Lifespan final pt 3 (terms)
1/26
Earn XP
Description and Tags
L8-
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
What are some risk factors for childhood anxiety?(5)
Withdrawn and inhibited temperament (avoidant style of coping)
Anxious parents reacting to anxious kids (being overprotective)
Family or neighborhood adversity
Life events, potentially interacting with maladaptive coping styles (Children who already engage in avoidance or threat-focused attention are more likely to interpret life events as overwhelming, leading to persistent anxiety.)
Being raised in a culture that values assertiveness (In cultures that highly value assertiveness, independence, or social boldness, inhibited children may experience greater mismatch with norms. This mismatch increases stress, draws negative feedback, and may heighten self-consciousness, contributing to anxiety.)
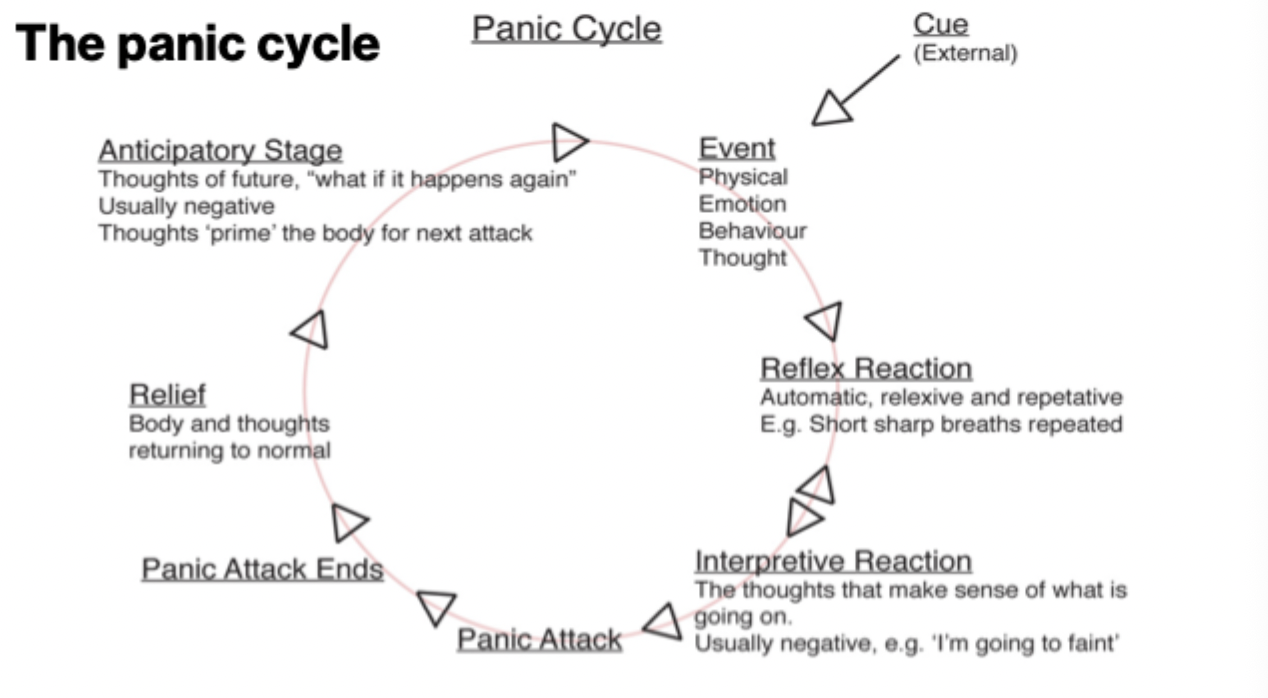
L8&L9: Describe the cycle of panic ( 8 steps)
Cue (external)
Event (physical, emotion, behavior, or thought)
Reflex reaction (Automatic, reflexive and repetitive, ex., short, sharp breaths)
Interpretive reaction (Thoughts that make sense of what’s going on, typically negative ex. I’m going to faint)
Panic Attack
End of panic Attack
Relief (body and thoughts go back to normal)
Anticipatory stage: thoughts of the future, like, “what if it happens again?”. Usually negative. Thoughts ‘prime’ the body for its next attack
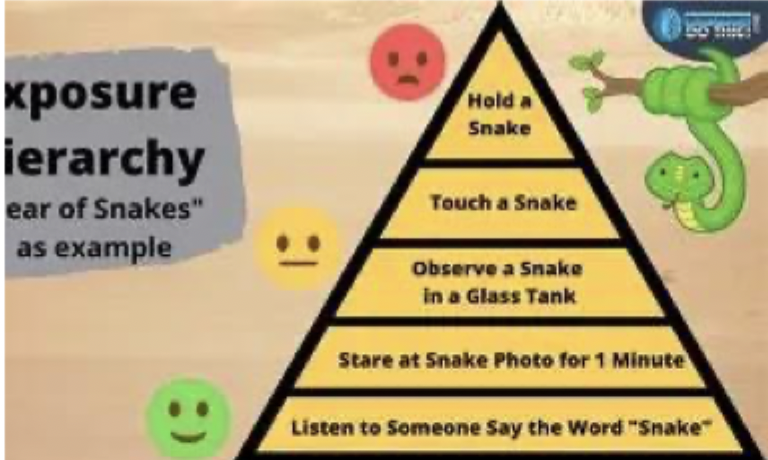
Describe exposure therapy for anxiety disorders (5)
and how habituation (TIME FRAME?) plays a role in recovery (L8)
Exposure therapy
Most effective treatment for anxiety disorders
identify fears
make a hierarchy
start low, increase difficulty within reason (can also jump around)
Stay in each situation for at least 20-30 minutes.
The role of habituation in recovery
habituation may occur across one session and across multiple sessions, habituation is the reason we must stay with a feared stimulus for so long
What is comorbidity?
Is it real?
What is it a product of?
Overlap is _____, and ______, not ______.
What is it?
co-occurrence of two or more mental disorders in the same individual, beyond what is expected by chance. EXTREMELY common in psychopathology.
By chance
If 10% of people have Disorder A
And 10% have Disorder B
Then by chance alone, we’d expect 1% (0.10 × 0.10) to have both.
👉 The co-occurrence rate is higher than would be predicted if the disorders were independent.
👉 This suggests shared risk factors, overlapping symptoms, or causal relationships.
is it real?
yes, but its not simply two separate disorders happening at once.
largely a product of shared underlying dimensions of psychopathology, such as internalizing (anxiety and depression) and externalizing (substance use, impulsivity)
Internalizing: Psychological problems in which distress is directed inward—toward the self.
Externalizing: Psychological problems in which distress is expressed outwardly through behavior.
overlap is expected and meaningful, not random
What are some potential explanations for comorbidity? (7 total)
SBGP(2)CEO
Symptom overlap: Diagnostic criteria share similar symptoms (e.g., sleep problems, concentration issues), inflating co-occurrence.
Diagnostic boundaries too similar: Some “separate” disorders may actually be variations of a broader internalizing condition.
Shared genetic vulnerability: Depression and anxiety share substantial genetic risk—especially neuroticism/negative affectivity.
Shared personality/temperament: High neuroticism increases risk for both disorders. Low positive affectivity increases risk for depression and social anxiety specifically.
Shared cognitive/behavioral processes: Rumination, worry, avoidance, and cognitive biases maintain both disorders.
Shared environmental risk factors: Early adversity (neglect, abuse), interpersonal stress, and life events involving danger + loss elevate risk for both.
One disorder increases risk for the other: Anxiety often precedes depression and can lead to depressive symptoms via impairment, stress, or demoralization.
What is scrupulosity? How does it manifest (what might obsessions and compulsions look like)? What does it say about OCD and the role of religion in psychopathology? (L9)
What is the presence of religious obsessions associated with?
How should treatment be framed for people struggling with this?
What is it: A subtype of OCD involving religious or moral obsessions (fear of committing sin, violating religious law, or being immoral)
How does it manifest?
Obsessions: fear of praying incorrectly, committing accidental sins, ritual impurity, violating dietary laws, offending god etc.
Compulsions: Excessive praying, checking, reassurance seeking from clergy, avoiding situations that trigger fear of sin
examples:
Judaism: fears of impurity, mixing milk and meat
Catholicism: fears of incorrect communion, missing sins in confession
What does it say about OCD and the role of religion in psychopathology?
Religion doesn’t cause OCD, it just shapes the content of the symptoms. Overall, religious context shapes phenomenology, not the etiology of psychopathology.
OCD hooks onto whatever matters most for the person
highly religious communities may normalize or unintentionally reinforce
Presence of religious obsessions is associated with poorer insight, more magical thinking, and sometimes poorer treatment response.
Effective treatment should not decrease religiosity; instead, OCD is framed as the barrier preventing authentic religious life.
What is mirror retraining and how is it used to treat BDD? (L9)
how is it used
what is the method called? (3 words)
Patient practices….
Helps patient tolerate distress by using ___________, _________ and ________, often paired with___________
What is it?
CBT based intervention, teaches patients to observe their appearance in a neutral and holistic way
Aims to counter BDDs habitual selective attention (zooming in on flaws, distorted self-perception)
How is it used?
Structured mirror sessions guided by a therapist: patient stands at a comfortable distance and views entire face and body, called balanced visual scanning, looking at all features equally (does not just zoom in on one flaw)
Patient practices describing appearance objectively
Helps patient tolerate distress by using exposure principles, reduces avoidance and compulsive checking, often paired with cognitive restructuring.
L10: Define and explain the positions of the neurodiversity versus neurodivergent (strength vs deficit-based) models of neurodevelopmental disorders.
Neurodiversity
ADHD and autism are ___________ in brain function that have ________ just like neurotypicality and should be treated as such.
symptoms reflect…
This viewpoint also reduces ______
Neurodivergence
ADHD and Autism are disorders that require ______ aimed at…
Symptoms cause marked impairment in ______, _______, and _______. Can also cause _______.
Core issue is _______ so interventions should focus on _______, _____, and ______.
Treatment priorities include: (4)
Neurodiversity (strength-based argument)
ADHD and autism are natural variations in brain function that have strengths just like neurotypicality and should be treated as such: changing the environment is just as important as changing the behavior.
Symptoms reflect a mismatch between the person and the environment
Many adults found that their ADHD symptoms disappeared when they found the right niche
Characteristics of ADHD can become assets in the right setting
This viewpoint also reduces shame
(Jolene Stockman, Paul Tough)
Neurodivergence (deficit-based argument)
ADHD and autism are disorders that require intervention, aimed at changing the person’s way of relating to the world (DSM, Russell Barkley)
Symptoms of ADHD and autism cause marked impairments in attention, executive functioning, and social communication. Can cause distress and impairment
Core issue is internal- so intervention should focus on reducing deficits, improving behavioral control, and increasing functioning across settings.
Treatment priorities include: behavioral modification, skills training, medication, and structured environments to help the person adjust to the demands of the world.
What are the components of recommended treatment for ADHD? 4 main components.
Both meds
Behavioral therapy for children and adolescents
Teaching positive communication skills, discipline
Same strategies/ treatments as for kids with behavior problems
Executive functioning skills building (CBT)
Using calendars, To Do lists, prioritization of tasks, problem solving
Doing tasks in bite-sized increments, being aware of and managing distractibility
Changing self-defeating thoughts
Lifestyle modifications: Structure/ routine, exercise, accommodations, sleep
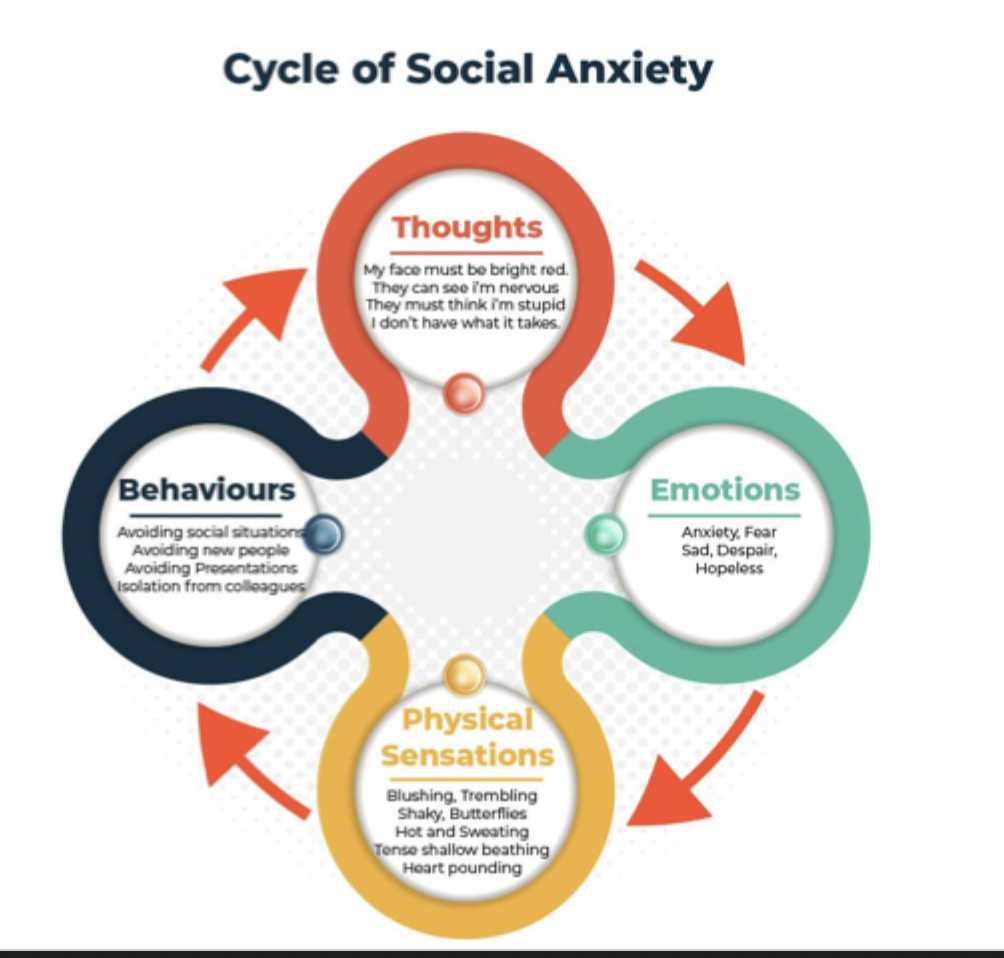
Describe the cycle of social anxiety
Thoughts: ex. my face must be red, they can see I’m nervous, they must think I’m stupid, I don’t have what it takes.
Emotions: ex. anxiety, fear, sadness, hopelessness
Physical sensations: ex. blushing, trembling, butterflies, sweating, pounding heart, shallow breathing
Behaviors: ex. avoiding social situations, avoiding new people, avoiding presentations, isolation from colleagues.
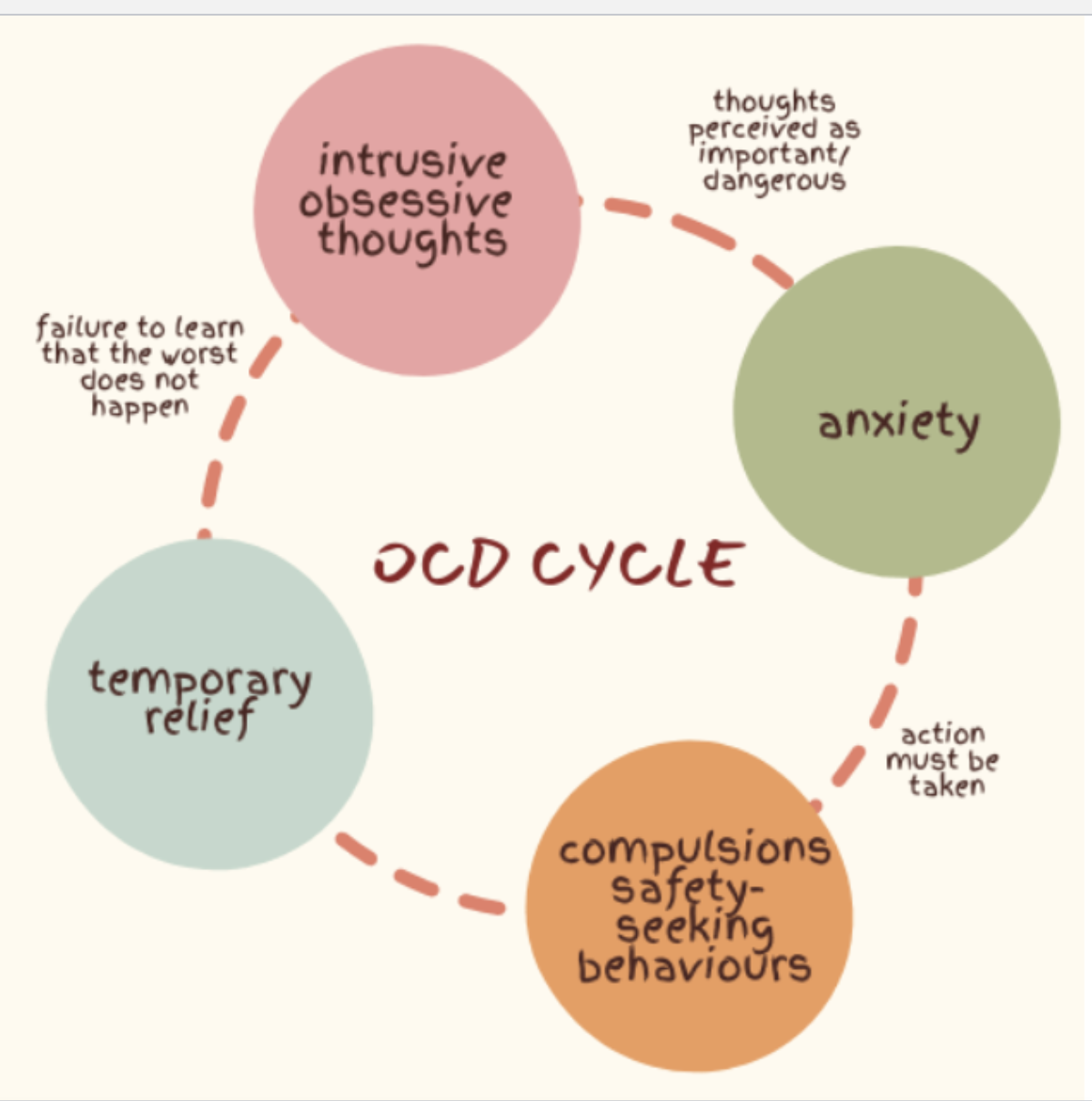
Describe the cycle of OCD (5)
Intrusive, obsessive thoughts (which are perceived as dangerous)
Anxiety- person believes action must be taken
Compulsions: Safety-seeking behaviors (can be behaviors or mental rituals)
Temporary relief- which prevents them from learning that the worst doesn’t happen without the compulsion
Cycle continues when they next get an intrusive/ obsessive thought.
How can we explain comorbidity?
SSCS
How can we explain it?
Ruscio and Khazanov recount several explanations:
Shared risk factors: many disorders have the same genetic, cognitive, emotional, and environmental vulnerabilities
Symptom overlap: DSM categories often include similar symptoms, leading to artificial comorbidity
Causal pathways between disorders: one disorder may increase vulnerability for another (ex., chronic anxiety may lead to depression)
Single underlying dimensions: disorders are not distinct categories, but expressions of broader latent factors
Why does comorbidity matter to your work as clinicians?
Why does it matter to your work as clinicians
Comorbidity is the rule, not the exception: clinicians should expect overlapping symptoms.
Prevents overpathologizing: symptoms may come from one underlying liability rather than “3 separate disorders.”
Treatment should target core mechanisms (avoidance, rumination, etc) rather than chasing multiple diagnoses. This will improve case conceptualization. Maybe someone just generally shows elevated internalizing.
How do HiTop and RDoC fit into the idea of comorbidity?
How do HiTop and Rdoc fit into this?
Both frameworks attempt to solve the comorbidity problem by moving away from DSM categories.
HiTOP (Hierarchical Taxonomy of Psychopathology)
Uses dimensions (e.g., fear, distress, antagonism) rather than categories.
Comorbidity is explained as disorders sharing the same higher-order dimension.
Provides a more statistically coherent and clinically intuitive organization of symptoms.
RDoC (Research Domain Criteria)
Focuses on neurobiological and behavioral systems (e.g., negative valence, arousal).
Avoids comorbidity entirely because it does not rely on DSM categories.
Helps explain why symptoms cut across disorders — they reflect dysfunctions in core psychological systems.
What is DBT?
used to treat?
Integrates ______, ______, and ______
Designed to improve which skills?
Structured, evidence-based therapy to treat chronic emotional dysregulation and self-harm behaviors seen in BPD
Integrates behavior therapy + mindfulness + dialectics (holding two opposing truths at once, ex. acceptance and change)
Designed to improve: emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness skills.
Describe gender differences and biases in diagnoses of personality disorders . What does this lead to?
1. Gendered diagnostic patterns (ASPD vs. BPD)
Women with ASPD are 5.1× more likely to be misdiagnosed as having BPD, even when the clinical presentation is identical.
Men are more readily diagnosed with ASPD, even when their symptoms align more with BPD, reflecting gender-role stereotypes (e.g., men = aggressive; women = emotional).
BPD is culturally viewed as a “female disorder,” whereas ASPD is viewed as a “male disorder,” influencing diagnostic decisions.
2. Sources of gender bias
DSM criteria may reflect gendered assumptions about behavior, such that similar symptoms (e.g., anger, impulsivity, interpersonal conflict) are interpreted differently depending on the patient’s gender, contributing to criterion bias.
Clinicians may rely on gender stereotypes when evaluating symptoms (e.g., irritability/aggression seen as “normal male traits”; emotional instability seen as “female traits”).
3. Clinical consequences of misdiagnosis
Misdiagnosing women with BPD instead of ASPD → ineffective treatment, increased stigma, and difficulty accessing appropriate care.
Misdiagnosing men with ASPD instead of BPD → exclusion from treatment, since ASPD is often an exclusion criterion in services; men may be denied evidence-based BPD therapies (e.g., DBT).
These patterns reinforce gender stereotypes and reduce access to appropriate interventions for both genders.
What is suicide crisis syndrome? (L11)
5 major signs
A means for assessing suicide without requiring disclosure of suicide risk: a way to detect imminent suicide risk without requiring the patient to verbalize suicidal thoughts or intent.
behavioral +emotional patterns that reliably indicate acute danger, even without stated intent.
Persistent and intense feelings of frantic hopelessness: individual feels trapped in a situation that feels intolerable and inescapable
affective disturbance (depression/ anxiety)
Loss of cognitive control (rumination/ rigidity)
Hyperarousal (agitation, hyper vigilance, irritability)
Social withdrawal
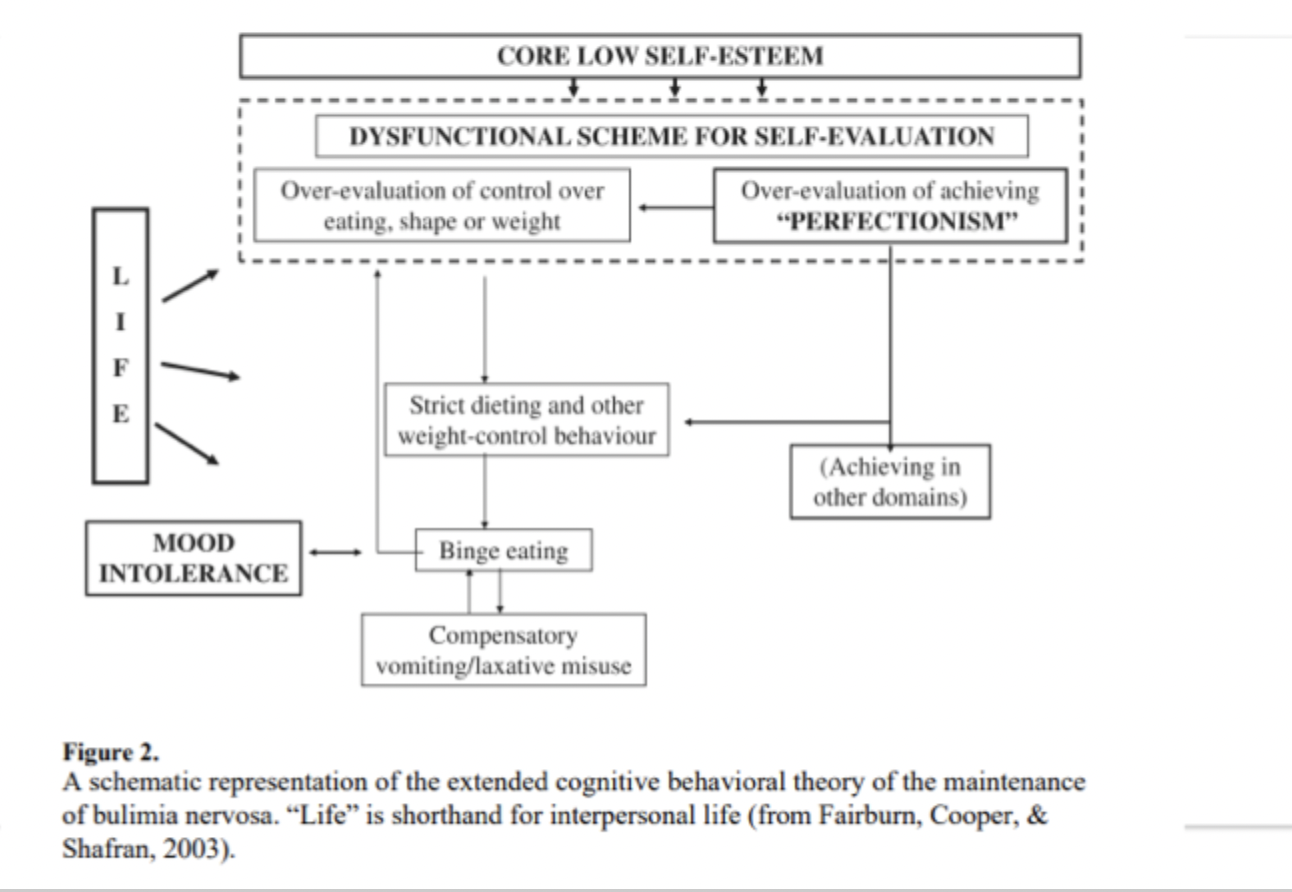
What are the main components of Fairburn’s transdiagnostic model of eating disorders? (L12)
At the core?
Step 2? (two possible aspects of this step?)
Step 3? examples?
Step 4 (results from what 2 things? reinforces what?)
Step 5? (______ behaviors, examples?, what does this do in the short term? In the long term? )
Step 6? Leads to and comes from? Occurs at same time as step ___.
Step 7, which occurs at all _____
These are more like aspects than steps.
At the core: Low Self Esteem- pervasive, longstanding sense of inadequacy or worthlessness
Dysfunctional Scheme for Self-Evaluation
a. Over-evaluation of eating, shape, and weight (self worth becomes almost entirely tied to weight control/ dietary success, drives strict eating rules and compensatory behaviors)
b. Perfectionism (over evaluation of achievement, unrealistically high standards in multiple life areas. Achieving in other domains can temporarily boost self evaluation but often reinforces rigidity)
Strict dieting/ weight control behaviors (comes either from over evaluation of eating/ shape/ weight or perfectionism in general)
restrictive eating, rigid rules, fasting, exercise
increases risk of binge eating when rules are broken or restriction becomes physiologically unsustainable
Binge eating (results from and leads to mood intolerance, mentioned #6)
Episodes of loss of control eating, triggered by dietary restraint, mood intolerance, or self-evaluation failures
Reinforces cycle of self criticism and attempts to gain control
Compensatory behaviors
Vomiting, laxatives, or purging
Reduce distress in the short term but maintain the cycle, keeping weight and shape at the center of self-evaluation.
Mood intolerance: leads to and comes from binge eating
Difficulty tolerating strong emotions
Leads to using ED behaviors (restriction, bingeing, purging) to escape/ regulate emotions
Interpersonal life (OCCURS AT ALL STAGES)
stressors, relationship problems, or social evaluation can worsen self esteem and trigger stricter dieting or binge-purging cycles.
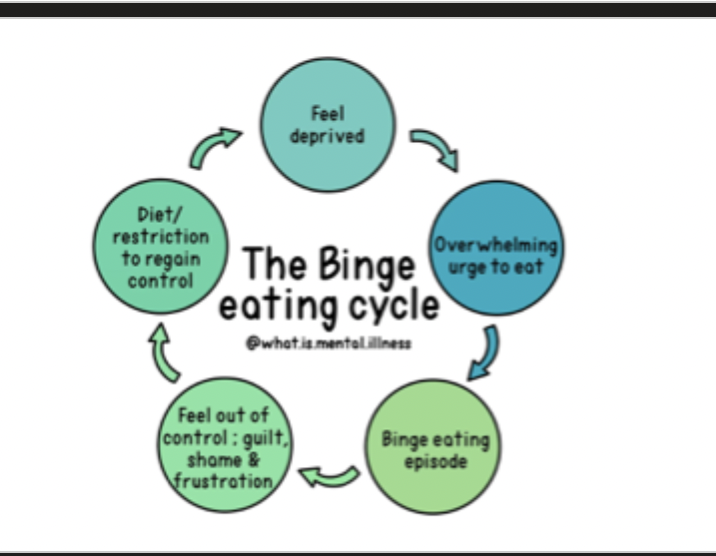
What is the binge cycle and how is it targeted in treatment?
Name the 5 steps of the binge eating cycle
How to target it?
Feel deprived
Overwhelming urge to eat
Binge eating episode
Feel out of control: guilt, shame & frustration
Diet/ restriction to regain control (can include purging behaviors)
How to target:
Make sure eating is regular,
emotional distress interventions, (CBT-E)
stimulus related (no problematic food within reach)
How does CBT-I treat insomnia? Name the steps. (1-6)
Tracking…
Sleep _____
_____ control
Sleep _____/____
_____ work
Outcome?
Tracking sleep with sleep diary
daily sleep log for 1-2 weeks
therapist uses this to calculate sleep efficiency (time asleep / time in bed) and spot patterns
Sleep hygiene (basic habits)
Caffiene, nicotine, alcohol timing
Heavy meals or intense exercise right before bed
Light exposure and screens before bedtime
Create a wind-down routine, same time every night
Stimulus control (re-training the bed=sleep)
Rules are usually something like
Go to bed only when sleepy
use the bed only for sleep, no scrolling, homework, etc
If you’re awake for 10-15 minutes, get out of bed, go to another room, and do a quiet, non-stimulating activity until sleepy, then return to bed
Wake up at the same time every morning
Avoid long naps
Sleep consolidation/ restriction
Based on sleep diary, therapist limits time in bed to account how much the person is actually sleeping
This builds sleep pressure, so the person falls asleep faster and wakes up less
As sleep efficiency improves, time in bed is gradually increased by small chunks
Cognitive work: minimizing catastrophic thoughts
Identify unhelpful sleep thoughts ex. if I don’t get 8 hours tomorrow will be a disaster
Challenge and replace with more realistic thoughts (one bad night won’t ruin everything)
Outcome & Maintenance
Over time
Faster sleep onset, fewer awakenings, better daytime functioning
Improvements often keep growing after treatment ends as habits stick
Therapist and client plan for relapse prevention (what to do if insomnia flares up again).
How is DBT used to treat BPD?
What are the three main things it targets? Name them in order.
What is chain analysis, 6 steps? How is it used?
What are the skill modules taught? (3)
What kind of balance is required of the therapist?
Some other strategies used by therapist?
What are some strategies to plan for the future?
Targets life-threatening behaviors first (ex. suicide and self harm) then therapy-interfering behaviors (ex. cancelling sessions last minute, leaving sessions early when things get emotionally intese rapid shifts between idealizing and devaluing the therapist), then quality of life issues
Uses chain analysis to break down: triggers → vulnerabilities → thoughts → emotions → behaviors → consequences; teaches clients to interrupt the chain with skills.
Skill modules
Distress tolerance: used early to reduce self-harm
Emotion regulation: teaching patients to understand, name, and modulate emotional responses
Interpersonal effectiveness: Assertiveness, boundaries, communication skills
Requires a constant balance from therapist with validation+ limit setting (therapist modeling balance between acceptance and change)
Uses irrelevance, humor, and dropping the rope technique
Encourages “cope ahead” planning to prepare for high-risk situations (what might this look like? Provide an example.)
Cope ahead ex. Cope ahead involves mentally rehearsing a stressful situation and planning specific skills to manage emotions and respond effectively.
What are the outcomes of DBT for people with BPD? name 3.
Increased ability to…
Significant reductions in _______ and improved _______
Improved functioning in _____, ______, and ______ settings.
Increased ability to ask for help, self-validate, and regulate emotions
Significant reduction in self-harm and improved stability
Improved functioning in community, family, and academic settings
What is the argument for keeping Orthorexia as a separate disorder from anorexia? (emerging clinical features?)
Distinct obsessional focus: ON is driven by purity/ health of food, not weight loss (motivations differ from anorexia)
Different behavioral patterns: individuals with ON rigidly pursue clean eating, rather than restricting calories or seeking thinness
Emerging clinical features: Qualitative reports suggest ON involves moralization of food, extreme health anxiety, and identity-driven dietary rules not captured by AN.
What are the arguments for combining orthorexia with anorexia?
High symptom overlap (name 3 overlapping symptoms)
Shared Psychological Mechanisms (name 3)
Lack of… ON may simply reflect…
High symptom overlap: both involve rigid rules, dietary restriction, and significant functional impairment, making differentiation challenging.
Shared psychological mechanisms: perfectionism, OCD traits, and need for control appear in both ON and AN
Lack of validated diagnostic criteria: without standardized criteria, ON may simply reflect a variant or subtype of restrictive eating pathology already encompassed within AN.
Why does the debate about combining vs keeping separate AN and ON remain unsolved?
Insufficient empirical data to determine if ON has a unique ______, ______, or ________ from AN.
Risk of…
Some researchers argue that ON may ultimately…
Insufficient empirical data to determine whether ON has unique etiology, course, or treatment response distinct from AN.
Risk of over-pathologizing healthy eating trends complicates classification decisions.
Some researchers argue ON may ultimately fit within a broader transdiagnostic framework of restrictive eating disorders (Researchers suggesting this think orthorexia isn’t fundamentally unique—instead, it may be another expression of these shared processes, similar to anorexia, atypical AN, ARFID with over-control, etc.)
What are the components to a case conceptualization?
Presenting problem
Relevant history
Diagnosis
Predisposing / precipitating / perpetuating / protective factors (4 Ps)
Mechanisms maintaining the problem
Treatment goals
Treatment plan