Trauma Care After Resuscitation (TCAR) ALL MODULES COMBINED QUESTIONS BANK WITH EXPERT SOLUTIONS + RATIONALES(DIAGRAMS INCLUDED)
1/1729
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
1730 Terms
Trauma Scope & Impact
-Most frequent cause of childhood disability
-50,000 children acquire permanent disabilities yearly
-Most common are TBIs
Common Pedi Trauma Etiologies
Motor Vehicles
-over 460,000 U.S. children injured each year
-3,000 deaths
Falls
-most frequent cause
Firearms
-leading cause of childhood death
-63% homicides; 30% suicides
Field Triage: Red Criteria
Injury Patterns
- Penetrating injuries to head, neck, torse
- Skull deformities
- Suspected spinal, pelvic, fractures
-Active bleeding
Mental Status & Vitals Signs
- GCS <6
- Pulse Ox <90%
Field Triage: Yellow Criteria
Mechanism of Injury
- High-risk auto crash
- Partial/Complete ejection
- Death in passenger compartment
EMS Judgement
- anticoagulant use
- suspicion of child abuse
Trauma Center Classifications
Level I:
- full range of specialist available 24/7
- trauma residency program
Level II:
- comprehensive trauma care
- 24 hr availability of essential personnel
Level III:
- resources for emergency resuscitation
- general surgeon promptly available
Level IV:
- initial evaluation, stabilization, and diagnostic capabilities
Trauma Care Implications: Child Size
Due to different sizes IV fluid rates, blood product volumes, and medications are weight-based
urine output measured in mL/kg
Evaluate hemorrhage as a percentage of child's normal circulating volume rather than total milliliters of blood lost
Multisystem injury highly likely in peds
Pediatric Anatomic & Physiologic Difference: Cardiovascular
-Presume tachycardia is due to hypovolemia
-When their circulating blood volume is low, compensation is easier through tachycardia and vasoconstriction
-Maintain normal systolic blood pressure until more than 25-30% of circulating blood volume is lost
-Tachycardia is earliest indicator of hypovolemia
Pediatric Anatomic & Physiologic Difference: Respiratory
-In children ribs and weak intercostal muscles limit chest expansion, makes breathing less effective
-Higher chances of atelectasis, pneumonia, and respiratory failure
-High susceptibility to barotrauma from overinflation
-in small kids with no visible neck, tracheal deviation and jugular vein distention cannot be adequately assessed
Pediatric Anatomic & Physiologic Difference: Spinal Cord
-Large heads and weak neck muscles predispose to high c-spine injuries
-Most infant c-spine occur at C1-C2
Pediatric Anatomic & Physiologic Difference: Brain
-Due to lower BP at baseline, young children sustain fewer epidural hematomas than do older kids
-More likely to experience injuries that produce generalized edema such as contusions, anoxic damage, and diffuse axonal injuries
-Children have greater degree of neuroplasticity which allows non-injured areas of brain to compensate
Pediatric Anatomic & Physiologic Difference: Abdominal
-Asplenic children and those with severe spleen injuries require prophylactic antibiotics for at least one year after injury
-Lap belt injuries: bruising, redness, and abrasions across abdomen requires evaluation for intra-abdominal lower thoracic and lumbar injuires
Pediatric Anatomic & Physiologic Difference: Urine Output
-Children less than age 2 are unable to efficiently concentrate urine due to immature renal responses; continue to excrete urine even when hypovolemic
-Normal Infant Urine Output (1-2 mL/kg/hr)
-Young children urine output (1-1.5 mL/kg/hr)
-Adult urine output (0.5-1 mL/kg/hr)
Pediatric Anatomic & Physiologic Difference: Glycemic Control
-Limited glycogen stores and can quickly become hypoglycemic
Pediatric Anatomic & Physiologic Difference: Musculoskeletal
-higher chances of incomplete fractures as bones are softer and springier
-pulmonary contusions blossom over time (12-72 hours after injury). Anticipate onset of progressive ventilatory compromise in hours and days post injury
-
Calculation of pediatric drug doses and fluid bolus volumes
Calculated by weight or length
Broselow tape: reliable way to identify appropriate medication doses in an emergency
Trauma
Event or circumstance resulting in physical, emotional, and/or life-threatening harm that has lasting adverse effects on the individual's mental, physical, and emotional health and social and/or spiritual well-being
What is the Trauma Process?
1. Event
-Single Event
-Chronic
-Complex
2. Experience
-Positive Stress
-Tolerable Stress
-Toxic Stress
3. Effect
-Activation of the HPA axis
-Emotional regulation disturbances
-Hyperarousal
-Problem-solving and executive function impacts
-Impaired attachments and social skills
-Gene expression alteration
HPA Axis
Interaction between the nervous and endocrine systems to produce the body's response to stress. Elevated levels of one of these hormones may lead to depression
Why use the TIC Approach?
-Minimize potentially harmful traumatic experience, encourage positive coping, provide emotional support
-Improve therapy outcomes and process
-Improve health outcomes
OT Value and Role in TIC
-Knowledge of therapeutic interventions
-Focus on meaningful activities
-Evidence-based practice skills
-Understanding of environmental context
-Serve individuals, families, and communities
-Serve clients across the lifespan
TIC-OT Model
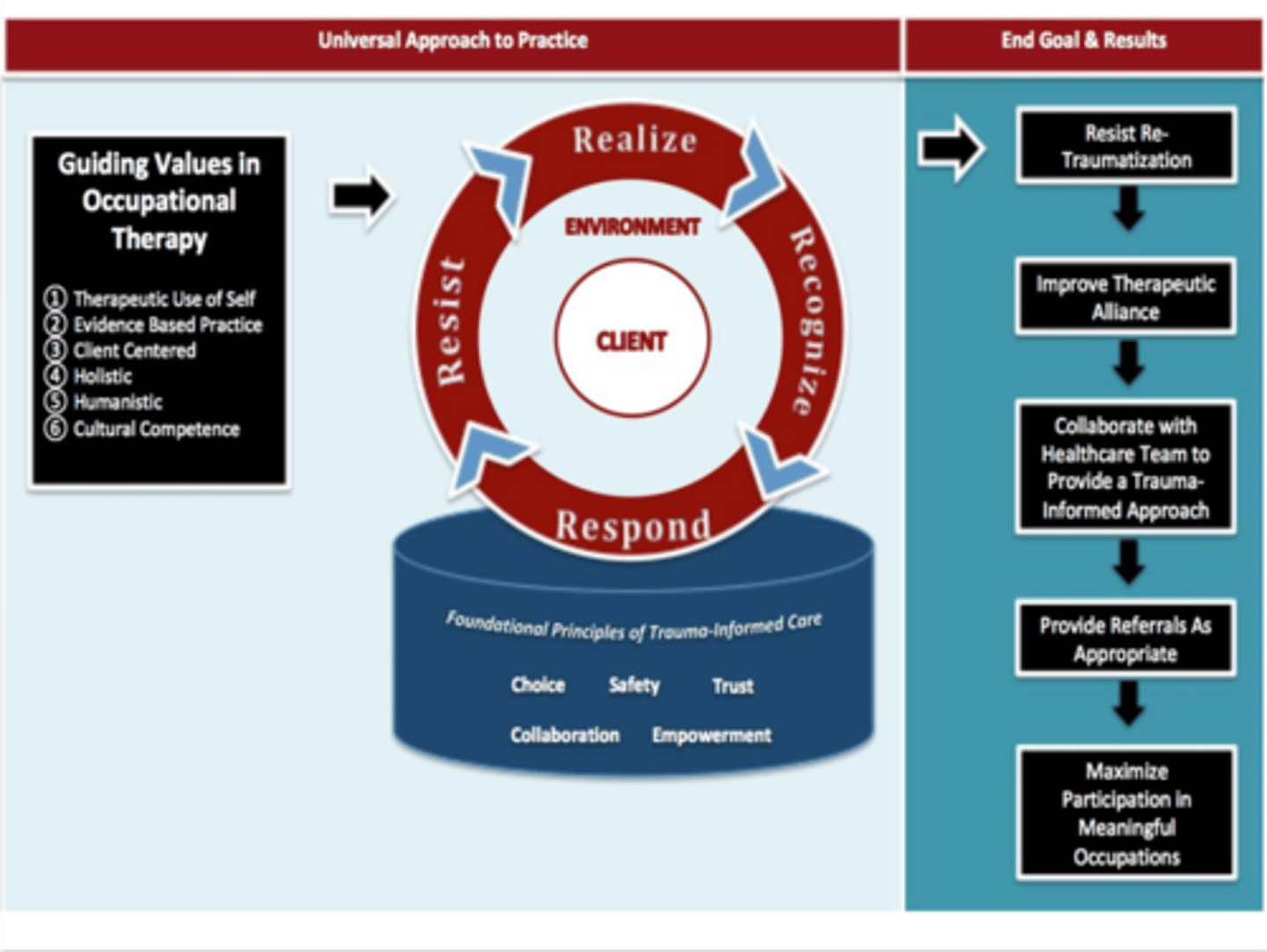
What are the guiding values of OT?
-Therapeutic Use of Self
-Evidence-Based Practice
-Holistic
-Humanistic
-Client Centered
-Cultural Competence
Therapeutic Use of Self
-Use empathy when working with client, family, and team
-Collaborate
-Build hope
-Build therapeutic alliance and trust
-Be aware of your verbal and non-verbal cues
-Help grow client's self-worth
-Respond to crisis points appropriately
Evidence-Based Practice
Use evidence for assessment and intervention
Holistic
-Include all domains of the individual in the assessment and intervention
-Allow flexibility in intervention
Humanistic
Support advocacy for needs
Client-Centered
-Client is the expert
-Encourage problem-solving
-Collaborate and offer choices
-Interventions reflect client's beliefs
Cultural Competence
-Respect cultural differences
-Be aware of cultural considerations
-Different cultures may require different therapeutic styles
-Recognize personal cultural biases and impact on therapeutic relationship
What are the Foundational Principles of TIC
1. Safety- physical and psychological security
2. Trust- strengthen therapeutic alliance with truth, reliability, and predictability
3. Choice- allow the client to have control of life by making decisions when faced with possibilities
4. Collaboration- client as a partner with shared power
5. Empowerment- encourage client to accomplish tasks of their own autonomy, encourage strength, and increase self-image
Safety- physical and psychological security
-Provide therapy in a safe and secure setting
-Ensure patient confidentiality
-Offer to address physiological needs
-Avoid shame inducing conversations/situations
-Ask before touching client
-Provide a safe place for client to express anger/frustrations without judgement
Trust- strengthen therapeutic alliance with truth, reliability, and predictability
-Use of Therapeutic Use of Self
-Follow through with what is said or promised
-Be transparent in therapy expectations and results
-Provide a vivid explanation of assessment and intervention
Choice- allow the client to have control of life by making decisions when faced with possibilities
-Have the client choose where, how, and when they will receive services, if possible
-Offer choices of interventions
-Offer choices ofthe order of activities during therapy
Collaboration- client as a partner with shared power
-Work with the client and family to set goals
-Work with the client and family to problem solve problems
-View and treat client as the expert in their understanding of themselves
-Encourage client feedback before, during and after
Empowerment- encourage client to accomplish tasks of their own autonomy, encourage strength, and increase self-image
-Encourage self-advocacy
-Identify and acknowledge strengths of the client
-Praise client for success in therapy
-Set realistic goals and acknowledge when they are met or need to be adjusted
Person-Environment Interaction
Community
-Connect with community supports to improve social and financial supports
-Reduce environmental stressors in the community as much as possible
-Refer client to other supports in the community
-Assist in prevention of future trauma by connecting to community support
Home/Family
-Educate household members about effects of trauma and how to limit future trauma
-Include siblings/caregivers
-Train/educate parents on effective parenting styles
School/Work
-Educate teachers and/or employers about the effects of trauma
-Support teachers and employers in adapting the environment to best meet the client's needs
What are the Four R's of TIC?
-Realize
-Recognize
-Respond
-Resist
Realize
Realize the prevalence of trauma and impact on health and well-being
-Observe escalated emotions/behaviors through trauma-informed lens
-Attend training on trauma-informed care in practice setting or community
Recognize
Recognize the presence of trauma and trauma's effect on occupation
-Advocate for the healthcare team to routinely screen/assess for trauma
-Interpret assessment results with trauma-informed lens
Respond
Respond appropriately by adapting approach to interacting with the client and communicate with the team effectively
-Provide emotional support and coping resources
-Emphasize continuity of care and collaboration among providers
-Refer to appropriate services
-Provide intervention as appropriate if trauma is impacting occupational participation
Resist
Resist Re-Traumatization
-Minimize potential triggers such as self-care activities, touching without asking, standing in close proximity
-Respond to trauma disclosures appropriately
End Goals and Results
-Resist Re-Traumatization
-Improve Therapeutic Alliance
-Collaborate with Healthcare team to provide trauma informed approach
-Provide referrals as appropriate
-Maximize participation in meaningful occupations
differential ddx: VINDICATED MEN
Vascular / Vessels
Infection
Neoplasm
Drugs & Diet (a.k.a. ingestions)
Idiopathic
Congenital
Autoimmune & Allergic
Trauma & Treatment SEs (a.k.a. idiopathic)
Endocrine (a.k.a. metabolic)
Deficiencies & Excesses
Musculoskeletal disorders
Environmental exposures
Neuropsychiatric disorders (a.k.a. neurologic, psychiatric)
differential ddx: VITAMINS ABCDEK
Vascular
Infectious / Inflammatory
Trauma / Toxic
Autoimmune
Metabolic
Iatrogenic / Idiopathic
Neoplastic
Social (e.g. child abuse, social deprivation)
Alcohol
Behavioral (psychosomatic)
Congenital
Degenerative / Drug
Endocrine / Exocrine
Karyotype (a.k.a. genetics)
ddx strategies: symptom complexes
ddx strategies: local anatomic approach
ddx strategies: systems approach
ddx strategies: mechanism approach
gross motor development: newborn
- limbs flexed, symmetrical pattern
- marked head lag on pulling up
gross motor development: 6 - 8 weeks
raises head to 45 degrees in prone position ("tummy time")
gross motor development: 6 - 8 months
sits without support (initially with a round back, the eventually with a straight back by 8 months)
By what age should infants be able to sit without support?
9 months
gross motor development: 8 - 9 months
crawling
gross motor development: 10 months
- stands independently
- cruises around furniture
gross motor development: 12 months
walks unsteadily (broad gait with hands apart)
By what age should infants be able to walk independently, even if unsteadily?
18 months
gross motor development: 15 months
walks steadily
gross motor development: 2.5 years
runs & jumps
vision & fine motor development: 6 weeks
follows moving object or face by turning the head (fixing & following)
By what age should an infant be fixing & following objects & faces?
3 months
vision & fine motor development: 4 months
reaches out for toys
By what age should infants be reaching out for toys?
6 months
When should an infant develop their palmar grasp?
4 - 6 months
vision & fine motor development: 7 months
transfers toys from one hand to another
By what age should infants be able to transfer toys from one hand to another?
9 months
When should an infant develop a mature pincer grip?
10 months
limit age: 12 months
vision & fine motor development: 16 - 18 months
makes marks with crayons
brick building: 14 months - 4 years
tower of three: 18 months
tower of six: 2 years
tower of eight or a train with four bricks: 2.5 years
bridge (from a model): 3 years
steps (after demonstration): 4 years
pencil skills: 2 - 5 years
drawn without seeing how it's done; copying can be done 6 months earlier
line: 2 years
circle: 3 years
cross: 3.5 years
square: 4 years
triangle: 5 years
hearing, speech & language development: newborn
startles to loud noises
hearing, speech & language development: 3 - 4 months
- vocalizes alone or when spoken to
- coos & laughs: aa, aa”
hearing, speech & language development: 7 months
- turns to soft sounds out of sight
- polysyllabic babble: “babababa, lalalalala”
Infants use sounds indiscriminately starting at _____ months & discriminately to parents at _____ months.
7, 10 (“Dada, Mama”)
hearing, speech & language development: 12 months
- two to three words other than "Dada" or "Mama"
- understands name “Drink”
hearing, speech & language development: 18 months
- 6 - 10 words
- is able to show two parts of the body (e.g. asking “Where is your nose?” & infant will point)
hearing, speech & language development: 20 - 24 months
joins two or more words to make simple phrases (e.g. “Give me teddy”)
hearing, speech & language development: 2.5 - 3 years
- talks constantly in 3 – 4-word sentences
- understands 2 joined commands (e.g. “Push me fast Daddy”)
social, emotional & behavioral development: 6 weeks
smiles responsively
By what age should infants smile responsively?
8 weeks
social, emotional & behavioral development: 6 - 8 months
puts food in their mouth
social, emotional & behavioral development: 10 - 12 months
- waves bye-bye
- plays peek-a-boo
social, emotional & behavioral development: 12 months
drinks from a cup with two hands
social, emotional & behavioral development: 18 months
holds spoon and gets food safely to mouth
social, emotional & behavioral development: 18 - 24 months
symbolic play
By what age should infants be engaging in symbolic play?
2 - 2.5 years
social, emotional & behavioral development: 2 years
- toilet training: dry by day
- pulls off some clothing
social, emotional & behavioral development: 2.5 - 3 years
- parallel play
- interactive play evolving
- takes turns
Shock
hypoperfusion= inadequate tissue perfusion
Aerobic metabolism
cell metabolism with O2
Anaerobic metabolism
cell metabolism without O2
Inadequate Volume (Hypovulimia)
loss of blood, loss of plasma
Inadequate Pumping
traumatic injury, heart attack, heart failure, obstruction
Inadequate Vessel Tone
Vessel Tone →systemic vascular resistance, BP= CO x SVR
Hypovolemic shock
inadequate volume (ex. burns, hemorrhage, dehydration)
Distributive shock
inadequate vessel tone (vasodilation and capillary permeability)
Neurogenic shock
caused by spinal cord trauma→lose sympathetic NS Signals→decreased heart rate and vasodilation→decreased CO and BP→decreased perfusion
Anaphylactic shock
extreme allergic reaction→systemic vasodilation and increase cap permeability →relative hypovolemia→decrease perfusion (swelling and constriction)
Psychogenic shock
fainting
Septic shock
exaggerated/systemic response to infection →systemic vasodilation and increase cap permeability→relative hypovolemia→decreased perfusion
Cardiogenic shock
inadequate pumping (ex. AMI, CHF, Dysrhythmia, cardiac meds, cardiac contusion)
Obstructive shock
inadequate pumping or blockage of flow (ex. Pulmonary embolism, Tension pneumothorax, Pericardial tamponade)