Growth and developement toddlers, preschool, and school age
1/139
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
140 Terms
what is a toddler
1-3 years of age. Fine and gross motor skills being developed: tolileting, feeding, grooming, dressing, autonomy, individuality, activities of daily living, motor skills, language development
Physical growth of toddler
Average weight gain = 3 to 5 lb per year
Length/height increases steadily in spurts (slower rate than infant)
Average increase 3 inches per year
About ½ adult height by age 2
Head size more proportional to body by age 3
Physiologic Changes #1 for toddlers
Anterior fontanel closes by 18 months
Brain = 90% adult size by age 2
Increased myelination = improved coordination, balance, and sphincter control/ toileting
Head circumference measured till 3 years old
Respiratory system
Alveoli continue to increase in number
Trachea and airways remain small compared to adult
Tonsils and adenoids are relatively large: increase risk for infection= possible airway occlusion
Cardiovascular system
Heart rate decreases
Blood pressure increases
Norm depends child age
Physiologic Changes #2 for toddlers
Gastrointestinal system
Stomach increases in size
Small intestine grows in length
Less frequent stools—color varies with diet
Bowel control typically achieved by end of toddler period
Genitourinary system
Bladder and kidney reach adult function by 16 to 24 months
Bladder capacity increases
Urethra remains relatively short which increases risk for UTIs
Musculoskeletal system
Muscles maturing
Swayback and pot belly until 3 years old
Developmental theories r/t toddlers
Erikson: autonomy vs shame:achieves autonomy and self control, seperates from caregiver.
Piaget: sensorimotor and preoperational; differentiaties self from objeccts; increased object permanence; beginning symbolic though-something rep something/associated meaning with something.
Freud
Sensory development
Hearing intact since birth: increased ability of movement and manipulation
Visual acuity continues to improve
May prefer certain smells
May prefer certain textures (soft vs. scratchy clothes)
Explore environment with all five senses!
Puts lots of things in mouth to learn abt them. Puts them at risk for harm
motor skill development for toddlers
Development of _hand eye is necessary for the refinement of fine motor skills.
Increased abilities of __mobility_and manipulation help the curious toddler explore and learn more about their environment
As the toddler masters a new task, they gain confidence to conquer the next challenge.
The senses of light, hearing, and touch are useful in helping to coordinate gross and fine motor movement.
Gross Motor Skills
Repeating gross motor movements and skills strengthen large muscle groups
They often use physical actions to express their emotions
Fine Motor Skills
Adequate vision is necessary for the refinement of fine motor skills because eye-hand coordination is crucial for directing the fingers, hand, and wrist in small muscle tasks
motor skill development for toddlers depending on age
15 months: Gross motor: Takes few steps on own. Fine motor: feeds self finger food.
18 months: Gross motor: walks independently, climbs on/off furniture, seats self in chair, climbs stairs w/ assistance. FIne motor: scribble, tries to use a spoon, trows a ball, stacks 3 to 4 cubes.
24 months: Gross motor: Runs, kicks ball, walks upstairs with assistance. FIne motor: Eats with a spoon, stacks 7 cubes, points to named pictures and objects, starting to turn knobs
30 months: Gross motor: jumps with both feet. Fine motor: Turns knobs, turns book page one at a time, takes off some clothing items
36 months: Gross motor: puts on some clothes by self. FIne motor: Strings items together, uses fork, copies a circle.
Communication and Language Development for toddlers
Language acquisition is automatic and spontaneous
Language skills are enhanced with practice
Encouraging children’s speech and reading, singing, rhyming to them help build language skills.
_Cognitive and imitation are important components in early language acquisition.
When the toddler learns to use of the word “why” they use it to challenge adults and keep them talking. It increases their understanding of the world.
Young children living in a bilingual family can learn more than one language at the same time.
2 years old: 2 words in sentences
2-3 years old: 2-3 word sentences
3 year olds: 3 word sentences
language developemnt for toddlers
12 months: receptive language: understands no. Expressive lnguage: imitates or uses gestures such as waving goodbye
15months: receptive language: follows command accompanied by a gesture. Expressive language: Uses a finger to paint things, looks for a familar object when named, tries to say one or two words other than dada and mama
18 months: receptive language: follows a one word w/out a gestures. Expressive language: tries to day three or more than dada and mama
24 months: receptive langauge: points to named body parts, points to pictures in books. Expressive language: sentences of 2 words, uses gestures like blowing a kiss or nodding yes
30 months: receptive langage: follows a series of two independant commands, names items when pointed and asks “what this”. expressice language: vocabulary of abt 50 words, sentences of to with an action word
36 months: uses at least two back and forth exchanges when conversing, understands physical relationships-on, in, under- Expressive language: most outside the family understand speech, asks why, where and what, verbalizes action happening in picture, says first name when asked.
emotional and social development for toddlers
Emotional development is focused on seperation and individualization
Seperate from caregivers • forming sense of control over self & environment
Emotionally labile; may have temper tantrums
Rituals and routines are important to provide stability and security for the toddler.
Toddlers rely on a security item to comfort themselves in stressful situations.
Aggressive behavior is normal in the toddler period, so parents should not blame them for the behavior, but should help them understand the results of this behavior.
Up to parent to hold firm boundaries.
Give limited choices to help reduce temper tantrums
Time out used to calm child. After address problems and what to do differently.
emotional and social developement for todddlers
Fears: loss of parents
Seperation anxiety
As toddlers become more independent, they can tolerate only brief periods of separation from their parents
Parents should be honest about leaving and telling them when they will return in language the child can understand (i.e., after lunch)
Fear of strangers:
Stranger anxiety
Somewhat fearful of strangers unless they are accompanied by a family member
Loud noises
the dark
Signs of developmental delay for toddlers
After independent walking for several months: persistent tiptoe alking, failure to develop a mature walking pattern
By 18 months: Not walking, speaking or not understanding the function or common houshold items
By 2 years: Does not use 2 word sentences, doesnt imitate actions, doesnt follow basic intructions, cant push a toy with wheels
By 3 years: difficulty with stairs, cant copy circle, little interest in other kids, doesnt understand simple instructions, cant build tower of more than four blocks, diff manipulating small, extreme difficulty in seperation from parent to caregiver, doesnt engage in make believe, freq falling, cant communicate in short phrases, unclear speech, persistent drooling
Developmental milestonees for the three year old
Developmental Milestone | Goal |
Gross motor |
|
Fine motor |
|
Psychosocial |
|
Cognitive |
|
Language |
|
Promoting heathly growth and development for toddlers
Foundations of Self esteem
Love and respect regardless of the child’s gender, behavior, or capabilities: avoid calling child bad, if not bad
Familiarity with the daily routine
Making expectations known through everyday routines helps to avoid confrontations
Knows what to expect and how to act
Preliminary discussion of what is going to happen and appropriate behavior with positive feedback helps prevent unwanted behavior
Limit setting (and remaining consistent with those limits) helps toddler master their behavior.
Toddler learn abt abt cooperation through the predictable flow of daily life
play for toddlers
Play is the major socializing medium for toddlers
Parents should limit television or screen time and encourage creative and physical play instead.
Parallel play– toddlers usually play alongside another child rather than cooperatively.
Don’t learn to share until in later toddlerhood
It is important to provide a variety of safe toys to allow the toddler many different opportunities for exploring the environment.
Adequate physical activity is necessary for the development and refinement of movement skills
At least 60 mins/day of structured physical activity
1-several hours of unstructured physical activity per day
Indoor and outdoor play areas should encourage play activities that use large muscle groups
Limit screen time until 18months; can talk to relatives on screen though.
Ages 2-5: limit noneducational media/device use to 1hr/weekday, up to 3 hrs/weekend.
Promoting safety for toddlers
Safety in the car: rear facing carseat- safer- causes less head, spine injuries, used up until 2, due to development of neck muscle and height and weight limit reached
safety in water: increased risk for drwning, head circumference bigger=prone to falling, dont know how to swim until till abt 4
Safety in the home: avoiding exposure to tobacco: decreases lung fx
Preventing injury
Preventing poisoning: lock up chemicals, leave in original packaging
Preventing injury for toddlers
Curiousity, mobility, and lack of impulse control all contribute to the incidence of unintentional injury. Have a limited understanding of boundaries and of danger: able to open drawers and doors, unlock deadbolts and climb. No guns in home, should be stored and locked away.
Risk of fall injuries from climbing or riding toys
able to reach and grab dangerous items from counters or stoves
Preventing poisoning for toddlers
Poor taste discrimation allows for indigestion of chemical or other materials
potentially poisonous substances should be stored out of the toddler’s reach, out of their sight, and in a childproof, locked in a cabinet: meds, alcohol, cleaning products, pesticides, wild mushrooms, plants, vape solution and edible cannabis, antifreeze, windshield washer solution, gasoline, kerosene, lamp oil
1 tsp of liquid nicotine is enough to kill a toddler, even skin contact can be dangerous.
Promoting nutrition for toddlers
The child younger than 2 years should not have his or her fat intake restricted
A diet high in nutrient-rich foods and low in nutrient-poor high-calorie foods should be restricted.
Limit juice intake to 4-6 ounces per day and milk to 16-24 ounces per day – with meals
Forcing to eat when not hungry can cause obesity problems
bribing to eat is not healthy. Should drink from normal cup
Ensure adequate intake of iron, vitamin D, calcium and zinc
Toddlers often refuse new foods. Reintroduce foods previously rejected.
The parent decides which foods will be served or offered and the toddler decides how much will be eaten.
promoting nutrtion and obesity prevention for toddlers
Greatest risk factor is having a parent with a high body mass index (BMI).
Calculate and plot the BMI on standardized growth charts. Trends over time may be predictive of the development of overweight or obeseity.
Excessive juice intake (limit to 4 to 6 ounces per day) during meals.
Limit sweets
Offer 3 small meals with 3 nutritious snacks per day
12-23 months: fruit- ½ to 1 cup/day vegetables- 2/3 to 1 cup/day
2-4 years: fruit- 1 to 1.5 cups/day vegetables- 1 to 2 cups/day
Sleep and rest for toddlers
Requirement
18-month-old requires 13.5 hours/day
24-month-old requires 13 hours/day
3-year-old requires 12 hours/day
A toddler should sleep through the night and take one daytime nap.
Transition to a youth or toddler bed when the child is capable of climbing over the rails
Its best to have a standard bed with a nightly routine.
Calm period with minimal outside distractions.
Teeth and gum health
The toddler should have a full set of primary (baby) teeth by age 30 months
Prevent dental caries
Brush with plain water until age 2 years. At 2 years begin using a pea-sized amount of fluoride toothpaste.
Avoid eating between meals and scheduled snacks
Use fluorinated water
Wean from the bottle and avoid using no-spill sippy cups after age 15 months. Can lead to dental cavities
Dental exams should begin at age 1 year.
addressing common developmental concerns for toddlers
Toddler over the age of 2 years is capable of exercising voluntary control
Watch for signs that toddler is ready for toilet teaching
Parents should be calm, positive and non-threatening. Use gentle praise and no reproaches
Temper Tantrums
Ensure the child’s safety and, if possible, leave the child in his or her room or limit the number of onlookers.
“Time-out” may be used to resolve a conflict of wills.
Negativism- normal developmental occurence: avoid asking yes or no questions, offer the child simple choices, do not ask if they “want” to do something, if there is no choice
Regression
Ignore the regressive behavior and praise age-appropriate behavior or attainment of new skills, may occur w/ new baby in house
Signs of being ready to potty train: pull pants up and down,dry all night, announce having to go to bathroom, and when they have to defecate
Tips on discipline for toddlers
Discipline should guide, correct, strengthen, and improve the child’s choices
Nonnegotiable issues include items such as not hurting themselves or others, not destroying property, and not placing themselves in unsafe conditions.
Respect the child as a person • Avoid pity
Be patient, firm but kind • Listen and be attentive
Reward and praise often • Encourage independence
Encourage open expression of feelings • Provide a healthy environment
Ignore negative behavior when safety allows • Model desired behaviors
Use familiar routines when possible • Offer choices
Try to understand the reason for the misbehavior • Maintain control of emotions
Pediatric nursing challenge in toddlers: Pain assessment
FLACC score. Toddler cant do self report pain assessment tool, cant give pain scale number
Common signs of child abuse
Physical abuse
Bruises, welts (may be at different stages of healing)
Signs of multiple fractures at different stages of healing
Lacerations or tears
Cigarette or immersion burns on extremities or buttocks
Head injuries
Swollen, blackened eyes
Sexual abuse
Difficulty walking or sitting
Bruises or bleeding from genitalia
Recurrent urinary tract infections
Symptoms of sexually transmitted illness
Inappropriate sexual behavior
Psychological/Abuse
Excessive anger, aggression
Poor peer relationships
Negativism, loss of pleasure
Low self-esteem, lack of trust
Developmental delays
Withdrawn behavior, regression
Preschoolers
Ages: 3-6. Should be able to bend over and not fall
Preschool child physical growth
Weight—average increase of 5-7 lbs (2.3-3.2 kg) per year
Stature—average increase of 2.5 to 3 in (6.75-7.5 cm) per year
Loses baby fat, gains muscle
Appears more upright and slender
Should continue to follow established growth curves
Preschool physiologic chnages
Neurologic
Spinal cord myelinated by age 3
Allows for bowel and bladder tshort and o be achieved
Respiratory
Alveoli increase in number
Airways increase in size
Cardiovascular
Heart rate decreases
Blood pressure increases slightly
Innocent heart murmur may be heard
HEENT
Eustachian tubes remain short and straight
20 decidious teeth should be present
Genitourinary
Urethra remains short in children, making them susceptible to UTI
Musculoskeletal
Bones increase in length and muscles strengthen and mature
Gross and fine motor skills increase
Developmental theories for preschoolers
Erikson: _Initiative vs. guilt (3 to 6 years)
Piaget: preoperational substages: preconceptual (2 to 4 years) and intuitive phases (4 to 7 years)
Kohlberg: punishment–obedience orientation (2 to 7 years)
Freud: phallic stage (3 to 7 years)
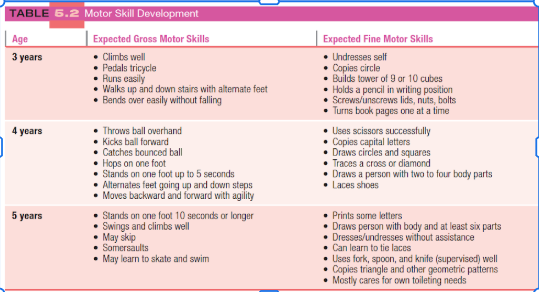
Motor skills for preschool
Communication and language development for preschoolers
Preschoolers use nouns, verbs, and adjectives in their sentences
4-year-olds – can form 3–4-word sentences and who, what, and where question
5-year-olds – can form sentences containing > 5 words with a vocabulary between 2000-2400 words.
Vocabulary increases through repetition and practice
Can express past, present, and future
May have difficulty with word pronunciation with some hesitancy is speech
Gentle correction without criticism
If a child uses an unacceptable word, a simple correction without a fuss is the best response.
Cognitive developement for preschoolers
Magical thinking: Believes thoughts are all-powerful
Animism: Attributes life-like qualities to inanimate objects
Imaginary friend: Creative way to sample activities/behaviors and practice conversation skills
Limited comprehension of word meaning: Left and right, causality, and time
Transduction: extrapolating from one situation to another, even with unrelated events
Centration: ability to focus or center attention on only one aspect of a situation at a time
Explain time in relation to event. Ex. test after lunch.
Emotional and social development for preschoolers
Friendships
Preschoolers learn how to make and keep a friend
Social skills:
Cooperation
Sharing (of things and feelings)
Kindness
Generosity
Affection display
Conversation
Expression of feelings
Helping others
Making friends
Temperament
Influenced by parent’s expectation of child’s behavior
Determines child’s task orientation, social flexibility, and reactivity
Fears
Exhibit variety of fears
Parents should acknowledge child’s fears
Reassurance and reality reinforcement are essential in helping them cope.
Common fears
Fear of dark
Fear of mutilation: a shot, scrape. Bandage helps soothe, to them.
Fear of abandoment: parents shouldnt sneak out, should tell child before leaving.
communicaton skills for preschoolers
4 years old: speaks in complete sentences with adult like grammear, follows a three part command, names common objects and familiar animals, vocab of 1500 words
5 years: can explain how to use something, talks abt past, future, and imaginary events, answers questions that use why and when, vocab of 2100
Growht and development promotion for preschoolers
Building self-esteem
maintaining routine and rituals
Setting limits and remaining consistent with them
Early recognition of signs of developmental delay
Supporting development of self-care activities (e.g., dressing, toileting)
Developing social skills within both the family and the larger society
Signs of developmental delay in preschoolers
4 years old: cant jump/ ride a tricycle, doesnt grasp crayon with thumb and finger, cant use the words “me” and “you” approp, doesnt engage in fantasy play.
5 years old: has little interest in playing with other children, cant build toer of six to eight blocks, cant use plurals or past tense, is easily distracted; cant concentrate on single activity for 5 mins
play in preschoolers
Developing initiative
Sincere encouragement for efforts and accomplishments
Opportunity to decide now and with whom they want to play
Offer a variety of things and activities with both intended purpose and others that allow for imaginative play.
Cooperative play (associative play)
Child must be able to understand limited rules
Have developed some social skills that permit them to begin to share and take turns.
Able to express their desires
Enjoy being with peers and interacting with them during play
Daily nutritional requirements
700 to 1,000 mg calcium
7 to 10 mg iron
19 mg fiber
Fat intake no less than 10% and no more than 35% daily calories
Saturated fats less than 10%
Diet high in nutrient-rich foods
Limited amounts of poor-, high-calorie foods (fruit juices) regular meals with healthy snacks in between
building healthy eating habits for preschoolers
Preschoolers are often erratic eaters!
Small portions on smaller-sized plates and bowls with appropriately-sized utensils
Encourage child to serve self
Allow child to decide when to stop eating (don’t force food)
Snacks should be high quality -lean proteins, whole grain, fruits, veggies, dairy)
Family mealtimes allow parents to model appropriate behaviors at meals and facilitate communication
RIsks of overweight and obesity for preschoolers
Overweight is defined as BMI at or above the 85th percentile and below the 95th percentile for age and sex
Obesity is defined as BMI greater than the 95th percentile for age and sex
According to the CDC, overweight or obese preschoolers “are 5 times as likely as normal weight children to be overweight or obese as adults.”
Consequences of childhood obesity include:
HTN, Hyperlipedemia, insulin resistance
Discrepancies of obesity vary with cultures
Preventing preschooler obesity strategies for preschoolers
Provide meals with the family and in a positive atmosphere.”
Varied diet with plenty of plant- based foods; water should be primary beverage; avoid sugary foods and beverages.
Physical activity – minimum of 60 mins./day of structured of at least 60 mins. to several hours per day of unstructured
“limit media consumption_to 30 minutes per day and do not permit a television in the child’s bedroom.”
Sleep and rest for preschoolers
Need 10-13 of sleep each day
Some children will take 1 nap
Follow a bedtime routine
Nightmares or night terrors are common in preschoolers
Nightmare-scary or bad dream followed by waking up, responsive to soothing, may have difficulty going back to sleep, may remember the dream
Night terrors-child sits up screaming, but is not fully awake; may have ↑ heart rate, ↑ respiratory rate, sweating; rapidly returns to sleep; child does not remember event
May have diff falling asleep
Need to have bedtime, and nightime routine
avoid stim activites before bed
Teeth and gum health in preschoolers
Daily dental hygiene
Provide a small, soft toothbrush
Provide toothpaste with fluoride
Teach the child to not swallow toothpaste
Ensure the child brushes daily in the morning and before bedtime
Show the child how to use a back-and-forth motion while the brush is against the gum line
Foods
Limit high sugar foods
Offer fresh fruits and vegetables daily
Health supervision
Dental visits every 6 months
discipline for preschoolers
Successful discipline results from a loving and nuturing environment in which the child’s self-esteem is fostered with well chosen limits that are consistently enforced.
The use of physical punishment (including spanking) has been associated with adult problems and is the least effect method of discipline.
Parents should anticipate situations that may lead to undesired behavior
Use distraction to change the child’s focus
Discuss misbehavior and explain why it is wrong or unacceptable.
Positive reinforcement for acceptable or desirable behavior
Punishment for undesirable, intentional behavior
Time out – 1 minute for each year (5 mins for a 5-year-old) in a boring corner of the room without distraction.
Removal of a privilege (playing with a favorite toy)
Important to discuss why they are being disciplined
lying with preschooolers
Lying is common
Parents must role-model desirable behavior
Not lie
Remain calm and demonstrate an even temper
Important to determine the reason for the lie prior to punishment
Did the child’s imagination get carried away
Should not punish the child but help them determine real vs. imaginary
To avoid punishment
If the child admits the truth, there should be a reduced punishment
The child must learn that lying is worse than the misbehavior itself.
Important for parents to determine ehy child is lying, to avoid punishment?
sex education and masturbation for preschoolers
ex Education
Before attempting to answer questions
Identify what the child is actually asking
Determine what the child already thinks about the subject
Answer simply, directly, and honestly the information that is being requested only.
Masturbation
Exploration of own genitalia is normal in preschoolers.
Don’t overreact to the behavior. It may increase the frequency
Explain that there are certain rules about this activity and that nudity and masturbation are not acceptable in public
Teach preschoolers that no other person can touch their private parts unless it is the parent, doctor, or nurse checking to see when something is wrong.
Preventing injury with prescholers
Preschoolers display poor judgment related to safety issues making close supervision of them important to avoid accidental injury during this period.
Gun (Ryckman)
Keep the gun unloaded
Keep the gun _locked
Store the ammunition locked and in a seperate place from the gun
Never let children know where the keys are located
Before the child goes to a friend's house,ask the friend's parent whether the family has firearms in the house and how they are stored.
Car
Forward facing car seat until age 4 years whose height meets the size requirement
Booster seat until a height of 145 cm 4’9and age of 8-12 years
The back seat is the safest place for a child to ride.
If a child < 12 years must ride in the front seat due to limited availability in the backseat, deactivate the passenger airbag.
Bicycle
Approved bicycle helmet at any time the child is riding
Correctly sized bicycle:
Balls of the feet should reach both pedals while the child is sitting on the seat and has both ands on the handlebars
Children younger than 5 years should have pedal brakes
Only ride on the sidewalk
Water
Never leave them unattended near pools or other bodies of water.
5-foot gate with latching gate around swimming pool
No diving, unless depth is verified safe by an adult
Life–saving devices readily available around pools
Not allowed to swim in a canal or fast-moving water source
Wear personal flotation device when riding in boats or fishing off riverbanks.
Preschooler pain assessment
wong-baker FACES pain resting scale
Schoolage child
Ages 6-11
Physical growth for schoolage children
Grow an average of 2.5 in per year
Increase weight by average of 7 lb per year
Early on, boys and girls are similar in height and weight
Later, girls may develop faster than boys in height and weight; boys will “catch-up” later
Secondary sexual characteristics begin to appear
Expectations of behavior should be consistent with age, not appearances
Organ system maturation for school aged children
Neurologic system:
Brain and skull grow very slowly; cognitive processes mature
Respiratory system:
Respiratory rates decrease; respirations are diaphragmatic in nature
Cardiovascular system:
Blood pressure increases and pulse rate decreases
Immune system:
Matures to adult level around 10 years old; fewer infections experienced
Gastrointestinal system:
Deciduous teeth replaced by permanent teeth; fewer gastrointestinal upsets; stomach capacity increases; caloric needs are lower, but appetite may increase
Musculoskeletal system:
Greater coordination and strength; muscle still immature and can easily be injured
Genitourinary system:
Bladder capacity increases (age in years + 2 oz)
Prepubescence occurs
Begins in the 2 years before the beginning of puberty with about a 2-year difference in onset between boys and girls
Characterized by the development of secondary sexual characteristics
A period of rapid growth for girls
A period of continued growth for boys
Sexual development in both boys and girls can lead to embarrassment concern over physical appearance, and low self-esteem.
menstrual period ranges from: 9-16
Educate abt body changes to promote comfort
Discuss emotional, social, resposibility, and risk of sexual activity
Gross motor and fine motor skills for schoolaged children
Gross Motor:
Coordination, balance, and rhythm improve
May become awkward as bodies growing faster than able to compensate
Fine Motor:
Hand usage improves
Eye–hand coordination and balance improve
Can write, print words, sew, or build models
Takes pride in activities requiring dexterity and fine motor skills, such as playing musical instruments
Benefits of physical activity for schoolaged children
Cardiovascular fitness
Weight control
Emotional tension release
Development of leadership and social skills
Sensory development for schoolaged children
Hearing:
Hearing screening to identify hearing loss
Avoid exposure to excessive noise to prevent hearing loss.
Vision:
Children should have an eye exam prior to the start of school and then annually
Signs of vision problems
Eye rubbing, squinting
Avoiding reading
Frequent HA
Holding reading materials close
Problems with depth perception or hand–eye coordination
Sports- related eye injuries and eye protection are important in this age group.
Amblyopia/lazy eye: one eye is more near sided than other
language and communication skills for schoolaged children
Vocabulary expands to 8,000 to 14,000 words
Culturally specific words are used
Reading efficiency improves language skills
More complex grammatical forms are used
Development of metalinguistic awareness occurs
Metaphors are beginning to be understood
Emotional and social developmental for schollage children
Temperament: common groups
Easy and adaptable
Slow to warm
Difficult and easily frustrated
Self-esteem development
Face the process of self-evaluation from a framework of either self confidence or self-doubt based on mastery of earlier developmental tasks of initiative and autonomy.
If school-age children regard themselves as worthwhile, they have a positive self-concept and high self-esteem
Emotional and social developmental for schoolage children fears
Age | Fear |
6-7 years | Strange loud noises, ghosts and witches, being alone at night, bodily injury, school |
7-8 years | Dark places, catastrophes, not being liked, physical harm |
8-9 years | Failure in school, being caught in a lie, divorce or separation of parents, being a crime victim. |
9-11 years | Becoming ill, heights, pain, evil people |
Parents should not cater to fears
Relaxation tech should be used to help manage fears
emotional and social developement for schoolage children
Peer relationships
Continuous peer relationships provide the most important social interaction
Learn to respect differing points of view
Peer groups establish norm and standards that signify acceptance or rejection
Teacher and school influences
Transmit values of society and establishes peer relationships.
Important in shaping the socialization, self-concept, and intellectual development of children.
Family influences
Beginning of peer group influences, with testing of parental and family values.
Beginning to strive for independence, but parental authority and controls continue to jmpact choices and values.
Developmental theories for schoolage children
Erickson: industry vs inferiority: interested in: how things are made, success on personal/ social tasks, outside activities, peers, learning
Piaget: concrete operational: learns by manipulating objects, no abstract thinking, understands time
Kohlberg: conventional: acts are wrong because you get punished; behavior is right or wrong.
Feud: Latency: focus on activities that develop social/ cognitive skills
More interested in own group of friends of same gender. More peer relationships vs romantic relationships
Safety issues for schoolaged children
Car safety
As presented in preschooler lecture
Rules of conduct for car rides must be established.
Children younger than 13 years of age should not ride in the front seat of a vehicle with an airbag.
Pedestrian safety
Children younger than 10 years should not be unsupervised pedestrians
Teach safe street and pedestrian practices
Bicycle and sport safety
Bike helmets (required by law in some states, but not in MI)
Helmets, knee and elbow pads for skating or skateboarding
Fire safety
Educate about the hazards of fire
Supervise children while cooking and microwaving food.
Water safety
School-age children should learn how to swim and learn water safety.
Safety precautins to teach children schoolage children
Wear protective equipment.
Observe traffic signals.
Practice water safety: learn to swim, and never swim alone.
Use the buddy system when walking to and from school.
Never talk to nor accept rides from strangers.
Always follow your instincts and avoid peer pressure.
Child maltreatment for schoolage children
Child maltreatment includes physical abuse, sexual abuse, emotional abuse and neglect
Physical abuse refers to injuries that are intentionally inflicted on a child and result in morbidity or mortality.
Sexual abuse refers to involvement of the child in any activity meant to provide sexual gratification to an adult.
Emotional abuse may be verbal denigration of the child or occur as a result of the child witnessing domestic violence.
Neglect is defined as failure to provide a child with appropriate food, clothing, shelter, medical care, and schooling.
A history of childhood abuse is associated with the development of anxiety and depressive disorders, suicidal ideation and attempts, and alcohol and drug use.
Child abuse for schoolage children
Assessment
Screening questions for children
Are you afraid of anyone at home?
Who could you tell if someone hurt you or touched you in a way that made you uncomfortable?
Has anyone hurt your or touched you in that way?
Questions for parents
Are you afraid of anyone at home?
Do you ever feel like you may hit or hurt your child when frustrated.
Child abuse-physical exam for schoolage children
Perform a gentle but through physical examination, using a soft touch and calm voice.
Observe the parent-child interaction, noting fear or an excessive desire to please.
Inspect the skin for bruises, burns, cuts, abrasions, contusions, scars, and any other unusual or suspicious marks.
Observe for inflammation of the oropharynx (may occur with forced oral sex).
Inspect the anus and penis or vaginal area for bleeding or discharge (which may indicate sexual abuse)
child abuse- nursing care in schoolaged children
Nursing Management
Refer suspected cases of neglect or abuse to Child Protective Services
When abusive activity is identified in the hospital, notify the social services ad risk management departments. Notify the charge nurse and may need to get assistance from the hospital security.
Provide consistent care to the abused child by assigning a core group of nurses to help foster a therapeutic relationship and trust in adults.
Role model appropriate caretaking activities to the parent or caregiver.
Call attention to normal growth and development parents helping to manage realistic expectations.
If a child is removed from the home and placed in foster care, provide the education necessary to assume the child’s care.
Nutrition assessment for schoolage children
Check height and weight compared to previous measurements; assess BMI for age
Nutrition history including a 24-hour recall of what was consumed
Inquire about family meals and the social aspects of eating including who prepares the meals
Solicit from both parent and child
Identify any knowledge gaps relating to nutrition
nutrtional needs in schoolage children
Needs vary based on age, gender and activity level
Needed calories decrease while appetite increases
Increased body fat occurs earlier in girls than boys
Diet preference established in preschool years persist
Children also need:
Fiber: 25 g for 4‐ to 8‐year‐olds; 26 to 31 g for 9‐ to 13‐year‐olds
Moderate to vigorous exercise for 60 minutes per day
Daily fruits and vegetables
Whole grain breads and cereals
Non-fat (skim) or low-fat milk
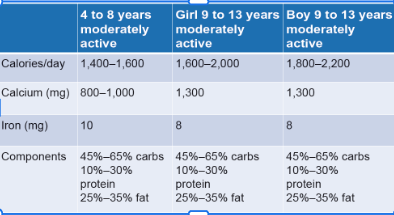
NUTRITIONAL NEEDS OF THE AVERAGE SIZED SCHOOL-AGE CHILD (AGE GROUPS)
Obesity management for schoolage children
Children and adolescents aged 6 years or older with a BMI >=95 should receive comprehensive, intensive behavioral interventions. Often multidisciplinary teams
Psychology sessions (targeting both parents and child), group sessions, information on healthy eating, safe exercising, and reading food labels.
Incorporate behavior change techniques such as problem solving, monitoring diet and physical activity behaviors, and goal setting.
Selecting healthy foods; regular meal planning ahead of time
Engaging in an active lifestyle; incorporating exercise into the daily schedule.
Family lifestyle changes are crucial and should not only focus on changing the child’s habits.
Promoting sleep and rest in schoolage children
10-12 hours of sleep required
Should have predictable bedtime expectations and wake-up times
Children may need help in winding down to promote sleep
Night terrors and sleepwalking may occur but should resolve by age 8 to 10 years
Developemntal concerns for schoolage concerns
Television and video games (setting limits on both the content and amount of time)
Too much time in front of a screen can lead to aggressive behavior, less physical activity, and obesity.
Healthy People 2030 recommend to limit screen time in children 2-17 years to <2 hours per day
Bullying
Defined s repeated negative actions by one or more persons against chosen victims.
There are usually three groups involved: the bully, the victim, and the bystanders.
Signs that a child is being bullied include sleeping problems, irritability, poor concentration,, problems with schoolwork, missing belongings or money, and frequent unexplained psychosomatic complaints- physical presentation of psychological stressors; stomach, head hurting-
Cyberbullying refers to usie of the Internet, phone or other technology to repeatedly harass or taunt persons.
School violence for school age children
School violence can be defined as any harm, whether physical or psychological, that is directed toward schoolchildren and their property
Two common factors known to contribute to school violence
Breakdown in communication in the home and school
Easy availability of weapons.
Signs that indicate a behavior may lead to violence
Difficulty getting along with peers
Outbursts of temper, violence directed toward pets
Decreased productivity in the home or at school
Sleeping or eating problems
Social isolation
Preoccupation with violent movies or video games
Promoting appropriate discipline in schoolage children
Children learn the natural and logical consequences of discipline
Parents should teach children rules established by the family, values, and social rules of conduct
Discipline should be consistent, applied fairly and focus on the development of the child
Positive acknowledgment of positive behavior are more likely to encourage those positive behaviors and promote development
Natural consequence: not discipline; Ex: leave bike in drive way, gets ran over by car.
Logical consequence: discipline.
Cultural influences on growth and development for schoolage children
Habits
Beliefs
Language
Religious customs
Values (Family vs. Peers)
Why is body water important
Medium in which body fluids are dissolved 2. Essential for cellular function 3. Where metabolic reactions take place
Distrubution of body fluids
Total Body Water (TBW) ◼ Intracellular fluid (ICF) – fluid contained within the cells ◼ Extracellular fluid (ECF) – fluid outside the cells ◼ __________ – contained within the blood vessels ◼ __________ – surrounding the cell ◼transcellular __________ – contained within specialized body cavities: cerebral spinal fluid, sinovial fluid, plural fluid
Infants and young children have a greater need for water and are more _vulnerable to alterations in _fluid_____ and electrolyte balance. • Infants have a greater fluid intake and output relative to size. • Water and electrolyte disturbances occur more frequently and more rapidly. _infant and young children_adjust less promptly to those alterations.
Loss can occur thru: heat, Respiratory
Total body fluid
Body water percentage for weight varies with age
Newborns highest percentage water: 75% total body water
ECF is 50% for a newborn and about 30% for toddlers
Decreases with increasing age – towards adolescence and in adults
45% total body water
Maintenance fluid requirements
FORMULA: Up to 10 kg 100 mL/kg/24 hr
11- 20 kg 1000 mL + 50 mL/kg for each kg above 10 kg
> 20 kg 1500 mL + 20 mL/kg for each kg above 20 kg
Normal range for urine specific gravity?
Normal range 1.016-1.022
In the absence of kidney disease. What does: low specific gravity indicate? Fluid volume excess
high specific gravity indicate?
Urine output
Reduced bladder capacity in infancy (30 ml in newborn).
Expected urine output in the infant and child is 0.5-2ml
General consideration is at least _1ml/kg/hr
One year old voids about 400 – 500 ml per day
Infant and toddlers void _9-10 time/day. By age 3 the average number of voids is the same as an adult
Adolescent average urine output is about 800 – 1,400 ml per day with an adult average number of voids 3-8 times/day.
Physiological Differences Place Infants at Risk for Overhydration, Dehydration, and Electrolyte Imbalances
Increased body surface area: allows larger quantities to be loss htru their skin, longer GI tract another source of fluid loss, especially if they have diarrhea
Increased metabolic rate
Kidneys are functionally immature at birth: have harder time concentrating urine
Higher fluid requirement: ingest and excrete a greater amount of fluid per kilogram of body weight: maintenance requirement include both water and electrolytes
COnditions that decrease fluid needs
CHF, SIADH, Kidney disease, Postoperatively Mechanical ventilation Increased intracranial pressure
Fluid overload s/s
_increased___________urine output ◼ Edema (_infants may have puffy eyelids_________ may have _weight gain__________) ◼ Elevated venous pressure ◼ Hepatomegaly ◼ Slow, bounding pulse ◼ __weight gain_____________ ◼ Lethargy ◼ Increased spinal fluid pressure ◼ CNS manifestations (seizures, coma) ◼ __full__ fontanel (<18 mos.) ◼
Laboratory findings: decreased specific gravity decreased hematocrit decreased serum electrolytes
Edema
Edema results from anything that
1. Alters the retention of sodium, such as renal disease or hormonal influences
2. Affects the formation or destruction of plasma proteins, such as starvation or liver disease.
3. Alters membrane permeability, such as nephrotic syndrome or trauma Edema may be localized to a small or large area, or it can be generalized.
Types of edema
Peripheral edema or localized or generalized palpable swelling of the interstitial space. :infants may have puffy eyelids as a sign of edema. Can be a sign of fluid volume overload related to excessive IV fluid infusion
Ascites, or the accumulation of fluid in the abdominal cavity (usually associated with renal or liver abnormalities)
Pulmonary edema, which occurs when interstitial volume increases
Cerebral edema, which is a particularly threatening form of edema caused by trauma, infection or other etiologic factors, including vascular overload of hypotonic solution
Overall fluid gain, which is especially seen in patients with kidney disease.
Nuring care for fluid overload
Management and Nursing Care ◼fluid restrictions _____________ adherence ◼ Administer _diuretics____________ ◼ Monitor vital signs ◼ Monitor neurologic signs, as necessary ◼ Monitor daily weights_________________ ◼ Review electrolyte labs ◼ Implement _seizure precautions______________
fever_\
tachypnea _
v/d
burns_
High output kidney failure
Diabetes insipidus
DKA_
Radiant warmer (preterm infant)
Phototherapy (infants)
Postoperative bowel surgery
Gastric suctioning
Dehydration comparison chart
Dehydration lab findings
Blood: ↑ hematocrit, Variable serum electrolytes, ↓ serum bicarbonate, ↑ BUN, ↑ serum osmolality ◼
Urine ↑ specific gravity
Dehydration- nursing care
Provide replacement of fluid losses: Oral replacement solution or IV fluid bolus
Provide maintenance fluid and electrolytes
Measure fluid intake and output
Monitor urine specific gravity
Monitor body weight
Monitor serum electrolytes
Pediatric maintenance IV fluids
The AAP recommends the use of isotonic solutions with adequate potassium chloride and dextrose for maintenance IV fluids in children: Dextrose: 5%, Sodium:
0.9 % NaCl (Normal Saline): Isotonic solution – Current recommendation, As maintenance IV solution may increase risk of hypernatremia & metabolic acidosis
*Concentration of NaCl is determined by clinical status ◼
Potassium: 20 mEq KCl/L = 10mEq/500mL: Do not hang an IV solution with K+ until urine output has been established
Electrolytes- Potassium
Major electrolyte in intracellular fluid
Function: neuromuscular_ & _cardiac__________
Nursing Considerations: Normal range _3.5-5.0_mEq/L: False increases can occur from specimen collection & dehydration
Patient physical assessment: Hypokalemia: most commonly caused by K+ loss though the use of some diuretics, diarrhea, or excessive sweating, or deficient dietary intake.
S & S: irregular heart rhythmm and cardiacdysrhythmias, general discomfort or irritability, muscle weakness, paralysis
Hyperkalemia: most commonly caused by renal failure or overaggressive treatment of deficiency.
S & S: heart rhythm and ECG changes tingling in the extremities, weakness, numbness, paralysis
Cardiac monitoring should be considered
Electrolytes- sodium
Major extracellular fluid electrolyte
Function: neuromusclar________________ & __fluid management_____________ ◼
Nursing Considerations: ◼
Normal range is _135-145___________mEq/L ◼ Physical assessment ◼
Hyponatremia can be caused by SIADH, subarachnoid hemorrhage, brain tumor, meningitis, or encephalitis ◼
S & S : general _fatigue_________, __weakness________, nausea, headache, confusion, seizure, coma, death ◼
Hypernatremia results from excessive Na+ intake or retention with excessive loss of water from diarrhea, diuretics, vomiting, sweating, heavy respirations or severe burns.
S & S: signs of _dehydration_________, twitching, _irritability____________, delirium, fatigue, weakness, nausea, headache, confusion, seizure, coma, death
Consider implementing _seizure precautions________________________
Why is pH so important in the body’s function?
Every metabolic reaction that takes place in the body is controlled by enzymes. ◼ They are very specific and operate within very specific environmental conditions involving temperature and narrow ranges of pH. What is pH? ◼ A gauge of ________________________________ What is normal pH of arterial blood? ◼ ________________for adults and children ◼ ________________for infants and children
Acid base balance
Metabolic activities produce acidic products. ◼ Ketone bodies ◼ Phosphoric acid ◼ Carbonic acid ◼ Lactic acid
All are regular metabolic outcomes
acid base regulation
Respiratory System: Removing CO2 (with deep, rapid breathing) ◼ Retaining CO2 (with shallow, slower breathing) ◼ Renal System ◼ Reabsorb CO2 (correction of acidosis) ◼ Excretion of CO2 (Correction of alkalosis)
ABG- normal
pH ◼ adults and children is 7.35 - 7.45 ◼ infants and children < 2 yrs. is 7.32 – 7.49 PCO2 (partial pressure of carbon dioxide) ◼ adults and children 35-45 mm Hg ◼ infants and children < 2 yrs. is 26-41 mm Hg HCO3 (bicarbonate) ◼ adults 21-26 mEq/L ◼ Newborns and infants is 16-24 mEq/l PaO2 (partial pressure of oxygen) ◼ Adults 80-100 mm Hg ◼ Newborns 60-70 mmhg