PH 370 Exam 1
1/111
Earn XP
Description and Tags
Lectures 1-12
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
112 Terms
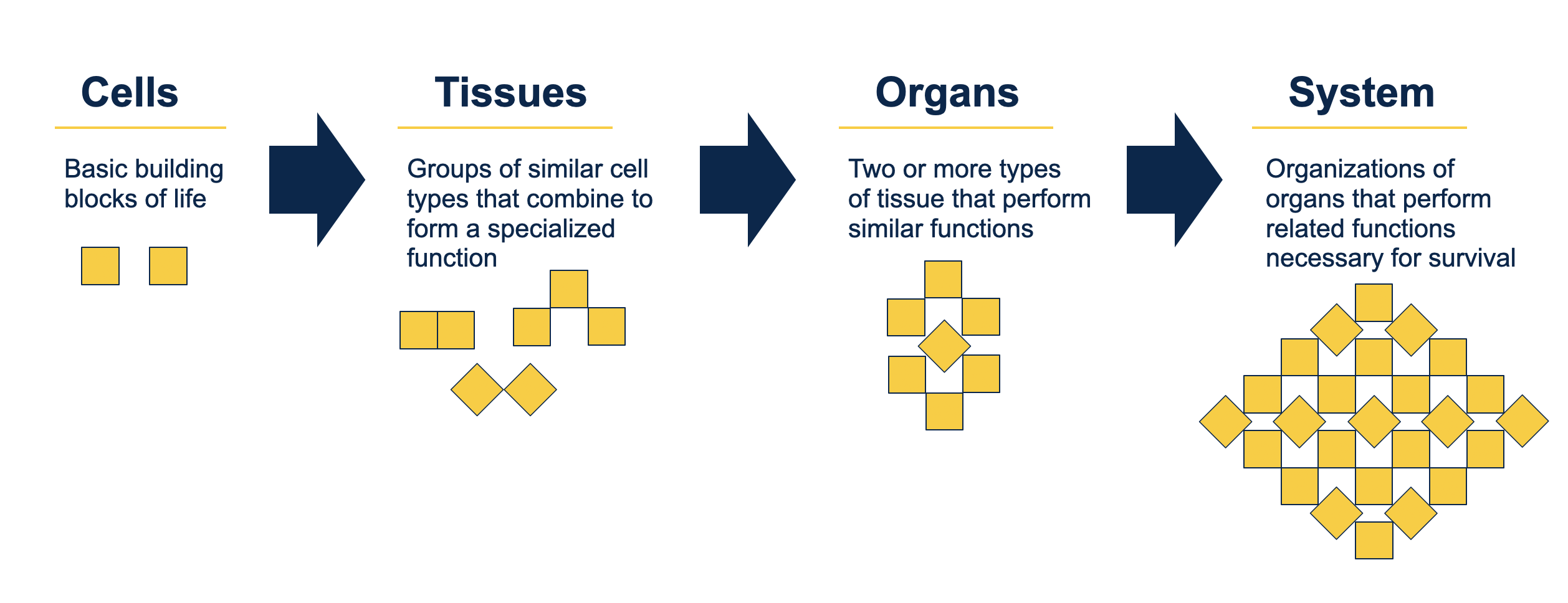
cells
tissues
organs
system
definitions
cells = basic building blocks of life,
tissues = groups of similar cell types that combine to form a specialized function
organs = 2+ types of tissue that perform similar functions
system = organization of organs that perform related functions necessary for survival
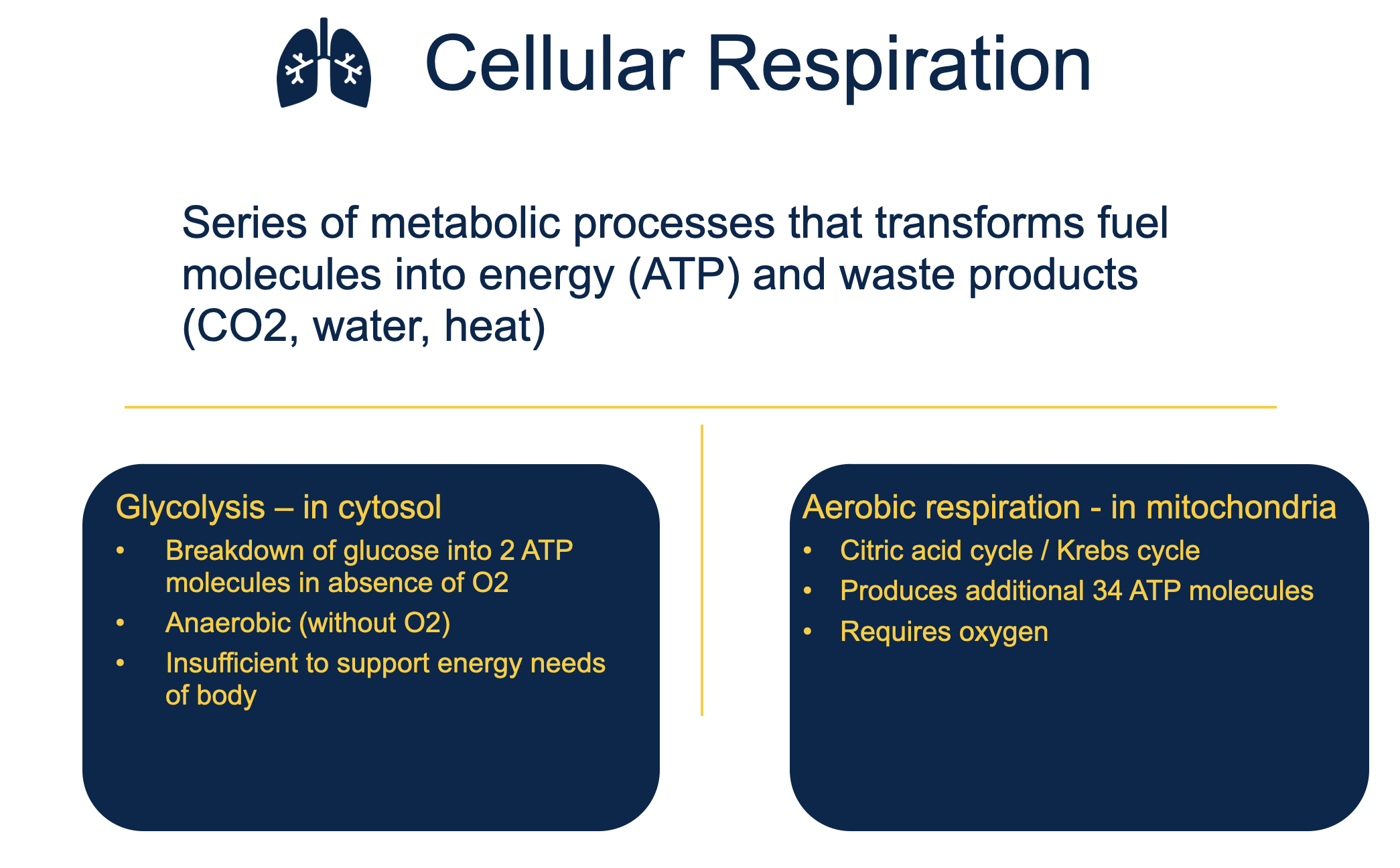
define cellular respiration
cellular respiration is a series of metabolic processes that transforms fuel molecules into energy (ATP) and waste products (CO2, H2O, heat)
aerobic = citric acid/krebs cycle
requires oxygen, in mitochondria, produced additional 34 ATP molecs
anaerobic = glycolysis
breakdown of glucose into 2 ATP molecs, absence of oyxgen, insufficient to support energy needs of body, in cytosol
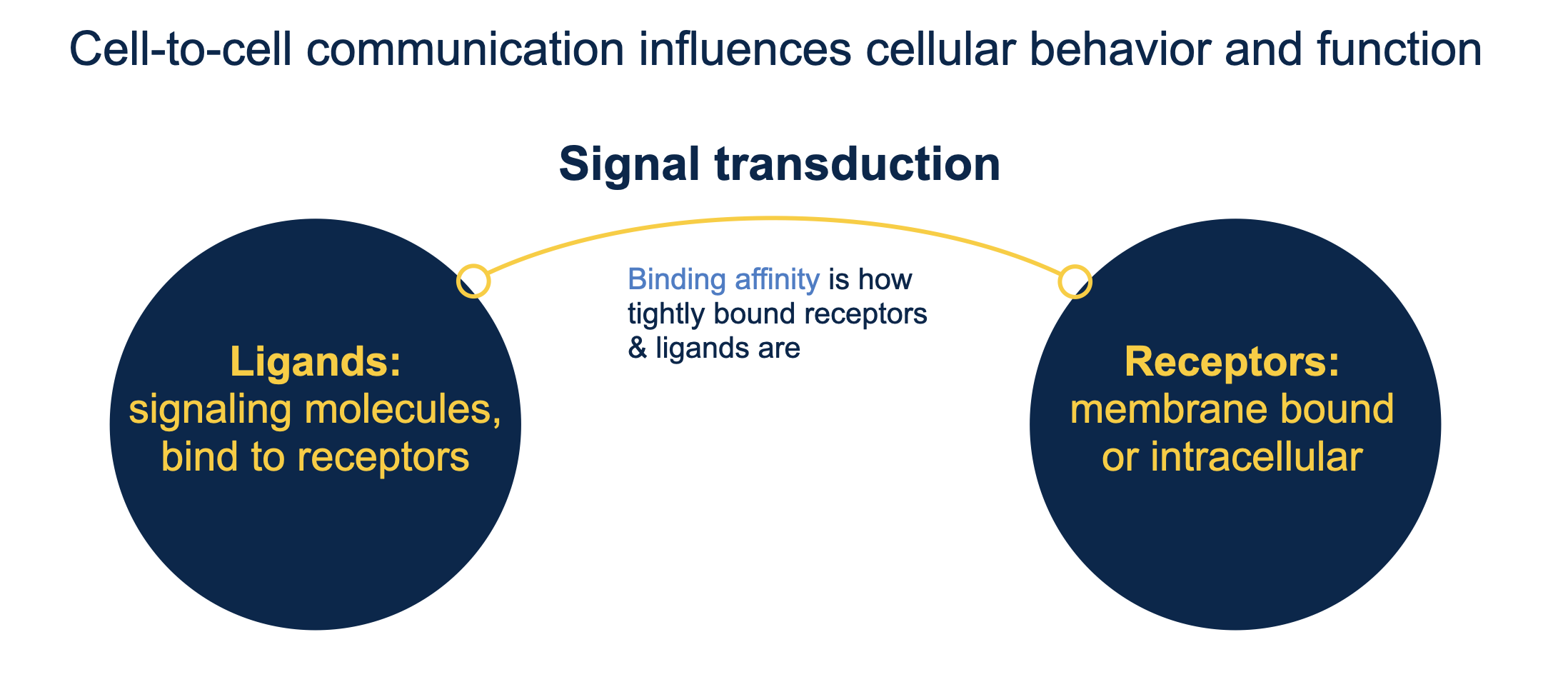
describe cellular communication
binding affinity is how tightly bound receptors and ligands are → signal transduction
ligands = signaling molecules, bind to receptors
receptors = membrane bound or intracellular
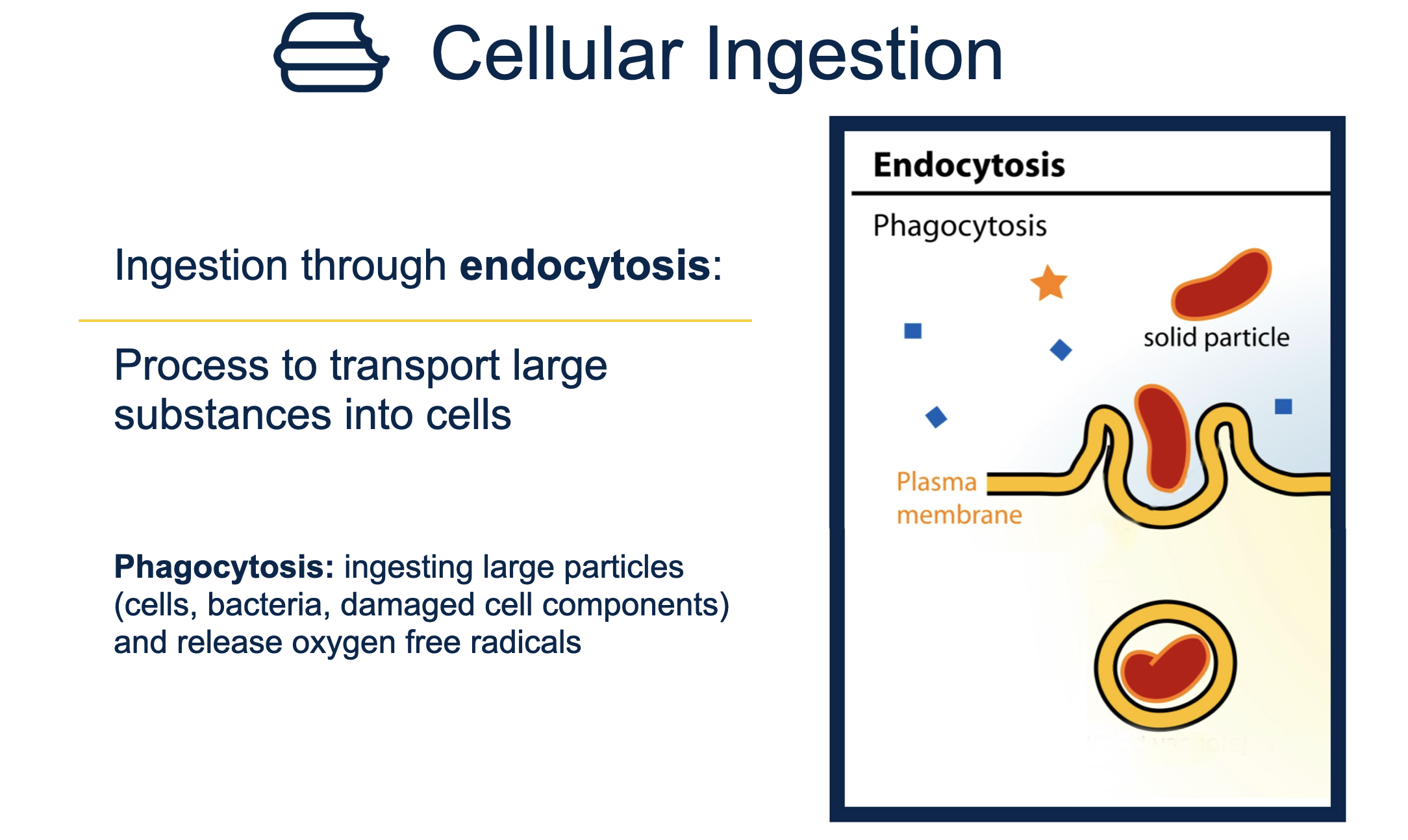
describe the types of cellular ingestion
endocytosis = transport large substances into cells
phagocytosis = ingest large particles and release oxygen free radicals
describe the different types of cellular reproduction (do not need to know phases)
Etiology
Etiology is the study of the cause or origin of a disease or condition. It involves understanding the factors that contribute to the development of a disease, including biological, environmental, and lifestyle influences.
Pathogenesis
pathogenesis = how disease leads to structural/physio changes that result in disease (biologic understanding)
Pathophysiology
study of the pathogenesis of disease
Health vs. Disease
health = when the body can perform vital functions normally/maintain homeostasis
disease = significant disturbance in homeostasis
Risk vs. Etiologic Factor
risk factors = increases probability of an indiv developing a disease or health condition
not all risk factors are etiologic factors
etiologic factors = the cause of disease/condition
all etiologic factors are risk factors
Modifiable
Signs vs. Symptoms
signs = evidence of disease observed on physical examination
symptoms = indications of disease reported by patient
Prognosis (acute, terminal, chronic)
prognosis = the predicted course and outcome of disease
acute = sudden onset, short duration
terminal = diseases that will end in death
chronic = slower, less severe onset and long duration
Edits to prognosis (remission, recurrence, relapse, exacerbation, complication)
remission = reduction/disappearance of signs and symptoms, not a cure
recurrence = return of sign/symptom after remission
relapse = return of disease after its apparent cure
exacerbation = increase in severity of a disease
complication = related disease of other abnormal state in person already with disease
Disease vs. Disorder vs. Syndrome
disease = signif disturbance in homeo of body that modifies vital functions
disorder = abnormality in function, not a disease itself, may or may not have specific signs of symptoms
ex. OCD
syndrome = a group of signs/symptoms related to a single underlying alteration in structure of function
ex. HELLP syndrome: breakdown of RBCs, abnormal liver function, low platelet count
Normal phase vs. preclinical phase vs. clinical phase of disease
Normal phase = no disease, encounter exposures which initiaite pathologic changes, before biologic onset of disease
1st degree prevention: remove causes of disease/immunization
preclinical phase = after etiologic exposure, results from biologic onset of disease, symptoms not present
2nd degree prevention = screen for, detect and treat disease early
clinical phase = symptoms are present, disease is diagnosed, disease is treated
3rd degree prevention = treat clinical disease to prevent death / complications
When do biologic changes start in relation to disease?
Biologic changes in relation to disease typically begin at the cellular or molecular level before clinical symptoms appear. This can occur during the early stages of disease development, often referred to as the preclinical phase, which may last for years. The exact timing varies depending on the disease and individual factors.
When are there symptoms of disease?
symptoms appear at the beginning of the clinical phase
not present in preclinical phase
For disease, when do we screen? when do we treat?
Screening (preclinical, 2nd degree): Typically recommended for asymptomatic individuals at risk for certain diseases (e.g., cancer, diabetes) based on age, family history, and risk factors.
Treatment (clinical, 3rd degree): Initiated when a disease is diagnosed, symptoms are present, or screening results indicate a need for intervention
Primary vs. Secondary vs. Tertiary Prevention of disease
remove causes of disease / immunization
screening for, detect/treat disease early
treat clinical disease to prevent death/complications
Active vs. Passive Transport
Active vs. Passive Transport
Active Transport: Movement of molecules against their concentration/electrochem gradient, requiring energy (ATP).
Passive Transport: Movement of molecules down their concentration gradient without energy input.
Diffusion vs. Facilitated Diffusion
Both are forms of passive transport
Diffusion: Movement of molecules from high to low concentration without energy.
Facilitated Diffusion: Movement of molecules across a membrane via protein channels, also without energy, but requires specific transport proteins.
Phagocytosis vs endocytosis
both are cellular ingestion
phagocytosis = ingest large particles and release oxygen free radicals
endocytosis = transport large substances into cells
Proliferate vs. Differentiate
both are methods of cellular reproduction
proliferate = increase the cell #
differentiate = changes in physical and functional properties of cells; directs cell to develop into specific cell types
Apoptosis vs. necrosis
apoptosis = programmed cell death, replace old cells w/ new, genetic signal
necrosis = cell death related to cell injury / inflammation
both are cell death
Describe the plasma membrane
Describe the nucelus
Describe the cytoplasm
cytoplasm:
Describe the rough ER
Describe the smooth ER
Describe the mitochondria
Describe the golgi complex
Describe the lysosome
Describe the peroxisome
What is the cellular function of Transportation? What are its key features?
Cellular Function of Transportation: Transportation in cells refers to the movement of substances across cell membranes to maintain homeostasis and facilitate cellular processes.
Key Features:
Passive Transport: Movement without energy (e.g., diffusion, osmosis).
Active Transport: Movement requiring energy (e.g., pumps, endocytosis).
Selectivity: Membranes regulate what enters/exits.
Transport Proteins: Assist in moving substances.
What is the cellular function of ingestion? What are its key features?
Cellular Function of Ingestion
Ingestion is the process by which cells take in nutrients and other substances from their environment.
Key Features
Nutrient Uptake: Cells absorb essential nutrients for energy and growth.
Endocytosis: Involves mechanisms like phagocytosis (cell eating) and pinocytosis (cell drinking).
Membrane Dynamics: Involves the alteration of the cell membrane to engulf materials.
Metabolic Processing: Ingested materials are processed for cellular metabolism and function.
What is the cellular function of secretion? What are its key features?
Secretion = extracellular release of prods
Secretion is the process by which cells produce and release substances to the external environment or into bodily fluids.
Key Features:
Types of Substances: Includes hormones, enzymes, neurotransmitters, and waste products.
Mechanisms: Can occur via exocytosis, where vesicles fuse with the plasma membrane.
Regulation: Controlled by various signals, including hormonal and neural stimuli.
Role in Homeostasis: Maintains balance in bodily functions and communication between cells.
What is the cellular function of respiration? What are its key features?
cellular respiration is a series of metabolic processes that transforms fuel molecs into energy (ATP) and waste products (CO2, H2O, heat)
glycolysis
breakdown of glucose to 2 ATP molecs
absence of oxygen (anaerobic)
insufficient to support energy needs of body
in cytosol
aerobic
citric acid / krebs cycle
in mitpo
produces additional 34 ATP molecs
What is the cellular function of communication? What are its key features?
Cellular communication is essential for coordinating activities within and between cells.
ligands and receptors work together to transduct signals
What is the cellular function of reproduction? What are its key features?
The cellular function of reproduction is to produce new cells, ensuring growth, repair, and maintenance of tissues.
proliferation and differentiation
What are the specialized functions in some cells? What are their key features?
Describe Hypertrophy: what it is, why, how is it different from normal?
hypertrophy is a cellular response to stress. it is when a cell increases in size due to hormone signaling or increase in workload.
Describe Metaplasia: what it is, why, how is it different from normal?
Metaplasia is the changing of one cell type to another in response to a persistent stressor
change to a cell better suited to environ
stressor removed → cells return to original type
may lead to pathogenic changes
Describe Atrophy: what it is, why, how is it different from normal?
Atrophy is a cellular response to stress which causes a decrease in size of a cell. this can be due to lack of movement, decrease O2 supply, nutritional deprivation, removal of hormone signals
Describe Hyperplasia: what it is, why, how is it different from normal?
hyperplasia is an increase in the # of cells in response to stress
Describe Dysplasia: what it is, why, how is it different from normal?
dysplasia is a change in cell size, shape, uniformity, arrangement, and structure in response to a stressor.
look abnormal under microscope
may return to normal or progress to cancer
Screening vs. Diagnosis
screening is the use of testing to sort out apparently well persons (asymptomatic) who probably have disease from those who probably do not. a goal of screening is to increase lead time.
Screening: done in preclinical phase, 2nd degree
Purpose: To identify individuals at risk for a condition.
Method: Often involves tests or questionnaires that are not definitive.
Example: Mammograms for breast cancer screening.
Diagnosis: clinical phase, 3rd degree
Purpose: To confirm the presence of a specific condition.
Method: Involves detailed tests and evaluations.
Example: Biopsy to diagnose cancer.
Lead time definition
Lead time is the interval by which the time of diagnosis is advanced by screening and early detection compared to usual time of diagnosis
Prevalence (point vs period)
prevalence = % of pop affected w disease for specified period
point prev = prev at specific point in time
period prev = prev over given period of time
Prev = (# of self reported cases in the study)/(# of persons in the study pop)
Incidence
% of specific pop thats newly affected w a disease in a given period of time
= (# ppl newly ill) / (# ppl at risk)
Define all-cause morality, group-specific mortality, and cause-specific morality
all cause = % of the pop that died during time period
group specific = % of pop of interest that died over period
cause specific = % of the pop that died due to a specific cause in period
Case fatality rate
the probability of dying from a disease, given that you have the disease
Proportionate mortality
% of total deaths that are due to a specific cause
What is the key criteria for screening programs?
importance / seriousness of outcome
alter natural history of disease
technically feasible
consider costs and benefits
acceptable to indiv and healthcare professional
recognized treatment
Describe USPSTF:
who are they?
what do they do and how do they do it?
What do their recommendations mean? (A, B, C, D, I)
US preventative services task force
the decision making body in the US that sets the guidelines for screening programs: who, when, where, how
indep panel of experts in primary care and prevention
systematically review the evidence
develops evidence based recommendations for clinical preventative services
pushed online and in peer reviewed medical journals
they review the evidence: benefits and harms of a preventative service in a primary care pop without symptoms
certainty and magnitude of net benefit
assignment of a letter grade
A - recommend service (high certainty of substancial net benefit)
B - recommend service (high certainty of moderate net benefit)
C - recommend selectively (moderate certainty small net benefit)
D - recommends against service / certainty of no net benefit
I - insufficient to assess → ?
Genetics vs. Genomics
genetics = study of single genes and their effects on health
9/10 top CODs have a genetic component
genomics = study of all the genes in the genome including their interactions (includes diseases with genetic and environmental contributions)
DNA
directs all cell activites
4 chem bases (AT/CG), double stranded phosphate backbone, bases connected via H bonds
intron vs exon
intron = noncoding portion of DNA, spliced out
exon = sections that code for proteins
Genes, chromosome, nucleosome
genes = discrete functional units, contain genetic code for protein synth, long stretches of DNA seq
chromosome = packaging unit for DNA, each chromo contains 1000s of genes, most cells in body are somatic
diploid = 46 chromos
22 pair + 2 sex chromos
nucelosome = a repeating unit of DNA that is wrapped around a core of proteins and is the fundamental building block of chromatin
Locus
locus = gene’s location on a chromosome
Autosome vs. Sex chromosome
Autosome vs. Sex Chromosome
Autosome:
Non-sex chromosomes.
Humans have 22 pairs of autosomes.
Involved in determining most traits.
Sex Chromosome:
Determine an individual's sex.
Humans have 1 pair (XX for females, XY for males).
Carry genes related to sexual development.
Diploid vs. Haploid
Diploid vs. Haploid
Diploid (2n):
46 chromos: 22 pair + 2 sex chromos
Contains two complete sets of chromosomes (one from each parent).
Found in somatic (body) cells.
Example: Human cells (46 chromosomes).
Haploid (n):
1 chromo of original pair, 22 autosomes, 1 sex chromo
Contains one complete set of chromosomes.
Found in gametes (sperm and egg cells).
Example: Human gametes (23 chromosomes).
Gametes
each have 23 chromos
hapoid
ova/sperm = products of meiosis by specialized cells in ovary or testes
meiosis = division that reduces the # of chromos in a parent cell by ½ and produces 4 gamete cells
Alleles
alleles are alternate forms of a gene, one allele on each paired chromo get one allele from each parent
homozygous = same allele from each parent
heterozygous = diff allele from each parent
Meiosis vs. Mitosis
Meiosis vs. Mitosis
Mitosis:
Purpose: Cell division for growth and repair.
Result: Two identical daughter cells (diploid).
Phases: One division (prophase, metaphase, anaphase, telophase).
Meiosis:
Purpose: Production of gametes (sperm and eggs).
Result: Four genetically diverse daughter cells (haploid).
Phases: Two divisions (Meiosis I and Meiosis II).
Key Differences:
Mitosis: Identical cells; Meiosis: Diverse cells.
Mitosis: One division; Meiosis: Two divisions.
Dominant vs. recessive vs. co-dominant
single gene traits
dominant = alleles that always produce their trait if present on either chromo
recessive = alleles that only produce trait if present on both chromos
co dom = alleles that both produce trait
Abnormal chromosome diseases
not inherited from a carrier parent
due to loss of chromo or extra chromo
loss of autosomal chromo = incompatible with life
karyotype = visual appearence of chromos
Congenital Diseases = present at birth or shortly after, not caused by genetic abnormalities, due to failure in development, cannot be transmitted to offspring
Describe gene disorders (???)
hereditary disorders: tracked via circle/square diagram
caused by inheriting defective genes that produce a defective protein or no proteins
clear understanding of inheritance patterns
Autosomal dominant pattern of inheritance
a. what are some gene applicable gene disorders?
single gene disorder
males and females affected equally
only need one parent
huntingtons, osteogenesis imperfect, marfan syndrome
Autosomal Recessive pattern of inheritance
a. what are some gene applicable gene disorders?
males and females equally affected
need 2 carriers
cystic fibrosis, PKU, sickle cell anemia
Sex Linked inheritance pattern
a. what are some gene applicable gene disorders?
x linked diseases more common bc X chromo is bigger
more common in males bc only one X chromo
color blindness, hemophilia, duchenne’s muscular dystrophy
Familial pattern of inheritance
a. what are some gene applicable gene disorders?
several diseases cluster in families, patterns not understood
can be multifactoral: several genes, shared environ
can use epidemiologic methods to estimate heritability
diabetes, allergies, epilepsy
Cancer
cancer = malignant tumor of potentially unlimited growth that expands locally by invasion and systematically by metastasis
cancer includes 100+ diff diseases
Malignant vs. benign
malignant = life threatening, rapid growth, invade surrounding tissue, may metastasize, irregular surfaces, cells dont resemble cells of origin, no uniform appearance, not encapsulated
prefix + carcinoma = of epithelial origin
prefix + sarcoma = of supportive tissue
benign = not life threatening, slow growth, remain local, wont metastasize smooth and symmetrical surface, look like cells of origin, uniform experience, encapsulated
tissue or origin + “oma”
Metastatic
metastasis = the development of secondary malignant growths
metastasize = spread to other sites in body via metastasis
Polyp
polyp = projects from an epithelial surface
cell or tissue or origin + “oma”
benign tumor
Carinogens
initiator (1) and promoter (2) of carcinogenesis
Carcinogenesis
carcinogenesis = the process of how cancer goes from normal to cancerous; uncontrolled cell division due to DNA mutations
Initiation = result of permanent genetic change due to a carcinogen (initiator)
Promotion = expansion of initiated cell by hyperproliferation in response to carcinogen
i. Altered apoptosis, tissue remodeling, and/or increaased inflammaion
Progression = stepwise transformation to malignancy, increased growth rate, invasiveness, metastasis and alteration in morphology
What are the stages of carcinogenesis? Describe them.
Initiation - needs a carcinogen to initiate
Promotion - needs a carcinogen to hyper proliferate
Progression - stepwise transformation to malignancy
What are the patterns of cancer trends? (geography, incidence, survival)
#2 COD in US
wide geo var in cancer incidence / mortality
What are the genes responsible for cell division? How do these lead to cancer?
The 4 types of genes that are responsible for cell division are Oncogenes, tumor suppressor genes, suicide genes, DNA repair genes
Oncogenes = tell cells when to divide
tumor suppressor genes = tell cells when not to divide
suicide genes = control apoptosis
dna repair genes = can cause cancer when they are mutated, which can lead to errors in DNA that cause cells to grow out of control
mutations can be inherited or acquired
Describe Oncogenes
mutated genes that can cause cancer by causing cells to grow and divide uncontrollably
Tumor Suppressor genes
genes that regulate cell growth and division to prevent cancer
represent the opposite side of cell growth control, normally acting to inhibit cell proliferation and tumor development
suicide genes
a gene that will cause a cell to kill itself through the process of apoptosis
DNA repair genes
genes that code for proteins which actively identify and fix damage to DNA within a cell
Describe the role of the immune system in cancer (???)
a. failure - (???)
b. immunosuppression - immunosuppressive meds are risk factor for cancer
c. infections - many infectious pathogens are risk factors for cancer
Describe the cancer prevention strategies
anti-initiation
alteration of carcinogen metabolism
removal of DNA reactive molecs: decrease phase 1 enzymes which damage dna thru oxidation and increase phase 2 enzymes which excrete carcinogens by reacting w free radicals (eat more antioxidants)
enhancement of DNA repair
anti-promotion/progression
scavenging electrophiles and free radicals, decreasing inflammation, suppressing proliferation (growth factors, estrogen), enhancing apoptosis, decreasing angiogenesis
behavioral factors
treatment
local = surgery, radiation therapy
systemic = chemo, hormone therapy, immunotherapy
can reduce cancer burden via prevention, screening, and treatment
stress vs stressor
stress = threat or percieved threat to homeostasis
stressor = agents or conditions that can produce stress and endanger homeostasis
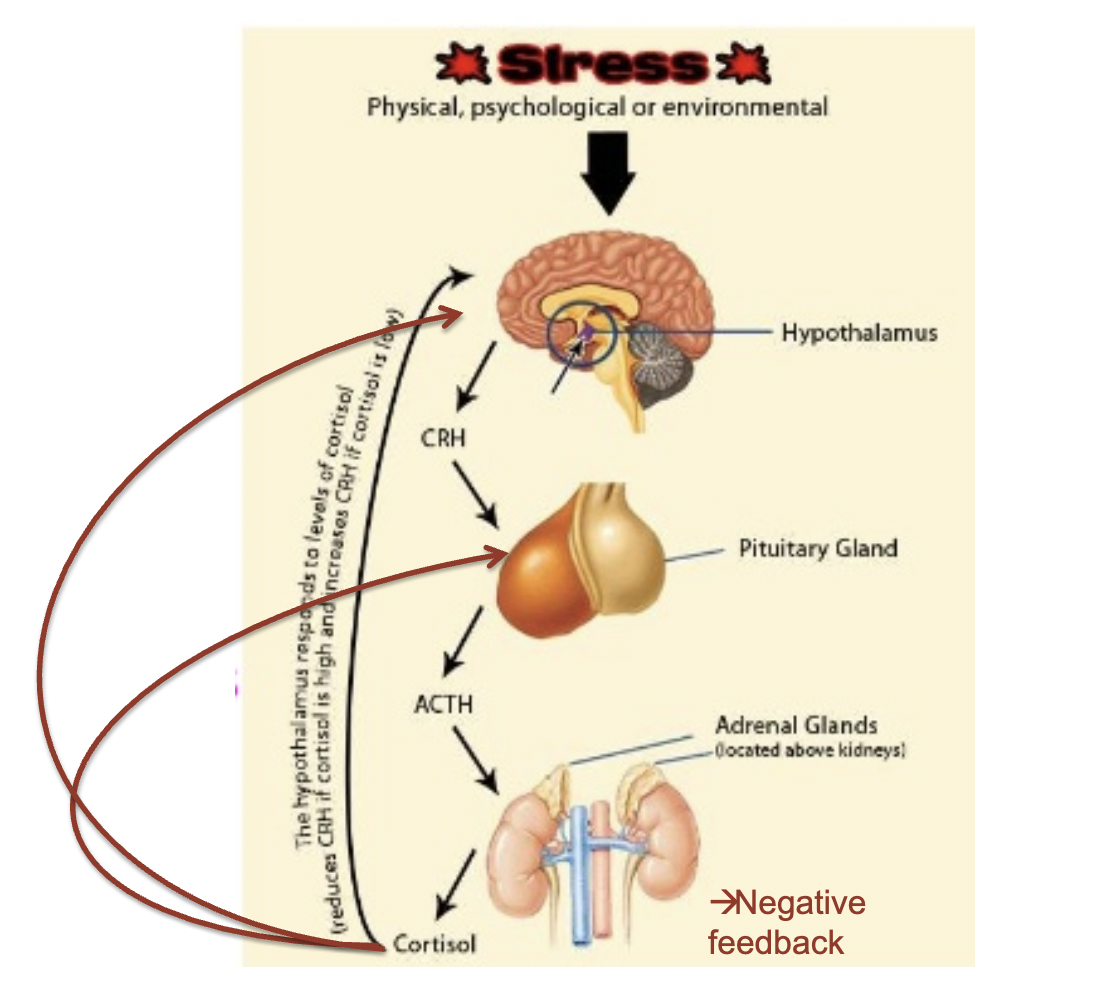
negative feedback
negative feedback causes the variable to change in a way that is opposite the initial change
most homeostatic mechs
initiating corrective mechs
involves input from nervous and endocrine systems (HPA axis)
goal to prevent sudden drastic change
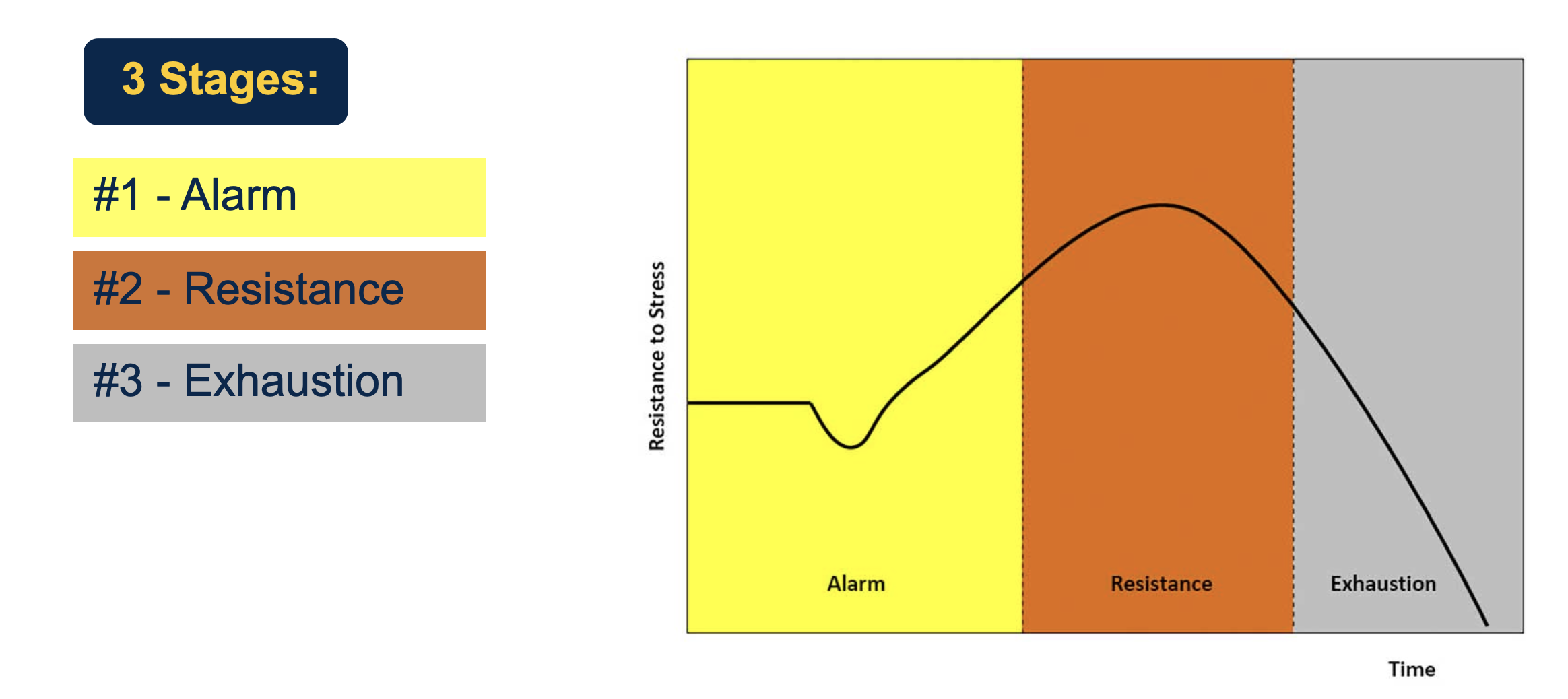
general adaptation syndrome - alarm, resistance, exhaustion stage
GAS = physiologic stages after response to stress
alarm stage: initial stages after stress exposure, fight/flight response
catecholamines and cortisol are released and other hormones are suppressed (growth, thyroid, reproductive)
resistance stage: body begins to repair itself after initial shock: chronic hypercortisolism and longterm hormone suppression is detrimental and ineffective
irritability, frustration, poor concentration
exhaustion stage: chronic stress results, energy depletion and weakened immune system, signif loss of homeostasis, fatigue, burnout, depression and anxiety
allostatic load
Allostatic load is the consequences of sustained or repeated activation of mediators of allostasis
leads to wear and tear and decreased efficiency of the system
our bodies are flexible; can slightly change set point in stress response
Adaptive functions - which are increased? decreased?
stress impacts adaptive functions
increases: vigilance, oxygenation, focused attention, nutrition to body
decreases: eating, growth, reproduction
Describe the homeostatic control mechanisms
stimuli = factor that changed in the persons environ
receptor = structure/organ that monitors changes in environ and sends info to the control center
control center = determines the set point for variable, analyzes info and coords response
effector = structure/organ that carries out response directed by control center
How do multiple effectors work?
multiple effectors allow stress system to achieve balance in multiple ways because the brain can utilize multiple effectors in response → more efficient and safeguard against failure of one effector
What is the role of the brain is responding to stress?
amygdala indentifies stressor
→ hypothalamus releases hormones to act on autonomic nervous system
→ secretes catecholamies / fight or flight response and activates HPA axis
HPA response / fight or flight
what signals
how the system can be shut down with negative feedback
stress → hypothalamus → CRH → pituitary gland → ACTH → adrenal gland → cortisol → neg feedback
Cortisol increases metabolism, vasoconstriction, anti inflammation, regulate blood glucose
catecholamines = also secreted from adrenal glands but as a neurologic response to receptive organs (can also have neg feedback on system)
CRH = corticotrophin releasing hormone
ACTH = adrenocorticotropic hormone
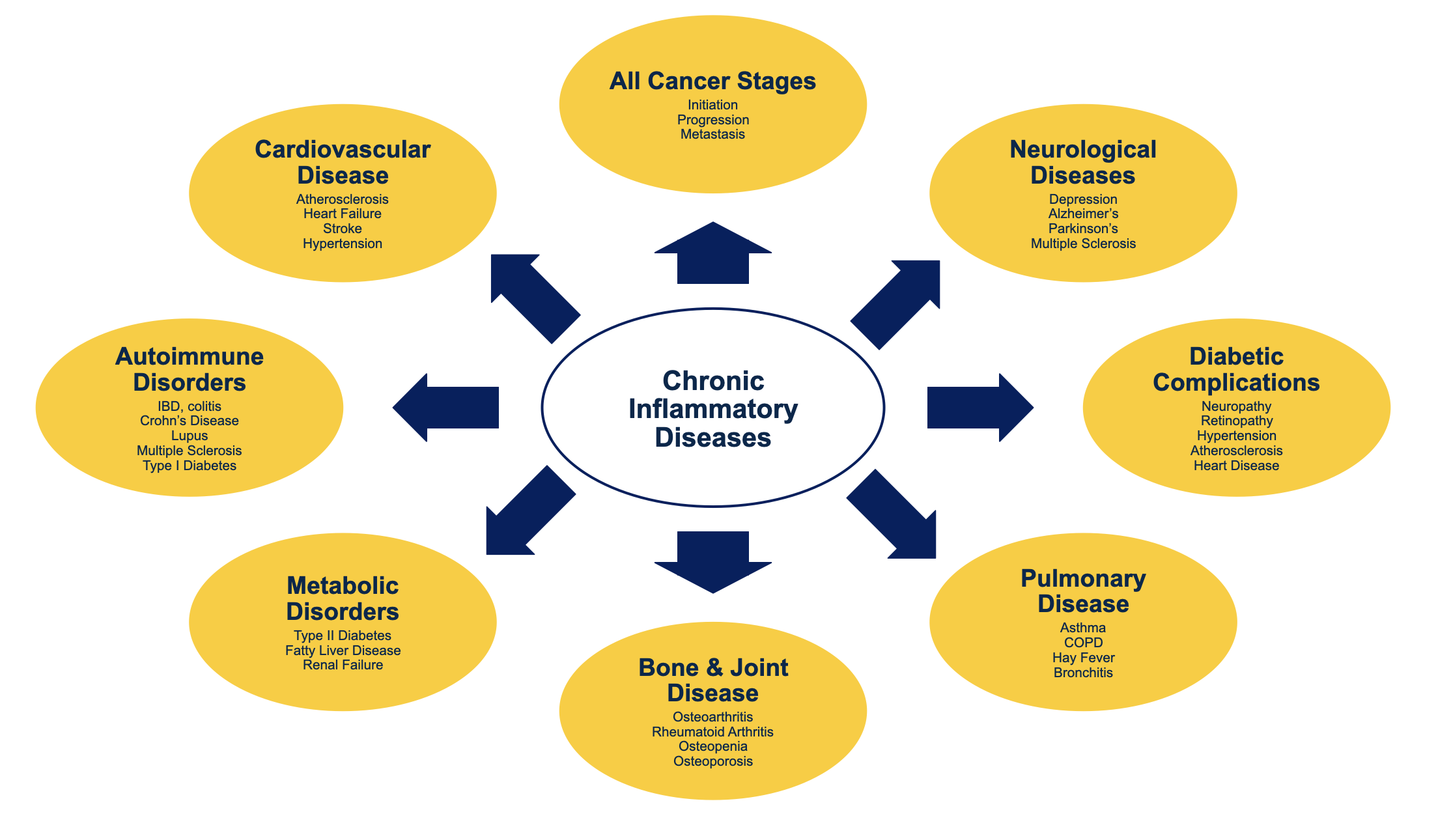
Acute vs. chronic inflammation
chronic inflammation = persistent or recurrent state of inflammation lasting several weeks or longer
results from unrelenting injury, persistent infectious process, prolonged exposure to toxic agent, autoimmune condition, obesity, aging, chronic illness consequences
acute inflamm response = expected body response to tissue injury, can be measured in hours/days
endogeneous vs. exogeneous
stimuli for acute inflammation
endogeneous = factors within the body that result in cellular/tissue injury
tissue necrosis, immune rxns
exogeneous = factors that invade/injure the body from the outside
inflammatory diseases (“-itis)
diseases characterized by inflammation of tissue or organ = arthritis (joints), colitis (colon), cystitis (bladder), otitis media (middle ear)
inflamm at core of many chronic conds
we should try to shut down the inflamm response
5 cardinal signs of inflammation
calor = heat
rubor = redness
dolor = pain
tumor = swelling
functio laesa = loss of function