Rehab Essentials Part 4 & 5: General and Local Anesthesia
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
What is the goal of general anesthesia?
Absence of all perceived sensations
What is the purpose of general anesthesia?
Allow detailed surgical procedures with minimal harm to patient
How was anesthesia before 1846?
1. Unconsciousness from strangulation or blow to head
2. Drugs for pain (alcohol, opium)
What happened in 1846 at Mass General?
First use of ether as anesthesia; led to development of safer, less toxic drugs
What are the requirements of general anesthesia? (5)
1. Loss of consciousness; perceived sensations
2. Amnesia
3. Inhibition of reflexes
4. Skeletal muscle relaxation
5. Safe, transient, predictable
What are the stages of general anesthesia?
1. Analgesia (not enough)
2. Excitement/delirium (bad)
3. Surgical anesthesia (desirable)
4. Medullary paralysis (bad)
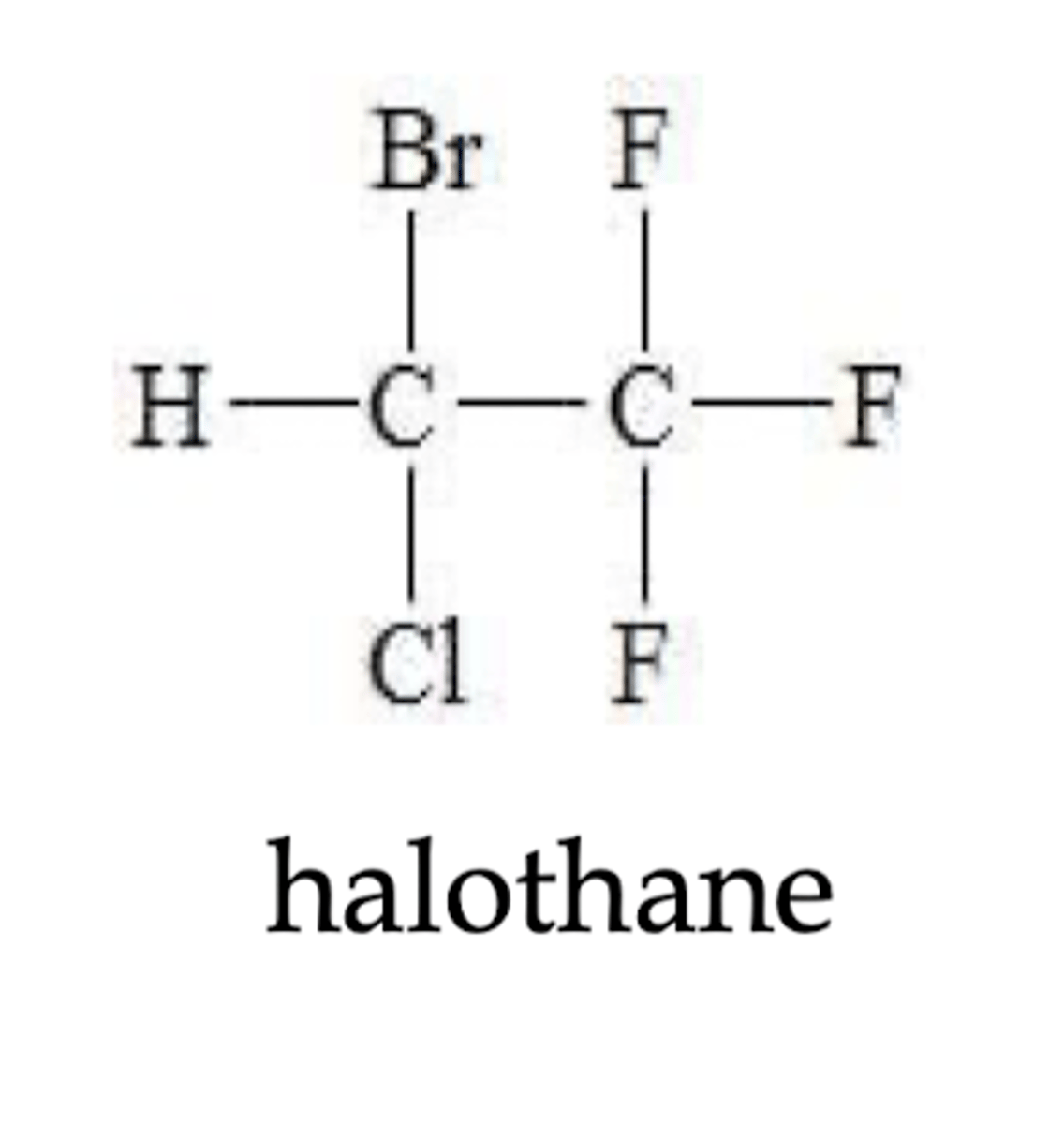
What are some inhalation agents of general anesthetics?
1. Halogenated liquids
2. Nitrous oxide
3. Other gases
What are some IV agents of general anesthetics?
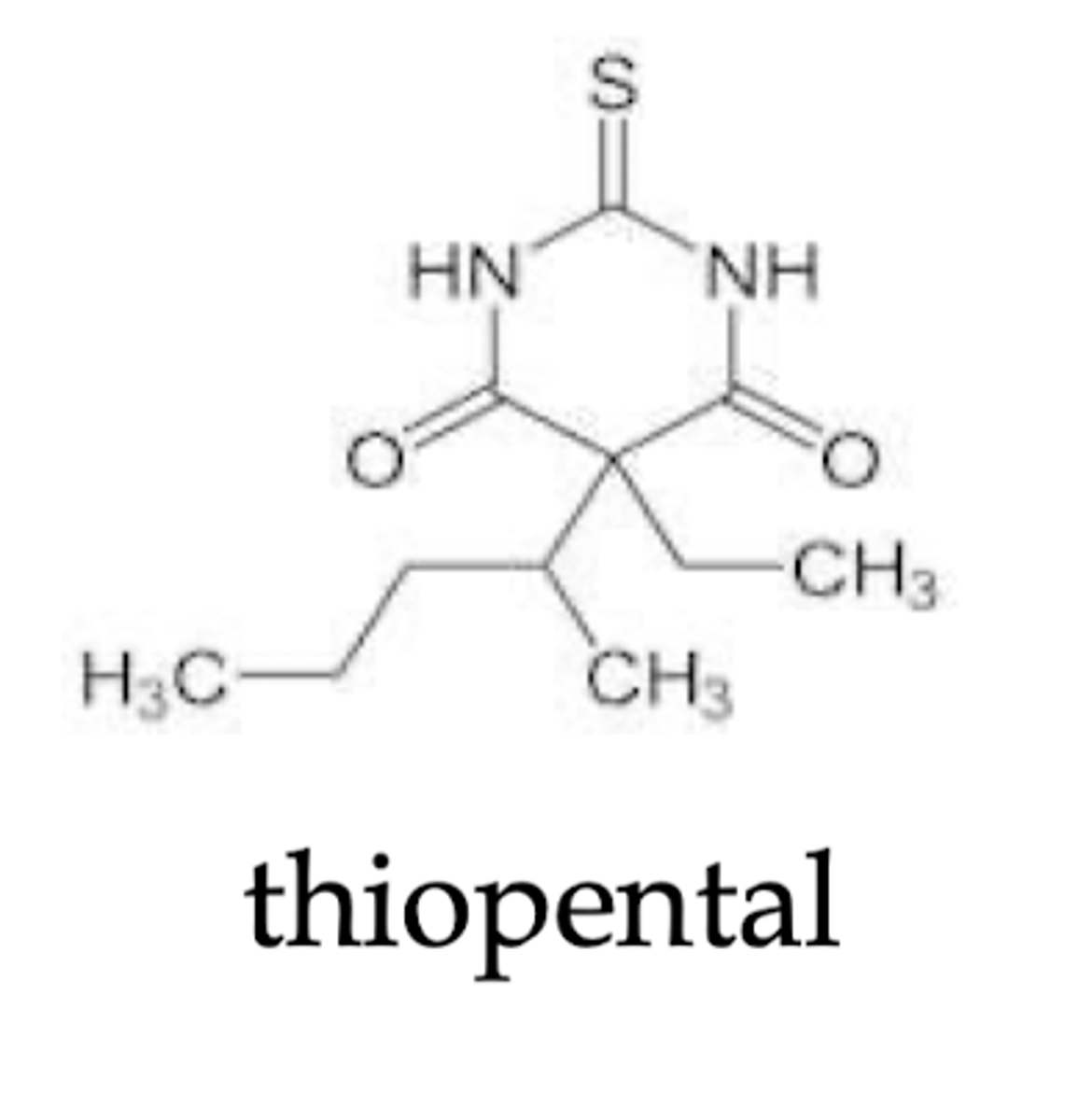
1. Barbiturates
2. Benzos
3. Opioids
Why would you use an injected anesthetic?
Take effect quickly, but more difficult to control level of anesthesia after injection
Why would you use an inhaled anesthetic?
Take effect more slowly, but easier to control level of anesthesia
How should general anesthesia be administered?
A small dose of the anesthetic can be injected IV to produce anesthesia very quickly, then the patient can be switched over to an inhaled agent to allow better control of surgery
What are the protocols of general anesthesia?
1. Start w/ small dose of injected to get patient under quickly
2. Switch to inhaled agent for duration of procedure
3. Start to withdraw inhaled agent ASAP
4.
What do contemporary general anesthesia use to provide "balanced" anesthesia?
2 or more agents
How can balanced anesthesia be created?
With a combination of injected (ex. thiopental), inhaled (ex. halothane), and of other drugs before, during, after surgery (but depends on length of surgery, and med status)
What is the mechanism of action for general anesthetics?
Increase inhibition or decrease excitaiton throughout the CNS
How do general anesthetics increase inhibition or decrease excitation thorughout the CNS?
1. Direct effect on lipid bylayer
2. Direct effect on neuronal receptors (ex. GABA, opioid receptors)
3. Combination of lipid and receptor effects
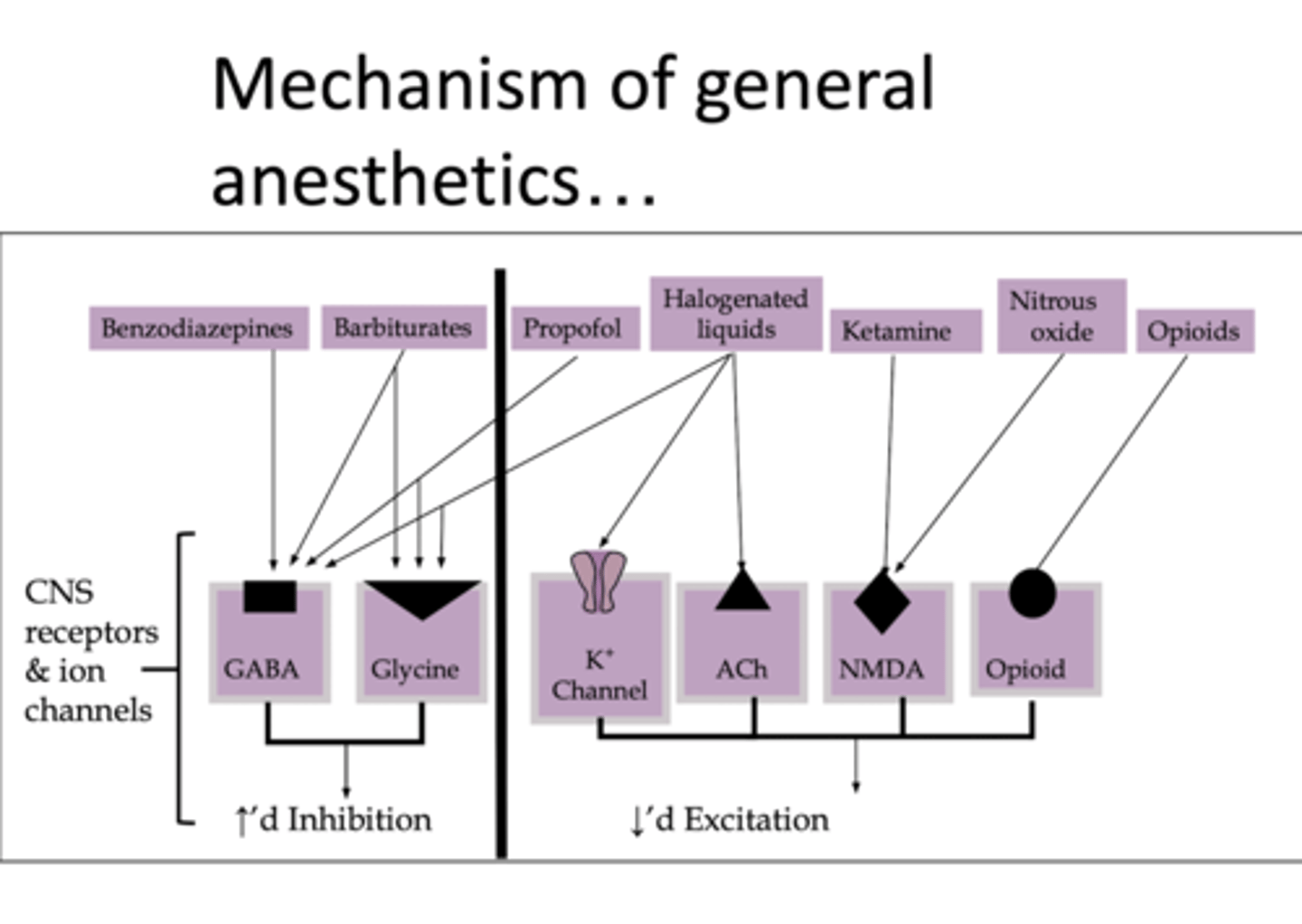
Which CNS receptors and ion channels increase inhibition?
1. GABA
2. Glycine
Which CNS receptors and ion channels decrease excitation?
1. K+ channel
2. ACh
3. NMDA
4. Opioid
Why are several drugs given pre-op or post op for anesthesia?
1. To relax and sedate patients prior to surgery
2. Reduce post-op nausea and vomiting
3. Reduce other problems related to anesthesia
What are neuromuscular junction blockers used to do?
Paralyze skeletal muscles to facilitate positioning on table, prevent spasms, and allow easier mechanical ventilation
What are the types of NMJ blockers?
1. Depolarizing (don't let it repolarize)
2. Nondepolarizing
What are examples of depolarizing NMJ blockers?
Succinylcholine
What are examples of nondepolarizing NMJ blockers?
1. Tubocurarine
2. Rocuronium
How long are effects of NMJ bockers?
Short duration of action; effects usually last a few minutes or so
What can NMJ blockers cause post-op?
Muscle soreness (esp. succinylcholine)
What may some patients lack in terms of NMJ blockers?
Metabolizing enzymes, so they remain paralyzed at end of surgery
What is the next step if patient remains paralyzed after surgery?
Effects can be reverse somewhat with cholinesterase inhibitors (neostigmine, edrophronium) or sugammadex (inactivates rocuronium, vecuronium)
What is dissocitive anesthesia?
Patient may remain conscious but indifferent to surroundings (dissociation)
How is dissociative anesthesia achieved?
By use of ketamine or combination of antipsychotic (droperidol) with opioid (fentanyl)
When is dissociative anesthesia useful?
In diagnostic/radiologic procedures, dressing changes, emergency surgeries
What are common residual effects of general anesthesia? (5)
1. Muscle soreness from NMJ blocker, prlonged/immobile position on operating table
2. Chills, shivering
3. Nausea, vomiting
4. Sore throat
5. Cognitive effects
What are short term cognitive effects of general anesthesia?
Confusion, lethargy quite common due to redistribution of anesthesia comvined with pain meds
What kinds of patients may long-term effects of general anesthesia on cognition/intellect occur in?
Older adults and patients with comorbities (heart failure, parkinsonism, Alzheimer disease)
What are rehabilitation concerns with general anesthetics? (2)
1. Use in burn debridement, dressing changes, etc
2. Dealing with residual effect (ex. muscle soreness, respiratory hygiene, confusion, altered cognition)
What can be given before or after surgery to increase patient comfort?
Sedatives, analgesics, or anxiolytics
What is the goal of local anesthesia?
Interrupt nerve conduction at site of application
What is the purpose of local anesthesia?
Prevent or relieve pain without loss of consciousness or systemic effects
What are typical local anesthetics?
"-caine" drugs: lidocaine, procaine, bupivicaine, etc.
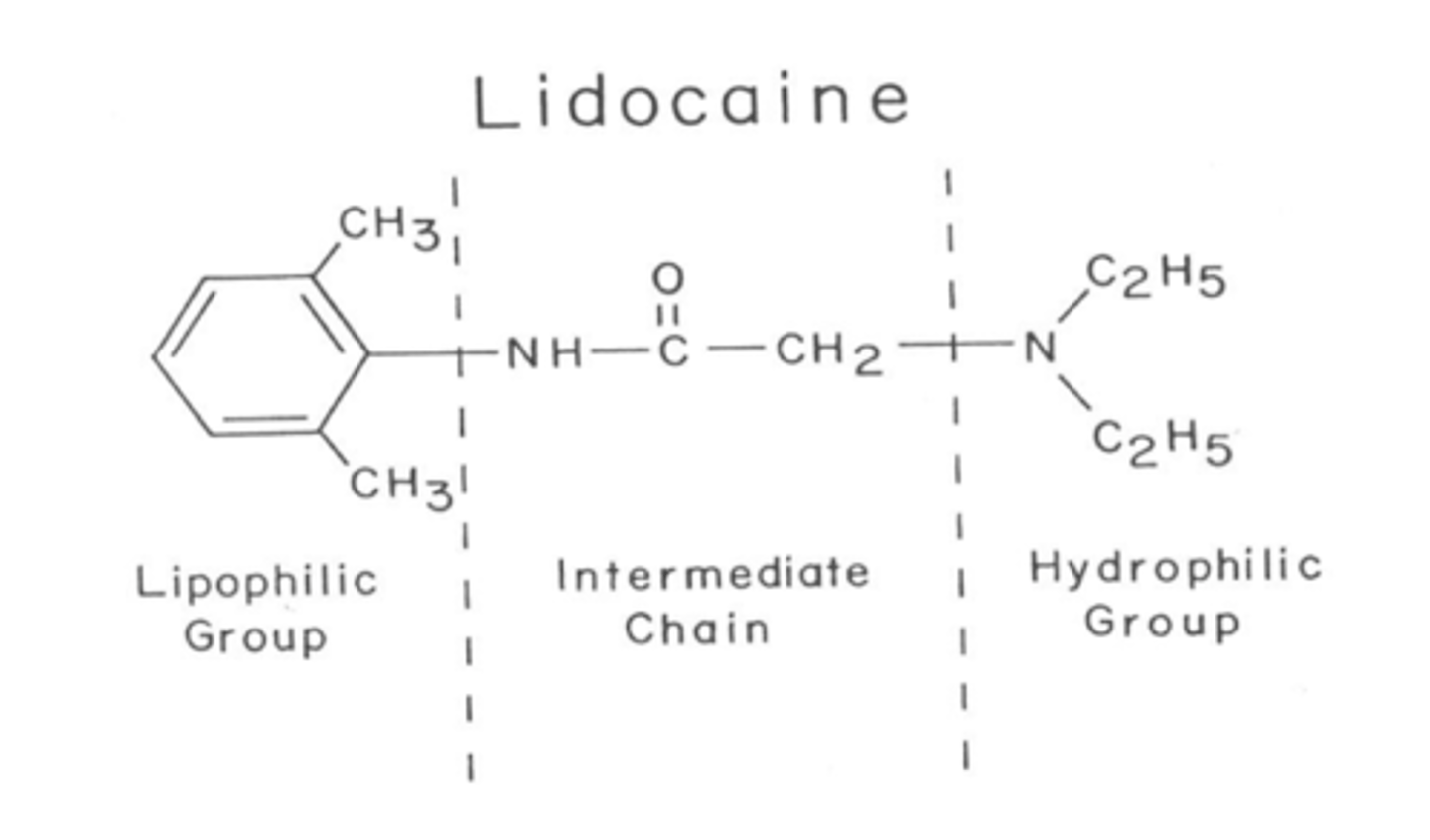
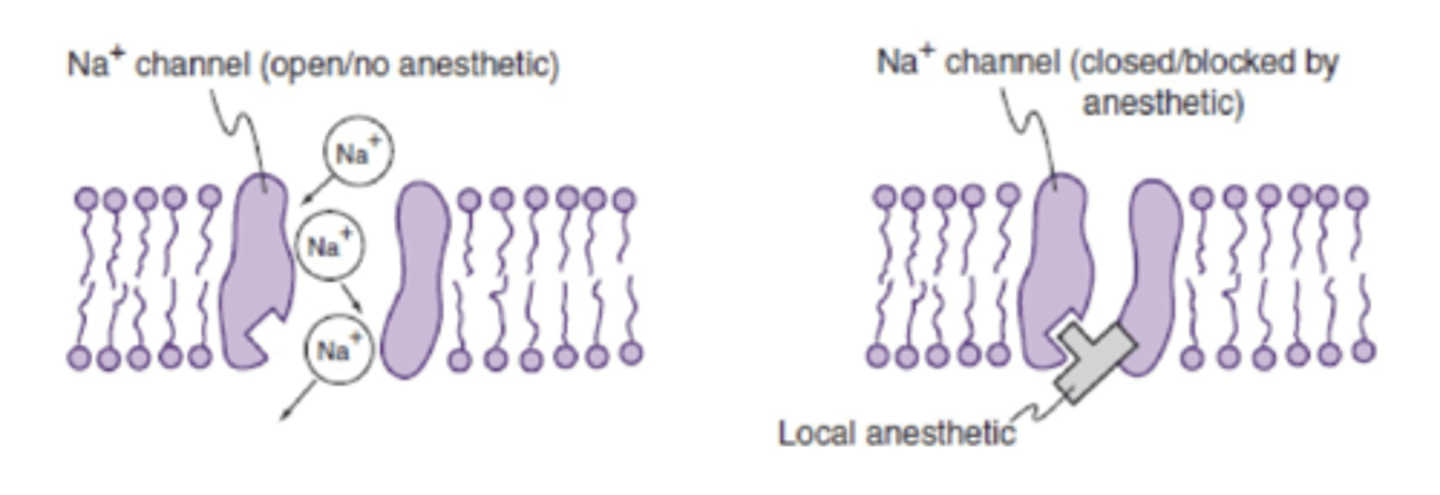
What is the mechanism of local anesthetics? (2)
1. Bind to sodium (Na+) channels in nerve membrane
2. Inactivate Na+ channel; prevent action potential conduction
What is the clinical use and administration of local anesthetic?
1. Topical
2. Transdermal
3. Infiltration
4. Nerve block
5. Spinal/epidural block
6. Sympathetic block
7. Intravenous regional anesthesia
How is topical anesthetic applied?
To surface of skin
What is topical anesthetic used for?
1. Pain relief
2. Minor burns
3. Abrasions
4. Prior to injection, IV insertion
5. Spasticity?
How does transdermal anesthesia work?
Movement through skin enhanced by: electricity (iontophoresis) or ultrasound (phonophoresis)

Should heat be applied to a transdermal patch?
No, this could increase absorption and result in systemic toxicity
What could increased entry of lidocaine into the blood stream cause?
Harmful systemic effects on the heart and brain
How does infiltration anesthetic work?
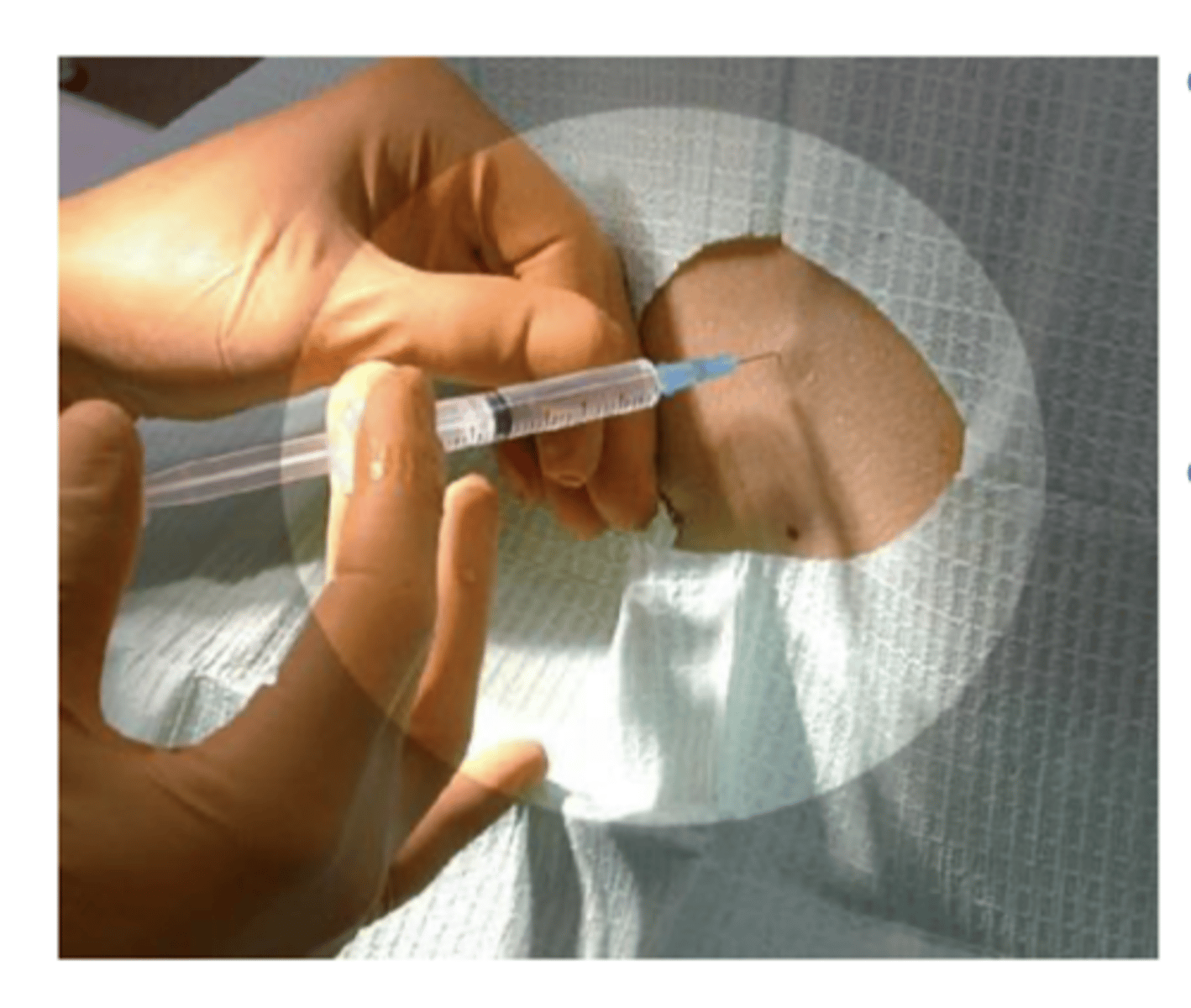
Injected subcutaneously to penetrate/infiltrate into selected area
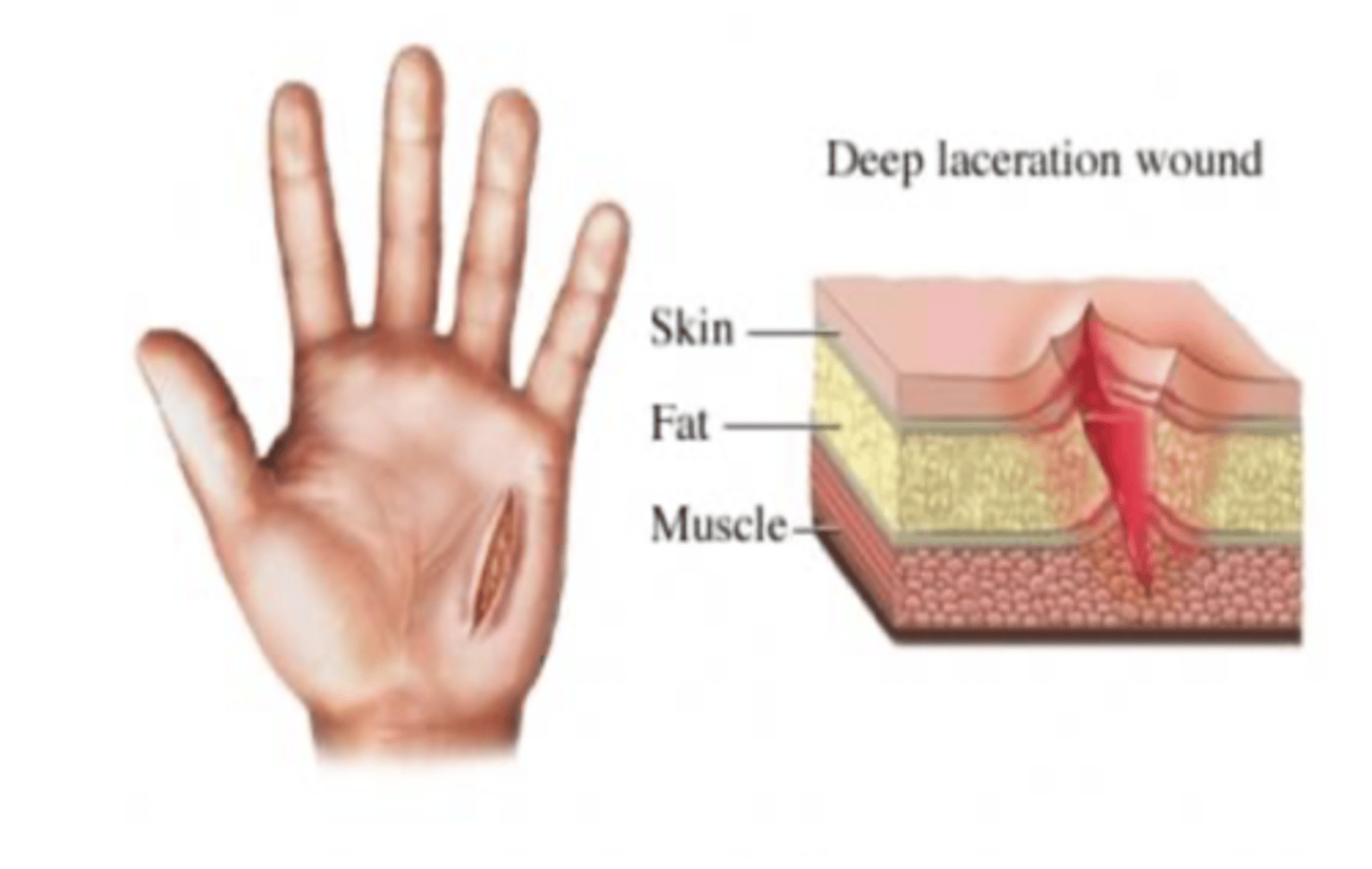
When is infiltration anesthetic commonly used?
Before suturing wounds
Where is a peripheral nerve block injected?
Close to nerve or nerve plexus
When are peripheral nerve blocks used?
Dental procedures, or other minor surgeries
What type of local anesthetic would you use to decrease minor skin irritation?
Topically
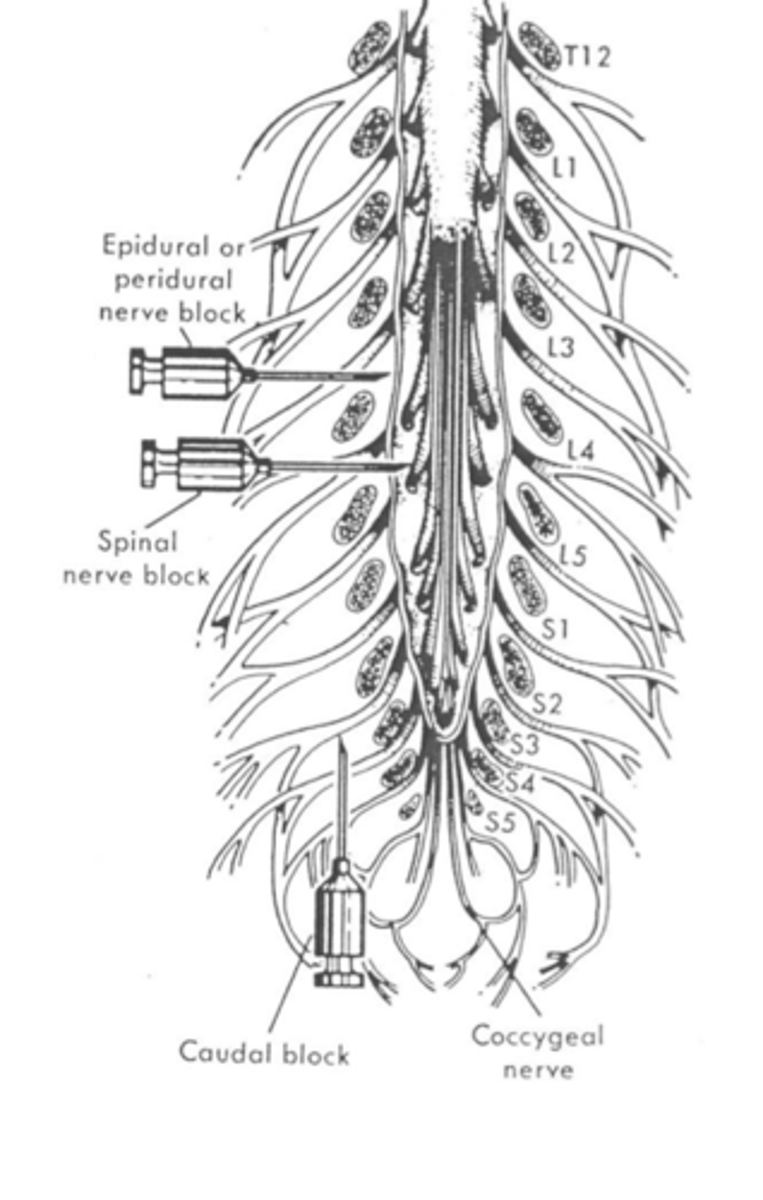
What is an epidural block?
Administration outside of dura
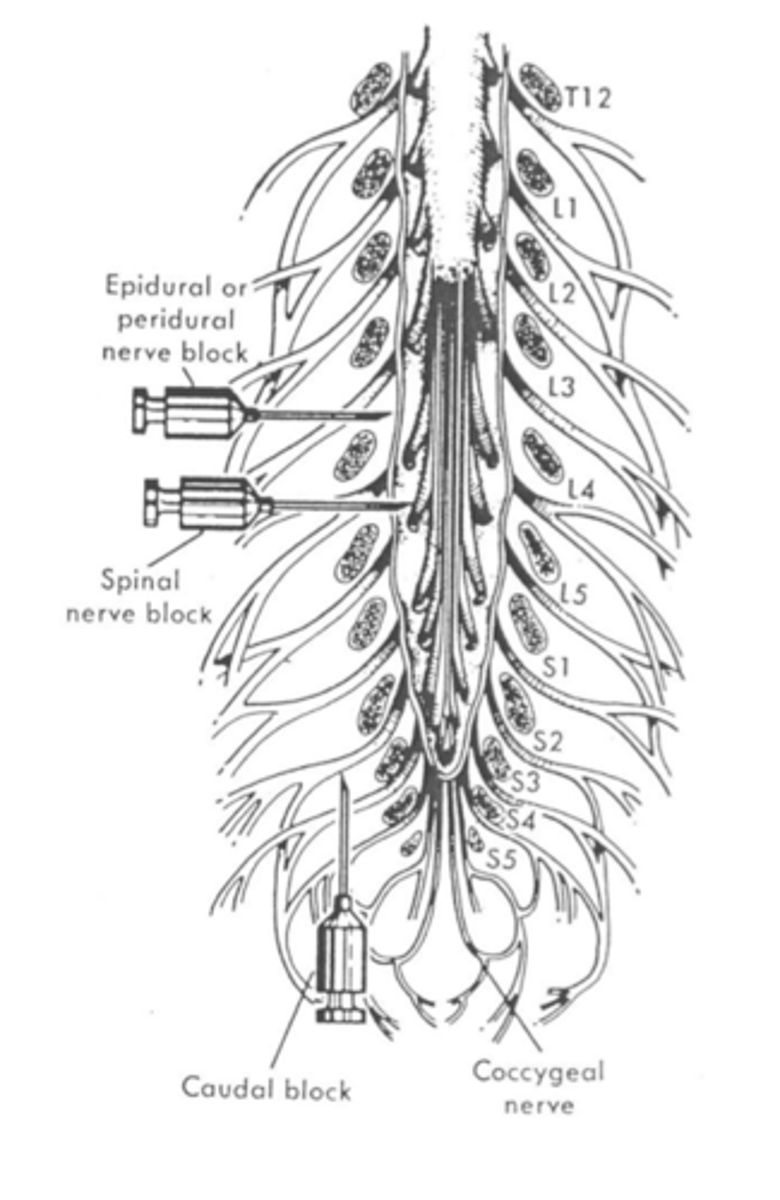
What is a spinal block?
Administration into subarachnoid space
What is a sympathetic block?
Decreases output from sympathetic nervous system to a certain part of the body
Where is a sympathetic block inserted near for the UE?
Stellate ganglion
Where is a sympathetic block inserted near for LE?
L4, L5 chain ganglia
What is an example of intravenous regional anesthetia?
Bier block
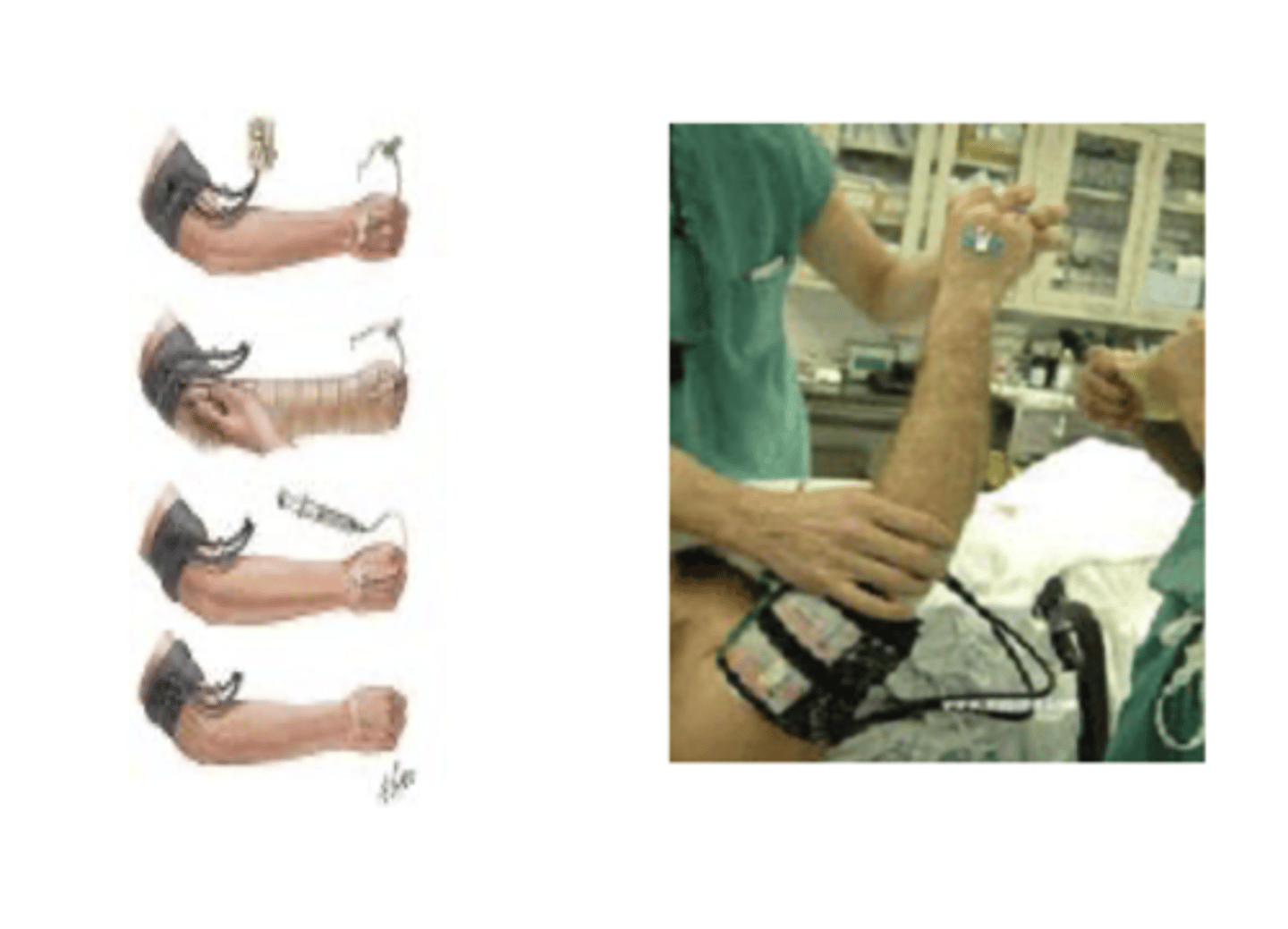
What is an intravenous regional anesthesia?
Local anesthetic directly into venous system (tendon repairs, ligament repairs)
How is a tourniquet used for intravenous regional anesthesia?
It's placed proximally to keep drug in limb
What is an intravenous regional anesthesia used for?
Some surgical procedures to treat CRPS/RSDS
What is a continous nerve block?
Small catheter is implanted near peripheral nerve to a specific region
How does a continous nerve block work?
Local anethetic dripped slowly/continously onto nerve
How is the efficacy of a continous nerve block?
Excellent post-op pain control
What are negative aspects of a continuous nerve block?
Loss of sensation, motor function, proprioception when nerve block is in effect
What is an example of a continuous nerve block?
Catheter inserted near femoral nerve for post op pain control after knee TKA

How should you determine if there are any residual effects after a continous nerve block?
Testing local sensation and muscle strength; systemic effects should also be rules out in case any local anesthetic has accumulated in blood stream
What are some possible residual systemic effects of a continuous nerve block?
1. Cardiac palpitations
2. Numbness in other tissues
3. Bladder dysfunction
What fibers are affected first in a differential nerve block?
Smallest, unmyelinated (pain, temp)
What fibers are affected last in a differential nerve block?
Largest, myelinated (proprioception, motor function)
What is the typical order of functional loss of a differential nerve block?
1. Pain
2. Temp
3. Touch
4. Proprioception
5. Motor
What are implications of local anesthetics for PT?
1. Transdermal administation for tx of pain via ionto- & phonophoresis
2. Use in RSDS/CRPS; or other acute and chronic conditions
3. Be alert for possible absorption Into systemic circulation...can cause "local anesthetic systemic toxicity" LAST
What is LAST characterized by?
1. CNS toxicity
2. Cardiotoxicity
What are signs of LAST CNS toxicity?
1. Ringing/buzzing in ears (tinnitus)
2. Agitation, restlessness, seizures
3. Decreased sensation in tongue and mouth, areas of skin
4. Later stages: CNS depression including resp depression and failure
What are signs of LAST cardiotoxicity?
1. Changes in HR (bradycardia)
2. Other ECG abnormalities
3. Clinical signs of cardiac depression (fatigue, dizziness)
4. Cardiac arrest
Where can local anesthetics be injected?
1. Near spinal cord
2. Near sympathetic ganglia
3. IV into a peripheral limb to decrease sensation in larger areas of the body