CBT
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
Edward Thorndike (1911)
law of effect
“behavior modification”
cat in a box with a pulley system
John Watson (1920)
Little Albert
baby with no fear of white rabbits/rats
conditions to be scared of it — struck a steel bar with a bate every time rat was there
ethical issue: unknown if he ever was deprogrammed and died at 6
generalized to other objects similar — rabbit, dog, mask
BF Skinner
operant conditioning — rewards and punishments
term behavior therapy
Skinner box — rat in a box
Joseph Wolpe (1940s/1950s)
beginnings of modern behavior therapy
reciprocal inhibition (theory)
Systematic desensitization rests on this
can’t feel 2 things at once
relaxation and can’t feel anxious when scared
Replace anxiety fear response with relaxed response
1st generation of CBT
basic learning research backgrounds
results were positive but it stalled
problems — people didn’t use the same theories and language
psychoanalysis dominated
research people not talking to clinical people
psychologists in different fields looked down on others in different fields
Second Gen of CBT
emphasis on cognition
behavior and cognition connected
Aaron Beck (founder of CBT)
widespread support — gradual replacement of psychoanalysis model
Third Generation of CBT
acceptance based mindfulness therapies
CBT didn’t make enough progress — missing some people
efficacy stalled — why haven’t we solved anxiety and depression
still need research why things work
Present Centeredness
what maintains the problem NOW
why are you here today
Empiricism
focus on what works empirically (in real test of it) to modify behavior, regardless of what should work theoretically
here to learn with you
Measurement
Strong focus on measurement of behavior before, during, and after treatment
homework, worksheets, tells us what works in real time
Session only 1 hour — CBT goes on after the session
even if someone doesn’t do work it gives us data
Dimensionality
Behaviors exist along different dimensions: intensity, frequency and duration
is it impairing functioning?
Lawfulness
behavior is not random, it can be predicted once you understand the cognitive, affective, and situational triggers
Functional Analysis
“often one part of a larger case conceptualization”
To change a behavior you need to carefully analyze and change the context of a behavior (what happens/exists before and after a behavior)
have to do more than just ask why? looking at triggers/big picture
way to understand certain behaviors, more narrow (case conceptualization: all behaviors, functional analysis: 1 behavior)
3 tenets of FA
Human affect, cognition, and behavior are idiosyncratic (aka “behaviors”)
Behaviors best understood in the “context” in which they occur
Behavior and context are an inseparable whole
“What happens when”
Process of detecting patterns or consistencies between behaviors and contexts
Detect patterns (aka “functional relations”) within ”behaviors” and “context”
Maintain Behaviors
all behavior is learned the same way whether helpful or unhelpful
no behavior is bad or good per se. it depends on CONTEXT
Individualized Approach
behavior is individually determined.
What creates, maintains, a particular behavior in one person may not create or maintain the same behavior in another
Chunking
break down problems into subparts and then target areas for intervention
ex: fear hierarchies: start small work up
Treatment Packages
Multiple behavior therapy techniques together to achieve treatment goals
see what works best
Operant Conditioning
rewards and punishments to modify behavior
voluntary responses vs. classical (involuntary responses)
rewarded behavior repeated
punished behavior less likely to occur
Stimulus and Consequences in Operant Conditioning
Stimulus Role
Positive: Application of Stimulus. Stiulus is presented or added
Negative: Removal or withdrawal of stimulus. Stiulus is taken away
Consequences
Reinforcement: behavior increases
Punishment: behavior decreases
Positive Reinforcement
add something the person likes — behavior increases
ex. money for getting an A makes it more likely student will keep getting As
Negative Reinforcement
Takes away something you do NOT like — behavior increases
ex. taking advil to relieve headach makes it more likely you will take it again
Positive Punishment
Add something you do NOT like — behavior decreases
ex. being yelled at
Negative Punishment
take away something you DO like — behavior decreases
being put in time out
Secondary Reinforcement
Something a person has learned
acquired its value only through repeated association with primary reinforcers
developed in our world: money, grades, gold stars
Primary Reinforcement
inherently desirable
item is reinforcing itself
need food, warmth, water
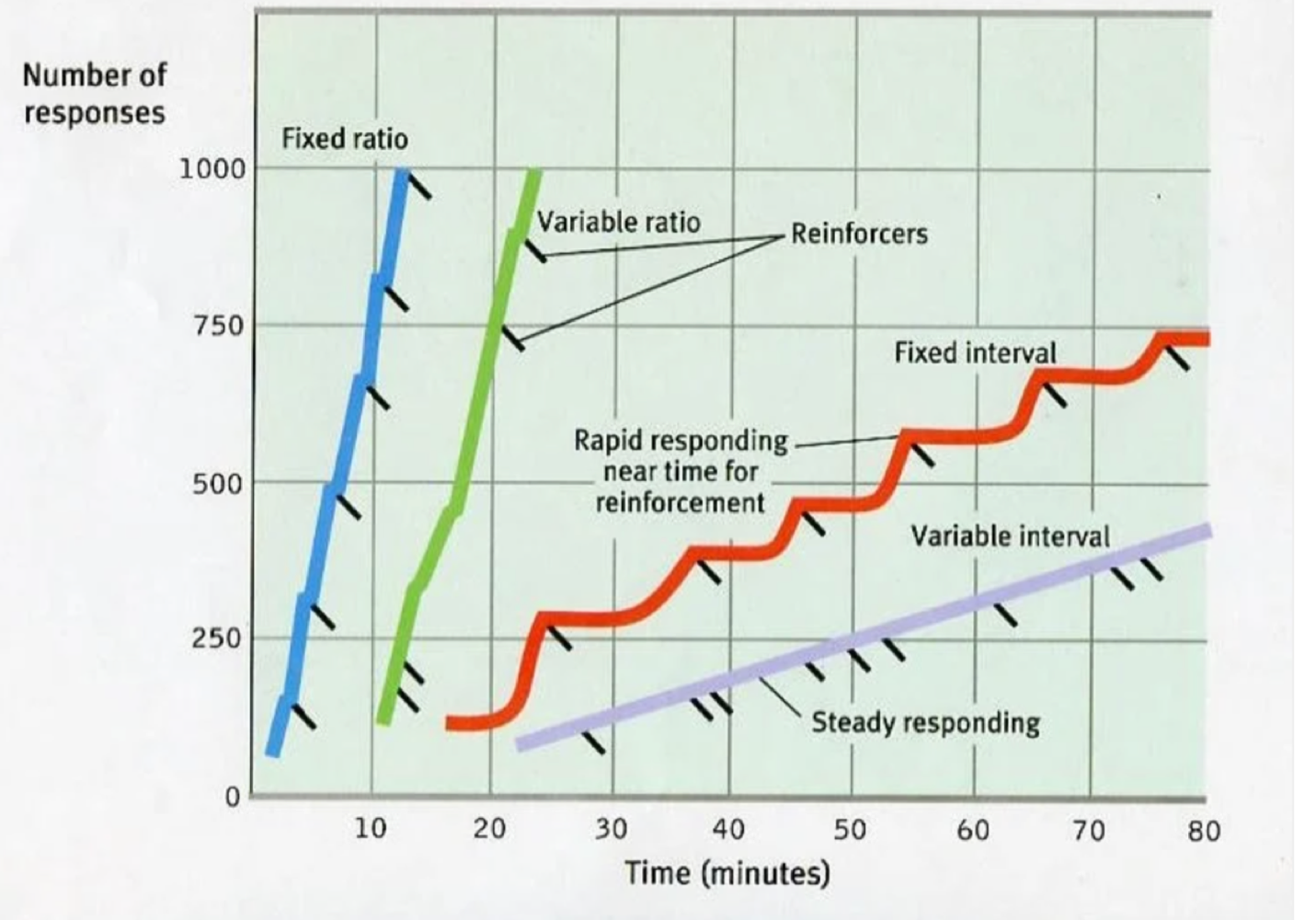
Schedules of Reinforcement
behavior modification technique which involves selectively reinforcing behaviors you want and withholding what you don’t want
continuously — every time
intermittent — not every time
4 types of intermittent schedules
Ratio (responses) Schedules vs Interval (time) schedules
fixed ratio — Reinforcement is delivered after a set, predictable number of responses.
variable ratio — Reinforcement is delivered after an unpredictable, variable number of responses. most resistant to extinction because you don’t know when reward will come. ex. gambling. consistent, persistent
Fixed interval — Reinforcement is delivered for the first response that occurs after a specific, predictable amount of time has passed. Good before because you know reward is gonna happen, behavior decreases after reward. Ex. trying a lot harder because you know youre going to get a raise
Variable interval - Reinforcement is delivered for the first response that occurs after an unpredictable, variable amount of time. constantly doing it because you don’t know when reward will happen
Extinction
loss of conditioned behavior
reinforcement is withheld from a preivously reinforced behavior — behavior decreases/elimanted
Extinction Burst
when a behavior is no longer followed by a reward, the individual may exhibit an increase in the frequency, duration, or intensity of that behavior. This increase in behavior is known as an extinction burst.
Case Conceptualization in CBT
working hypothesis on what’s happening with patient, how disorder is developped maintained, triggered. contextual. Often CBT therapists share canse conceptualizaztion
Understanding of patient’s presenting problem
identify variables related to difficulties
identify treatment targets, goals, and objectives
broad hypothesis of a person (all behaviors)
A method and clinical strategy to obtain and organize info about the patient
incorporates ares such as learning history, maintaining factors, and presenting problem
can work as a map or blueprint of treatment based on personalized factors
should continually be updated throughout treatment
Process: descriptive emphasis (derived from assessment), treatment recommendations, review and update
“The formulation is a hypothesis about the mechanisms causing and maintaining the patient’s problems. The therapist uses the formulation (and other information) to develop a treatment plan and obtain the patient’s informed consent to it.
Comorbidity
when conditions present together. the simultaneous presence of two or more diseases or medical conditions in a patient.
Idiographic
individualized/unique features of someone
Nomothetic
how they look like everyone else, ex base rates
Why use Case Conceptualization?
To better understand behavior
To increase empathy
To identify ways to engage clients
To identify targets for intervention
To create a shared understanding of a child or adolescent
Efficacy
how well it works in controlled environment, internal validity
Effectiveness
does it work in real world, external validity
5 Ps
Presenting problem: what the pt and clinician identify as difficulties.
Predisposing factors: biological, genetic, environmental, psychological, or personality risk factors
Precipitating factors: significant events preceding onset of disorder
Perpetuating factors: repeating behavioral, cognitive, or biological patterns that maintain dysfunction
most important in CBT case conceptualization
Protective factors: strengths and supports
broad biopsychosocial formulation of overall case
big-picture understanding of person’s history, context, and strengths
SORC Model for case formulation
S — Stimuli (triggers, procedes it)
O — Organism factors (everything that happens in brain (thoughts, feelings, emotions)
R — Response (observable behavior (avoiding eyecontact, shaking, not speaking)
C — Consequence (short term, long term)
functional analysis of a specific behavior/problem
practical for IDying and changing specific behaviors
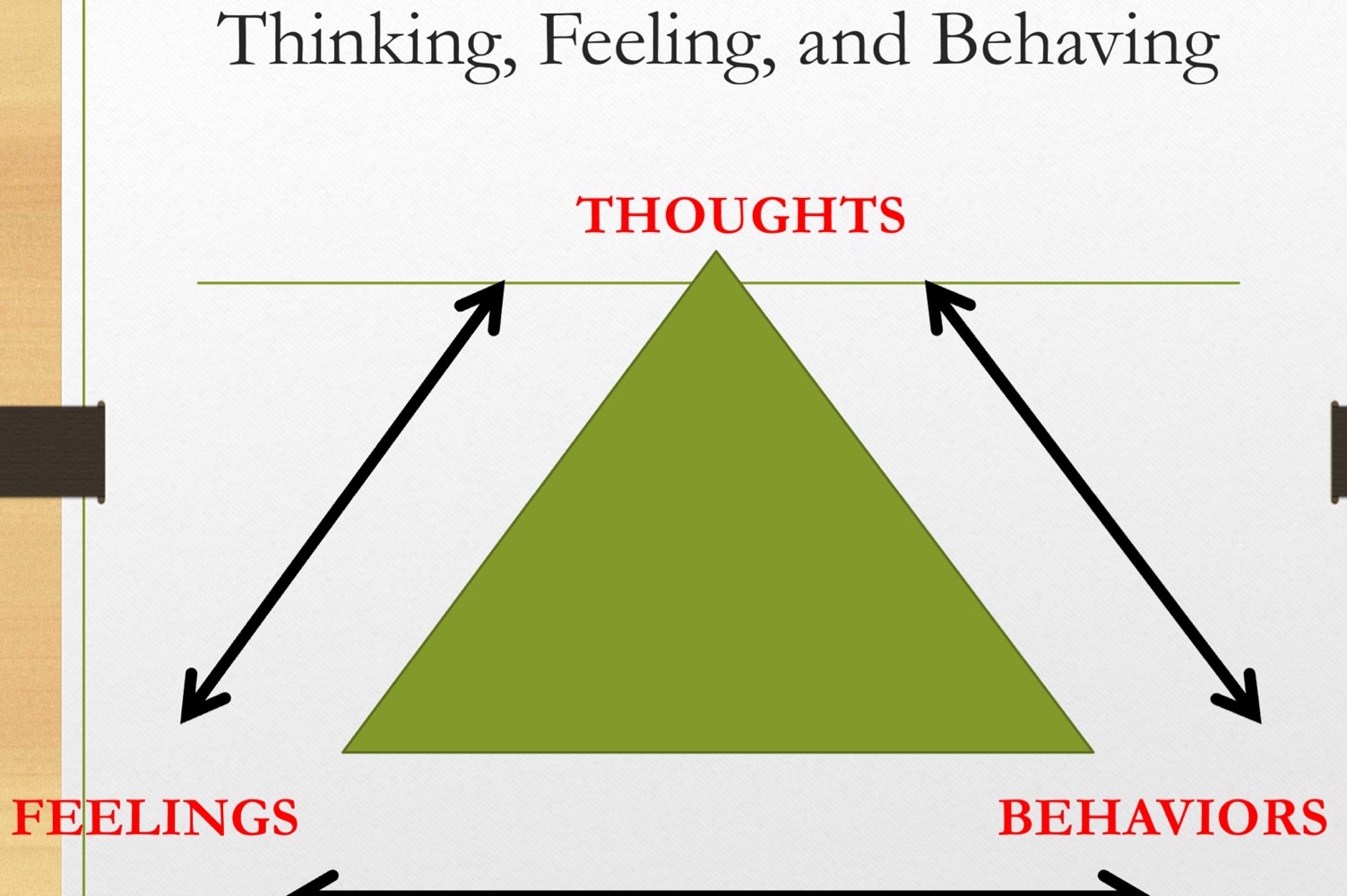
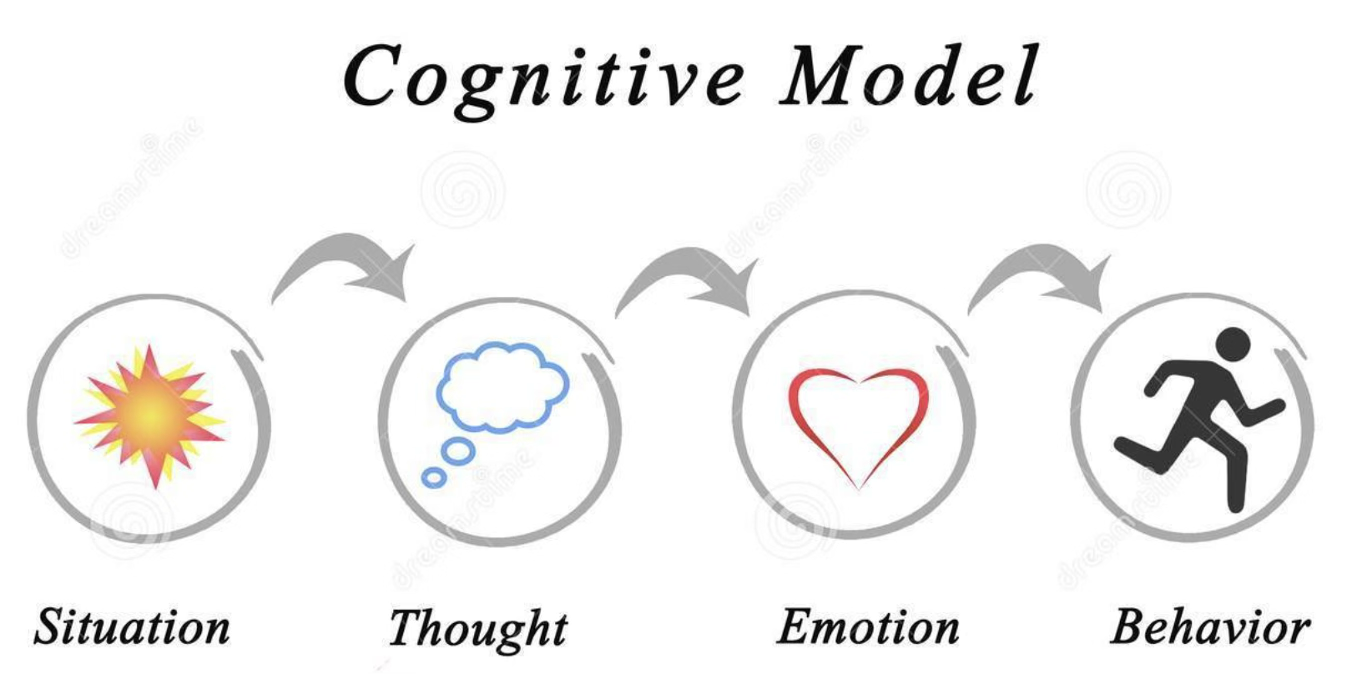
Cognitive Behavioral Triangle
thoughts, emotions, behaviors all linked
if we can make thoughts more truthful, we can help your behaviors and feelings
General Principles of CBT
•Cognitive behavioral therapy is:
•Semi‐structured, time‐sensitive, active;
•Based on a case conceptualization;
•Focused on skill development; and
•Oriented toward a hypothesis‐testing approach.
•Clinician and client work collaboratively with a focus on a strong relationship.
•All interventions aim at cognitive change.
Stages of Traditional Exposure therapy
Psychoeducation
Joint Formulation
Creation of the fear hierarchy
Systematic Enaction of hierarchy
Can be ordered, random, top-down… depends on the client
Process/integrate new learning (can include some cognitive work)
Relapse prevention
Why is psychoeducation important
Necessary for understanding anxiety disorders in a way that leads to a clear rational for using exposure therapy
Providing and ensuring buy in of treatment rationale/psychoeducation increases compliance
Leads to a shared road map for functional assessment/treatment planning
Allows therapist and patient to understand how to optimize learning during exposure
Effective in Preventing relapse by teaching patient how to be their own therapist
Facilitates troubleshooting (e.g., non-adherence, therapist discomfort)
Fear/Panic vs Anxiety/Worry
Fear/Panic – Present-Oriented Mood State
Immediate fight or flight response to danger or threat
Abrupt activation of the sympathetic nervous system
Strong avoidance/ escapist tendencies
Anxiety/Worry – Future-Oriented Mood State
Apprehension about future danger or misfortune (“anticipatory fear”)
Physical symptoms of tension/apprehension (e.g., muscle tension, etc.)
Characterized as negative affect (manifests with physiological, behavioral, and cognitive components)
Both anxiety & fear are “normal,” helpful emotional states - in normal doses
Common themes: anxiety
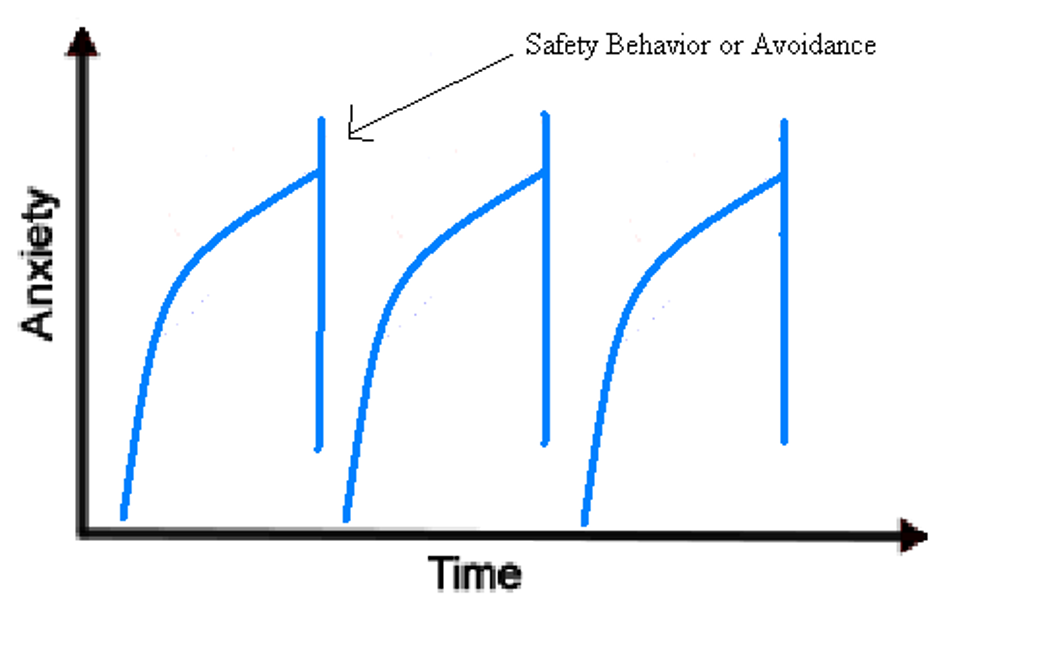
triggers —> thought/interpretations —> elevated anxiety —> behaviors (avoid, safety behavior, distract, ruminate) —> short term reduced anxiety but prolonged and worsened anxiety in long term
Anxiety is maintained by safety behaviors/avoidance
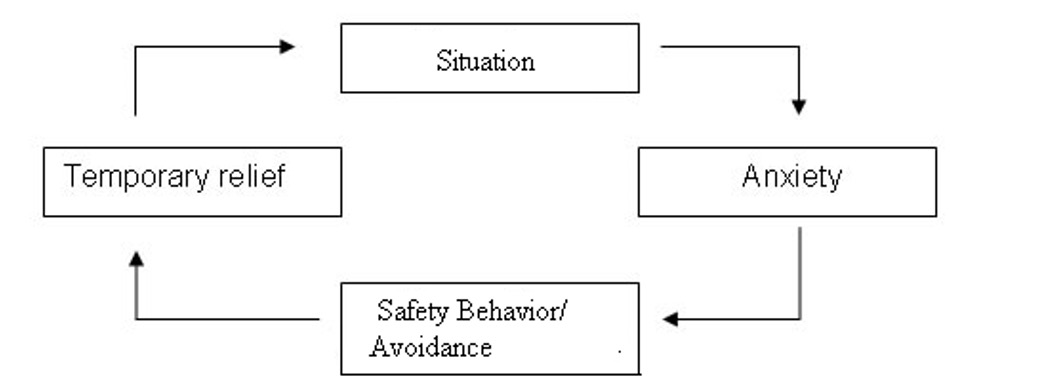
Safety Behavior
don’t allow you to fully experience the anxiety you should be feeling
coping mechanisms people use to reduce anxiety
Avoidance ex. eye contact, parties, places associated with panic
Impression management ex. rehearsing sentences or monitoring ones’s behavior
Checking ex. locks, symptoms
Neutralizing rituals ex. rituals to feel safe (pacing, squeezing hands, checking)
Exposures
Type of psychological treatment that helps people face their fears by gradually exposing them to situations that cause distress.
imaginal exposure
in vivo exposure (go out and do it)
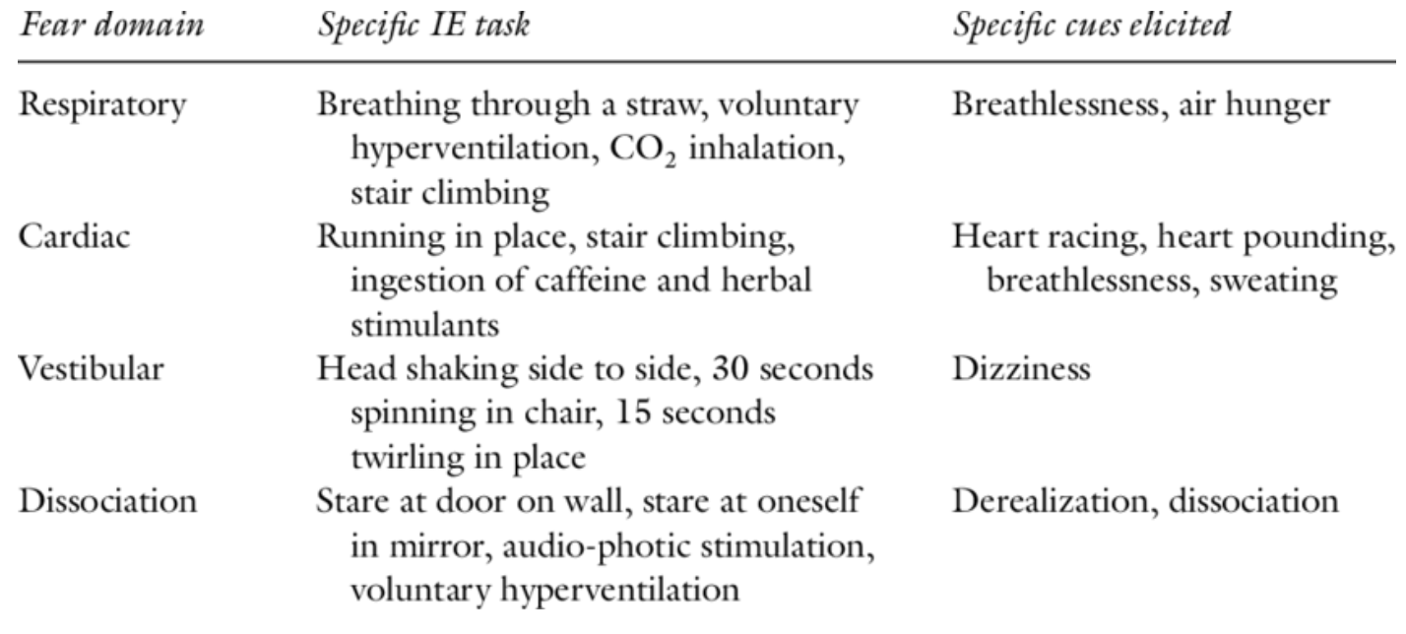
interoceptive exposure (feel physical sensations: running/ breathing fast)
virtual reality
Pacing of Exposures
gradual —> steps, work way up
flooding —> do it all at once
systematic desensitization —> engage in behavior while simultaneously engaging in relaxation (Dr. Foster has mixed feelings, don’t really learn to face anxiety)
How does exposure help
Old thinking —> habituation (get used to sensation) and extinction (fear goes away)
New thinking —> inhibitory learning
create new learning pathways that are ideally stronger than old ones
old one doesn’t go away that’s why there’s a risk of relapse
more you practice, stronger new learned response becomes over old response (Old response not gone just not as prominent as learned response from exposure)
Self-efficacy
emotional processing — process in a safe enviornement first
General Rules for exposure
allow sufficient time
if you do it for 35 mins here, you can do it at home by yourself
with in sessioni anxiety reduction is good but not neccesary
what Is necessary is homework (more you do it more anxiety decreases)
Don’t do anything to reduce anxiety in middle of exposure
keep an eye out for safety behaviors
need to learn they aren’t feeling better because of the safety behavior but because fully feeling anxiety can create and develop new learning behaviors (that the event isn’t that bad)
engaing in behaviors they think help but worsen anxiety long term
even if a ‘bad’ response happens you got through it! you handled it
don’t give patient anything you wouldn’t do
CBT for panic disorder
Barlow’s Panic Control Therapy (PCT)
3 components:
Physical, Cognitive, Behavioral
Psychoeducation, particularly re fight-or-flight response
Normalizes physiological sensations
“Scanning”/”detecting” cognitive biases
Cognitive treatment
Psychoeducation
Interoceptive exposure
Build in exposure for agoraphobia throughout.
CBT for PTSD
Prolong Exposure for PTSD
manualized versions from 8-15 sessions, 90-120 mins per sess
individualized
psychoeducation
trauma assessment
breathing
imaginal exposure —> go back to the trauma, keep eyes close, tell your story and sit with it
invivo exposure
Cognitive Processing Therapy
EMDR (eye movement desensitzation and restructuring)
looking at light back and forth to be engaged in exposure
SUDS
subjective units of distress scale
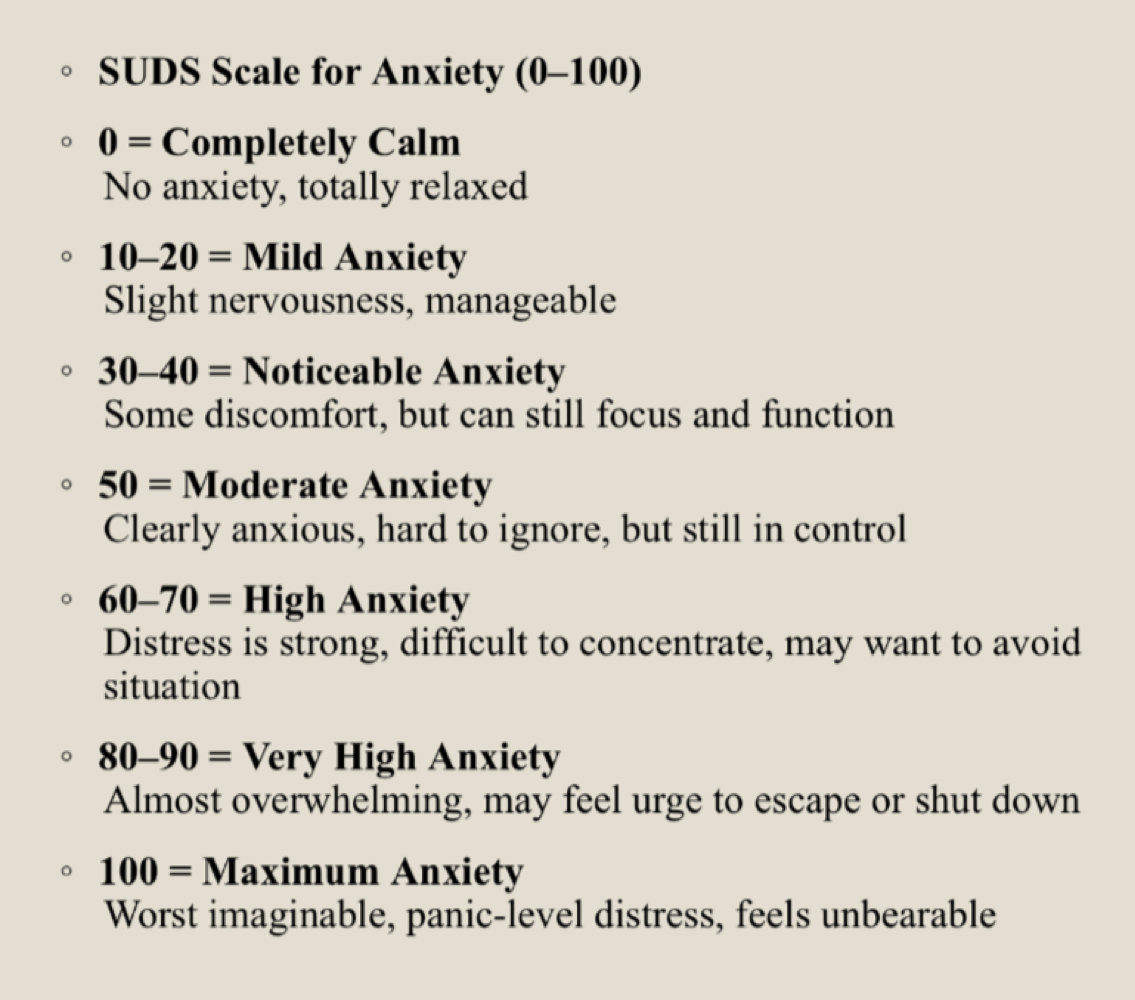
Creating a Fear Hierarchy
teach SUDS scale — anchor points
use info from intake and knowledge of typical triggers
stay cognizant of what they can do at home (include imaginal, invivo, simulated, and interoceptive as needed)
target primary fears
if needed, reorder list so highest scenario is at top
rate anxiety for scharios when engaging and NO avoidance behaviors
Start at something a little hard but want them to succeed to increase feelings of self-efficacy and willingness to do future exposures
overcorrect — if you can do this you can do easier things (if you lick a toilet bowl you can eat at a restauarnt)
CBT for OCD
EXRP — exposure response prevention
strong evidence that this is better than relaxation and anxiety management
more effective than other CBT
involves gradually exposing individuals to their feared stimuli (exposures) while preventing them from engaging in their compulsive rituals (response prevention).
Blood Injection Injury Phobia
unique because it’s assoicated with fainting
vasovagal response (sudden drop in heart rate and BP)
bradicardia — heart rate slower rate than normal
bradys and BD drop associated with phobia and then fainting
blood pressure drop in bradicardia
can’t do run of the mil exposure — be in contact with medical provider (or client should be)
applied tension paired with exposure
prior to exposure — tense body parts to elevate heart rate and BP so when it drops shouldn’t drop to fainting
Generalized Anxiety Disorder
Worry = a chain of catastrophising thoughts that are predominantly verbal
Maladaptive worry generates a repetitive range of negative outcomes in which the individual attempts to generate coping solutions until some internal goal is achieved (e.g., “a sense of control”)
People with severe anxiety want to control things — treatment can be learning to live with not knowing things.
Worry exposure is a specific variant of imaginal exposure
Threatening mental images and their corresponding unpleasant emotional arousal are avoided by worrying in words and sentences
Exposure = sustained imaginal exposures of actual worse case scenarios ripe with imagery and emotional content.
worry diary as a type of exposure
what are you most scared of happening? what would happen if it did? could you work through it
Non-compliance
exposure can have a high drop out
need to have a buy in
meet someone where they are, hear them and their concerns (UNDERSTAND THEM), make sure they understand it
enlist at home support, ID real barriers to complience, psychoedu, prep clients ahead oftime for difficulty of tx, if needed reduce difficulty of exposures
CBT for Depression
behavior activation and cognitive restructuring
antidepressants are helpful but CBT can help relapse because you’re learning skills
best is a combo for severe depression
cycle of depression (BA targets actions that tie into feelings b/c in CBT all related)
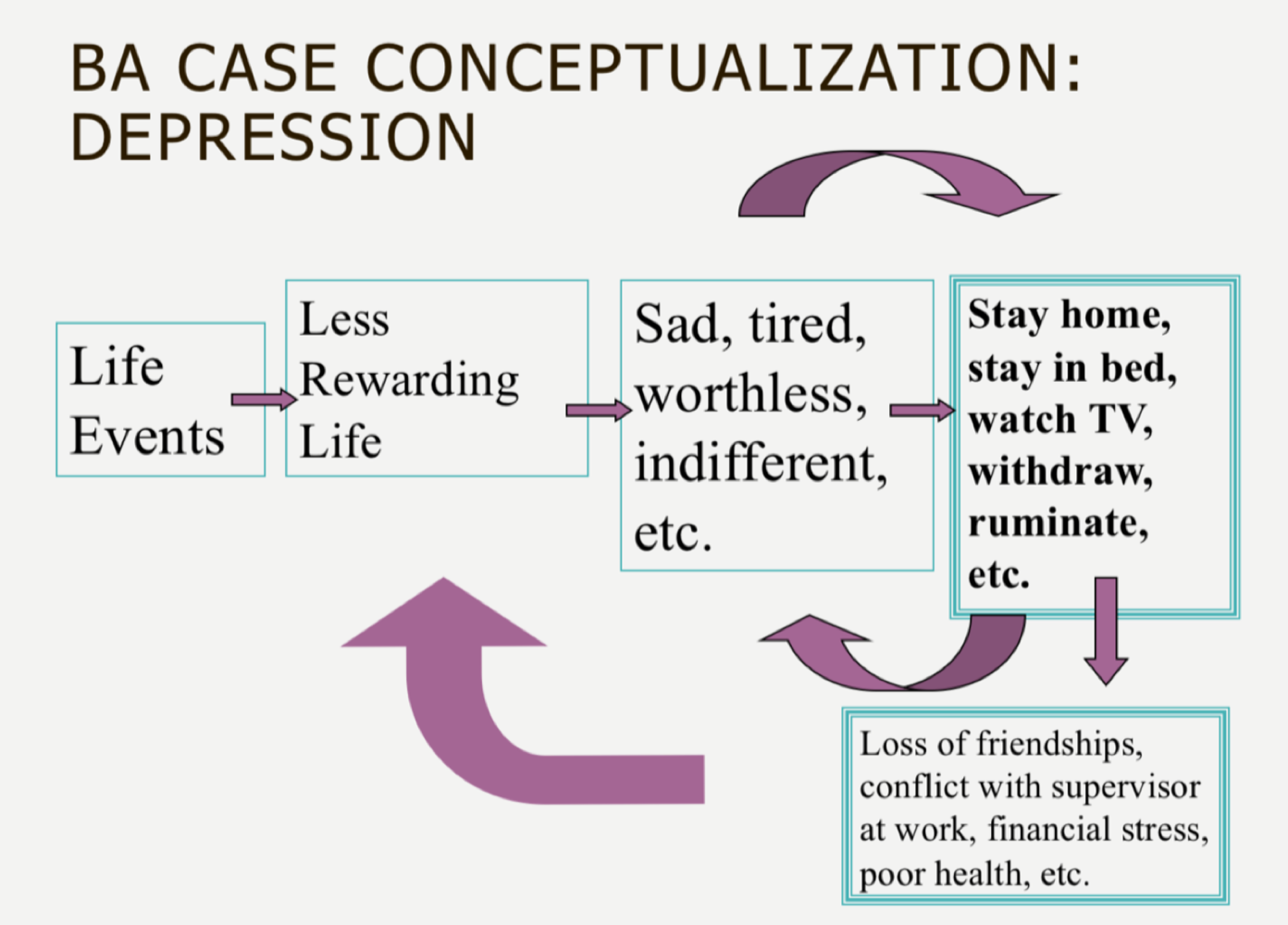
Behavior Activation
identifying things they enjoyed doing before and giving them ways to reaccess it
Based on premise that limited rewarding experiences and reduced ability to experience positive reward from the environment maintain depression
Aims to systematically increase activation such that patients may experience greater contact with sources of reward in their lives and solve life problems that allow them to lead a more rewarding life
strong efficacy, can be used as stand alone treatment for cognitive restructuring
Key elements:
Behavioral case conceptualization
Activity monitoring and scheduling
Identification and elimination of avoidance patterns
Establishment of healthy routines
Behavioral strategies for targeting worry or rumination
Goals are specific to the individual
Activity Chart
Central tool in BA
baseline assessment of activity and relationship with mood
ongoing monitoring of activity and mood
evaluate progress
Routine Regulation
tool in BA
work with patient to develop regular routine for basic life activities: sleeping, eating, exercise, Basic self-care, work/school, chores
Rumination
can function as avoidance, can maintain depression
just can’t stop thinking, circles, argue with self
Focus on context and consequences of rumination ,not content
Cognitive Triad and Depression Aaron Beck
3 types of negative thoughts lead to depression
negative views about the world: no one values me, everyone ignores me
negative views about oneself: I’m worthless, I wish I was different
negative views about the future: things will never change, only gets worse
Clinical Implementation of CT
protocols typically 12-25 weekly sessions (2x weekly initially for severe depressives)
model: cognitive triad (self, environment, & future)
importance of nonspecifics (warmth, genuineness, accurate empathy)
rational, linear thinking
highly directive
collaborative relationship
buy in, can’t just tell them how to think
Intro to cognitive model
Eliciting and recording automatic thoughts
Testing and/or questioning automatic thoughts
Use of Socratic questioning very important in cognitive therapy!
Identifying and adopting alternative/adaptive thoughts
“Act as if”
“Try on for size”
Core belief work (sometimes)
CT: Focus on content of thinking
“I was depressed all day yesterday because I was thinking about how my sister really doesn't’t love me.”
What is the evidence that this thought is accurate?
What would it mean if it were true?
Can you think of another way to interpret what your sister said?
Why must everyone love you?
CT: Focus on context and consequences of thinking
“I was depressed all day yesterday because I was thinking about how my sister really doesn’t love me.”
When did you start thinking that?
How long did it last?
What were you doing while you were thinking that?
How engaged were you with the activity, context, etc.?
What were consequences of thinking about that?
Cognitive Model
In CBT, the model behind it is that there is a situation that leads to a thought, leading to an emotion, leading you to engage in specific behaviors
The thought aspect is why people feel and react differently to different situation
We’re trying to change the thought
Not just for depression
Linear process
First step is to become aware of the thought → thought record
if we can restructure someone’s thought, we can restructure emotional experience, is true for a lot of experiences (even if not all)
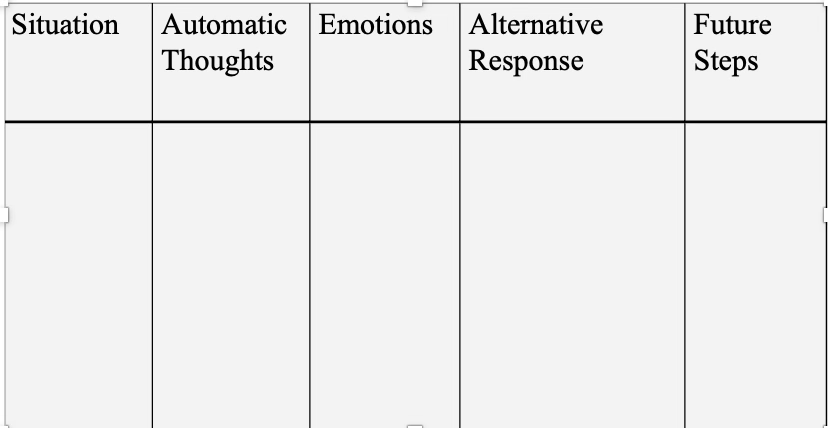
Thought Record
part of CT
thought record —- go in the real world and come back, tell me about situation, and what was emotion, and if you need to work backwards to figure out what were your thoughts (usually start with first three then as treatment progresses implant second)
used to see what thoughts were happening after a situation that led to emotion and behavior
Automatic Thoughts
can be a picture, often in short hand, running underlying thoughts not necessarily in full sentences (like news running footer)
lonely... getting sick... can't stand it... cancer... no good.”
Sometimes automatic thought is a brief reconstruction of some event in the past
Specific messages
A young man who fears rejection tells himself, "She doesn't want you. You look silly."
Different than unconscious —- we have at our grasp / we have access to it we’re just not paying attention to it
almost always believed
reflexive and plausible
plausible because they are hardly noticed, let alone questioned or challenged
therapists want to notice them AND challenge them
often couched in terms of "should," "ought," “can’t” or "must."
People torture themselves with "shoulds"
Automatic thoughts tend to “awfulize”
predict catastrophe, see danger in everything, and always expect the worst
Awfulizers are the major source of anxiety.
hard to turn off
Weaving through the fabric of your internal dialogue.
come and go with a “will of their own”
They tend to act as cues for each other.
Everyone has had the experience of one depressing thought triggering a long chain of associated depressing thoughts.
Learned
Since childhood people have been telling you what to think
You have been conditioned by family, friends, and the media to interpret events a certain way
good case conceptualization helps us figure out where they are learned
even if they are true (to an extent) — how helpful is it to focus on it?
have to go deeper sometimes and find out what’s driving automatic thoughts
How do we start noticing automatic thoughts
many patients are unaware of their thinking patterns
they will often be more aware of their emotions than of what precipitated emotions
how do we help notice?
work backward from affect — what was the emotional experience? work backwards
take a reasonable guess
what might someone else think in this situation that could lead to the emotion I’m experiencing
“shoulds"— commonly come up, trigger for therapist to notice that it’s usually inaccurate and unhelpful
common cognitive distortions that will lead to automatic thoughts
All-or-nothing thinking
Self Centered (thinking in extremes): Umbrella way of thinking (not a cognitive distortion — the bold and italics are cog distortions)
All-or-nothing thinking (also called black-and-white, polarized, or dichotomous thinking): You view a situation in only two categories instead of on a continuum
Example: “If I’m not a total success, I’m a failure.”
Mind Reading
Self Centered (thinking in extremes): Umbrella way of thinking (not a cognitive distortion — the bold and italics are cog distortions)
Mind reading: You believe you know what others are thinking, failing to consider other, more likely possibilities.
you actually don’t know what other people are thinking
Example:
“He thinks that I don’t know the first thing about this project.”
“Everyone hates me”
“I know when I go to school, the people there do not like me”: went to school and smiled, people smiled back, changed her entire thinking and realized her belief wasn’t true
“Should” and “must” statements
Self Centered (thinking in extremes): Umbrella way of thinking (not a cognitive distortion — the bold and italics are cog distortions)
“Should” and “must” statements (also called imperatives): You have a precise, fixed idea of how you or others should behave, and you overestimate how bad it is that these expectations are not met.
Example:
“It’s terrible that I made a mistake. I should always do my best.”
“I should’ve known better”
“Should’ve done better on that test”
Magnification/minimization
Minimizing and mislabelling: These distortions involve giving less weight to positive things and more weight to negative things.
Magnification/minimization: When you evaluate yourself, another person, or a situation, you unreasonably magnify the negative and/or minimize the positive.
Example:
“Getting a mediocre evaluation proves how inadequate I am. Getting high marks doesn’t mean I’m smart.”
Labeling/mislabeliing
Minimizing and mislabelling: These distortions involve giving less weight to positive things and more weight to negative things.
Labeling/mislableing: You put a fixed, global label on yourself or others without considering that the evidence might more reasonably lead to a less disastrous conclusion.
Example:
“I’m a loser. He’s no good.”
“I suck”
Overgeneralization
Assuming the worst: assuming the worst can lead to depression
Overgeneralization: You make a sweeping negative conclusion that goes far beyond the current situation.
Example:
“[Because I felt uncomfortable at the meeting] I don’t have what it takes to make friends.”
Emotional Reasoning
Assuming the worst: assuming the worst can lead to depression
Emotional reasoning: You think something must be true because you “feel” (actually believe) it so strongly, ignoring or discounting evidence to the contrary.
Example: “I know I do a lot of things okay at work, but I still feel like I’m a failure.”
I feel like I am a failure = I am a failure
Mental Filter
Assuming the worst: assuming the worst can lead to depression
Mental filter (also called selective abstraction): You pay undue attention to one negative detail instead of seeing the whole picture.
Example:
“Because I got one low rating on my evaluation [which also contained several high ratings] it means I’m doing a lousy job.”
Disqualifying or Discounting the Positive
Assuming the worst: assuming the worst can lead to depression
Disqualifying or discounting the positive: You unreasonably tell yourself that positive experiences, deeds, or qualities do not count.
Example:
“I did that project well, but that doesn’t mean I’m competent; I just got lucky.”
Yeah I got a good review, but this is why it was still bad
negating — that doesn’t count
Personalization
Assuming the worst: assuming the worst can lead to depression
Personalization: You believe others are behaving negatively because of you, without considering more plausible explanations for their behavior.
Example:
“The repairman was curt to me because I did something wrong.”
he was hurt because of me, I know I did something wrong (even if you have no evidence to support)
Catastrophizing
Assuming the worst: assuming the worst can lead to depression
Catastrophizing: :This prompts people to jump to the worst possible conclusions
Example
“I’ll be so upset, I won’t be able to function at all.”
Making a mountain out of a moll hill
If I fail this test, I’m gonna fail the program, never have a job
Cognitive Distoritions
Type of automatic thoughts.
Automatic thoughts happen so fast, people not paying attention to them, the reason why they’re called Common Cognitive Distortions suggests that the thinking isn’t based in reality — distorted, a sign we should question it
in the model, this thinking comes first and then the emotion
how these thoughts if believed can lead to really negative emotions, if you keep having them, serious potential pathology
Elicit automatic thoughts
Ask them how they are/were feeling and where in their body they experienced the emotion.
Elicit a detailed description of the problematic situation.
Request that the patient visualize the distressing situation.
Suggest that the patient role-play the specific interaction with you (if the distressing situation was interpersonal).
Elicit an image.
Supply thoughts similar or opposite to the ones you hypothesize actually went through their minds.
Ask for the meaning of the situation.
Phrase the question differently.
Evaluating Thoughts
treat it a little like an experiment
Examine the validity of the automatic thought.
How true is it?
Explore the possibility of other interpretations or viewpoints.
De-catastrophize the problematic situations
what does it mean if they don’t like you? Could you live like that?
what does it mean if your thought is right
acceptance
Recognize the impact of believing the automatic thought.
how much is it impacting your life that you believe it
your spending a lot of energy on it, and your life is so much bigger than this (even if it is true, and what would it mean if it was)
Gain distance from the thought.
time helps
more distance you have allows you to evaluate it more fairly
Take steps to solve the problem.
experiment, try to solve
what would happen if you smiled when you went to work
1. What is the evidence that supports this idea
What is the evidence against this idea?
2. Is there an alternative explanation or viewpoint?
3. What is the worst that could happen (if I’m not already thinking the worst)? If it happened, how could I cope?
What is the best / worst that could happen?
What is the most realistic outcome?
4. What is the effect of my believing the automatic thought?
What could be the effect of changing my thinking?
5. What would I tell____________[a specific friend or family member] if he or she were in the same situation?
6. What should I do?