Pathophysiology E3: MSK PT II
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
osteoblasts vs osteocytes and osteoclasts
• Osteoblasts: build bone by forming type 1 collagen & proteoglycans which construct the bone matrix (osteoid tissue)
• Osteocytes: mature bone.
• Osteoclasts: move over the bone and produce proteolytic enzymes that break down the matrix →calcium and phosphate into the bloodstream.
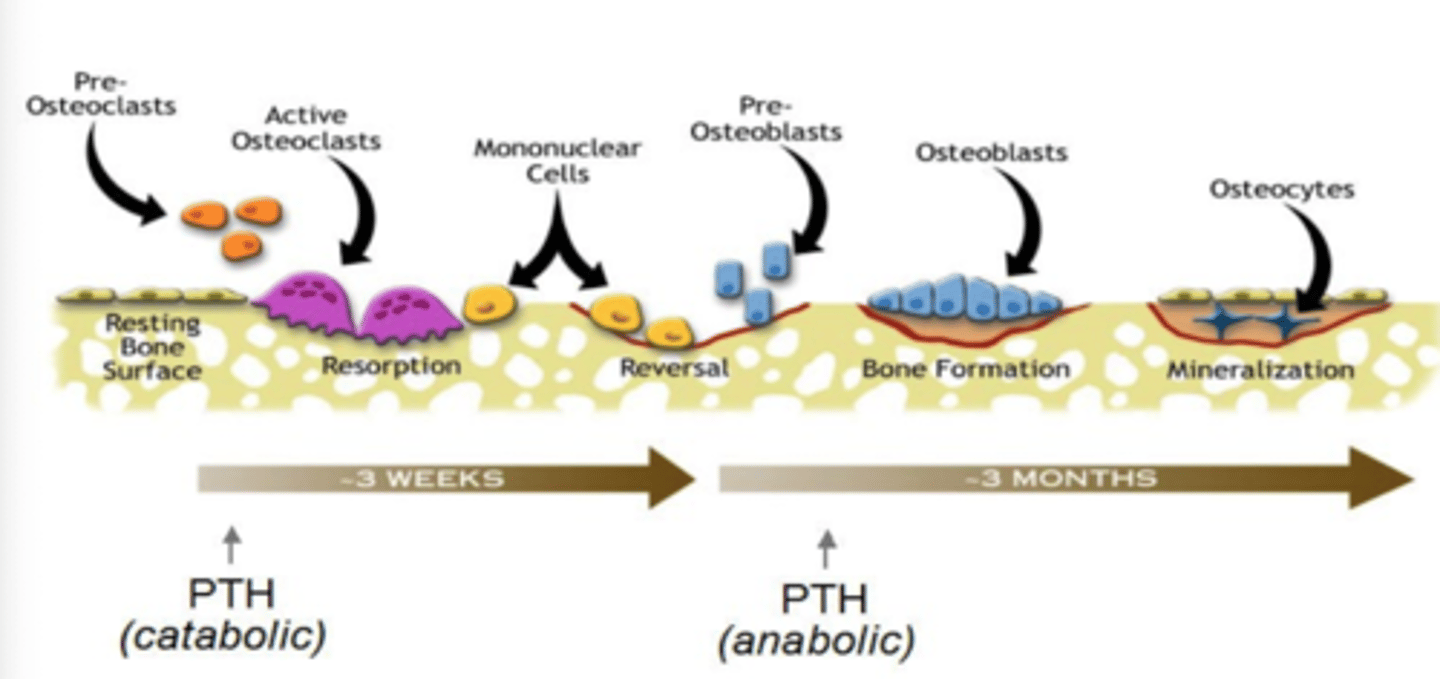
What occurs with PTH acutely and chronically in bone remodeling?
PTH released with hypocalcemia
PTH release acutely will promote breakdown of bone (catabolic)
pre-osteoclasts develop into active osteoclasts>breakdown bone/release Ca2+.
PTH release chronically will promote formation of bone (anabolic)
pre-osteoblasts develop into active osteoblasts>form new bone
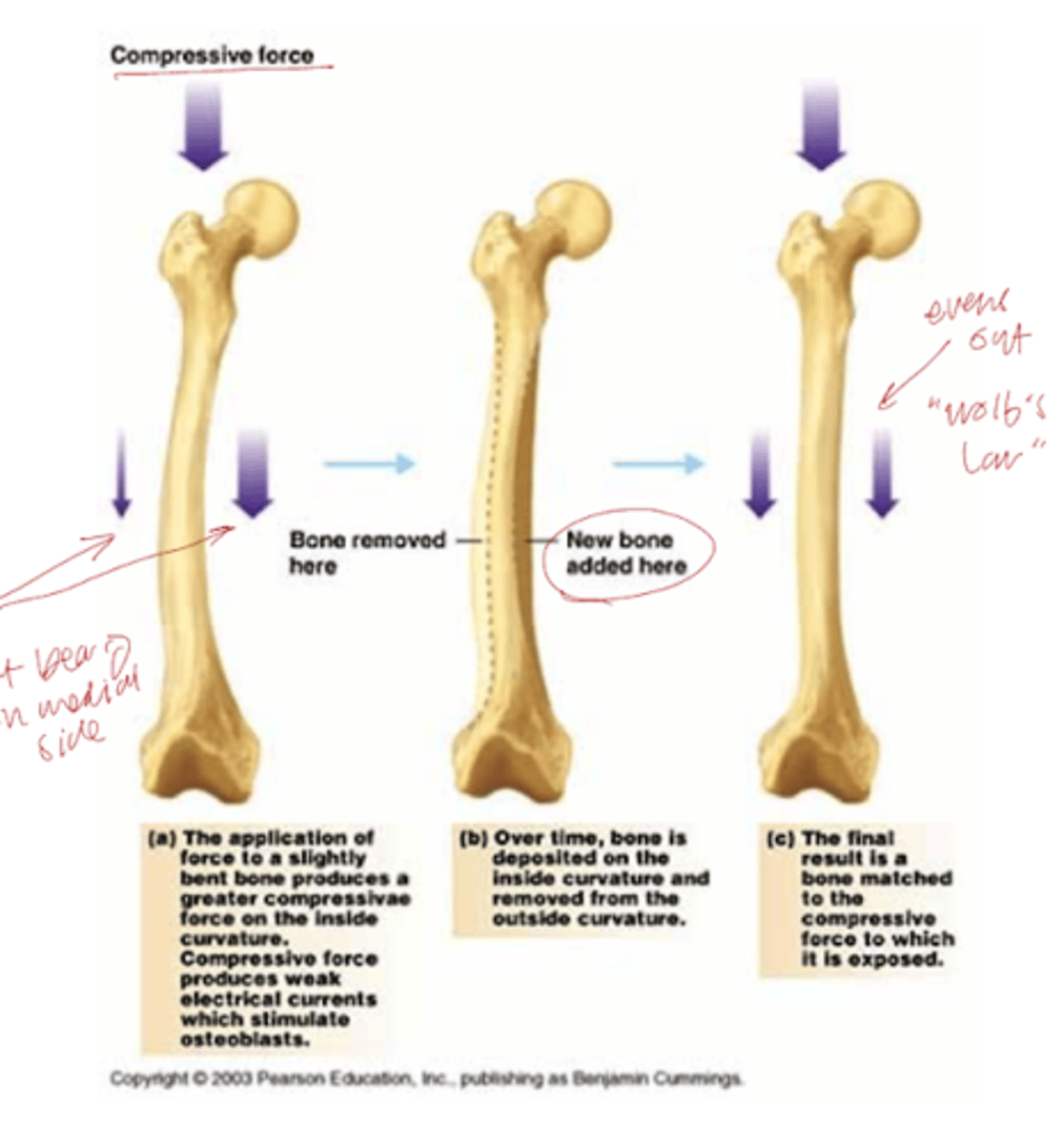
How can the bone respond to changes in stress?
Through bone remodeling (Wolf's Law) - bone can change shape and adjust depending on where there is more stress on the bone
How does PTH release regulate the kidneys?
Kidneys: inc phosphate diuresis by dec resorption of phosphate allows for inc tubular resorption of calcium
Stimulates the kidney to make activated form of vitamin D
How does PTH release regulate the intestines?
inc permeability of gut cells to calcium
What is the affect of Vitamin D at the intestines, bone and kidney?
GI: inc synthesis of Ca-binding protein
Bone: thought to play a role in mineralization
Kidney: feedback on itself
What is the main effect of steroids? Why is this important to monitor in RA pt?
Impaired skeletal growth, dec bone formation & bone mass
RA pt benefit from anti-inflammatory properties but need DEXA scan annually to monitor bone density!!
What is a big reason osteoporosis occurs in post-menopausal women?
Estrogen is a key hormone for maintaining bone mass!!
At menopause, estrogen levels drop→ skeleton rapidly loses bone mass.
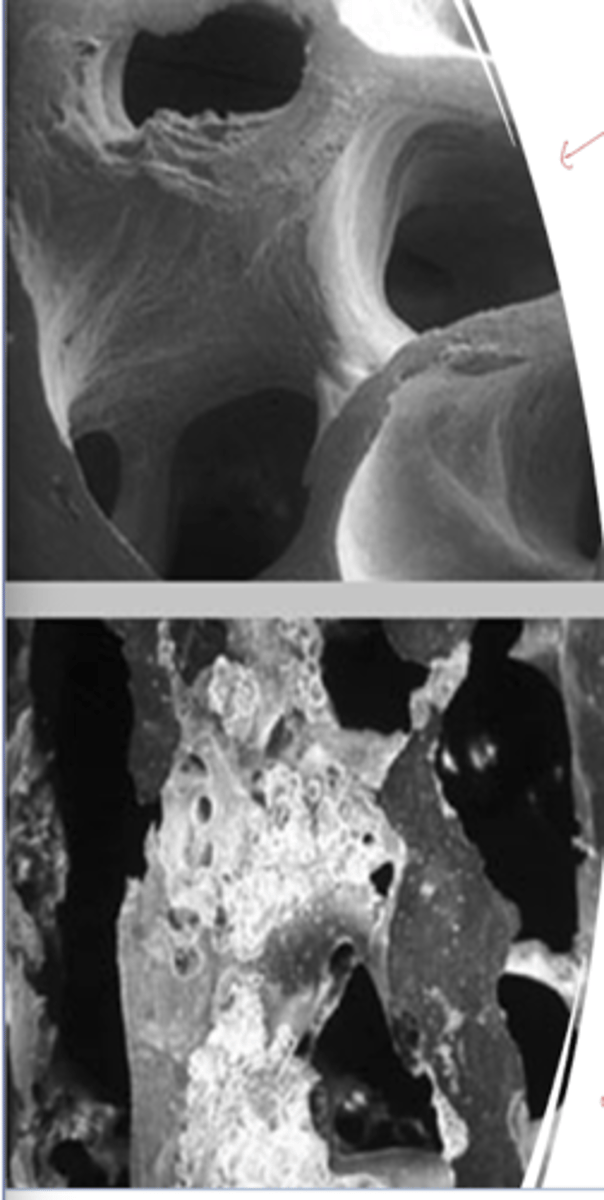
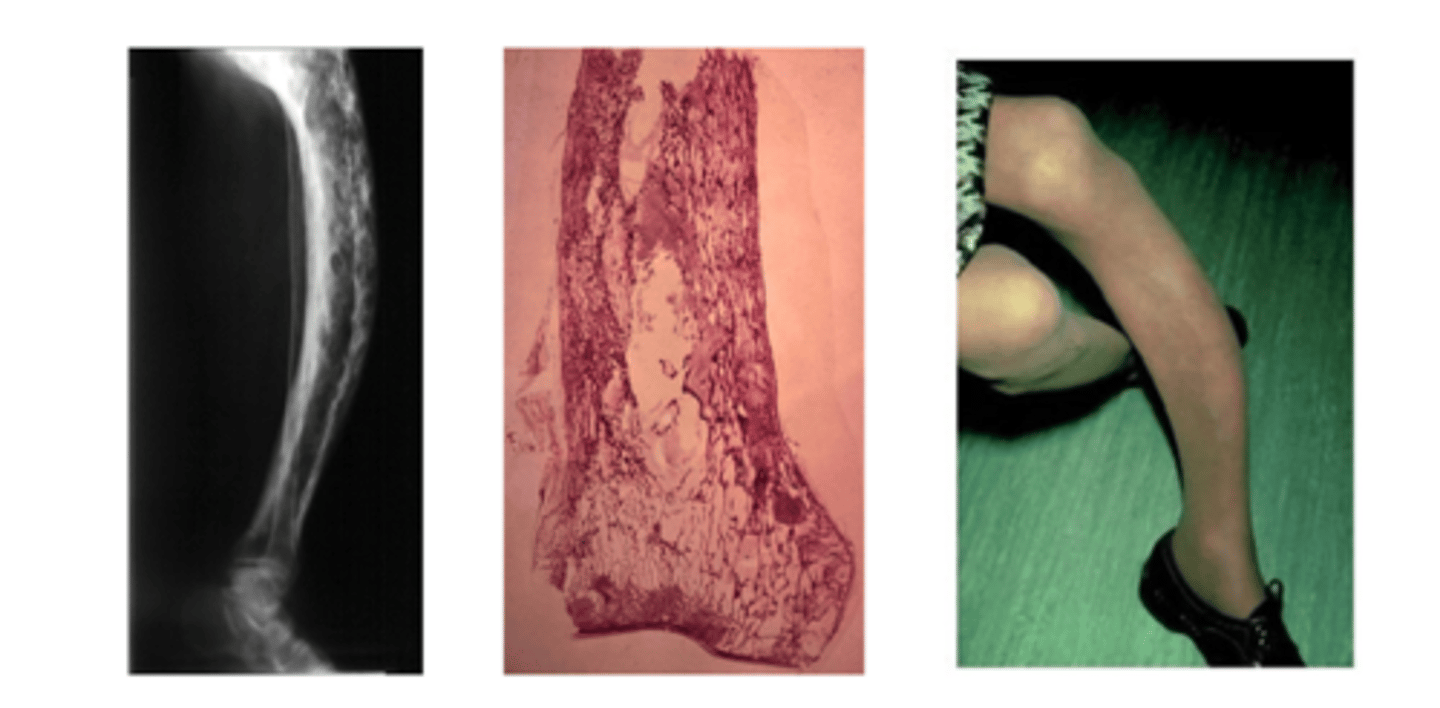
What is paget's dz (osteitis deformans)?
Chronic condition characterized by disordered bone remodeling
• Excessive bone resorption results in lytic lesions, followed by disorganized & excessive bone formation
AKA bone is getting destroyed but is not getting repaired well
etiology of pagets?
unknown! may be viral in origin. common in persons of english descent
What are the 3 phases of pagets?
• "hot" (osteoclastic) stage - breakdown of bone
• Mixed stage - cortex thickens causing bones to become larger than normal and distorted (trying to rebuild)
• "cold" (burnt out) stage - little cellular activity. Radiographs show thickened & disordered bones
*pt can be in all stages at once or in a diff order
What is a typical imaging sign for paget's dz?
imaging - mosaic pattern --> disordered formation
Clinical manifestations of pagets
Pain in affected bone
Skull is frequently involved
• Becomes very heavy & may collapse over C1, compressing the brain & spinal cord
• Hearing loss follows involvement of the ossicles
High output cardiac failure- rare
blood shunted to bones due to inc demand (constant building and breaking down) --> less blood to kidney
**often incidental dx
What is gout? What other dz is it associated with?
A metabolic disorder characterized by an elevated serum uric acid concentration (hyperuricemia)
• Incidence has inc with the rise in obesity & HTN
• Monosodium urate crystals deposit in and around joints and tendons (supersaturate) --> crystallize out of solution
What are the 2 classifications of gout?
• Primary – hyperuricemia w/o any other disease
• 1/3 of cases
• Secondary – occurs in association with another illness that results in hyperuricemia
• ↑ DNA turnover (leukemia, lymphoma, S/P chemotherapy)
Uric acid results from degradation of what?
Purine catabolism!
What are 3 potential etiologies of gout (think about purines)?
1. Overproduction of purines
2. ↓ urinary uric acid excretion
• 90% of idiopathic cases result form impaired renal
uric acid excretion (not high dietary intake)
3. Diuretic administration- water loss results in higher concentrations of uric acid in the blood.
4. ↑ catabolism (breakdown) of nucleic acids due to greater
cell turnover
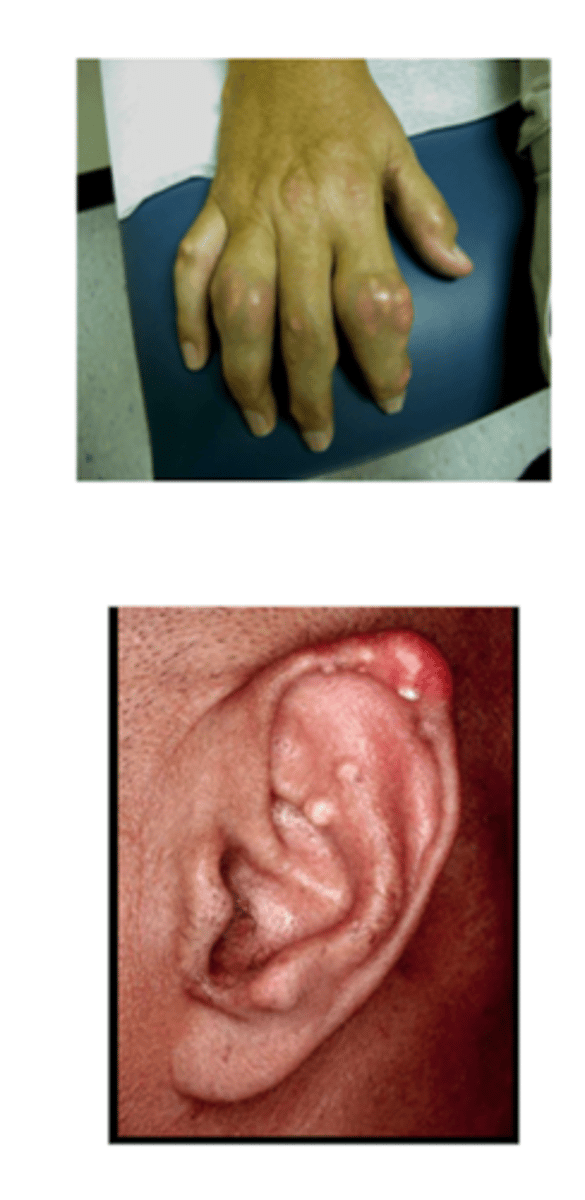
Where are common sites of deposition of uric acid crystals?
AFFECTS COOLER JOINTS
• Avascular tissues - cartilage
• Relatively avascular tissues - tendons, ligaments
• Cooler peripheral joints - toes, ankles
• Cooler tissues - ears
• In severe, long-standing disease - larger central joints & organ parenchyma, such as kidney
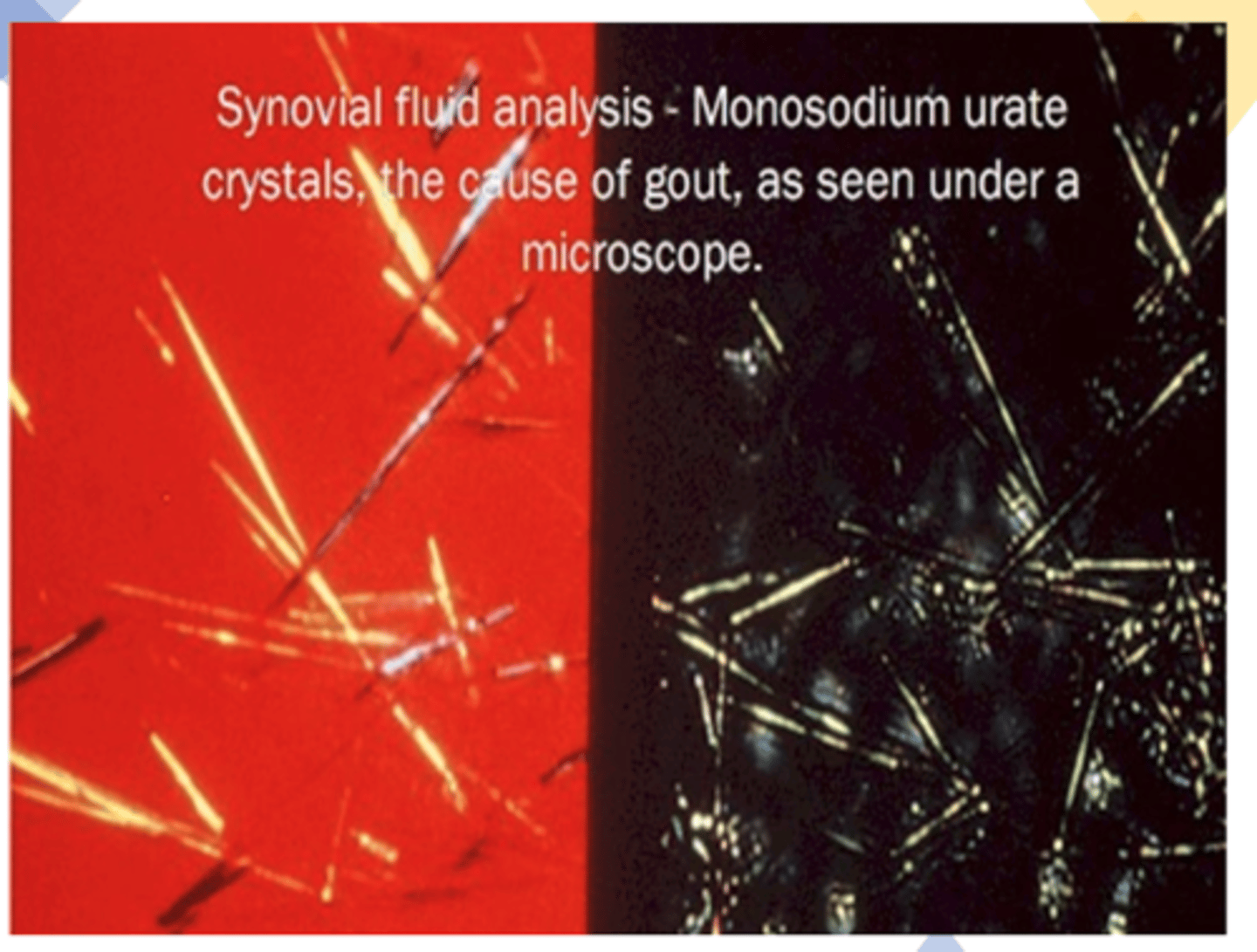
Explain the pathophys of goiut
1. The monosodium urate crystals cause an acute inflammatory reaction→ severe pain "exquisitely tender"
Activate the kinin system local vasodilation, pain, & swelling & the complement pathway --> red, warm, tender, fever
2. Phagocytosis of crystals by macrophages stimulates the release of proinflammatory cytokines (neutrophils come in)
3. inflammatory response down regulates spontaneously & completely over several days (w/o therapy)
Is gout typically unilateral or bilateral?
Typically monoarticular --> podagra (great toe affected)
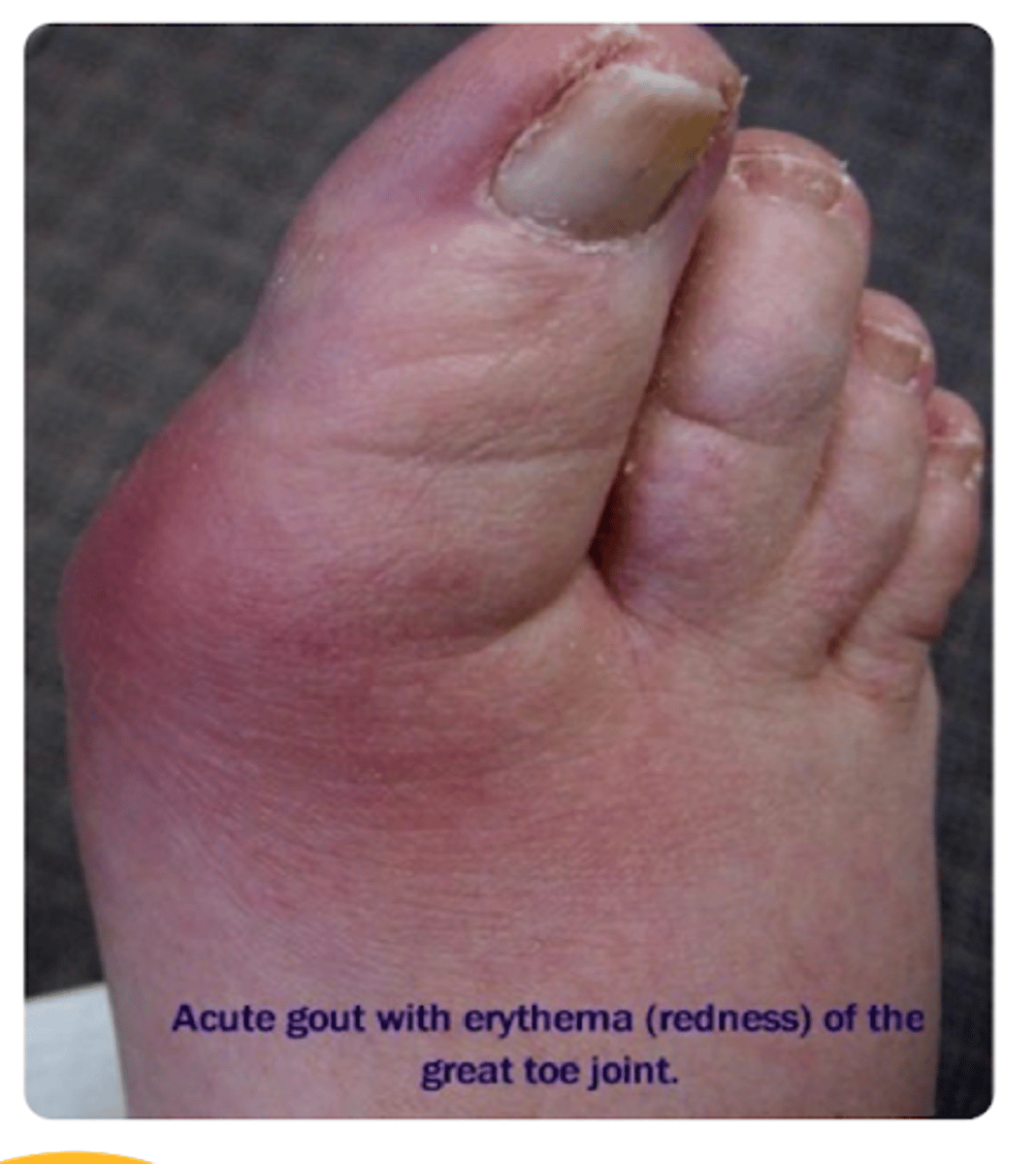
What are podagra, tophi, and erosive arthritis?
Podagra and episodic oligoarticular arthritis
• Can awaken pts in the night with dramatic pain, redness, swelling, & warmth
Tophi form – firm, irregular subcutaneous deposits of urate crystals
• Found along:
• Tendinous tissues
• Extensor surfaces of joints & tendons
• Outer helix of the ear
Erosive arthritis: can develop w repeated attacks to same joint
What finding is key in dx of gouty arthritis?
birefringent urate crystals