2.4 Cartilage
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
Define the perichondrium and state its function.
The perichondrium is a dense connective tissue sheath surrounding hyaline and elastic cartilage (but absent in fibrocartilage and articular cartilage). It contains fibroblasts and capillaries that supply nutrients to chondrocytes via diffusion and contributes to appositional growth.
List two locations where fibrocartilage is found.
Intervertebral discs and pubic symphysis (also menisci, tendon/ligament insertions).
Why is cartilage repair limited?
Due to its avascular nature (relies on diffusion for nutrients) and low cellularity.
Compare interstitial and appositional growth in cartilage, including the cell types involved.
Interstitial: Chondrocytes divide within lacunae, secreting new matrix to expand cartilage from within (e.g., growth plates).
Appositional: Chondroblasts in the perichondrium produce matrix, adding layers to the surface (e.g., bone widening).
Explain why articular cartilage lacks a perichondrium and the clinical implications of this.
Articular cartilage is exposed to joint movement, requiring a smooth surface; a perichondrium would disrupt articulation. Its absence limits repair capacity, leading to degenerative conditions like osteoarthritis.
How does the matrix composition of elastic cartilage differ from hyaline cartilage, and how does this relate to its function?
Elastic cartilage contains elastin fibers (in addition to Type II collagen and proteoglycans), providing flexibility for structures like the epiglottis and pinna.
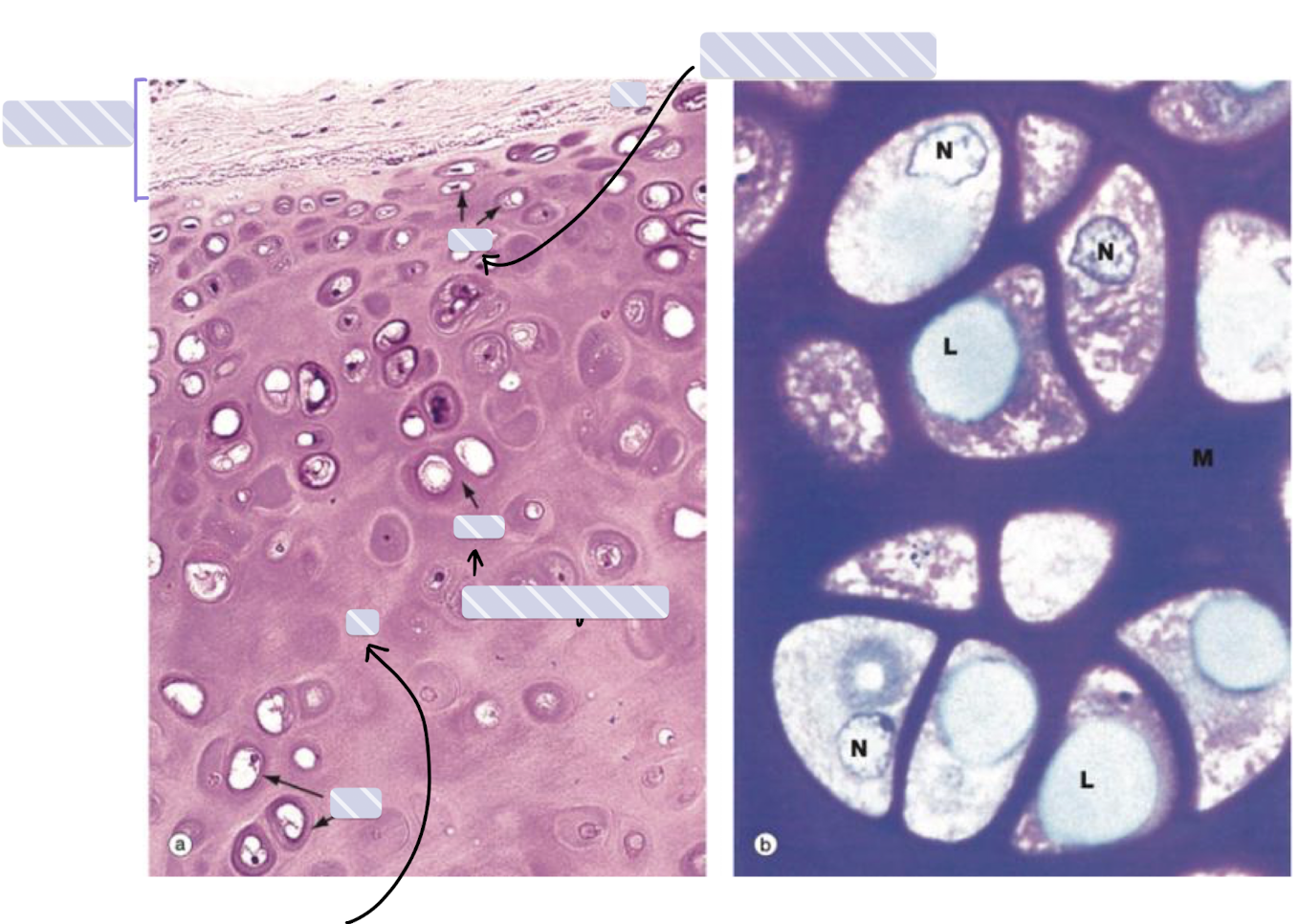
Explain how the composition of cartilage matrix contributes to its mechanical properties.
The high water content (bound to proteoglycans like aggrecan) provides resilience and compressive strength, while collagen fibers (Type II in hyaline/elastic, Type I in fibrocartilage) offer tensile strength. The proteoglycan aggregates trap water, creating a hydrated gel that resists deformation.
Why is cartilage avascular, and how does this impact its metabolism and repair?
The dense extracellular matrix limits blood vessel infiltration. Nutrients and oxygen diffuse from the perichondrium or synovial fluid, leading to slow metabolic rates and poor regenerative capacity after injury.
Compare and contrast the roles of chondroblasts and chondrocytes in cartilage maintenance.
Chondroblasts: Active cells in the perichondrium that secrete new matrix during appositional growth.
Chondrocytes: Mature cells trapped in lacunae that maintain existing matrix (synthesizing collagen/proteoglycans) but have limited proliferative capacity.
Why does interstitial growth occur only in young cartilage, while appositional growth persists in adults?
Interstitial growth requires chondrocyte division and matrix expansion, which is restricted in mature cartilage due to matrix rigidity (especially in calcified tissues like bone).
Appositional growth continues via the perichondrium, where chondroblasts remain mitotically active.
How does the extracellular matrix differ between hyaline cartilage and fibrocartilage, and how does this relate to their functions?
Hyaline cartilage: Type II collagen + high proteoglycan content → smooth, flexible support (e.g., articular surfaces).
Fibrocartilage: Type I collagen + fewer proteoglycans → high tensile strength for weight-bearing (e.g., intervertebral discs).
Explain why elastic cartilage is more flexible than hyaline cartilage, despite both containing Type II collagen.
Elastic cartilage contains elastin fibers embedded in its matrix, allowing reversible deformation (e.g., in the epiglottis during swallowing).
Why does fibrocartilage lack a perichondrium, unlike hyaline and elastic cartilage?
Fibrocartilage blends with dense connective tissue (e.g., tendons/ligaments), so it relies on fibroblasts for matrix production rather than a distinct chondrogenic layer.
How does osteoarthritis illustrate the functional importance of articular cartilage?
Degeneration of articular cartilage (due to wear/tear or inflammation) exposes underlying bone, causing pain, stiffness, and reduced joint mobility. Its avascular nature limits self-repair.
Why might a ruptured intervertebral disc heal poorly compared to a fractured bone?
The disc’s fibrocartilage has minimal blood supply and low cellularity, whereas bone is highly vascularized and undergoes active remodeling via osteoblasts/clasts.
Predict the consequences of a congenital defect in proteoglycan synthesis (e.g., aggrecan deficiency) on cartilage function.
Reduced proteoglycans → decreased water retention → loss of compressive resilience, leading to joint instability (e.g., premature osteoarthritis) or skeletal dysplasia.