SKELETAL ANAPHY
1/174
Earn XP
Description and Tags
FOR P TOW
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
175 Terms
Support
General Functions where the skeleton serves as the structural framework for the body by supporting soft tissues and providing attachment points for the tendons of most skeletal muscles.
Protection
General Function where the skeleton protects the most important internal organs from injury. For example, cranial bones protect the brain, and the rib cage protects the heart and lungs
Assistance in Movement
General Function where most skeletal muscles attach to bones; when they contract, they pull on bones to produce movement.
Mineral homeostasis (storage and release)
General Function where Bone tissue makes up about 18% of the weight of the human body. It stores several minerals, especially calcium and phosphorus, which contribute to the strength of bone. Bone tissue stores about 99% of the body’s calcium. On demand, bone releases minerals into the blood to maintain critical mineral balances (homeostasis) and to distribute the minerals to other parts of the body.
18%
How much does bone tissue makes up of the weight in the body?
99%
How much bone tissue stores in the body’s calcium
Blood Cell Production
General Function where within certain bones, a connective tissue called red bone marrow produces red blood cells, white blood cells, and platelets, a process called hemopoiesis. Red bone marrow consists of developing blood cells, adipocytes, fibroblasts, and macrophages within a network of reticular fibers. It is present in developing bones of the fetus and in some adult bones, such as the hip (pelvic) bones, ribs, sternum (breastbone), vertebrae (backbones), skull, and ends of the bones of the humerus (arm bone) and femur (thigh bone). In a newborn, all bone marrow is red and is involved in hemopoiesis. With increasing age, much of the bone marrow changes from red to yellow.
Hemopoiesis
A connective tissue called red bone marrow produces red blood cells, white blood cells, and platelets
Triglyceride storage
General function where Yellow bone marrow consists mainly of adipose cells, which store triglycerides. The stored triglycerides are a potential chemical energy reserve.
206
How many bones does an adult have (mostly paired)
Axial and Appendicular Skeleton
The divisions of the skeletal system
80
How much bone does an Axial Skeleton have?
126
How much bone does an Appendicular Skeleton have?
Axial Skeleton
80 bones that lie around the longitudinal axis of the human body. Makes up the trunk, back, neck, and head.
Appendicular Skeleton
126 bones. Forms the upper and lower limbs/extremities/appendages. Girdles connect the extremities to the axial skeleton.
8
How many bones does Cranium have?
14
How many bones does Face have?
1
How many bones does Hyoid bone have?
6
How many bones does the Auditory Ossicles have?
26
How many bones does the Vertebral column have?
1
How many bones does the sternum have?
24
How many bones does the Ribs have?
2
How many bones does Clavicle have?
2
How many bones does Scapula have?
2
How many bones does Humerus have?
2
How many bones does Ulna have?
2
How many bones does Radius have?
16
How many bones does Carpals have?
10
How many bones does Metacarpals have?
28
How many bones does Phalanges have?
2
Hip, pelvic, or coxal bone
2
How many bones does Femur have?
2
How many bones does Patella have?
2
How many bones does Fibula have?
2
How many bones does Tibia have?
14
How many bones does Tarsals have?
10
How many bones does Metatarsals have?
28
How many bones does Phalanges have?
Bone
A hard, dense connective tissue that forms most of the adult skeleton.
Extracellular Matrix
15% water, 30% collagen fibers, 55% crystalized mineral salts.
Calcium phosphate combines with calcium hydroxide to form crystals of hydroxyapatite
Calcification
crystallization and hardening of combined mineral salts in the framework formed by the collagen fibers of the extracellular matrix; initiated by osteoblasts.
Bone Hardness
crystallized inorganic salts
Bone Flexibility
collagen fibers
Osteoprogenitor Cells
Unspecialized bone stem cells derived from the mesenchyme (tissue from which almost all connective tissues are formed). Undergoes cell division to form osteoblasts. Found along the inner portion of the periosteum, in the endosteum, and in the canals within bone that contain blood vessels.
Osteoblast
Bone-building cells. They synthesize and secrete collagen fibers and other organic components needed to build the extracellular matrix of bone tissue, and they initiate calcification. As osteoblasts surround themselves with extracellular matrix, they become trapped in their secretions and become osteocytes.
Osteocytes
Mature bone cells; does not undergo cell division. Maintains the daily metabolism of the bone tissue e.g. exchange of nutrients and wastes with the blood.
Osteoclasts
Bone-resorption cells. A collection of monocytes that releases powerful lysosomal enzymes and acids that digest the protein and mineral components of the underlying extracellular bone matrix.
Long
Flat
Short
Irregular
Sesamoid
Classification of the bones
Long Bones
Typically longer than they are wide
Shaft with enlarged ends
Contain mostly compact bone; spongy bone at ends
Flat Bones
Thin, flattened, and usually curved
Two thin layers of compact bone sandwich a layer of spongy bone between them
Short Bones
Generally cube-shaped
Contain mostly spongy bone with an outer layer of compact bone
Irregular Bones
Irregular shape
Do not fit into other bone classification categories
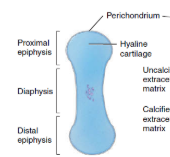
Diaphysis (shaft)
Makes up most of bone’s length
Composed of compact bone
Periosteum
Outside covering of the diaphysis
Fibrous connective tissue membrane
Perforating (Sharpey’s) fibers secure periosteum to underlying bone
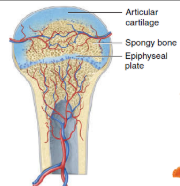
Epiphysis (ends)
Composed mostly of spongy bone enclosed by thin layer of compact bone
Articular Cartilage
Covers the external surface of the epiphyses
Made of hyaline cartilage
Decreases friction at joint surfaces
Epiphyseal line
Remnant of the epiphyseal plate
Seen in adult bones
Epiphyseal Plate
Flat plate of hyaline cartilage seen in young, growing bone
Causes lengthwise growth of a long bone
Periosteal Arteries
enter the diaphysis through Volkmann’s canals; supply the periosteum and outer part of compact bone
Nutrient Artery
enters through the nutrient foramen near the center of the diaphysis; divides into proximal and distal branches; supplies the inner part of compact bone tissue of the diaphysis and spongy bone tissue in the epiphyseal plates Enters through the nutrient foramen (a small opening in the diaphysis of long bones)
Nutrient Foramen
a small opening in the diaphysis of long bones
Metaphyseal arteries
enter the metaphyses of a long bone; supplies the red bone marrow and bone tissue of the metaphyses
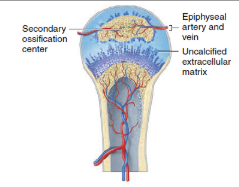
Epiphyseal arteries
enter the epiphyses of a long bone; supplies the red bone marrow and bone tissue of the epiphyses.
Sensory (Afferent) Nerves:
Found mostly in the periosteum
Responsible for pain sensation (especially in fractures or periostitis)
Autonomic (Sympathetic) Nerves:
Regulate blood flow in bone marrow and vessels
Influence bone metabolism and blood pressure regulation
The initial formation of bones in an embryo and fetus;
The growth of bones during infancy, childhood, and adolescence until their adult sizes are reached;
The remodeling of bone (replacement of old bone by new bone tissue throughout life); and
The repair of fractures (breaks in bones) throughout life
Bone formation occurs in four principal situations
Patterns of ossification in embryo and fetus
Intramembranous ossification
Endochondral ossification
Development of the ossification center
Specific chemical messages cause the cells of the mesenchyme to cluster together and differentiate, first into osteoprogenitor cells and then into osteoblasts. Osteoblasts secrete the organic extracellular matrix of bone until they are surrounded by it.
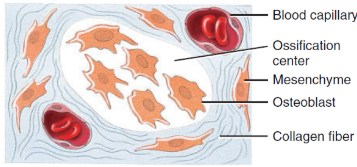
Calcification
The secretion of extracellular matrix stops, and the cells, now called osteocytes, lie in lacunae and extend their narrow cytoplasmic processes into canaliculi that radiate in all directions. Within a few days, calcium and other mineral salts are deposited and the extracellular matrix hardens or calcifies (calcification).
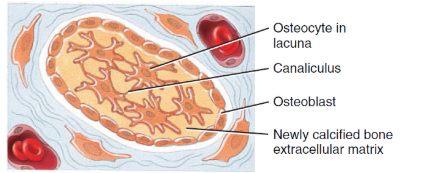
Formation of trabeculae
As the bone extracellular matrix forms, it develops into trabeculae that fuse with one another to form spongy bone around the network of blood vessels in the tissue. Connective tissue associated with the blood vessels in the trabeculae differentiates into red bone marrow.
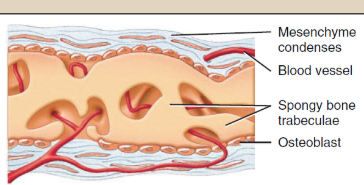
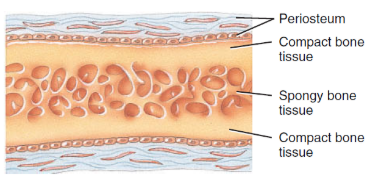
Development of the periosteum
The mesenchyme condenses at the periphery of the bone and develops into the periosteum. Eventually, a thin layer of compact bone replaces the surface layers of the spongy bone, but spongy bone remains in the center. Much of the newly formed bone is remodeled (destroyed and reformed) as the bone is transformed into its adult size and shape.
Endochondral Ossification
Occurs in long bones
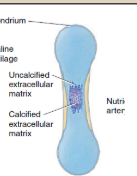
Development of the cartilage model
Specific chemical messages cause the cells in mesenchyme to crowd together in the general shape of the future bone, and then develop into chondroblasts. The chondroblasts secrete cartilage extracellular matrix, producing a cartilage model consisting of hyaline cartilage
Growth of the cartilage model
Once chondroblasts become deeply buried in the cartilage extracellular matrix, they are called chondrocytes. The cartilage model grows in length by continual cell division of chondrocytes, accompanied by further secretion of the cartilage extracellular matrix. As the cartilage model continues to grow, chondrocytes in its midregion hypertrophy (increase in size) and the surrounding cartilage extracellular matrix begins to calcify.
Lacunae
As these chondrocytes die, the spaces left behind by dead chondrocytes merge into small cavities called
Interstitial/Endogenous growth
Growth from within; increase in length.
Appositional/Exogenous growth
Growth at the outer; increase in thickness. Due to deposition of extracellular matrix material on the cartilage surface of the model by new chondroblasts that develop from the perichondrium.
Development of the primary ossification center
Primary ossification proceeds inward from the external surface of the bone. A nutrient artery penetrates the perichondrium and the calcifying cartilage model through a nutrient foramen in the midregion of the cartilage model, stimulating osteoprogenitor cells in the perichondrium to differentiate into osteoblasts. Once the perichondrium starts to form bone, it is known as the periosteum. Near the middle of the model, periosteal capillaries grow into the disintegrating calcified cartilage, inducing growth of a primary ossification center, a region where bone tissue will replace most of the cartilage. Osteoblasts then begin to deposit bone extracellular matrix over the remnants of calcified cartilage, forming spongy bone trabeculae. Primary ossification spreads from this central location toward both ends of the cartilage model
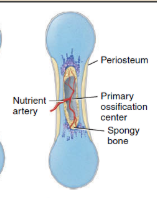
periosteum
Once the perichondrium starts to form bone, it is known as the
Development of the medullary (marrow) cavity
As the primary ossification center grows toward the ends of the bone, osteoclasts break down some of the newly formed spongy bone trabeculae. This activity leaves a cavity, the medullary (marrow) cavity, in the diaphysis (shaft). Eventually, most of the wall of the diaphysis is replaced by compact bone.
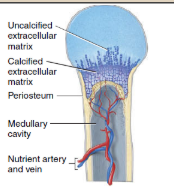
Development of the secondary ossification centers
When branches of the epiphyseal artery enter the epiphyses, secondary ossification centers develop, usually around the time of birth. Bone formation is similar to what occurs in primary ossification centers. However, in the secondary ossification centers spongy bone remains in the interior of the epiphyses (no medullary cavities are formed here). In contrast to primary ossification, secondary ossification proceeds outward from the center of the epiphysis toward the outer surface of the bone.
Formation of articular cartilage and the epiphyseal (growth) plate
The hyaline cartilage that covers the epiphyses becomes the articular cartilage. Prior to adulthood, hyaline cartilage remains between the diaphysis and epiphysis as the epiphyseal (growth) plate, the region responsible for the lengthwise growth of long bone
The epiphyseal (growth) plate
Is a layer of hyaline cartilage in the metaphysis of a growing bone that consists of four zones
Zone of resting cartilage
This layer is nearest the epiphysis and consists of small, scattered chondrocytes. The term “resting” is used because the cells do not function in bone growth. Rather, they anchor the epiphyseal plate to the epiphysis of the bone.
Acts like a "base camp" of quiet cartilage cells, just holding the growth plate in place.
Zone of proliferating cartilage
Slightly larger chondrocytes in this zone are arranged like stacks of coins. These chondrocytes undergo interstitial growth as they divide and secrete extracellular matrix. The chondrocytes in this zone divide to replace those that die at the diaphyseal side of the epiphyseal plate.
This is the "growth zone" where cartilage cells multiply and make the bone longer.
Zone of hypertrophic cartilage
This layer consists of large, maturing chondrocytes arranged in columns. Here, cartilage cells get bigger, preparing for the next stage.
Zone of calcified cartilage
The final zone of the epiphyseal plate is only a few cells thick and consists mostly of chondrocytes that are dead because the extracellular matrix around them has calcified. Osteoclasts dissolve the calcified cartilage, and osteoblasts and capillaries from the diaphysis invade the area. The osteoblasts lay down bone extracellular matrix, replacing the calcified cartilage by the process of endochondral ossification. As a result, the zone of calcified cartilage becomes the “new diaphysis” that is firmly cemented to the rest of the diaphysis of the bone.
Cartilage dies, hardens, and is replaced by new bone—this is where bone is built.
Bone Remodelling
The ongoing replacement of old bone tissue by new bone tissue
Bone resorption
removal of mineral and collagen fibers by osteoclasts
Bone deposition
addition of minerals and collagen fibers by osteoblasts
5%
percentage of total bone mass in the body is being remodeled
4% per year
Renewal rate for compact bone
20% per year
Renewal rate for spongy bone
Vitamin A
Vitamin that stimulates osteoblast activity
Vitamin C
Vitamin that stimulates collagen synthesis
Vitamin D
Vitamin that increases calcium absorption from foods in the Gi tract to the blood