Exercise Physiology Exam 2 (Nervous and Endocrine Systems)
1/89
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
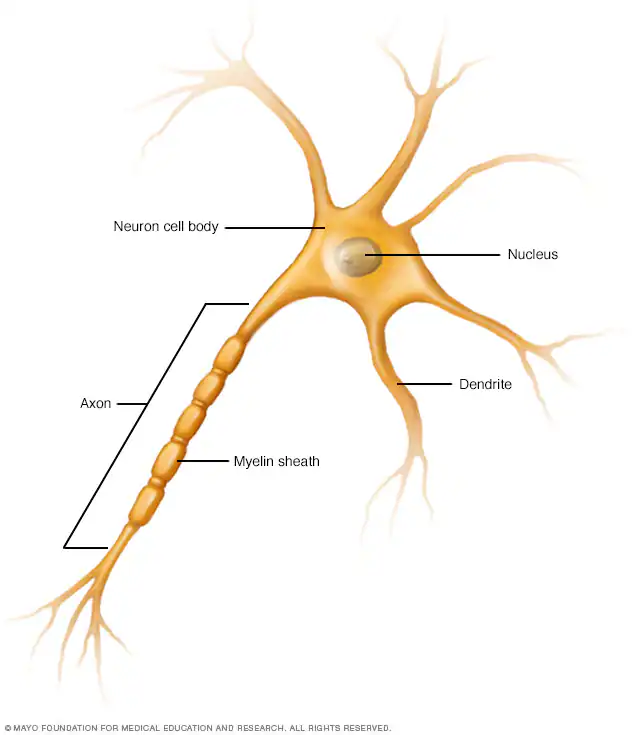
Axon
The neurons transmitter
Conducts signal away from cell body
Dendrites
Receives signals from other neurons
Soma
Also called the cell body
Contains the nucleus
Ion distribution (RMP)
ETC crates a charged gradient
High concentration of K+ inside of neuron
Move freely in and out of cell help maintain distrobution
High concentration of Na+ outside of neuron.
Inside is negative and outside is postive
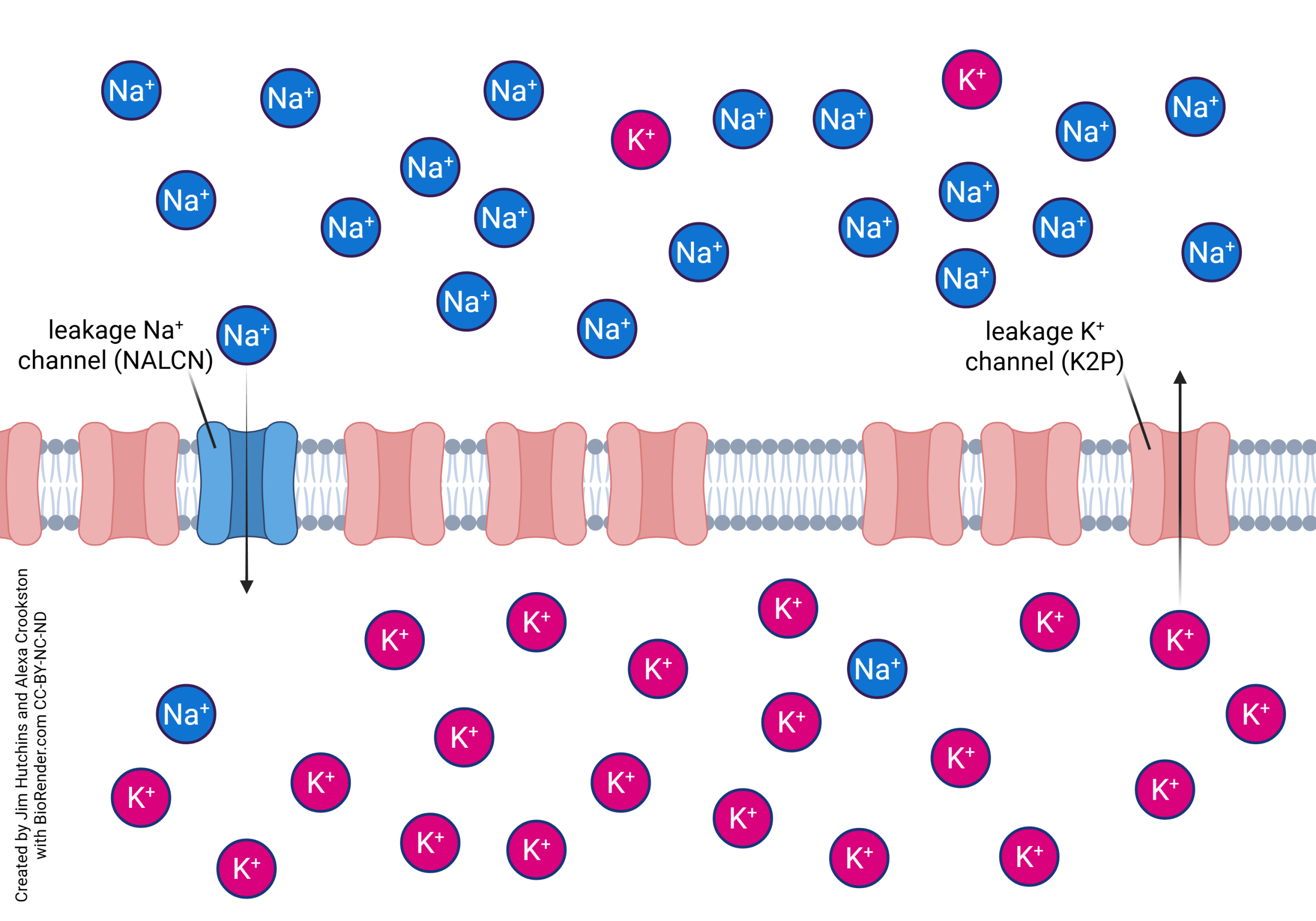
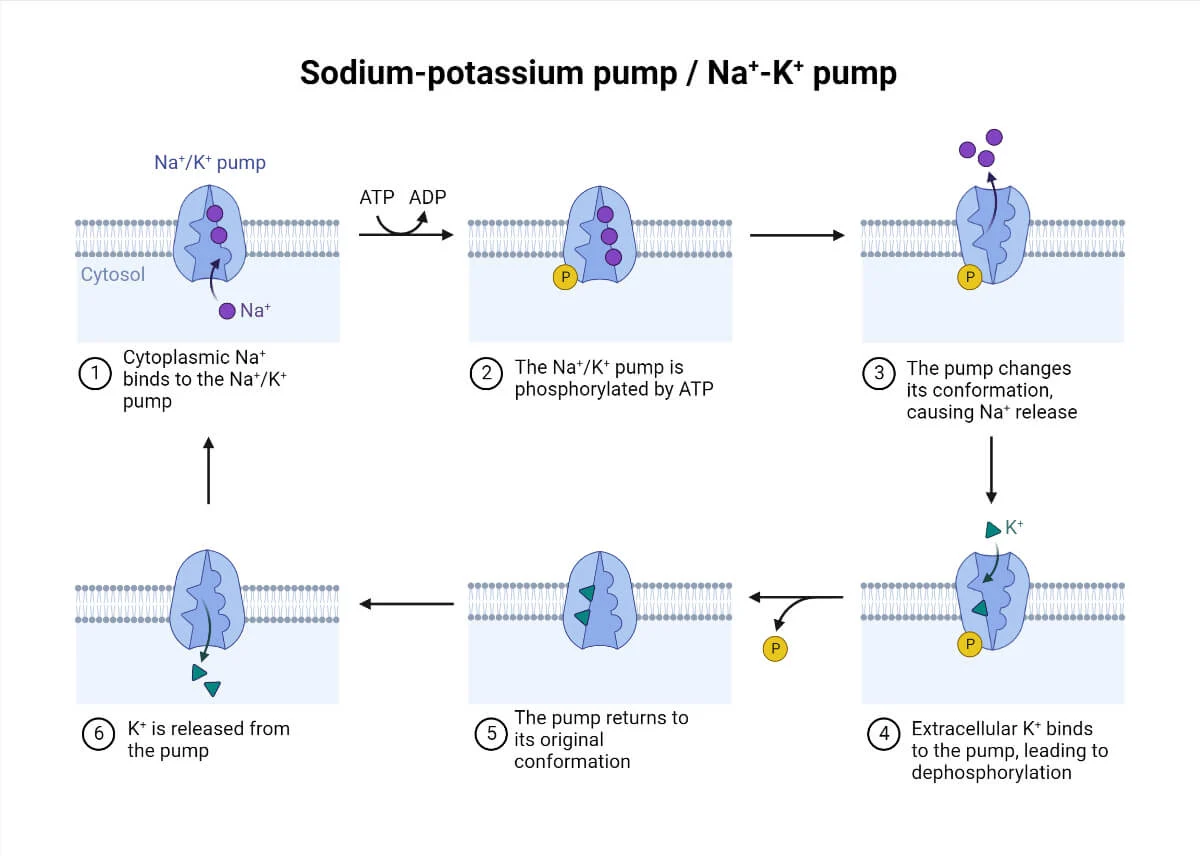
How is RMP maintained?
Sodium Potassium Pump
enzyme that pumps out 3 Na+ for every 2 K+ in
Keeps RMP at -70mV (imbalance creates negative charge)
Negative because of proteins do not cross the membrane
Cost ATP
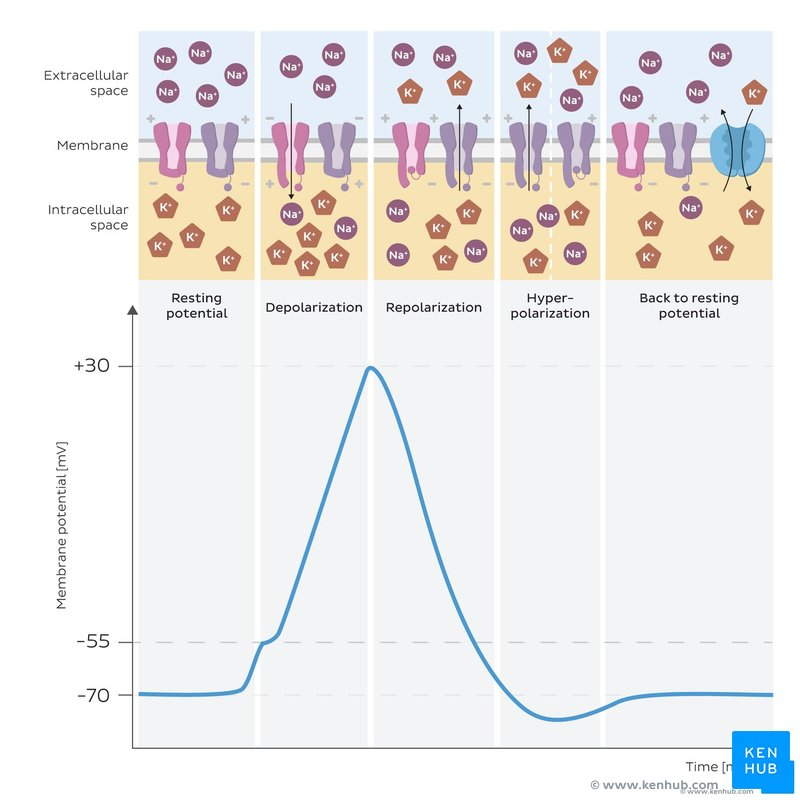
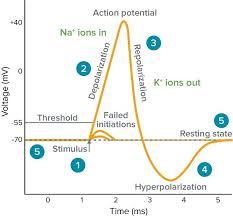
Depolarization
The inside of the cell becomes less negative than the outside of the cell
Causes action potencial
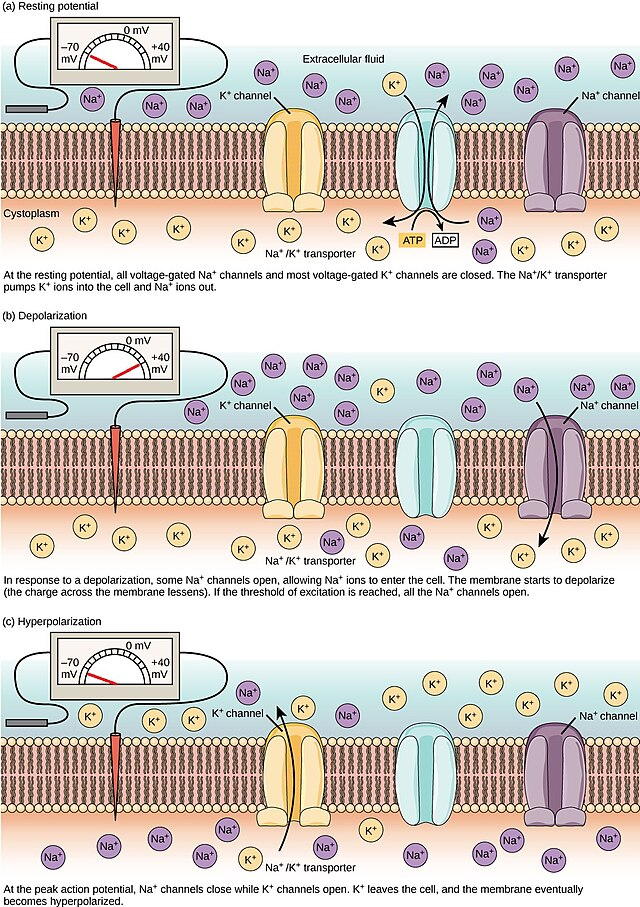
Hyperpolarization
The inside of the cell becomes more negative than the resting membrane potential
Resistant to creating an action potential
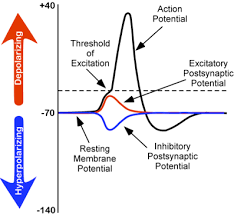
Inhibitory potential
Reduces membrane potential lower than the RMP to make the cell less likely to fire an action potential.
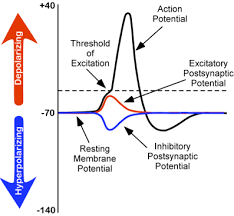
Excretory potentical
Increases the RMP to increase the likelihood of an action potential
How are action potentials initiated?
Normal RMP → deplararization (15mV-20mV above RMP or threshold potential) → Threshold is met or exceeded → all-or-nothing → action potential
(Summation is the combination of several graded potentials)
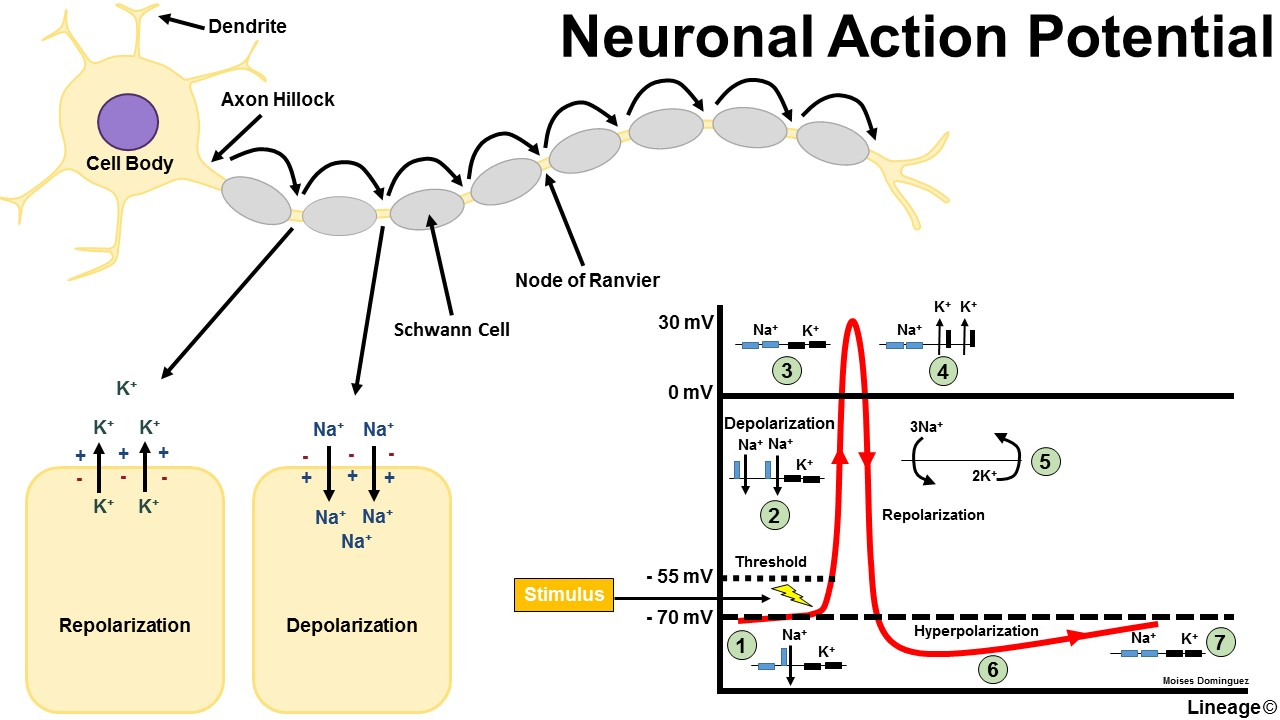
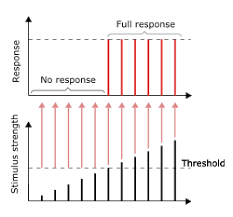
All or Nothing response
When depolarization meets or exceeds threshold potential → action potential
rising RMP → voltage gated Na+ channels open → votage continues to rise until all Na+ channels open → RMP rises to a certain point (too high) → Na+ channels to close → K+ channels to open → ending of the action potential → repolarization (hyperpolarization → normal RMP)
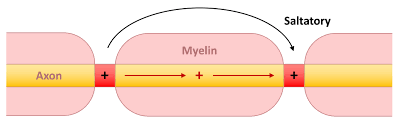
Saltatory conduction
Action potential travels from one break in mylin to the next
“jumps” for faster conduction
action potential is 5-50 times faster in mylinated than unmylinated
Neuron size
Smaller: Easier to active but conduct slower (smaller and have more resistance)
Larger: Harder to activate but conduct faster (larger and have less resistance)
Myelin
A fatty substance that insulates nerve fibers and facilitates faster action potential conduction through saltatory conduction.
Steps of action potential
1. The resting state
2. Depolarization
3. Propagation of an action potential
4. Repolarization
5. Return to the resting state with the help of the sodium-
potassium pump
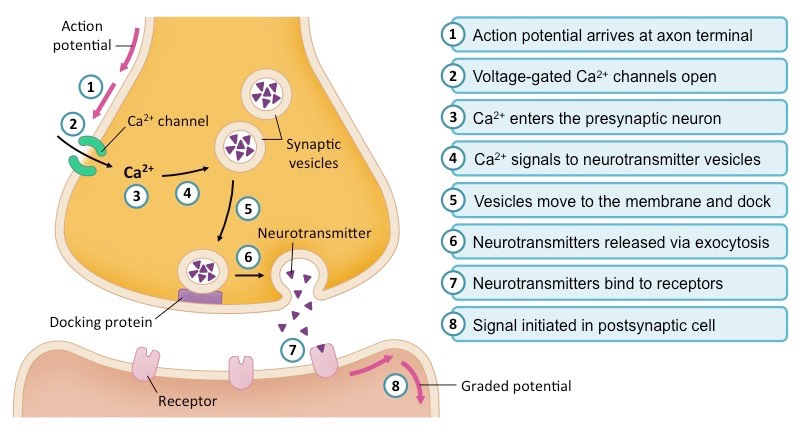
Synapse/ transmission
Impulse → pre-synaptic axon terminal → synaptic vesicals release nuerotransmitters → synaptic cleft → Nuerotranmistters bind postsynaptic receptors (adjacent neuron)
Can only be transmitted from dendrite to cell body
Neuromuscular junction
Synapse for muscles / motor neuron meets muscle
Motor neuron → neurotransmitters → synaptic cleft → bind receptors muscle cell
RMP more negative in muscle
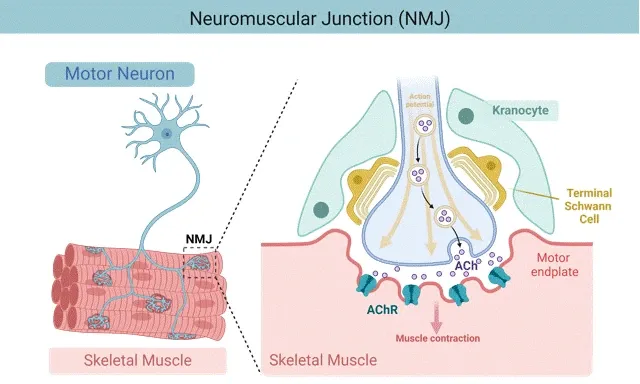
Acetylchonline
Opens up sodium channels (excitatory in skeletal muscle)
Released form parasympathetic neurons
Can be inhibitory (stops sodium channels in heart)
Norepineohrine
Sympathetic nervous response
Inhibitory (exercise) or excitatory depending on the receptor
aids in the body's response to stress and exercise, increasing heart rate and blood flow.
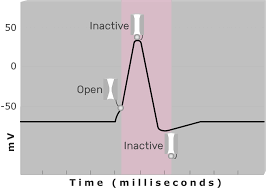
Refractory period
Sodium gates close for a short period of time
Will NOT respond to further simulation and limits firing frequency
Nerve and muscle cells go through this
Time is takes for the muscle fiber to repolarize
Cerebellum
Controls movement and balance
Cerebrum
Fine adjustments and fine-tuning of motor movements
higher cognitive functions (including reasoning, emotion, and memory)
Brain Stem
Control of respiratory and cardiovascular systems
regulation of reflexes such as swallowing and heart rate.
connects the brain to the spinal cord.
Afferent
to the brain
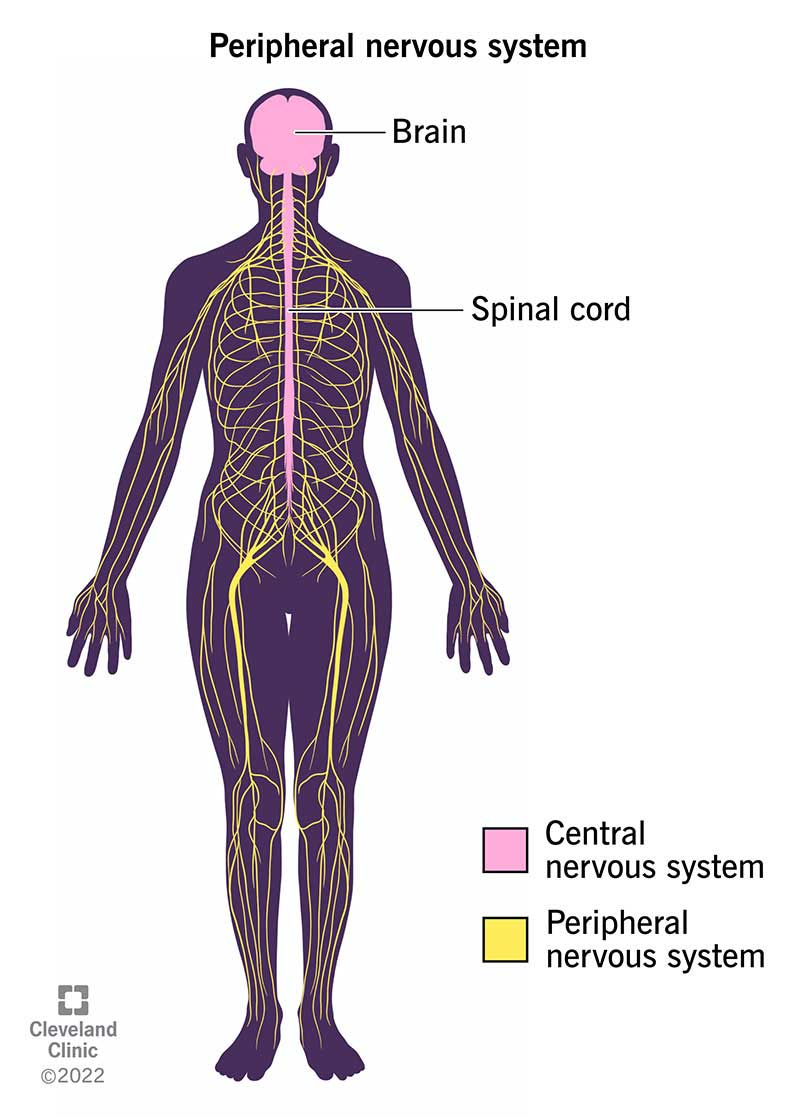
Peripheral Nervous system
12 pairs of cranial nerves connected with the brain.
31 pairs of spinal nerves connected with the spinal cord.
Sensory division: carries sensory information from the body via afferent fibers to the CNS.
End in either SC or brain
Motor division: transmits information from CNS via efferent fibers to target organs.
Autonomic nervous system: controls involuntary internal functions.
Afferent Neuron Pathways Motor
Afferent neuron pathways carry sensory information from the body to the central nervous system
processes it and sends motor commands back out through efferent neurons to control movement.
efferent
from the brain
Afferent Neuron Pathways Sensory
carry sensory information from receptors in the body (like skin, muscles, and organs) to the brain and spinal cord for processing
allows the nervous system to detect stimuli such as touch, temperature, pain, and proprioception.
Efferent Neuron Pathways Motor
carry signals away from the brain to muscles and glands, enabling movement and response.
Afferent Neuron Pathways Sensory
carry sensory information from receptors in the body—like skin, muscles, and organs—toward the central nervous system for processing
allows the brain and spinal cord to detect and respond to stimuli such as touch, temperature, pain, and body position.
mechanoreceptors
respond to mechanical forces such as pressure, touch, vibration, or stretch
Thermoreceptors
respond to changes in temperature
Nocicreceptors
respond to painful stimuli
Photoreceptors
respond to light to allow vision.
Chemoreceptors
respond to chemical stimuli from foods, odors, and changes in blood concentrations
Muscle and nerve joint nerve endings
Kinesthetic receptors
Muscle spindle
Golgi tendon organ
Kinesthetic receptors
In joint capsules sense position and movement of joints
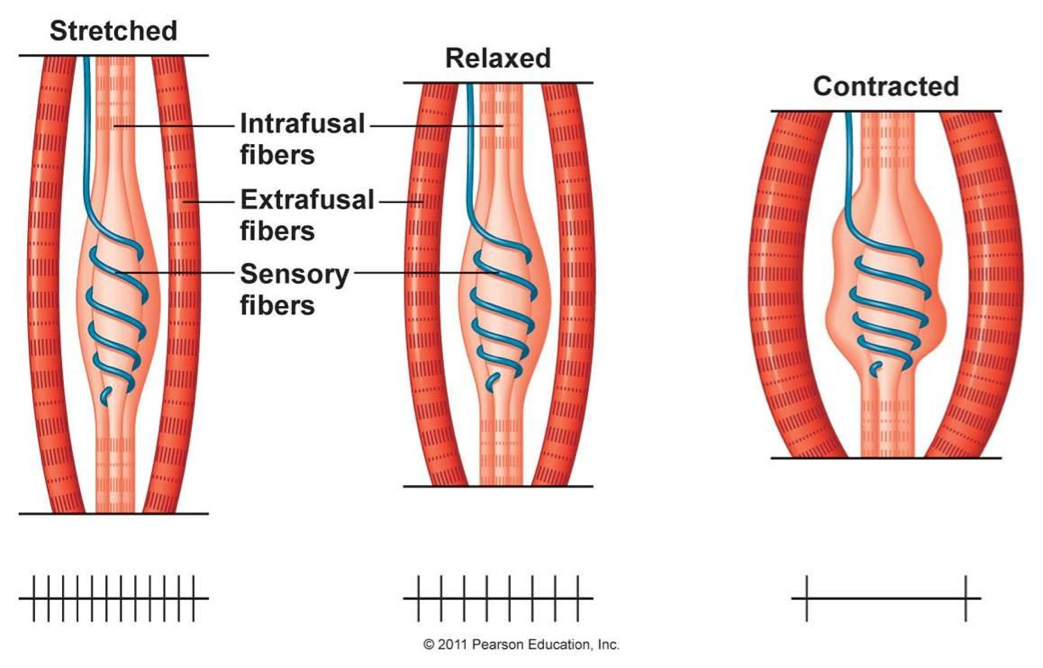
Muscle Spindle
sense how much a muscle is stretched
key role in proprioception, providing feedback to the nervous system about muscle length and changes in length.
Cause stretch/myotatic reflex
Contraction of the muscle when it is stretched too hard, too fast, or both. (protect from tearing or straining)
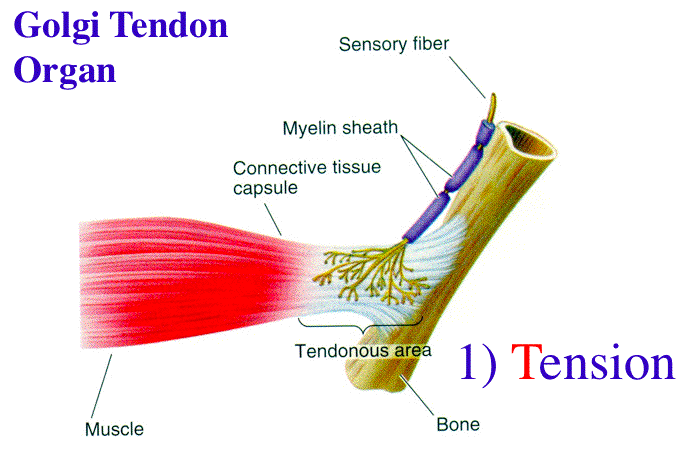
Golgi Tendon Organ
detect tension of a muscle on its tendon, providing information about the strength of muscle contraction
Tension → relaxation
Causes relaxation reflex or inverse stretch reflex
Too much tension on a muscle GTO’s will send signals to the spinal cord to cause the muscle to relax (ensure it does not tear or stain)
Fight-or-Flight response
Sympathetic nervous system
Increase in body functions to prepare the body for perceived threats, involving increased heart rate, blood pressure, and energy availability.
Actions that oppose the sympathetic system
decrease heart rate
Constricts coronary vessels
Constricts tissues in the lungs
Target organs SNS during exercise
heart, blood vessels, bronchioles, respiratory muscles, skeletal muscles, adrenal medulla, pancreas, pupils, digestive tract
Prepare the body for danger by increasing heart rate, blood flow, and oxygen delivery while diverting blood from non-essential functions.
Target organs of PNS during exercise
Nerves, Heart, bronchioles (mild bronchoconstriction → low oxygen need), digestive, badder, reproductive organs
Helps the body relax
Suppressed during exercise but is simulated after to restore homeostasis
Motor control
Deliberate action
reflexes
Deliberate action
Reflexes
Actions of the muscle spindle
muscle contraction triggered resist further stretching
Muscles attached to spindle stretched neurons on spindle transmit info CNS (spinal cord) about muscle length
Middle of spindle dose not contract but stretches
Detect quick stretch → contraction (ensure muscle does not rip or tear)
Actions of the Golgi tendon
Detect changes in tension
Inhabit contracting (antagonist) muscles and excite antagonist muscles prevent injury
Smooth movements
information to Spinal cord
Conscious movement
primary motor cortex → voluntary muscle movements
Clusters of nerves in the basal ganglia initiate sustained repetitive movements
Cerebellum controls fast, complex muscular activities
Motor units and size principle (henneman’s size principle)
The number of motor units depends on the force needed/ produced
Recruits ST units (most fatigue resistant) then FT (Less fatigue resistant but more explosive)
exceptions explosive movements
Engrams
are the physical traces of memory in the brain, representing the storage of learned information and experiences.
Stored in pre-motor movements
slower (sensory portion)
Rapid movements (motor portion)
Nervous system
immediate response
immediate/short term effects
localized
endocrine system
slower response
longer lasting
more general effect
endocrine
ductless glands that secrete hormones directly into the bloodstream.
exocrine
glands that secrete hormones through ducts to target organs.
Sweat glands
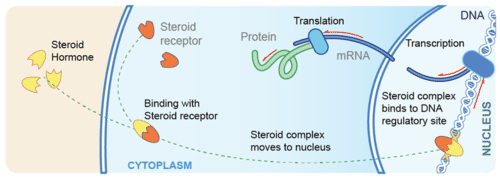
Steroid hormones
made of lipid molecules
diffuse easily through cell membrane
chem structure similar to cholesterol
secreted by the…….
adrenal cortex: cortisol
ovaries: estrogen
testes: testosterone
placenta: estrogen
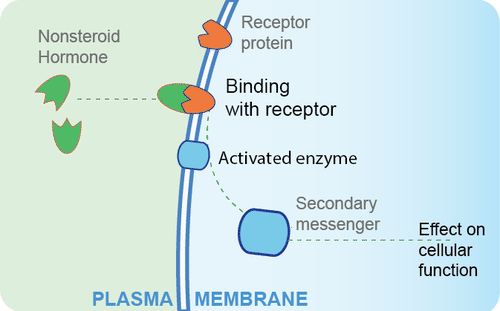
nonsteroid hormones
built of amino acids
Cannot diffuse through membranes
Bind to receptors on outside of cell to cause changes on inside of cell
cause cascade (enzymes and secondary messengers) that leads to DNA activation and transcription and translation
Two types
amino acids derivatives: epinephrine
Protein/ peptide hormones: insulin
prostaglandins (where they come from and what do they do?)
3rd class of pseudo hormones
Derived from arachidonic acid
fatty acid (part of cell membrane)
Act as local hormones (immediate area)
inflammatory response (swelling, vasodilation)
Sensitize nociceptor free nerve ending (pain)
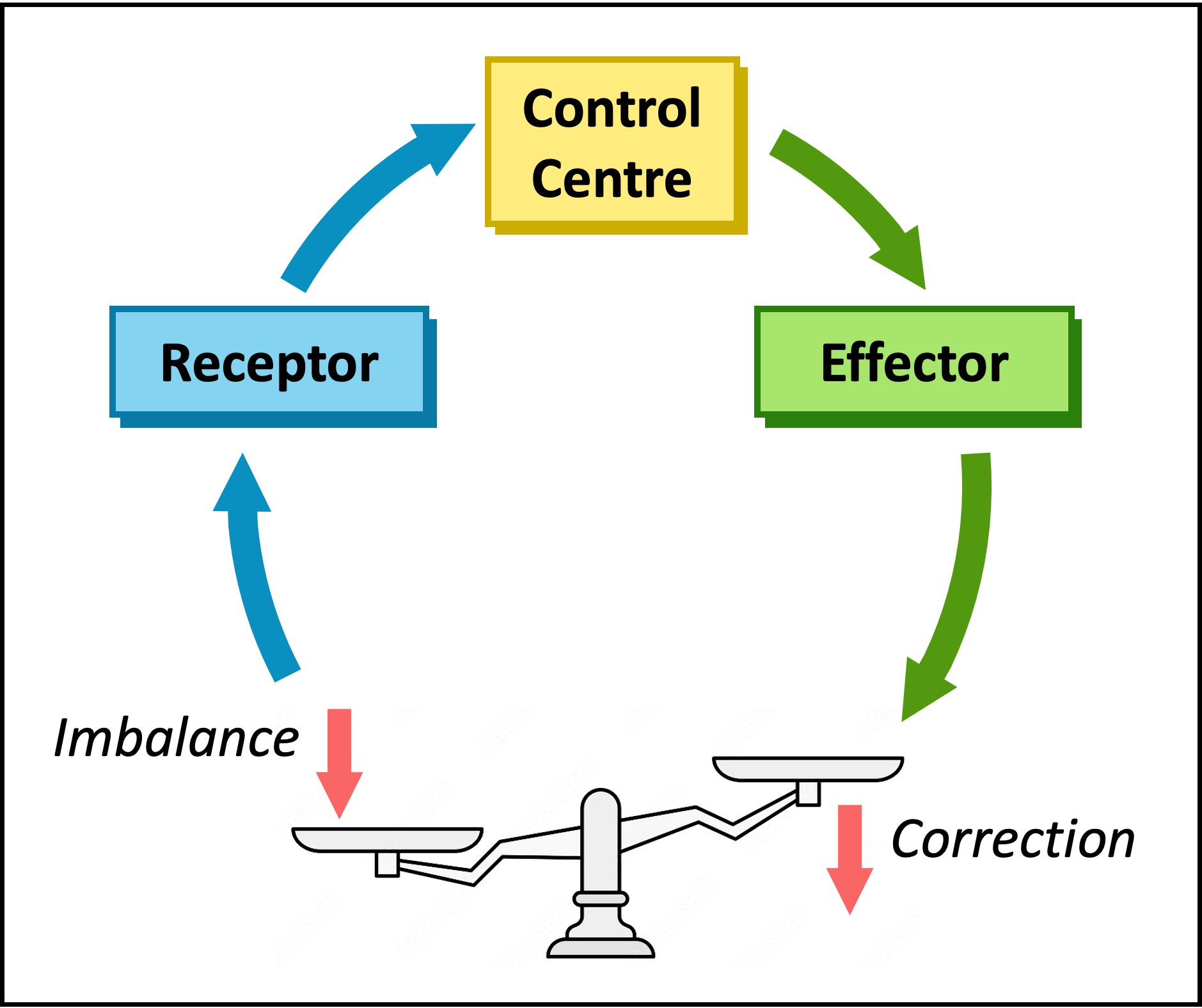
Negative feedback
secretion of hormone causes change that inhibits further secretion of the hormone
key way to maintain homeostasis in the body.
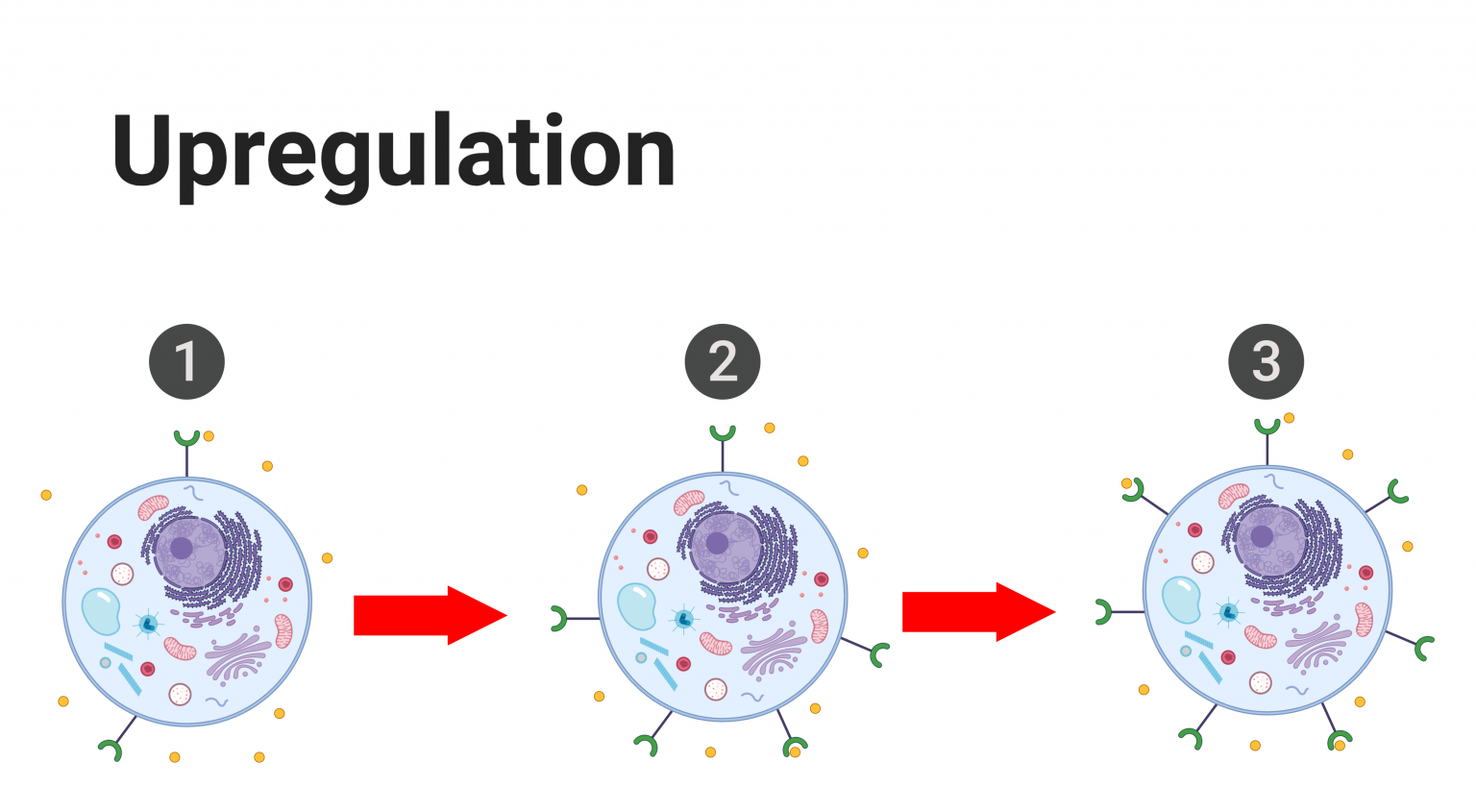
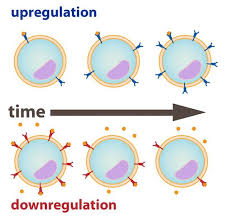
Up regulation
Increase the number of cell receptors (more receptors for the hormone to bind to)
lower concentration of hormone remains in blood plasma for enhancing hormone sensitivity and effectiveness.
Often times good
down regulation
Decrease in cell receptors, reducing hormone sensitivity leading to higher hormone concentrations in blood plasma.
often times bad (type 2 diabetes)
Pituitary gland
relay between nervous system and endocrine systems
produces and secretes hormones regulating various bodily functions, including growth and metabolism depending on the signals from the nervous system and hypothalamus
Posterior pituitary
Hormones
Antidiuretic hormone
Oxytocin
Controlled by nervous signals
Anterior pituitary
Hormones
growth hormone
thyrotropin
Luteinizing hormone
Prolactin
Adrenocorticotropin
Exercises increases all six hormones
4 tropic hormones
control function of other glands
adrenal glands, gonads, thyroid
Other
prolactin and GH
Growth hormone
promotes muscle growth and hypertrophy → amino acid transport
simulates breakdown of fat
levels elevated during aerobic exercise in proportion to exercise intensity
higher the intensity more produced
Thyroid gland
Hormones
T3 (triiodothyronine), T4 (thyroxine)
Increase metabolic rate 60-100%
increased protein. enzymes synthesis, size and number of mitochondria in cells. FFA availability for oxidation, promote rapid cellular uptake glucose, enhance glycolysis
increases secondary messengers in cells
Calcitonin
metabolizes calcium
not strong regulator in adults
Adrenal Medulla
medulla (inner)
cortex (outer part)
Hormones
catecholamines: epinephrine, norepinephrine
stimulate sympathetic NS prepare for action
Increase heart rate and force of heart contraction, blood pressure, reparation, metabolic rate (glycogenolisys, and release if glucose and FFA in blood)
allow more blood transported to skeletal muscles → vasodilation and vasoconstrictions
Adrenal cortex
Mineralocorticoids
maintain electrolyte balance extracellular fluids
Aldosterone → sodium retention → retain more water
Glucocorticoids
Maintain contant plasma glucose levels between meals
Cortisol: important stress hormone
Gonadocorticoids
Released addition released by reproductive organs lesser amounts
Androgens, estrogens, progesterones
Pancreas
Both endocrine and exocrine
Insulin (only hormone lowers blood glucose)
secreted → plasma glucose elevated (hyperglycemia)
promotes glucose uptake cells (muscles + connective tissues)
Promotes glycogenesis
inhibits gluconeogenesis
Building and storing state
Glucagon
Secreted → plasma glucose lowered (hypoglycemia)
Increases liver glycogenolysis
increases gluconeogenesis
Raises blood glucose
How training effects glucagon and insulin?
Up regulation for glucagon (have to release less hormone)
glucagon increases when exercises
Training increases the receptors for glucagon
Untrained higher glucagon levels then trained
Down regulation for insulin
Insulin decreases when exercises
Able to better target tissues that need glucose
Training reduces the receptors for insulin
increased cellular receptors for glucose
increase sensitivity for glucose
Untrained has lower insulin levels then trained
Androgens
Testosterone
male 2nd sex characteristics
major anabolic hormone
stimulates muscle hypertrophy
Estrogens
Female 2nd sex characteristics
muscle function
Progesterone
Prepares for pregnancy
Kidney
Erythropoietin: regulates red blood cell production (stimulates production of blood cells)
Important for adaptation to training and to altitude due to the oxygen-carrying capacity of red blood cells
Major endocrine glands for metabolic regulation
anterior pituitary gland
thyroid gland
adrenal gland
pancreas
Hormones produced by these affect metabolism if carbs and fats during exercise
Hormones
Chemical messengers that travel in blood to regulate various physiological processes in the body.
Binds to specific receptors on cells (specific target organ)
2,000-10,000 receptors per cell
Can be released by non-endocrine tissues (nerve endings, adipose tissue)
Adequate glucose for exercise needs
glucose re-uptake by liver
glucose uptake by muscles
Increase circulating glucose metabolism (counter the effects of insulin)
glucagon
epinephrine
norepinephrine
cortisol
Increase blood glucose
Circulating glucose during exercise affected by
Growth hormone
increases FFA mobilization, decreases cellular glucose uptak
T3 + T4
increase glucose catabolism and fat metabolism
amount of glucose regulated from liver depends on exercise intensity and duration
As Exercise intensity increases…
catecholamine release increases
glycogenolysis rate increases (liver and muscles)
Muscle glycogen used before liver glycogen
As exercise duration increases….
more liver glycogen utilized
increase muscle glucose uptake → increase glucose release
as glycogen stores decrease, glucagon levels increase
Cortisol and exercise
Peaks during exercise, increases glucose availability then decreases as exercise progresses to longer durations
Insulin and carb metabolism during exercise
enables glucose uptake in muscle
During exercise
insulin concentrations decrease
cellular insulin sensitivity increases
more glucose uptake into cells
use less insulin
FFA mobilization and fat metabolism endurance exercise preformance
glycogen depleted → fat energy substrates
response → hormones accelerate fat breakdown (lipolysis)
Triglycerides → FFA + glycerol
FFA transported → muscles
rate of triglyceride breakdown → FFA may determine the rate of cellular fat metabolism
Lipolysis stimulated by…
Decreased insulin
Epinephrine*
Norepinephrine*
Cortisol*
Growth hormone
(Stimulate lipolysis via lipase)
(can also promote glucose metabolism)
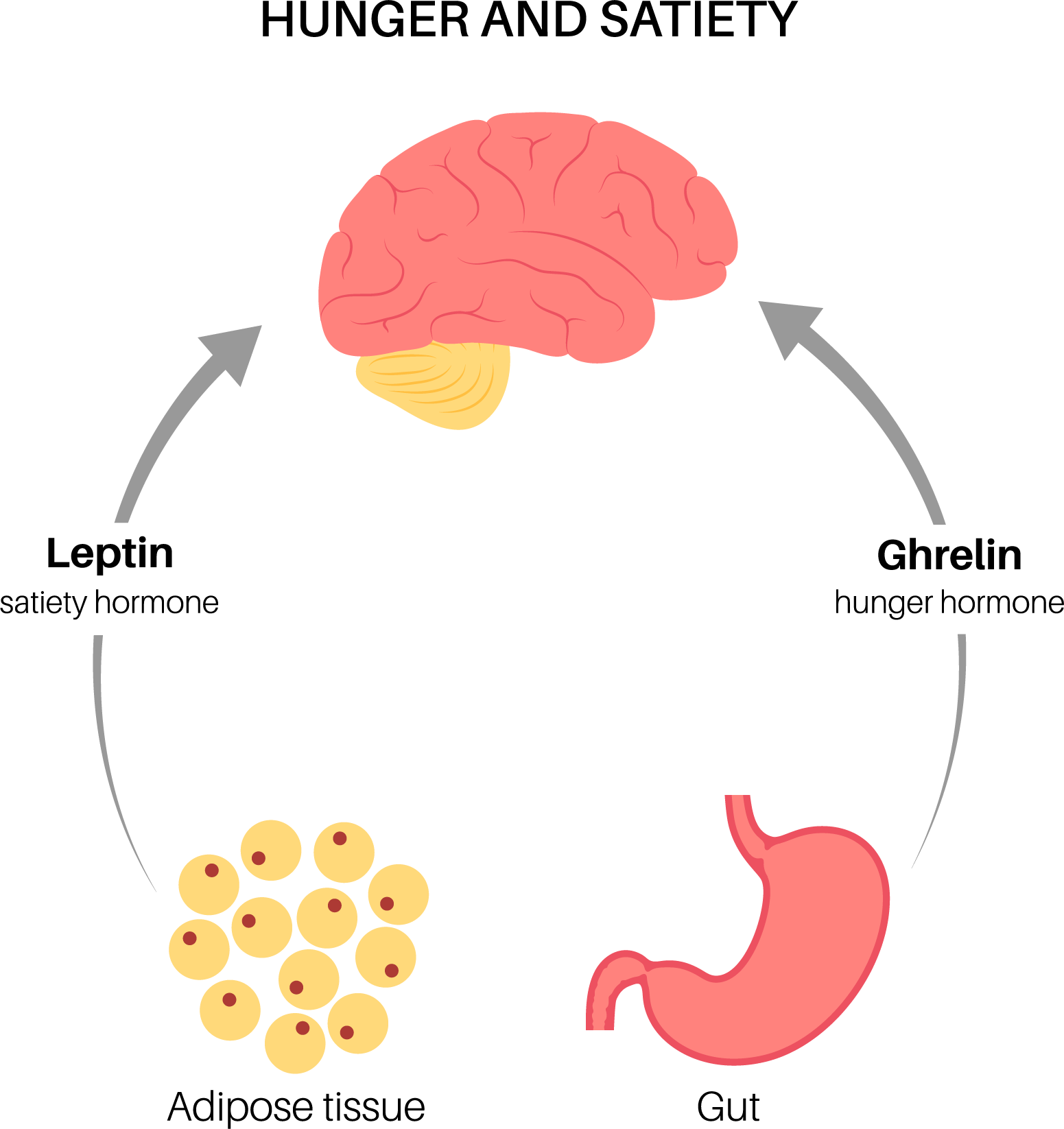
Hunger Hormones
Cholecytokinin (CCK): stimulated by full stomach (released by intestine)
Ghrelin: Triggered by empty stomach → hunger (secreted by pancreas)
Leptin: acts on the brain to suppress hunger (secreted by fat cells)
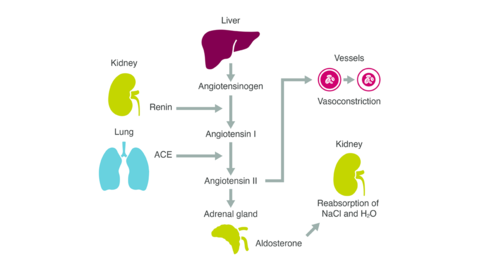
How renin, ADH, and aldosterone interact to maintain plasma volume
Renin: increases blood pressure and regulates blood volume, converts angioteninogen → angiotensin 1 → (by enzymes) angiotensin 2 (causes vasoconstriction → raises blood pressure)
increases blood volume (sodium retention) and pressure
Simulated by low blood pressure → loss of fluid
Aldosterone: Regulates fluid/electrolyte balance
sodium retention → water retention → increases blood pressure and volume
Antidiuretic hormone/ vasopressin: fluid regulation
increases water reabsorption from urine
concentrate electrolytes in blood
Increases blood osmolarity
How they work together: Renin released from kidneys response low blood pressure → Renin → angiotensin 1 → production angiotensin 2 → promotes secretion of aldosterone from adrenal glands + stimulates thirst/ production of ADH → Urine volume decreases. Regulate/maintain homeostatic plasma volume → controlling blood pressure + fluid balance
Osmolarity
is the measure of solute concentration in a solution, reflecting the number of osmoles of solute per liter of solvent. It plays a crucial role in fluid balance and the movement of water across cell membranes.
Hemoconcentration
highly concentrated blood
thick/ increased viscosity
hard for heart to pump blood
Hemodilution
Unconcentrated blood
More fluid/ too much water
Low solutes
thin/ decreased viscosity