4) Aqueous and Vitreous
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
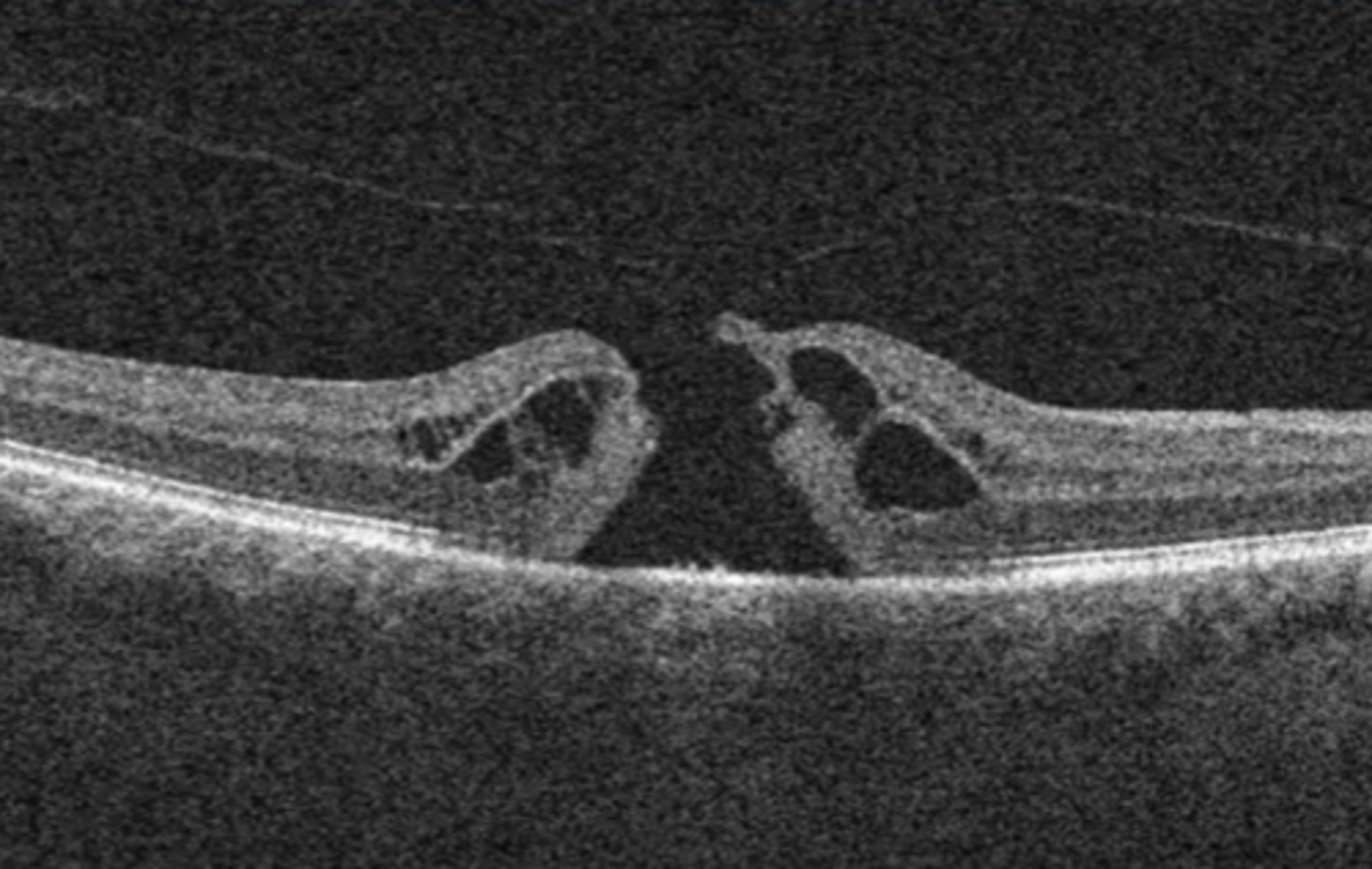
anterior chamber angle
structures from POSTERIOR to ANTERIOR:
-Iris
-Ciliary body (CB)
-Scleral spur (SS)
-Trabecular meshwork (TM)
-Schwalbe's Line (SL)
I Can See The Line
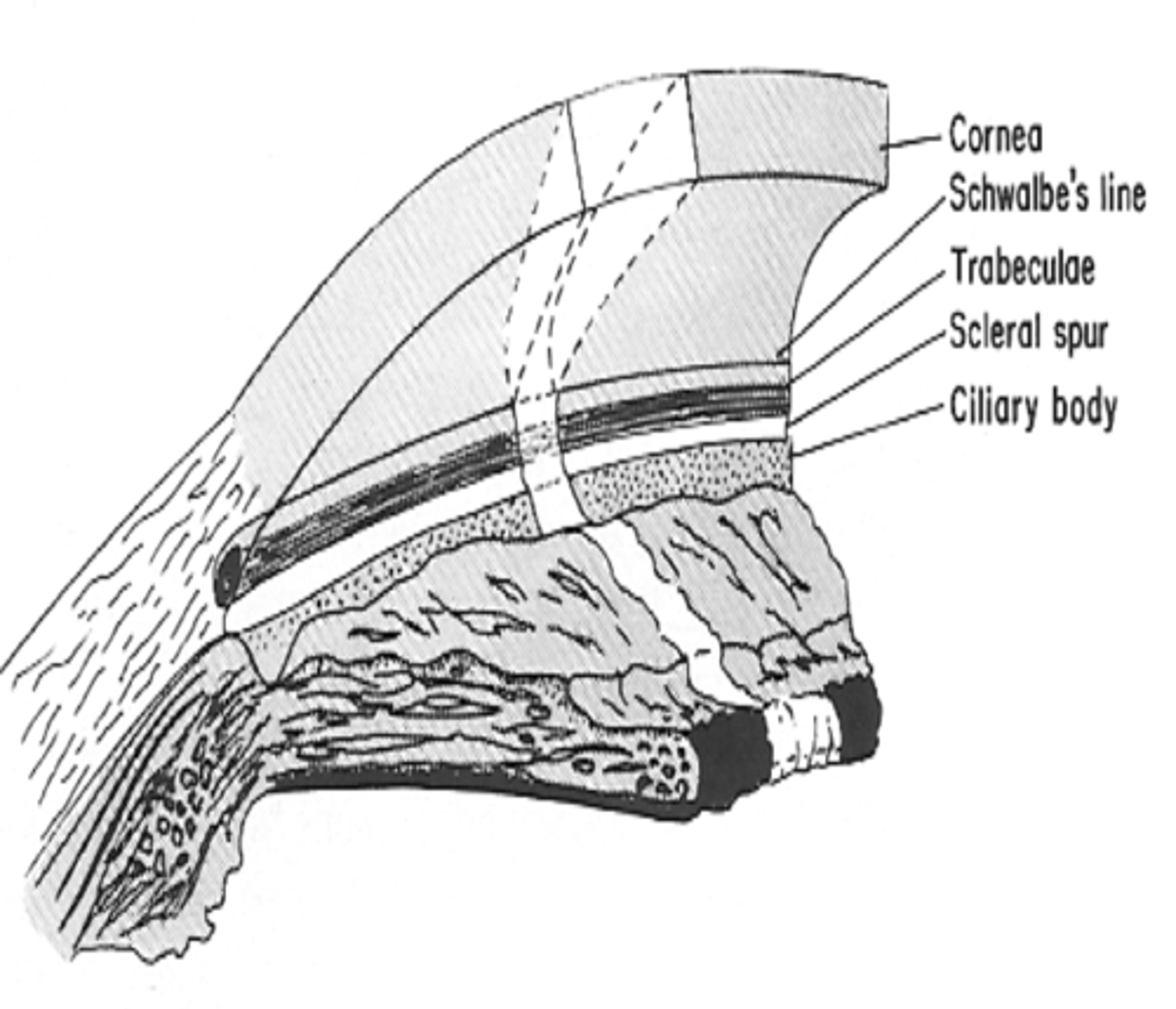
scleral spur (SS)
determines pathway of outflow for aqueous humor.
above SS: conventional (trabecular/SC).
below SS: unconventional (uveoscleral).
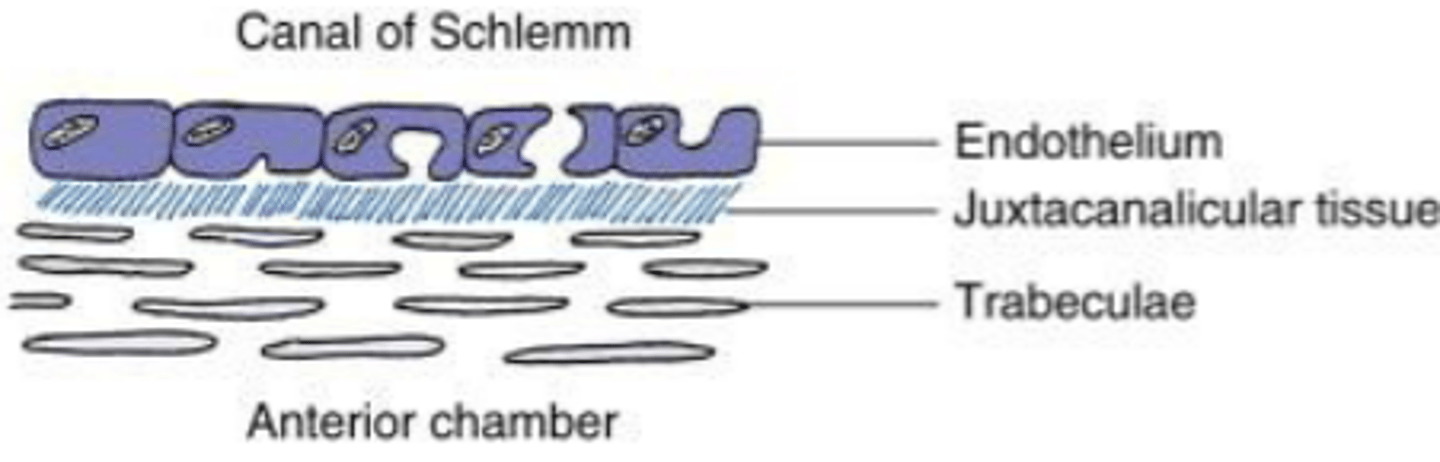
trabecular meshwork (TM)
open latticework with flat, perforated sheets.
apex: termination of Descemet's membrane
-fewer sheets
base: at scleral spur.
-more sheets
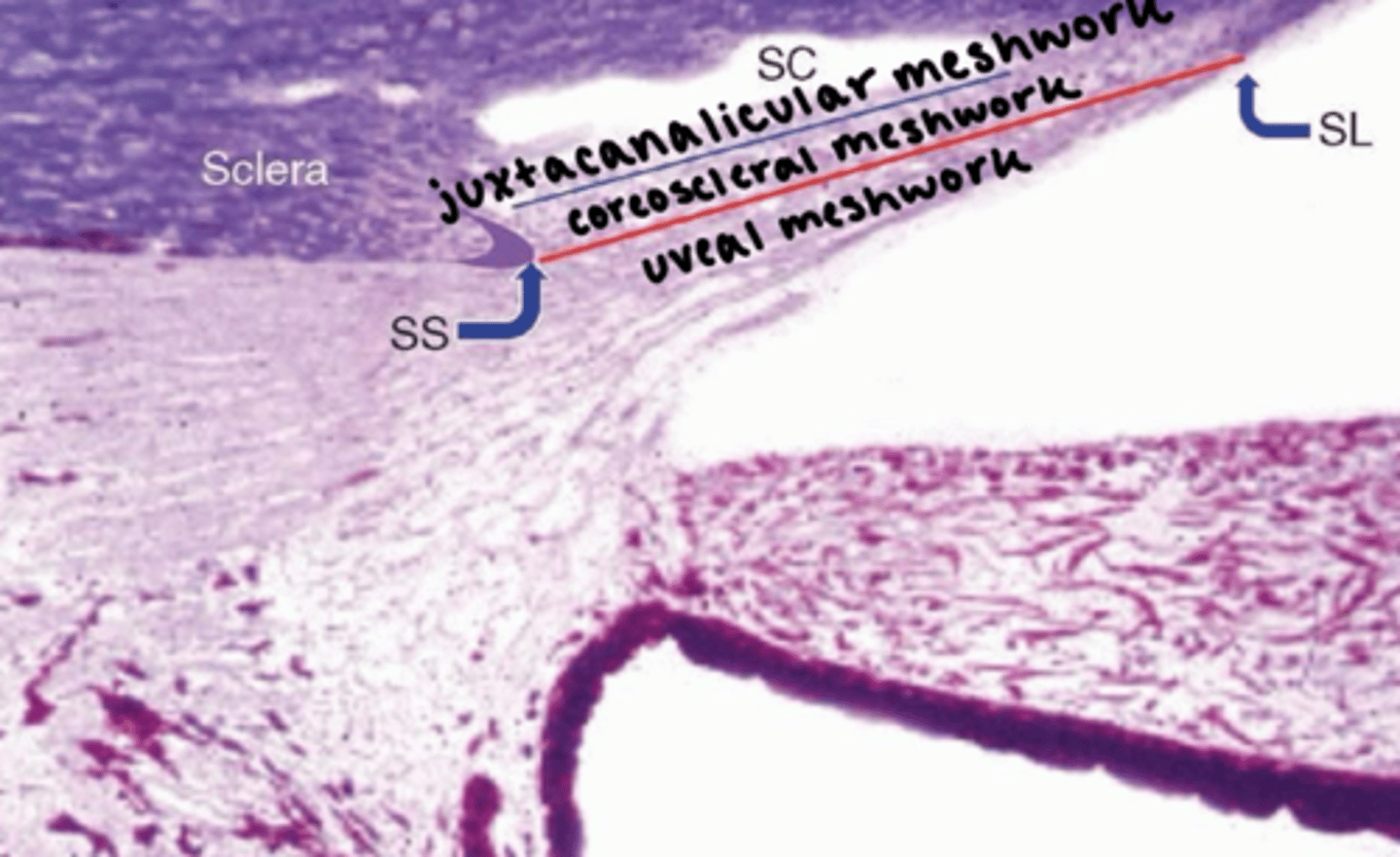
two divisions:
1. uveal meshwork
2. corneoscleral meshwork
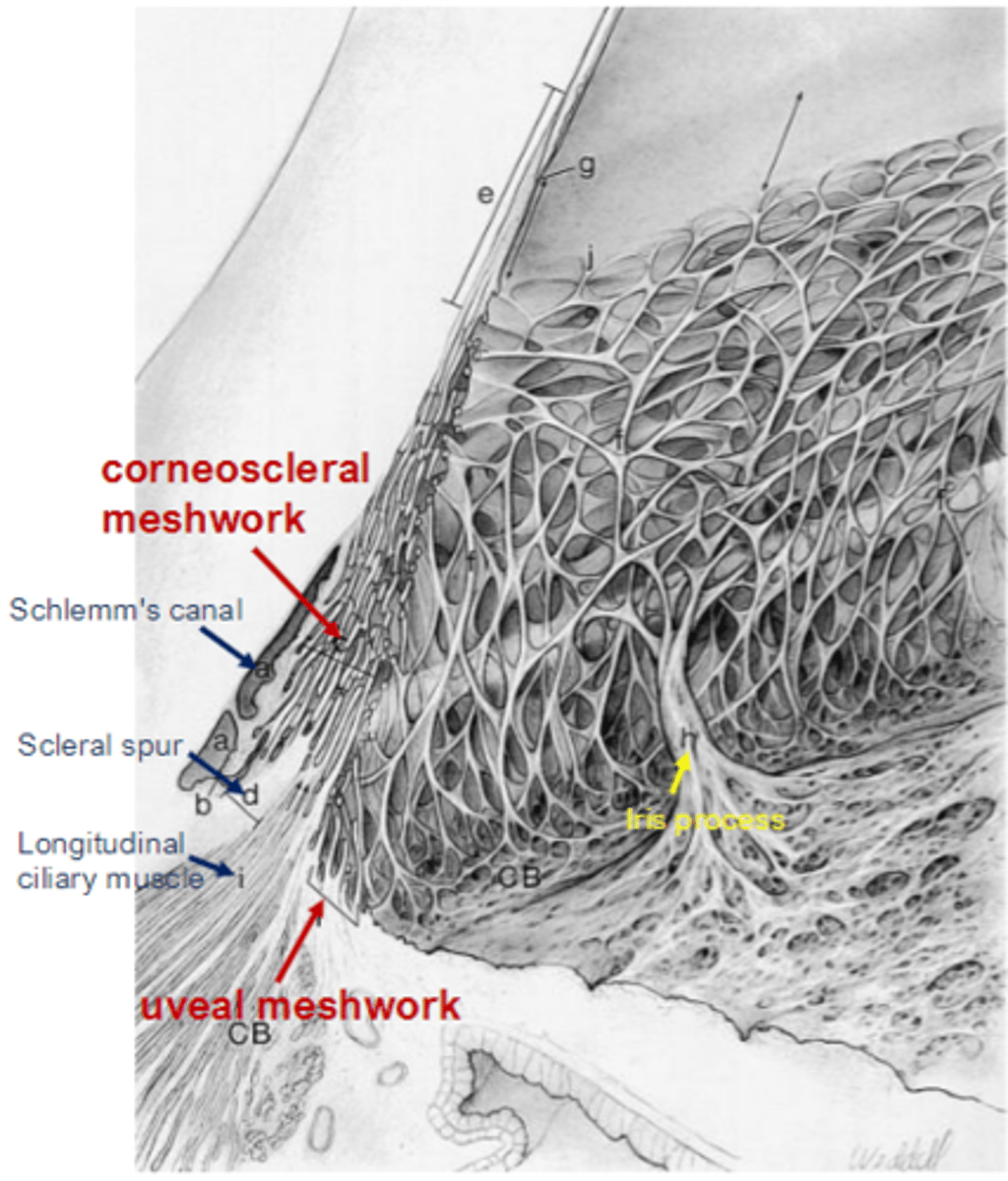
uveal meshwork
closest to anterior chamber.
cord-like with large pores.
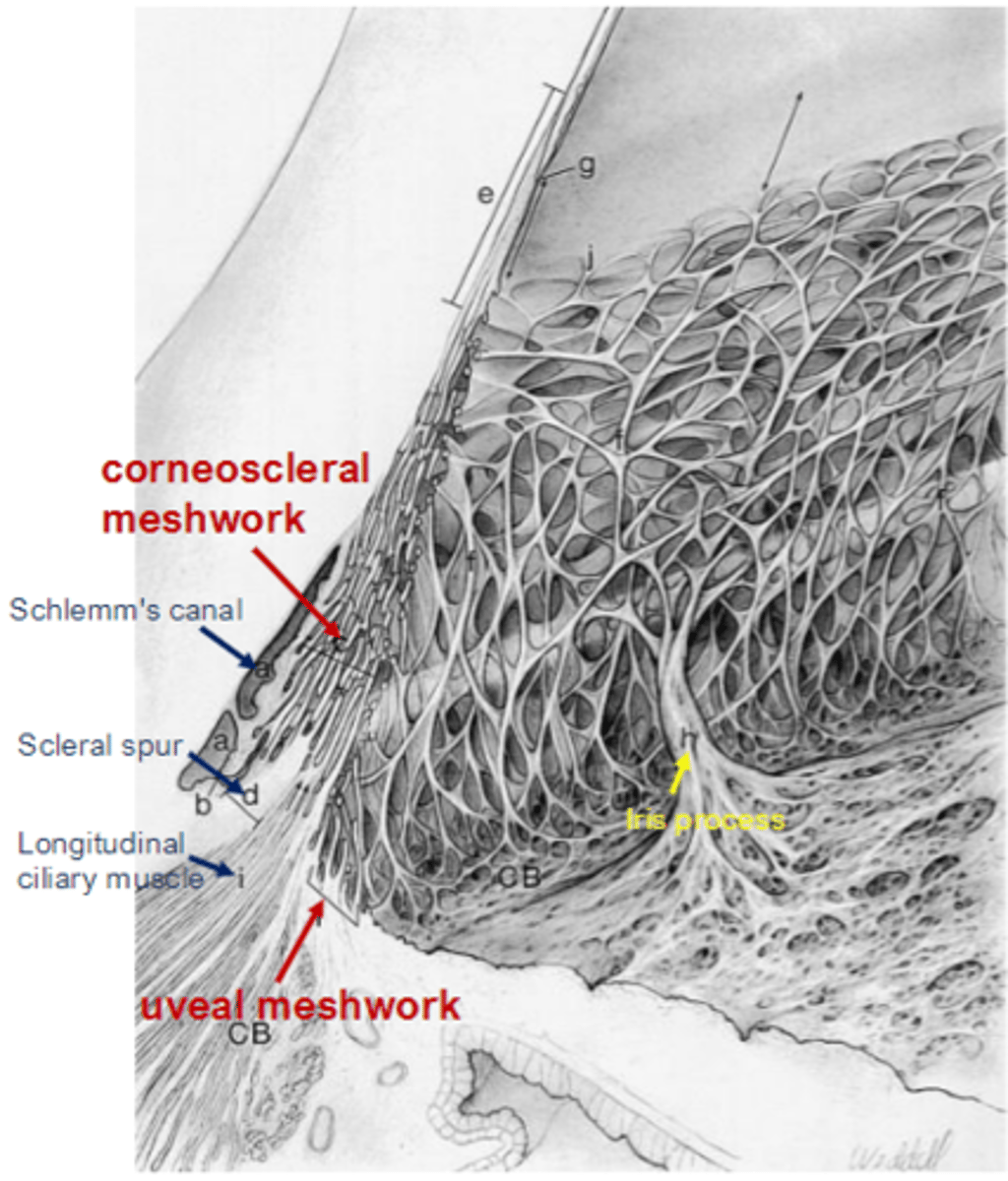
corneoscleral meshwork
attaches to the scleral spur.
sheet-like with medium pores.
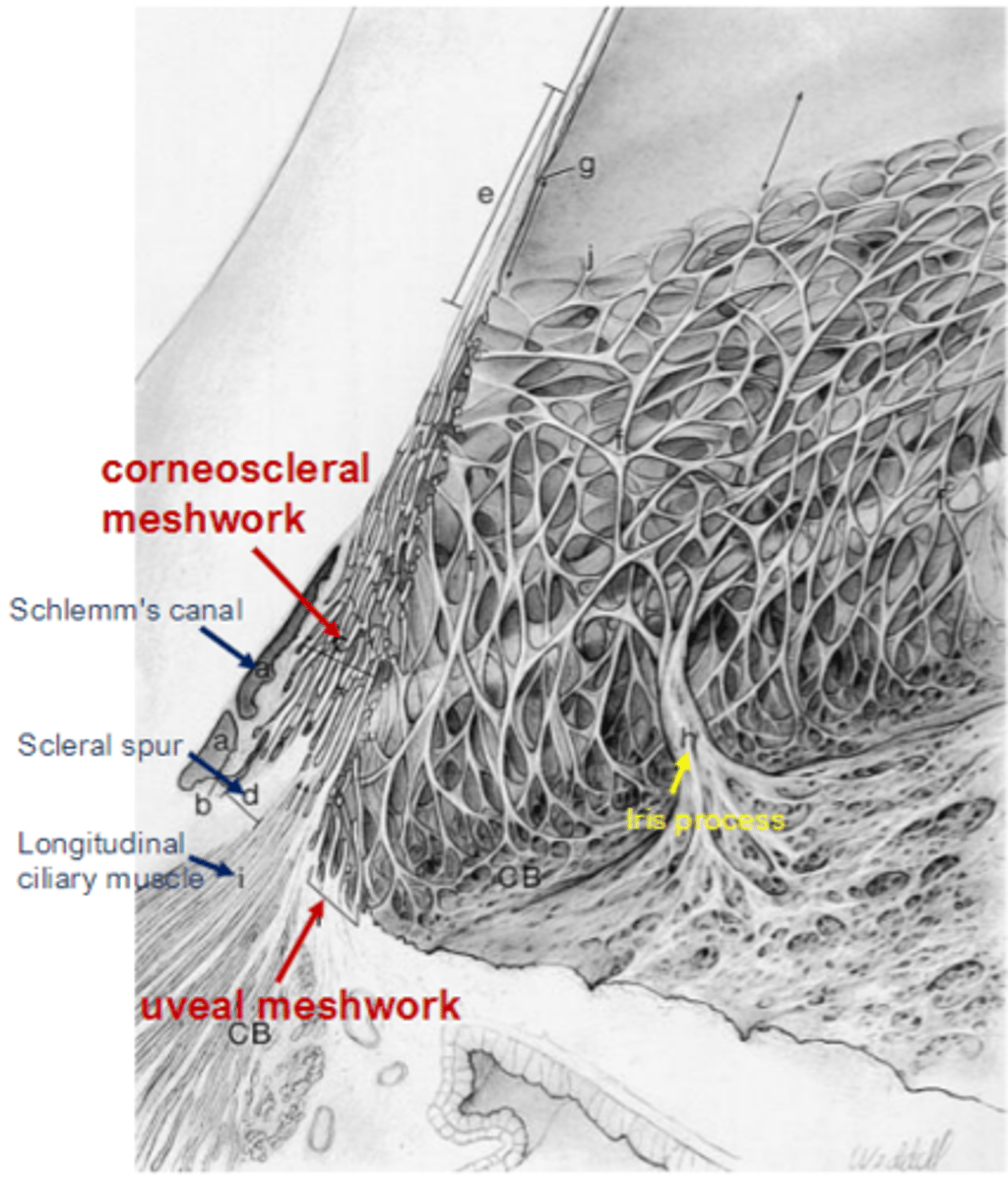
juxtacanalicular connective tissue (JCT)
contains the 3 S's:
-Schlemm's canal
-Scleral spur
-Schwalbe's line
small pores.
most resistance (problems with JCT can increase IOP).
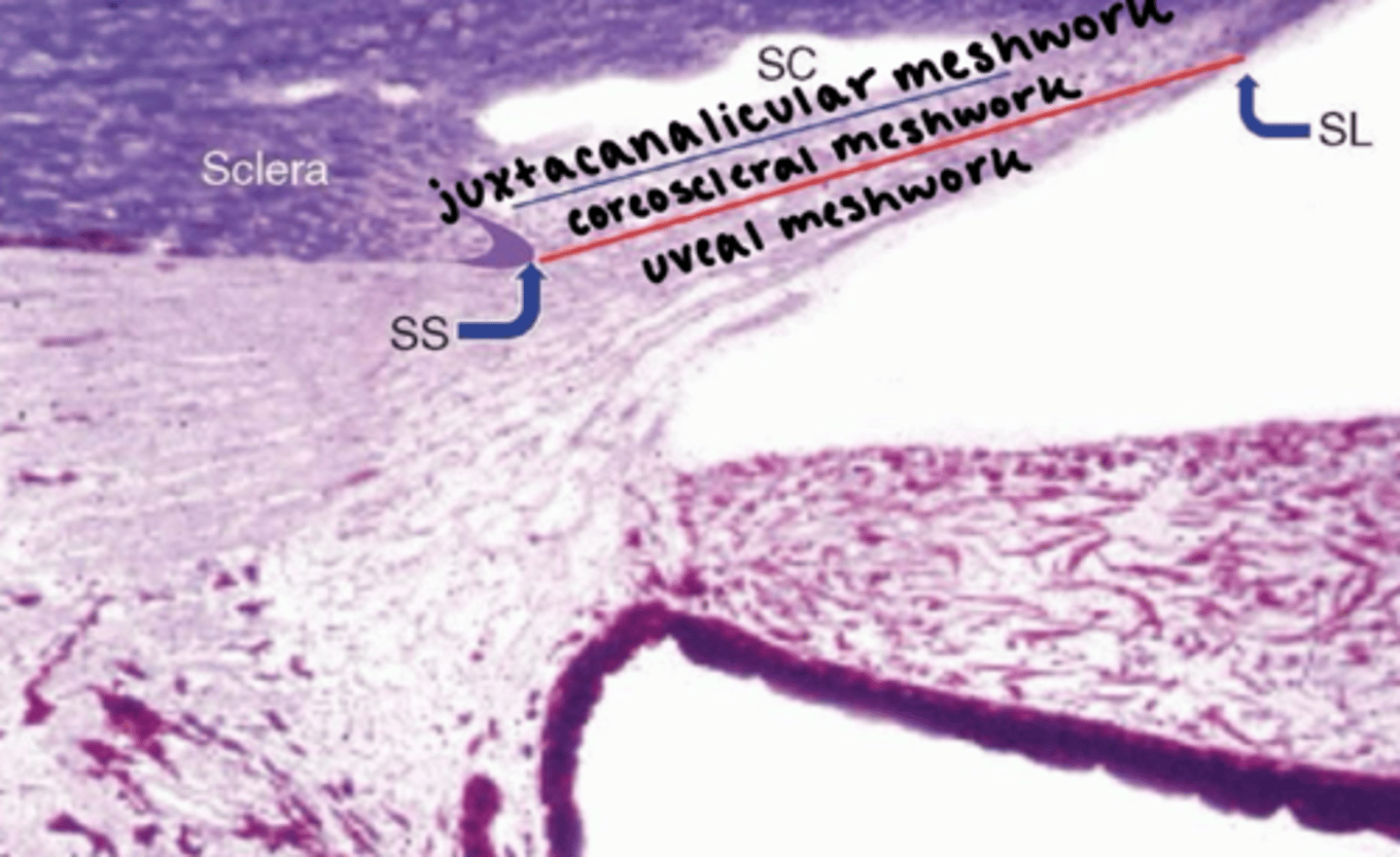
Schlemm's canal
outer to TM, anterior to SS.
lumen is lined with endothelial cells.
continuous endothelium, discontinuous basement membrane.
contains pressure-dependent "giant vacuoles."
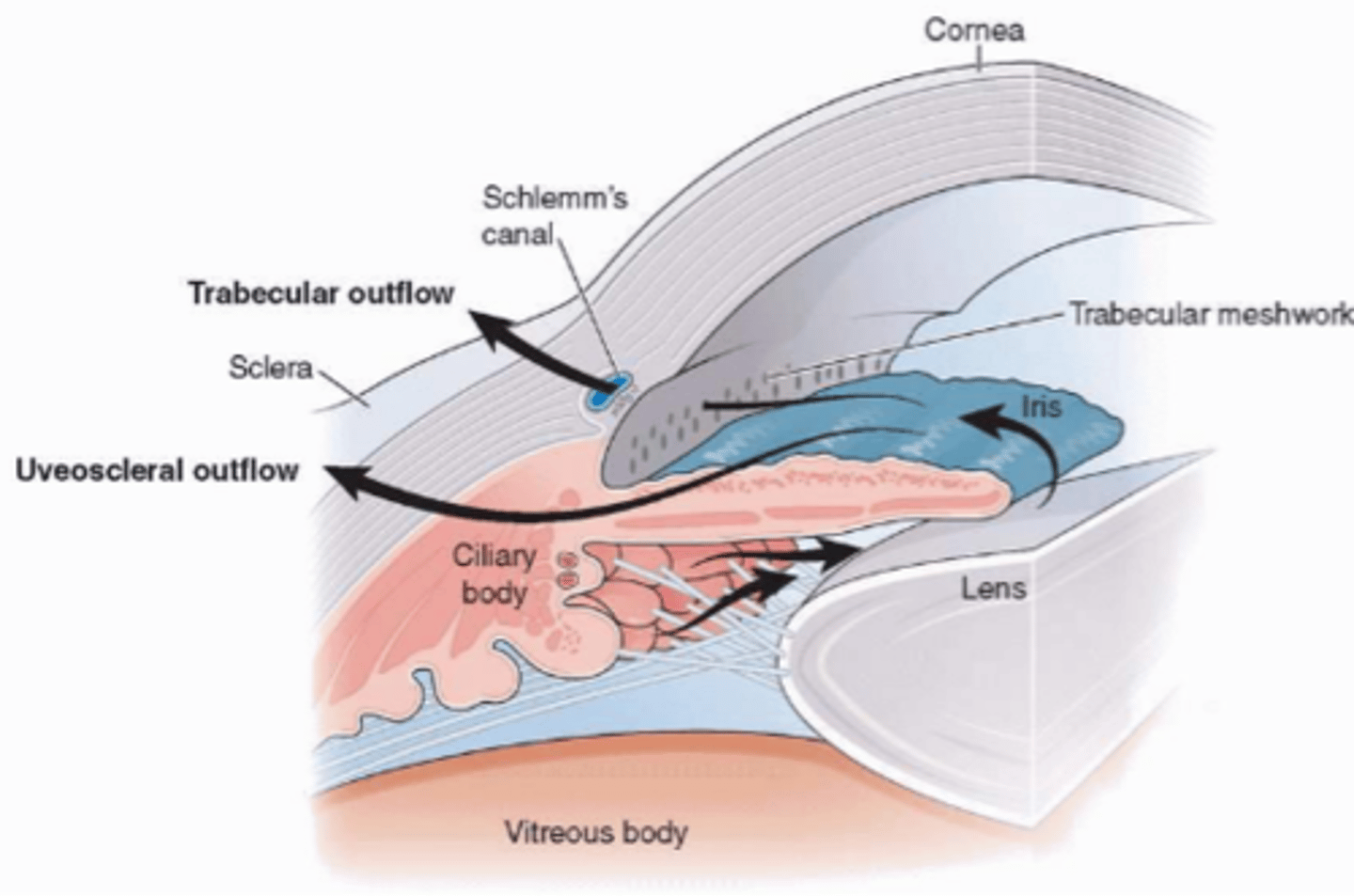
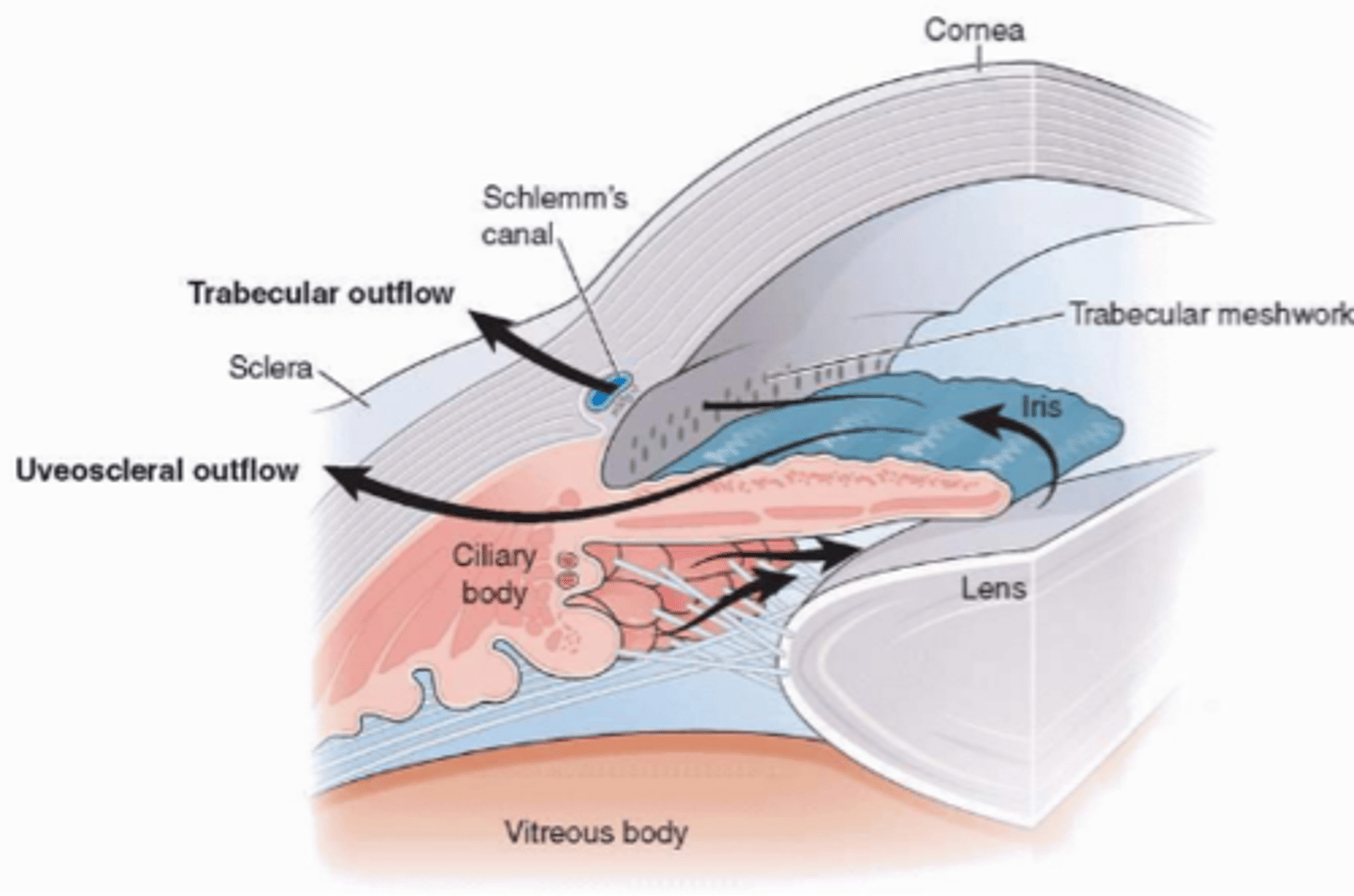
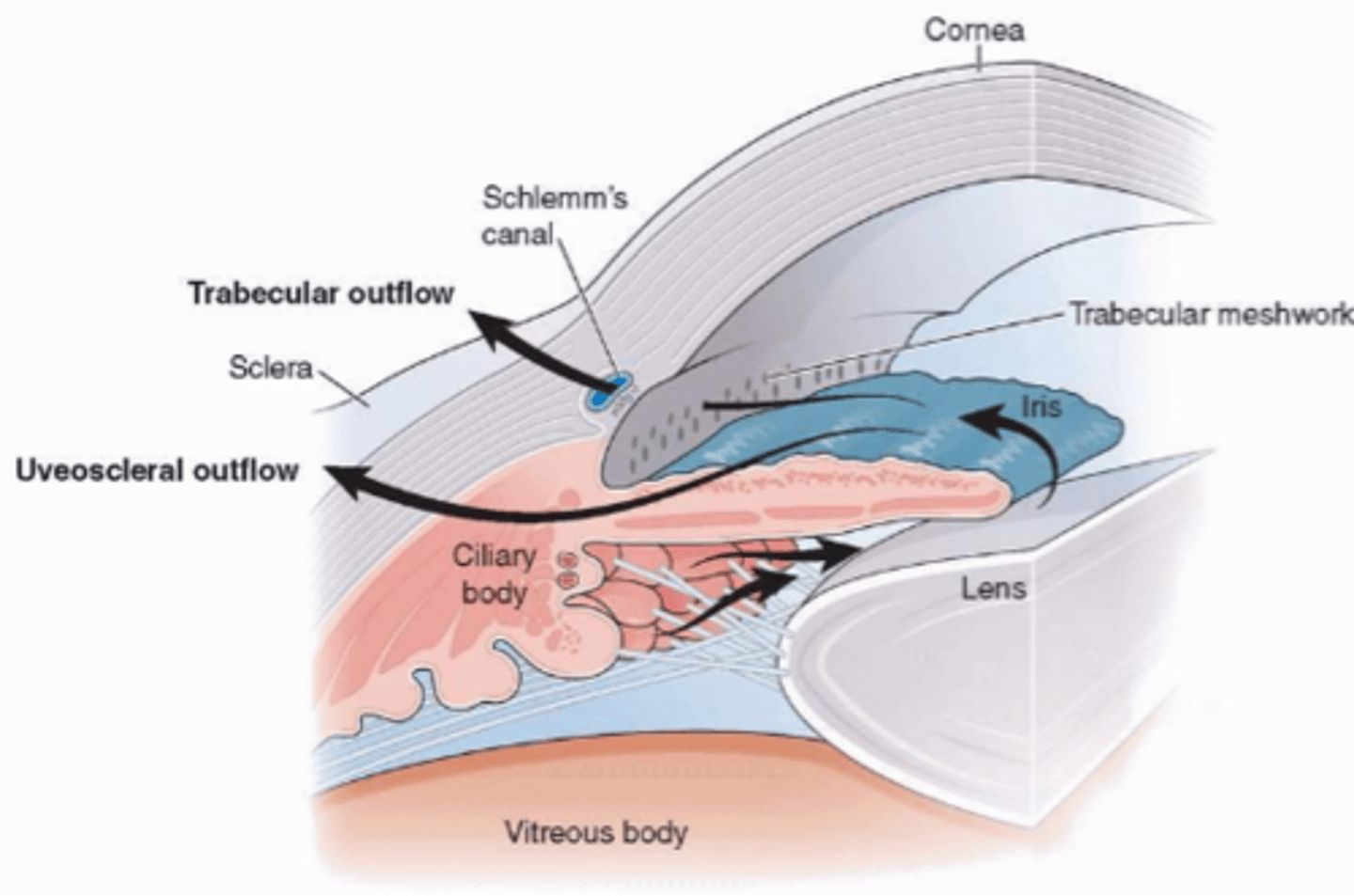
aqueous flow
1. aqueous produced in the pars plicata of ciliary body.
2. secreted into the posterior chamber.
3. travels into anterior chamber via pupil.
from here, aqueous will choose one of two pathways:
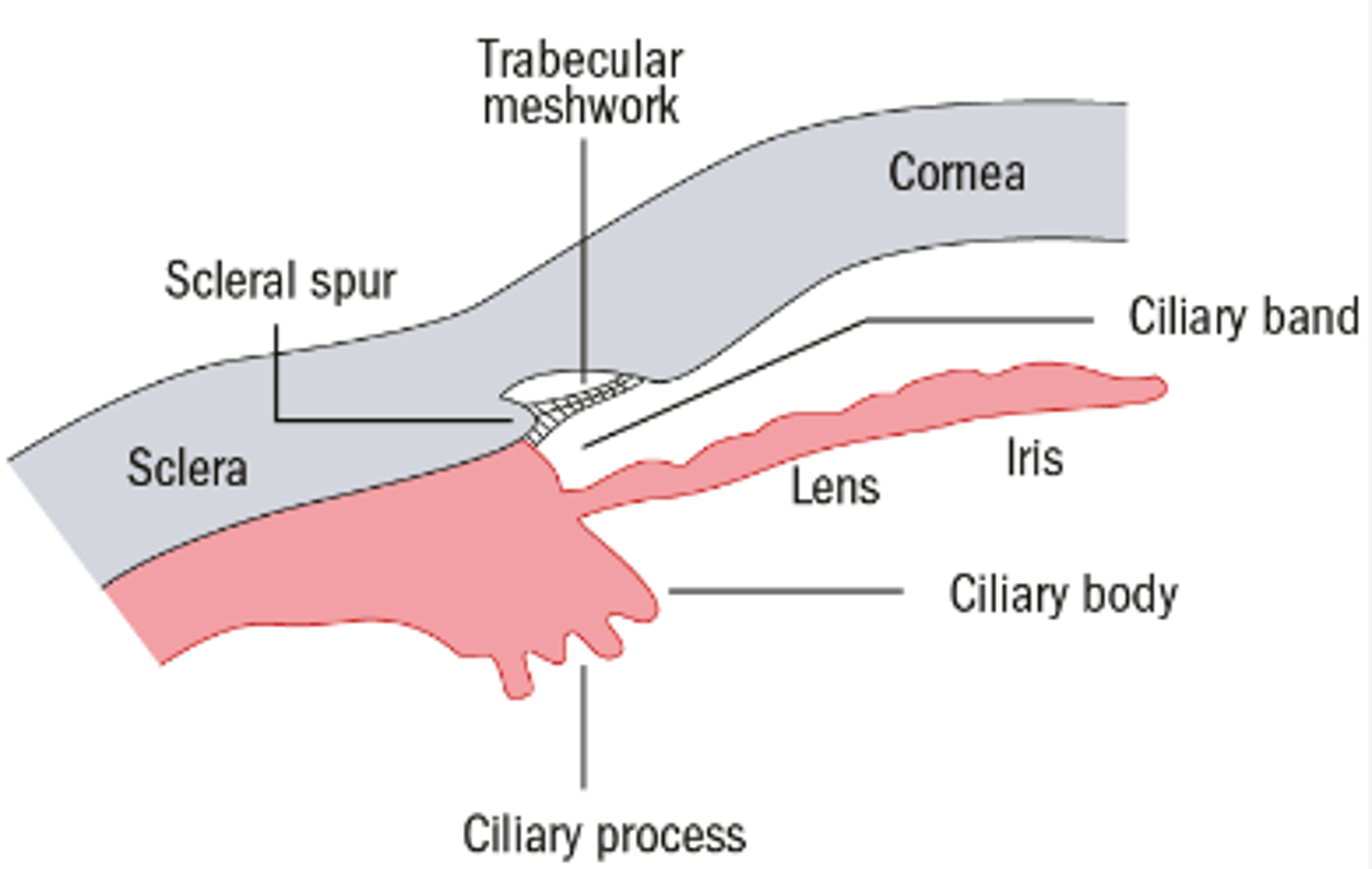
1. uveoscleral/unconventional outflow
2. trabecular/conventional outflow
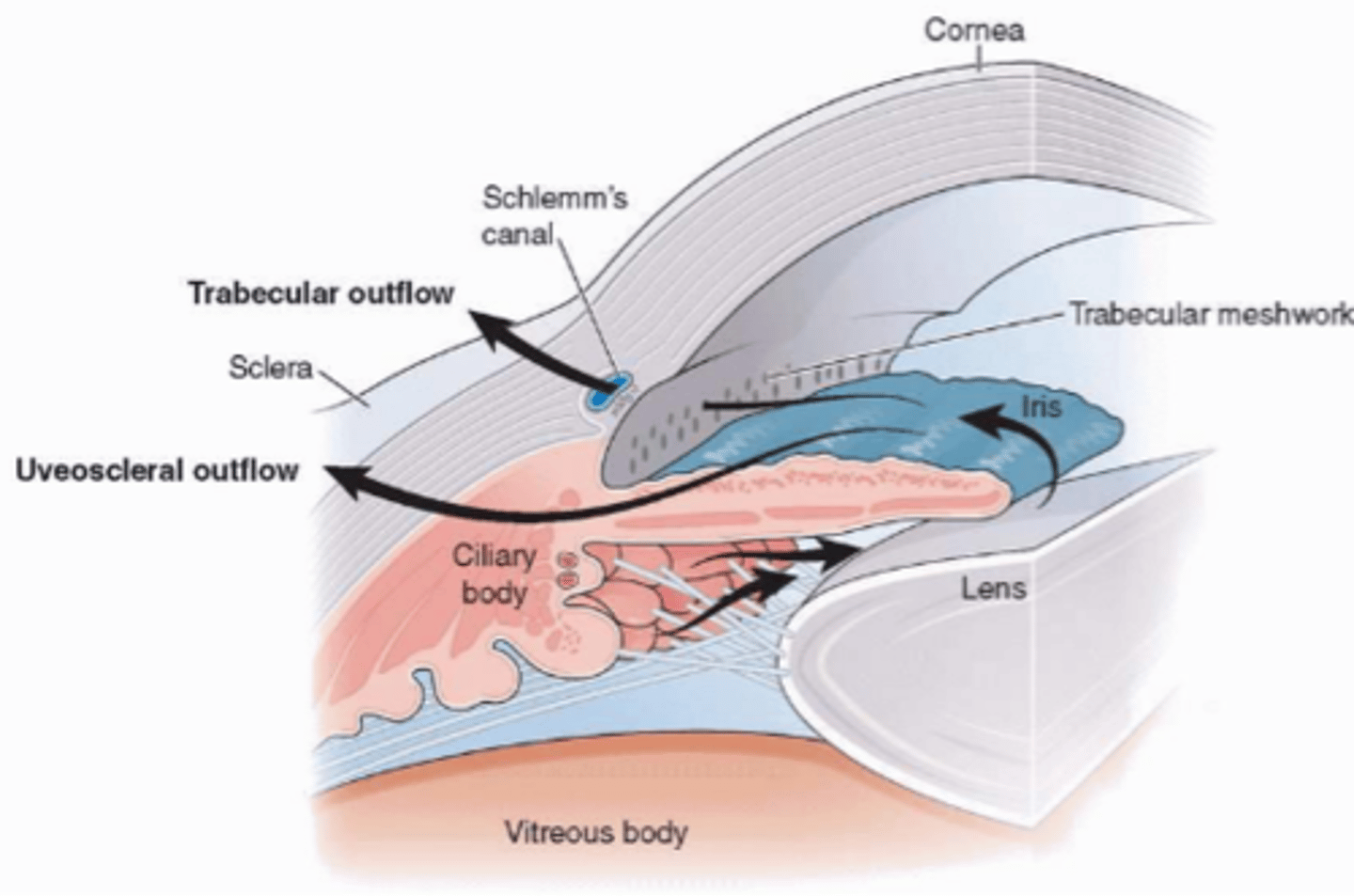
what determines whether aqueous humor will enter the trabecular pathway or the uveoscleral pathway?
the position of the scleral spur.
above SS: trabecular/conventional outflow
below SS: uveoscleral/unconventional outflow
what drives the movement of aqueous?
convection currents.
the corneal is cool, the iris is warm.
aqueous flows up along warm iris.
uveoscleral outflow
unconventional pathway of aqueous outflow (below SS).
only a small amount of aqueous takes this pathway.
route:
1. uveoscleral meshwork
2. ciliary body
3. suprachoroidal space
4. sclera OR the anterior ciliary and vortex veins.
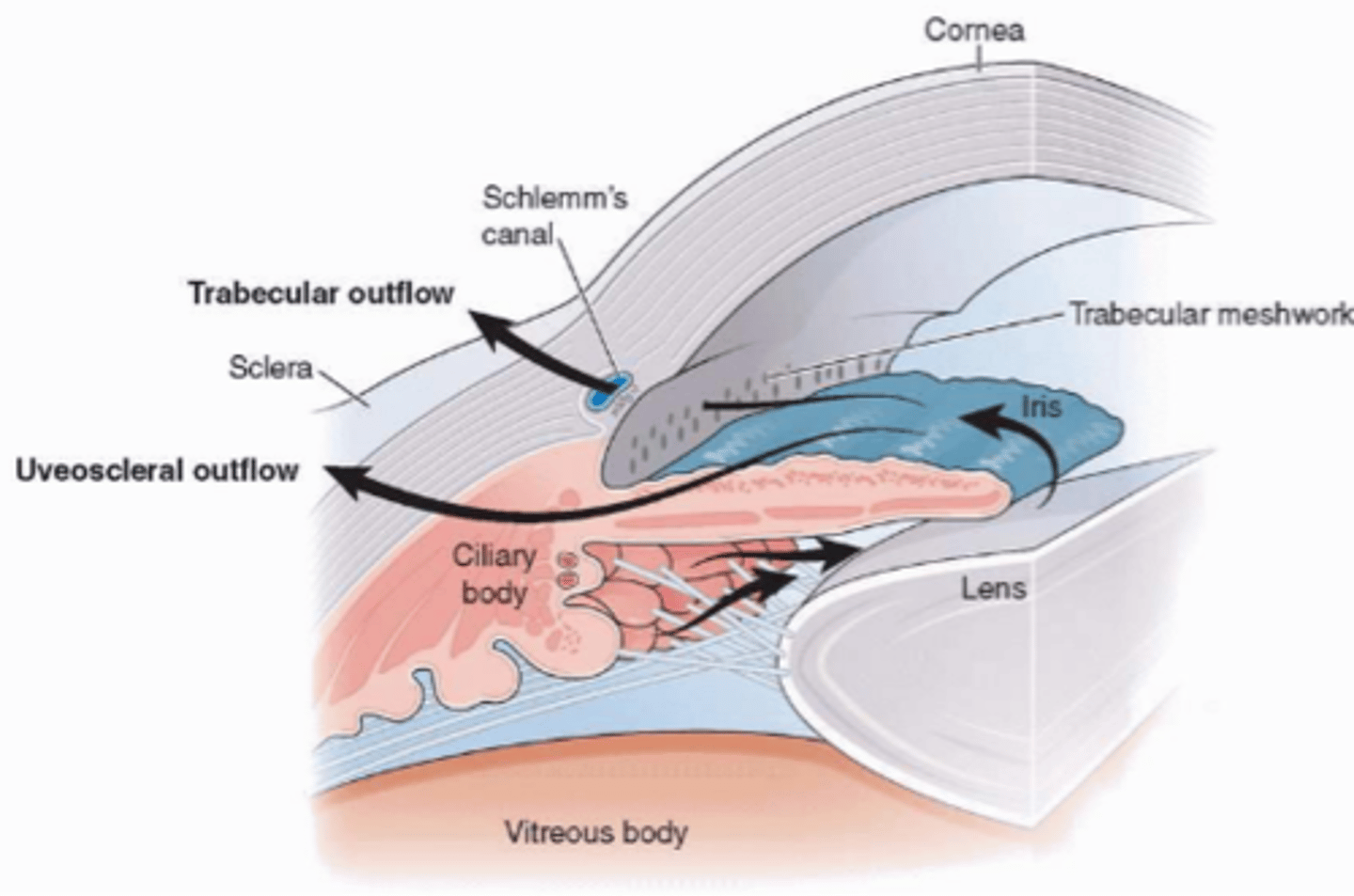
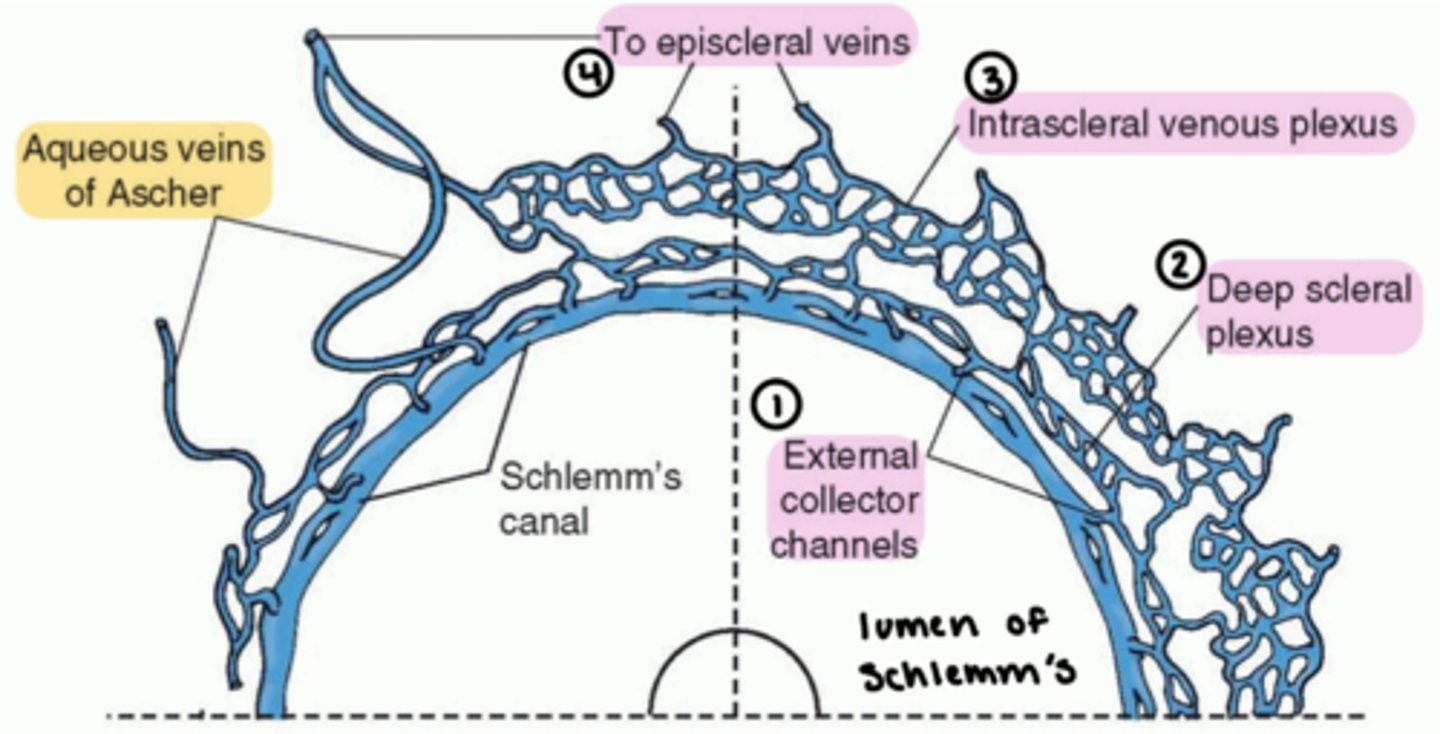
conventional outflow
trabecular pathway of aqueous outflow (above SS).
a greater portion of aqueous takes this pathway.
route:
1. uveoscleral meshwork
2. corneoscleral meshwork
3. JCT
4. Schlemm's canal (giant vacuoles)
5. external collector channels
6. deep scleral plexus
7. intrascleral venous plexus
8. episcleral veins
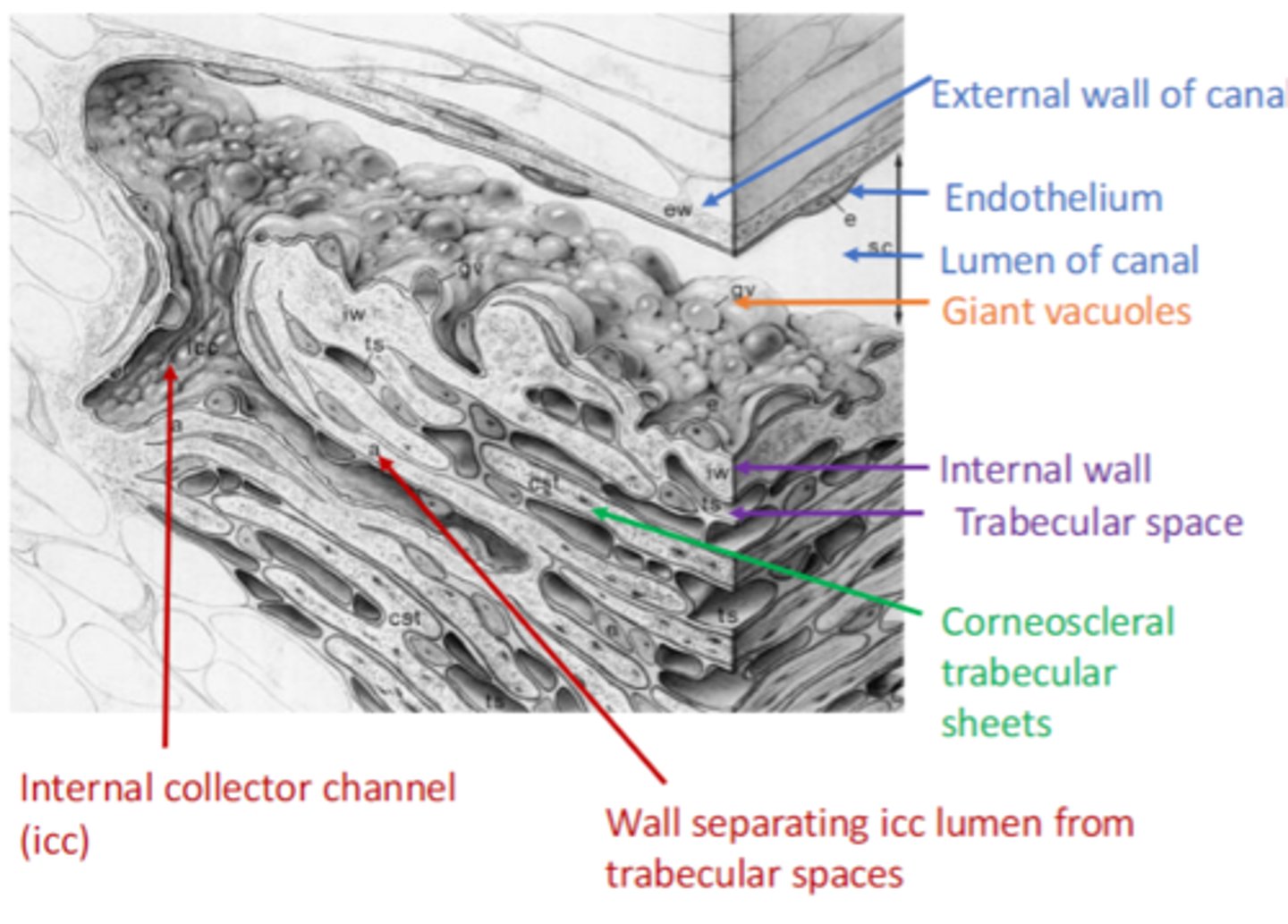
giant vacuoles in Schlemm's canal
endothelial cells lining the inner wall of the canal contain giant vacuoles.
ensures that aqueous outflow via the conventional pathway is transient, unidirectional, and passive.
-aqueous flows only into the canal.
cellular factors can increase the permeability of this endothelium.
internal collector channels (of Sondermann) (icc)
increases the surface area of Schlemm's canal.
the distal outflow pathways beyond Schlemm's canal
5. external collector channels.
6. deep scleral plexus
7. intrascleral venous plexus
8. episcleral veins
10% of patients have Aqueous veins of Ascher:
-bypasses this tortuous pathway.
-goes straight from Schlemm's canal to episcleral veins.
aqueous and intraocular pressure (IOP)
faucet = ciliary body
drain = outflow
the faucet and drain need to be matched.
if there is increased IOP, it is usually due to the outflow (drain).
which aqueous outflow pathway is unaffected by IOP? which is affected?
uveoscleral/unconventional pathway is unaffected by IOP.
conventional/trabecular pathway is affected by IOP.
factors affecting IOP
-resistance
-accommodation
how does resistance to outflow affect IOP?
resistance to outflow can elevate IOP.
there is normally little resistance to aqueous passage through TM (unless pigment or debris is accumulated).
however, the JCT has the highest resistance.
so, the location of JCT can affect IOP.
how does accommodation affect IOP?
fibers of the scleral spur, ciliary muscle, and TM are connected.
therefore, ciliary muscle contraction during accommodation can alter TM spaces and elevate IOP.
aqueous flow equation
flow in (aqueous production) = flow out (aqueous drainage).
for example: increased resistance reduces flow out, leading to increased IOP.
measuring IOP
a tonometer is used to measure IOP.
two types on Tonometry:
1. Indentation tonometry
2. Applanation tonometry
Indentation tonometry
less commonly used.
measures the depth of indentation made by a known weight.
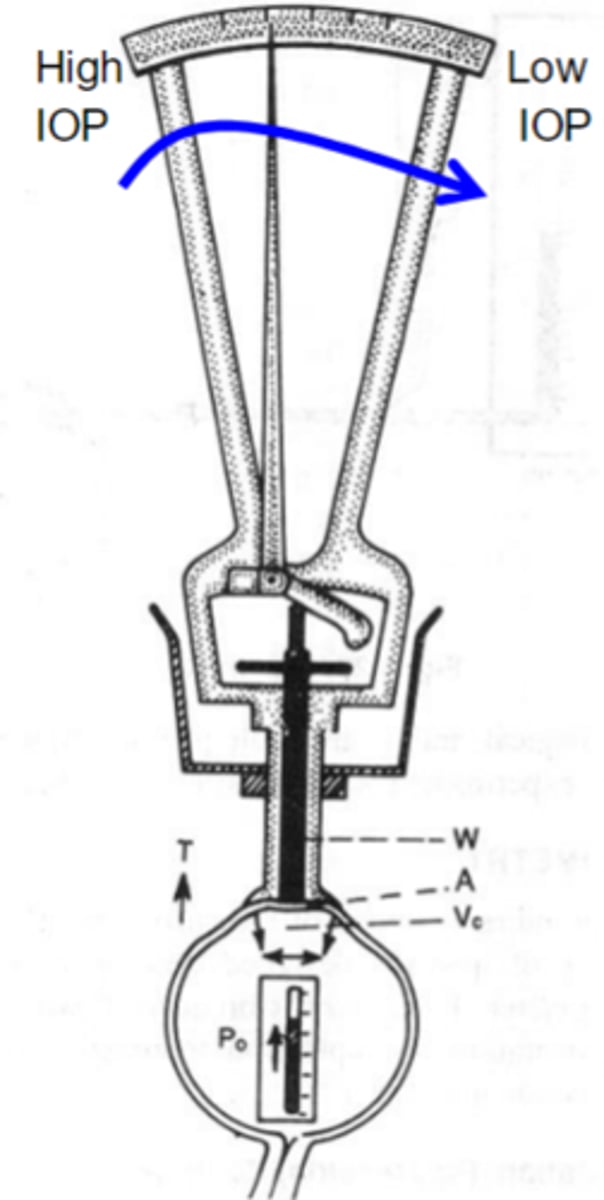
Applanation tonometry
most widely used and accurate.
measures the force required to flatten a known area of the corneal surface.
types of Applanation tonometry:
-Goldman tonometry
-Non-contact tonometry (NCT) or Air puff.
Goldman tonometry
gold standard (most accurate).
based on Imbert-Fick law.
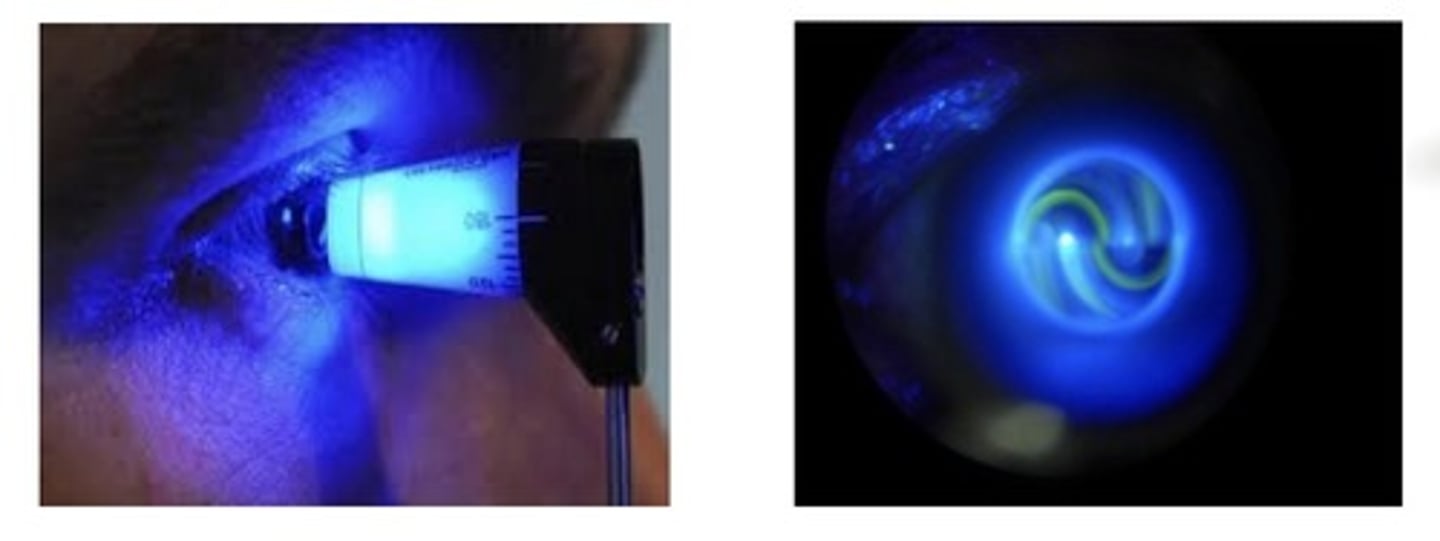
Non-contact tonometry (NCT)
Air puff.

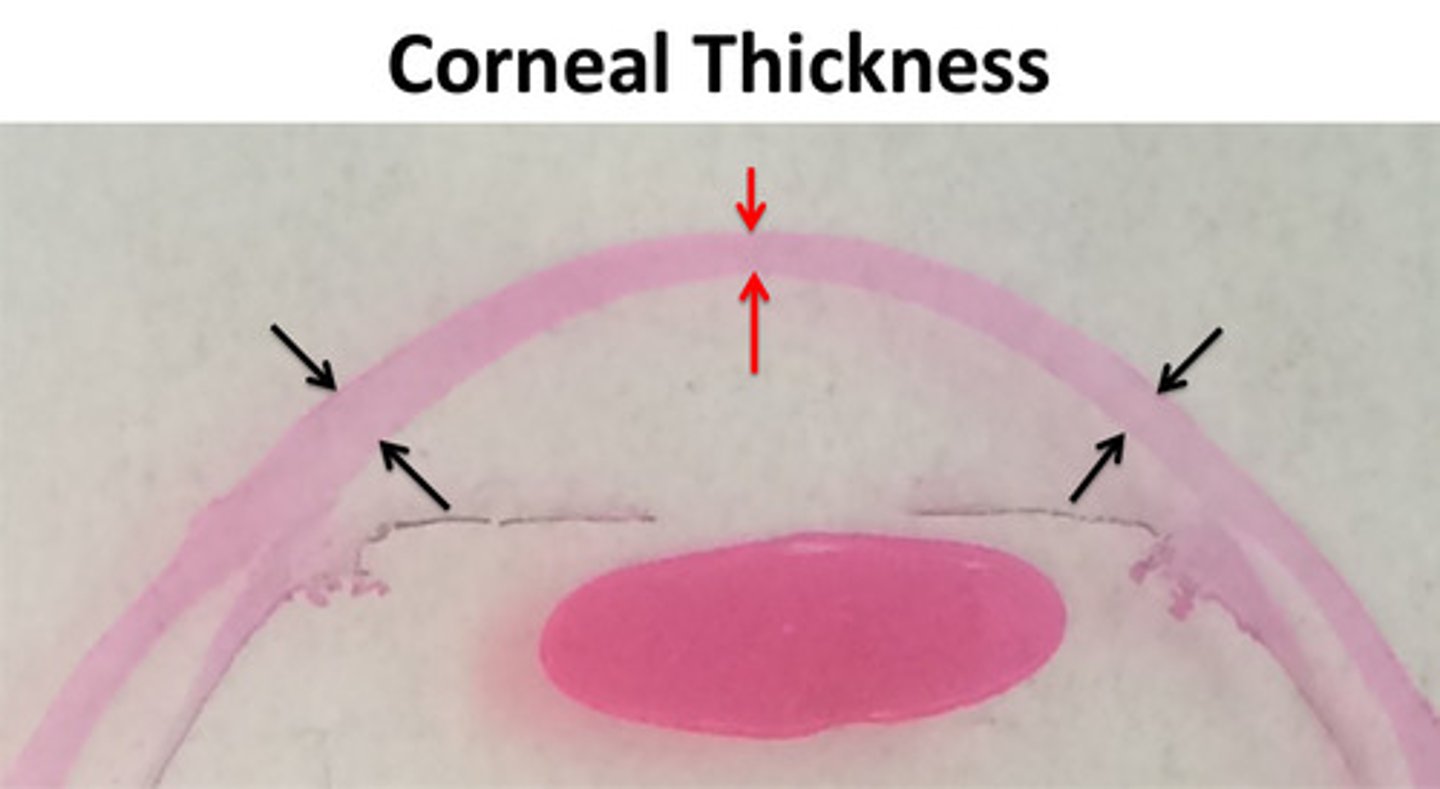
what are measurements of Applanation tonometry affected by?
central corneal thickness (CCT)
increased CCT: artificially high IOP.
decreased CCT: artificially low IOP.
drugs that affect IOP
-cholinergic agonist (Pilocarpine)
-carbonic anhydrase inhibitors
-prostaglandins
-rho-kinase inhibitors (Rhopressa)
cholinergic agonist (Pilocarpine)
causes iris sphincter and ciliary muscle to contract.
iris sphincter contracts: miosis
ciliary muscle contracts: opens TM
not well tolerated.
carbonic anhydrase inhibitors
inhibits enzymes needed for ionic transport.
not well tolerated.
prostaglandins
enhances uveoscleral outflow.
well tolerated.
rho-kinase inhibitors (Rhopressa)
loosens junctions across Schlemm's canal.
decreases production of extracellular matrix.
widens TM space.
surgical treatments for glaucoma
-Argon laser trabeculoplasty (ALT)
-Selective laser trabeculoplasty (SLT)
-Trabeculectomy
-Endoscopic cyclophotocoagulation
Argon laser trabeculoplasty (ALT)
less common.
high laser energy.
-damages TM, causing it to contract and scar.
permanent.
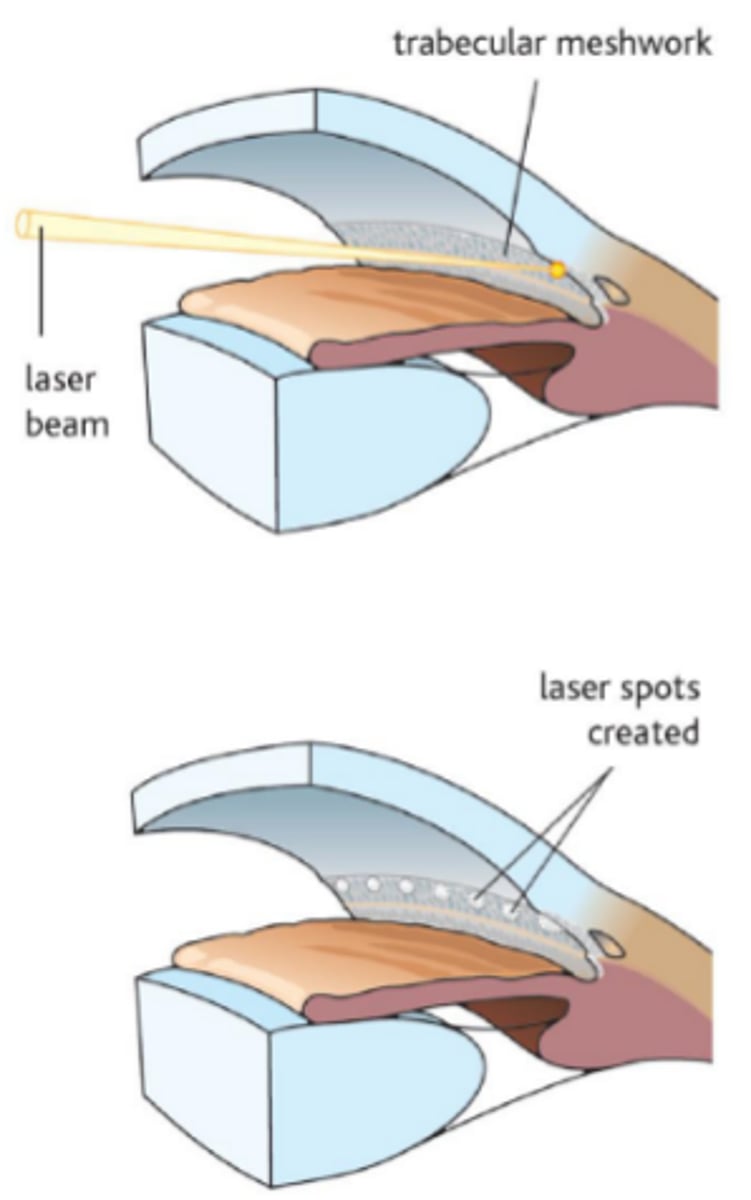
Selective laser trabeculoplasty (SLT)
more common.
lower laser energy.
-absorbed selectively.
can be repeated.
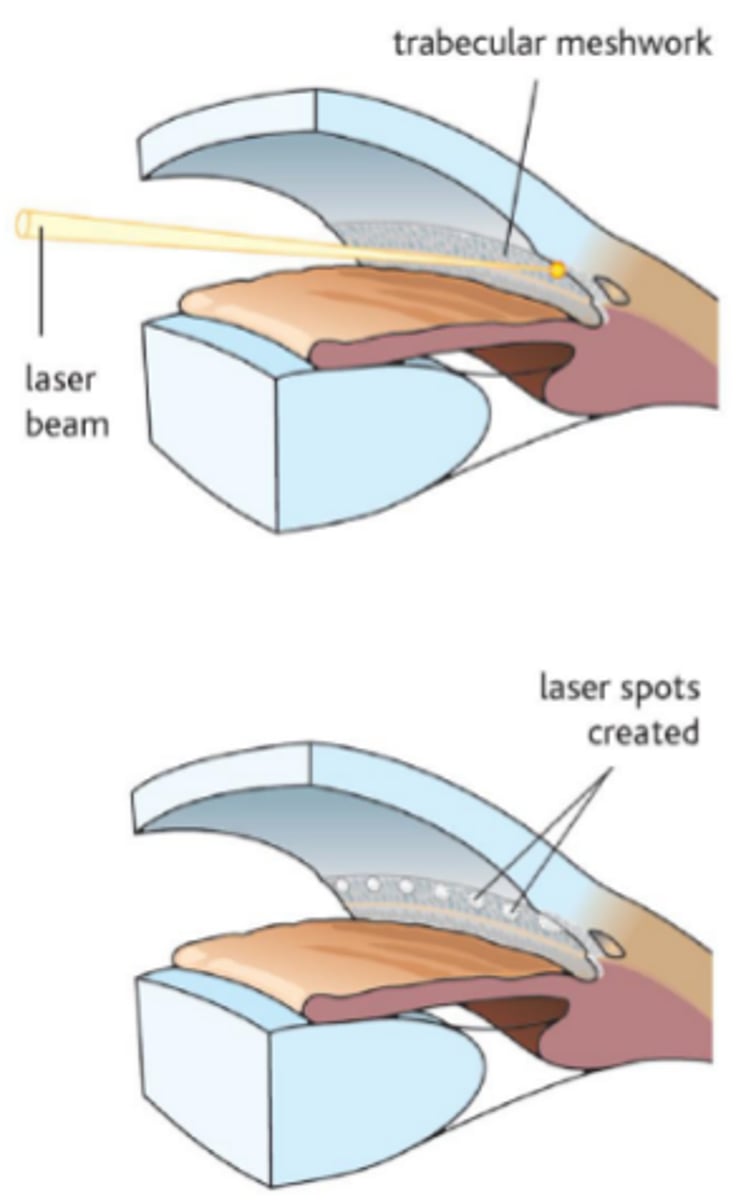
Trabeculectomy
wedge of TM is removed.
forms a scleral flap (filtering bleb).
aging changes in the TM
TM thickens, forms plaques.
decrease in TM facility is offset by the decrease in aqueous production!
-therefore, IOP is relatively stable with age.
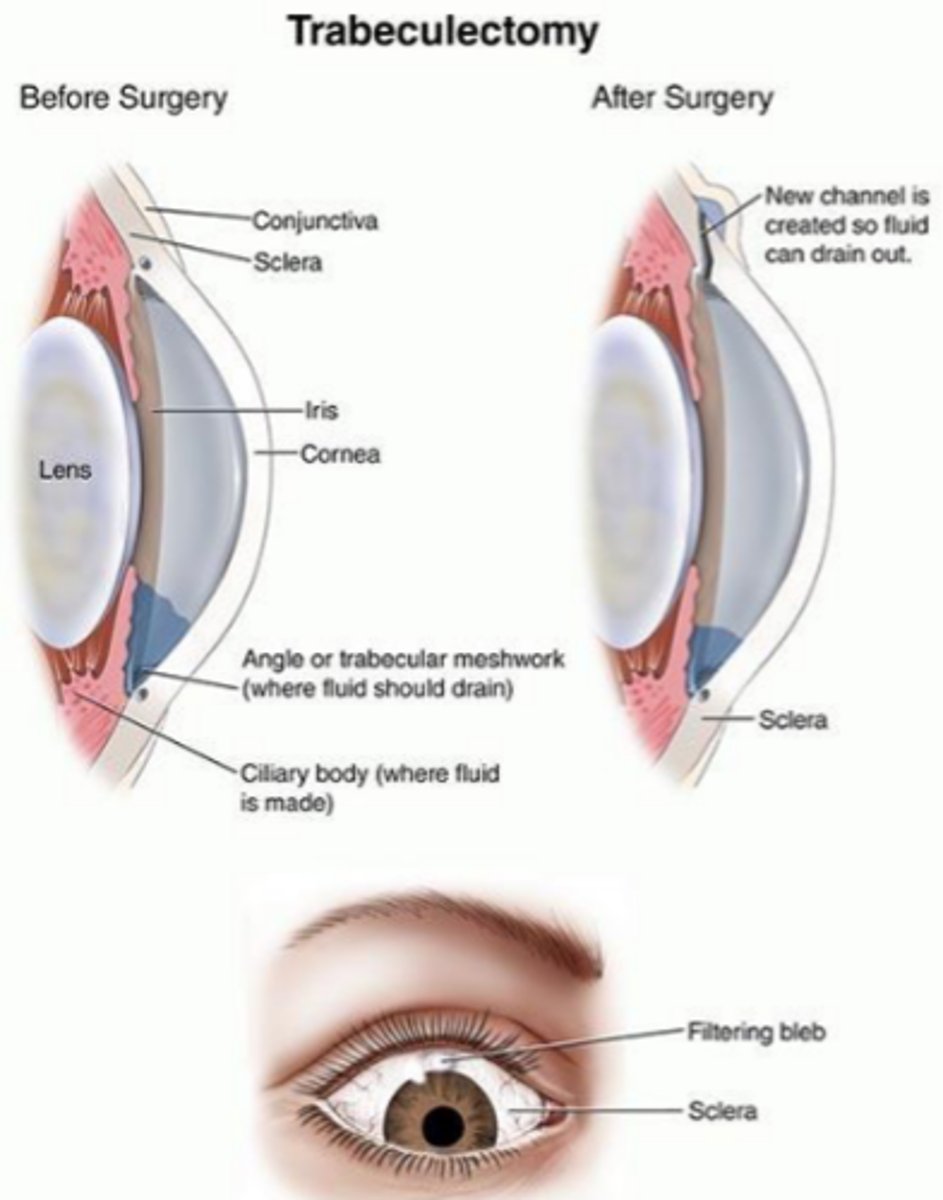
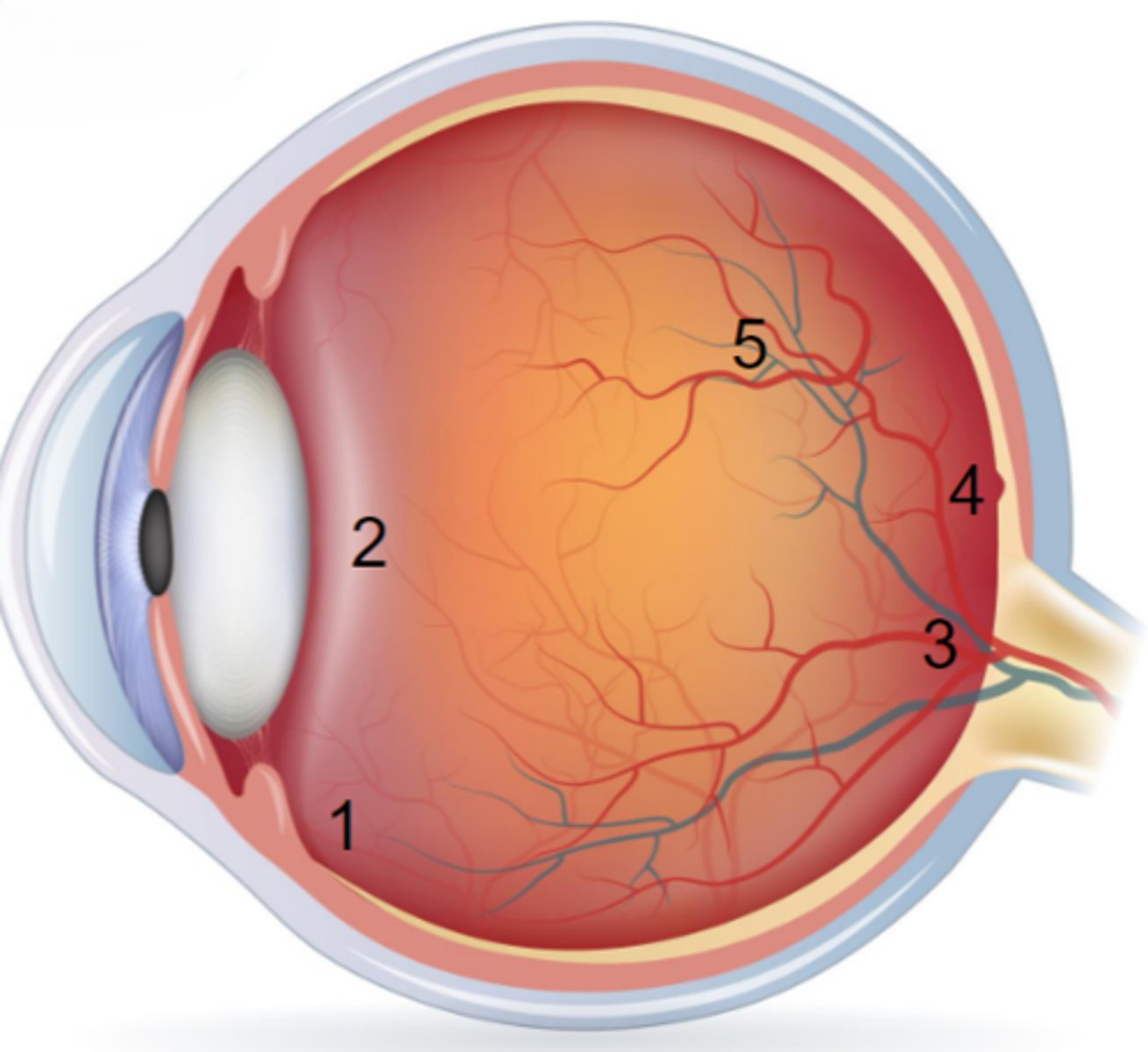
vitreous chamber
75-80% of eye volume.
core of viscoelastic gel.
encased in hyaloid membrane, or vitreous face.
functions of vitreous
1. physical support holding the retina in place next to the choroid.
2. storage area for metabolites for the retina and lens.
3. acts as a "shock absorber"
4. transmits and refracts light
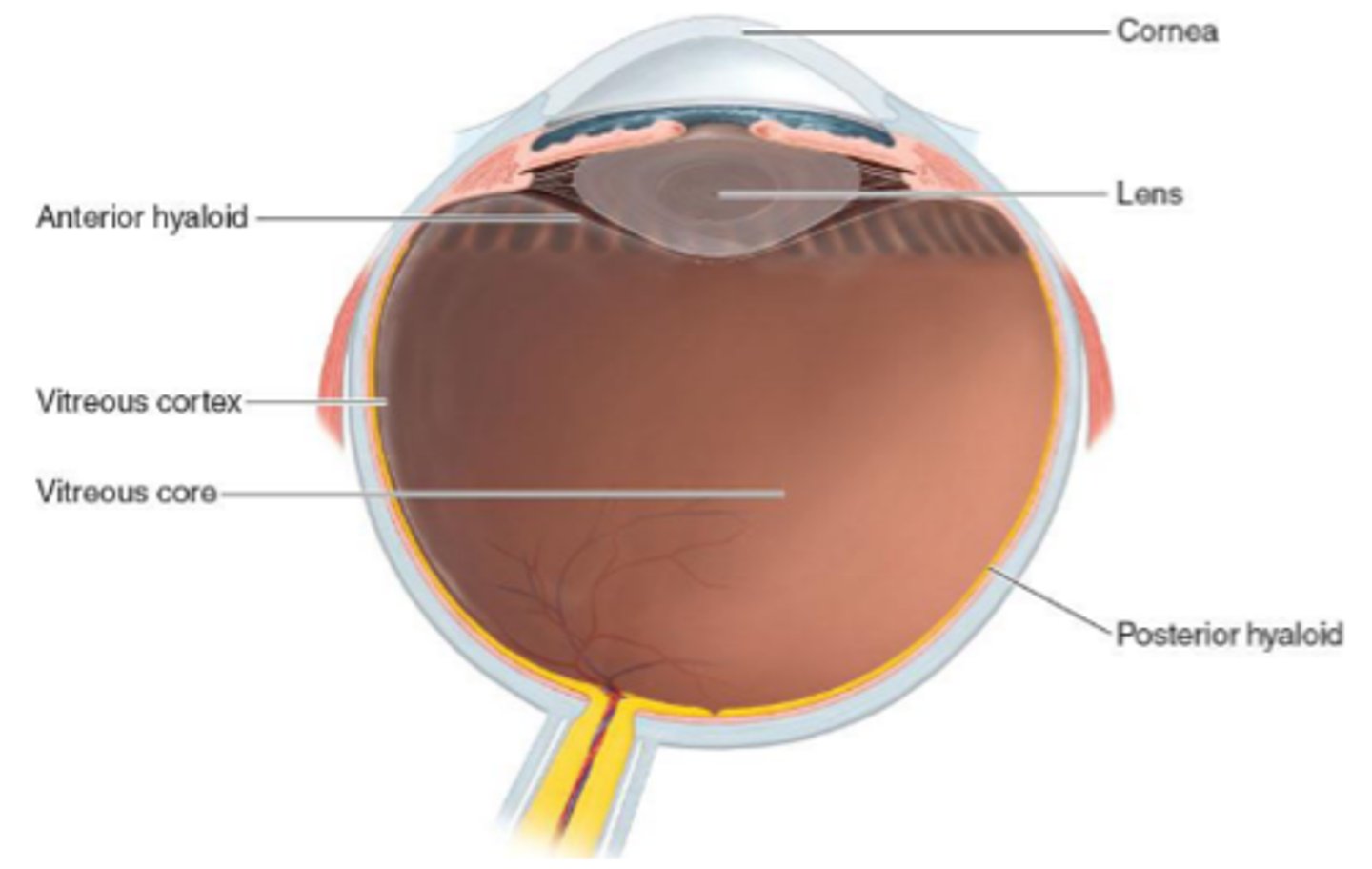
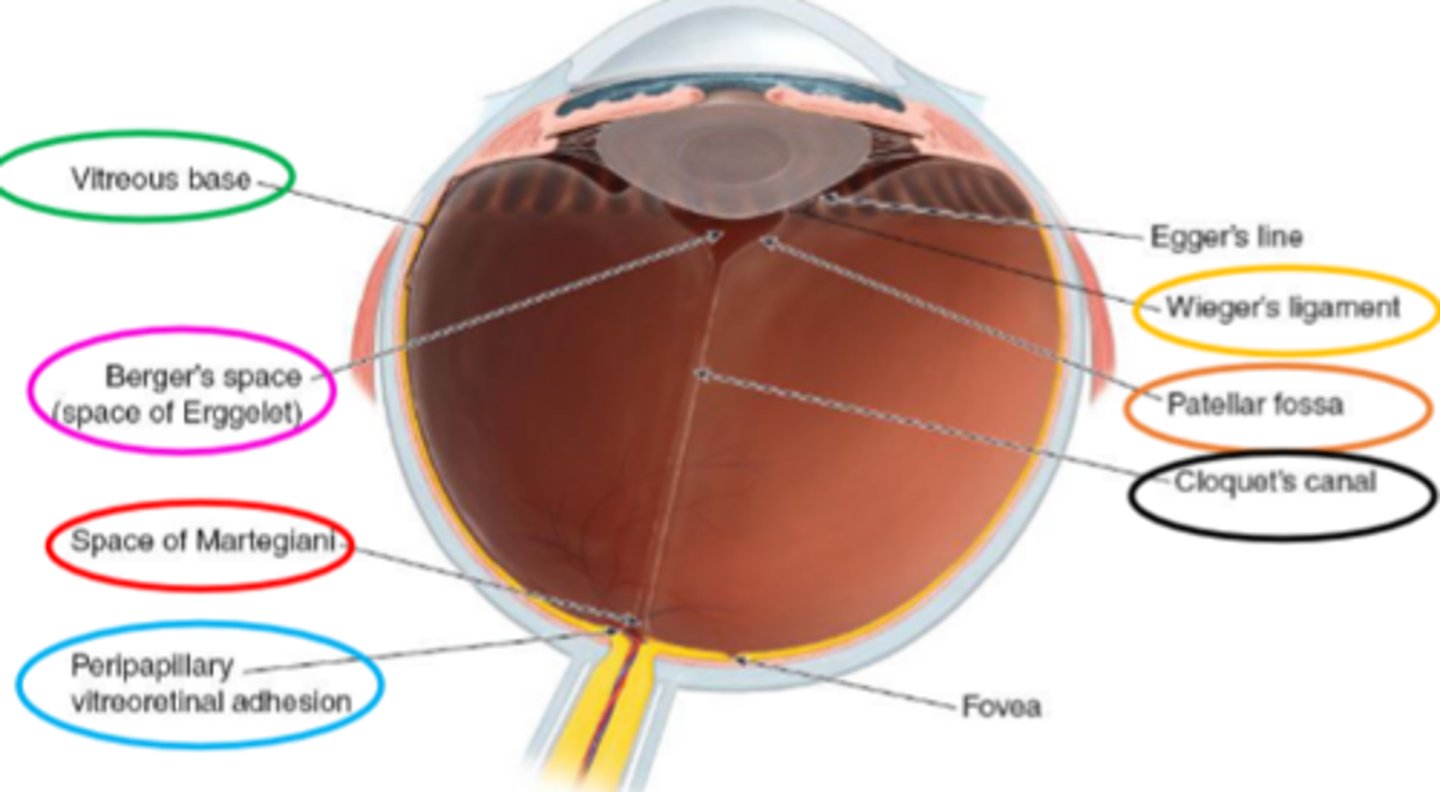
Vitreous base
in the region of the pars plicata and ora serrata.
the strongest attachment of the vitreous body to the wall of the eye.
separates anterior and posterior hyaloid membrane.
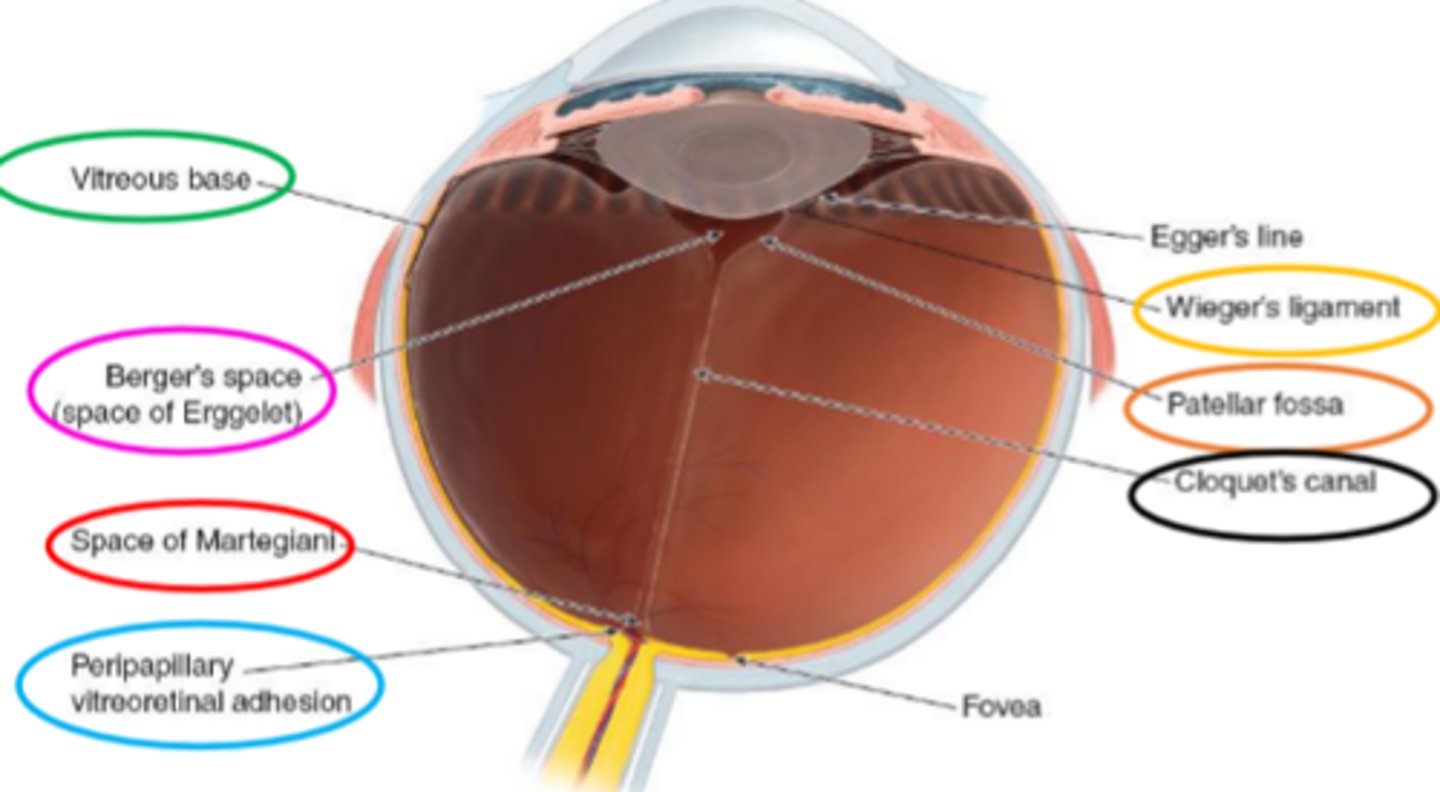
Berger's/Erggelet's space
separates the anterior hyaloid face from the posterior lens capsule.
bounded by Wieger's ligament.
hyaloideocapsular (Wieger's) ligament
part of the hyaloid membrane that is attached to the lens capsule.
bounds Berger's/Erggelet's space.
Patellar fossa
portion of the anterior hyaloid membrane within the confines of Wieger's ligament.
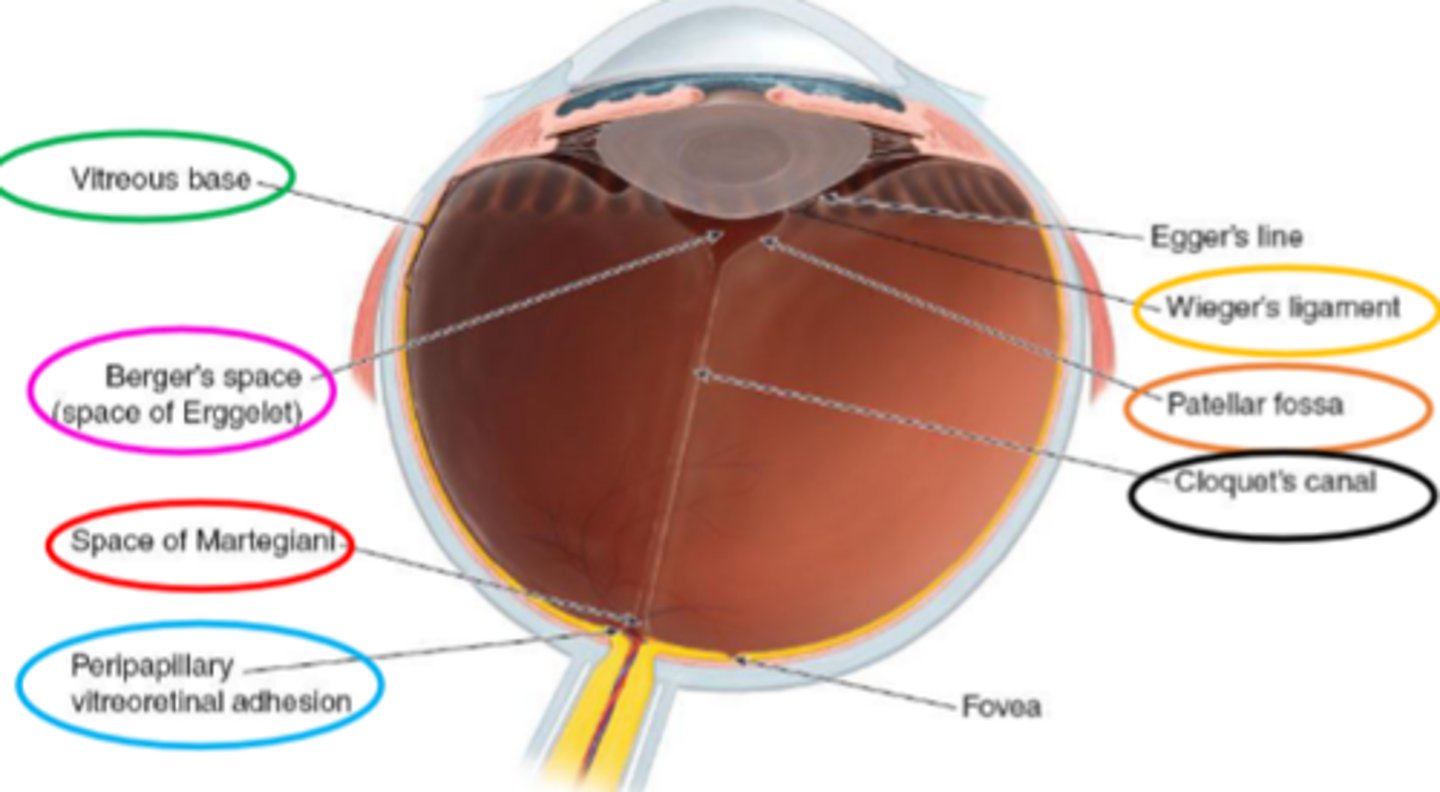
Peripapillary vitreoretinal adhesion
attachment of the vitreous body around the optic nerve.
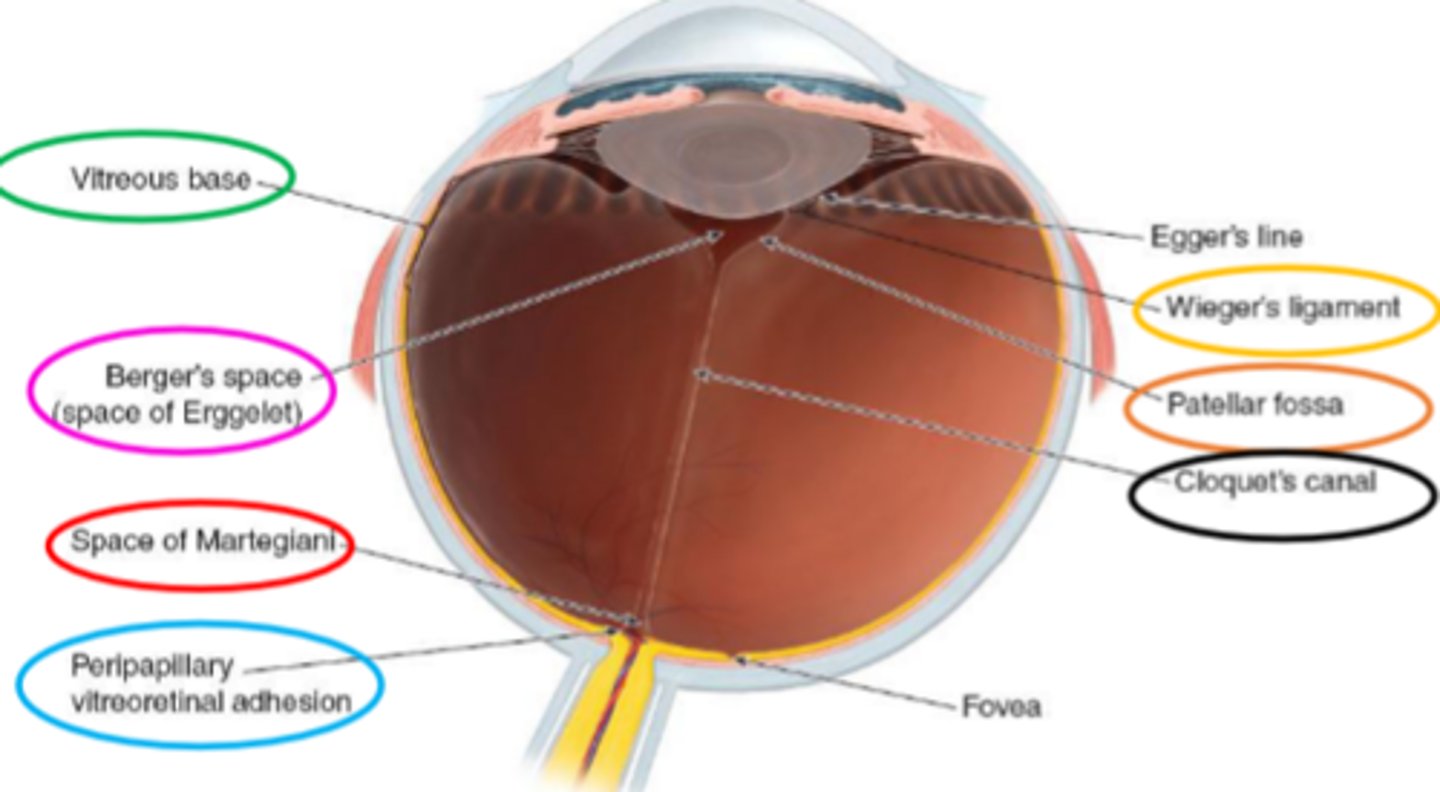
Space of Martegiani
space overlying the optic nerve.
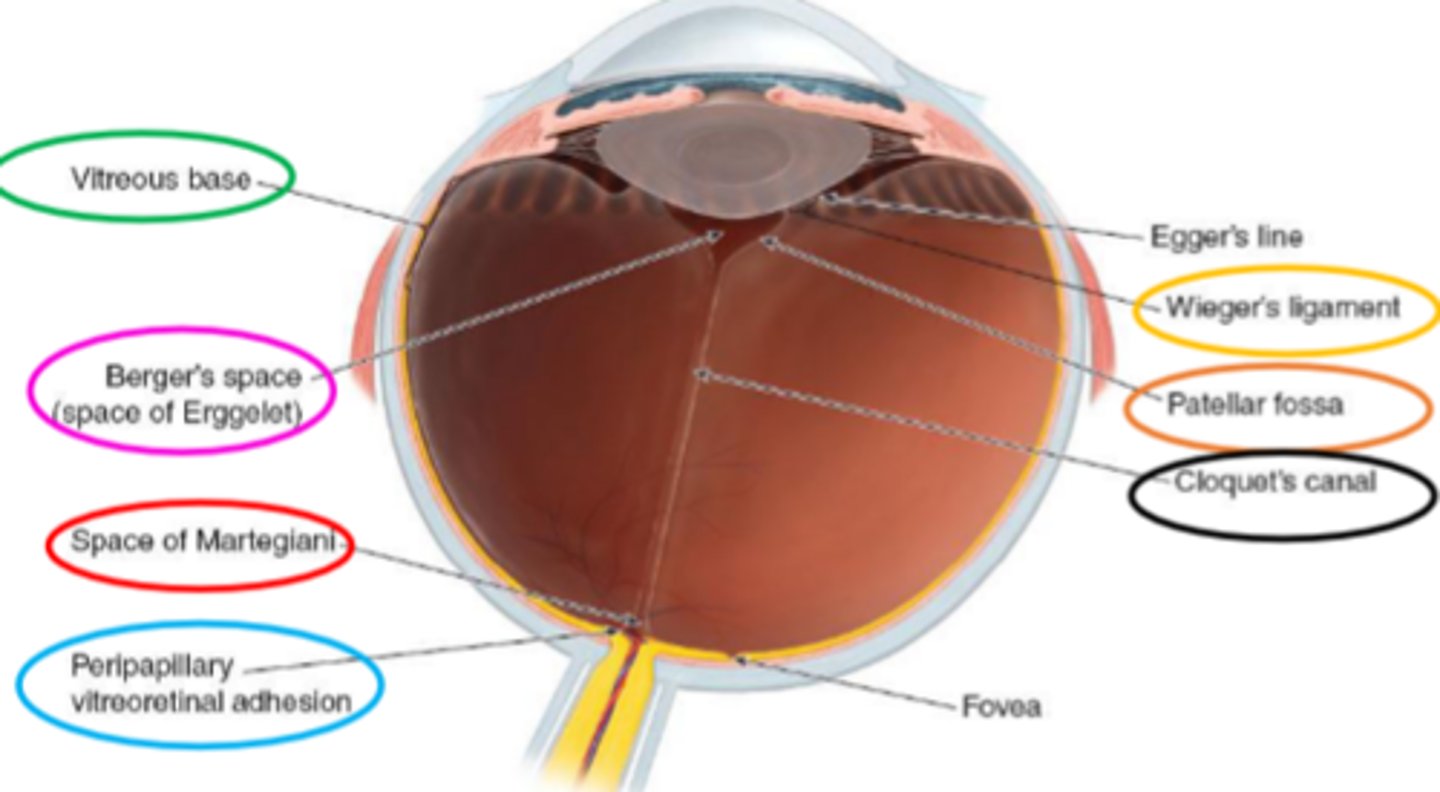
Cloquet's canal
the remnant of the primary vitreous.
extends from the space of Martegiani to Berger's space.
vitreous attachments
strongest to weakest:
-Ora serrata/vitreous base
-posterior Lens
-optic Disc
-Macula
-Retinal Vessels
OLD MR. V
important for trauma patients: helps determine which part of the vitreous is likely to detach first.
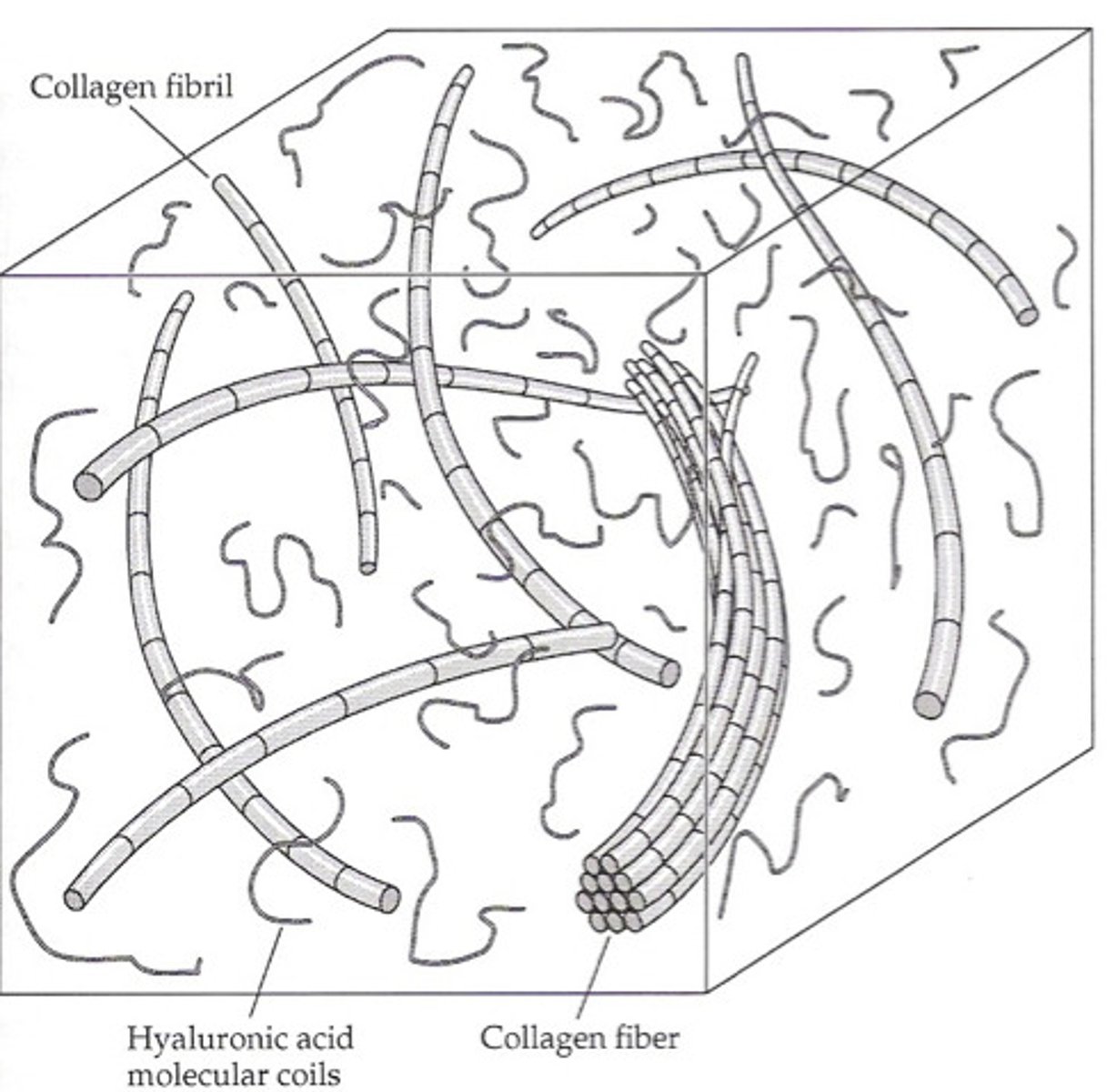
vitreous composition
transparent, dilute solution.
mostly water (98-99.7%)
-salts
-soluble proteins
-hyaluronic acid within a meshwork of insoluble collagen
(HA-collagen complex).
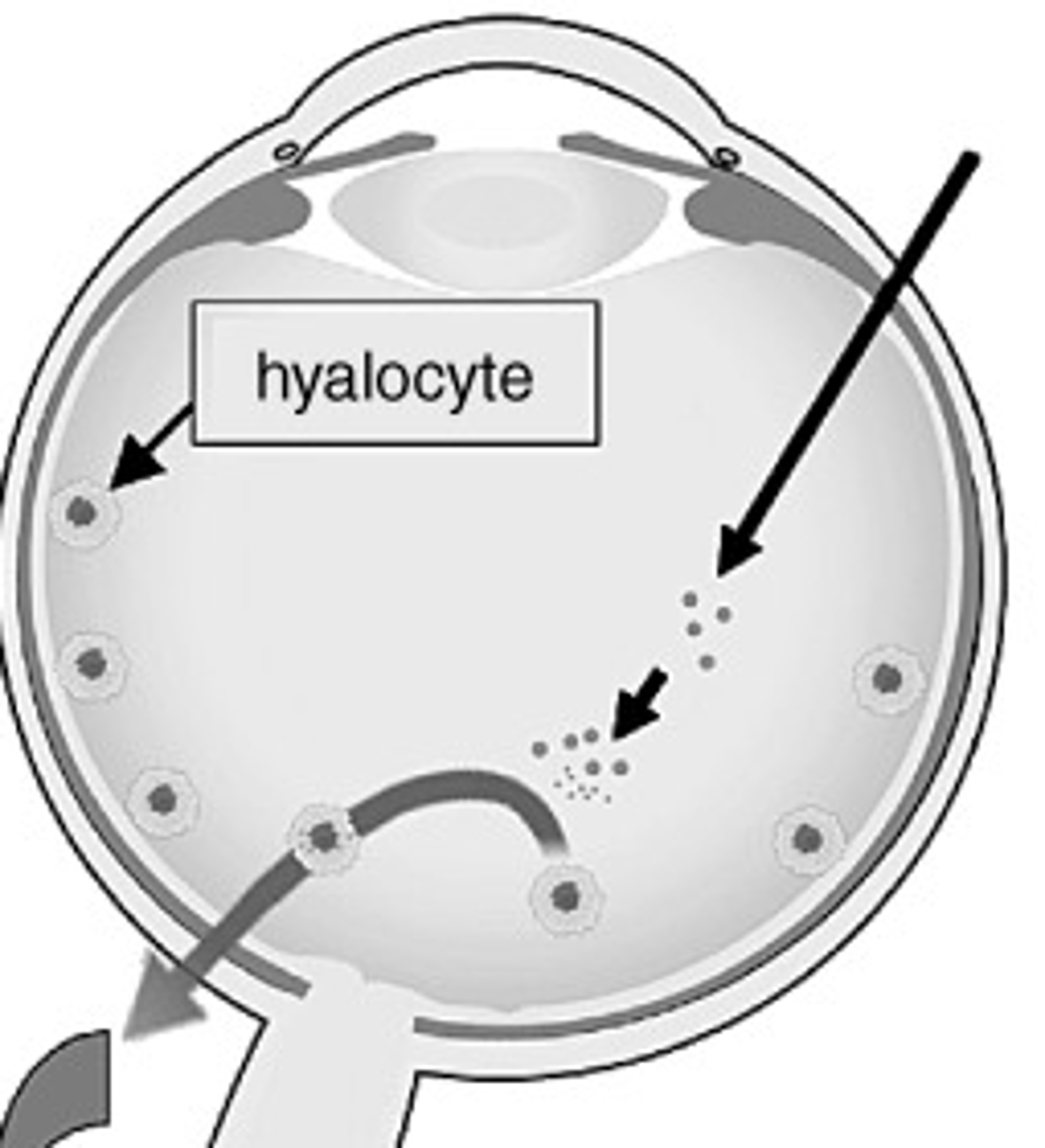
hyalocytes
vitreous cells.
located in a single, widely spaced layer.
they make hyaluronic acid and glycoproteins for collagen.
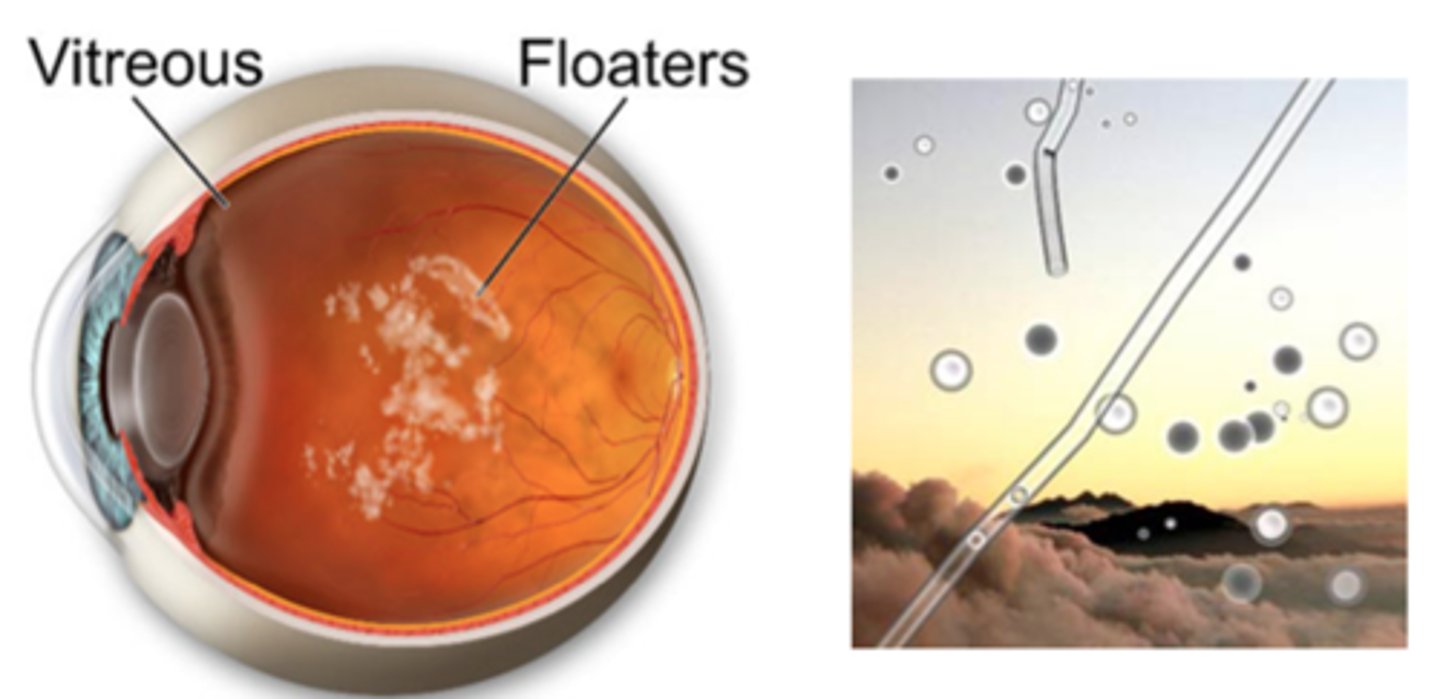
floaters
disruption in HA-collagen complex causes aggregation of collagen fibrils.
large enough to see clinically.
vitreous syneresis (vitreous liquefaction)
vitreous contains the antioxidant ascorbate.
young patients:
-vitreous is a gel.
-gel vitreous has a higher concentration of ascorbate.
-oxygen is consumed at a faster rate.
-less oxidative stress.
older patients:
-vitreous becomes more liquid with age.
-liquid vitreous has a lower concentration of ascorbate.
-oxygen is consumed at a slower rate.
-more oxidative stress.
can also occur after a vitrectomy after the lens is exposed to a greater concentration of oxygen.
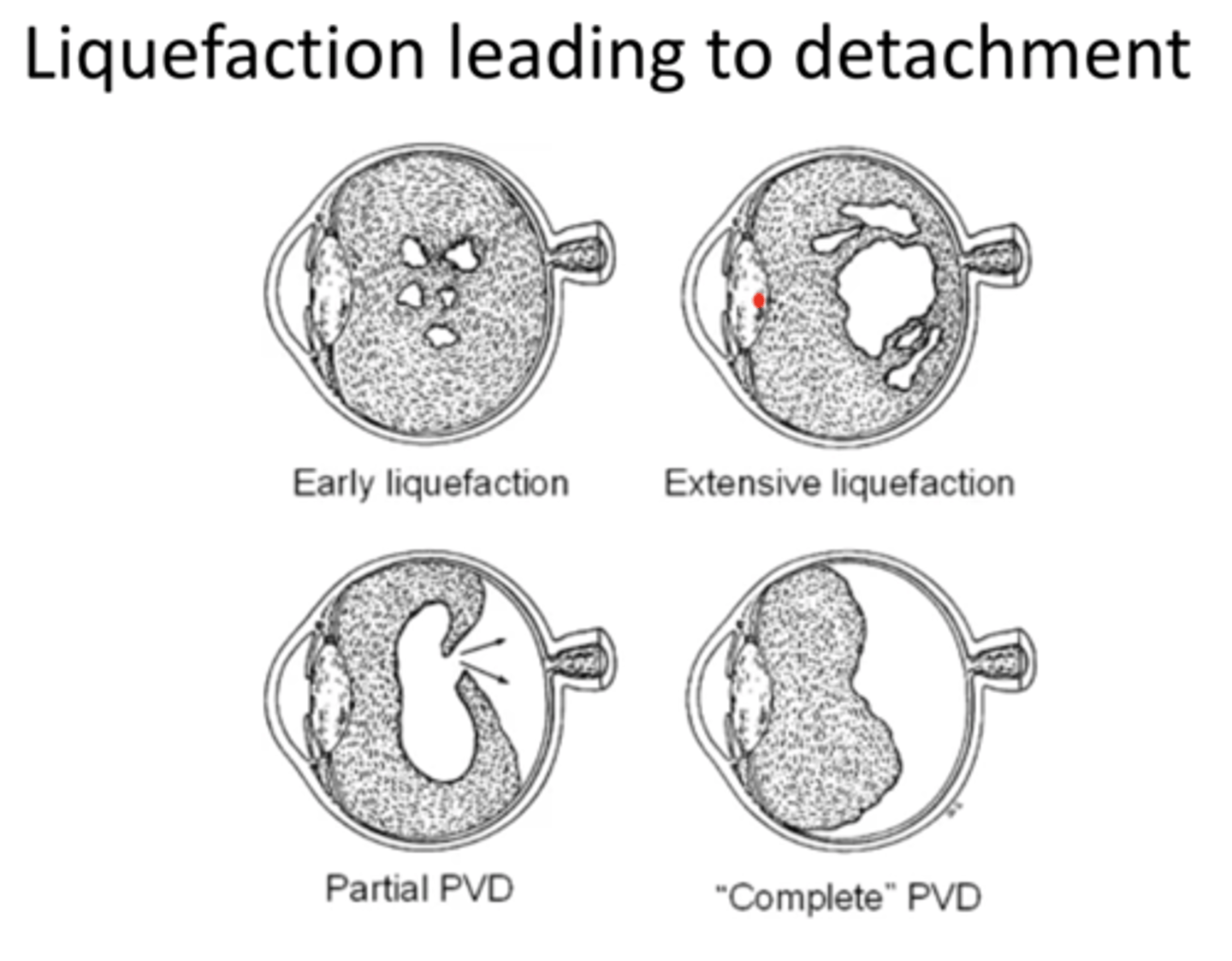
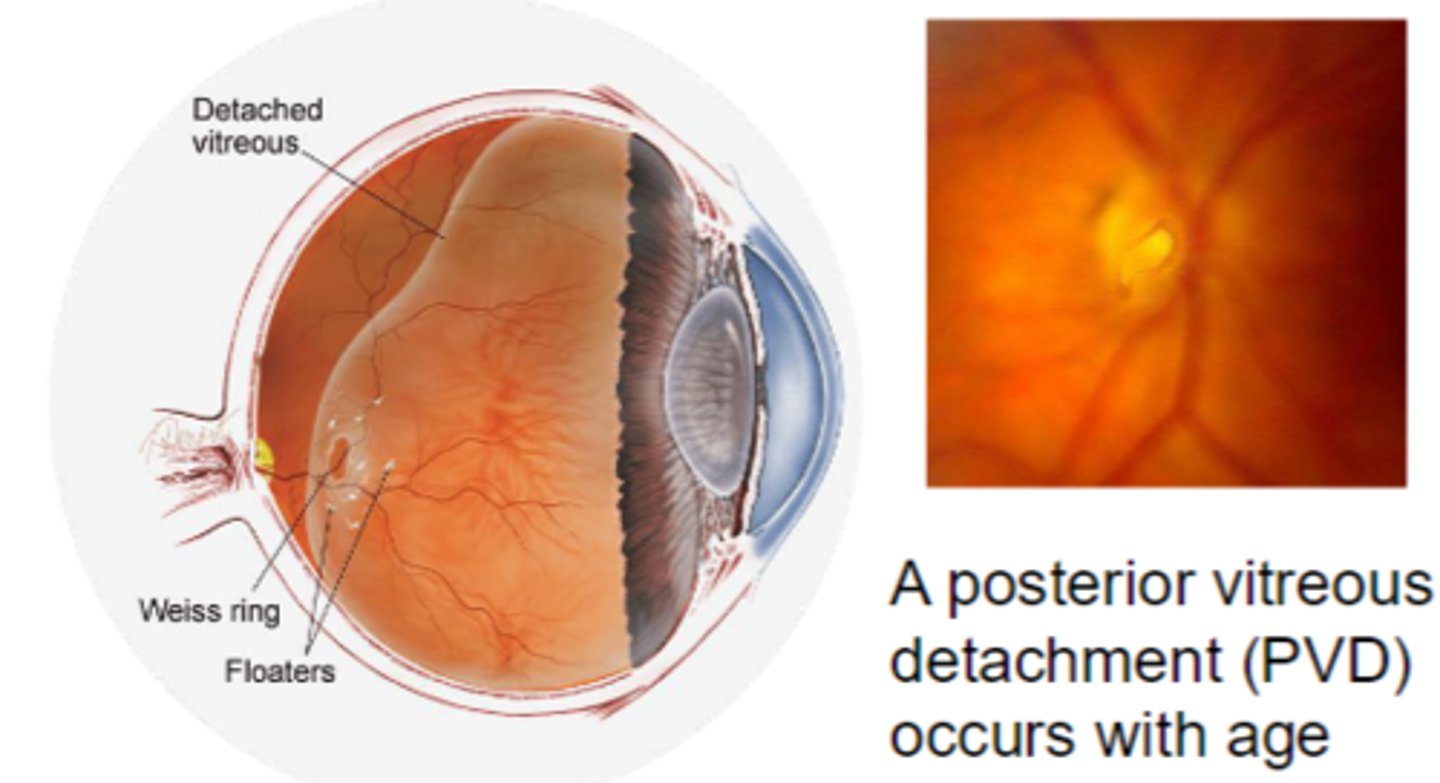
Posterior Vitreous Detachment (PVD)
occurs with age.
occurs when the vitreous detaches from the Peripapillary vitreoretinal adhesion.
causes a circular condensation (Weiss ring).
flashes of light and floaters are common.
Vitreomacular Traction
occurs when there is contraction of the connections between the vitreous cortex and macula.
causes distortion of macula, or a macular hole.
results in reduced or distorted VAs.