Lecture 36: Seizure and Epilepsy in adults
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
73% at four years
after two unprovoked non-febrile seizures, the chance of having another is
seizure
a transient occurrence of signs or symptoms due to abnormal excessive or synchronous neuronal activity in the brain
epilepsy
•a chronic disease of the brain characterized by an enduring predisposition to generate epileptic seizures, and by the neurobiological, cognitive, psychological, and social consequences of this condition
•the occurrence of two unprovoked seizures occurring at least 24 hours apart .
-at least two unprovoked seizures more than 24 hours apart
-one unprovoked seizures and a probability of further seizures
-at least two seizures in a setting of reflex epilepsy
What criteria is required to define epilepsy?
-individuals who had an age dependent epilepsy syndrome but are now past the applicable age
-seizure free for at least 10 years off seizure medications
epilepsy is considered to be no longer present for...
generalized onset seizures
what type of seizure
-originating at some point within rapidly engaging bilaterally distributed networks
focal onset seizure
what type of seizure?
defined as originating within networks limited to one hemisphere. May originate in subcortical structures
yes! but they still have to rapidly engage in bilaterally distributed networks
can generalized seizures be asymmetric?
absence seizures
all nonmotor seizures are considered
level of awareness
focal seizures are classified by
absence seizures
•Childhood or teenage onset
•Sudden onset, without aura, prompt offset
•Momentary loss of consciousness
•Eyelid flutter/minor automatisms
•3-15 seconds duration
•Family History
3 Hz spike-wave/HV sensitive
EEG of absence seizures:
tonic seizures
-sudden stiffening
-extension maximal in arms
-a few seconds in duration
-associated with falls and injury
-refractory the therapy
tonic seizures
what type of seizure is extra-temporal in origin and refractory to therapy
flattening/high frequency discharge
EEG of tonic seizures:
atonic seizure
-abrupt onset
-sudden loss in tone
-head drop/falls/injuries
-a second or two in duration
-poor response to AEDs
-poor overall prognosis
slow spike-wave/flattening
EEG of atonic seizure
myoclonic seizures
-sudden jerks
-usually bilateral, maximal in arms
-one second in duration
-often multiple
-may be photic or sensory triggered
-often maximal on awakening
generalized polyspike-wave burst
EEG of myoclonic seizure:
tonic-clonic seizures
•Loss of Consciousness
•May have a focal or generalized onset
•Tonic Extension of limbs (about 20-40 sec)
•Evolves to rhythmic clonic jerking of extremities (about 30-50 secs)
•Cessation of breathing, tongue biting, incontinence
•Post-ictal sleep
variable, often obscured
EEG of tonic-clonic seizure
•occurs abruptly and includes limb extension bilaterally
-Air ejected forcefully against tightened vocal cords is responsible
for the "epileptic cry" associated with a tonic-clonic seizures.
describe the tonic phase of a TCS:
epileptic cry
-occurrs during tonic phase of TCS
-air ejected forcefully against tightened vocal cords
synchronous muscle contraction
describe the clonic phase of TCS:
simple partial seizures
focal seizures without impairment of consciousness are aka
focal seizures without impairment of consciousness
what type of seizure:
•Motor, sensory, psychic or autonomic signs or symptoms
•Preservation of consciousness & awareness
•May progress to dyscognitive seizures or tonic-clonic seizures
interictal-focal sharp or slow; ictal-rhythmic discharge or often normal
EEG of simple partial seizures
complex partial seizures
focal discognitive seizures are aka
complex partial seizures
what kind of seizure?
•Altered consciousness/awareness
•Duration 30 secs to 3 min
• Purposeless automatisms – Arms– Oral
•Amnesia
•Semiology varies with site of origin
interictal-sharp waves or spikes; ictal-focal or bilateral rhythmic sharp
EEG of focal dyscognitive seizures
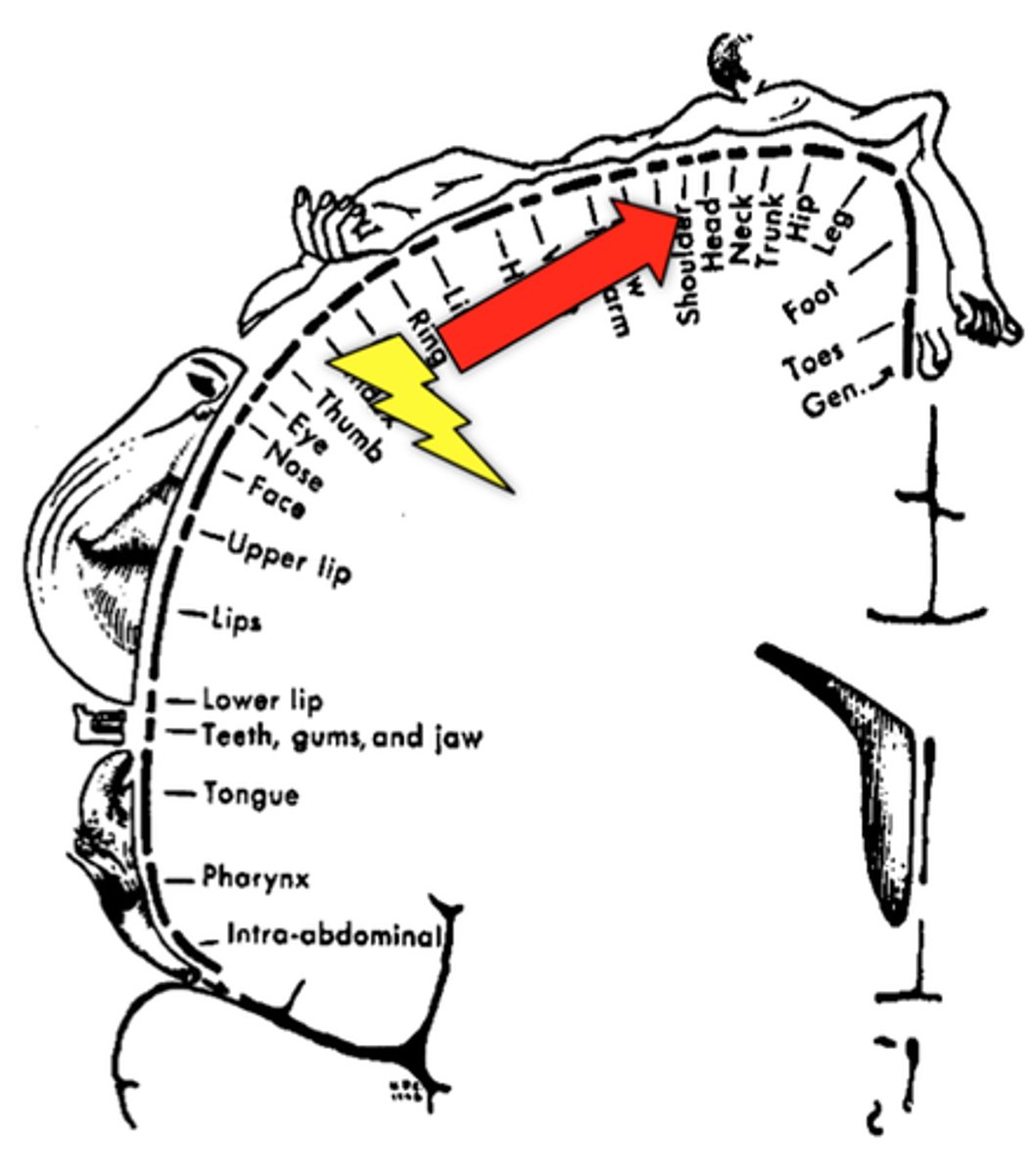
Jacksonian March
The wave-like movement of a seizure from a point of focus to other areas of the brain.
-focal seizure in adults
-has a large cortical representation
symptom
syndrome
seizure is a _____ and epilepsy is a _________
-too much excitation by NT glutamate, aspartate; too much sodium or calcium influx
AND/OR
-too little inhibition by NT GABA; inward chloride or outward potassium currents
cellular mechanisms of seizure generation:
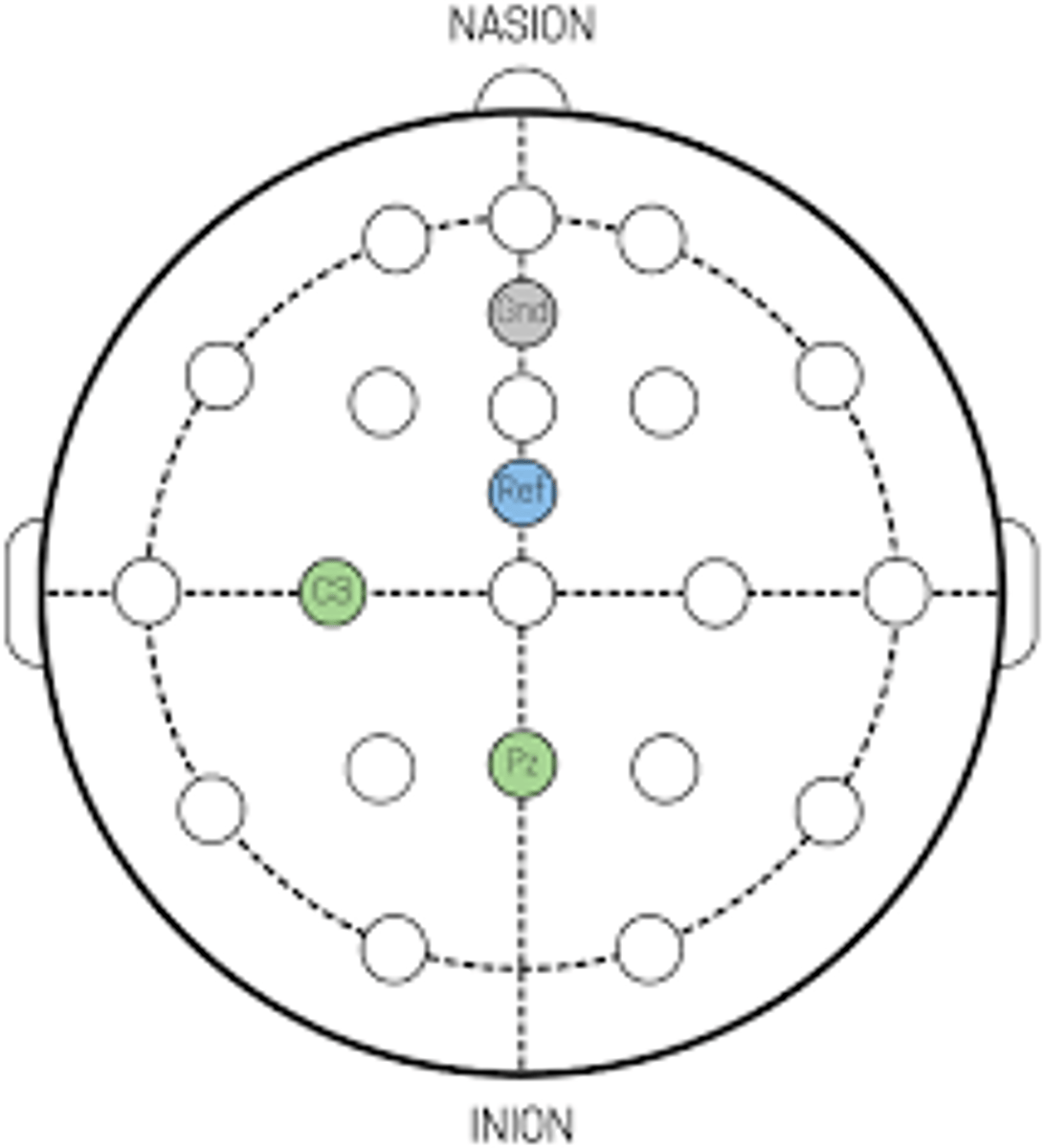
10/20 placement
electrode placement for evaluating seizure/epilepsy in adults:
-precipitants
-metabolic and electrolyte imbalance
-intoxication
-withdrawal
-sleep deprivation
-hormonal variations
-stress
-fever
-concussion
questions to consider when evaluating seizure:
-family hx, hx of febrile seizures, hx of head trauma, hx of meningitis, hx of stroke or other structural lesions
main risk factors for seizure:
CBC, electrolytes, glucose, calcium, magnesium, phosphate, hepatic and reenal function
blood tests to order for evaluation of a first seizure
•Lumbar puncture only if meningitis or encephalitis suspected and potential for brain herniation is ruled out
why would you order an LP for evaluation of a first seizure?
sodium inactivation
Phineas' Lamborghini Car Tops Vals
what mechanism do these AED drugs use?
Phenytoin, Carbamazepine, Lamotrigine, Topiramate, Valproic acid,
GABA activation
Gabby Tops Phineas and Val Via her Tiny Benz
what mechanism do these AED drugs use?
Gabapentin, Topiramate, Phenobarbital, Valproic acid, Benzodiazepine, Tiagabine, Vigabatrin.
blocks T-type calcium channel
MOA of ethosuximide
barbituates, phenytoin, carbamazepine
-has significant drug interaction
what AEDs are P-450 inducers?
depakote
What AED is a weak P-450 inhibitor?
Hepatotoxicity, neutropenia, thrombocytopenia, teratogenicity( neural tube defects in the fetus)
adverse effects of Valproate
Hepatotoxicity, aplastic anemia, agranulocytosis, diplopia.
adverse effects of carbamazapine
Gingival hyperplasia, hirsutism, teratogenicity, ataxia, neuropathy.
adverse effects of phenytoin
Steven-Johnson syndrome ( a bullous form of erythema multiforme that involves mucous membranes and large areas of the body)
adverse effects of ethosuximide and lamotrigine
status epilepticus
defined as a seizure that persists for a sufficient length of time or is repeated frequently enough that recovery of consciousness between attacks does not occur .
-an episode of more than 30 minutes of continuous seizure activity or,
-two or more sequential seizures spanning this period without full recovery between seizures
criteria to define status epilepticus
5-20 minutes
minimum time-frame of a status-epilepticus event:
Lorazepam
-immediately follow with phenytoin or fosphenytoin
in the first 2 min of a status epilepticus event, treat with
addtional phenytoin or fosphenytoin
if a status epilepticus event lasts more than 20 min, treat with
phenobarbital
if a status epilepticus event lasts more than 30 min, treat with
additional phenobarbital
if a status epilepticus event lasts more than 50 min, treat with
anesthesia with midazolam or propofol
if a status epilepticus event lasts more than 60 min, treat with
long duration and those who have severe physiologic disturbance
•The outcome is usually worse in patients with status epilepticus of .
Paroxysmal Disorders
cerebral function characterized by spontaneous electric discharges from the cerebral cortex
•Transient ischemic attacks (TIAs)
•Panic attacks
•Convulsive Syncope
•Complicated Migraines
•Pseudo seizures
DDx of paroxysmal disorders
•distinct visual phenomena including simple or complex visual hallucinations, visual distortions, hemianopsia and amaurosis.
manifestation of occipital epilepsy
migraines
seizures in adults are often misdiagnosed as
pseudo seizures
seizure-like activity such as twitching or loss of consciousness without electrical disruptions in the brain
-common symptom of conversion or somatization disorder
-post-ictal confusion often absent; loss of motor control is rare
aura
common pre-seizure symptom distinct from psedo seizure
tonic, clonic feature, epileptic cry, injury( tongue bitten), incontinence etc
during seizure symptoms (distinct from pseudo seizure)
disorientation, confusion, weakness (todd's paralysis)
post-seizure symptoms distinct from pseudo seizure
•Lumbar puncture only if meningitis or encephalitis suspected and potential for brain herniation is ruled out
why would you order an LP for evaluation of a first seizure?