Urinary System & Fluid Balance
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
renal artery
segmental artery
interlobar artery
arcuate artery
interlobar artery (again)
afferent arteriole
glomerulus
efferent arteriole
peritubular capillaries OR vasa recta
interlobar vein
arcuate vein
interlobar vein
renal vein
What is the pathway of renal circulation?
filtration: glomerulus
exchange: vasa recta and peritubular capillaries
Between the following capillaries: glomerulus, vasa recta, and peritubular capillaries, which are for filtration and which are for exchange (reabsorption and secretion)?
liquid that only contains water and plasma (minus plasma proteins)
filtrate is the fluid that is filtered through the glomerulus and enters the nephron
What is filtrate?
blood contains formed elements and plasma, filtrate only contains water and plasma without proteins
blood is found in the glomerulus and filtrate is found in the glomerular capsule
What is the difference between blood and filtrate (in composition and where it’s found in the renal corpuscle)?
renal corpuscle (containing glomerulus and glomerular capsule)
proximal convoluted tubule (PCT)
nephron loop
distal convoluted tubule (DCT)
collecting duct
List the parts of the nephron
blood flows through the glomerulus (water and solutes move across wall of glomerular capillaries into capsular space)
filtrate enters the PCT, then the:
nephron loop
DCT
collecting ducts
papillary duct in renal papilla (now considered urine)
urine goes through the minor calyx, major calyx, renal pelvis, ureter, and then bladder
How does filtrate and urine flow through the nephron?
nephrons that contain long loops that extend deep into the renal medulla
this establishes a salt concentration gradient in the medulla that concentrates the urine and allows the body to conserve water (water exits tubule and enters the interstitial fluid)
What are juxtamedullary nephrons?
most common nephron, has short loops mainly found in the renal cortex
performs excretory and regulatory functions (like filtering blood and maintaining blood pressure)
What are cortical nephrons?
sympathetic division
nerves extend to the afferent and efferent arterioles and the juxtaglomerular apparatus, which decreases urine production
parasympathetic division
effects are unknown
The kidneys are innervated by both divisions of the ANS. Explain the effects each division has on the kidneys.
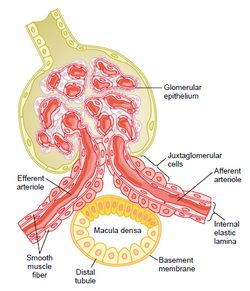
a structure in the kidney responsible for regulating systemic blood pressure and filtrate formation (GFR)
contains:
granular cells
in afferent arteriole, they contract the arteriole and synthesize, store, and release renin
macula densa
epi cells in the DCT that detect changes in NaCl concentration of tubular fluid and signals granular cells to release renin
What is the juxtaglomerular apparatus?
glomerular filtration
some water and dissolved solutes from the blood are separated and enter the capsular space of renal corpuscle
tubular reabsorption
some components of the tubular fluid move from the tubules and collecting ducts back into the blood
all vital solutes and most water are reabsorbed, excess solutes and waste remain in tubules
tubular secretion
movement of solutes out of the blood from the peritubular capillaries and vasa recta into the tubular fluid to be excreted in urine
water and secreted substances are eventually excreted from the body as urine
What are the three steps of urine formation?
endothelium
fenestrated, allows plasma to pass through (no large substances though)
basement membrane of glomerulus
restricts passage of large plasma proteins
visceral layer of glomerular capsule
filtration slits restrict the passage of most small proteins
*diagram on page 960
What are the three parts of the filtration membrane (in the glomerulus)?
CAN
water, glucose, amino acids, ions, urea, some hormones, ketones, and very small amounts of proteins
CANNOT
leukocytes, erythrocytes, platelets, and large proteins
What materials can and cannot pass through the glomerular filtration membrane?
glomerular hydrostatic pressure (HPg)
the blood pressure WITHIN the glomerulus
pushes water and some solutes out of glomerulus into the capsular space, high pressure
blood colloid pressure (OPg)
osmotic pressure exerted by dissolved solutes, draws fluid BACK into glomerulus
capsular hydrostatic pressure (HPc)
pressure in capsule due to filtrate, STOPS the movement of additional fluid
remember: OPg and HPc are AGAINST HPg
What are the three pressures affecting filtration at the glomerular filtration membrane?
concept that filtration occurs when pressures PROMOTING filtration are greater than those OPPOSING filtration
HPg - (OPg + HPc) = NFP
What is net filtration pressure (NFP)?
glomerular filtration rate (GFR)
solutes and water in tubular fluid
and amount of substances in urine
What three things increase due to increased NFP?
filtrate reabsorption
What is the one thing that decreases due to increased net filtration pressure (NFP)?
the rate of the volume of filtrate that is formed (volume/unit of time)
influenced by:
diameter of the afferent arteriole
the surface area of the filtration membrane
What is glomerular filtration rate (GFR) and what two things influence it?
when components within the tubular fluid move across the tubules and into the peritubular capillaries or vasa recta, returning to the blood
water and vital solutes are reabsorbed
where: primarily in the PCT (but can also happen everywhere else)
What is tubular reabsorption and where on the nephron does this occur?
the movement of solutes out of the blood within the peritubular capillaries and vasa recta and into the tubular fluid
selective
where: primarily in the PCT and DCT
What is tubular secretion and where on the nephron does it occur?
98%-100% is reabsorbed
two ways reabsorption happens:
Na+ moves down its concentration gradient from the tubule lumen into the tubule cells
(cells lining the tubules, Na+ eventually leaves the cells via Na+/K+ pumps and into the blood)
hormonal reabsorption
aldosterone and ANP
How much Na+ is reabsorbed in the PCT and what are the two ways reabsorption happens?
aldosterone
stimulates synthesis of Na+ channels and Na+/K+ pumps
this increases Na+ reabsorption
aldosterone maintains blood pressure and volume by decreasing urine output
ANP
inhibits Na+ reabsorption in the PCT and collecting tubules
this stops the release of aldosterone (results in increased water and Na+ secretion)
ANP decreases blood volume and pressure
How does aldosterone and ANP regulate Na+ reabsorption?
how much:
65% reabsorbed in the PCT
10% reabsorbed in the nephron loop
DCT and collecting ducts: controlled by hormones
how water is reabsorbed:
water moves via osmosis and is reabsorbed by paracellular transport between principal cells of the tubular walls
can also move out via aquaporins (because of hormonal control)
How much water is reabsorbed along the nephron and how does it happen?
ADH
binds to principal cells in the collecting tubules and ducts, providing extra aquaporins to increase water reabsorption
aldosterone
increases the number of Na+/K+ pumps (Na+ reabsorbs, water follows)
How does ADH and aldosterone increase water reabsorption?
60%-80% is reabsorbed, 10%-20% happens in the thick segment of the nephron loop
K+ reabsorption depends on Na+ movement:
if Na+ is reabsorbed, water follows
this increases the concentration of solutes in the tubular fluid, creating a gradient between the tubule and interstitial fluid
K+ moves down the gradient from the tubular fluid and into the interstitial fluid (then the blood)
How much potassium is reabsorbed along the nephron and how does it happen?
60% Ca2+ and 90%-95% PO43-
regulated by parathyroid hormone (PTH)
inhibits phosphate reabsorption in the PCT, but stimulates Ca2+ reabsorption
this causes blood Ca2+ to rise
What percentage of calcium and phosphate is secreted and how does it happen?
bicarbonate: yes
moves freely, but does not get reabsorbed (to prevent alkaline blood)
H+: no
most remains in blood
Is bicarbonate and H+ filtered in the renal corpuscle?
causes vasoconstriction of the afferent and efferent arterioles
this decreases GFR
decreased GFR = less filtrate/tubular fluid in nephron = less reabsorption
How does angiotensin II affect tubular reabsorption?
the maximum rate of substances that can be reabsorbed (or secreted) across tubule epithelium per a certain time
depends on the number of transport proteins in tubule membrane
What is transport maximum?
effect:
causes blood to become hypertonic (high in solutes, water leaves cells and causes them to shrivel)
how to fix it:
more water is reabsorbed from filtrate in the nephron and ADH is also released to further increase water reabsorption
both cause decreased urine output
How does dehydration affect blood osmolarity, and how does the body fix it?
composition
95% water, 5% solutes (salt, nitrogenous waste, some hormones and drugs)
volume
average 1-2 L per day
variations due to fluid intake, bp, temperature, diuretics, etc.
pH
normally between 4.5 and 8.0
more acidic with more protein in diet, more alkaline with veggies and fruit
specific gravity
density of a substance compared to density of water
slightly higher than water (due to solutes)
color
ranges from clear to dark yellow (depends on concentration of urobilin)
Describe the characteristics of urine (composition, volume, pH, specific gravity, and color)
continuous sympathetic stimulation causes:
relaxation of the detrusor muscle of bladder to accommodate urine
constriction of the internal urethral sphincter to retain urine
the external urethral sphincter is continuously stimulated to remain contracted
Describe the storage reflex for storing urine
volume of the bladder reaches 200-300 mL
baroreceptors (responds to stretch) signal sensory neurons
micturition center of brain sends nerve signals
parasympathetic stimulation causes detrusor muscles to contract and the internal urethral sphincter to relax
remember, the external urethral sphincter is consciously controlled
Describe the micturition reflex for excreting urine
MALE
bladder
anterior to rectum
urethra
functions as a passageway for urine and sperm
longer and made of three parts
FEMALE
bladder
anteroinferior to uterus
urethra
only function is to transport urine, shorter than male
What are the differences between the male and female urinary tract?
age
infants have the highest percentage of fluid
elderly people have the lowest percentage
children, young adults, and adults are between
sex
male adults have about 60% body fluid
female adults have about 55% body fluid
How does body water percentage vary based on age and sex?
INTRAcellular fluid (ICF)
fluid within the cells
2/3 of all body fluid
EXTRAcellular fluid (ECF)
fluid outside the cells, two types:
interstitial fluid (IF) - surrounds cells
blood plasma
1/3 of all body fluid
What are the two fluid compartments of the body?
moves in response to changes in osmolarity
when one compartment is hypo or hypertonic to another, water moves by osmosis from one compartment to another until the concentration is equal
example: drinking water
water enters the blood from the GI tract, plasma osmolarity decreases, and water moves from into the interstitial fluid then into the cells
How does water move between fluid compartments?
decreased blood volume and pressure
increased blood osmolarity
decreased salivary secretions
When you are dehydrated, what factors stimulate the thirst center in the brain?
increased blood volume and pressure
decreased blood osmolarity
increased salivary secretions
distension of the stomach (stretch caused by fluid entering)
What stimuli inhibits the thirst center of the brain?
urine output:
decreases urine output to increase blood volume and pressure
it additionally stimulates the thirst center and causes vasoconstriction of systemic blood vessels (to increase systemic bp)
How does ADH regulate urine output? Also, what does it do to the thirst center of the hypothalamus?
to maintain:
pH
acid-base balance
blood pressure
hydration
nerve and muscle function
heart health
Why is it important to maintain electrolyte balance?
99% found in ECF, 1% in ICF
the amount lost in urine is regulated by ADH, ANP, and aldosterone
most important electrolyte in determining blood plasma osmolarity and regulating fluid balance
Na+
98% found in ICF, 2% in ECF
only the ECF portion is regulated
required for neuromuscular activities and controlling heart rhythm
most is lost in urine
most lethal of all electrolyte imbalances
K+
most abundant anion in the ECF
found in the stomach as HCl, participates in inhibitory postsynaptic potentials, and has a part in transporting CO2 in the form of HCO3-
associated with Na+
follows Na+ by electrostatic interactions
obtained in the diet, lost in sweat, stomach secretions, and urine
Cl-
most abundant electrolyte in bone and teeth (99%)
needed for muscle contraction and neurotransmitter release
can exist bound to a protein (albumin), associated with phosphate, or in an unbound/free state
obtained in the diet, lost in urine, feces, and sweat
Ca2+
most abundant anion in bone and teeth (85%)
component of DNA, RNA, and phospholipids
acts as an intracellular buffer and urine buffer
regulated in similar ways to Ca2+ (because majority is bound to calcium)
PO43-
primarily found in bone or within cells
abundant ICF cation
important for enzyme reactions, helping Na+/K+ pumps, and muscle relaxation
obtained in the diet (via beans, peas, or leafy greens) and lost by sweat and urine
Mg2+
7.35 - 7.45
staying in this range is critical for:
regulating enzyme activity
preventing protein denaturation
and ensuring oxygen is delivered to all tissues
What is the normal pH range of the body, and why is it so important to maintain pH?
nutrients absorbed in the GI tract (from proteins and wheat)
waste produced from cells (like lactic acid)
What are two major things that cause an increase in blood acidity (increase in H+ concentration)?
antacid ingestion
vomiting with the loss of HCl
List two things that cause an increase in blood alkalinity (loss of H+)
function: substances that prevent large changes in pH after an acid or base is added to a solution, consists of a weak acid and weak base
protein buffering system
consists of proteins found in cells and blood plasma
amine group acts as a weak base to buffer acids, and carboxylic acid is a weak acid that buffers bases
phosphate buffering system
found in ICF
buffers metabolic acids produced by cells
net result: strong acid buffered to produce a weak acid
bicarbonate buffer system
most important in the body
weak base (HCO3-) and weak acid (H2CO3)
net result: strong acid buffered to produce a weak acid, and a strong base buffered to produce a weak base
Describe the function of buffers and list the 3 types of chemical buffering systems in the body
by regulating levels of carbonic acid
body at rest:
CO2 is eliminated from the lungs at the same rate body cells are producing CO2
body during exercise:
high blood levels of CO2 are detected by chemoreceptors and is relayed to the respiration center of the brain
breathing rate and depth change
How does the respiratory system control pH?
pH is too low (acidic)
all filtered HCO3- is reabsorbed along the nephron
more HCO3- is synthesized and absorbed and excess H+ is secreted into filtrate (these both increase pH)
pH is too high (basic)
renal tubules do not reabsorb all filtered HCO3-
HCO3- is secreted into filtrate and H+ is reabsorbed in exchange
How do the kidneys control pH?