Haemolymphatic Oncology 2: Feline Lymphoma Myeloma ; Leukaemia in Cats and Dogs
1/65
Earn XP
Description and Tags
Understand the common clinical presentations of cats with lymphoma, and differential diagnoses • Describe the diagnosis and staging of feline lymphoma • Understand and distinguish between treatment options for lymphoma • Understand the potential toxicities of treatment • Understand the clinical presentations of dogs and cats with leukaemia • Describe the diagnosis of leukaemia, and where treatment is possible
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
feline lymphoma:
prevalance in cat tumour? is it common?
age at presentation?
breed predispose? wb anatomical preference
any other environmental factor increasing risk?
25% of feline tumours
Age varies with anatomical site
No breed incidence
Cranial mediastinal in oriental breeds and feLV
environmental tobacco smoke exposure
what are the anatomical forms of feline lymphoma
alimentary
renal
CNS
nasal
mediastinal
extraodal
multicentric
Role of FeLV in feline lymphoma
exposure but recovered: 5x increased risk
persistent infection: 50-62x increased risk
FeLV and FIV positive: 80X increased risk
FIV positive: 5x increased risk
FeLV/FIV often associateed with cranial mediastinal tumour
FeLV infection reduced in UK
shift to older cats
increased alimentary, reduced cranial mediastinal
Feline Lymphoma anatomic location: Multicentric
is multicentric common in cats? are the lymphadenopathy symmetrical or not?
age?
in what situation would thei mass self resolve? what breed predispose?
multicentric lymphoma + ymmetrical generalised lymphadenopathy rare in cats
Regional lymphadenopathy more common
any age
generalised lymphadenopathies mimicing lymphoma
Young cats, non-neoplastic origin, generally self-resolve
BSH in New Zealand
clinical signs of multicentric feline lymphoma
name 1 identical to dog
name 5 that is cat specific. give them a group name
Non-painful lymph node enlargement
can be systemicallly unwell
Hyporexia • Depression • Non-specific malaise • Pyrexia • (PU/PD)
genereal lymphanopathy is an important clinical sign. name ddx other than lymphoma (5)
Retroviral, viral, bacterial, fungal, mycobacterial and (protozoal), infections
Other haemopoietic malignancies
Immune-mediated disease
Idiopathic lympahdenopathy
Metastatic disease (also for locoregional LN enlargement)
feline mass at Submandibular or Cervical: it could be lymphoma. what are the
clinical presentations?
give neoplasia ddx
what other structure can be involved
can be solitary or miltiple submandibular/ cervical swelling
Lymphoma: High grade or Hodgkin’s like disease (more indolent)
metastatic disease
salivary gland, thyroid, vocal cord etc.
Submandibular or Cervical mass: other ddx
Abscesses
Reactive nodes
Mycobacterial infection
Salivary gland, thyroid and other masses
Feline Lymphoma: Cranial Mediastinal
young/ old common?
breed predisposition
clinical presentation 5
what may you notice at a physical exam? 2
what other structures are at the site
Younger cats, oriental breed
Respiratory distress
Regurgitation/ dysphagia (due to mass compression)
Weight loss
Lethargy, exercise intolerance
Cough (rare)
physcial exam
Palpable reduction in compressibility of chest
Displaced apex beat— caudally
thymus!
non- neoplastic, Cranial Mediastinum mass in a cat.
list common differentiatls 3
list Other causes of pleural effusion 3/4
Thymoma (main ddx in older cats)
Other cranial mediastinal lymphadenopathy (see above)
Other causes of pleural effusion
Congestive cardiac failure
Pyothorax
FIP
trauma induces Haemothorax
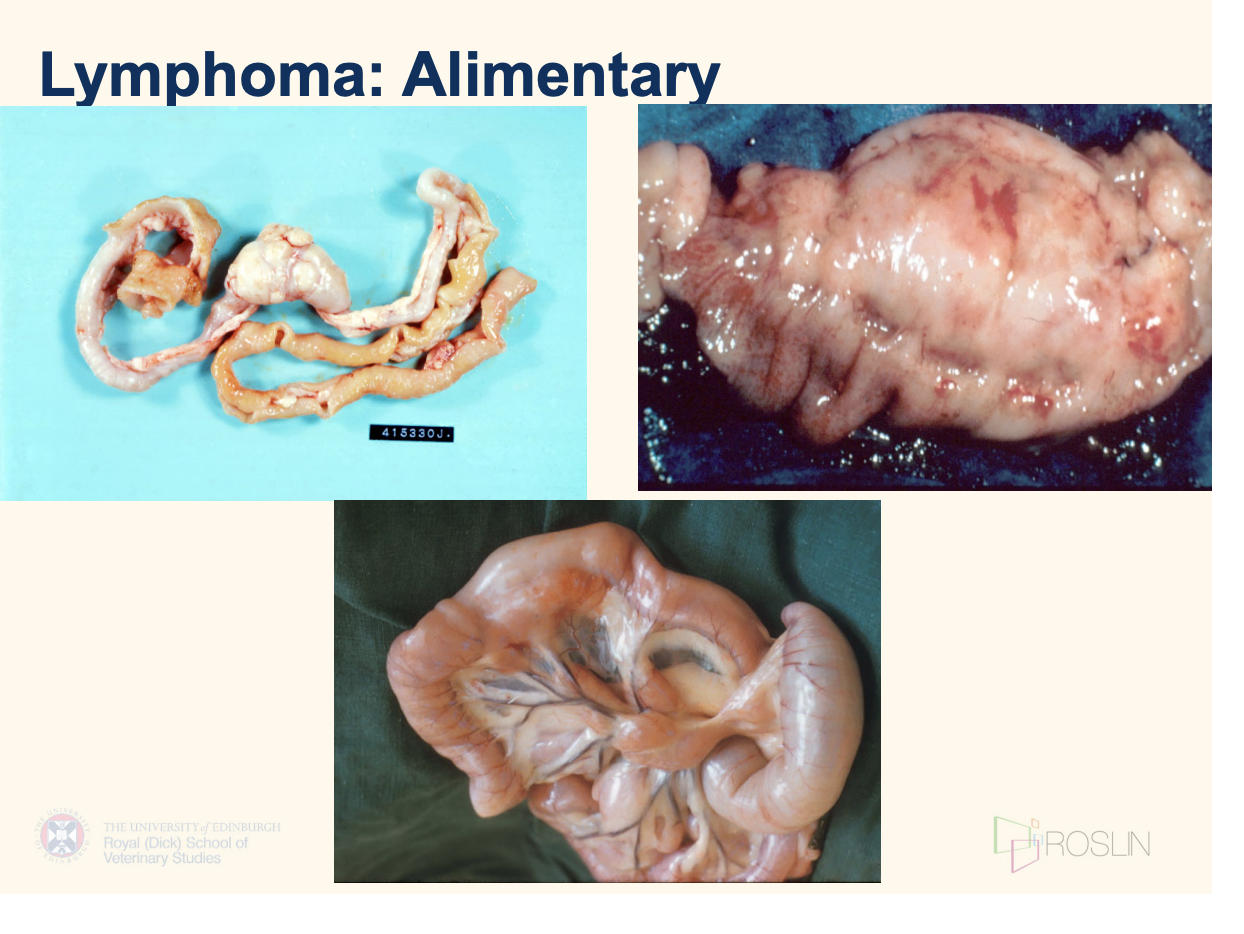
Feline lymphoma anatomical location: alimentary canal
what form of lymphoma can they be?
age— more common in?
clinical presentation— they can be different depending on ______
clinical signs are non specific. name
can be Low-grade or high-grade (multiorgan involvement)
Older cats
presentation depends on whether infiltration is diffuse/ mass-like
Hypo/anorexia – more common and severe in cats than dogs
—> Insidious weight loss
Diarrhoea
Malabsorption/PLE
Occasionally vomiting (cat>dog)
mass gastric / SI involvement—> secondary gastritis
picture:
what are other alimentary ddx other than lymphome?
note that alimentary/GI signs are various and very nonspecific
name 1 specific disaese that could cause GI sign
what are other causes of mesenteric lymphadenopathy (5)
name 3 other types of intestinal mass
other causes of GI signs
IBD
All other causes of mesenteric lymphadenopathy
FIP
Peritonitis of other aetiologies
IBD
Metastatic neoplasia
Pancreatitis
Mycobacterial infection
Other intestinal masses
(carcinoma, leiomyoma, leiomyosarcoma)
what is common is cats with alimentary lymphoma?
low B12; hypocobalaminaemia
Feline lymphoma anatomical location: Extranodal
give the most common extranodal sites (3)
what are their respective clinical presenation?
CNS, Nasal/ retrobulbar, renal
CNS : signs depend on site
Nasal/ retrobulbar
nasal discharge. epistaxis, obstruction
exophthalmos— beyond nasal cavity common
Renal (cat> dog)
malaise, anorexia
organomegaly (bilateral)
azotaemia (often severe @ time of dx)
Other findings: feline lymphoma
consider common paraneoplastic syndrome? 3 what about in cats? 1
compared to lymphoma, hypercalcaemia is more common in1
what else is often needed in cat lymphoma, especially alimentary locations?
Paraneoplastic syndromes is rare in cats
Hypercalcaemia (more likely in myeloma)
Hypergammaglobulinaemia
Immune mediated disease
cobalamin supplpiment (B12) as hypocobalanimaemia common
list diagnosis approaches in feline lymphome
FNA cytology, biopsy, clin path
imaging?
using FNA cytology for feline lymphoma diagnosis
often use with ____ and ____
what is a challange in cytology in cats? is what area is lymphoma hard to diagnose
then where is it easier to dx on FNA? what needs concurrent biopsy?
what is often high grade?
can you use LN FNA in that location?
often have to use with histopath and cytology
multicentric/peripheral: often low-grade small cell or mixed lymphomas
Difficult to differentiate from reactive hyperplasia , less diagnostic
Cranial mediastinal and extranodal—> higher grade
Easier to diagnose on FNA
Renal often require biopsy
GI often high-grade (can be low)
LN FNA in GI rarely diagnostic
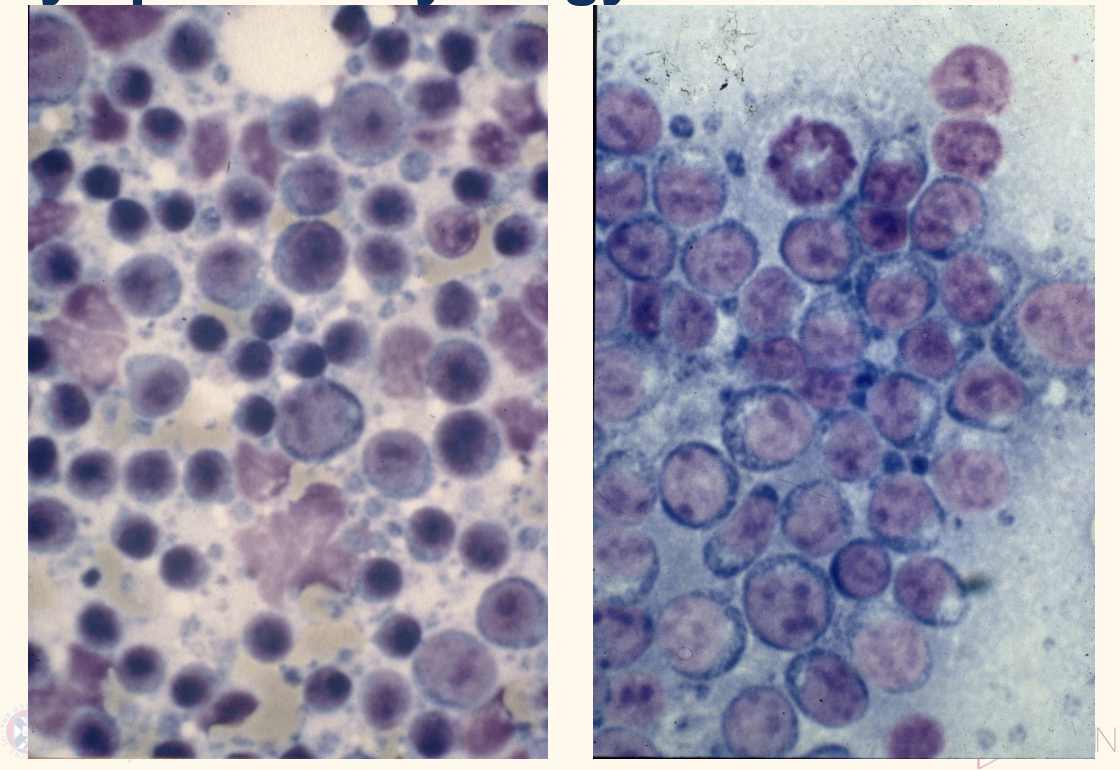
using cytology to diagnose feline lymphoma
describe what you would see in cytology, high grade lymphoma 4
lymphoma on R,
high-grade lymphoma
monomorphic population of large lymphoblasts (>50%).
nuclei with clumped chromatin, multiple, pleomorphic
basophillic cytoplasm than normal small lymphocyte
Mitotic figure
using biopsy to diagnose feline lymphoma
how and where would u do LN biopsy (1)
avoid what node 1
caution in tools 1
describe extranodal lesion/ big node leision biopsy
what if you also suspect mycobacterial or fungal?
Excisional biopsy of node 23g needle: popliteal good
submandibular as often recctive for dental issue
avoid trucut except renal
Wedge biopsy from extranodal lesion or enormous node
Impression smears
keep fres tissue if suspecct mycobacterial disease (or fungal)
if granulomatous indication—>PCR
why can cat lymphoma diagnosis be tricky?
secific it to:
low grade GI lymphoma 3
CNS lymphoma 3
what else can you do
Low-grade alimentary vs IBD
PARR (specific not sensitive)
Negative unhelpful
CNS lymphoma
PARR done on CSF + epidural
Often no/few tumour cells in CSF
Rarely solitary: may find other sites on staging
Bone marrow aspirate? rare
when do you clinical pathologgy in feline lymphoma cases?
effectiveness of haem?
how could haem suggest lymphoma
how does biochem reflect lymphoma
name 4 things to look out for
what else do you look out or in dogs with GI involvement
Haematology / biochemistry required before chemotherapy
Haematology non-specific in most cases
10-15% have abnormal cells in circulation
These suggest lymphoma
Neutrophilia, thrombocytopenia, lymphopenia, eosinopenia
Mild non-regen anaemia
Abnormal lymphoid cells
Biochemistry may reflect organ involvement
Hypoalbuminaemia (poor prognosis if multicentric)
Azotaemia— renal
Hepatic involvement
paraneoplastic syndrome
Measure cobalamin (B12)
feline lymphoma and Bm involvement
use in routine staging?
name BM asipiration site
Unknown how many cats have BM involvement; Haematology poor indicator.
Rarely used in routine staging but may be useful in CNS disease
occasional +ve for FeLV cat
proximal femur. humurus
Feline Lymphoma: FeLV Testing
importance
what does it test? what do you do if come back +ve?
FeLV +ve→ poorer response to chemo and prognosis
Detects viral core protein p27
Single positive should be confirmed
Care with “in house” tests
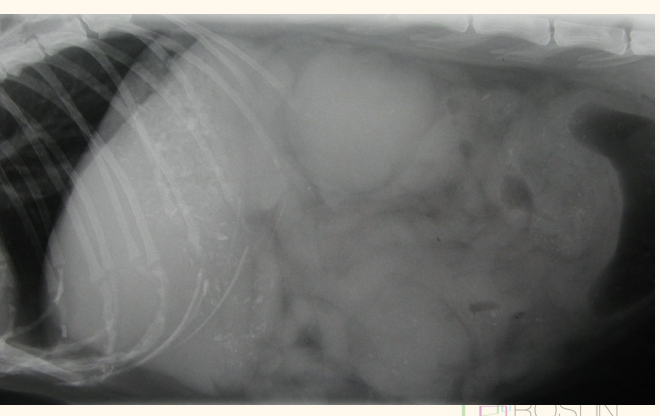
diasg img for feline lymphoma used fro staging
cxr, axr, us
Diagnostic Imaging: CXR in feline lymphoma
list structures and their features of LN 4
wb pulmonary whatd u see 1
what else do u look for 2
CXR also used used for? 2
Lymph node enlargement
cranial mediastinal
suprasternal
tracheobronchial nodes
thymus
Pulmonary infiltration
Little data on the appearance of round cell tumour infiltrates in cats
Pleural effusion + Concurrent disease
MONITORING REMISSION and Staging
Diagnostic Imaging: AXR in cat lymphoma
if the owner cannot afford abdo us what do u do
what would you look for, consistent with lymphoma 4
name the abdo lyph nodes
lots can be palpated
Internal lymph node enlargement
sublumbar lymphadenopathy
mesenteric lymphadenopathy
Hepato/splenomegaly
Peritoneal effusion
Concurrent disease
Diagnostic Imaging: Ultrasound in cat lymphoma
US can be used to look for
apprearance?
name 2 other thing US is used for in lymphoma
cranial mediastinal and abdominal masses
Appearance can be variable
also used for
renal/ cranial mediatinal FNAs/tru-cut biopsies guide
Monitoring of remission
Clinical Staging, Grading, Typing of feline lymphoma
how to stage cats?
2e?
Cats dont fit in the standard clinical staging boxes
anatomical location: none useful
histopathological: none establish
immunophenotype none prognostic
feline Lymphoma: Prognostic Indicators +ve 2
Achieving CR
small volume, extranodal disease
feline Lymphoma: Prognostic Indicators -ve
name 2
name effect FeLV status have on remission
Failure to achieve CR
previous corticosteoird therpay
FeLV +ve status
chance of remission, duration
Treatment of Lymphoma
name 4
one that we dont use
what else is important
None
Corticosteroids
COP regimes
Doxorubicin-containing regimes – CHOP
Non-continuous regimes – Poorly evaluated for cats
(B12/cobalamin supplementation)
MST without therapy: feline lymphoma
4 wk
COP: feline lymphoma
excellent protocol for cats
High dose COP —75% CR
1 year survival 49%, 2 year survival 40%
doxorubicin containig CHOP: Feline lymphoma
3
doxorubicin is controversial
single agent poor response
MST disappointing — 5-6 months
outcome
goal? 3
what would probably happen
what do you do then?
Goal is to induce complete remission
no detectable tumour
good QOL
Most cats develop drug resistance and relapse
Rescue therapy: small % cured
describe high dose cop
10 week protocol
pred per
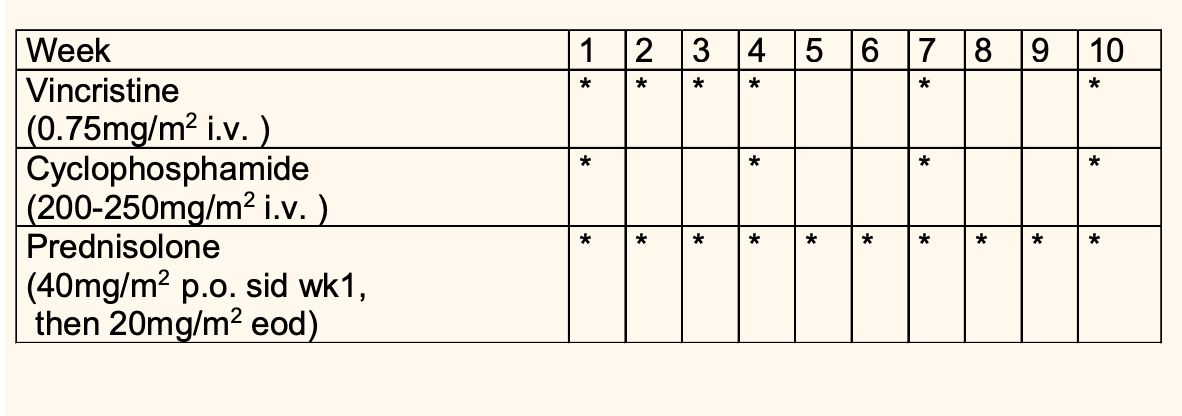
cat specific consideration for COP
name alteranative to cyclophosphamis
Vincristine ? Mild transient inappetance
Cyclophosphamide GI effects tend to be hyporexia ?altered taste/subclinical stomatis, alopecia: whisker loss and coat changes, (Sterile haemorrhagic cystitis rare in cat)
Prednisolone Hyperadenocorticism Coat changes Malassezia, seborrhoea (smelly feet!)
Alternatives to Cyclophosphamide
Chlorambucil (only if in remission) 20mg/m 2 q21days in high dose COP 5-6mg/m 2 every other day (equivalent) or 2mg every other day or 20mg/m2 q 14-21 days for low grade alimentary
Melphalan 20mg/m 2 q21 days Care re cumulative myelosuppression
use of doxi/epirubicin in cat
CHOP still used in some centre. reword
Poor response to dox as single agent
Fewer than 30% CR– Poor response as rescue agent
CHOP – Reasonable remission and survival times in some multidrug studies – Small numbers, only CRs achieved survival comparable to COP
Patient Monitoring
Remission – Check achieves and maintains remission – Often requires imaging $
Toxicity
Myelosuppressive agents • check haem prior to every bolus dose • on low dose chlorambucil, check at appropriate intervals
intermittently check urine —> for UTI—> pyrlonephritits, kidney problem
Treatment: Solitary Lymphomas feline
Surgical excision – e.g. intestinal mass • Radiotherapy – e.g. nasal lymphoma • Very few lymphomas are solitary – esp true of cats – e.g. 75% of cats presenting with CNS lymphoma have lymphoma in other sites • Adjunctive chemo or chemo as sole therapy
cat Alimentary Lymphoma: tx
Surgical excision of solitary mass lesion – Must biopsy nodes • ? Follow up chemotherapy • Extensive infiltration – Staggered induction to reduce risk of perforation • Adequate supportive therapy (b12, food, appetitie stimulent, antiemetic
• Gastric lymphoma very difficult to treat • Low grade may respond very well to chlorambucil and prednisolone only (mostly hihg grade)
feline Renal Lymphoma- azotemia as prog fator?
response rate?
involcement?
Degree of azotaemia is not prognostic • Overall low response rate and poor survival time • High incidence of CNS involvement in cats with renal lymphoma – few agents cross the blood brain barrier – add cytosine arabinoside in induction ? • Possible association with nasal/retrobulbar lymphoma
feline Cutaneous Lymphoma tx
Generally non-epitheliotrophic in cats • Generally not very responsive to chemotherapy – Possible role for lomustine • ?Role of retinoids – in amelioration of clinical signs • (? Other agents e.g. interferon) • Possible indolent form affecting head and neck • NB subcutaneous leisionusually aggressive
felien lymphoma rescue therapy
Second remissions are generally shorter than first – Cats more difficult to rescue than dogs – Low response rates, median progression free intervals 14-166 days • Usually alter regime completely – Anthracycline (doxorubicin/epirubicin) • 22% response rate, less than 10% CR – Lomustine • PFI 180d for gastrointestinal, 26 days for other – Lomustine, methotrexate, cytosine (LMC) • 46% response rate – MOPP (mechlorethamine, vincristine, prednisolone, procarbazine) and variants • 10/23 CR (mainly alimentary)
solitary mediatinal : radiation 9(CNS?)
Multiple Myeloma/Myeloma Related Disorder
how to dx
Functional B cell (plasma cell) tumour : Variable presentation
Hypergammaglobulinaemia • Hyperviscosity signs – ocular, neuro, GI, PU/PD, malaise – Hypercalcaemia • GI, PU/PD, malaise – Bone lesions
Lameness • Mild -cytopenias
dx wtih BM aspiration and SPE to confirm
MRD diagnosis: mathopneumpnic
BM aspirate: plasma cell
PCR
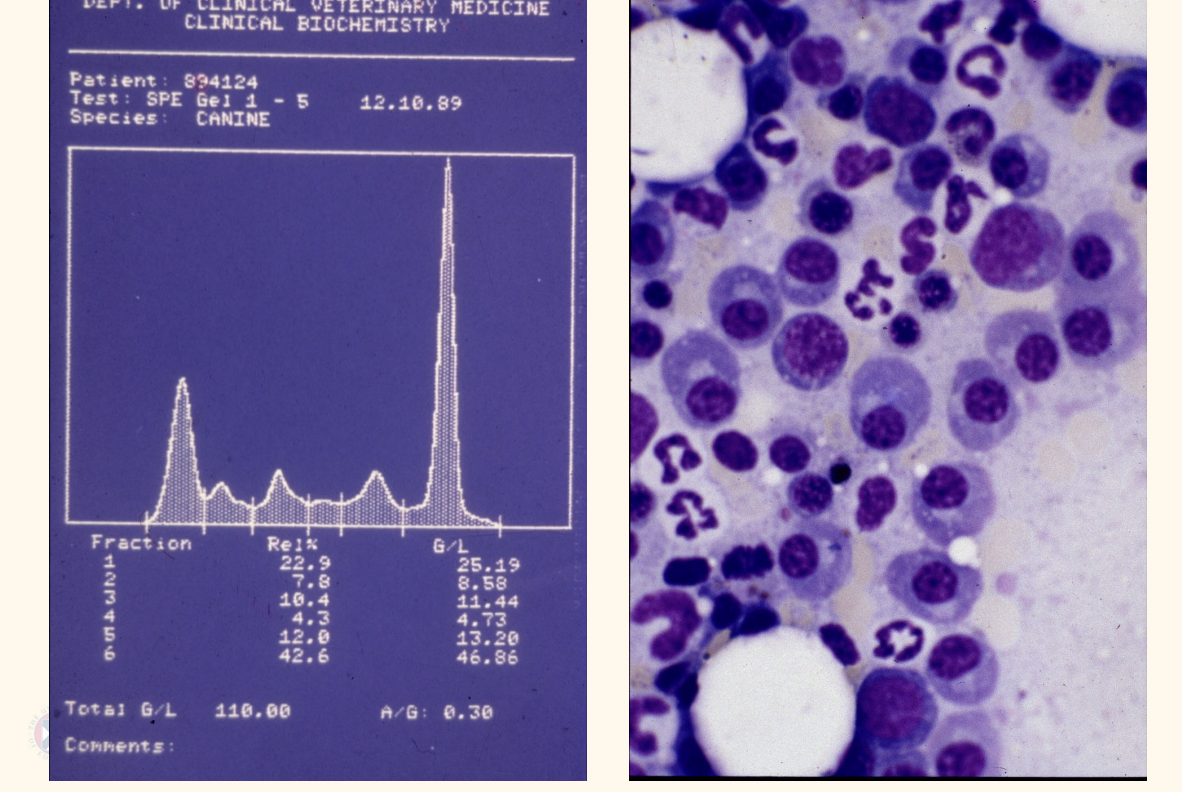
MRD tx
h melphalan and prednisolone • Median survival times are 12m or more • Add other agents if response is poor or at relapse • Negative prognostic indicators – Proteinuria – Hypercalcaemia/azotaemia (common) – Extensive bone lesions
Leukaemia occurs when vs
lymphoma occurs when
leukemia: neoplastic transformation occurs in the BONE MARROW
lymphoma: neoplastic transformation occurs in the peripheral lymphoid tissue
– Cells in acute lymphoblastic leukaemia and high grade lymphoma look similar • Leukaemia is CD34+ve because arises from stem cells • Lymphoma is CD34-ve because arises from lymphoid cells
fudamentally difference diseaes
lymphoid/ Lymphoid or myeloid – Depends on cell of origin • More precise determination of lineage will help identify treatment – Presentation is essentially the same • Acute or chronic – Reflects clinical presentation – Correlates with stage at which neoplastic transformation has occurred
acute leukemia
Transformation of stem cell results in failure to differentiate – Stem cells/committed blasts (usually CD34+ve) • Rapid proliferation • Arrested/defective maturation • Marrow rapidly becomes overcrowded – Normal cell production fails – -cytopenias • Clinical signs are severe, course is rapid
Chronic Leukaemia
Transformation occurs in the stem cell but differentiation is not blocked – Cells may look morphologically mature and normal – May function abnormally • Proliferation not controlled but slower than acute • Effects on normal haemopoiesis less devastating • Clinical signs less severe • Course insidious
What causes clinical signs in leukemia px
DISRUPTION OF NORMAL HAEMOPOIESIS – Effects of -cytopenias
Hyperviscosity if there are vastly elevated circulating cell numbers
Paraneoplastic syndromes — clincial sign, infiltration of liver, spleen and other organ
Organ infiltration resulting in functional compromise
presentation of Acute Leukaemia
History of malaise, hyporexia, PU/PD
Clinical signs – Lethargy – Pyrexia – Hepatosplenomegaly – Mild lymphadenopathy – Pallor – Sepsis – Haemorrhage – Hyperviscosity
leukemia: neutropenia as indication of disruption of normla haemapoiesis
e first manifestation of failure of haemopoiesis – Use storage pool to replenish circulating pool • Runs out after about 5 days
Reduced host defence against pathogens
Malaise • Pyrexia • Sepsis, septic shock – Often from Gram -ve organisms in the GIT • Septic shock • Reduced inflammatory response – Difficulty identifying foci of infection
thrombocypopoaeamiaas indication of disruption of normla haemapoiesis
Thrombocytopenia with or before neutropenia – Impairment of primary coagulation • Petechial and ecchymotic haemorrhages • Bleeding from mucous membranes – Epistaxis – Melaena • Ooze from small wounds • (Significant or ongoing haemorrhage may contribute to anaemia) • (?immune mediated destruction)
Anaemia generally mild – Normocytic, normochromic – Non-regenerative • (?
Secondary immune mediated haemolytic anaemia) – ? Esp lymphoid leukaemias
Cats with AL often have moderate or severe anaemias – Marrow infiltration – Immune mediated destruction – FeLV infection blocking erythropoiesis – Secondary myelofibrosis
Leukocytosis big nastl blacst
In most cases abnormal cells are released into the circulation • May not be an absolute increase in white cell count in all cases • Leukaemia without circulating blasts – Aleukaemic leukaemia – More common in cats • Very large numbers of cells can lead to hyperviscosity – Capillary sludging – Poor perfusion of end vessels • CNS signs • Ocular signs • Renal compromise
Biochemical Abnormalities in leukaemia
Azotaemia • Monoclonal gammopathy • Hypoproteinaemia • Hypercalcaemia • Raised liver enzymes • (Hyperkalaemia) • (Hypoglycaemia)
— check Blood smear and haem
Acute leukaemias: diagnosis
Circulating abnormal cells – Usually in high numbers • Pancytopenia • Difficult to determine morphologically if atypical blasts are lymphoid or myeloid – Flow cytometry – Also useful to differentiate stage V lymphoma from ALL: CD34 specific
Acute leukaemias: treatment
Prognosis poor – Requirement for supportive care – Dose intensity required • ALL – CHOP based protocols – Median survival times 16-120 days •acute myeloid leukemia – Many protocols – Doxorubicin/cytarabine – MST 15-60 days
Chronic Leukaemia: presentation
Chronic myeloid leukaemias rare – Differentiate from other causes of extreme neutrophilia • Mostly chronic lymphocytic leukaemia – CLL • Older dogs
Mild clinical signs – Insidious onset – Lethargy – Mild splenomegaly – Mild lymphadenopathy – Anaemia
May be incidental finding
Chronic Leukaemia: CLL
Not all need treated
Respond well to chlorambucil and prednisolone – 70% have normalisation of count •
Median survival times 1 to 3 years – T CLL better than B CLL
No blast crises in dogs but B CLL patients may develop a high grade lymphoma – Richter’s syndrome— resistant to ???
Polycythaemia/Primary Erythrocytosis
Rare – uncontrolled erythroid proliferation – hyperviscosity
Differentiate Polycythaemia/Primary Erythrocytosis from other causes of erythrocytosis
Relative • hypovolaemia – Secondary to hypoxia • respiratory disease, cardiac disease with left to right shunts – Inappropriate EPO production • renal disease (esp neoplasia), other tumours
Polycythaemia/Primary Erythrocytosis tx
Treat with hydroxyurea/hydroxycarbamate – antimetabolite • Phlebotomy in emergency