Dental Procedures & Techniques- Ch 28-27/TEST
1/75
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
Detection
the process of identifying the presence of something, such as teeth imperfection or decay in dentistry.
extraoral
outside the oral cavity
furcation
space or branching between two roots of a tooth
intraoral
located within the oral cavity
Mobility
the ability to move; in dentistry, it refers to the movement of teeth within its bone structure
morphologically, morphologic, morphology
branch of biology that deals with form and structure
palpation
to examine by touch, such as feeling for abnormalities within soft tissue
probing
to explore or examine within the use of an instrument
restoration
bringing something back to its natural or normal state, an example is the use of a dental material to restore a tooth
Why Patients Seek Dental Care
As a new patient to begin dental care
As an emergency patient when in pain or experiencing discomfort
For consultation with a specialist
As a returning patient for continued assessment and care
Dental Assistant Duties
Assist the patient with completion of patient information forms
Take and record vital signs
Chart and record the dentist’s findings during the extraoral and intraoral examinations
Expose intraoral and extraoral radiographs
Take preliminary impressions and fabricate diagnostic models
Take extraoral and intraoral photographs
Organize the patient record
Prepare for the case presentation
Visual Evaluation
The examination always begins with a visual evaluation of the patient’s extraoral and intraoral conditions
Enables the dentist to determine an overall assessment of the type of dental care received previously
Reveals any existing conditions that have not been treated
Specific examination areas include the following:
Face
Lips
Soft tissue within the mouth
Tongue
Tooth structure
Restorations
Missing teeth
Palpation
The examiner uses his or her fingers and hands to feel for:
Texture
Size
Consistency of the hard and soft tissue
This technique is especially useful for detecting extraoral swelling and is the primary way of detecting swollen lymph nodes
Instrumentation
The use of instruments to examine the teeth and surrounding tissues
Type of instruments commonly utilized to examine the teeth: Mouth mirror and explorer
Type of instrument used to examine the gingival tissues: Periodontal probe
Detection: Dentist uses an explorer to detect imperfections in tooth surfaces
Probing: Dentist or dental hygienist uses the periodontal probe to assess the gingiva for the presence of periodontal pockets

Digital Imaging
Caries lesions
Occlusion and TMJ analysis and diagnosis
Digital radiography: Intraoral and extraoral
Patient education
Shade matching
The computer-aided design/computer-aided manufacturing (CAD/CAM) system and intraoral imaging
Digital Photography
A diagnostic tool used for intraoral and extraoral structures
It provides the dentist and patient with a visual means of identifying and understanding specific problems
Recording the Dental Examination
Charting symbols, abbreviations, and color coding can be used in the recording process to indicate various conditions and existing restorations
Specific criteria that must be known before charting include the following:
Black’s classification of cavities
Tooth diagrams
Tooth-numbering systems
Color coding
Abbreviations
Tooth Diagrams
Anatomic and geometric designs are the most frequently used dental charting systems
Anatomic diagram: Illustrations resemble the actual crown and root of the tooth
Geometric diagram: Circle represents each tooth
The circle is divided to represent each tooth surface
Tooth-Numbering Systems
Universal numbering system
Begins with the maxillary right third molar and concludes at the mandibular right third molar
ISO/FDI system
Assigns a two-digit number to each tooth
Palmer notation system
Uses a bracket to designate the four quadrants of the mouth
Color coding
A visual notation to differentiate between treatment that has already been completed and treatment that still needs to be completed
Black or blue symbols represent dental work that has been completed
Red symbols indicate treatment that needs to be completed at future dental appointments
Once work has been completed, you will mark over the red with a black or blue notation to indicate that the work has been completed
Black’s Classification of Cavities
Standard classification system is universal to all dentists and is used to describe the location of decay and the best method for restoring a tooth
Black’s original classification included Class I through Class V
Class VI was added at a later date
Abbreviations
For single-surface restorations, charting abbreviations are based on the names of the tooth surfaces
B—buccal
D—distal
F—facial
I—incisal
L—lingual
M—mesial
O—occlusal
In multiple-surface restorations, two or more surfaces are involved
The combined surfaces become one name on which the abbreviation is based
The rule for combining two surfaces is to substitute the letter “o” for the -al ending of the first surface
For distal and occlusal, disto-occlusal (DO)
For mesial, distal, and occlusal, mesio-occlusodistal (MOD)
Charting
Dental charting systems are available in a variety of diagram styles
Symbols are placed on the tooth diagram of the dental record to represent the various treatments and the types of dental material used to restore the tooth or teeth
Important to learn the charting symbols for treatment to be completed as well as for treatment already provided
Clinical Examination of the Patient
Role of the clinical assistant is to escort the patient to the clinical area for the examination process
You will follow a routine protocol for the patient
The patient is seated in the dental treatment area, draped with a patient “napkin,” and positioned for the dentist to begin the examination
Soft Tissue Examination
Involves a complete examination of the cheeks, mucosa, lips, lingual and facial alveolar bone, palate, tonsil area, tongue, and floor of the mouth
This examination requires the use of visual assessment and palpation
The purpose is to detect any abnormalities in the head and neck area of the patient
Examination and Charting of the Teeth
The dentist examines each surface of each tooth and dictates findings to the dental assistant, who records the findings on the clinical examination form of the patient’s record
It is essential that all entries are recorded correctly and accurately
Examination and Charting of the Periodontium
Overall health condition of gingiva
Signs and location of inflammation
Location and amount of plaque and calculus
Areas of unattached gingiva
Areas of periodontal pockets measuring greater than 3 mm
Presence of furcation involvement
Mobility
The Treatment Plan
Level I: Emergency care, relieves immediate discomfort
Level II: Standard care, restores the patient to normal function
Level III: Optimum care, restores the patient to maximum function
Treatment Plan Presentation
On completion of a thorough clinical examination, an appointment will be scheduled to present the treatment plan to the patient
Typically, a 30-minute to a 1-hour appointment without interruptions is scheduled for the patient
It is important to have available the diagnostic tools to present the case
The dentist should have readied the patient chart, radiographs, diagnostic casts, and treatment plans
Other visual aids might include the following:
Before-and-after photographs
Diagnostic casts of similar cases
Models of proposed appliances
The patient is made comfortable, and the dentist takes care to present all information in terms that the patient can understand
After the presentation has been made, the dentist or finance manager will present the fee estimate for each treatment option
The patient is encouraged to ask questions and to discuss the advantages and disadvantages of each plan
When the patient makes a decision and accepts a treatment plan, he or she is giving informed consent for treatment
The finance manager will explain the payment plans and make necessary financial arrangements with the patient
When these arrangements have been completed, the patient is scheduled for treatment
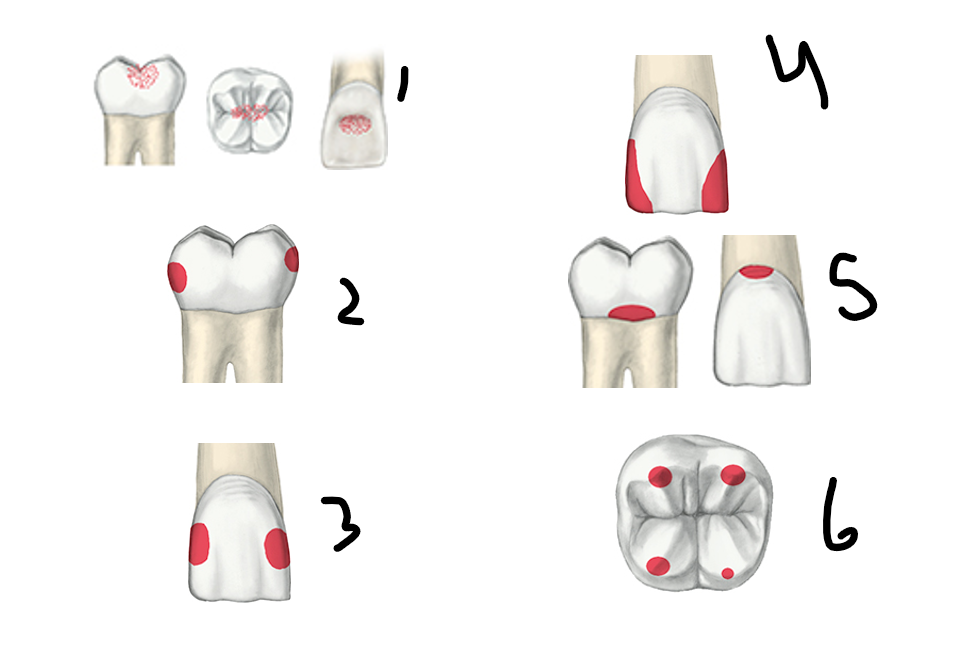
Label type of tooth issue from 1-6
Class 1- decay on the occlusal surfaces in the pits and curves
Class 2- decay on proximal surfaces of posterior teeth
Class 3- Mesial and distal decay
Class 4- decay is on mesial or distal side that includes incisal edge
Class 5- Gum line decay also known as cervical decay
Class 6- decay that is on the cusp tips
Abbreviations
For single-surface restorations, charting abbreviations are based on the names of the tooth surfaces, which are?
Single Abbreviations:
B—buccal
D—distal
F—facial
I—incisal
L—lingual
M—mesial
O—occlusal
The rule for combining two surfaces is to substitute the letter “o” for the -al ending of the first surface
For distal and occlusal, disto-occlusal (DO)
For mesial, distal, and occlusal, mesio-occlusodistal (MOD)
Soft Tissue Examination
Involves a complete examination of the cheeks, mucosa, lips, lingual and facial alveolar bone, palate, tonsil area, tongue, and floor of the mouth
This examination requires the use of visual assessment and palpation. The purpose is to detect any abnormalities in the head and neck area of the patient
Examination and Charting of the Periodontium
Specific periodontal findings to be recorded include the following:
Overall health condition of gingiva
Signs and location of inflammation
Location and amount of plaque and calculus
Areas of unattached gingiva
Areas of periodontal pockets measuring greater than 3 mm
Presence of furcation involvement
Mobility
The Treatment Plan
Types of treatment plans
Level I: Emergency care, relieves immediate discomfort
Level II: Standard care, restores the patient to normal function
Level III: Optimum care, restores the patient to maximum function
Treatment Plan Presentation
On completion of a thorough clinical examination, an appointment will be scheduled to present the treatment plan to the patient
Typically, a 30-minute to a 1-hour appointment without interruptions is scheduled for the patient
It is important to have available the diagnostic tools to present the case
The dentist should have readied the patient chart, radiographs, diagnostic casts, and treatment plans
Other visual aids might include the following:
Before-and-after photographs
Diagnostic casts of similar cases
Models of proposed appliances
The patient is made comfortable, and the dentist takes care to present all information in terms that the patient can understand
After the presentation has been made, the dentist or finance manager will present the fee estimate for each treatment option
The patient is encouraged to ask questions and to discuss the advantages and disadvantages of each plan
The patient is made comfortable, and the dentist takes care to present all information in terms that the patient can understand
After the presentation has been made, the dentist or finance manager will present the fee estimate for each treatment option
The patient is encouraged to ask questions and to discuss the advantages and disadvantages of each plan
When the patient makes a decision and accepts a treatment plan, he or she is giving informed consent for treatment
The finance manager will explain the payment plans and make necessary financial arrangements with the patient
When these arrangements have been completed, the patient is scheduled for treatment
Factors That Can Affect Vital Sign Readings
Emotional factors
Stress
Fear
Physical factors
Illness
Drinking or eating
Exercise
Temperature
Degree of the hotness or coldness of the body’s internal environment
Metabolism: Process of physical and chemical changes that takes place in the production of the body’s heat
During an illness, a person’s metabolism increases for the purpose of elevating the body’s temperature
Most bacteria and viruses cannot survive in excess heat, and this is the body’s way of defending against such diseases
Temperature Readings
Thermometer is the instrument used to measure body temperature
Temperature readings are calibrated according to the Fahrenheit (F) or the Celsius (C) scale
Average range of oral temperature of a resting person is 97.6º F to 99º F
The average body temperature is higher in infants and younger children than in adults
Types of Thermometers
Digital
Battery operated, a timing system shows a digital reading after 30 seconds
A disposable sheath slides over the probe before insertion
Tympanic
An infrared signal is bounced off the eardrum, and an accurate reading is provided within 2 seconds
Temporal scanner
Uses surface temperature of artery of forehead
Glass
Many states have banned the use of mercury thermometers because of health hazards

pulse
The pulse is the rhythmic expansion of an artery each time the heart beats
The pulse may be taken at various sites
Radial artery: Inner surface of wrist
Brachial artery: Inner fold of the upper arm
Carotid artery: Alongside the larynx
Pulse characteristics
Rate: Number of beats that occurs during the counting period
Rhythm: Pattern of the beats, such as an occasional skipping, speeding up, or slowing down of a beat
Volume: Force of the beat, such as a strong or a weak beat
Pulse readings
Make sure the patient is positioned with his or her arm at the same level or lower than the heart
The arm should be well supported and extended straight out
Normal pulse rate in resting adults: 60 to 100 beats per minute
In a child: 70 to 120 beats per minute
It is difficult to detect any possible arrhythmia (irregularity) in the heartbeat in times shorter than 30 seconds
Respiration
The process of inhaling and exhaling, or breathing
Respiration characteristics
Rate: Total number of breaths per minute
Rhythm: Breathing pattern
Depth: Amount of air inhaled and exhaled
Respiration readings
Adult: 10 to 20 breaths per minute
Children and teenagers: 18 to 30 breaths per minute
BP
Blood pressure reflects the amount of work the heart has to do to pump blood throughout the body
Two pressures of the heart
Systolic: Reflects the amount of pressure it takes for the left ventricle of the heart to compress or push oxygenated blood out into the blood vessels
Diastolic: The heart muscle at rest when it is allowing the heart to take in blood to be oxygenated before the next contraction
BP equipment
The equipment used when taking a patient’s blood pressure are the sphygmomanometer and the stethoscope
Sphygmomanometer
Includes the blood pressure cuff and meter
The cuff is a cloth wrap that holds an inflatable rubber bladder
A rubber bulb is attached to the cuff with rubber tubing
To get an accurate reading, it is important to use the appropriately sized cuff
Arm circumference 8 to 10 inches—“small adult” cuff
Arm circumference 10½ to 13 inches—“adult” cuff
Arm circumference 13½ to 17 inches—“large adult” cuff
Arm circumference 17½ to 20 inches—“adult thigh” cuff
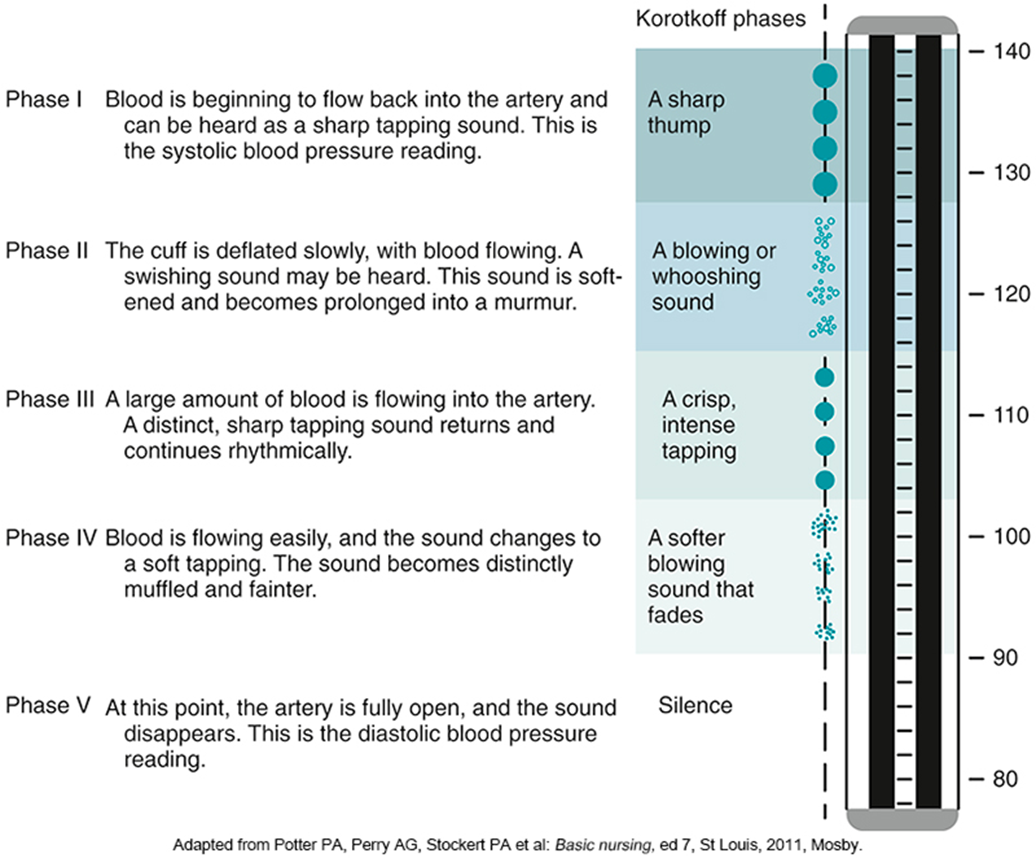
The stethoscope is used to amplify Korotkoff sounds
A series of sounds produced by the blood rushing back into the brachial artery, which has been collapsed by the pressure of the blood pressure cuff
As the pressure in the cuff is slowly released, the stethoscope picks up a distinct thumping sound that grows louder and then softens to a murmur
Five phases of Korotkoff sounds occur during deflation of the blood pressure cuff
An automated electronic blood pressure device is used in many practices today to simplify and speed the taking of blood pressure
Wrist blood pressure monitors can be accurate if used exactly as directed
These devices are extremely sensitive to body position
The arm and wrist must be at heart level, with the patient quiet and still
BP readings
A situation may arise in which it is necessary to take several pressure readings to obtain an accurate or average reading
If this occurs, allow the deflated blood pressure cuff to remain on the patient for a minimum of 10 minutes before you obtain another reading
If taken too soon, the reading may be incorrect
Medical considerations
The stress and anxiety of a dental procedure could possibly elevate a patient’s blood pressure
Many drugs have adverse effects that can interfere with dental treatment
A patient who has been diagnosed with hypertension should be under the care of a physician during a treatment regimen
Advanced Monitoring Procedures
Additional patient monitoring techniques are being introduced into dental surgical procedures as a standard of monitoring a patient’s health status in a noninvasive way
Monitoring patients during the preoperative, operative, and postoperative phases can occur as an expanded function once the certified dental assistant has completed a board-approved course in these procedures
Pulse oximetry
Pulse oximetry is used for measuring the concentration of oxygen in the blood
This procedure is of particular importance for monitoring oxygenation and pulse rate throughout anesthesia and during the recovery phase
The pulse oximeter works by passing a beam of red and infrared light through a pulsating capillary bed
Oxygenated blood is bright red
Deoxygenated blood is more blue-purple
The oximeter detects the pulse, and then subtracts the intensity of color detected when the pulse is absent
The remaining intensity of color represents only the oxygenated red blood
A fit, healthy person should have an oxygen saturation level between 95% and 99%
Electrocardiogram (ECG)
A procedure that measures the electrical activity of the heartbeat
In dentistry, the ECG can be used as a preventive measure when a patient is undergoing general anesthesia or IV sedation in a hospital or outpatient setting
The chest leads are placed on the patient at specific locations
The machine then amplifies the natural electrical currents generated by the electrical impulses of the heart and the pattern is traced on graph paper
With each beat, an electrical impulse or wave travels through the heart
The ECG records a series of waves that move above or below a baseline value
This wave causes the muscle to squeeze and pump blood from the heart
Each deflection corresponds to a particular part of the cardiac cycle
Arrythmias
Sinus arrhythmia: Rate or rhythm is altered
Atrial arrhythmia: The atria contracts before the next cardiac cycle
Atrial flutter: The atria is beating at an extremely rapid rate
Ventricular arrhythmia: The ventricles contract before the next cardiac cycle
Ventricular tachycardia: The ventricles are beating at an extremely fast rate
Ventricular fibrillation: Total electrical dysfunction
Asystole: No heartbeat
Patient Education
It is estimated that 50 million Americans have high blood pressure
Approximately one fourth of that population is not aware of their medical condition
By taking a patient’s blood pressure at every visit, not only are you gathering vital information for the patient’s treatment that day, but you may also be saving that person’s life
antecubital space
small grove or fold in the inner arm, at or “in front of” (ante) the elbow (cubitus)
arrhythmia
abnormally and irregularity in the force or rhythm of the heartbeat
blood pressure (BP)
measurement of the force and rate of the pressure of the blood in the circulatory system
brachial
relating to the upper arm (brachium), as in the brachial artery
carotid
the two major arteries on each side of the neck that carry blood to the head and neck.
diastolic
the last sound heard when taking blood pressure; the normal rhythmic relaxation and dilation of the heart chamber
electrocardiogram
a test that records the electrical activity of the heart and records electrical currents associated with heart muscle activity.
korotkoff
specific sounds heard in the stethoscope during blood pressure measurement.
metabolism
the process by which your body converts what you eat and drink into energy
oximetry
test to measure the oxygen concentration in the blood
palpate
to examine or explore by touching
pulse
the rhythmic beating of the arteries produced by regular contractions of the heart
radial
related to the radius (bone) or forearm (antebrachium), as in the radial artery
rate
a quantity measured, as in breaths and heartbeats
respiration
the act of haling or exhaling; breathing
rhythm
a sequence or patterns, such as the heartbeat or breathing
sphygmomanometer
an instrument used when measuring blood pressure
stethoscope
an instrument used for listening to sounds produced within the body
systolic
the first sound heard with taking blood pressure, which is the rhythmic contraction of the heart, especially of the ventricles
tachycardia
abnormally rapid heart rate, typically over 100 beats per minute.
temperature
degree of hotness or coldness of a body or an environment
thermometer
an instrument for measuring temperature
tympanic
related to or resembling a drum, as in the tympanic membrane, or the eardrum
volume
quantity or amount, as in force of the heartbeat