Lab values slides
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
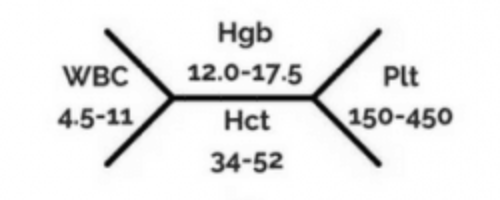
What is in the top, bottom, right and left of a common hematology chart that providers might give a PT?
Top: hemoglobin (g/dL)
Bottom: hematocrit (%)
Left: WBC (thousands/mm3)
Right: Platelet (thousands/mm3)
What are normal values for men and women for hemoglobin? What units?
Men: 14-18 g/dL
Women: 12-16 g/dL
What are normal values for men and women for hematocrit? What units?
Men: 42-52%
Women: 37-47%
What are normal values for WBC? What units?
5,000-10,000/mm3
What are normal values for platelets? What units?
150,000-400,000/mm3
What matters more for deciding therapy/tx approach: lab values, or S/S and pt appearance?
S/S appear more. Their history/subjective info is also very helpful, but lab values represent one point in time where as S/S represent what is currently going on. Both are clearly important.
What should be done if HGB level is >10 g/gL?
Therapy as indicated, not low enough to be super concerning, but definitely watching pt extra closely.
What should be done if HGB level is 8-10 g/dL? What should you expect to see?
Expect poor cardiopulm reserve/limit, monitor vitals closely (especially sPO2 for tissue perfusion, potential orthostatic hypotension, tachycardia). Monitor closely, but still probably can treat.
What should be done if HGB level is <7-8g/dL? What should you expect to see?
Tx might be contra. Go based on S/S, blood transfusion likely indicated, monitor closely.
What should be done if HGB level is <5-7 g/dL? What should you expect to see?
Critical low value, heart failure and death risk. Pt needs blood transfusion. PT more likely contraindicated.
What should be done if HGB level is 20g/gL? What should you expect to see?
This indicates inc. blood viscosity → capillary blockage/tissue ischemia (too many RBCs to perfuse adequately) likely not right time to treat.
What are 3 common less alarming reasons for HGB levels to be low?
Chronic conditions like cancer, chemo, kidney disease, etc. Pts usually chronically anemic
Surg post-op (300ml blood loss = 1.5 unit drop Hg
Fluid dilution: hypovolemic pt gets IV flush → hemodilution but because of high fluid volume, not low HGB levels.
What are the main 3 general activity guidelines for hematocrit (HCT) levels?
<25%: Light ROM, isometrics
>25%: light exercise, SxS approach
>30-35%: Ambulation, resistance as tolerated
What are causes and symptoms of Anemia? Should an anemic pt be treated?
Causes: Acute blood loss (external or internal), destruction or dec. production of RBCs
S/S: pale, weak, listless, easy fatigue, DOE, rapid/shallow pulse
Tx: Have they had transfusion? Monitor vitals&S/S closely. 2nd person for dec. fall risk. Risk v benefit
What are causes and S/S of erythrocytosis? Should this pt be treated?
Causes: myeloproliferative disorder (marrow producing too much RBCs), hypoxia in tissues (causing need for RBC production), high altitudes, heavy tobacco smoking, chronic lung disease, congenital heart defects
S/S: Headache, dizziness, blurred vision, dec. mental acuity, altered sensation hands/feet (d/t blocked capillaries)
Tx: Inc. risk for CVA and thrombosis, risk v reward.
Describe leukocytosis. What Dx’s and S/S are associated?
WBC > 10,000/mm3
Dx: Infection, leukemia, PNA, neoplasms, inflammation, tissue necrosis
S/S: Fever, chills, sore throat, fatigue
Describe Leukocytopenia. What Dx’s and S/S are associated?
WBC < 5,000/mm3
Dx: Bone marrow fail, radiation, chemo, HIV, autoimmune disease
S/S: Stiff neck, sore throat, fever/chills, headache, mouth ulcers, frequent infections
Describe neutropenia. What precautions need to be taken?
WBC < 1,500/mm3
Reverse isolation, neutropenic precautions (PT wear mask in room, Pt wear mask outside of room). Inc. risk of infection. If PT is sick, don’t treat this pt. No fresh fruit/flowers.
What are platelets, what is their function, and what is their normal value range and high/low critical value?
Platelets are cytoplasmic fragments of megakaryotes in bone marrow. They function in hemostasis and initiate clotting mechanisms.
Normal range: 150-400K/mm3
High critical value: 1 million/mm3
Low critical value: <20K/mm3
What is the name /value range for high platelet count? What causes this, and what are the S/S?
Thrombocytosis is a platelet count >400,000/mm3. It is caused by infection/inflammation, or genetic myeloproliferative conditions.
S/S: Inc. thrombosis formation, paradoxical inc. risk for bleeding (d/t damaged capillaries from excess platelets), HA, dizziness, weakness, chest pain, tingling hands/feet (d/t blocked/damaged capillaries)
What is the name/value range for low platelet count? What causes this, and what are the S/S? What needs to be avoided with this condition?
Thrombocytopenia is when platelet count is <150K/mm3. It is caused by bone marrow suppression (like radiation, chemo, etc)/leukemia, and cytotoxic drugs.
S/S: Bruising, epistaxis, hematuria, oral bleeding, petechiae, inc. risk of bleeding
Avoid: bumps, bruising, resistive exercise (intramuscular bleeding risk), valsalva (rupture blood vessels), falls, etc. All inc. riskiness d/t inc. bleeding risk.
Should a pt w/ platelet count of 20-50K/mm3 be treated?
Likely ok to treat, but monitor closely. Doing less intense exercises, AROM exercise w/ or w/out resistance, walking as appropriate.
When platelet count is <20K/mm3 what should be considered for tx?
Might be able to do ther-ex w/out resistance. Risk for spontaneous bleeding, petechia, ecchymosis, prolonged bleeding time.
<20K/mm3 is the low critical value range.
When platelet count is <10K/mm3 and/or temp is >100.5, what considerations need to be made for tx?
Most likely not treating this pt. Risk for spontaneous CNS, GI, and/or resp tract bleeding. PT contraindicated.
Is blood transfusion alone a direct contra-indication to PT? What considerations should be made?
Blood transfusion alone is not a PT contraindication except for first 15 mins of transfusion. Depends on current HGB level. Watch for S/S of transfusion-related immunomodulation (TRIM) reactions and circulatory overload (basically CHF signs). Extreme caution w/ fall risk, monitor vitals, careful to not dislodge transfusion site (safety risk and blood is expensive)
What are S/S of Transfusion-related immunomodulation (TRIM) reactions and circulatory overload?
Tachycardia, cough, dyspnea, crackles, HA, HTN, distended neck veins, fever, dyspnea, rash, hypotension. Basically CHF S/S.
Describe prothrombin time and International normalization ratio. What do they examine the function of? What are their normal range values? What is the difference between them, what medication is associated with them?
Prothrombin time (PT) examines the function of the extrinsic system in the clotting cascade. Normal values are 11-13.5 seconds, it measures the time to stop bleeding.
International normalization ratio (INR) is a normalized value for global usage of the extrinsic system in the clotting cascade. Normal value is 0.9-1.1.
Coumadin (warfarin generic) is an anticoagulant that thins blood and brings a low clot time (too fast clot, risk of blood clot) higher to a therapeutic time range.
Describe partial thromboplastin time and activated partial thromboplastin time. What do they examine the function of? What are their normal range values? What’s the difference between them, and medication is associated with them?
Partial thromboplastin time (PTT) examines the function of the intrinsic system in the clotting cascade. Normal values are 60-70 seconds, it measures the time for the intrinsic system to stop bleeding.
Activated partial thromboplastin time (aPTT) is the same thing, but w/ an activator so it clots faster (30-40 seconds), results are available in 1 hour.
Lovenox and Heparin are anticoagulants that thin the blood in the intrinsic system of the clotting cascade to bring a low clotting time up to a therapeutic range.
What is the therapeutic range (target range) for INR after anticoagulation? What would a higher number mean?
2-3. Higher would mean thinner blood so inc. risk of bleeding.
What considerations need to be made for PT when a pt has INR of <4.0, 4-5, >5-6, and 5-9?
<4: Do eval and regular routine, don’t progress any exercises until in therapeutic range.
4-5: Avoid resistive exercise. Light exercise, RPE<11
>5-6: Coumadin stopped (blood too thin already), administer Vit K or fresh frozen plasma. Do eval for DC planning, determine level of function. No tx.
5-9: Avoid excessive activity. Bed rest. may do eval only for d/c planning or to determind level of function. Consult w/ team. Monitor vitals closely.
What are the terms/values for coagulation being above/below target/goal range? What risks are associated with each?
Subtherapeutic levels: coagulation level below goal. INR<2. Risk for clotting, forming embolisms. Coumadin could potentially help?
Supratherapeutic levels: Coagulation level above goal. INR>3. Risk for bleeding, hemorrhage. Can be reversed w/ Vit. K or fresh frozen plasma
What is D-Dimer indicative of? What is it’s normal value, and what is it a measure of? What are higher levels associated with? What should be done w/ higher levels?
D-Dimer shows that clotting has occurred (not necessarily that a clot has formed). It’s produced by action of plasmin on X-linked fibrin. Normally 0.5mg/L, it is a measurement of fibrin degradation.
High levels associated with DVT, PE so screen for DVT and PE.
T/F: moving/walking is likely to mobilize an existing blood clot.
False, highly unlikely to mobilize the blood clot w/ mobilization of the body.
What is more concerning, a superficial or deep venous thrombosis?
Deep is more concerning.
What is the purpose of anticoagulation therapy? Does it remove an existing clot?
Anticoagulation therapy reduces the risk of another clot, but doesn’t remove the existing clot.
What are the S/S of PE that we need to educate a pt about?
Sudden chest pain, cough, difficulty breathing, anxiety, LOC, inc RR, cyanosis, lightheadedness.
Describe what is included in DVT prohpylaxis
Early mobilization is a large deterrent of blood clot formation.
Ankle pumps
Thrombo-embolytic deterrent hose
Sequential compression devices
Pharmacological intervention
How much of body weight is water? How is the water in the body distributed between Intra/extracellular?
60% of BW is water
2/3 is intracellular
1/3 is extracellular (intersititial spaces, plasma, trans-cellular compartment
What is Anasarca?
Generalized/systemic edema in interstitial spaces.
Where does fluid go with high capillary hydrostatic pressure?
Water is pushed out of the capillary, so into interstitial space.
Where does fluid go with high interstitial hydrostatic pressure?
Water is pushed out of the interstitial space and into the capillary.
Where does fluid go with capillary colloidal osmotic pressure?
Fluid is pulled into the capillary since concentration gradient is higher inside the capillary than outside. Fluid goes in to equalize the concentration gradient.
Where does fluid go with interstitial colloidal osmotic pressure?
Fluid is pulled into the interstitial space since the concentration gradient is higher inside the interstitial space than in the capillary. Fluid goes into interstitial space to equalize the concentration gradient.
What are the 4 main mechanisms for edema?
Inc. capillary hydrostatic pressure (pushes fluid out of capillary)
Dec. capillary colloidal pressure (lower concentration gradient in capillary, so water pulled to interstitial space)
Inc. capillary permeability (allows fluid to flow through when it shouldn’t)
Obstruction of lymphatic flow (Not allowing fluids to be properly regulated.
What conditions would cause edema d/t inc. capillary hyrdostatic pressure?
CHF, HTN, inc. venous pressure
What conditions would cause edema d/t dec. capillary colloidal pressure?
Conditions w/ loss of proteins: liver failure/cirrhosis, malnutrition/starvation, injury/burns, kidney disease.
What conditions would cause edema d/t inc. capillary permeability?
Conditions w/ inc. semimembanous pore size: burns, inflammation, immune response.
What conditions would cause edema d/t inc. obstruction of lymphatic flow?
Cancer, surgical removal of lymph nodes, burns, injury/trauma, infection blocking nodes.
What is hypovolemia, how can it be caused (2 mechanisms), and what are S/S?
Dec. state of extracellular volume
Caused by limited intake (dec. thirst mechanism d/t CVA, dementia, aging) or excessive loss (vomiting, sweating, burns, uncontrolled DM, diarrhea, fever)
S/S: lightheadedness (dec. BP), dry mucus membranes, tachycardia (weak d/t low volume, and rapid), poor skin turgor, AMS
What is hypervolemia, what causes it, what are S/S? What special precautions need to be taken?
Hypervolemia is inc. state of extracellular volume
Caused by excessive intake (too much IV fluid, hypertonic IV pulls fluid out of capillary, blood transfusion) or inadequate output (CHF, renal insufficiency, steroid use, hyperaldosteronism, low protein diet, liver failure/cirrhosis.
S/S: pitting/dependent edema, SOB, anasarca, bounding pulse, HTN, tachycardia, moist crackles
What is the difference between graduated compression stockings and thromboembolytic deterrent (TED) hose? When should caution be used with either of these?
Thromboelmoblytic deterrent (TED) hose: <20 mmHg pressure, no gradient, preventative, post surgery or bedrest/immobility pt. Temporary
Graduated compression stockings: Higher pressure distally than proximally (pressure gradient), prescription strength (20-30, 30-40, 40-50 mmHg ranges), can be OTC custom fit, often w/ venous insifficiency and varicose veins.
Caution w/ CHF, CKD, arterial insufficiency. Blood is already not flowing properly, don’t want to compress even more.
What functions are impacted by the electrolyte balance? What system primarily maintains the electrolyte balance?
Nerve function
Muscle contraction/relaxation
Cardiac rhythm/conduction
Bone health
Blood coagulation
Maintenance of proper fluid balance in body
Primarily maintained by the renal system to retain/excrete appropriate amounts of electrolytes as appropriate.
What goes in each of the sections of the medical short hand for electrolyte values? (hint: top left, middle, right ; bottom left, middle, right, and far right)
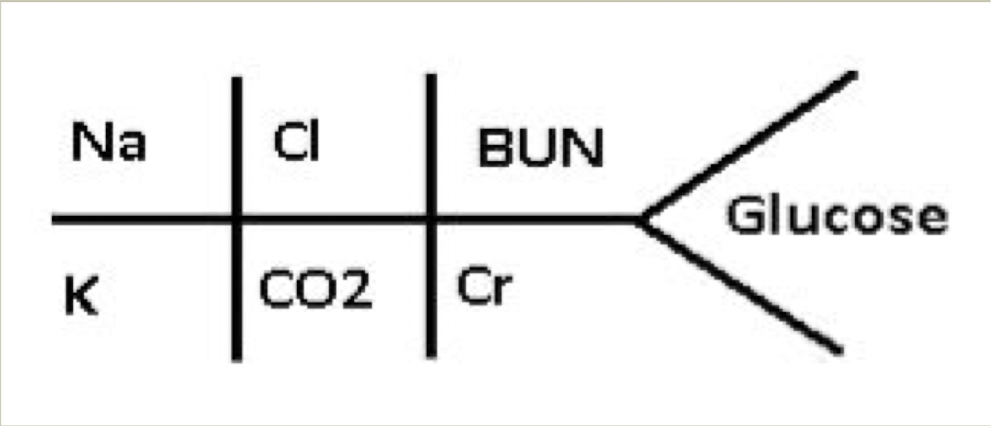
Top:
Left: Na (sodium)
Middle: Cl (chlorine)
Right: BUN (blood urea nitrogen)
Bottom:
Left: K (potassium)
Middle: CO2 (carbon dioxide)
Right: Cr (creatinine)
Far Right: Glucose
What are normal, high and low values for Na+? Are these levels referring to intra or extracellular concentrations?
Normal range for Sodium (Na+) is 136-145 mEq/L
Hyponatremia (low sodium) is anything < 136 mEq/L
Hypernatremia (high sodium) is anything > 145 mEq/L
Describe hyponatremia. How is it defined, what is it associated with, what are S/S?
Hyponatremia (low sodium): Anything < 136 mEq/l
Associated: dec. Na+ intake, Inc. H2O, Inc. Na+ loss (vomiting/GI suctioning/diarrhea), burns (Brings Na+ into cell), excess diuretic therapy, decompensated CHF, liver disease, syndrome of inappropriate antidiuretic hormone (SIADH)
S/S: Nausea, vomiting, headache, AMS, muscle weakness, malaise, fatigue, lethargy, seizure
Describe hypernatremia. How is it defined, what is it associated with (what can those causes lead to?), what are S/S?
Hypernatremia (high sodium): Anything > 145 mEq/L.
Associated: dehydration (d/t hypovolemia w/ dec. H2O intake → postural hypotension since not enough BP ; Inc. Na+ intake w/ normal fluid volumes (results in hypervolemia d/t excess fluid in extracellular space → elevated BP, weight gain, venous distention, edema
What are normal, high, and low values for K+? Are these values referring to intra or extracellular concentrations?
Normal: 3.5-5 mEq/L
Hypokalemia (low K+): anything <3.5 mEq/L
Hyperkalemia (high K+): Anything >5 mEq/L
Referring to extracellular concentrations of potassium
Describe hypokalemia. How is it defined, what are it’s general causes, and S/S?
Hypokalemia (low K+): Anything <3.5 mEq/L
Causes: Malnutrition (Low K+ intake), Vomiting, diarrhea, GI drainage tubes (decreasing body K+ stores), Insulin → Inc. uptake of glucose and K+ → dec. extracellular conc.
S/S: Muscle weakness/cramping, fatigue, conduction abnormalities (AV block, V-tach, fibrillation, sinus bradycardia)
Describe hyperkalemia. How is it defined, what can cause it, what are S/S?
Hyperkalemia (high K+): Anything above 5 mEq/L
Causes: Inc. K+ intake, renal insufficiency (not excreting enough), Shifts of K+ from ICF → ECF d/t cell damage, insulin deficiency (not uptaking K+ into cell), muscle damage, crush injuries, burns, meds (Heparin, NSAIDS, ACE inhibitors, Beta blockers)
S/S: Muscle weakness → paralysis, nausea/vomiting, paresthesias, cardiac conduction abnormalities (tachycardia → bradycardia → cardiac arrest since inc. excitability initially → weakness → paralysis)
What is more dangerous/concerning between hypo/hyperkalemia, why?
Hyperkalemia is more concerning. Both can lead to conduction abnormalities, but hyperkalemia has a more risky chain of events.
Hyperexcitability initially → weakness → paralysis of muscles (heart is a muscle), so tachycardia → bradycardia → cardiac arrest
What are normal, high, and low values for Ca++ values?
Normal: 8.5-10.5 mg/dL
Hypocalcemia (low Ca++): Anything < 8.5 mg/dL
Hypercalcemia (high Ca++): Anything > 10.5 mg/dL
Describe hypocalcemia. How is it defined, what is it associated with, what are S/S?
Hypocalcemia (low Ca++):Anything <8.5 mg/dL
Associated: Limited CA+ intake, chronic renal insufficiency (Ph retention → Ph binds w/ Ca+, so less free Ca+), Vit D def. (Vit D → calcitrol which inc. Ca+ update form GI, so less of that), hypoparathyroidism (dec. PTH → dec. Ca+ release from bone so less ECF CA+)
S/S: Inc. NM excitability → tetany, muscle twitching, convulsions, abdominal cramping, numbness/tingling, fatigue, confusion, hyper-reflexia, cardiac arrythmias
What two tests being positive indicates hypocalcemia? What would be a positive result on these two tests?
Trousseau sign: Flexor spasm distally as BP cuff pressure increases showing hyperexcitability
Chvostek sign: Tap facial nerve → edge of mouth twitches, showing hyperexcitability
Describe hypercalcemia. How is it defined, what is it usually caused by, what does it inc. risk for? What are S/S?
Hypercalcemia (high Ca+): Anything >10.5 mg/dL
Caused by hyperparathyroidism (inc. PTH → inc. Ca+ pulled from bone), bone cancers, PTH-secreting tumors, so primarily issues with bone/PTH.
Increases risk for osteoporosis d/t Ca+ being pulled from bone
S/S: Drowsiness, fatigue/weakness, ataxia, loss of muscle tone, lethargy, nausea/vomiting, constipation, polyuria, polydipsia (many of these symptoms d/t slowed nerve conduction causing systemic issues.
What lab markers are considered protein/protein metabolites? What are their normal value ranges? What is an inc. in these levels together called, and what is it often associated with?
Blood urea nitrogen (BUN): 10-20 mg/gL
Creatinine: 0.6-1.2 mg/dL
Inc. in BUN and Cr- is Azotemia. It can lead to dec. activity tolerance, and is often associated w/ kidney dysfunction.
What are normal levels of BUN? What are inc/dec levels of it associated with?
Normal blood urea nitrogen (BUN): 10-20 mg/dL
Inc BUN: CHF, MI, DM, renal insufficiency, inc. muscle (protein) catabolism
Dec BUN: liver failure
What are normal levels of Cr-? What is Cr- a good indicator of? What is associated w/ inc. Cr-?
Normal Creatine (Cr-) levels: 0.6-1.2 mg/dL
Cr- is a good indicator of kidney function/GFR
Inc Cr-: CHF, renal dysfunction, nephritis, urinary tract obstruction, MD/myasthenia gravis/rhabdomyolysis (muscle breakdown → inc. Cr- in blood stream), acromegaly
Describe/define abnormal levels of glucose (hypo and hyper).
Hypoglycemia: Anything <50mg/dL. This creates a SNS response and catecholamine release → tachycardia, Htn, tremor, irritability, sweating, hunger, HA, weight changes, mental dullness, confusion, amnesia, seizures, paralysis, paresthesias, dizziness, visual disturbances, LOC.
These neural signs d/t intracellular edema d/t low ECF so relative ICF high conc.
Hyperglycemia: Anything >200 mg/dL. Associated w/ polyphagia, polydipsia, dry mouth, itchy skin, tingling in feet/heels, cardiac arrythmia, stupor, coma, seizures (neural signs d/t intracellular dehydration since H2O follows concentration gradient)
How would PT/exercise protocol be impacted when glucose levels are <100 or >250? What about >300-350mmol/L?
<100: Potentially give pt juice or something (check w/ nursing first)
>250: Caution for exercise d/t risk of ketoacidosis since too much glucose in blood stream so burning fat
>300-350: No exercise if ketones in urine d/t risk of developing ketoacidosis.
What are normal vitals we monitor and their ranges?
BP: <119/79
O2 sat: >93-95. Concerned if <90, pt qualifies for O2 if < 88
RR: 12-20
HR: 60-100
What is normal, elevated, Stage 1/2HTN for BP?
Normal: <120/<80
Elevated 120-129/<80
Stage 1 HTN: 130-139/80-89
Stage 2 HTN: >140/>90