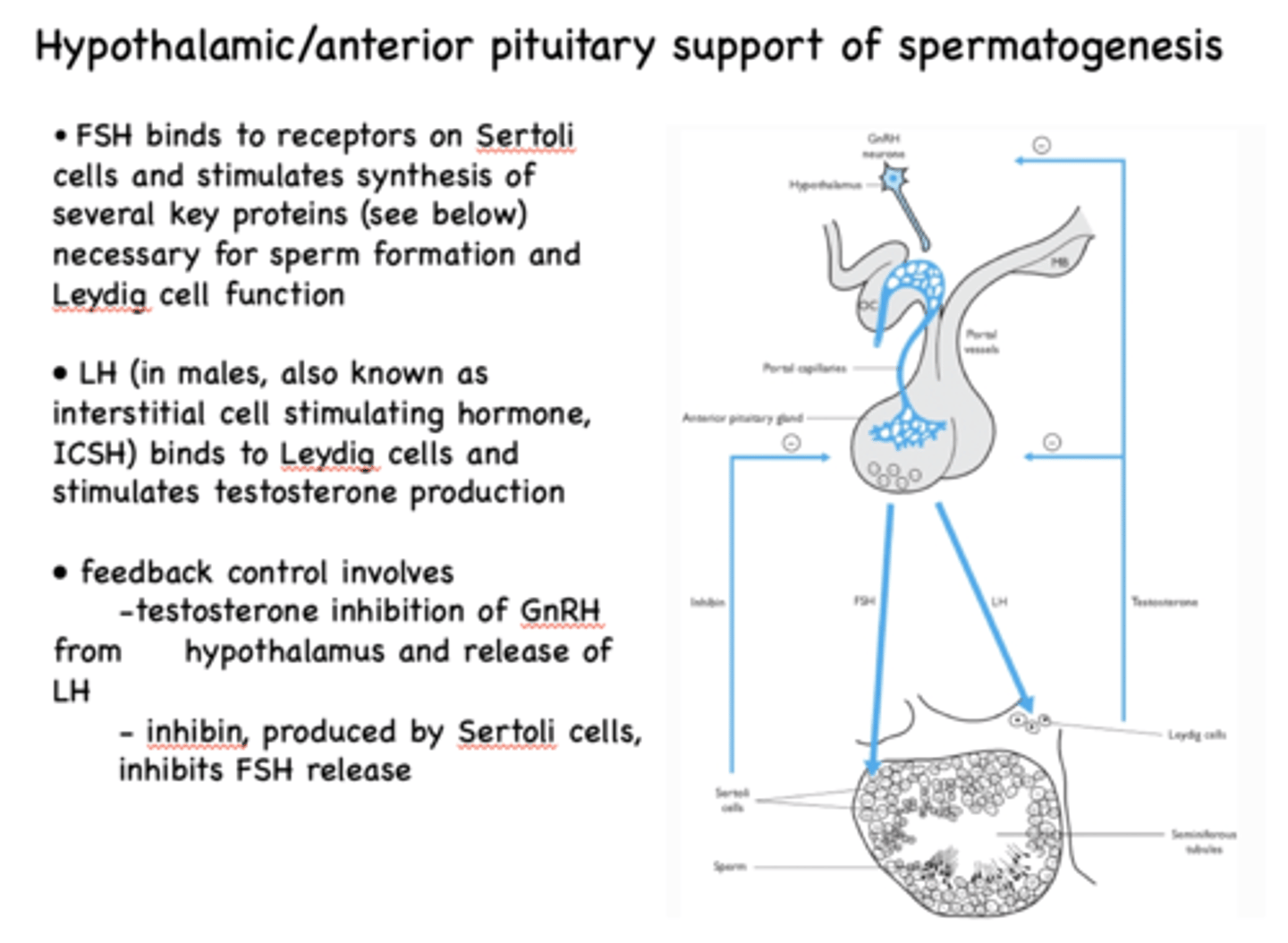
increasing levels of testosterone will inhibit the production of _______ at the level of the anterior pituitary
LH
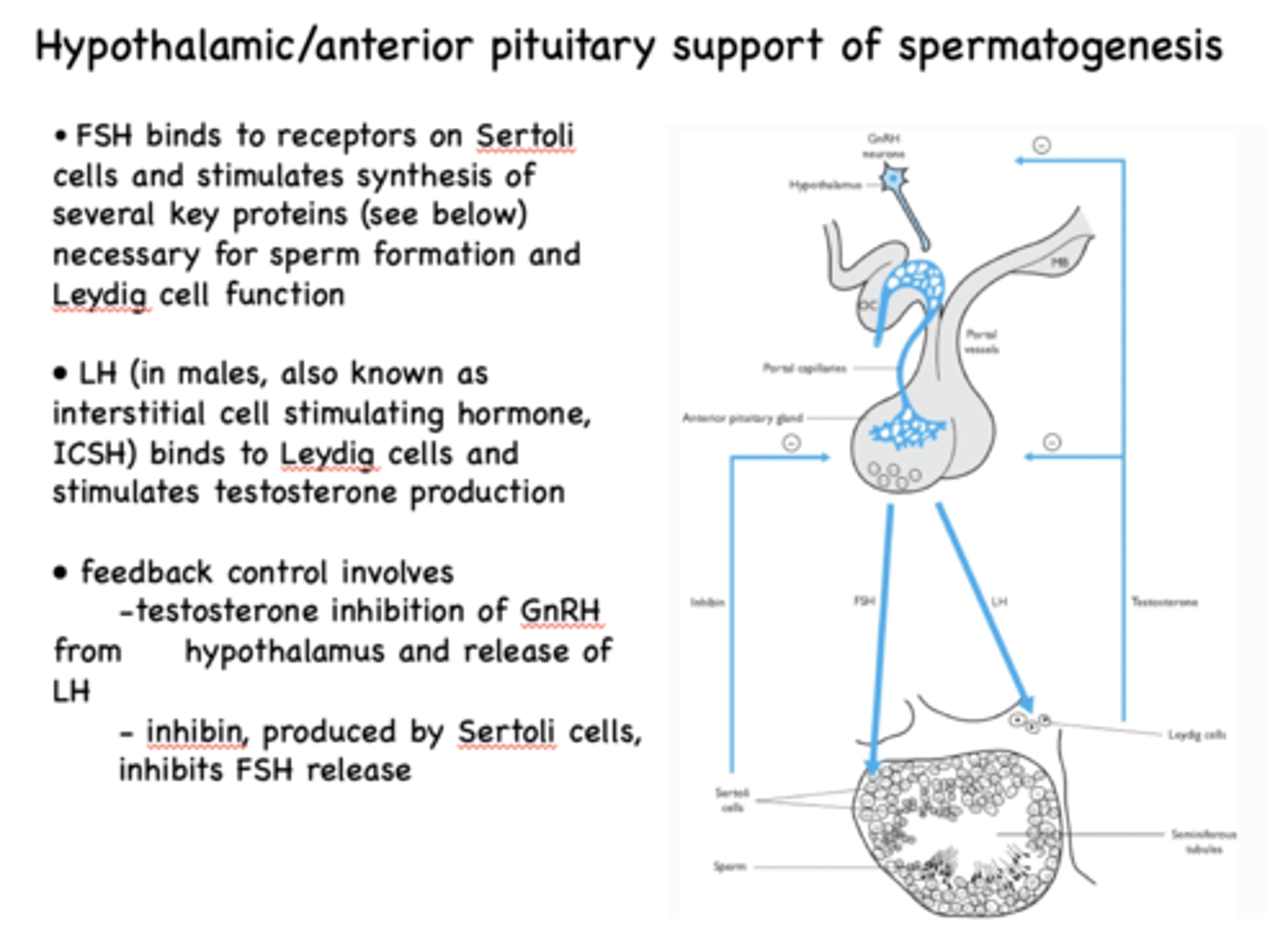
increasing levels of testosterone will inhibit the production of __________ at the level of the hypothalamus
GnRH
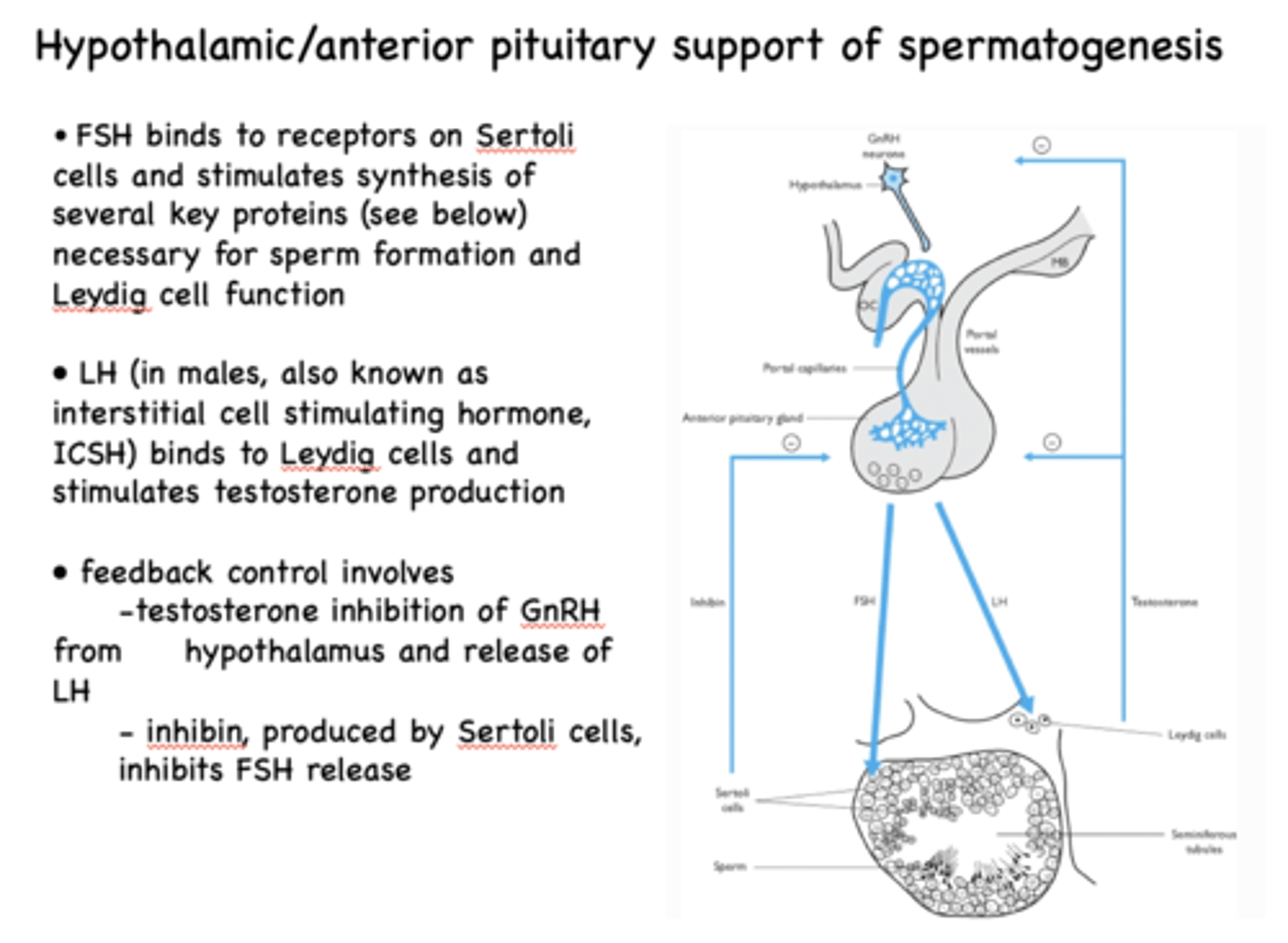
_____________ produced by Sertoli cells, inhibits FSH release
inhibin
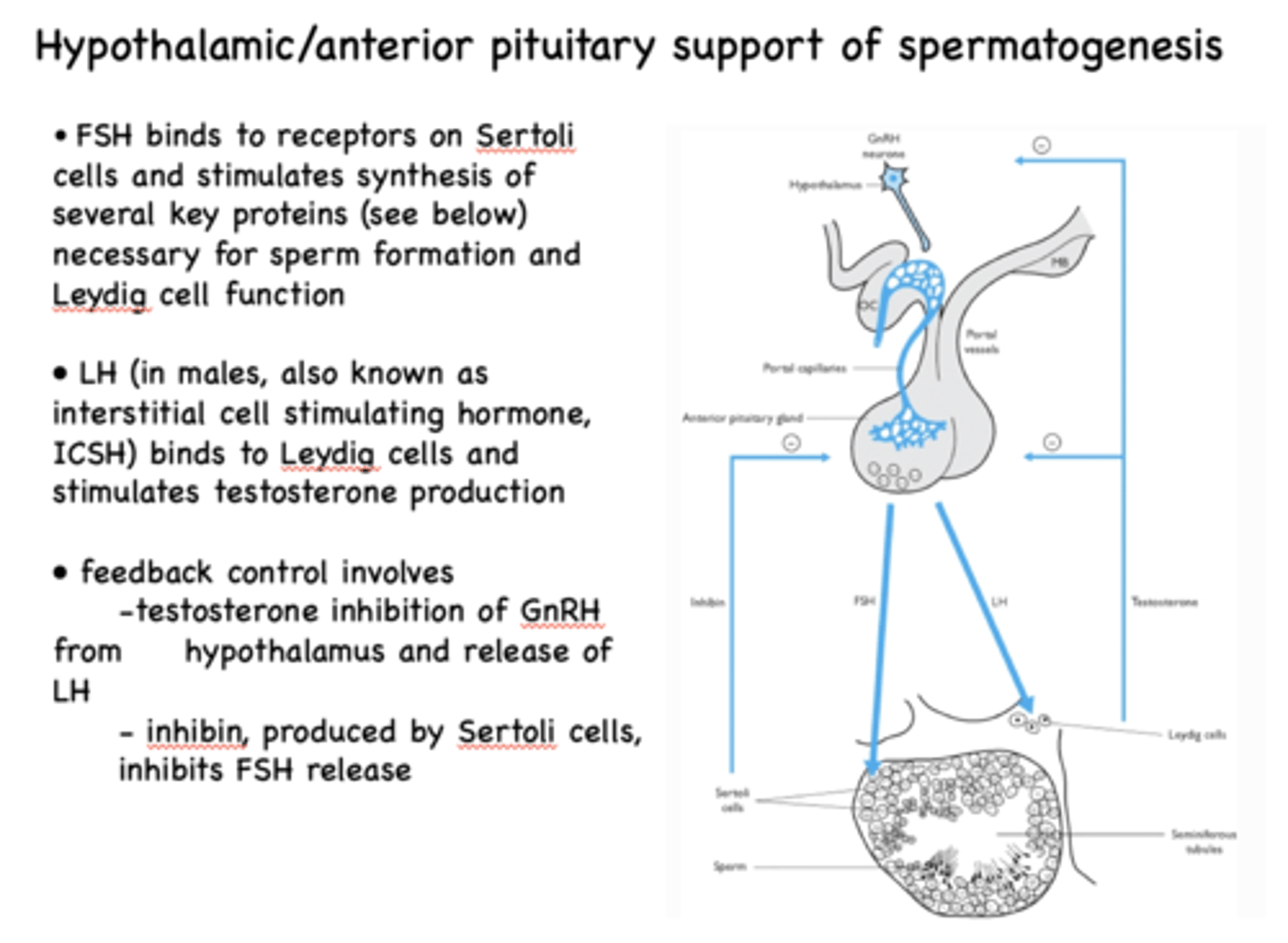
increasing levels of inhibin will inhibit the production of _________ at the level of the anterior pituitary
FSH
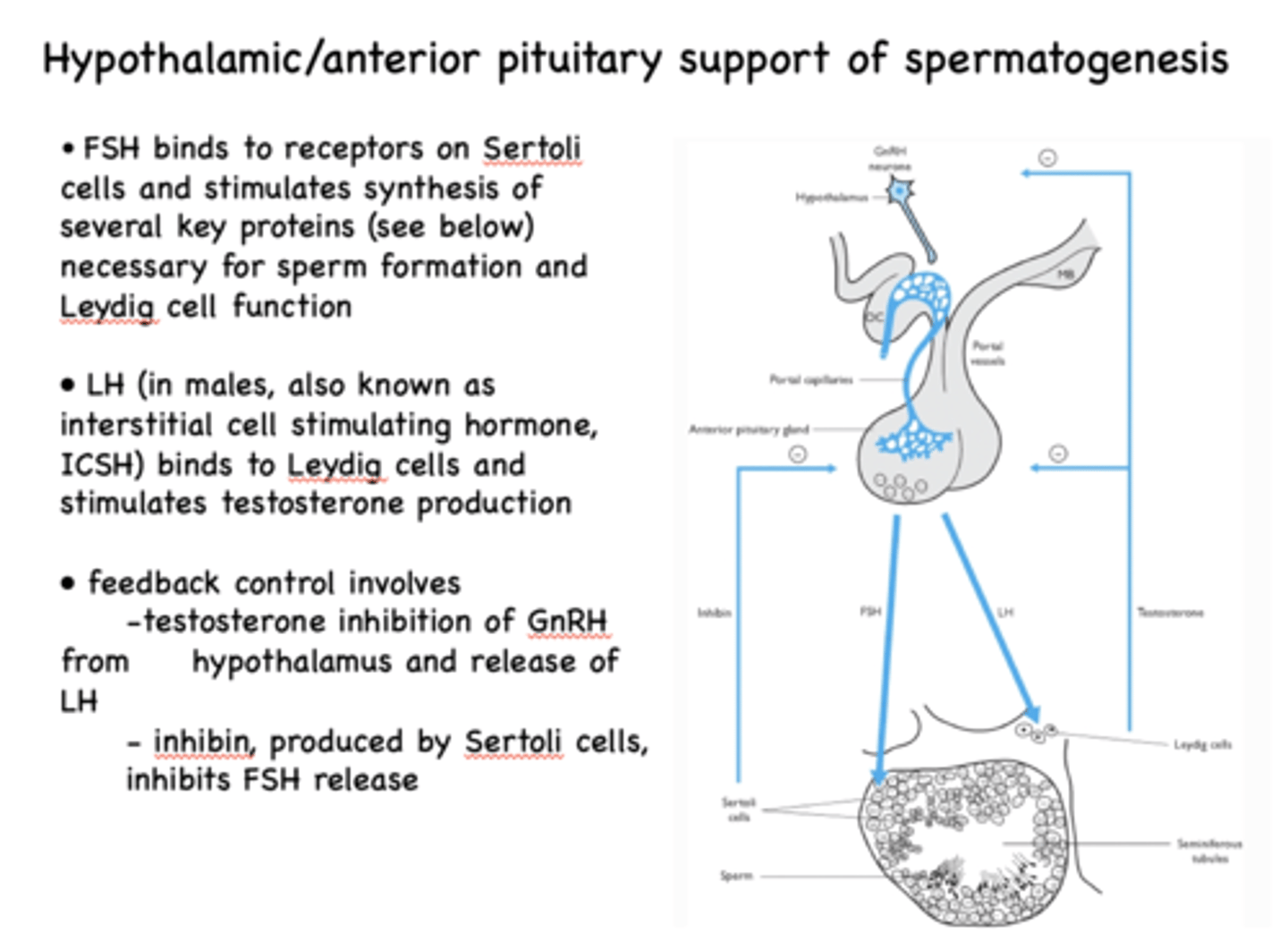
What acts on leydig cells as growth factor and inhibits FSH release?
inhibins
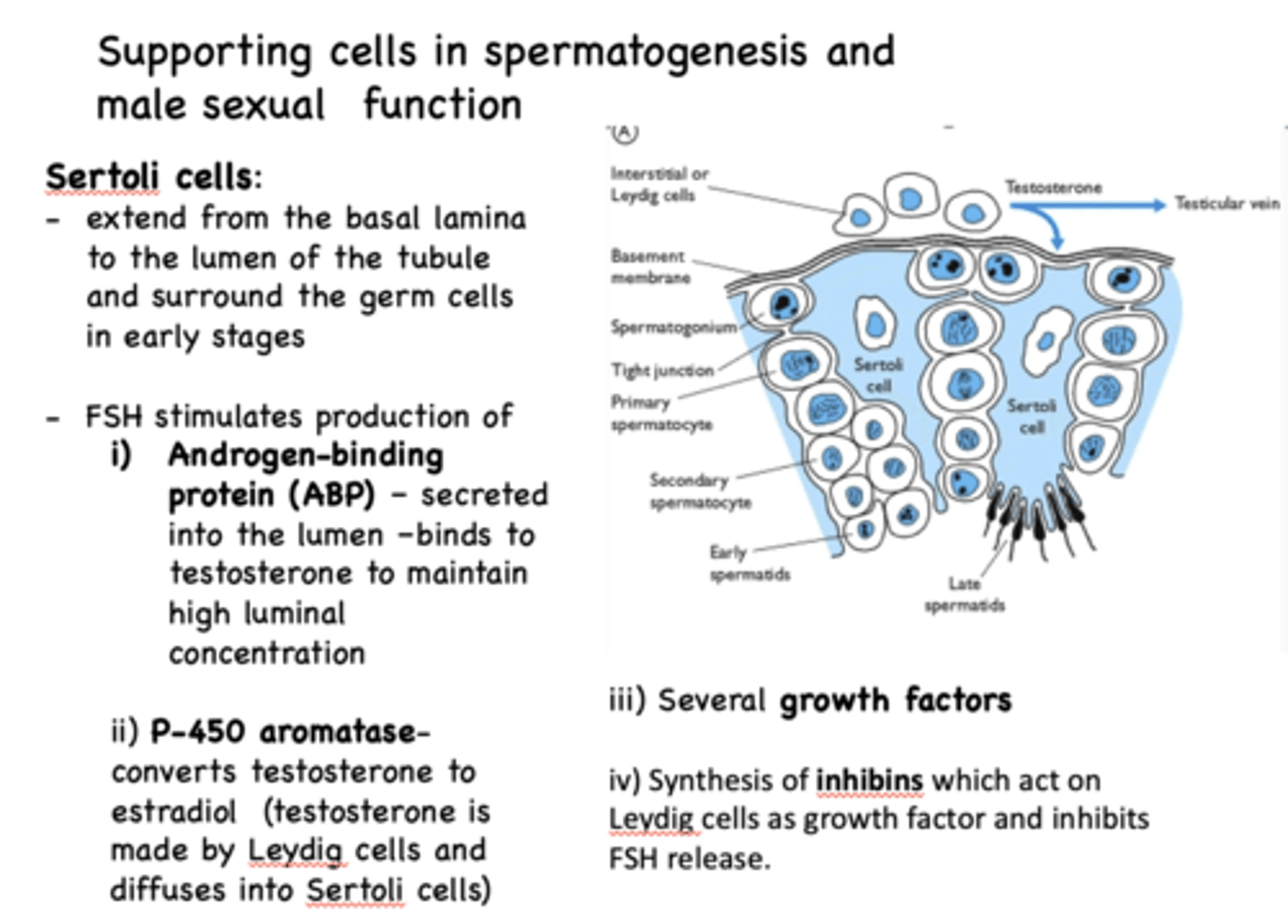
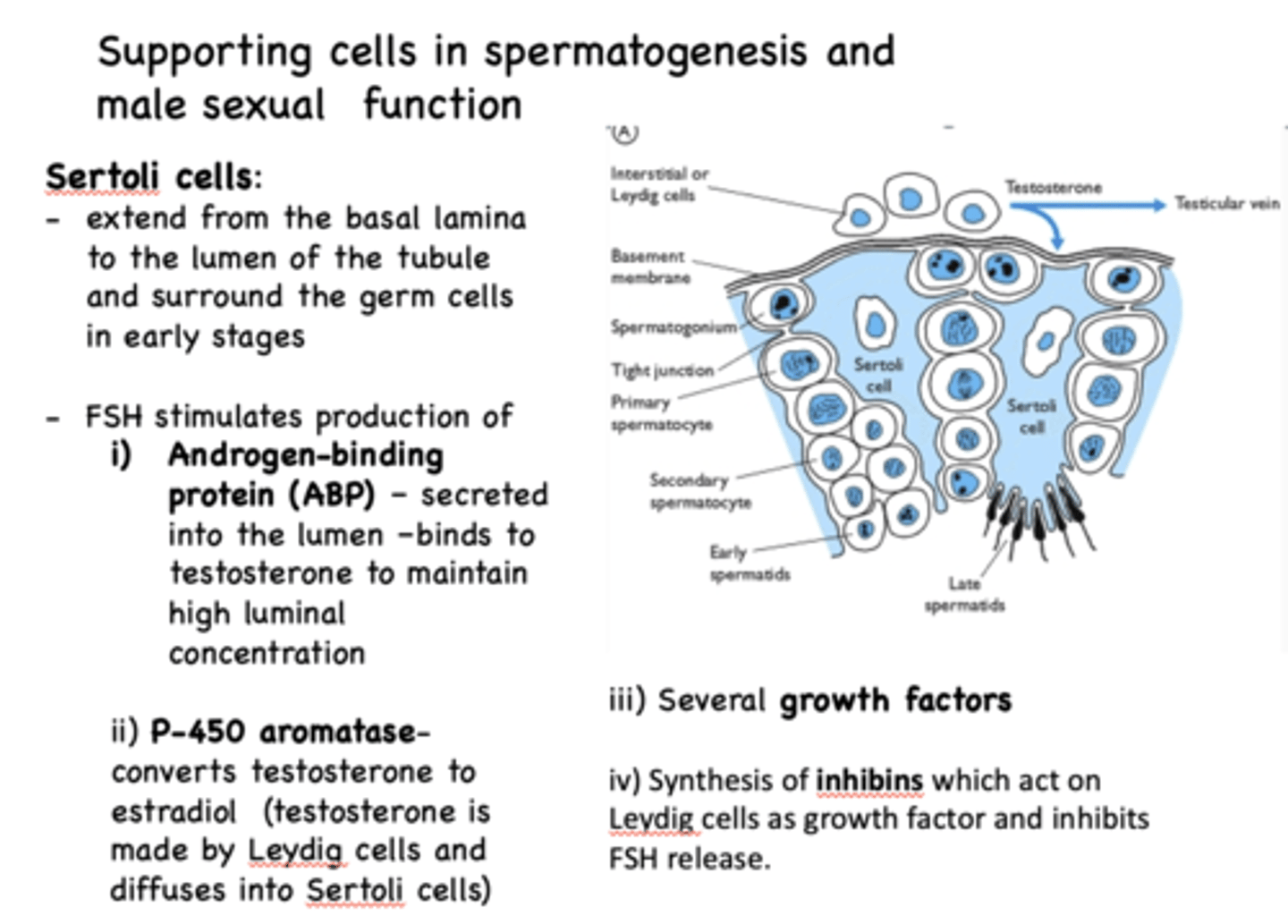
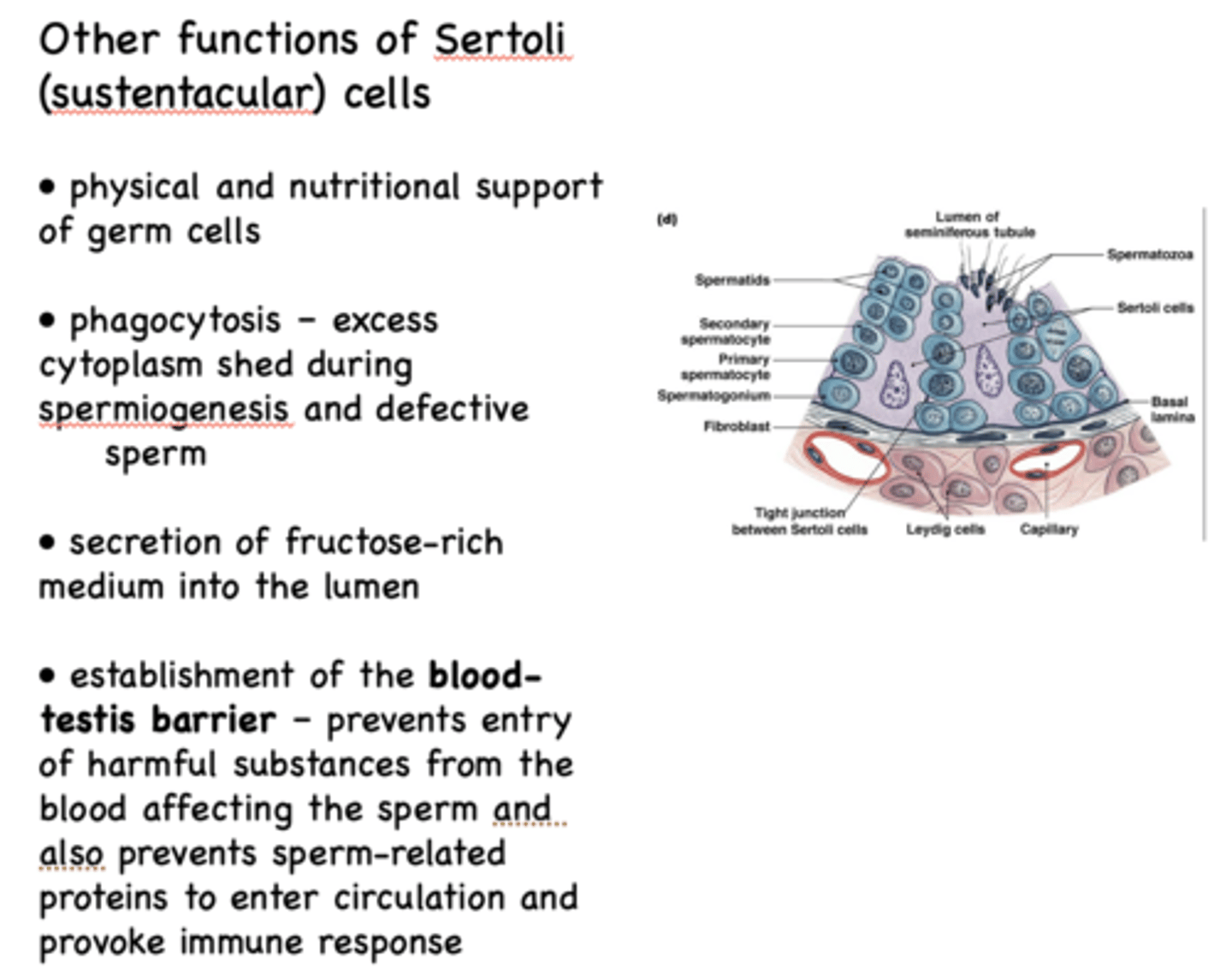
______________ extend from the basal lamina to the lumen of the tubule and surround the germ cells in early stages
Sertoli cells
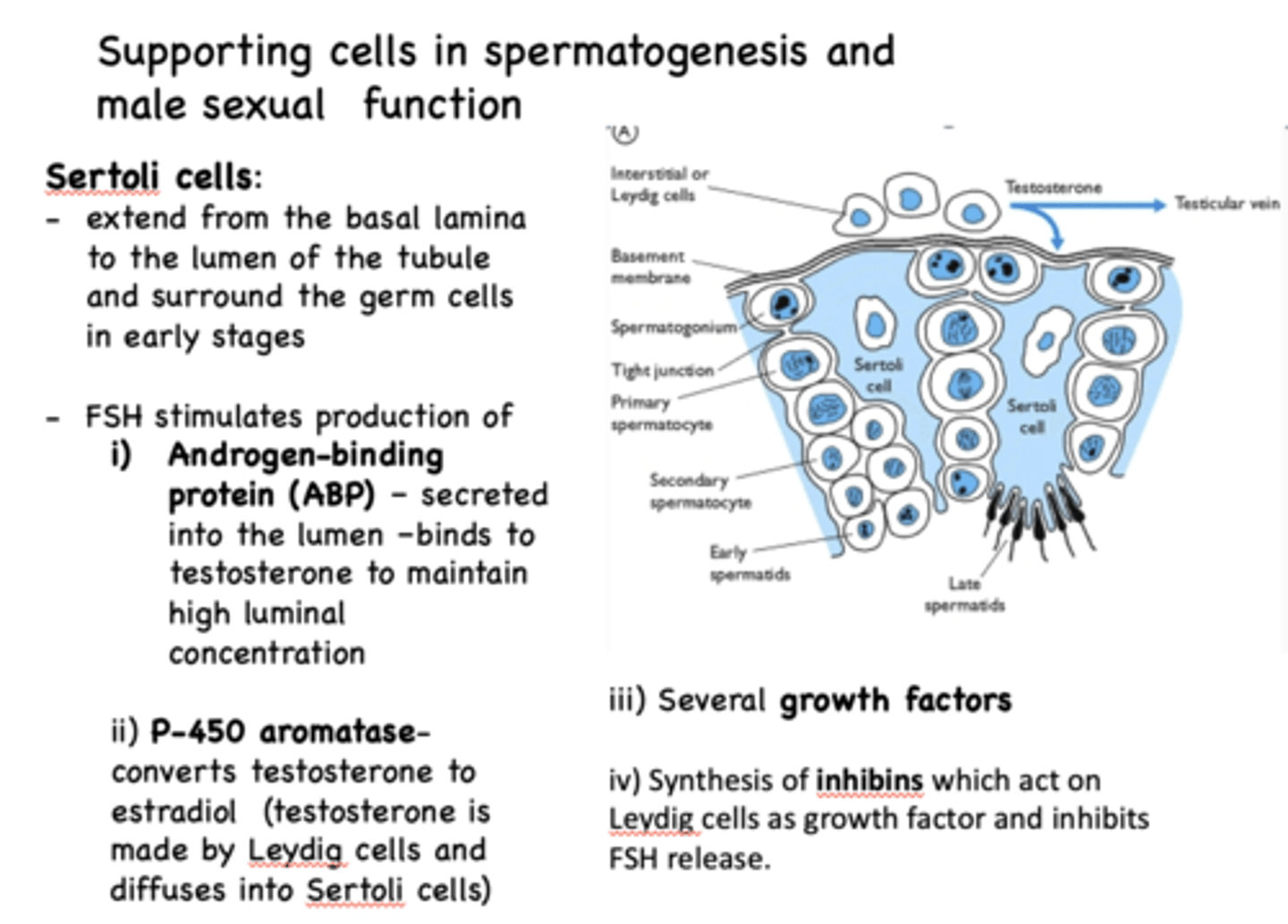
__________ stimulates production of Androgen Binding Protein, which binds to testosterone to maintain high luminal concentration
FSH
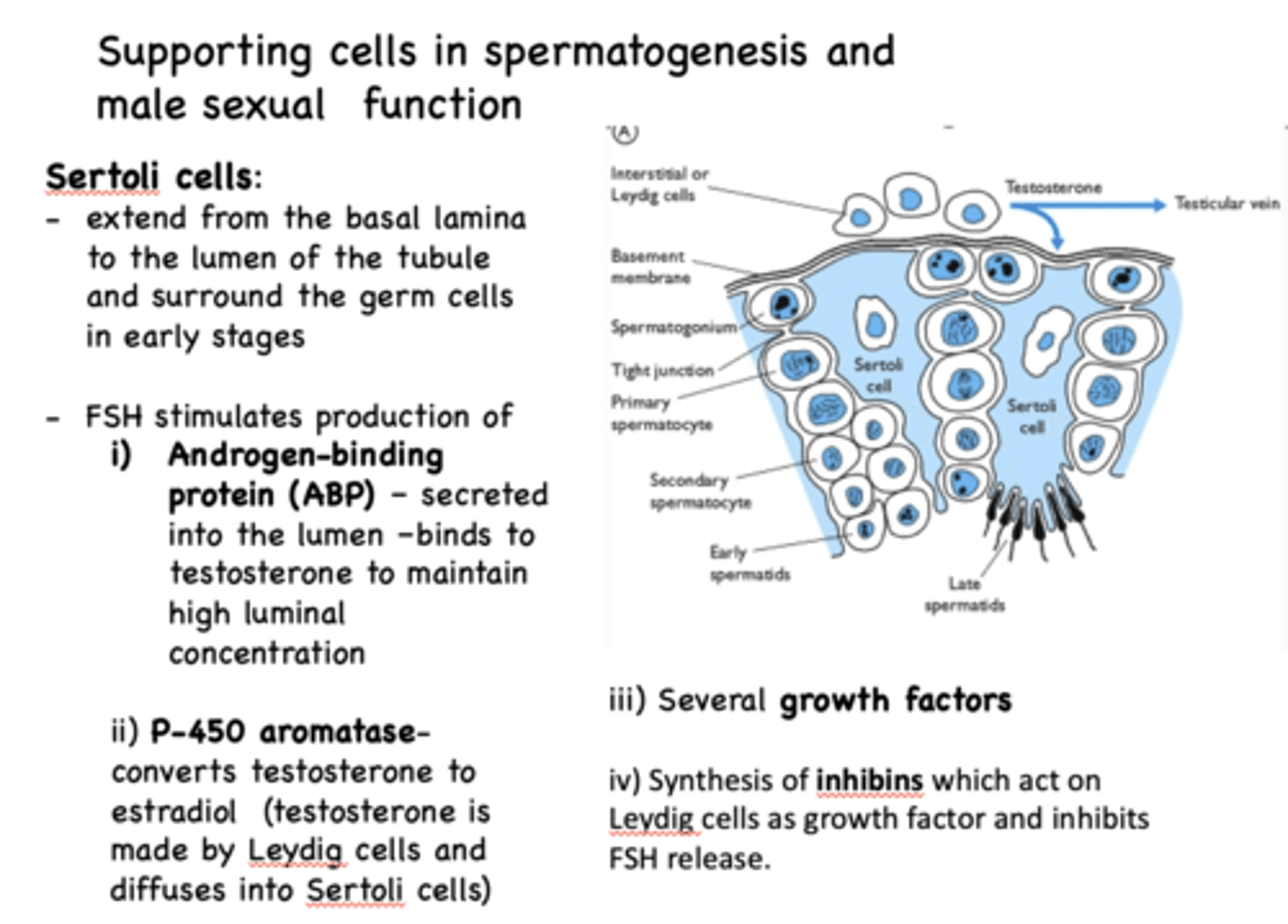
What converts testosterone to estradiol?
P-450 aromatase
What cells provide physical and nutritional support of germ cells?
Sertoli cells
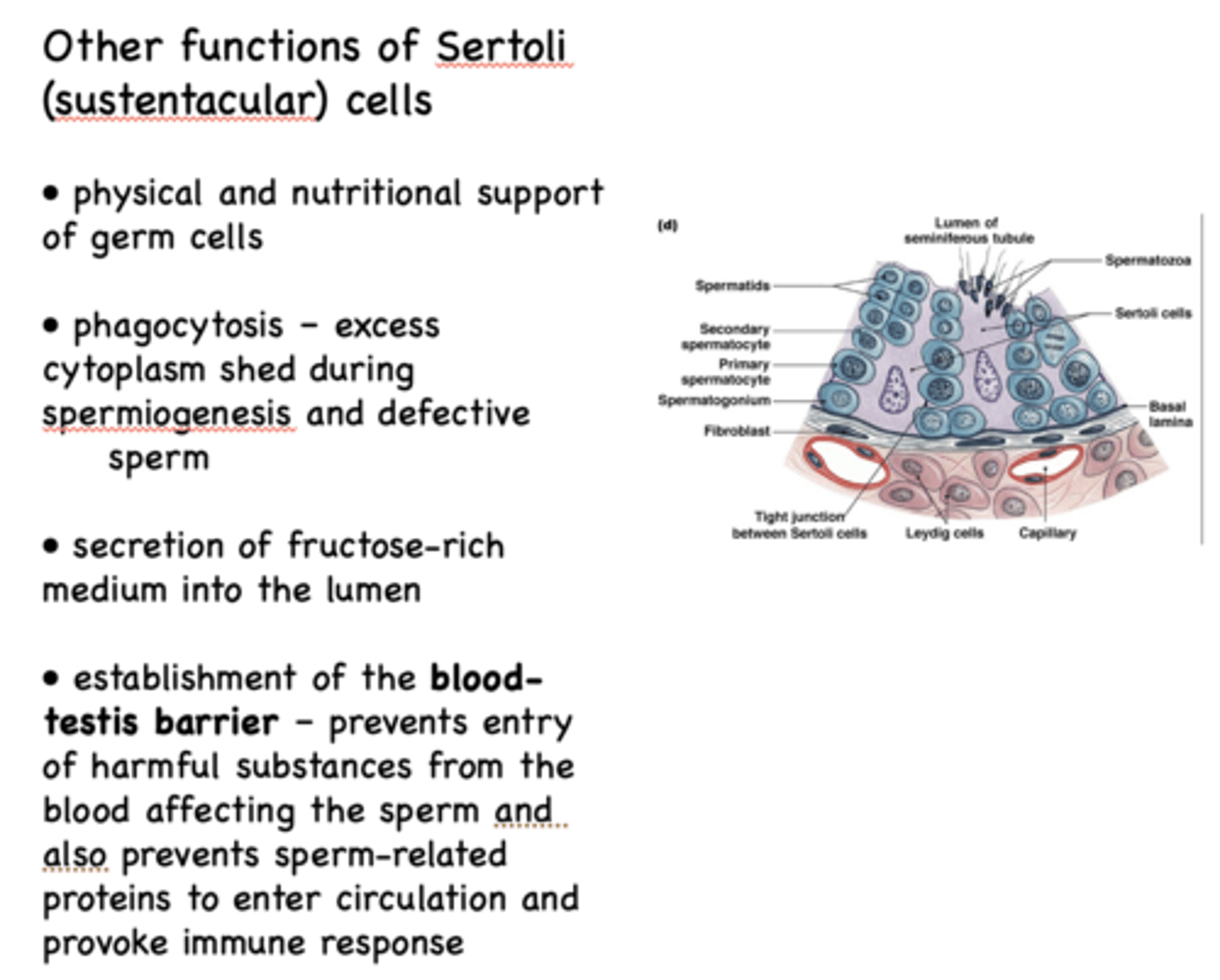
What cells phagocytose excess cytoplasm shed during spermiogenesis and defective sperm?
Sertoli cells
What cells secretion of fructose-rich medium into the lumen?
Sertoli cells
Define the following:
Prevents entry of harmful substances from the blood affecting the sperm and also prevents sperm-related proteins to enter circulation and provoke immune response
Blood-testis barrier
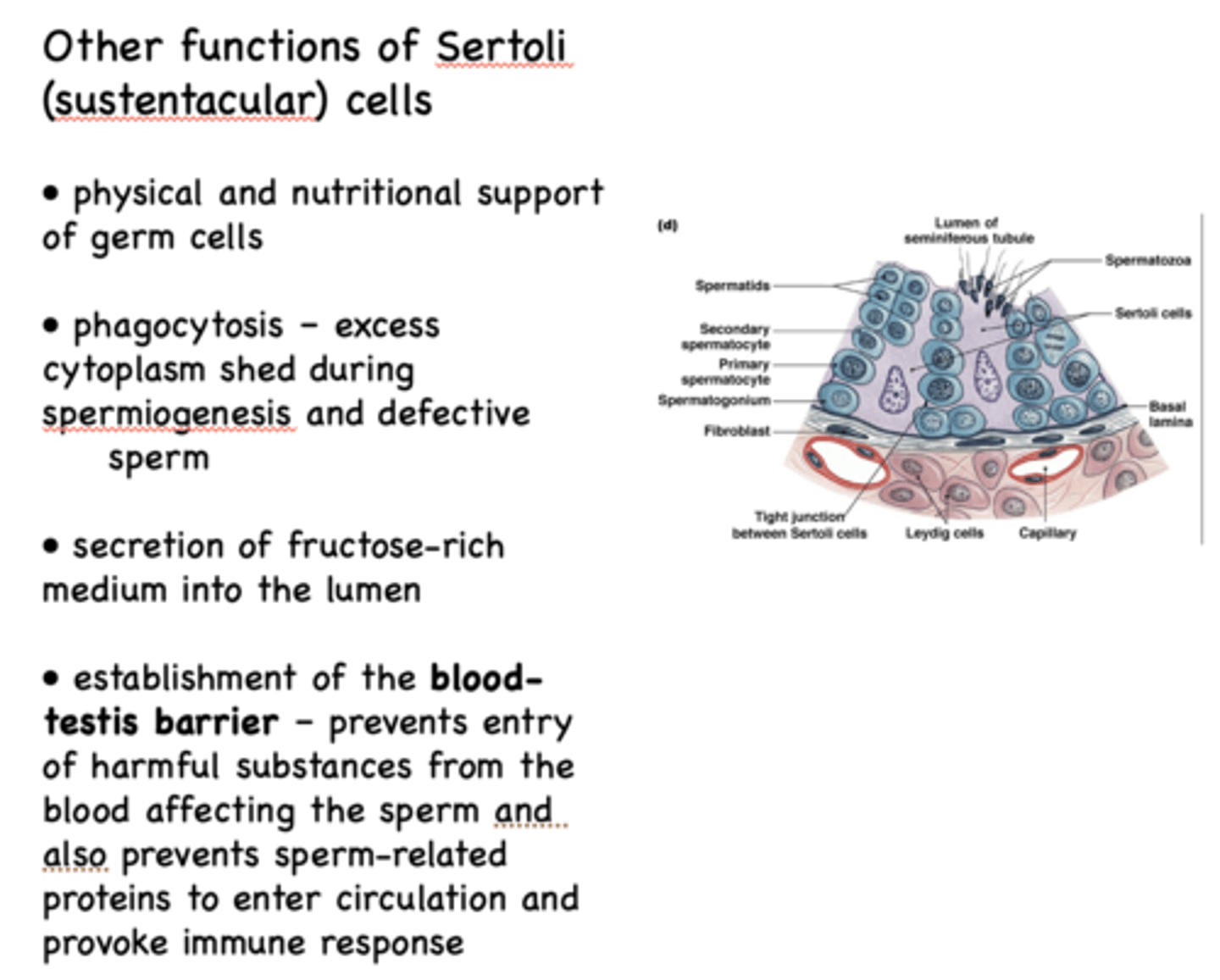
What cells establish the blood-testis barrier?
Sertoli cells
what 4 things do Sertoli cells produce?
- Androgen-binding protein (ABP)
- P-450 aromatase
- Growth factors
- Inhibin
What cells are located between the seminiferous tubules?
Leydig cells
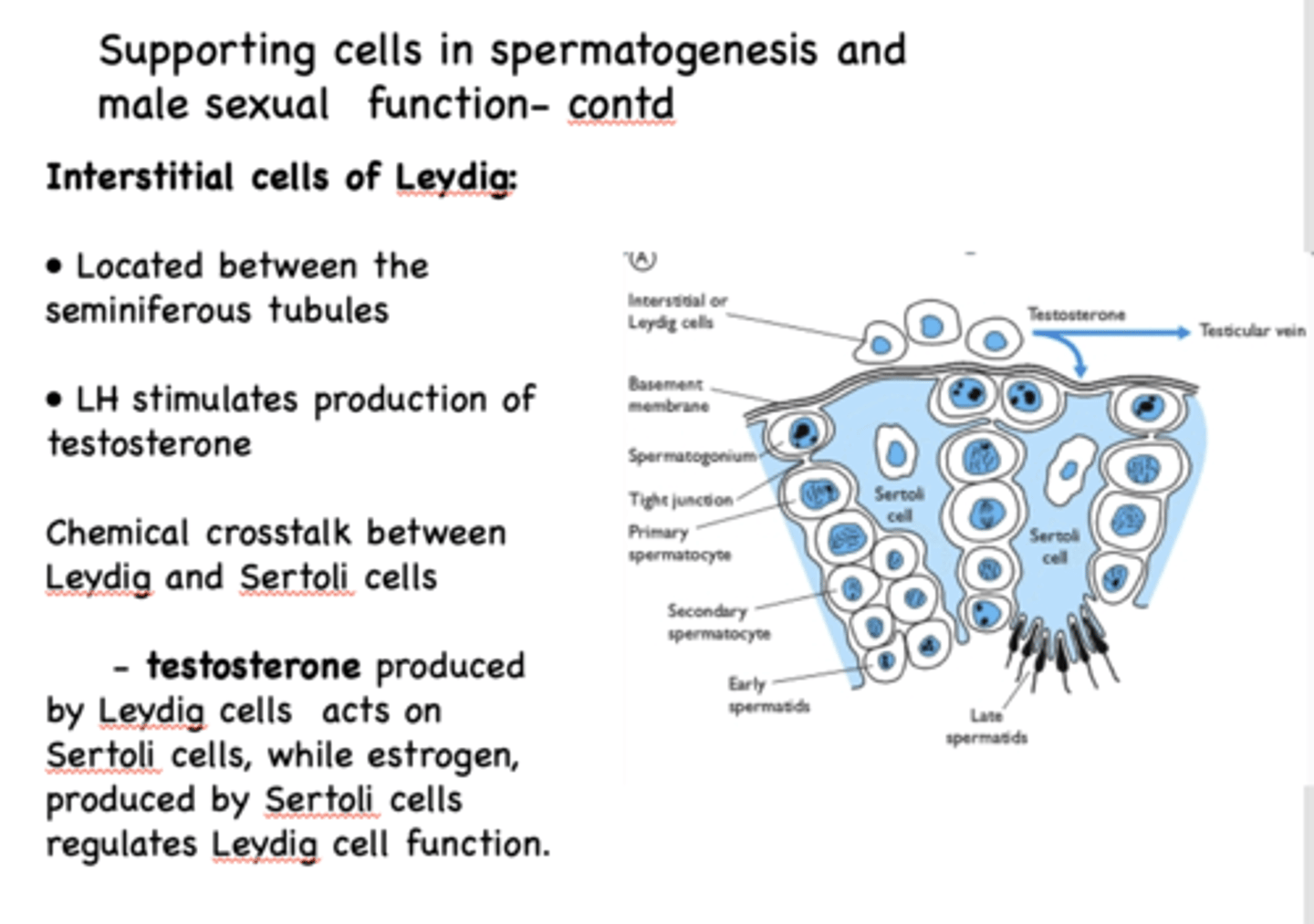
testosterone produced by __________ acts on Sertoli cells
Leydig cells
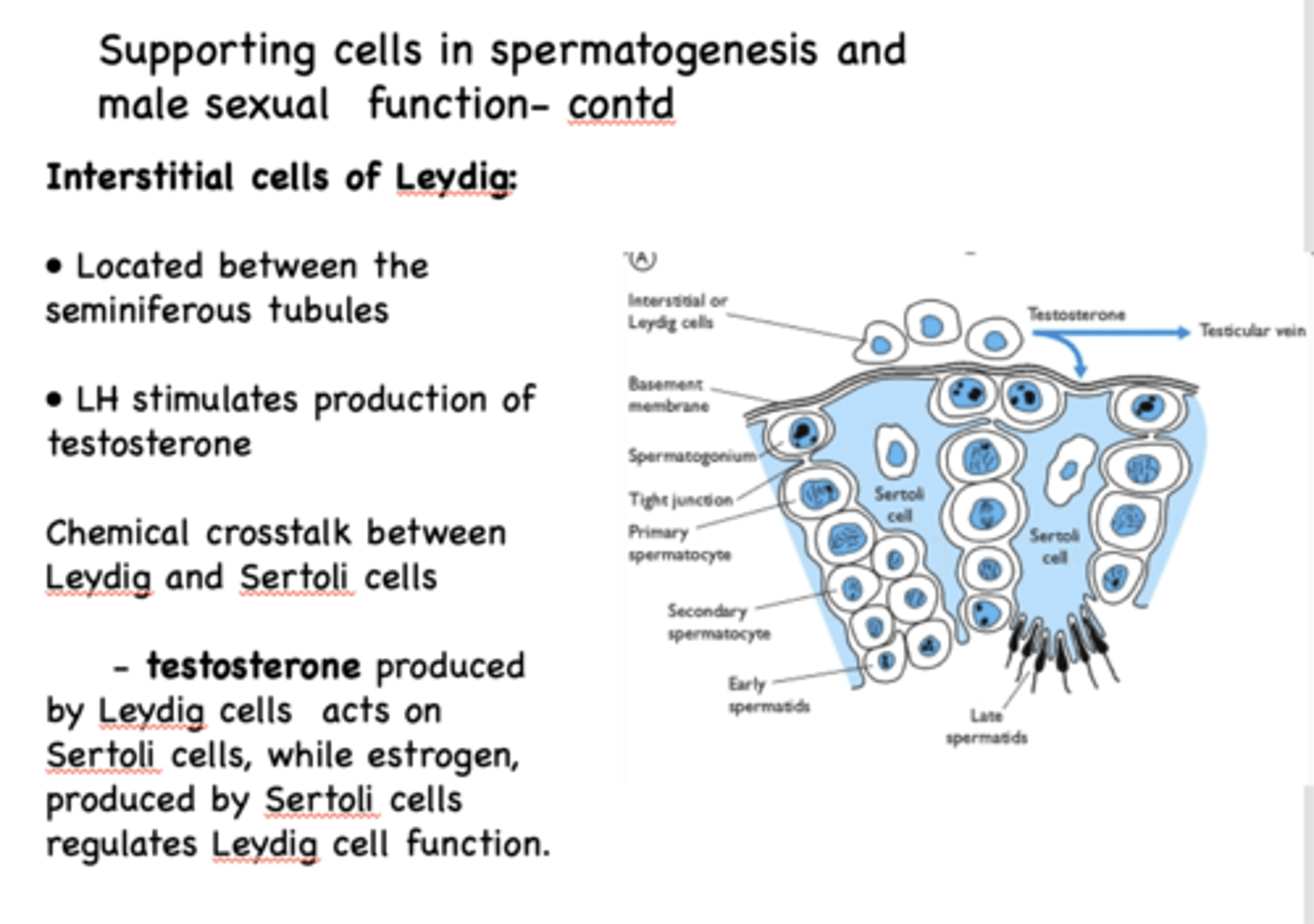
estrogen, produced by __________ regulates Leydig cell function
Sertoli cells
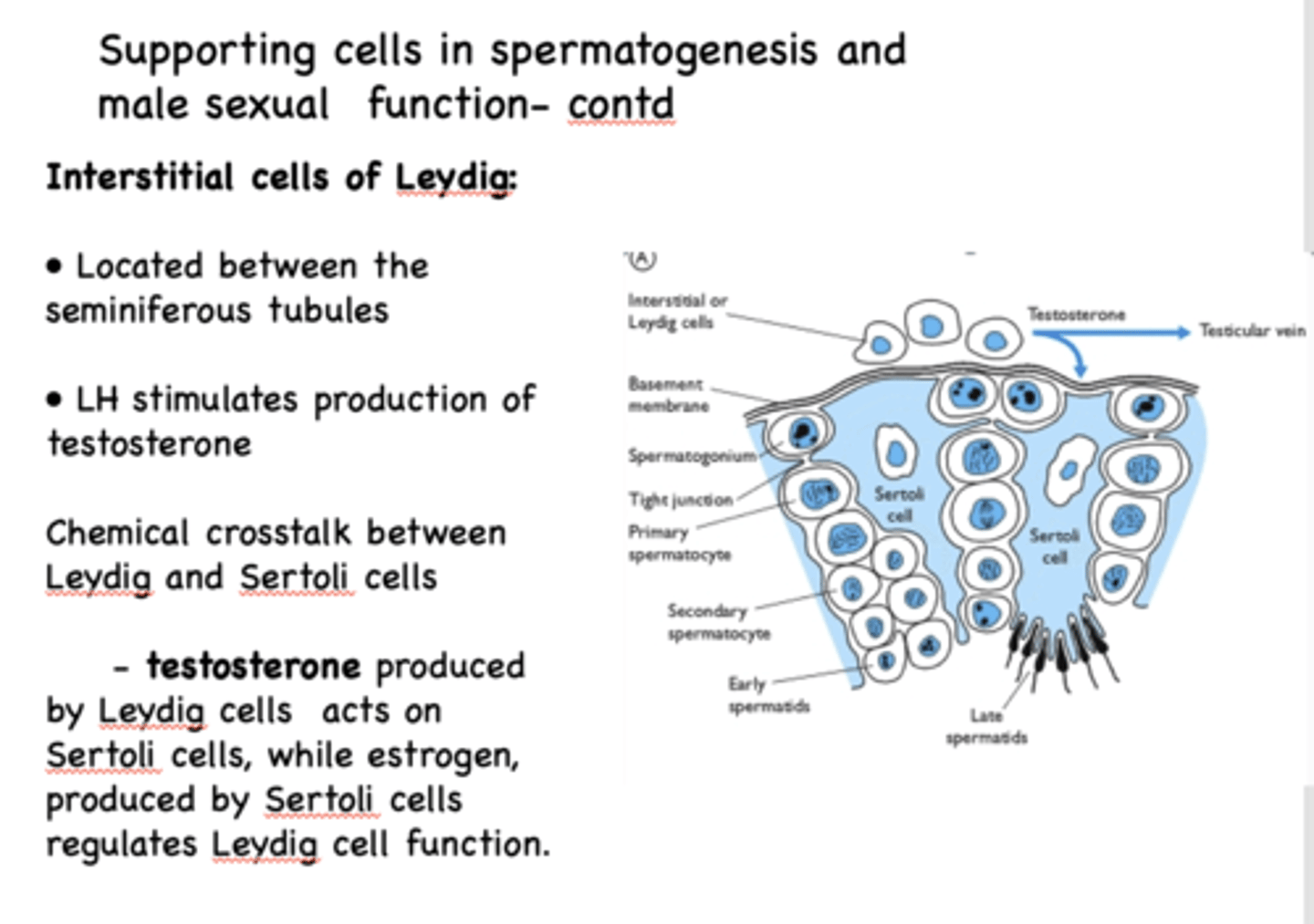
What stimulates production of testosterone?
LH
What sexual characteristics depend upon increased androgens at puberty?
Primary
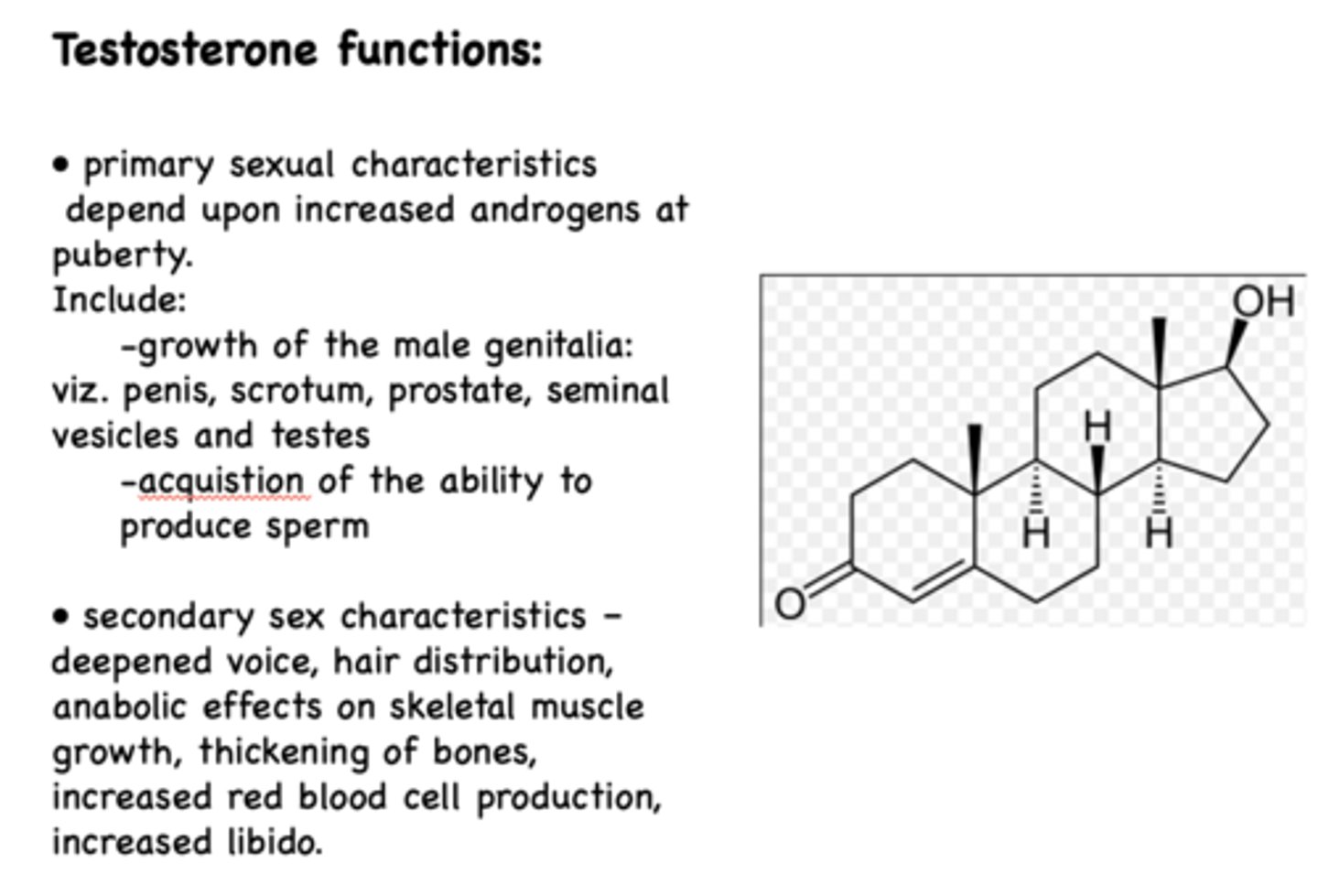
growth of the male genitalia is a ______________ sexual characteristic
primary
acquistion of the ability to produce sperm is a ______________ sexual characteristic
primary
deepened voice, hair distribution, anabolic effects on skeletal muscle growth, thickening of bones, increased red blood cell production, increased libido are _______ sexual characteristics
secondary
The _____________ is ~4-5 meters in length- sperm take from 12-26 days to travel its length - during this time, the sperm gains forward motility and undergoes changes in metabolism and shape
epididymis
in what location of the male reproductive organ does sperm gain forward motility and undergoes changes in metabolism and shape?
epididymus
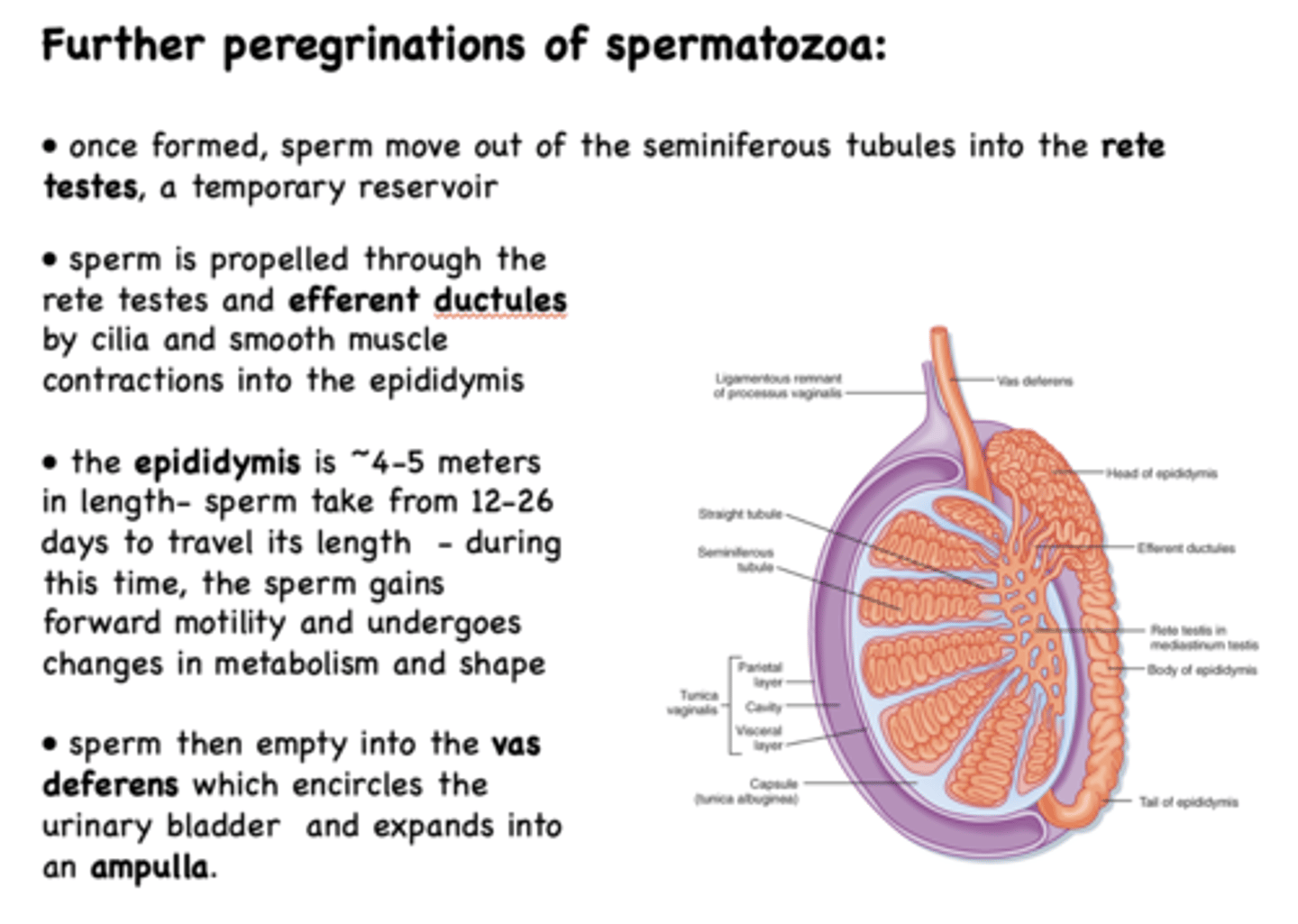
from the epididymus, sperm moves to the ______________
ductus (vas) deferens
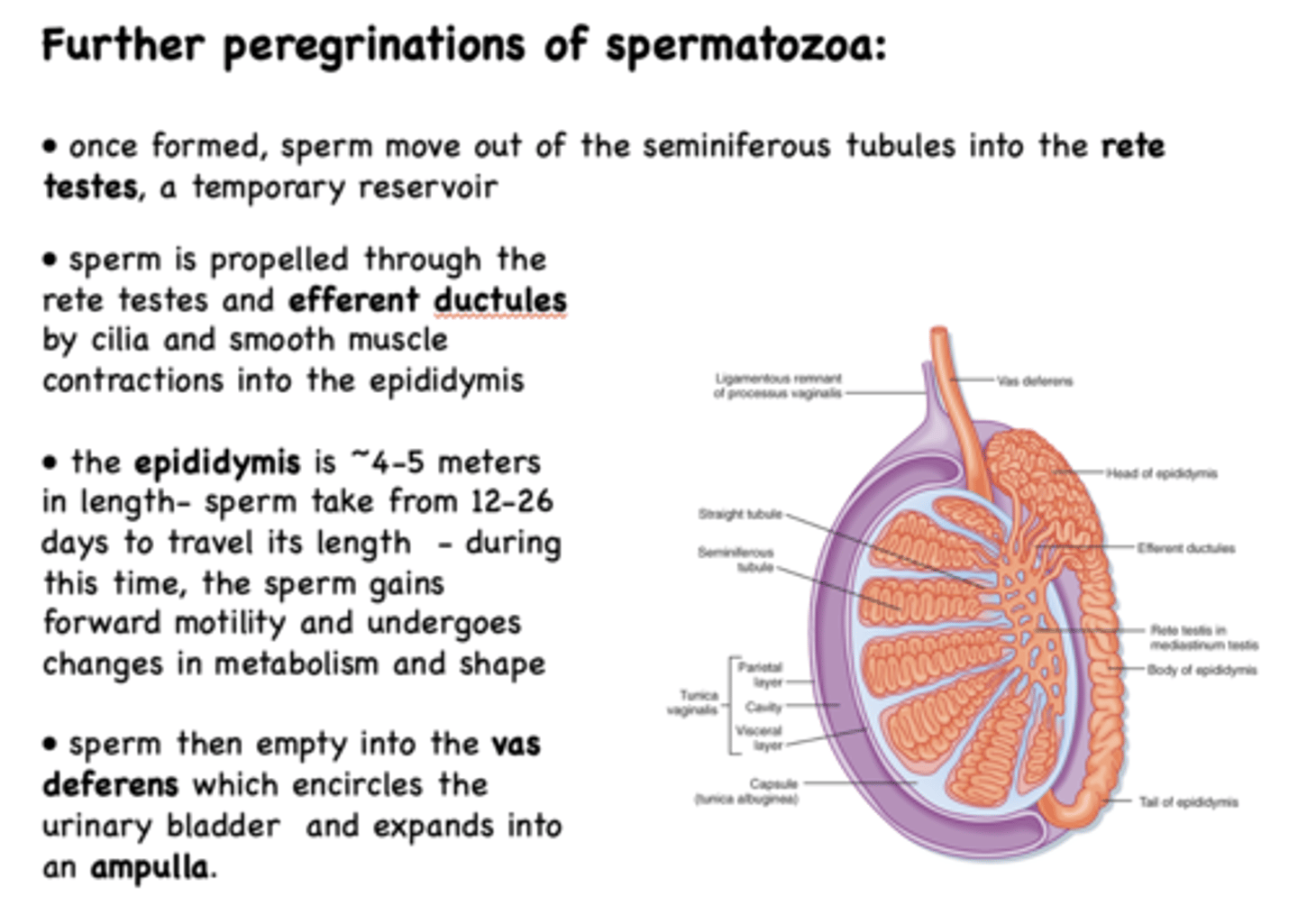
sperm then empty into the ______________ which encircles the urinary bladder and expands into an ampulla
ductus (vas) deferens
sperm empty into the vas deferens which encircles the urinary bladder and expands into the _____________
ampulla
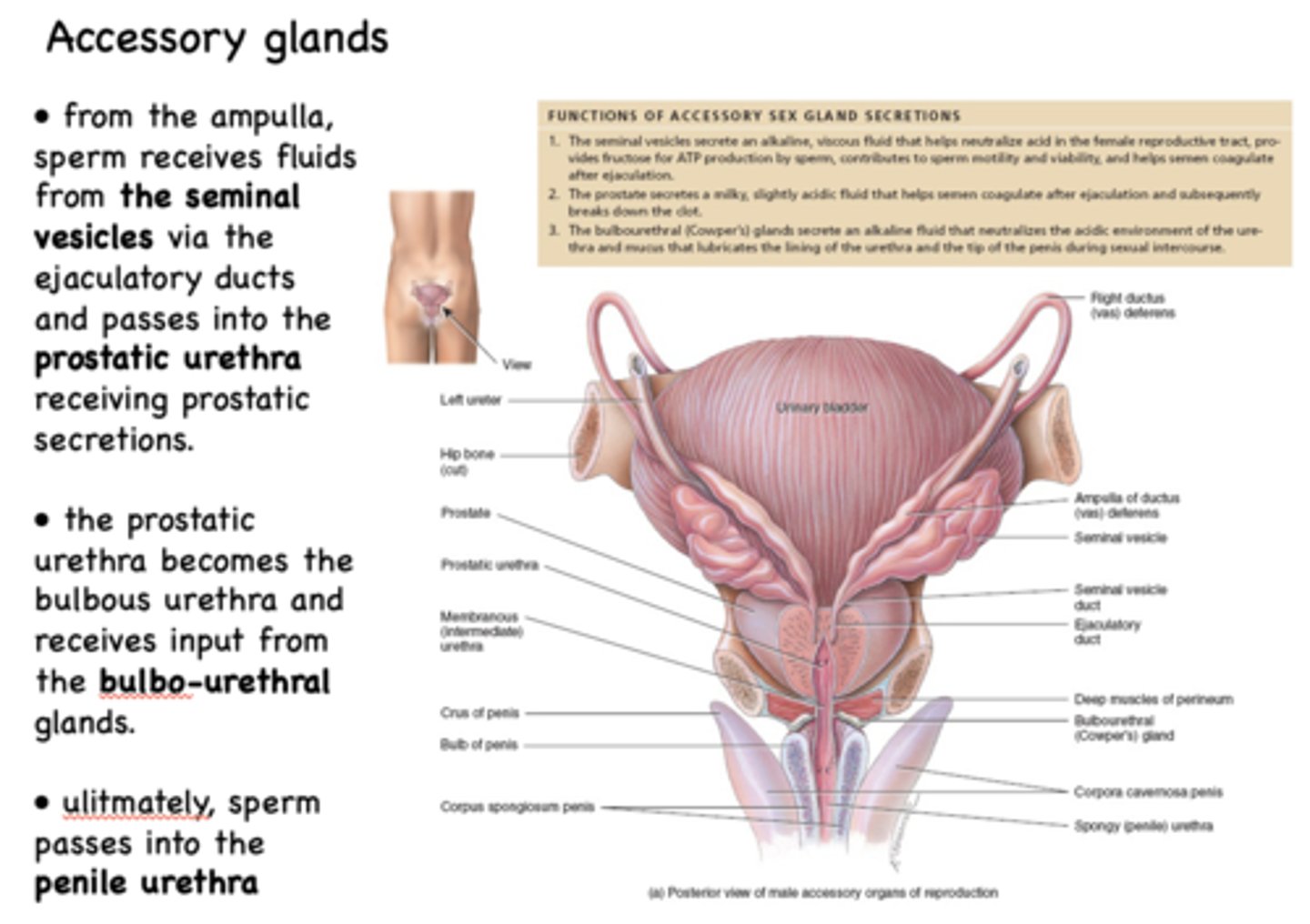
from the ampulla, sperm receives fluids from the _____________ via the ejaculatory ducts
seminal vesicles
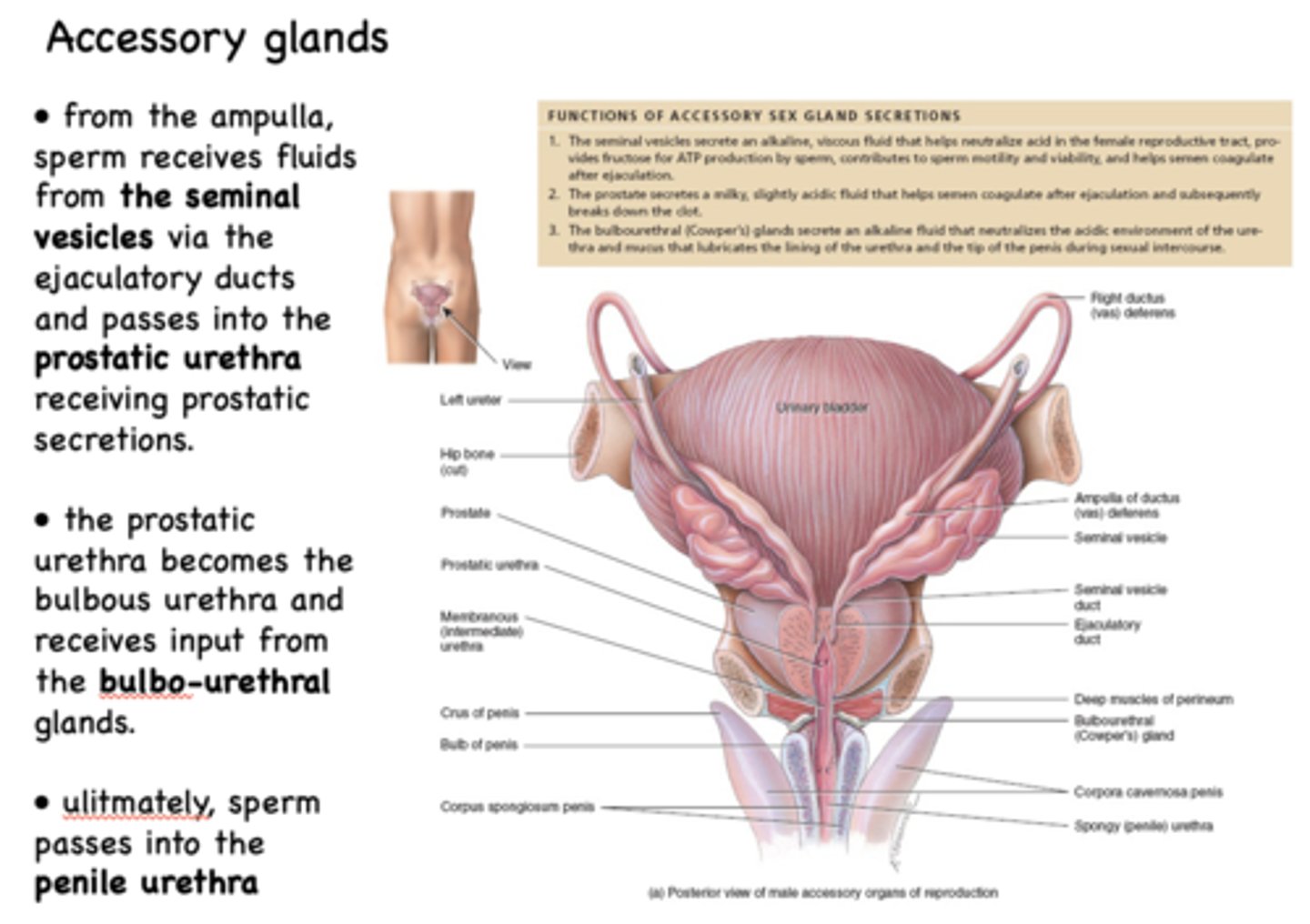
from the ampulla, sperm receives fluids from the seminal vesicles via the ejaculatory ducts and passes into the _____________ receiving prostatic secretions
prostatic urethra
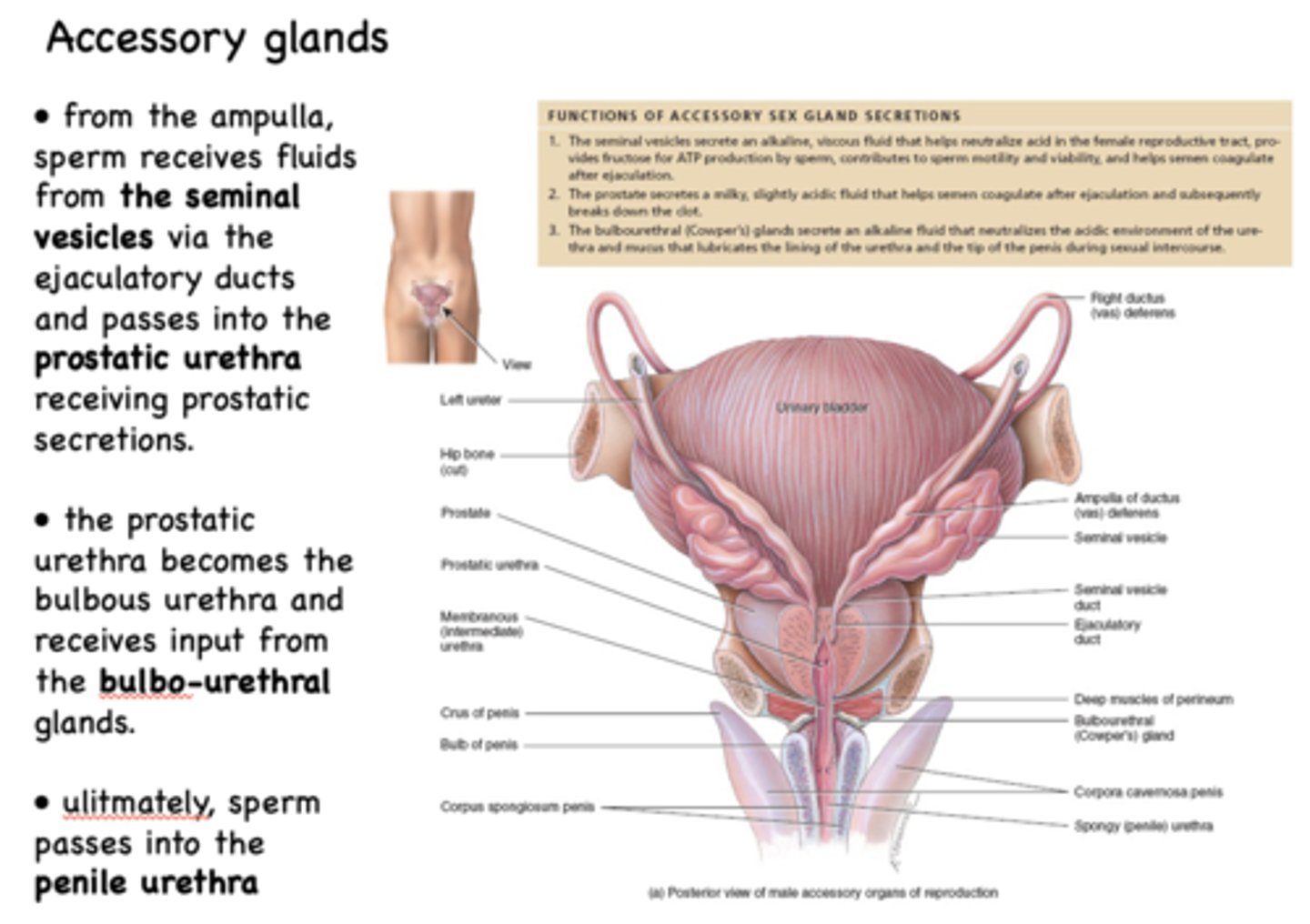
the prostatic urethra becomes the _____________
bulbous urethra
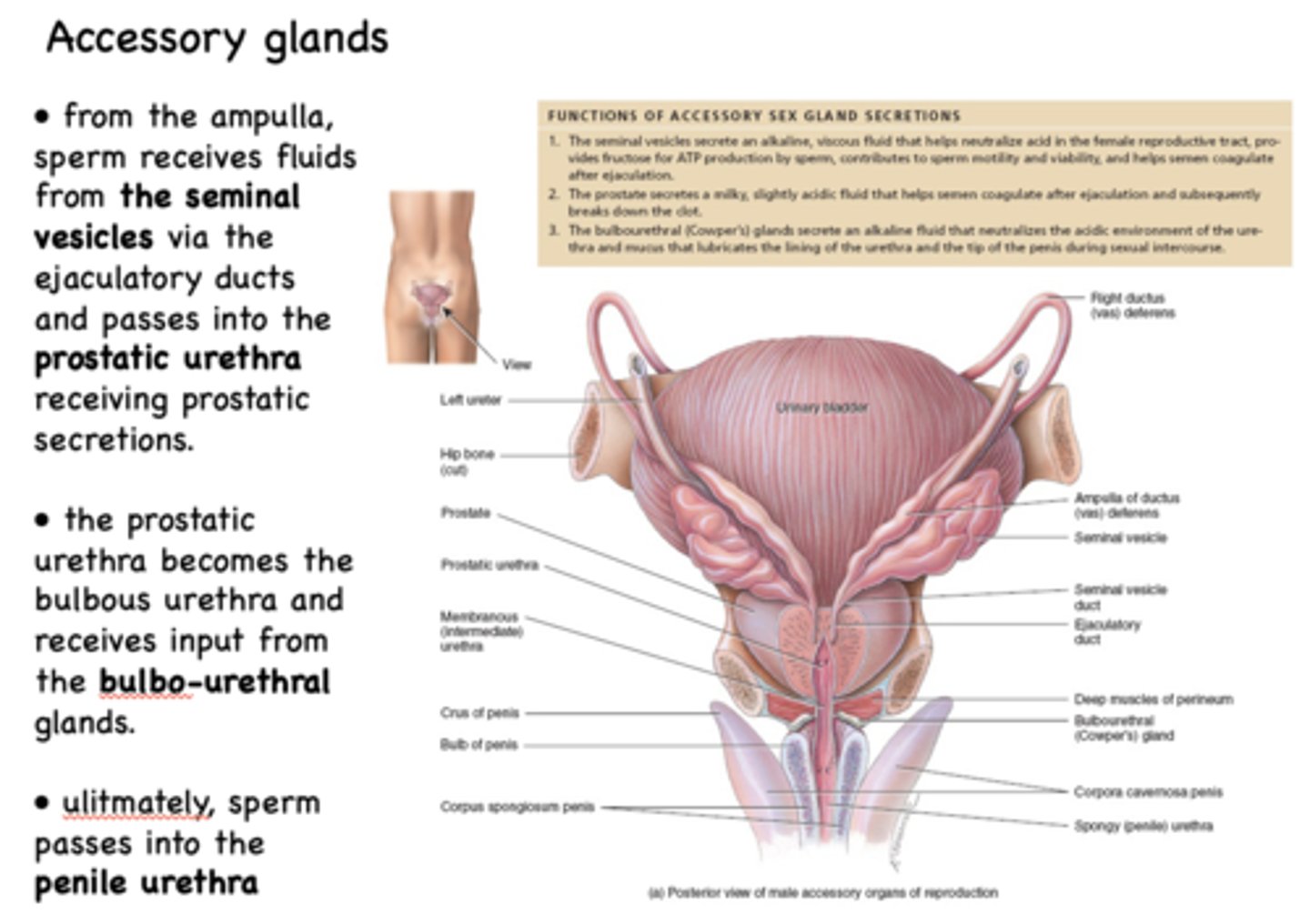
the prostatic urethra becomes the bulbous urethra and receives input from the _____________
bulbo-urethral glands
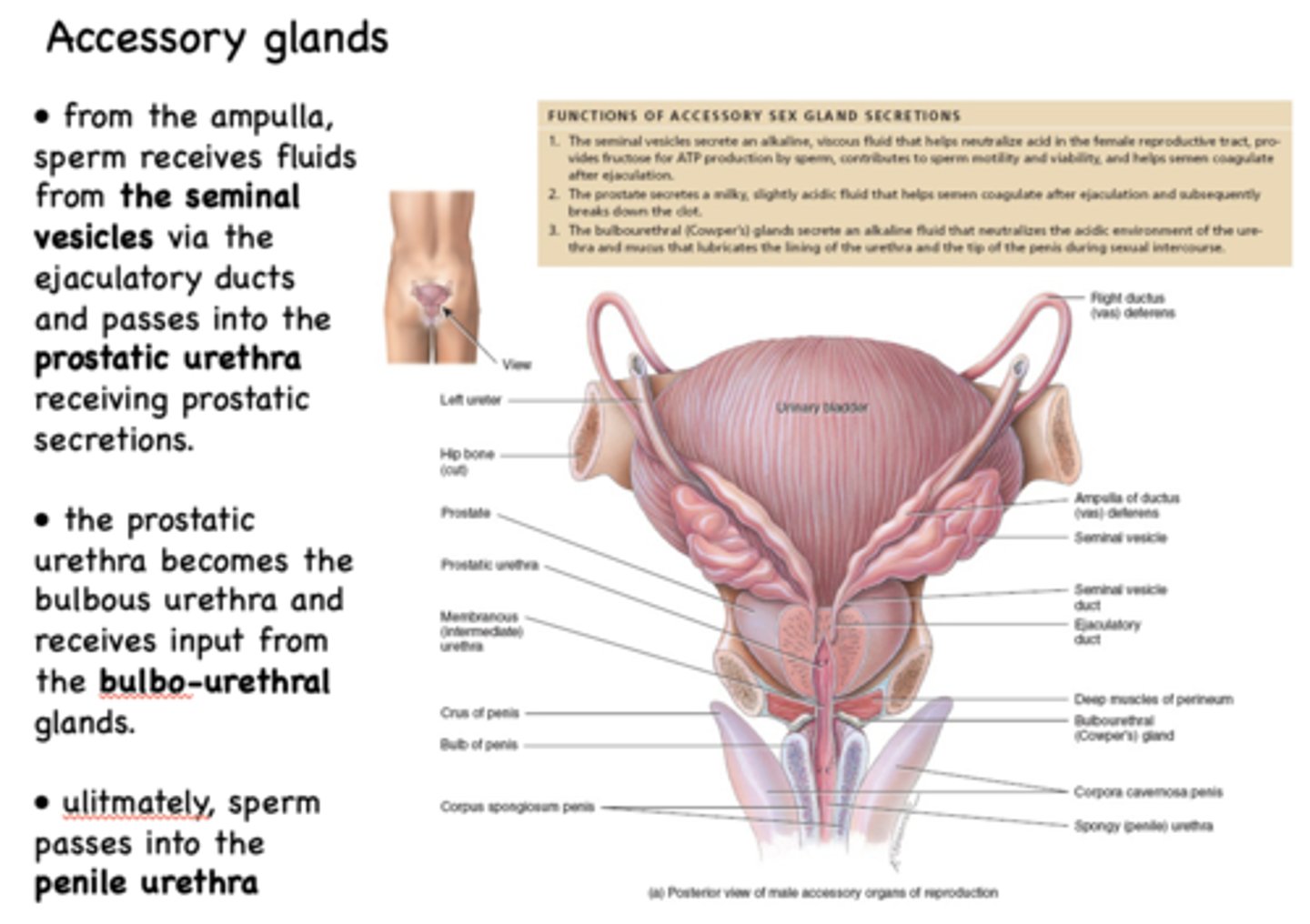
ultimately, sperm passes into the _____________
penile urethra
typical ejaculate contains _____% sperm with a small amount of fluid from the epididymis and vas deferens
10%
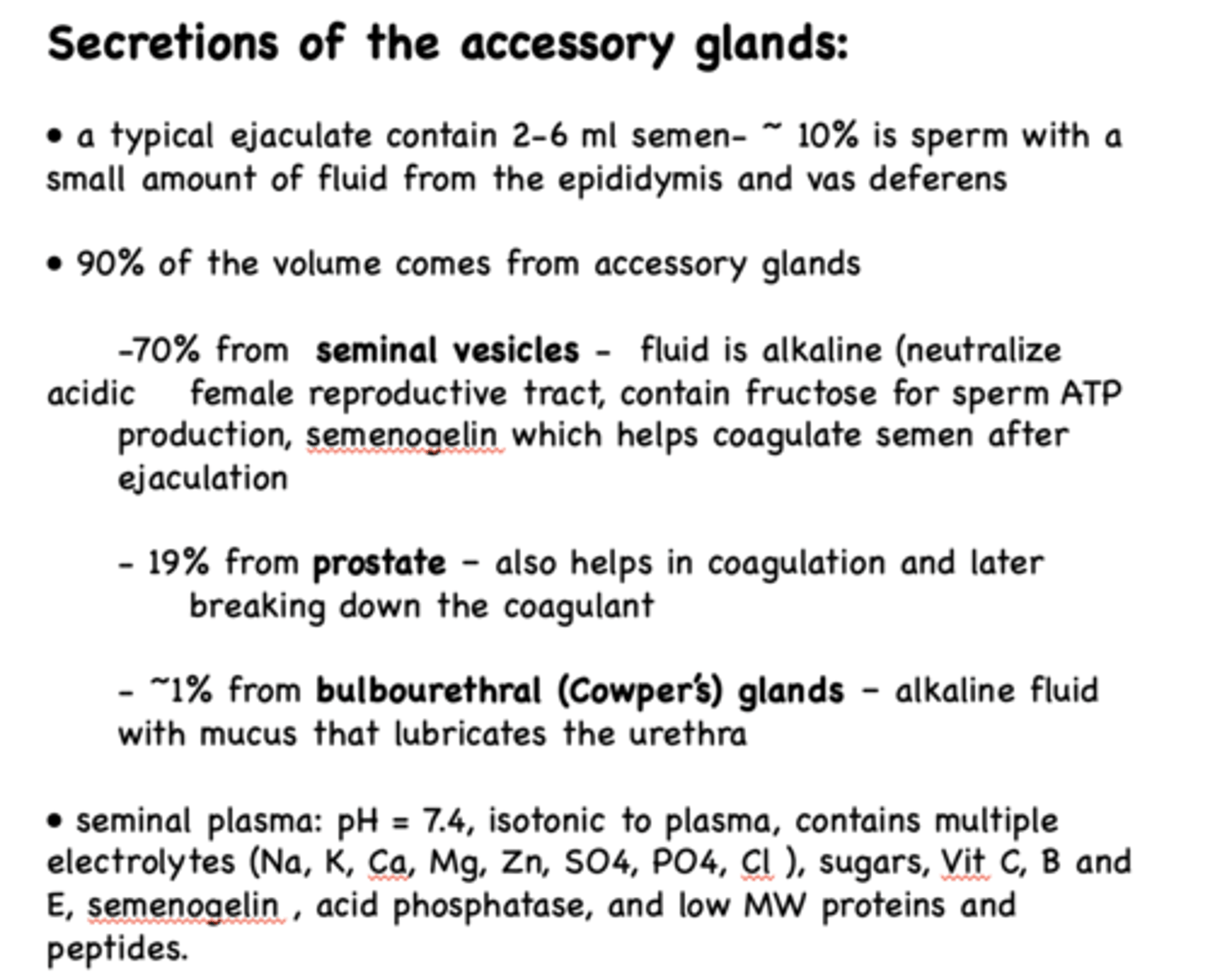
What percent of volume of ejaculate comes from accessory glands?
90%
typical ejaculate contains ____% from the seminal vesicles
70%
typical ejaculate contains _____% from the prostate
19%
typical ejaculate contains ___% from the bulbo-urethral glands
1%
What has the following characteristics:
- Fluid form here is alkaline
- Neutralize acidic female reproductive tract
- Contain fructose for sperm ATP production
- Semenogelin which helps coagulate semen after ejaculation:
seminal vesicles
fluid formed in ___________ also helps in coagulation and later breaking down the coagulant
prostate gland
fluid form in ___________ is alkaline fluid with mucus that lubricates the urethra
bulbo-urethral glands
What is the pH of the seminal plasma?
7.4
in terms of tonicity, seminal plasma is _______ to plasma
isotonic
T/F: The testes, epididymis, accessory glands and erectile tissue are all innervated by sympathetic and parasympathetic systems - penis also has afferent and efferent connections to the somatic nervous system
True
The male sex act involves what three processes?
- Erection
- Emission
- Ejaculation
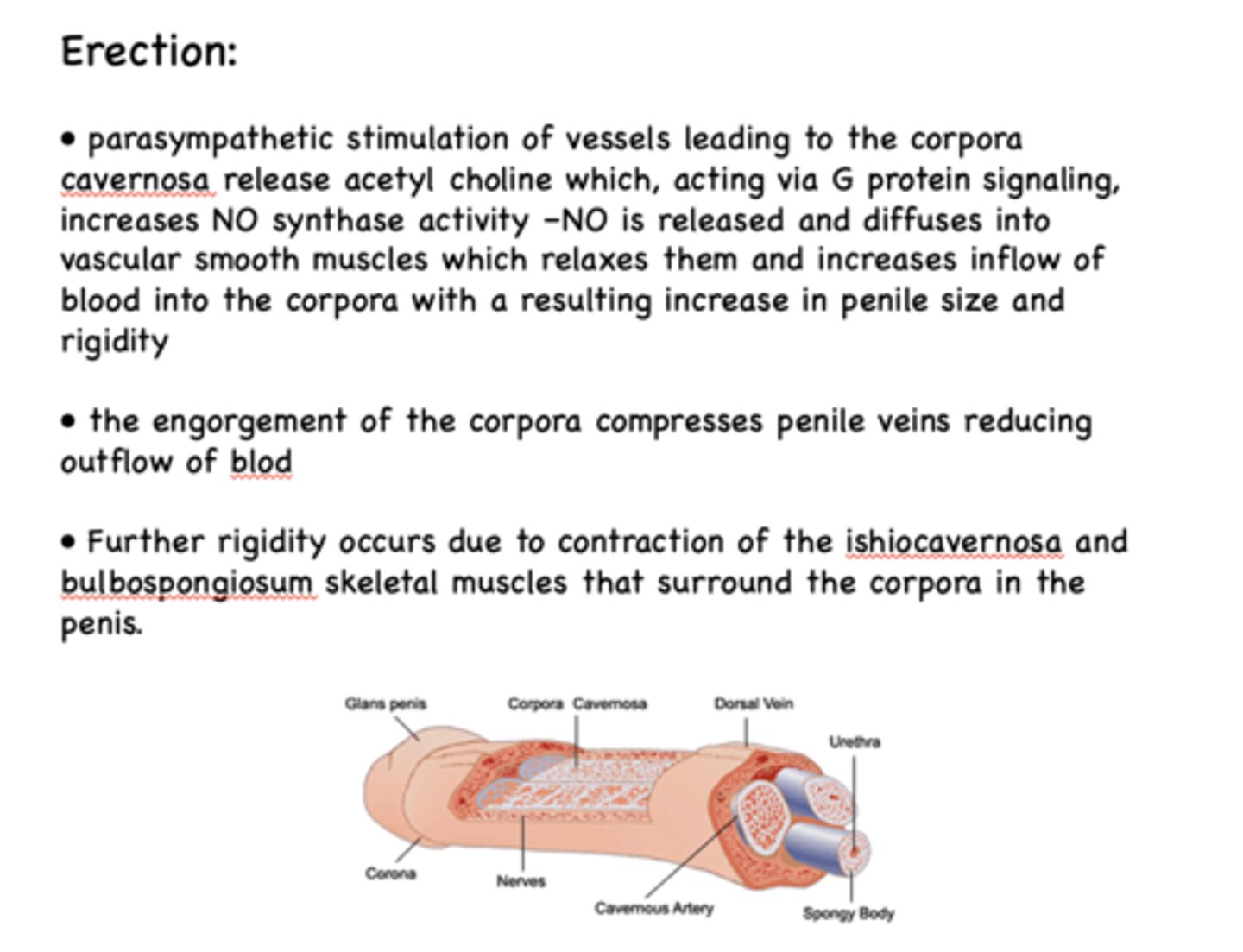
What has the following characteristics:
- Parasympathetic stimulation of vessels leading to the corpora cavernosa release ACh which, acting via G protein signaling, increases NO synthase activity
–NO is released and diffuses into vascular smooth muscles which relaxes them and increases inflow of blood into the corpora with a resulting increase in penile size and rigidity
erection
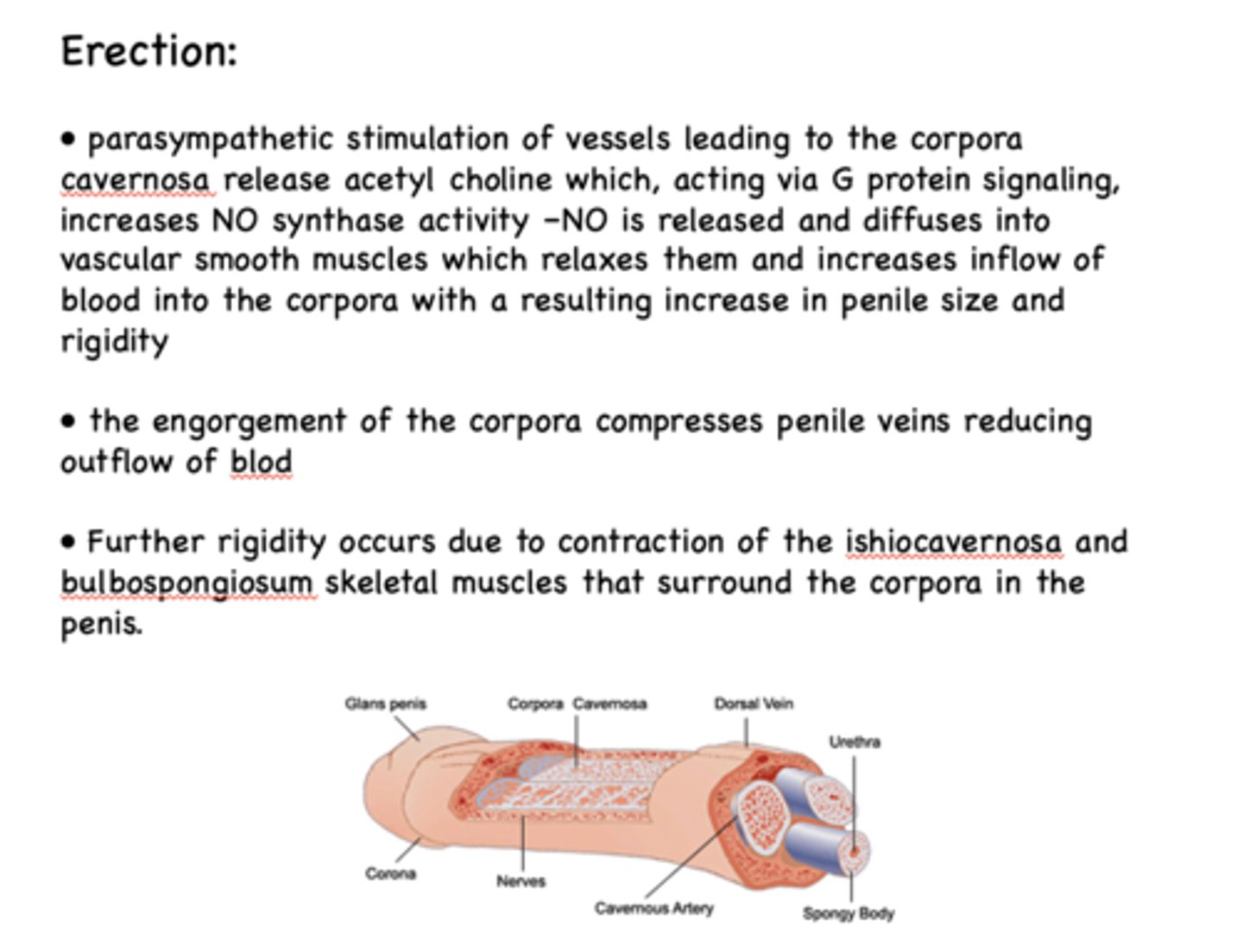
erection is a process controlled by _________ stimulation
parasympathetic
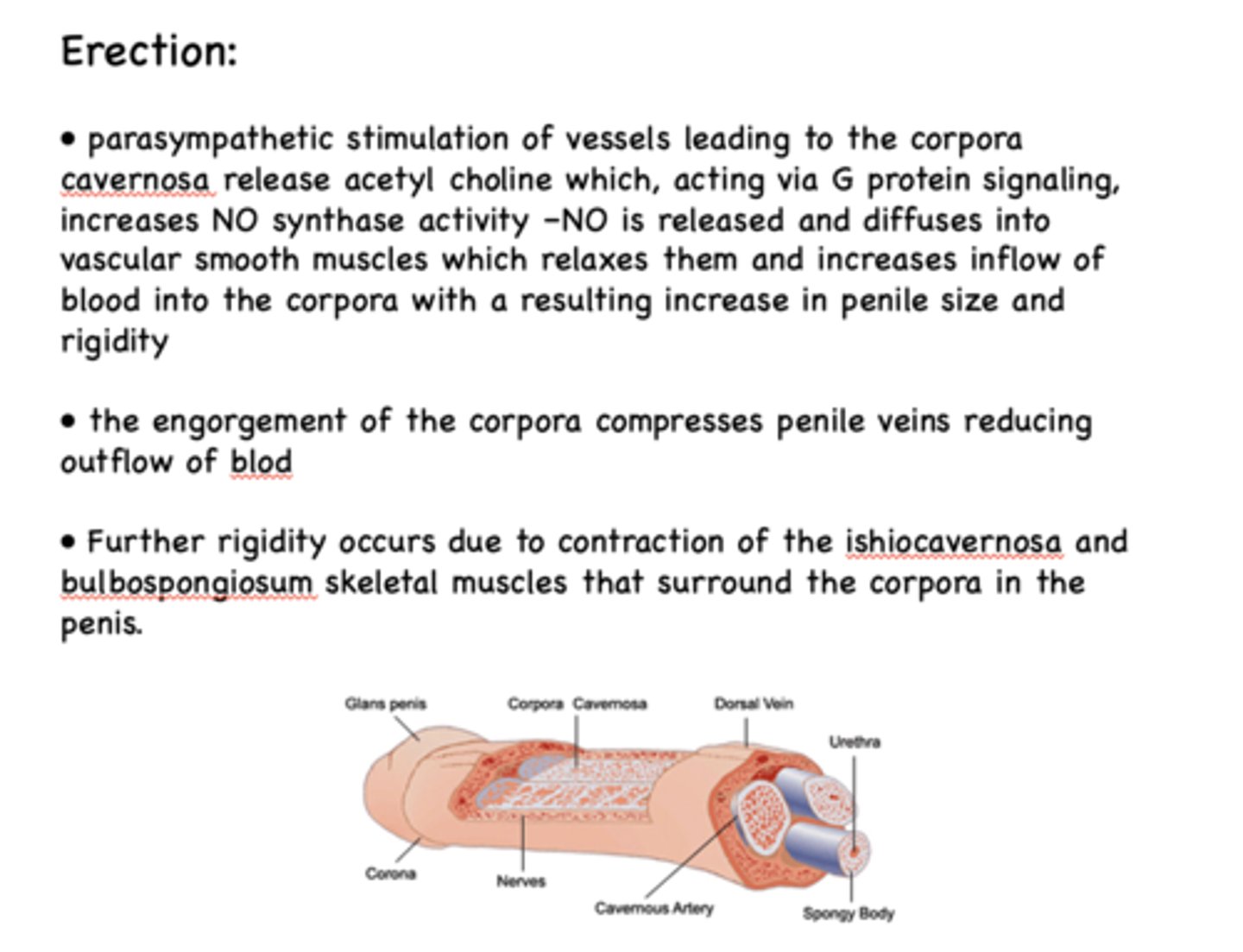
The engorgement of the ___________ compresses penile veins reducing outflow of blood
Corpora
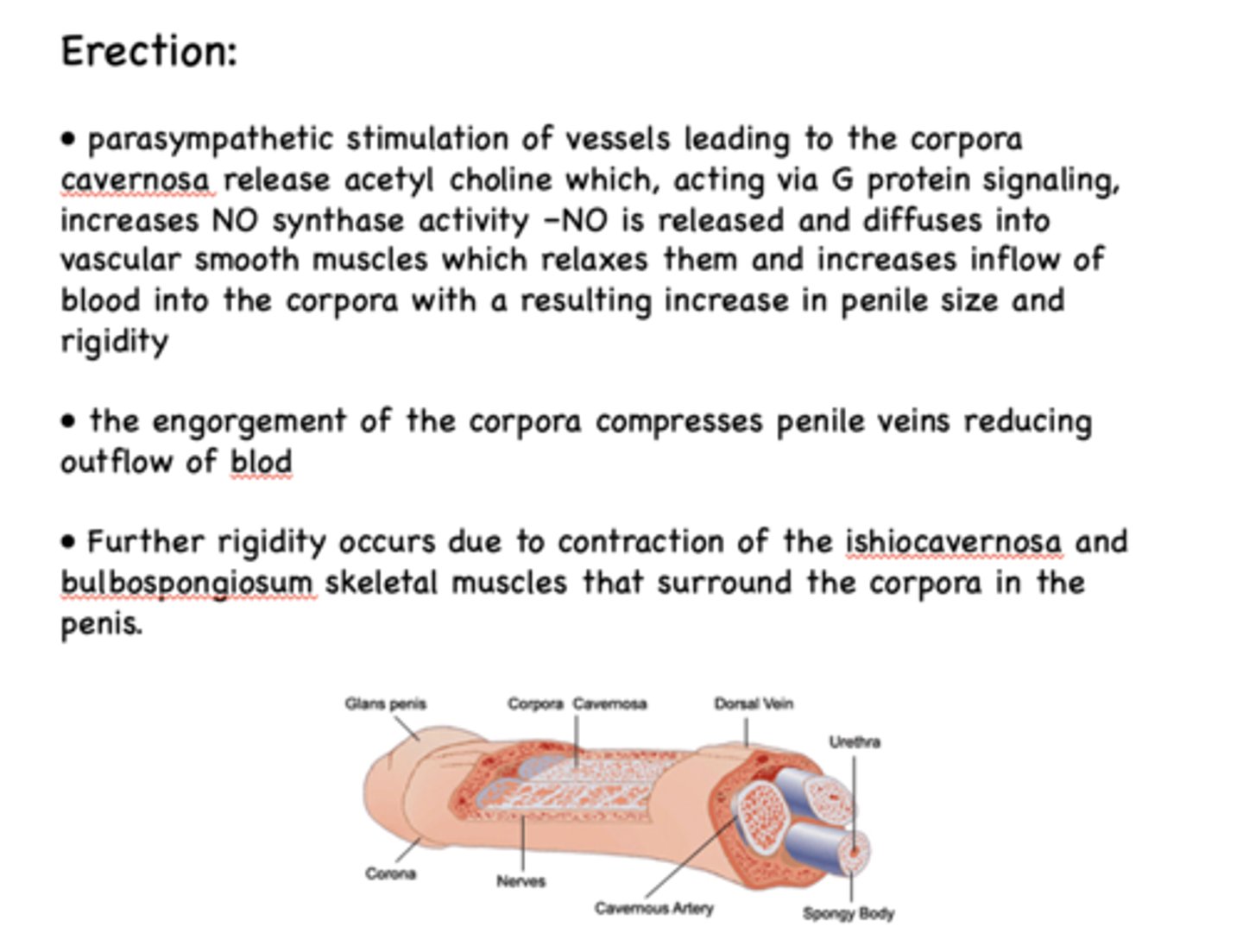
Rigidity occurs due to contraction of the ishiocavernosa and bulbospongiosum skeletal muscles that surround the ___________ in the penis
Corpora
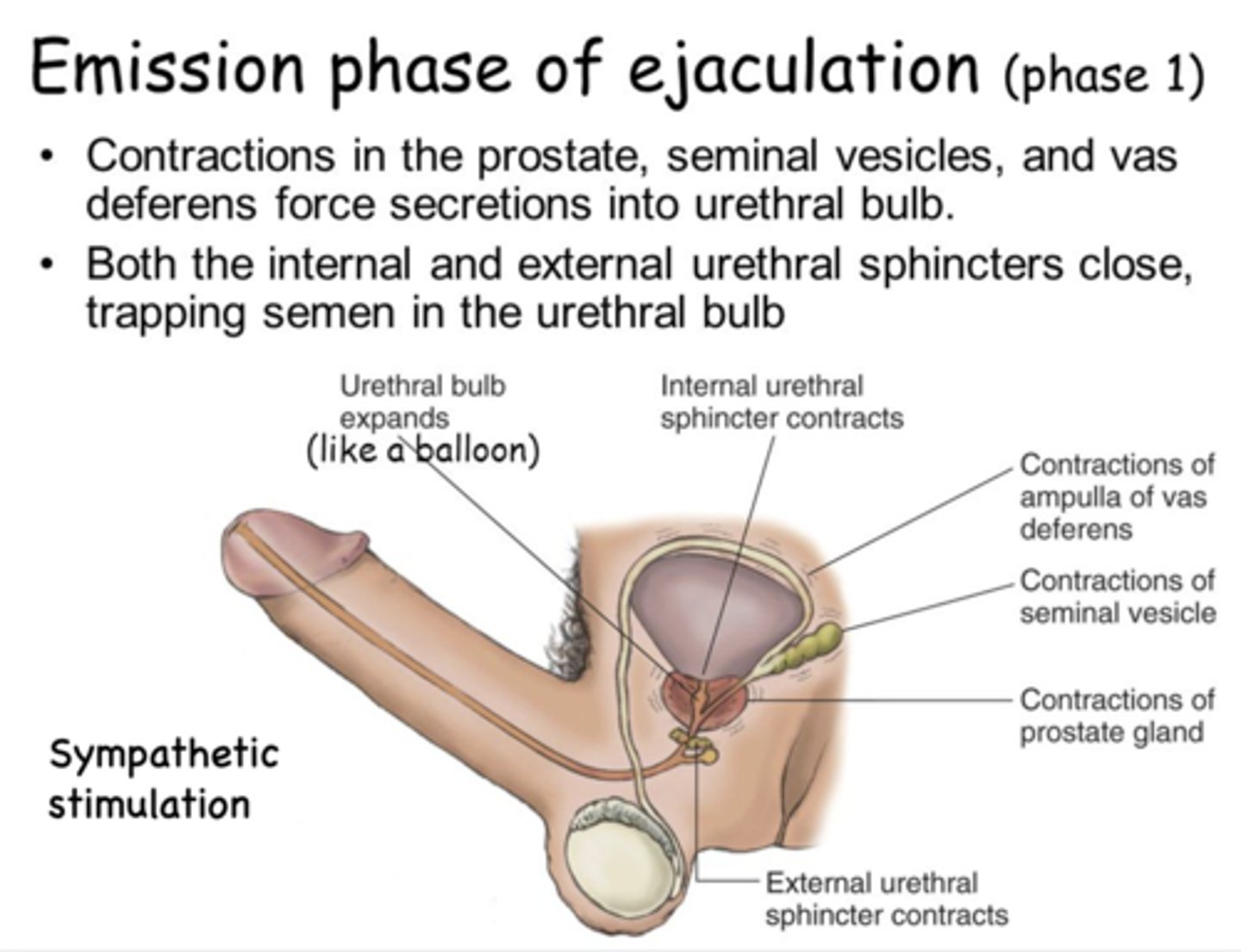
What ejaculation phase has contractions of the prostate, seminal vesicles, and vas deferens force secretions into the urethral bulb?
emission phase of ejaculation
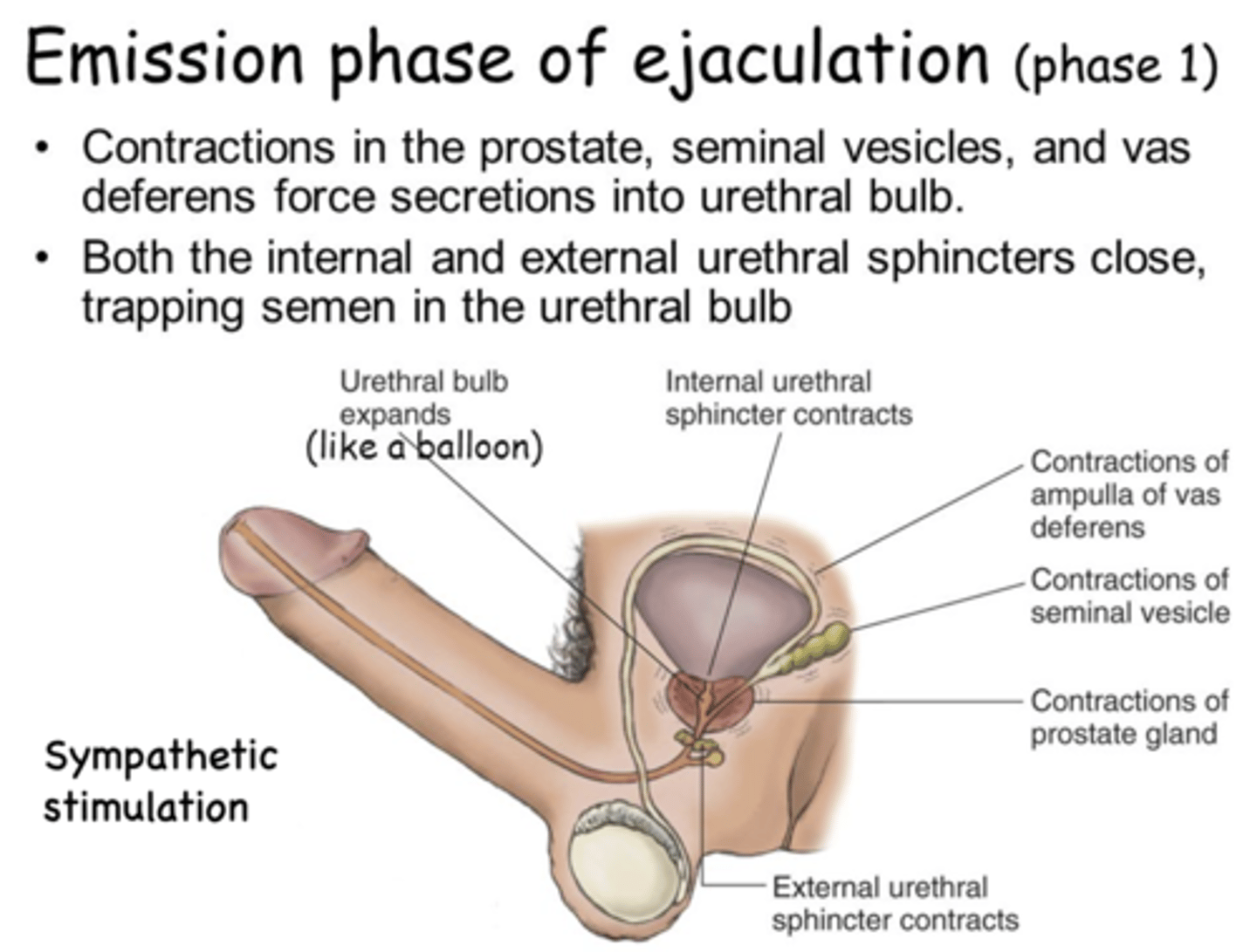
What ejaculation phase do the internal and external urethral sphincters close, trapping semen in the urethral bulb (like a balloon)?
emission phase of ejaculation
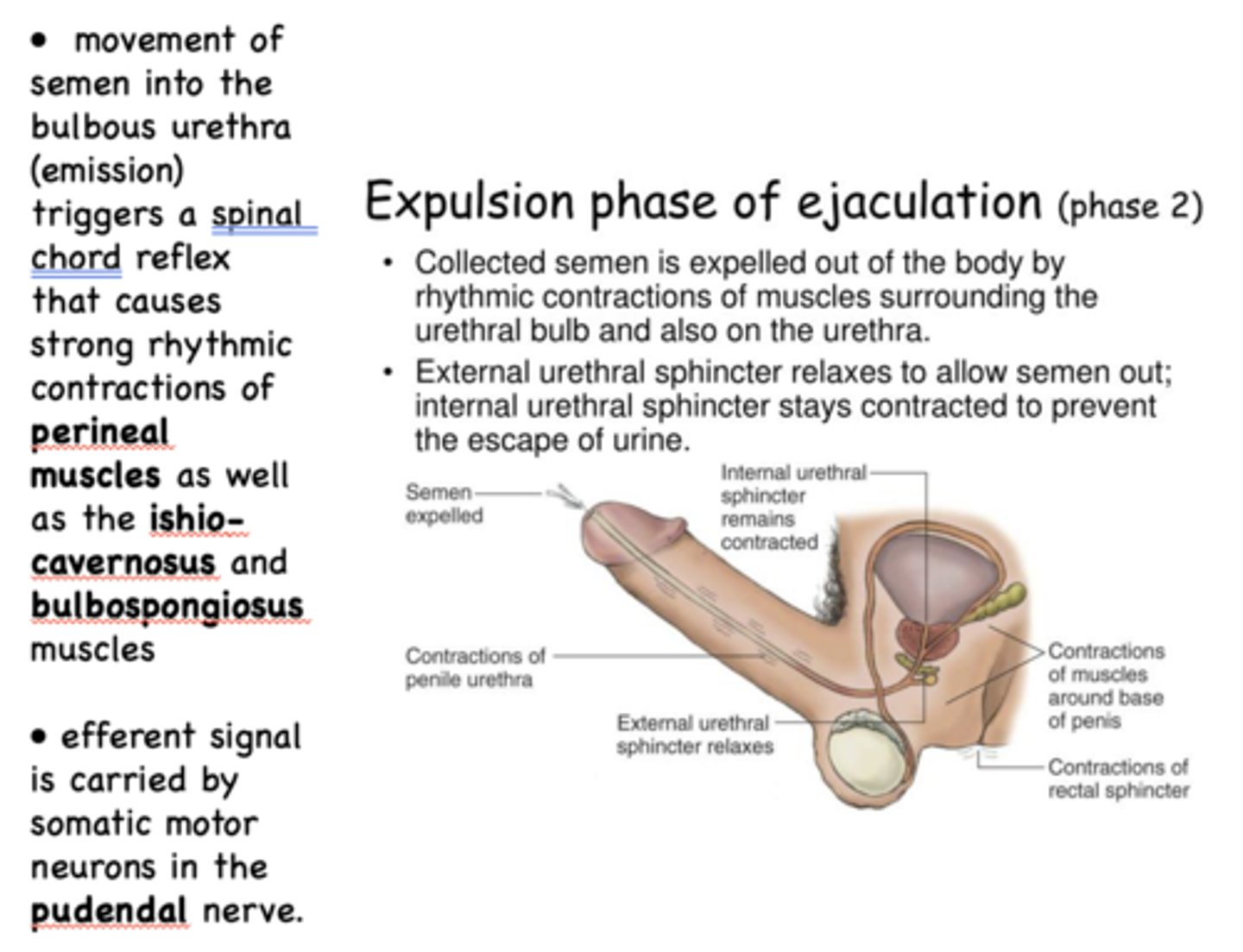
What ejaculation phase is collected semen is expelled by rhythmic contractions of the surrounding muscles?
expulsion phase of ejaculation
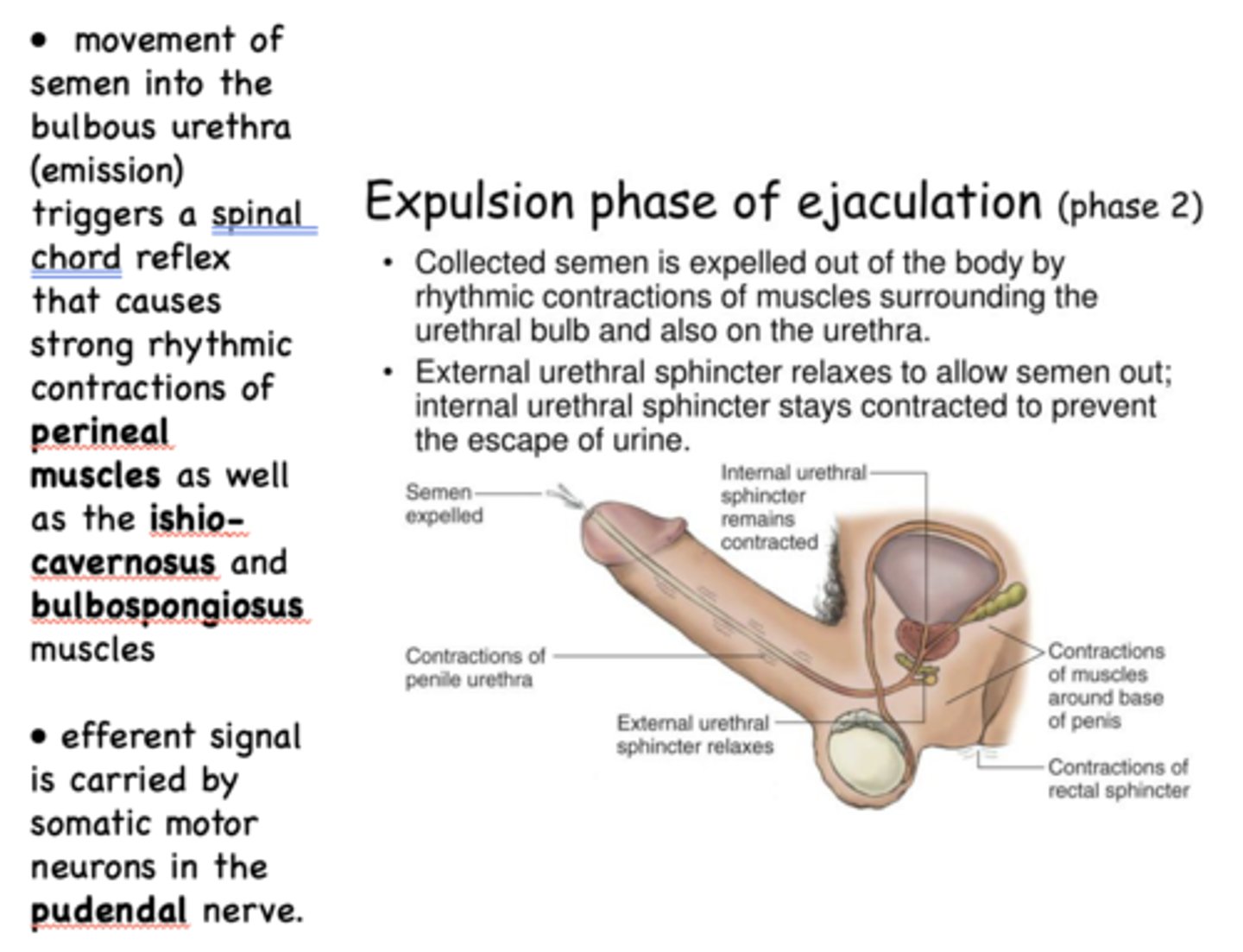
In expulsion phase of ejaculation, external urethral sphincter ______ to allow semen out, while internal urethral sphincter ________ to prevent urine flow
external: relaxes
internal: contracts
the emission phase of ejaculation is a process controlled by _________ stimulation
sympathetic
movement of semen into the bulbous urethra (emission) triggers a spinal chord reflex that causes strong rhythmic contractions of 3 muscles:
- Perineal muscles
- Ishio-cavernosus muscles
- Bulbospongiosus muscles
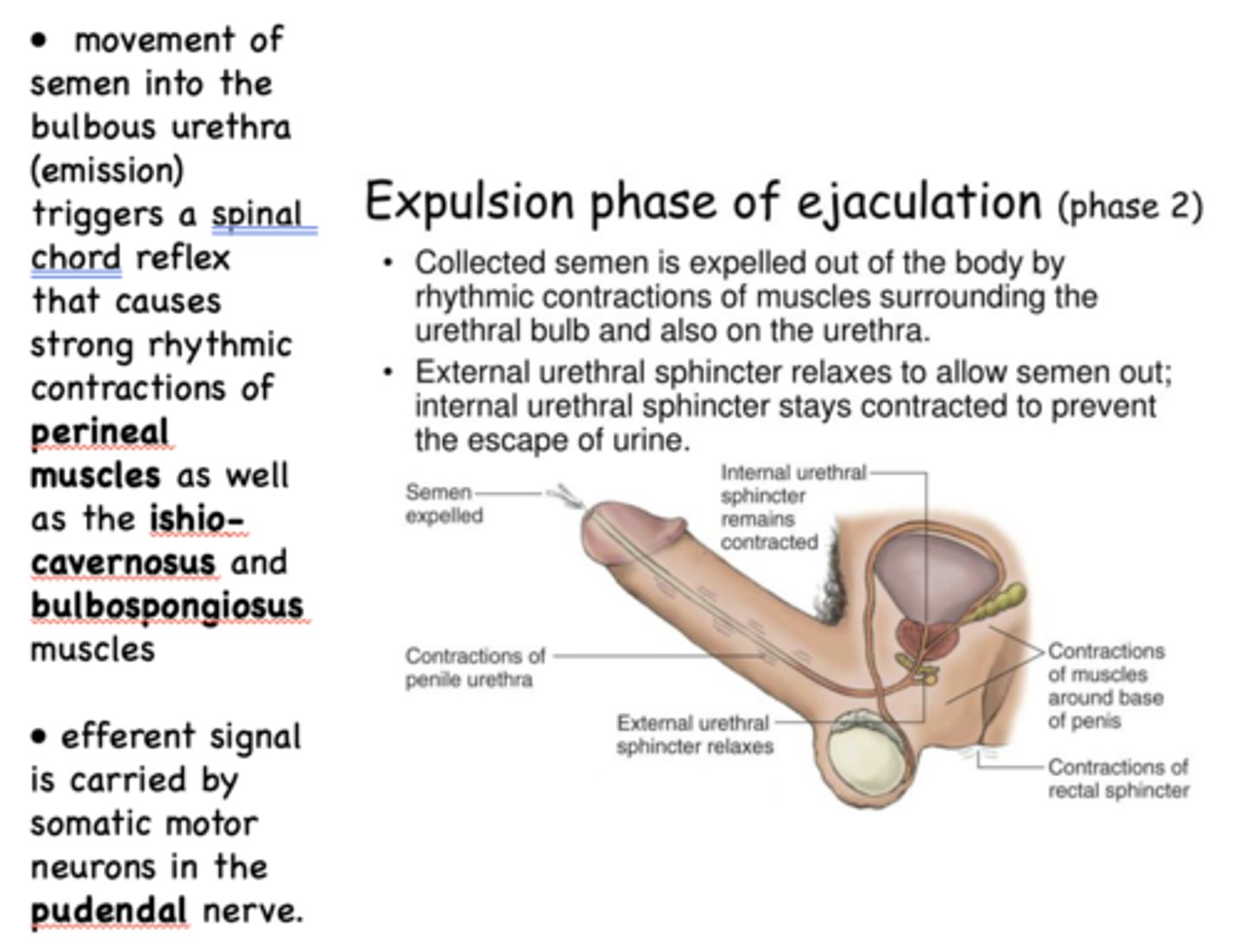
during the expulsion phase of ejaculation, efferent signal is carried by somatic motor neurons in the ___________ nerve
pudendal
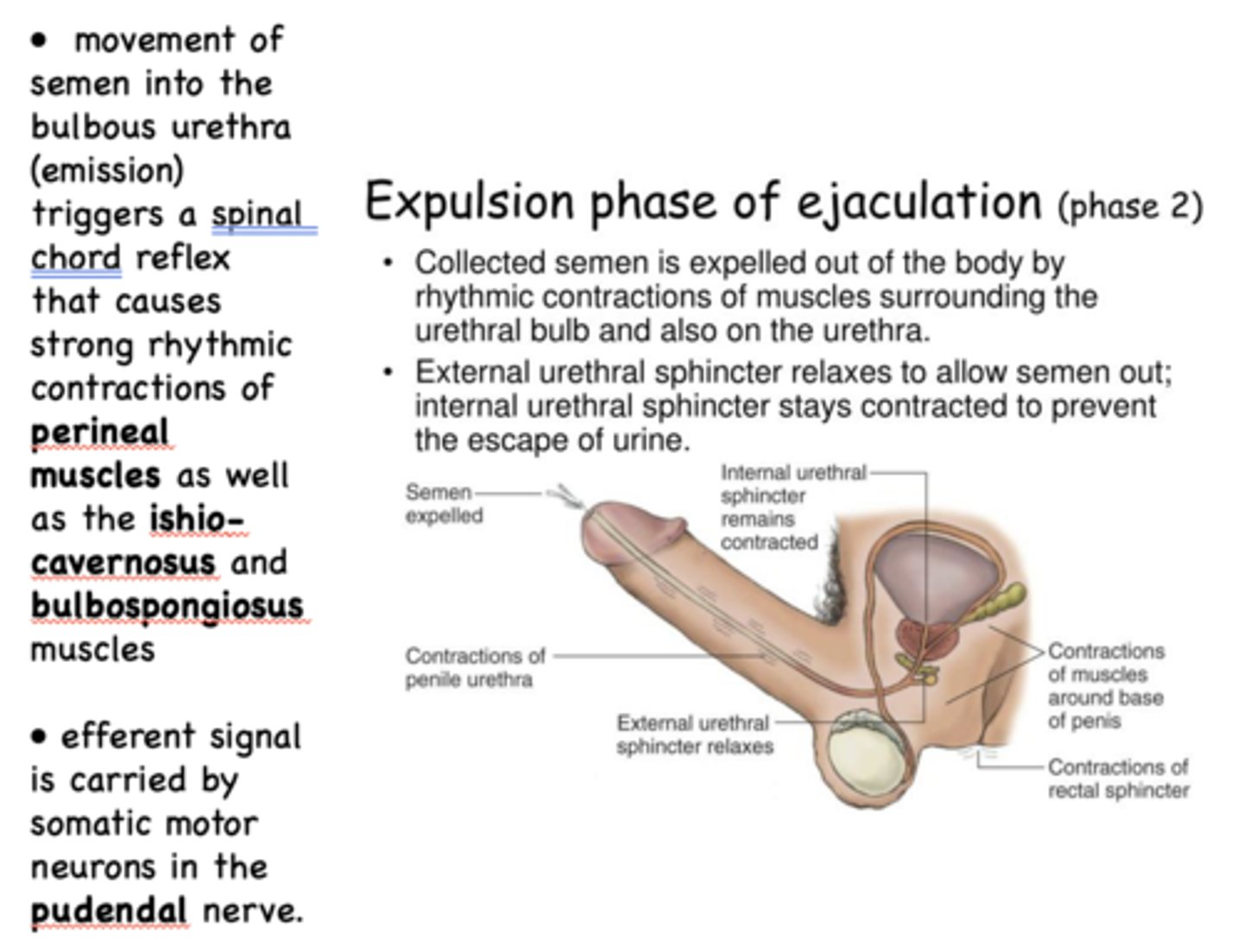
during the expulsion phase of ejaculation, the internal sphincter is _______
contracted
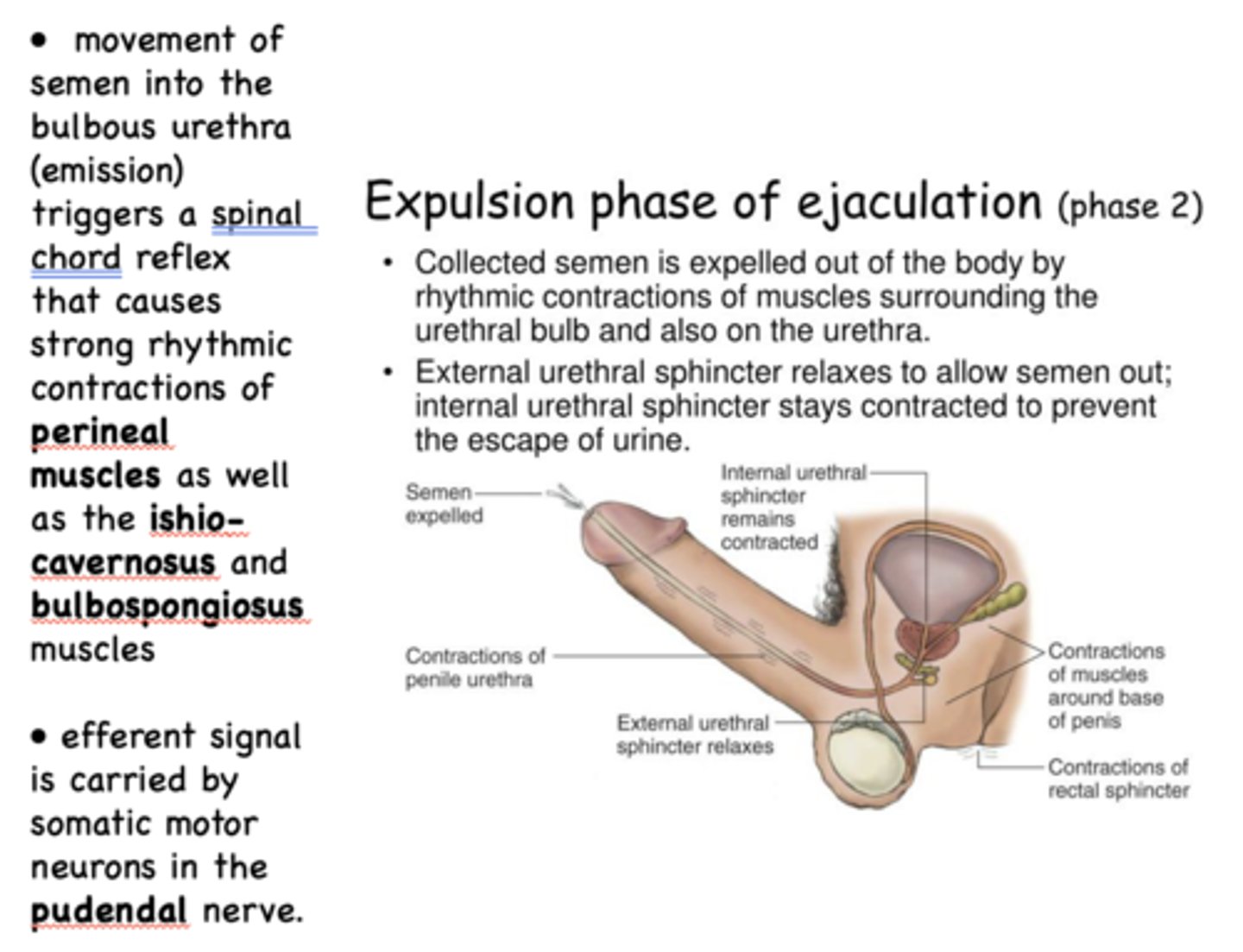
during the expulsion phase of ejaculation, the external sphincter is _______
relaxed
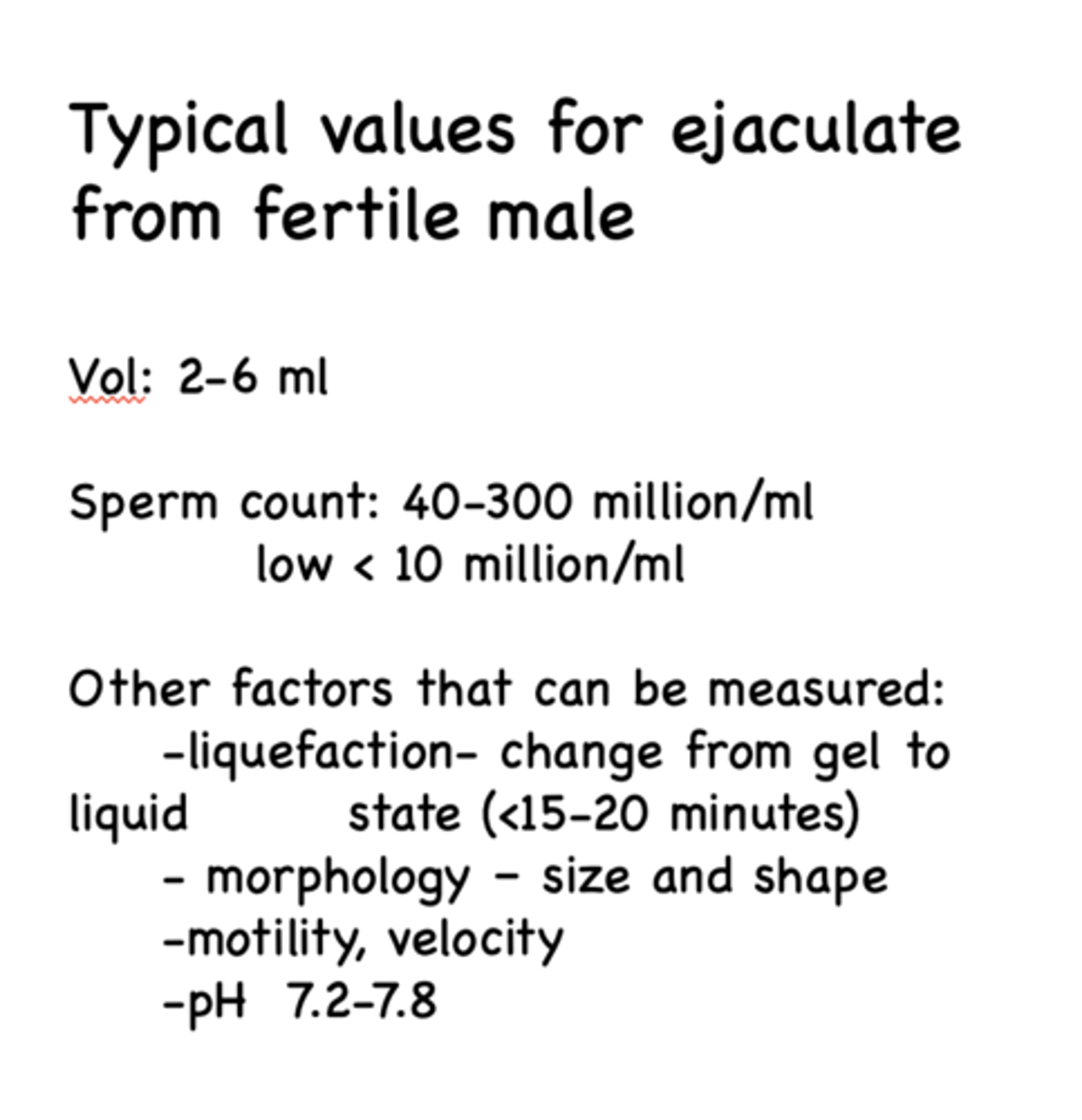
about how much sperm is found from ejaculate from fertile male?
40-300 million/ml
what are some factors that can be measured for ejaculate from fertile male?
- Liquefaction
- Morphology
- Motility/velocity
- pH