BMSC 208 - Post Midterm
5.0(2)
5.0(2)
Card Sorting
1/214
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
215 Terms
1
New cards
Describe the sequence of organs within the digestive system from mouth to anus
\- Mouth, esophagus, stomach, small intestine, large intestine, rectum, anus
2
New cards
What are the four layers of the GI tract wall?
\- Mucosa
\- Submucosa
\- Muscularis external
\- Serosa
\- Submucosa
\- Muscularis external
\- Serosa
3
New cards
What are the 3 major parts to the mucosa? How is the mucosa different in the stomach compared to the small intestine?
\- Epithelium
\- Lamina propria
\- Muscularis mucosae
\- Stomach: Rugae – gastric folds to increase surface area
\- Small intestine: Plicae – increases SA
\- Lamina propria
\- Muscularis mucosae
\- Stomach: Rugae – gastric folds to increase surface area
\- Small intestine: Plicae – increases SA
4
New cards
In the mucosa what is the function of the epithelium? What are the junctions of the epithelium like in the stomach and small intestine? What is the life span?
\- Function: transporting epithelial cells
\- Stomach/colon: junctions tight
\- Small intestine: leaky junctions
\- Lifespan: short, constantly reproduced 17 billion daily
\- Stomach/colon: junctions tight
\- Small intestine: leaky junctions
\- Lifespan: short, constantly reproduced 17 billion daily
5
New cards
What is the lamina propria?
\- 2nd layer of mucosa
\- Nerves, blood vessels, lymph vessels
\- Nerves, blood vessels, lymph vessels
6
New cards
What is the muscularis mucosae?
\- 3rd layer of mucosa
\- Alters surface area available for absorption
\- Alters surface area available for absorption
7
New cards
What is the Submucosa?
\- 2nd layer of GI tract
\- Contains large vessels
\- Submucosal plexus – major nerve networks in enteric nervous system
\- Contains large vessels
\- Submucosal plexus – major nerve networks in enteric nervous system
8
New cards
What is the muscularis externa?
\- 3rd layer of GI tract
\- Smooth muscle that can decrease diameter or length of tube
\- Myenteric plexus
\- Smooth muscle that can decrease diameter or length of tube
\- Myenteric plexus
9
New cards
What is the serosa?
\- 4th layer of GI tract
\- Outer covering of connective tissue
\- Outer covering of connective tissue
10
New cards
What is the primary function of the digestive system?
\- Move nutrients, water, and electrolytes from external environment into internal environment
11
New cards
What are the two challenges the body faces during digestion?
\- Avoiding autodigestion: breaking down food small enough without digesting cells of GI tract
\- Defense: absorbing water and nutrients without absorbing bacteria, viruses, pathogens
\- Defense: absorbing water and nutrients without absorbing bacteria, viruses, pathogens
12
New cards
What are the four digestive processes?
* Digestion: chemical and mechanical breakdown of food into absorbable units
* Secretion: movement of material from cells into lumen or ECF
* Absorption: movement of material from GI lumen to ECF
* Motility: movement of material through GI tract as a result of muscle contraction
* Secretion: movement of material from cells into lumen or ECF
* Absorption: movement of material from GI lumen to ECF
* Motility: movement of material through GI tract as a result of muscle contraction
13
New cards
What are the 3 different types of motility?
\- Migrating motor complex (motilin)
\- Peristaltic contractions
\- Segmental contractions
\- Peristaltic contractions
\- Segmental contractions
14
New cards
What is the migrating more complex?
\- Happens between meals
\- Contraction that begin in stomach and end in large intestine
\- Cleansing - Sweeps food remnant and bacteria out of upper GI tract into large intestine
\- Contraction that begin in stomach and end in large intestine
\- Cleansing - Sweeps food remnant and bacteria out of upper GI tract into large intestine
15
New cards
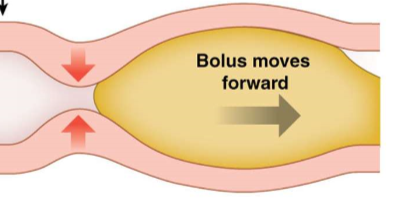
What are peristaltic contractions?
\- Progressive wave on contraction of circular muscle behind food
\- Produce forward movement
\- Produce forward movement
16
New cards
What are segmental contractions?
\- Small segments alternatively contract and relax circular and longitudinal
\- Little or no net forward movement
\- Responsible for mixing
\- Little or no net forward movement
\- Responsible for mixing
17
New cards
The ENS is made up of?
\- Submucosal and myenteric plexuses
18
New cards
What are similarities of ENS to CNS?
1. Intrinsic Neurons:
1. GI Nerve plexuses lie completely in wall
2. Interneurons completely in CNS
2. Transmitters/modulators
1. Many ENS identical to CNS
3. Support cells
1. ENS: Glial cells
2. CNS: astrocytes
4. barriers
1. ENS: Capillary diffusion barrier around ganglia
2. CNS: Blood brain barrier
5. Own Integrating Center
1. Both function autonomously
19
New cards
What are short reflexes? Examples
\- Reflexes that originate and integrated in ENS without outside input
\- Local stimuli – distention and presence of food
\- Submucosal plexus – secretion from GI cells
\- Muscularis externa (myenteric plexus) - motility
\- Local stimuli – distention and presence of food
\- Submucosal plexus – secretion from GI cells
\- Muscularis externa (myenteric plexus) - motility
20
New cards
What are long reflexes?
\- Reflex Integrated in CNS (origin can be in/out of ENS)
\- Outside ENS (cephalic reflex): feedforward and emotional reflexes
* Feedforward: outside ENS stimuli sight/smell of food sends info to ENS to prepare digestive system by salivation, stomach growls
* Emotional: emotions (CNS) send signal to ENS ex. Traveler’s constipation, butterflies
\- Outside ENS (cephalic reflex): feedforward and emotional reflexes
* Feedforward: outside ENS stimuli sight/smell of food sends info to ENS to prepare digestive system by salivation, stomach growls
* Emotional: emotions (CNS) send signal to ENS ex. Traveler’s constipation, butterflies
21
New cards
Can both longs and short reflexes secrete GI peptides? What do they act as?
\- Yes
\- Hormones or paracrine signals
\- Hormones or paracrine signals
22
New cards
GI peptides either excite or inhibit ____ and _____
\- Motility
\- Secretion
\- Secretion
23
New cards
Where can GI peptides be secreted in GI tract?
\- Lumen for apical membrane receptors
\- ECF to act on neighbouring cells
\- ECF to act on neighbouring cells
24
New cards
What is the integrated function within the digestive system?
\- Cephalic/oral : occurring before food enters stomach
\- Gastric: digestive processes in stomach
\- Intestinal: digestive processes in intestines
\- Gastric: digestive processes in stomach
\- Intestinal: digestive processes in intestines
25
New cards
Explain the cephalic phase of digestion including the processes and reflexes involved.
\- Digestive processes occur before food enters mouth
\- Long reflex begin in brain (feed forward)
\- Increased parasympathetic output from medullas to salivary glands and ENS
\- Long reflex begin in brain (feed forward)
\- Increased parasympathetic output from medullas to salivary glands and ENS
26
New cards
What nervous system drives GI function? What inhibits?
\- Parasympathetic drives
\- Sympathetic inhibits
27
New cards
What are the four functions of saliva?
\- Soften and moisten food
\- CHO digestion (amylase)
\- Taste from dissolving food
\- Defense (lysozyme)
\- CHO digestion (amylase)
\- Taste from dissolving food
\- Defense (lysozyme)
28
New cards
What are the 3 salivary glands and explain why they are not identical in the solutions they produce.
\- Parotid: infront of ear, watery solution with amylase
\- Submandibular: under mandible, watery solution, amylase, some mucus
\- Sublingual: under tongue, mainly mucus
\- Submandibular: under mandible, watery solution, amylase, some mucus
\- Sublingual: under tongue, mainly mucus
29
New cards
Salivary glands are _____ glands, with secretory epithelium arranged in grapelike clusters of cells called ____
\- Exocrine
\- Acini
\- Acini
30
New cards
The release of saliva is primarily under _______ control
\- parasympathetic
31
New cards
What is deglutition?
\- Reflex that pushes a bolus of food or liquid into esophagus (swallowing)
32
New cards
What occurs in the process of deglutition?
\- Stimulus: pressure of tongue pushing bolus against soft palate and back of mouth
\- Activates: sensory neurons going to medulla
\- Reflex: soft palate elevates to close off nasopharynx, muscle contractions move larynx up and forward, epiglottis close trachea
\- Result: as food moves down, lower esophageal sphincter tension relaxes, food enters stomach
\- Activates: sensory neurons going to medulla
\- Reflex: soft palate elevates to close off nasopharynx, muscle contractions move larynx up and forward, epiglottis close trachea
\- Result: as food moves down, lower esophageal sphincter tension relaxes, food enters stomach
33
New cards
What are the three general functions of the stomach?
1\. Storage: store and regulate passage into small intestine
2\. Digestion: chemical and mechanical into chyme
3\. Defense: destroy bacteria/pathogens in food, pathogens trapped in airway brought to stomach via mucociliary escalator
2\. Digestion: chemical and mechanical into chyme
3\. Defense: destroy bacteria/pathogens in food, pathogens trapped in airway brought to stomach via mucociliary escalator
34
New cards
Explain the process of the gastric phase of digestion (storage and motility) upon swallowing food.
\- Receptive relaxation: parasympathetic neurons to ENS relax fundus. Distends to hold more volume and enhances motility
\- Propulsion: peristaltic waves move chyme from antrum to pylorus
\- Retropulsion: larger particles moved backwards (need to be small to squeeze through pylorus)
\- Propulsion: peristaltic waves move chyme from antrum to pylorus
\- Retropulsion: larger particles moved backwards (need to be small to squeeze through pylorus)
35
New cards
What is the function of gastric secretions?
\- Protect and digest
36
New cards
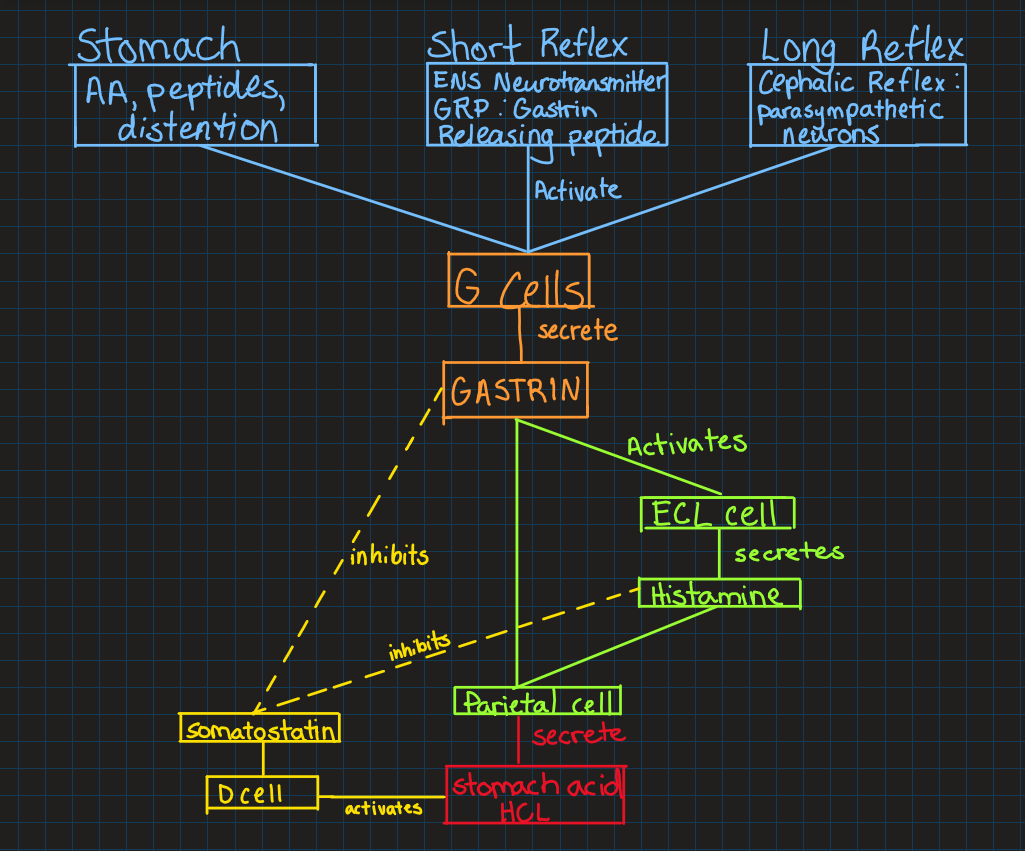
Explain the release of gastrin (hormone) including what cells release it, stimulus, and what gastrin stimulates.
Stimulus:
o Stomach: presence of amino acids, peptides, and distention
o Short reflexes: ENS neurotransmitter GRP gastrin-releasing peptide
o Long reflexes: cephalic – parasympathetic neurons stimulate G Cell
Receptors: G-cells, found deep in gastric glands, release gastrin into bloodstream
Stimulates:
o Directly: parietal cells to release acid
o Indirectly: histamine release from enterochromaffin like cells (ECL) to stimulate parietal cells
o Stomach: presence of amino acids, peptides, and distention
o Short reflexes: ENS neurotransmitter GRP gastrin-releasing peptide
o Long reflexes: cephalic – parasympathetic neurons stimulate G Cell
Receptors: G-cells, found deep in gastric glands, release gastrin into bloodstream
Stimulates:
o Directly: parietal cells to release acid
o Indirectly: histamine release from enterochromaffin like cells (ECL) to stimulate parietal cells
37
New cards
Functions of gastric acid
\- Enzyme activation: Stimulates pepsinogen release, converted to pepsin (active enzyme that digests protein)
\- Protein denaturation: easier for pepsin to digest
\- Defense: kills bacteria and microorganisms
\- Amylase inactivation: stops CHO digestion
\- Somatostatin release from D cells (can inhibit gastric secretion – decrease gastrin and histamine)
\- Protein denaturation: easier for pepsin to digest
\- Defense: kills bacteria and microorganisms
\- Amylase inactivation: stops CHO digestion
\- Somatostatin release from D cells (can inhibit gastric secretion – decrease gastrin and histamine)
38
New cards
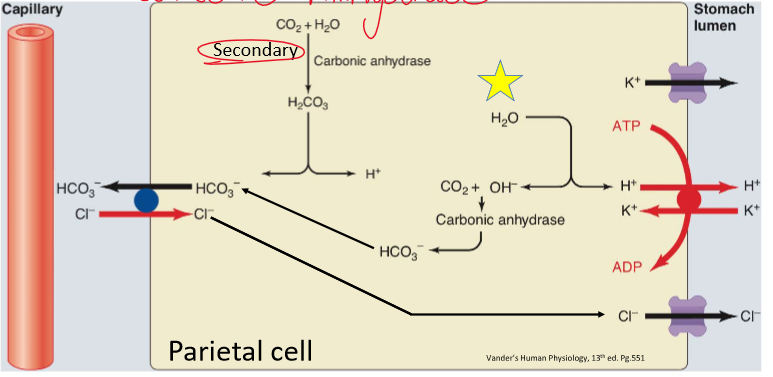
Explain the process of HCl stomach acid secretion
1\. **H+ from H20 within cell actively transported to lumen of stomach**
2\. Leftover OH in cell combines with CO2 via carbonic anhydrase -> HCO3
3\. HCO3 out to basolateral, Cl – in cell
4\. **Cl- diffuses to stomach following electrochemical gradient**
5\. Net result: secretion of HCL into stomach
2\. Leftover OH in cell combines with CO2 via carbonic anhydrase -> HCO3
3\. HCO3 out to basolateral, Cl – in cell
4\. **Cl- diffuses to stomach following electrochemical gradient**
5\. Net result: secretion of HCL into stomach
39
New cards
Describe/Draw the overall activation of gastrin release and stomach acid
40
New cards
What is the impact of acid secretion stimuli on apical transporters?
* transporters normally stored in vesicles
* stimuli cause exocytosis and insertion of apical transporters…allows for acid formation and secretion
* stimuli cause exocytosis and insertion of apical transporters…allows for acid formation and secretion
41
New cards
The stomach produces what two enzymes?
\- Pepsin
\- Gastric lipase
\- Gastric lipase
42
New cards
What is the stimulus for pepsin and gastric lipase secretion? How is pepsin and gastric lipase released?
\- Stimulant: acid secretion
\- Gastric lipase co-secreted with pepsin
\- Pepsinogen released from chief cells, H+ in stomach converts pepsinogen to pepsin
\- Gastric lipase co-secreted with pepsin
\- Pepsinogen released from chief cells, H+ in stomach converts pepsinogen to pepsin
43
New cards
What are the 3 paracrine secretions of the stomach? (hint: What gastrin acts on, and what those products stimulate)
\
\- ECL : Histamine
\- Parietal cell: intrinsic factor
\- D cell: somatostatin
\- ECL : Histamine
\- Parietal cell: intrinsic factor
\- D cell: somatostatin
44
New cards
What cells produce histamine? What is the function of histamine?
\- ECL enterochromaffin like cells
\- Activates H2 receptors on parietal cells to stimulate HCl secretion
\- Activates H2 receptors on parietal cells to stimulate HCl secretion
45
New cards
What cells produce intrinsic factor? What is the function of intrinsic factor?
\- Parietal cells
\- acid secretion and Vitamin absorption: forms a complex with B12
\- acid secretion and Vitamin absorption: forms a complex with B12
46
New cards
What cell produces somatostatin? What is the function of somatostatin?
\- D cells
\- Negative feedback loop for acid secretion
\- Acts on G cells (gastrin), parietal cells (gastrin), ECL cells (histamine)
\- Inhibits pepsinogen release
\- Negative feedback loop for acid secretion
\- Acts on G cells (gastrin), parietal cells (gastrin), ECL cells (histamine)
\- Inhibits pepsinogen release
47
New cards
Under normal conditions, the gastric mucosa protects itself from autodigestion by acid and enzymes with a _________?
\- Mucus-bicarbonate barrier
48
New cards
What cells produce the mucus-bicarbonate barrier? What are the stimulants?
\- Mucus cells in gastric glands secrete mucus and HCO3
\- Mucus forms a physical barrier, bicarbonate creates chemical buffer under mucus
\- Stimulants: parasympathetic input for both, irritation for mucus, H+ for HCO3
\- Mucus forms a physical barrier, bicarbonate creates chemical buffer under mucus
\- Stimulants: parasympathetic input for both, irritation for mucus, H+ for HCO3
49
New cards
What is a peptic ulcer?
\- Excessive acid production
\- Gastrin secreting tumors
\- H pylori bacteria major contributor
\- Gastrin secreting tumors
\- H pylori bacteria major contributor
50
New cards
Why must amount of chyme entering the small intestine be controlled?
\- Chyme undergone relatively little chemical digestions, so entry must be controlled to avoid overwhelming the small intestine
51
New cards
How is motility controlled in the small intestine?
\- Segmental and peristaltic contractions
\- Exposes nutrients for absorptions and controls speed to allow for digestion
\- Exposes nutrients for absorptions and controls speed to allow for digestion
52
New cards
What promotes motility in the small intestine?
\- Parasympathetic innervation, gastrin, cholecystokinin
\- Sympathetic innervation inhibits
\- Sympathetic innervation inhibits
53
New cards
What structure maximizes surface area in the small intestine?
\- Plicae (large folds)
\- Microvilli (seaweed) also secrete mucus
\- Microvilli (seaweed) also secrete mucus
54
New cards
What are crypts?
\- Invagination of lumen wall
\- Contain hormones and fluid secretory cells, stem cells
\- Contain hormones and fluid secretory cells, stem cells
55
New cards
Describe the hepatic portal system.
\- Venous blood from GI tract does not go directly to heart
\- Liver acts as a filter, so blood from GI tract taken goes to hepatic portal vein, then to liver for filtration, then to heart
\- Metabolizes drugs and xenobiotics
\- Liver acts as a filter, so blood from GI tract taken goes to hepatic portal vein, then to liver for filtration, then to heart
\- Metabolizes drugs and xenobiotics
56
New cards
The function of the large intestine is to?
\- Store and concentrate fecal matter
57
New cards
What is the gastroileal reflex?
\- Food leaving the stomach causes contraction of ileum and relaxation of ileocecal valve (between end of small intestine and beginning of large)
58
New cards
Chyme that enters the colon continues to be mixed by?
\- Segmental contractions
59
New cards
What are the secretions of the large intestine?
\- Minimal and primarily consist of mucus from goblet cells
60
New cards
What are the 3 types of motility in the large intestine?
1\. slow segmental contractions
2\. Haustral rolling or churning
3\. mass peristalsis
2\. Haustral rolling or churning
3\. mass peristalsis
61
New cards
What is haustral rolling or churning?
\- Thickened bands of longitudinal muscle layer taenia coli
\- Creates pouches called haustra
\- Creates pouches called haustra
62
New cards
What is mass peristalsis or mass movement?
\- Gastrocolic reflex
\- A wave of contraction decreases the diameter of a segment of colon and sends a substantial bolus of material forward
\- Associated with eating and distensions of the stomach
\- Responsible for sudden distension of rectum that triggers defecation
* making room for food
\- A wave of contraction decreases the diameter of a segment of colon and sends a substantial bolus of material forward
\- Associated with eating and distensions of the stomach
\- Responsible for sudden distension of rectum that triggers defecation
* making room for food
63
New cards
What are the endocrine secretions of the pancreas? From what cells? Examples? Stimuli?
\- Hormones
\- From islet cells
\- Ex. Insulin and glucagon
\- From islet cells
\- Ex. Insulin and glucagon
64
New cards
What are the exocrine secretions of the pancreas?
\- Digestive enzymes produced in acini (similar to salivary)
\- NaHCO3 watery solution sodium bicarbonate produced in duct cells
\- NaHCO3 watery solution sodium bicarbonate produced in duct cells
65
New cards
What are pancreatic enzymes secreted as? Are they active, if not what will activate them?
\- Secreted as zymogens that must be activates upon arrival in intestine
\- Brush border enteropeptidase converts trypsinogen to active trypsin
\- Trypsin convers other pancreatic zymogens
\- Brush border enteropeptidase converts trypsinogen to active trypsin
\- Trypsin convers other pancreatic zymogens
66
New cards
What is the purpose of the pancreas producing NaHCO3 and transferred to small intestine?
\- To neutralize acid entering from the stomach
67
New cards
Pancreas bicarbonate production requires high levels of enzyme _______
\- Carbonic anhydrase
68
New cards
Explain what happens to the pancreas with cystic fibrosis
\- Inherited mutation causes defective or absent CFTR channel protein
\- Secretion of Cl- and fluid stop, mucus continues = thick mucus
\- Mucus clog small pancreatic ducts and prevents digestive enzyme secretion into intestine
\- Secretion of Cl- and fluid stop, mucus continues = thick mucus
\- Mucus clog small pancreatic ducts and prevents digestive enzyme secretion into intestine
69
New cards
What does the liver secrete? From what cells?
\- Bile
\- Hepatocytes
\- Hepatocytes
70
New cards
What are the three main components of bile
\- Bile salts (bile/Acid/amino acid)
\- Bile pigments (bilirubin)
\- Cholesterol
\- Bile pigments (bilirubin)
\- Cholesterol
71
New cards
What is the function of bile?
\- Bile salts: detergents for fat digestion (emulsion of large fat droplets in chyme broken to smaller, stable particles by bile salts)
\- Drugs and xenobiotics excreted in bile
\- Drugs and xenobiotics excreted in bile
72
New cards
Most water is absorbed in the? Additional water absorbed in the?
\- Small intestine
\- Colon
\- Colon
73
New cards
How is water absorbed in the small intestine and colon? Pathway? What ion also uses this pathway/
\- Absorption of nutrients moves solute from lumen of intestine to ECF, creating an osmotic gradient that allows water to flow
\- Water and K+ move through the paracellular pathway
\- Water and K+ move through the paracellular pathway
74
New cards
How is NA and CL absorbed?
\- Both move across cells
\- Na+ enters cells by multiple pathways, Na+ KATPase pumps Na+ into ECF
\- Cl enters from Cl HCO exchanger and a basolateral CL channel to move across cells
\- Na+ enters cells by multiple pathways, Na+ KATPase pumps Na+ into ECF
\- Cl enters from Cl HCO exchanger and a basolateral CL channel to move across cells
75
New cards
Explain the digestion of fats
\- Bile salts from liver coat fat droplets
\- Pancreatic lipase and colipase break down fats into monoglycerides and fatty acids stored in micelles
\- Pancreatic lipase and colipase break down fats into monoglycerides and fatty acids stored in micelles
76
New cards
Explain absorption of fats.
\- Micelles contact brush border
\- Fatty acids an monoglycerides diffuse through enterocyte membrane
\- Cholesterol transported
\- TGs reformed in ER and pack with cholesterol in chylomicrons
\- Fatty acids an monoglycerides diffuse through enterocyte membrane
\- Cholesterol transported
\- TGs reformed in ER and pack with cholesterol in chylomicrons
77
New cards
What is enterohepatic circulation?
\- Not enough bile made for even 1 meal, so lots of bile recycling
\- Only 5% of bile silts excreted in feces, 95% recycled
78
New cards
What are gall stones?
\- Hardened deposits likely due to excess cholesterol or bilirubin
79
New cards
Explain carbohydrate digestion
\- Salivary and pancreatic amylase breaks down glucose polymers to disaccharides
\- Disaccharide broken down to monosaccharides by brush border enzymes known as disaccharidases
\- Disaccharide broken down to monosaccharides by brush border enzymes known as disaccharidases
80
New cards
Explain carbohydrate absorption for glucose and galactose, and fructose. What transporters are used for the monosaccharides to enter the mucosa, exit?
\- Glucose and Galactose: (CO TRANSPORT WITH NA)
o Apical Na+ glucose symporter SGLT
\- Fructose
o Apical GLUT5,
\- Exit with GLUT 2
o Apical Na+ glucose symporter SGLT
\- Fructose
o Apical GLUT5,
\- Exit with GLUT 2
81
New cards
What is the primary energy source for enterocytes (intestinal cells)?
\- Glutamine
\- Glucose-6-phosphate not formed and free glucose stays high
\- Glucose-6-phosphate not formed and free glucose stays high
82
New cards
Explain protein digestion. What are the two broad groups of enzymes for protein digestion?
\- Endopeptidases (proteases)
\- Exopeptidases
\- Exopeptidases
83
New cards
What is the function of endopeptidases?
\- Attack peptide bonds forming fragments
\- Released as zymogens (pepsin, trypsin, chemotrypsin)
\- Released as zymogens (pepsin, trypsin, chemotrypsin)
84
New cards
What is the function of exopeptidase? What are the two?
\- Release single amino acids from peptides one at a time
\- Aminopeptidases act on amino terminal end
\- Carboxypeptidases act on carboxy-terminal end
\- Aminopeptidases act on amino terminal end
\- Carboxypeptidases act on carboxy-terminal end
85
New cards
Explain Protein absorption for single AAs and Di/tri peptides
\- Single AA: NA cotransporters (apical) and Na exchangers (basolateral)
\- Di/tripeptides: oligopeptide transporter (H+ cotransporter)
\- Di/tripeptides: oligopeptide transporter (H+ cotransporter)
86
New cards
Most oligos digested to ______ in cell (peptidases) and exit via _____ exchanger
\- Single AAs
\- Na-AA exchanger
\- Na-AA exchanger
87
New cards
Some peptides larger than 3 amino acids are transported via?
\- Transcytosis
88
New cards
Small peptides could potential act as _____ stimulating antibody production causing an _____
\- Antigens
\- Allergic reaction
\- Allergic reaction
89
New cards
How are vitamins absorbed?
\- Fat soluble ADEK absorbed with fats
\- Water soluble CB mediated transport
\- B12 absorbed in ileum after forming a complex with intrinsic factor from parietal cells
\- Water soluble CB mediated transport
\- B12 absorbed in ileum after forming a complex with intrinsic factor from parietal cells
90
New cards
How are minerals absorbed?
\- Active transport
91
New cards
Chyme entering the intestine activates what nervous system?
\- Enteric
92
New cards
The effect of chyme entering the intestine and activating the enteric nervous system causes?
\- Decreased gastric motility
\- Decreased gastric secretion
\- Decreased gastric emptying
\- Increases intestinal motility and secretions
\- Decreased gastric secretion
\- Decreased gastric emptying
\- Increases intestinal motility and secretions
93
New cards
The intestinal phase is regulated by what 3 factors? Through what 3 signals/reflexes?
\- Distention
\- Acidity
\- Digestive products
\- Short reflex
\- Long reflex
\- Endocrine signaling
\- Acidity
\- Digestive products
\- Short reflex
\- Long reflex
\- Endocrine signaling
94
New cards
What 3 hormones reinforce the “decrease motility” signal in the stomach?
\- Secretin
\- Cholecystokinin (CCK)
\- Gastric inhibitory peptide (GIP)
\- Cholecystokinin (CCK)
\- Gastric inhibitory peptide (GIP)
95
New cards
Secretin – Released from what cell? When is it released? Primary role? Mechanisms? Outcomes?
\- S cell
\- Released by presence of acidic chyme entering small intestine
\- Primary role: acid regulation
o Stimulates bicarbonate secretion from pancreas duct cells
o Bile production in liver
o Inhibits acid secretion, Inhibits gastric motility, gastric emptying
\- Released by presence of acidic chyme entering small intestine
\- Primary role: acid regulation
o Stimulates bicarbonate secretion from pancreas duct cells
o Bile production in liver
o Inhibits acid secretion, Inhibits gastric motility, gastric emptying
96
New cards
CCK – secreted by what cells? When is it secreted? Primary functions? Outcomes?
\- I cell
\- Secreted into bloodstream if chyme contains fatty acids and amino acids
\- Increased pancreatic enzyme secretions from acini
\- Increased bile secretion from gallbladder
\- Inhibits gastric acid secretion, gastric motility, gastric emptying
\- Secreted into bloodstream if chyme contains fatty acids and amino acids
\- Increased pancreatic enzyme secretions from acini
\- Increased bile secretion from gallbladder
\- Inhibits gastric acid secretion, gastric motility, gastric emptying
97
New cards
GIP: gastric inhibitory peptide (glucose dependent insulinotropic peptide) and GLP 1 – glucagon like peptide – What cells release them? When is it released? Primary function? Outcomes?
\
\
\- K cells: GIP
\- L cells : GLP 1
\- Hormone released if meal contains CHO
\- Maintains glucose homeostasis - Feed forward to increase insulin release
\- Decrease acid secretion
\- Decrease gastric motility
\- L cells : GLP 1
\- Hormone released if meal contains CHO
\- Maintains glucose homeostasis - Feed forward to increase insulin release
\- Decrease acid secretion
\- Decrease gastric motility
98
New cards
Intestinal motility is influenced primarily by?
\- ENS neurons (myenteric plexus)
99
New cards
In the fed state, intestinal motility occurs from? In the fasting state, motility occurs from?
\- Fed: mostly segmental contraction, occasionally peristaltic contractions
\- Fasting: migrating motor complex (MMC)
\- Fasting: migrating motor complex (MMC)
100
New cards
What stimulates the migrating motor complex in the intestinal phase?
\- Motilin (hormone)
\- Secreted by Mo cells
\- Secreted by Mo cells