SALIVA & SALIVARY PROTEINS
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
what is saliva
a secretion of proteins and glycoproteins in a buffered electrolyte solution
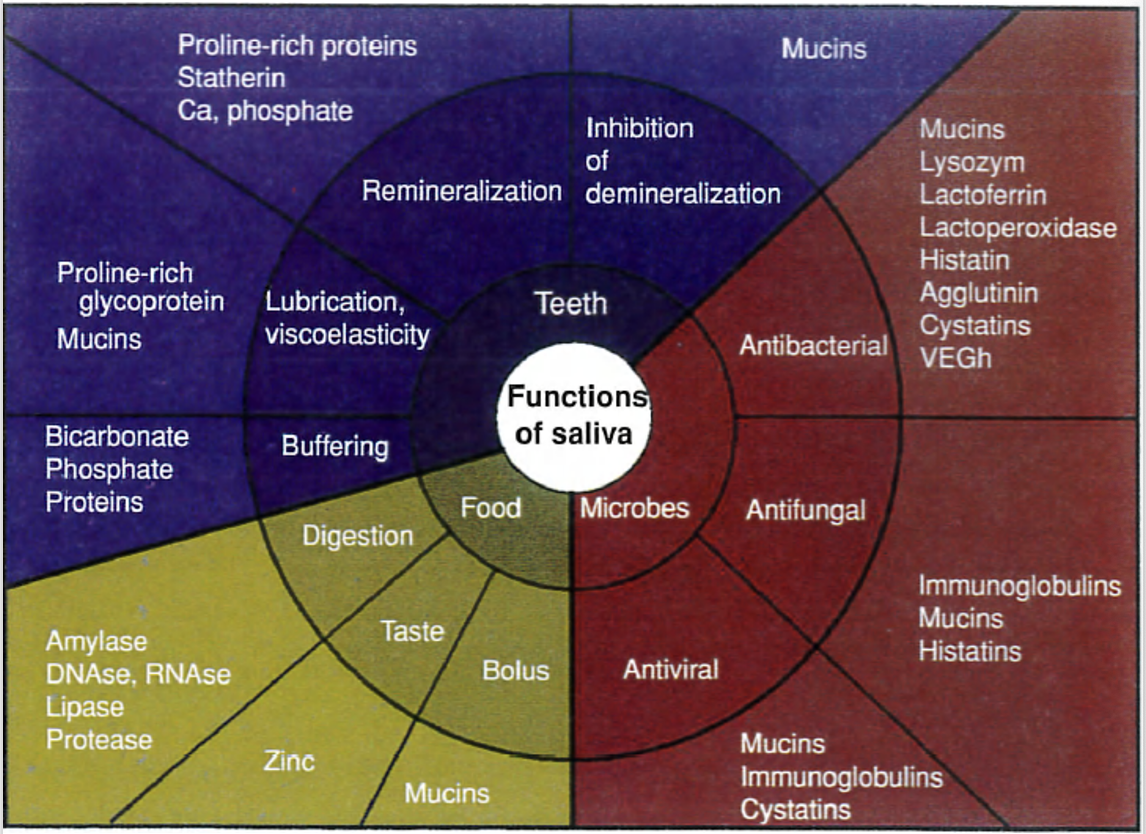
what are the functions of saliva (7)
lubricant for:
mastication
swallowing
speech
oral hygiene - washes away debris
defensive function - has anti-bacterial/ viral/ fungal properties
maintenance of oral pH - pH ≈ 7.2
bicarbonate/ carbonate buffer system for rapid acid neutralisation
contains digestive enzymes
a solvent necessary for taste
remineralisation - contains Ca2+ and PO43-
what is saliva dysfunction associated with (3)
oral pain
infections
increased risk of dental caries
what is the average flow rate in ml/ min
0.3-7ml per minute (depends on activity)
what is the daily salivary secretion volume in adults from both major and minor salivary glands
800-1500ml from major and minor salivary glands
what does the pH of saliva range from
6.2-7.4
serous saliva VS mucous saliva
serous saliva
mainly contains enzymes like alpha amylase for starch digestion
mucous saliva
contains mucins for lubrication of mucosal surfaces
what type of salivary glands are the parotid, submandibular, sublingual and minor salivary glands
parotid = serous
submandibular = seromucous
sublingual = seromucous but predominantly mucous
minor salivary glands (> 600) = mainly mucous
what factors affect the composition and amount of saliva produced (8)
flow rate
circadian rhythm - we produce less saliva at nighttime
type and size of gland
duration and type of stimulus
diet
drugs
age
gender
what is mucositis and how is it classified
mucositis: the painful inflammation and ulceration of the mucosa lining the digestive tract i.e. mouth and GI tract (xerostomia can increase the risk of mucositis)
classified by Grades 1-4
outline Grade 1 mucositis
soreness
± erythema
mild symptoms
intervention not needed
outline Grade 2 mucositis
erythema
ulcers
moderate pain
patient can still swallow
outline Grade 3 mucositis
considered severe mucositis
extensive pain
ulcers with extensive erythema
patient cannot swallow food
outline Grade 4 mucositis
considered severe mucositis
life-threatening consequences
alimentation is not possible
what is mucositis often caused by
chemotherapy/ radiotherapy
what type of salivary gland are Von Ebner’s
serous
outline the protein composition of saliva
proteomics and peptidomics used to analyse saliva
3652 protein detected
12,562 peptides detected
51% of proteins and 79% of peptides also contained in plasma proteins
proteins in saliva are similar to proteins in plasma just in smaller amounts
what proteins are found in saliva
amylase
mucin - MG1
mucin - MG2
histatin
statherin
proline rich protein (PRP)
cystatin
😫
what are the main types of mucins and outline each
MG1
78% CHO
15% protein
7% sulphate
O-glycosylated
N- and C termini are rich in cysteine
MG2
glycosylated
contains threonine-rich tandem repeats
what characteristics do MG1 and MG2 share
terminal sialic acid groups
form complexes with other salivary molecules
glycosylated
which salivary proteins are antimicrobial
lysozyme
sialoperoxidase/ lactoperoxidase
lactoferrin
histatins
secretory IgA
IgG
outline lysozyme
also known as muramidase
cleaves bacterial peptidoglycan - major component of Gram positive bacterial cell walls
outline sialoperoxidase/ lactoperoxidase
sialoperoxidase/ lactoperoxidase
cleaves terminal sialic acid groups of bacteria
peroxidase enzyme
produce oxidised intermediates through catalysis of hydrogen peroxide
outline lactoferrin
present in body secretions like breast milk and neutrophil granules
binds to free iron ions (Fe3+) which bacteria use for nutrients - removes the substrate needed for bacterial growth
binds to LPS of bacterial cell walls (major component of Gram negative bacteria outer membrane)
outline histatins
unique to saliva
very small proteins
antifungal and antibacterial as well
disrupt membrane function
bind to LPS and other receptors causing formation of reactive oxygen species
binds to tanins, mucins and enamel
what is the main immunoglobulin found in mucous secretions
secretory IgA - antimicrobial
where is secretory IgA found
tear glands
salivary glands
mammary glands
respiratory system
GU tract
GI tract
what is secretory IgA produced by
B-lymphocytes adjacent to mucosal cells
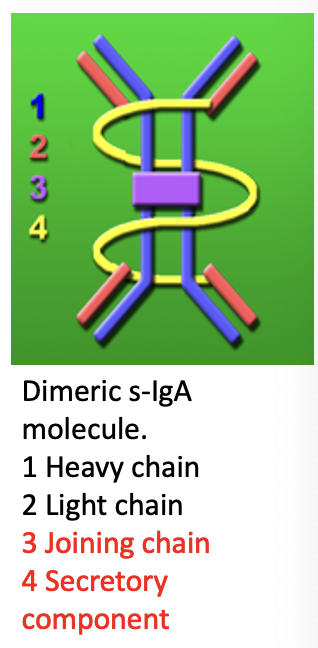
what is the structure of secretory IgA
heavy chain
light chain
joining chain - not found in serum IgA
secretory component - not found in serum IgA
which glands have the highest secretory IgA
saliva in minor salivary glands have the highest level of secretory IgA
when are levels of sIgA highest
highest levels in the morning
lowest levels in the evening
» follows circadian rhythm (gradually decreases as day goes on)
why do levels of sIgA vary
levels vary in response to physical and psychological stress through interactions with the autonomic nervous system
also affected by flow rates - concentration normally decreases as flow rates increase
outline IgG
derived from serum
mainly neutralises and inhibits microbial adhesion
may opsonise
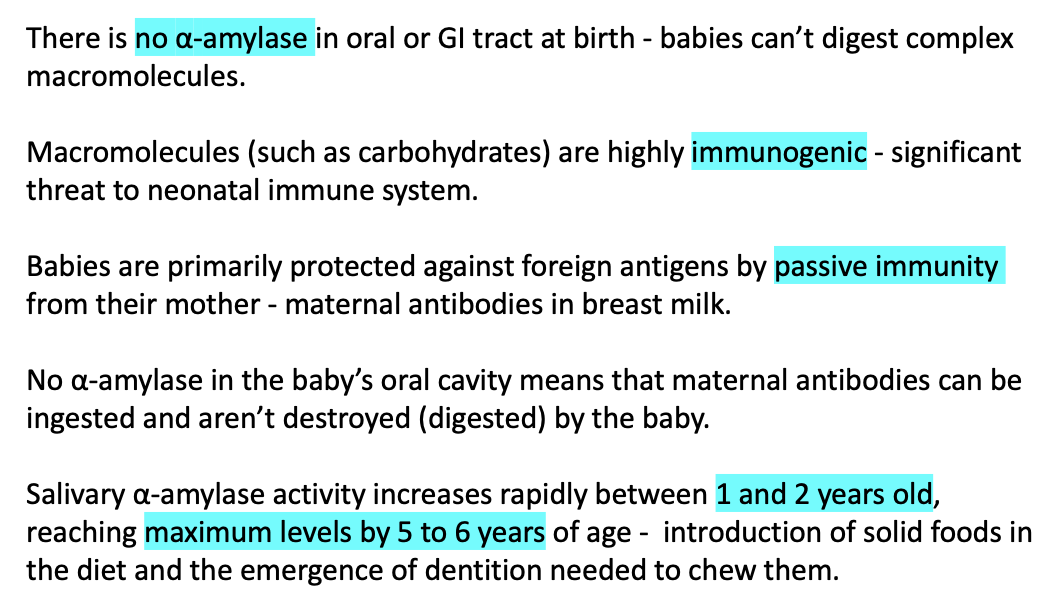
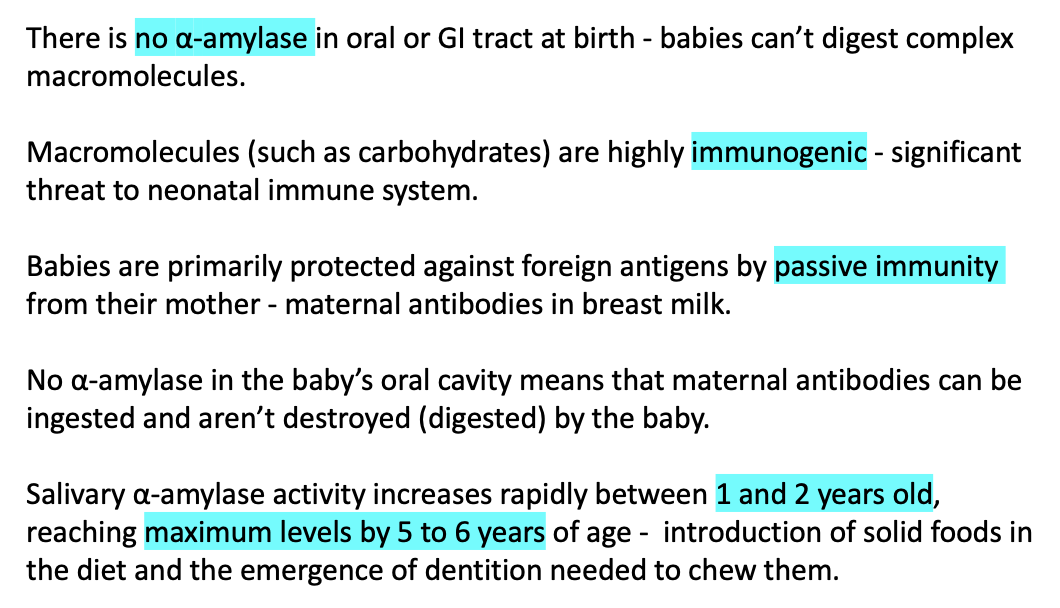
outline the function of alpha amylase
enzyme that degrades starches to amylose and amylopectin (polysaccharides)
causing release of a sweet taste
what is the structure of amylose
linear, unbranched chain of alpha glucose
coiled structure
D-glucose molecules in an alpha 1,4 linkage
what is the structure of amylopectin
long chain
branched chain with alpha 1,6 linkages
what are dextrins
short chains of glucose units resulting from starch breakdown
what stimulus increases the levels of salivary alpha amylase
stress - action of sympathetic nervous system
which salivary proteins are involved in enamel protection
statherin
proline rich proteins
cystatins
outline statherin
inhibits CaPO4 precipitation and crystal growth (component of pellicle)
helps maintain Ca2+ supersaturation
outline proline rich proteins
glycosylated form - lubrication
acidic form - inhibits CaPO4 precipitation
mediates bacterial adhesion
binds to tannins
outline cystatins
cysteine rich proteins
inhibits CaPO4 precipitation
inhibits cysteine proteases
which salivary proteins help remineralisation and how do they do so
PRPs and statherin helps remineralisation
they keep enamel pores open so calcium and phosphate ions can diffuse into enamel
do PRPs and statherin prevent calculus formation
no
because they are not found in plaque so if degraded, does not prevent calculus formation
why is saliva an effective diagnostic tool
non-invasive
rapid
cost-effective
precise
simple
what conditions can saliva be used to test for
stress
Alzheimer’s
Parkinson’s
sleep disorders
TB
periodontal disease - based on IL-1 protein
concussion